
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 April 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1142299
This article is part of the Research Topic Reviews in Preventative Health for Stroke and Education to Stroke Prevention View all 6 articles
Background: The estimated lifetime risk of stroke was the highest in East Asia worldwide, especially in China. Antihypertensive therapy can significantly reduce stroke mortality. However, blood pressure control is poor. Medication adherence is a barrier as patients’ out-of-pocket costs have risen. We aimed to take advantage of a free hypertension pharmacy intervention and quantified the impact on stroke mortality.
Methods: A free pharmaceutical intervention program was implemented in Deqing, Zhejiang province in April 2018. Another non-pharmaceutical intervention, social distancing due to the pandemic of Coronavirus disease 2019 (COVID-19), was also key to affecting stroke mortality. We retrospectively collected the routine surveillance data of stroke deaths from Huzhou Municipal Center for Disease Prevention and Control in 2013–2020 and obtained within-city mobility data from Baidu Migration in 2019–2020, then we quantified the effects of both pharmaceutical intervention and social distancing using Serfling regression model.
Results: Compared to the predicted number, the actual number of stroke deaths was significantly lower by 10% (95% CI, 6–15%; p < 0.001) from April 2018 to December 2020 in Deqing. Specifically, there was a reduction of 19% (95% CI, 10–28%; p < 0.001) in 2018. Moreover, we observed a 5% (95% CI, −4 – 14%; p = 0.28) increase in stroke mortality due to the adverse effect of COVID-19 but it wasn’t statistically significant.
Conclusion: Free hypertension pharmacy program has great potential to prevent considerable stroke deaths. In the future, the free supply of low-cost, essential medications that target patients with hypertension at increased risk of stroke could be taken into account in formulating public health policies and guiding allocations of health care resources.
Stroke remains the leading cause of mortality and morbidity worldwide (1). The estimated lifetime risk of stroke was the highest in East Asia, with China facing the greatest challenges especially (2, 3). The risk factors for stroke are high systolic blood pressure, smoking, diabetes, and lack of physical activity (3, 4). High systolic blood pressure accounted for 2.54 million deaths in 2017 in China, of which 95.7% were due to cardiovascular diseases (CVD) (3). Growing evidence suggests pharmacological blood pressure lowering for primary and secondary prevention of CVD across different levels of blood pressure is cost-effective (5, 6). Earlier clinical trials in Chinese Older Adult people confirmed that active systolic antihypertensive therapy can significantly reduce the mortality and morbidity of stroke in hypertensive patients (7, 8).
Prescription medications have experienced many years of growth in costs, and as deductibles and co-pays have risen, so have patient out-of-pocket costs (9). It is hypothesized that higher costs can lead to potentially harmful changes in patient behavior, including taking lower doses than recommended or discontinuing beneficial medications (10). If medication adherence is a barrier, blood pressure will not be significantly reduced, nor will downstream cerebrovascular health (11, 12). The 2018 China Chronic Disease and Risk Factor Surveillance (CCDRFS) study showed that only one-third of Chinese hypertensive patients received antihypertensive treatment, and of those receiving treatment, 11% had blood pressure effectively controlled (13). While results of cross-sectional analyses from the National Health and Nutrition Examination Survey (NHANES) showed that the hypertension treatment was higher than 50% among US adults aged ≥25 and among those treated, over 60% had blood pressure controlled well (14). The prevention and control of non-communicable diseases in China are not optimistic compared with other countries and it has caused a major economic burden (14, 15). However, few studies have focused on the effect of low-cost essential medications provided for free by the local government on stroke. It is unclear, to what extent the implementation of a free pharmacy program could decrease the risk of stroke mortality.
Social distancing decreases an individual’s likelihood of contracting Coronavirus disease 2019 (COVID-19), however, the risk of chronic diseases due to lack of physical activities and social support is increasing. As recommended, all adults, even those with chronic conditions, should engage in at least 150 min a week of moderate-intensity exercise (16). However, in early 2020 due to the pandemic of COVID-19, in which nationwide social distancing was implemented, the intensity of exercise greatly decreased and the time of stay-at-home increased.
In this study, we aimed to take advantage of the free hypertension pharmacy program in Deqing County, Huzhou, Zhejiang Province to investigate the effectiveness and degree of pharmaceutical intervention in decreasing the disease burden of stroke. We quantified the impact of pharmaceutical intervention on stroke mortality. In addition, we assessed the changes in stroke mortality due to the pandemic of COVID-19, to disentangle the social distancing effect from the pharmaceutical intervention effect.
Huzhou, a northern city in Zhejiang Province, consists of two districts Wuxing, Nanxun, and three counties Deqing, Anji, and Changxing. From April 1, 2018, Deqing County began launching a free pharmaceutical intervention program, designed to increase medication adherence in patients with hypertension and hyperglycemia and reduce complications from other chronic diseases by providing certain prescription medications for free. Medicines include Nifedipine Extended-Release Tablets, Metoprolol Tartrate Tablets, Captopril Tablets, Hydrochlorothiazide Tablets, Clonidine Hydrochloride Tablets for hypertension and Metformin Hydrochloride Extended-Release Tablets, Gliclazide Modified-Release Tablets for type 2 diabetes. For patients who can receive free drugs, the essentials are as follows: (1) having local household registrations; (2) enrolled in the Family Doctor Contracted Service. Subsequently, family physicians will develop personalized treatment plans, and then free medications can be obtained from the community health center. The details of the implementation of the program can be seen in the Supplementary Figure S1.
In addition to free hypertension pharmaceutical intervention, non-pharmaceutical interventions (NPIs) exist concurrently during the COVID-19 pandemic in early 2020. Social distancing is a set of measures of NPIs, which has been recommended to reduce the chance of infection among high-risk populations and the burden on health care systems. It is useful for the containment and delay of contagious diseases by maintaining a physical distance between people and reducing the number of times people come into close contact with each other.
When the Chinese government officially confirmed on January 20, 2020 that the Novel Coronavirus can transmit from person to person, a social distancing policy rapidly swept across most cities in China. Impressively, within-city population mobility declines sharply and people chose to stay at home. As of March 14, 2020, when new confirmed cases decreased to 20, most provinces had lowered the level of emergency responses and within-city population movements gradually returned to pre-pandemic levels. We thus defined the strict social distancing period as January 20 to March 14. Stay-at-home made both physical activities and social support weakened during this period, which enabled us to examine the adverse effects on stroke mortality.
We retrospectively collected the routine surveillance data of stroke deaths reported by the Death Registration System of the Huzhou Municipal Center for Disease Prevention and Control from 1 January 2013, through 31 December 2020.
We obtained within-city mobility data from the Baidu Migration website,1 a map offered by a Chinese multinational technology company called Baidu. Specifically, Baidu Migration provides three migration intensity indices: the daily in-migration index (IMI) of a city, the daily out-migration index (OMI) of a city, and the daily within-city migration index (WCMI). And WCMI is the exponent result of the ratio of the daily number of people flowing in the city to the number of residents of the city, which can be used to measure the degree of recovery of city vitality. In this study, we only extracted the daily WCMI in 2019–2020 at the city-day level, which represents the population movements only in Huzhou itself per day.
Our research was conducted in accordance with the Declaration of Helsinki. No informed consents were required by patients, all data included in this study were kept confidential without personal identifiers.
We classified the data on stroke deaths by calendar time and districts. The data on stroke deaths from 2013 to 2020 were then organized into weekly time series data. Considering the characteristic of Huzhou, inter-city population mobility can be deemed relatively small in our study, thus we only focused on the changes in within-city population movements, and compared the values of WCMI as Jan 20 to March 14 in 2020 with corresponding values from the same lunar calendar periods in 2019.
Descriptive statistics were presented by t-test, linear regression and correlation analysis. Moreover, Serfling regression model was applied to estimate the effects of pharmaceutical intervention and social distancing at the population level, respectively. Serfling model was initially designed to develop a “standard curve of expected seasonal mortality” (17). Weekly stroke deaths are characterized by time series data. After initial exploratory data analysis and model validation, we formulated an adjusted Serfling model using Fourier terms with a 52-weeks cycle and a 26-weeks cycle in this study. The time metric in the model was continuous calendar time in weeks unit, a variable that was included as a covariate to approximate the secular trend of stroke deaths, wherein sinusoidal transformations of the time metric were introduced in pairs to capture the seasonality of stroke deaths over time. To mitigate the risk of spurious results in our analysis, we also fitted Serfling regression models in other regions with similar characteristics with Deqing but without a free pharmacy program. A two-tailed p-value < 0.05 was considered statistically significant. All statistical analyses were conducted using R software, version 4.1.1 (R Foundation for Statistical Computing).
The number of stroke deaths shows a declining trend over years from 2013 to 2020 in Deqing, Huzhou (β = −7.17, p = 0.29), whereas the other four districts or counties in Huzhou remain increasing (all β > 0), as shown in Supplementary Table S1.
The number of weekly stroke deaths in Deqing (blue line) was demonstrated with fitted data (red line) using a Serfling model (model estimates fitted on the data of 2013–2017 stroke deaths and predictions made on 2018–2020), as shown in Figure 1.

Figure 1. Number of weekly stroke deaths in Deqing, 2013–2020. Blue line depicted actual number of stroke deaths per week from January 2013 to December 2020. Red line predicted trends of stroke deaths using Serfling regression model based on 2013–2017 historic data in the counterfactual world in which pharmaceutical and non-pharmaceutical intervention were not implemented. Green shadows were presented as the reduction in stroke deaths, indicating those timepoints when actual number of stroke deaths was less than predicted number of deaths after the free hypertension pharmacy program. The dashed vertical lines showed the time when the free pharmaceutical intervention program in Deqing (April 1, 2018) and large-scale social distancing due to the pandemic of COVID-19 (January 20, 2020) were implemented.
The total number of reported deaths of stroke since the intervention program for the 2018–2020 season was 1,514, and 176 persons were deemed in reduction of expected for the cyclical regression. After the implementation of pharmaceutical intervention program since April 2018, as shown in Figure 2, the actual number of stroke deaths was significantly lower by 10% (95% CI, 6–15%; p < 0.001) from April 2018 to December 2020 in Deqing, compared to the predicted number. Under the assumption of a free hypertension program implemented in other four districts or counties in Huzhou, Serfling regression results showed that the reduction in actual stroke deaths compared with predicted numbers from 2018 to 2020 was only statistically significant in Anji county (t = −2.59, p < 0.01), as shown in Supplementary Table S2.
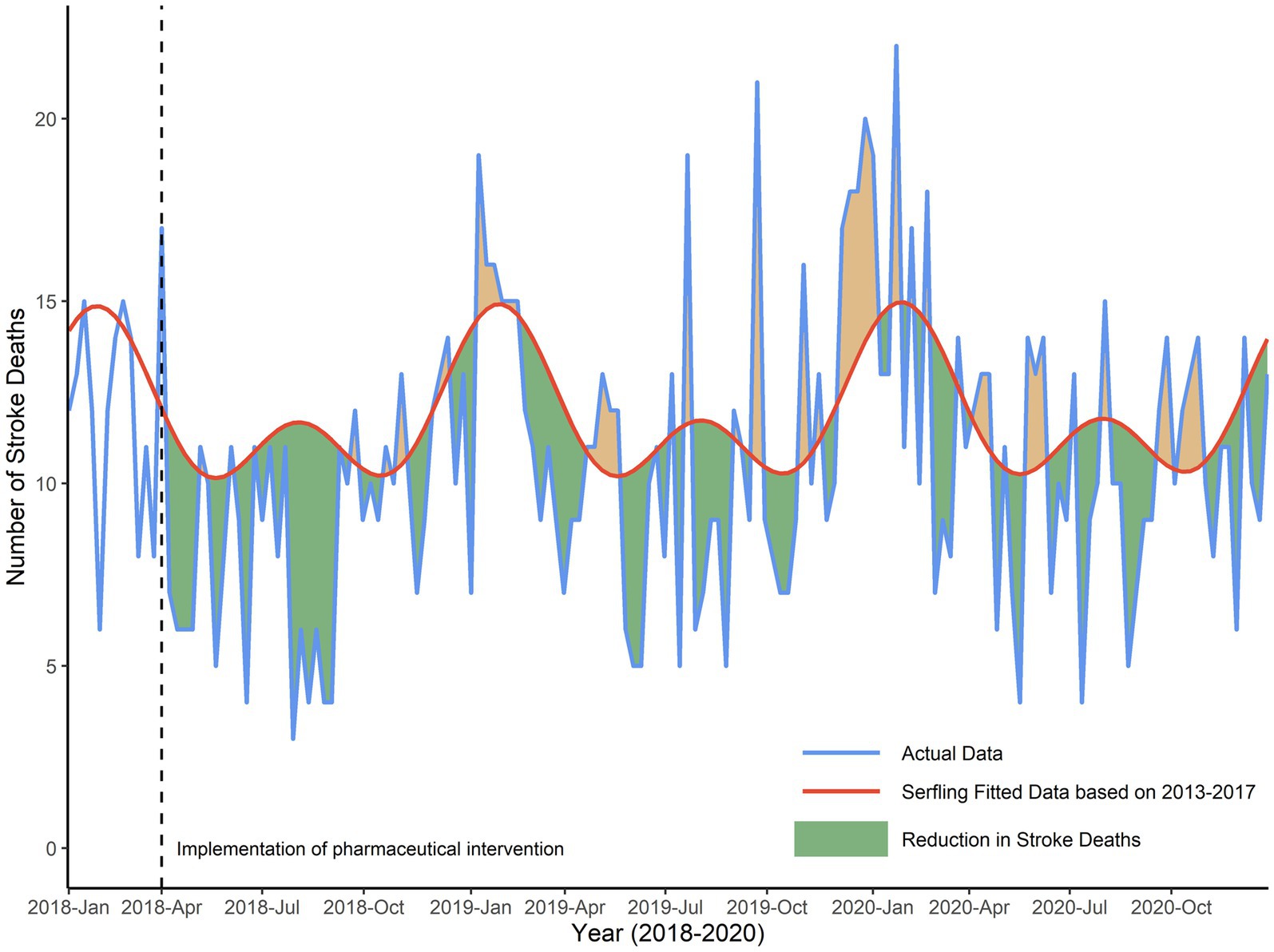
Figure 2. Reduction in number of weekly stroke deaths in Deqing, 2018–2020. Green shadows were presented as the reduction in actual stroke deaths compared with predicted numbers from 2018 to 2020, due to the presence of both pharmaceutical and non-pharmaceutical interventions. Orange shadows were presented as the increase in actual stroke deaths compared with predicted numbers.
To be specific, as shown in the left panel of Figure 3, the actual number was significantly lower than the predicted number, with a reduction of 19% (95% CI, 10–28%; p < 0.001) in 2018. However, compared to the predicted number of stroke deaths, the reduction of stroke deaths was not statistically significant both in 2019 and 2020. As shown in the right panel of Figure 3, the actual number was lower by 7% (95% CI, −2 – 16%; p = 0.13) in 2019. And there was a reduction of 8% (95% CI, −0.4 – 16%; p = 0.06) in 2020 (figure not shown).
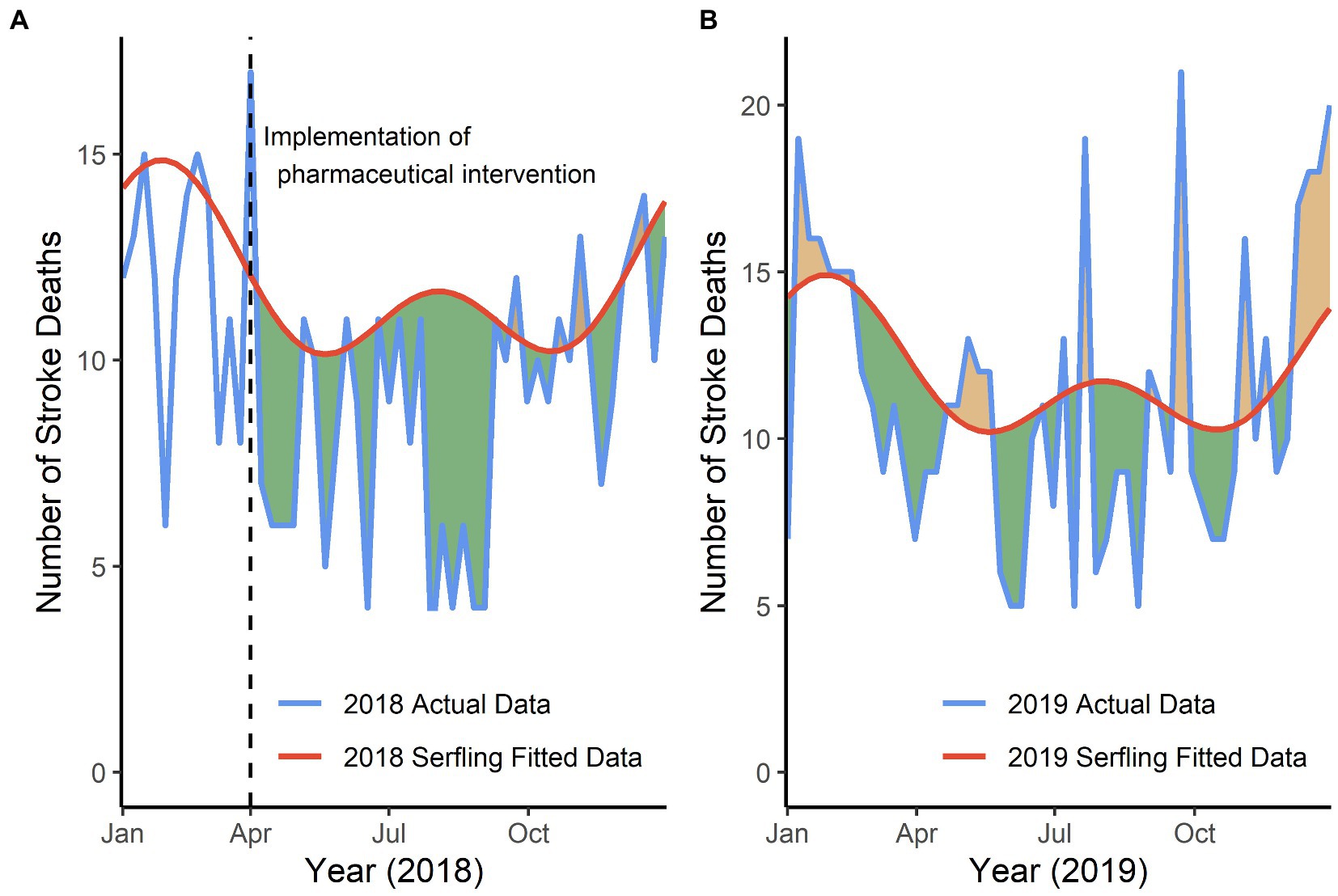
Figure 3. Reduction in number of weekly stroke deaths in Deqing, 2018–2019, respectively. (A) Green shadows were presented as the reduction in actual stroke deaths compared with predicted numbers since April 2018, in the presence of only pharmaceutical intervention effect, in which there was a significant reduction of 19% (t = −4.26, p < 0.001). (B) Green shadows were presented as the reduction in actual stroke deaths compared with predicted numbers in year 2019, in the presence of only pharmaceutical intervention effect, in which there was a reduction of 7% (t = −1.47, p = 0.15).
Besides, the proportion of weekly reduction in the number of stroke deaths showed no significant change over time in 2018 (r = −0.21, p = 0.19) and 2019 (r = −0.23, p = 0.10) in Deqing.
During the COVID-19 pandemic in early 2020, the average number of monthly stroke deaths was 51 in the first half of 2020, whereas it was 47 in the first half of 2019 in Deqing. And the average numbers of monthly stroke deaths from 2013 to 2017 were all greater than 50, the number in 2018 would not be included in the comparison due to the implementation of the intervention program in April.
Specifically, we calculated changes in population movements as January 20 to March 14 in 2020 and compared the findings with corresponding changes from the same lunar calendar periods in 2019, during which the city was free of COVID-19 incidence and social distancing, we observed a significant decrease in the daily WCMI in 2020 (95% CI, 1.05–1.64, p < 0.001).
To further disentangle the social distancing effect from the pharmaceutical intervention effect, we assumed that the decrease in the number of deaths caused by the pharmaceutical intervention throughout the year 2020 in Deqing was identical to the average decreasing level from April 2018 to December 2019, which was approximately equal to 12% (95% CI, 6–18%; p < 0.001), and then quantified an additional increase caused by social distancing was 5% (95% CI, −4 – 14%; p = 0.28), as shown in Figure 4. Finally, there still existed a reduction of 8% in the number of weekly stroke deaths in 2020 compared with predicted data, though it is not statistically significant.
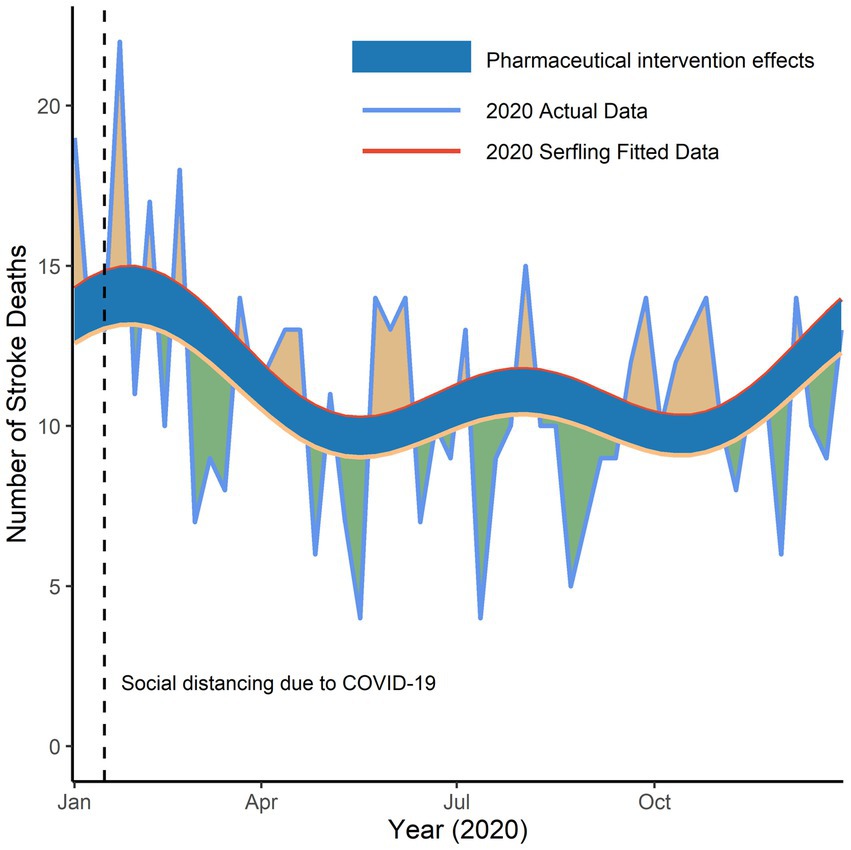
Figure 4. Reduction in number of weekly stroke deaths in Deqing, 2020. Yellow line represented adjusted predicted stroke deaths in 2020 after a large-scale social distancing due to the pandemic of COVID-19 was implemented. Blue shadows were presented as the pharmaceutical intervention effects throughout year 2020. Green shadows were presented as the reduction and orange shadows as the increase in actual stroke deaths compared with predicted numbers.
In this study, we found that free pharmaceutical intervention was effective on the control of blood pressure, and the mortality of stroke also decreased. And stroke mortality was estimated decreasing 10% since the implementation of the intervention program. Specifically, there was a reduction of 19% in 2018. We also found that in the counterfactual world in which the other four districts or counties in Huzhou implemented the free pharmacy program, Anji was the only region that had stroke deaths declined. The decline could be attributed to the implementation of an intervention project launched by Fuwai Hospital in China. This comprehensive intervention project aimed at reducing the morbidity, recurrence, and mortality of CVD, Anji had participated in the program since 2015. As a result, compared with other regions in Huzhou, we concluded there occurred a decrease in stroke mortality in Deqing with the implementation of the free pharmacy program.
Previous studies of high blood pressure and CVD mainly focused on two aspects: one is the association between blood pressure and risk of CVD across different blood pressure levels, and the other is the cost-effectiveness of hypertension treatment for CVD prevention, whereas no evidence has ever been presented for quantitative evaluation on the impact of the implementation of a free hypertension pharmacy program on CVD prevention. The findings from our study add to existing evidence on the benefits of antihypertensive drug therapy by quantifying the impact on stroke mortality. In our large study, we investigated the effectiveness and degree of pharmaceutical intervention in decreasing stroke mortality at the population level. Our findings are in line with those of the randomized controlled trials, findings from large-scale analyses of randomized trials suggested that antihypertensive medications can be viewed as an effective tool to prevent cardiovascular mortality and morbidity, rather than simply reducing blood pressure (5, 18). A detailed study of age-stratified and blood-pressure-stratified effect of antihypertensive medications found pharmacological blood pressure reduction to be effective for CVD prevention across a wide range of ages, with no significant difference in relative risk reductions among different baseline systolic or diastolic blood pressure levels. It suggested effectiveness for antihypertensive treatment for older adults, even when their blood pressure is not highly abnormal (19). A modeling study in China suggested that treating all hypertension would prevent about 690,000 strokes (20). On contrary, it is worth noting that some researchers still insisted on common clinical practice for antihypertensive treatment that lowering blood pressure would have an uncertain or even detrimental effect. For instance, the UK NICE guideline recommends blood pressure-lowering treatment for primary prevention of CVD is not considered relevant when baseline systolic blood pressure is less than 140 mm Hg (21). Likewise, New Zealand’s Ministry of Health recommends screening adults for overall cardiovascular risk at first, and only individuals diagnosed at high risk for CVD and together with high blood pressure can receive antihypertensive drug treatment (22).
Adherence to regular and adequate chronic medications is a barrier for low-and middle-income residents. To reduce the burden of medical costs and encourage access to medicines, full coverage policies have been established in many countries worldwide. Few studies, however, have examined the effectiveness of CVD mortality on patients with hypertension accessing free medications. The relationship between costs and medication adherence has been widely studied (23). For example, Brazilian ‘Farmácia Popular’ program offered 17 kinds of hypertensive and diabetic medicines for free and improved adherence remarkably (24). A field survey in rural communities in Shandong Province in China also suggested that the provision of basic medicines at no charge for hypertensive patients increased medication adherence and overall all, patients in the intervention group had their blood pressure controlled lower than before the intervention, which is consistent with the evidence from our study (25). Recently, a modeling study in China also implied that full implementation of the essential medicines program will be important for reaping the benefits of improved hypertension control for preventing CVD (20).
The second main finding of our study was the observation that an extra 5% increase in the mortality of stroke during the COVID-19 pandemic, which may be attributable to the social distancing policy. But it wasn’t statistically significant, part of the reason for this was the short observation period of the adverse effect of COVID-19. On the other hand, it is precisely because of the existence of pharmaceutical intervention effect that the impact of social distancing on the changes of stroke mortality was not significant. However, the large-scale social distancing did greatly decrease within-city mobility among people from all walks of life during the outbreak, possibly leading to a lack of physical activity among all age groups, especially older people. An analysis of more than 150,000 patients with baseline hypertension with an average follow-up of 7.1 years showed that, compared with patients in the lowest quartile of physical activity, other groups all had a significantly lower risk of death from stroke, regardless of exercise intensity (26). Even for those who do not meet the minimum recommended exercise intensity, the risk of cardiovascular death also decreased significantly (27, 28). Social distancing not only caused a direct reduction in physical activity but also had a negative effect on mental health during the pandemic. Multiple longitudinal studies showed that individuals who experienced social isolation and loneliness tended to have more unhealthy behaviors (29–31), such as smoking and alcohol abuse, that may further be associated with the progression of CVD. Evidence from a large US prospective cohort study suggested social isolation and loneliness in the era of COVID-19 were independently associated with a modestly higher risk of CVD (32). Results from a population-based cohort study in rural areas in China demonstrated that older people with depression have increased all-cause mortality, which was not confounded by other cardiovascular risk factors. These indicate the need for more psychological interventions for people with CVD or risk factors of CVD (33).
Social distancing policy can also have a negative effect on timely medical care help. One hypothesis explaining the phenomenon may be that patients were fear of infection or contagion during the outbreak. The feeling may have been amplified by stay-at-home orders due to the strict social distancing policy and overwhelming news about the virus from the media during early 2020. However, delays in seeking medical care or even not seeking care would have a detrimental effect on stroke outcomes. Results from a Hong Kong study showed that there was a prolongation in stroke onset to hospital arrival time and a significant reduction in individuals arriving at the hospital within 4.5 h during the COVID-19 pandemic (34). Several studies in other countries such as United States, Brazil, Spain reported similar findings (35–37). Also, as the therapeutic time window for reperfusion for acute ischemic stroke is narrow (38), any delays in treatment would harm patients’ quality of life, and increase the risk of recurrence and mortality. Further studies based on retrospective population-based cohorts are needed to investigate how COVID-19 has led to changes in stroke epidemiology and the long-term impact on its clinical outcomes. Moreover, studies focusing on the association between individual patients’ behavior during COVID-19 and their functional outcomes are warranted.
Possible mechanisms have been proposed to elucidate the association between blood pressure lowering and stroke prevention. Repeated fluctuations in blood flow caused by the rise or fall of blood pressure increase mechanical stress on the arterial walls, leading to the process of vascular remodeling, such as arterial stiffening (39, 40), endothelial dysfunction (41–43), platelet activation (44), and inflammation (43, 45, 46). The human brain consists of tens of billions of neurons, due to its structural complexity and interconnected neural circuit, cerebrovascular microvasculature is especially vulnerable to blood fluctuations, possibly leading to cerebral small vessel disease like stroke (47, 48).
The mechanisms through which social distancing is associated with stroke may involve both decreasing activities of daily living and changing health status. The status of social distancing may affect cardiovascular health by dysregulating neuroendocrine system, disturbing autonomic function (49), triggering inflammatory reactions (50), and increasing long-term allostatic load (51). Also, the experiences of isolation and loneliness may directly activate the hypothalamic–pituitary–adrenal axis and the sympathetic nervous system, leading to enhanced inflammation and oxidative stress, then developing atherosclerosis and elevated systolic blood pressure (52, 53).
The main strength of our study is that we formulated a regression model under counterfactual scenarios and quantify the effect caused by interventions. Firstly, compared with other intervention evaluation methods in time series design, Serfling regression model does a reasonable job approximating the secular trend of stroke deaths by treating cyclical calendar time as a continuous predictor, wherein sinusoidal transformations of the time metric are introduced in pairs to capture the patterns of seasonally varying outcomes over time. Secondly, our study covered long-time periods in settings with large repositories of historical data from healthcare administrations and the validity was high for evaluating the temporality between free hypertension pharmacy program and stroke mortality. Thirdly, our study investigated not only the impact of the free provision of essential medications to prevent stroke, but also the adverse effects of changes in lifestyle and mental health status on stroke mortality due to social distancing.
Several limitations should be noted. Firstly, lagged effects of medications in our model were not considered. But it had been proved that the mean of the finalized model residuals is close to zero and autocorrelation function plot suggests there is no significant correlation in the residual series. It may partially attenuate the estimates but would not change conclusions substantially. Secondly, no specific data were available on how many patients in the population had received free antihypertensive treatment in our study. But we know the number of patients receiving free medications was the highest in 2018, it decreased in 2019 and slightly increased in 2020, which kept in line with the decreasing trend in stroke mortality over time. We hope to make improvements and analyze the association between the number of patients receiving different classes of drugs and the changes in stroke mortality in future studies. Thirdly, we could not rule out the influence of some unmeasured confounders, for instance, the provision of free risk factor modifying medications may also have a positive effect on the prevention of other conditions, such as diabetes, and kidney diseases. Fourthly, the location of the intervention program is in a developed and rich county, which may slightly overestimate the impact and limit the generalizability of our findings.
Further research that bypass the abovementioned limitations can be carried out to advance the evidence on blood pressure lowering and stroke prevention. Low-cost essential antihypertensive medications for hypertension control have been proven cost-effective by many researchers, we hope to roll out intervention programs and conduct a more in-depth evaluation of the impact over time. What’s more, we can evaluate the intervention effect at the individual level in the future. In addition, a detailed subgroup analysis on changes in mortality by gender or age can also be included in the analysis.
We quantified the impact of free pharmaceutical intervention and social distancing in changing stroke mortality in Deqing, Zhejiang Province. Notably, our study examined the degree of hypertension control that would minimize the risk of stroke mortality and it suggested free hypertension pharmacy program has great potential to prevent at least 10% of stroke deaths in our country. These findings highlight the effectiveness of promoting free medications for preventing stroke in patients with hypertension.
Free supply of low-cost, essential medications that target patients with hypertension at increased risk of stroke could be taken into account in formulating public health policies and guiding allocations of health care resources, which may be cost-effective in reducing disease burden and economic burden in the future.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
QZ: data analysis and interpretation, graphic visualization, and drafting and revision of the manuscript. MY, MJ, and PZ: data collection and interpretation, and revision of the manuscript. GQ and YY: study concept and design, and revision of manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by a grant for clinical research from Shanghai Municipal Health Commission (20214Y0020) to YYao, a grant from Shanghai Municipal Nature Science Foundation (22ZR1414600) to YYao, a grant for the young leading talents from Shanghai Municipal Health Commission (2022YQ076) to YYao. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We gratefully acknowledge all patients who participated in the study and health professionals who helped with the data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1142299/full#supplementary-material
1. Kisa, A, Kisa, S, and Collaborators, GS. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 26:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Wang, YJ, Li, ZX, Gu, HQ, Zhai, Y, Jiang, Y, Zhao, XQ, et al. China stroke statistics 2019: a report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for neurological diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. (2020) 5:211–39. doi: 10.1136/svn-2020-000457
3. Zhou, M, Wang, H, Zeng, X, Yin, P, Zhu, J, Chen, W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
4. Yusuf, S, Joseph, P, Rangarajan, S, Islam, S, Mente, A, Hystad, P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. (2020) 395:795–808. doi: 10.1016/S0140-6736(19)32008-2
5. Collaboration. BPLTT. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. (2021) 397:10285. doi: 10.1016/S0140-6736(21)00590-0
6. Volpe, M, and Patrono, C. The key role of blood pressure lowering in cardiovascular prevention irrespective of baseline blood pressure and risk profile. Eur Heart J. (2021) 42:2814–5. doi: 10.1093/eurheartj/ehab320
7. Huo, Y, Li, J, Qin, X, Huang, Y, Wang, X, Gottesman, RF, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. (2015) 313:1325–35. doi: 10.1001/jama.2015.2274
8. Gao, P, Mei, K, Li, H, Dai, Q, Guo, X, Zhang, D, et al. Clinical efficacy and safety of combination therapy with amlodipine and Olmesartan or an Olmesartan/hydrochlorothiazide compound for hypertension: a prospective, open-label, and Multicenter clinical trial in China. Curr Ther Res Clin Exp. (2019) 90:99–105. doi: 10.1016/j.curtheres.2015.09.001
9. Reed, ME, Warton, EM, Kim, E, Solomon, MD, and Karter, AJ. Value-based insurance design benefit offsets reductions in medication adherence associated with switch to deductible plan. Health Aff (Millwood). (2017) 36:516–23. doi: 10.1377/hlthaff.2016.1316
10. Wu, YM, Huang, J, and Reed, ME. Association between high-deductible health plans and engagement in routine medical care for type 2 diabetes in a privately insured population: a propensity score-matched study. Diabetes Care. (2022) 45:1193–200. doi: 10.2337/dc21-1885
11. Zhang, M, Meng, Y, Yang, Y, Liu, Y, Dong, C, Xiao, J, et al. Major inducing factors of hypertensive complications and the interventions required to reduce their prevalence: an epidemiological study of hypertension in a rural population in China. BMC Public Health. (2011) 11:301. doi: 10.1186/1471-2458-11-301
12. Wang, H, Yip, W, Zhang, L, Wang, L, and Hsiao, W. Community-based health insurance in poor rural China: the distribution of net benefits. Health Policy Plan. (2005) 20:366–74. doi: 10.1093/heapol/czi045
13. Zhang, M, Wu, J, Zhang, X, Hu, CH, Zhao, ZP, Li, C, et al. Prevalence and control of hypertension in adults in China, 2018. Zhonghua Liu Xing Bing Xue Za Zhi. (2021) 42:1780–9. doi: 10.3760/cma.j.cn112338-20210508-00379
14. Foti, K, Wang, D, Appel, LJ, and Selvin, E. Hypertension awareness, treatment, and control in US adults: trends in the hypertension control Cascade by population subgroup (National Health and nutrition examination survey, 1999-2016). Am J Epidemiol. (2019) 188:2165–74. doi: 10.1093/aje/kwz177
15. Fang, M, Wang, D, Coresh, J, and Selvin, E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med. (2021) 384:2219–28. doi: 10.1056/NEJMsa2032271
16. Piercy, KL, Troiano, RP, Ballard, RM, Carlson, SA, Fulton, JE, Galuska, DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
17. Serfling, RE. Methods for current statistical analysis of excess pneumonia-influenza deaths. Public Health Rep. (1896). 1963) 78:494–506.
18. Ettehad, D, Emdin, CA, Kiran, A, Anderson, SG, Callender, T, Emberson, J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. (2016) 387:957–67. doi: 10.1016/S0140-6736(15)01225-8
19. Rahimi, K, Bidel, Z, Nazarzadeh, M, Copland, E, Canoy, D, Wamil, M, et al. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet. (2021) 10305:398. doi: 10.1016/S0140-6736(21)01921-8
20. Gu, D, He, J, Coxson, PG, Rasmussen, PW, Huang, C, Thanataveerat, A, et al. The cost-effectiveness of low-cost essential antihypertensive medicines for hypertension control in China: a modelling study. PLoS Med. (2015) 12:e1001860. doi: 10.1371/journal.pmed.1001860
21. Health NIF, Excellence C. Hypertension in adults: diagnosis and management. National Institute for Health and Care Excellence (NICE) (2016) doi: 10.3399/bjgp20X708053
22. Health Mo. Cardiovascular disease risk assessment and management for primary care. Ministry of Health Wellington (2018).
23. Luiza, VL, Chaves, LA, Silva, RM, Emmerick, ICM, Chaves, GC, de Araújo, SCF, et al. Pharmaceutical policies: effects of cap and co-payment on rational use of medicines. Cochrane Database Syst Rev. (2015) 5. doi: 10.1002/14651858.CD007017.pub2
24. Emmerick, ICM, Campos, MR, Luiza, VL, Chaves, LA, Bertoldi, AD, and Ross-Degnan, D. Retrospective interrupted time series examining hypertension and diabetes medicines usage following changes in patient cost sharing in the ‘Farmácia Popular’ programme in Brazil. BMJ Open. (2017) 7:e017308. doi: 10.1136/bmjopen-2017-017308
25. Yu, B, Zhang, X, and Wang, G. Full coverage for hypertension drugs in rural communities in China. Am J Manag Care. (2013) 19:e22–9.
26. Fan, M, Yu, C, Guo, Y, Bian, Z, Li, X, Yang, L, et al. Effect of total, domain-specific, and intensity-specific physical activity on all-cause and cardiovascular mortality among hypertensive adults in China. J Hypertens. (2018) 36:793–800. doi: 10.1097/HJH.0000000000001601
27. Bennett, DA, Du, H, Clarke, R, Guo, Y, Yang, L, Bian, Z, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol. (2017) 2:1349–58. doi: 10.1001/jamacardio.2017.4069
28. Wen, CP, Wai, JP, Tsai, MK, Yang, YC, Cheng, TY, Lee, MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. (2011) 378:1244–53. doi: 10.1016/S0140-6736(11)60749-6
29. Brandt, L, Liu, S, Heim, C, and Heinz, A. The effects of social isolation stress and discrimination on mental health. Transl Psychiatry. (2022) 12:398. doi: 10.1038/s41398-022-02178-4
30. Sherman, DK, Kim, HS, and Taylor, SE. Culture and social support: neural bases and biological impact. Prog Brain Res. (2009) 178:227–37. doi: 10.1016/S0079-6123(09)17816-0
31. Walker, D, and Beauchene, RE. The relationship of loneliness, social isolation, and physical health to dietary adequacy of independently living elderly. J Am Diet Assoc. (1991) 91:300–4.
32. Golaszewski, NM, LaCroix, AZ, Godino, JG, Allison, MA, Manson, JE, King, JJ, et al. Evaluation of social isolation, loneliness, and cardiovascular disease among older women in the US. JAMA Netw Open. (2022) 5:e2146461. doi: 10.1001/jamanetworkopen.2021.46461
33. Zhou, W, Hopkins, A, Zaman, MJ, Tao, XG, Rodney, A, Yao, Y, et al. Impacts of heart disease, depression and their combination on all-cause mortality in older people: a rural community-based cohort study in China. BMJ Open. (2020) 10:e038341. doi: 10.1136/bmjopen-2020-038341
34. Teo, KC, Leung, WCY, Wong, YK, Liu, RKC, Chan, AHY, Choi, OMY, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. (2020) 51:2228–31. doi: 10.1161/STROKEAHA.120.030105
35. Desai, SM, Guyette, FX, Martin-Gill, C, and Jadhav, AP. Collateral damage - impact of a pandemic on stroke emergency services. J Stroke Cerebrovasc Dis. (2020) 29:104988. doi: 10.1016/j.jstrokecerebrovasdis.2020.104988
36. Diegoli, H, Magalhães, PSC, Martins, SCO, Moro, CHC, França, PHC, Safanelli, J, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. (2020) 51:2315–21. doi: 10.1161/STROKEAHA.120.030481
37. Montaner, J, Barragán-Prieto, A, Pérez-Sánchez, S, Escudero-Martínez, I, Moniche, F, Sánchez-Miura, JA, et al. Break in the stroke chain of survival due to COVID-19. Stroke. (2020) 51:2307–14. doi: 10.1161/STROKEAHA.120.030106
38. Prabhakaran, S, Ruff, I, and Bernstein, RA. Acute stroke intervention: a systematic review. JAMA. (2015) 313:1451–62. doi: 10.1001/jama.2015.3058
39. Zhou, TL, Henry, RMA, Stehouwer, CDA, van Sloten, TT, Reesink, KD, and Kroon, AA. Blood pressure variability, arterial stiffness, and arterial Remodeling. Hypertension. (2018) 72:1002–10. doi: 10.1161/HYPERTENSIONAHA.118.11325
40. Mitchell, GF, van Buchem, MA, Sigurdsson, S, Gotal, JD, Jonsdottir, MK, Kjartansson, Ó, et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: the age, gene/environment susceptibility--Reykjavik study. Brain. (2011) 134:3398–407. doi: 10.1093/brain/awr253
41. Angeli, F, Reboldi, G, and Verdecchia, P. Blood pressure variability and risk of stroke in chronic kidney disease. J Hypertens. (2020) 38:599–602. doi: 10.1097/HJH.0000000000002339
42. Rothwell, PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. (2010) 375:938–48. doi: 10.1016/S0140-6736(10)60309-1
43. Xu, S, Ilyas, I, Little, PJ, Li, H, Kamato, D, Zheng, X, et al. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies. Pharmacol Rev. (2021) 73:924–67. doi: 10.1124/pharmrev.120.000096
44. Ikeda, Y, Handa, M, Kawano, K, Kamata, T, Murata, M, Araki, Y, et al. The role of von Willebrand factor and fibrinogen in platelet aggregation under varying shear stress. J Clin Invest. (1991) 87:1234–40. doi: 10.1172/JCI115124
45. Parissis, JT, Korovesis, S, Giazitzoglou, E, Kalivas, P, and Katritsis, D. Plasma profiles of peripheral monocyte-related inflammatory markers in patients with arterial hypertension. Correlations with plasma endothelin-1. Int J Cardiol. (2002) 83:13–21. doi: 10.1016/S0167-5273(02)00021-9
46. Suzuki, Y, Ozawa, T, Kurata, T, Nakajima, N, Zamponi, GW, Giles, WR, et al. A molecular complex of ca(v)1.2/CaMKK2/CaMK1a in caveolae is responsible for vascular remodeling via excitation-transcription coupling. Proc Natl Acad Sci U S A. (2022) 119:e2117435119. doi: 10.1073/pnas.2117435119
47. Ma, Y, Song, A, Viswanathan, A, Blacker, D, Vernooij, MW, Hofman, A, et al. Blood pressure variability and cerebral small vessel disease: a systematic review and meta-analysis of population-based cohorts. Stroke. (2020) 51:82–9. doi: 10.1161/STROKEAHA.119.026739
48. Tully, PJ, Yano, Y, Launer, LJ, Kario, K, Nagai, M, Mooijaart, SP, et al. Association between blood pressure variability and cerebral small-vessel disease: a systematic review and meta-analysis. J Am Heart Assoc. (2020) 9:e013841. doi: 10.1161/JAHA.119.013841
49. Grippo, AJ, Lamb, DG, Carter, CS, and Porges, SW. Social isolation disrupts autonomic regulation of the heart and influences negative affective behaviors. Biol Psychiatry. (2007) 62:1162–70. doi: 10.1016/j.biopsych.2007.04.011
50. Loucks, EB, Berkman, LF, Gruenewald, TL, and Seeman, TE. Relation of social integration to inflammatory marker concentrations in men and women 70 to 79 years. Am J Cardiol. (2006) 97:1010–6. doi: 10.1016/j.amjcard.2005.10.043
51. Seeman, TE, Singer, BH, Ryff, CD, Dienberg Love, G, and Levy-Storms, L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. (2002) 64:395–406. doi: 10.1097/00006842-200205000-00004
52. Franklin, SS, Wt, G, Wong, ND, Larson, MG, Weber, MA, Kannel, WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham heart study. Circulation. (1997) 96:308–15. doi: 10.1161/01.CIR.96.1.308
Keywords: stroke, hypertension, pharmaceutical intervention program, social distancing, Serfling regression model
Citation: Zhou Q, Yu M, Jin M, Zhang P, Qin G and Yao Y (2023) Impact of free hypertension pharmacy program and social distancing policy on stroke: A longitudinal study. Front. Public Health. 11:1142299. doi: 10.3389/fpubh.2023.1142299
Received: 03 February 2023; Accepted: 28 March 2023;
Published: 18 April 2023.
Edited by:
Aleksandra Piechota-Polańczyk, Jagiellonian University, PolandReviewed by:
Aleksandra Kopacz, Jagiellonian University, PolandCopyright © 2023 Zhou, Yu, Jin, Zhang, Qin and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meihua Jin, aHV6aG91am1oNjgyMUAxNjMuY29t; Ye Yao, eXlhb0BmdWRhbi5lZHUuY24=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.