
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 25 May 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1142134
Introduction: Data on the epidemiology of ischemic stroke (IS) with large vessel occlusion (LVO) are scarce although there is a need to better assess future demands for dedicated facilities in an aging population. This study aimed to estimate the number of expected cases of IS with LVO of the anterior circulation in the French population by 2050.
Methods: IS were retrieved from the population-based registry of Dijon, France (2013–2017). Patients with LVO were identified and age-and sex-standardized incidence rates were calculated to estimate the number of expected cases in the whole French population by 2050 according three scenarios: stable incidence; a decrease in incidence rates of 0.5%/year in people >65 years old; a decrease in incidence rates of 0.5%/year in overall population.
Results: 1,067 cases of IS with LVO were recorded in Dijon over the study period, corresponding to crude incidence rate of 22/100,000/year (95% CI: 18–25). By 2050, the number of cases is expected to increase by 51 to 81% according to the various scenarios, to reach between 22,457 cases (95% CI: 10,839 – 43,639) and 26,763 cases (95% CI: 12,918 – 52,008) annually. This increase will be mainly driven by patients >80 years old, with a rise of cases between +103% and +42% in this age group. The proportion of patients >80 years old among overall IS with LVO will increase from 43 to 57% approximately.
Conclusion: The expected massive increase in IS with LVO highlights the need for a rapid action to cover stroke care requirements.
With the advent of mechanical thrombectomy (MT) as acute treatment of ischemic stroke (IS) due to large vessel occlusion (LVO) of the anterior circulation, patients’ outcome dramatically improved (1). Although MT is now considered as the standard of care of IS with LVO therapy, in addition with intravenous thrombolysis when indicated (2), it can be performed only in centres with interventional neuroradiology facilities, the number of which is limited in a vast majority of countries. This shortage in specialised medical resources poses a number of challenges for pre-hospital triage of patients suspected of suffering an IS, and the referral to MT-capable centres. Because of the ongoing aging population, an increase in the annual total number of strokes has been observed over the past decades, and this trend will dramatically magnify in coming years (3–5). These epidemiological perspectives represent a threat to the sustainability of health systems. In particular, there is an urgent need to plan for the future resources required for the acute management of IS patients with LVO.
Therefore, the aim of this study was to estimate the number of expected cases of IS with LVO of the anterior circulation in the French population by 2050.
All cases of IS were retrieved from the Dijon Stroke Registry (6, 7), an ongoing prospective population-based study that complies with the criteria for conducting “ideal” incidence stroke studies, and the guidelines for the reporting of incidence and prevalence studies in neuroepidemiology according to Standard of Reporting of Neurological Disorders (STROND). The methodology of the Dijon Stroke Registry has been described extensively elsewhere (6, 7). Briefly, case-collection relies on multiple overlapping sources of information to identify first-ever and recurrent hospitalized and not hospitalized cases of stroke among residents of the city of Dijon France (currently 156,000 inhabitants). For this study, analyses were restricted to IS patients registered between 1st January 2013 and 31st December 2017.
To assess the presence of a LVO in IS patients, all cervical and intracranial arterial imaging exams were systematically reviewed by stroke-trained investigators. A LVO of the anterior circulation was defined as an occlusion site affecting the terminal intracranial internal carotid artery, M1 and M2 segments of the middle cerebral artery (including tandem occlusions), or A1 and A2 segment of the anterior cerebral artery. Patients with isolated extracranial internal carotid artery occlusion were not included in this group since the benefit of MT in them has still to be demonstrated. In addition, LVO was considered only if it was responsible for the acute IS.
Annual incidence rates of IS with a proximal occlusion of the anterior circulation were calculated according to age groups, and sex, and were expressed per 100,000 people with 95% CIs assuming a Poisson distribution as previously reported (6). Denominators concerning the population of Dijon were based on census data provided by the French National Institute of Statistics. The estimation of the number of cases of IS with LVO of the anterior circulation in France was obtained by standardization to age-and sex-specific incidence found in the Dijon Stroke Registry over the period 2013–2017 (6). Expected number of cases until 2050 were assessed according to three different scenarios: stable age-and sex-specific incidence rates, a decrease in incidence rates of 0.5%/year in people over 65 years old, a decrease in incidence rates of 0.5%/year in overall population. The number of French inhabitants by 2050 was obtained by data from the Institut National de la Statistique et des Etudes Economiques (8). Statistical analysis was performed with STATA 13 software (StataCorp LP, College Station, TX, United States).
The Dijon Stroke Registry was approved by following national ethics boards: the Comité d’Evaluation des Registres (French National Committee of Registers), Santé Publique France (French Institute for Public Health Surveillance), and the Commission Nationale Informatique et Liberté (French data protection authority). In accordance with the French legislation, boards waived the need for written patient consent.
From 2013 to 2017, 1,060 cases of acute IS were recorded (mean age: 76.0 ± 15.8 years, 53.9% women). Information about arterial imaging was available in 971 (91.6%) patients. A LVO of the anterior circulation was observed in 167 patients (17.2%). Corresponding crude incidence rate was 22/100,000/year (95% CI: 18–25). Based on the age and sex-standardized incidence rates, we estimated that the number of IS with LVO in France in 2015 was 14,824 cases per year (95% CI: 6,540 – 31,371), including 8,190 cases in women (95% CI: 3,992 – 16,351) and 6,634 cases in men (95% CI: 2,548–15,020) (Table 1).
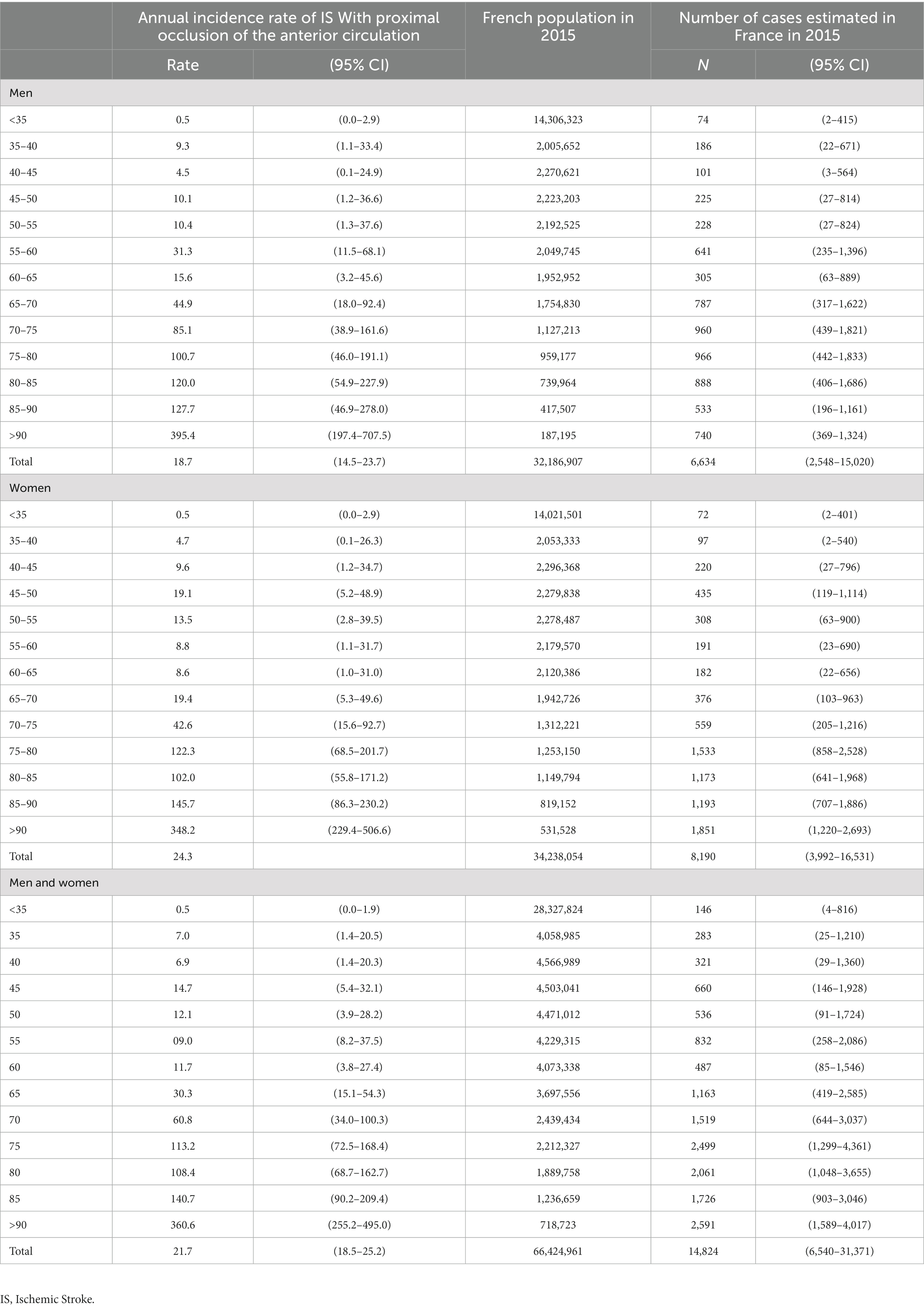
Table 1. Annual incidence rates of ischemic stroke with a proximal occlusion of the anterior circulation in Dijon, France, from 2013 to 2017 (expressed as n/100,000/year) and projection of absolute number of cases in the French population in 2015.
A steady increase in the number of IS cases with LVO of the anterior circulation is expected in France from 2015 to 2050, whatever the incidence trend scenario considered (Figure 1). Assuming a stable incidence, this number will increase by 81%, corresponding to 26,763 cases in 2050 (95% CI: 12,918 – 52,008), including 14,243 cases in women (95% CI: 7,666 – 25,813) and 12,520 cases in men (95% CI: 5,252 – 26,195). Considering a decrease in incidence by 0.5%/year in people >65 years old, the expected number of cases will rise by 55% with 22,975 cases in 2050 (95% CI: 10,940 – 45,336) including 12,186 cases in women (95% CI: 6,472 – 22,460), and 10,789 in men (95% CI: 4,468 – 22,876). Finally, if the incidence decreases by 0.5%/year in the entire population, the expected number of cases will increase by 51% with 22,457 cases (95% CI: 10,839 – 43,639) including 11,951 cases in women (95% CI: 6,432 – 21,660) and 10,506 cases in men (95% CI: 4,407 – 21,979).
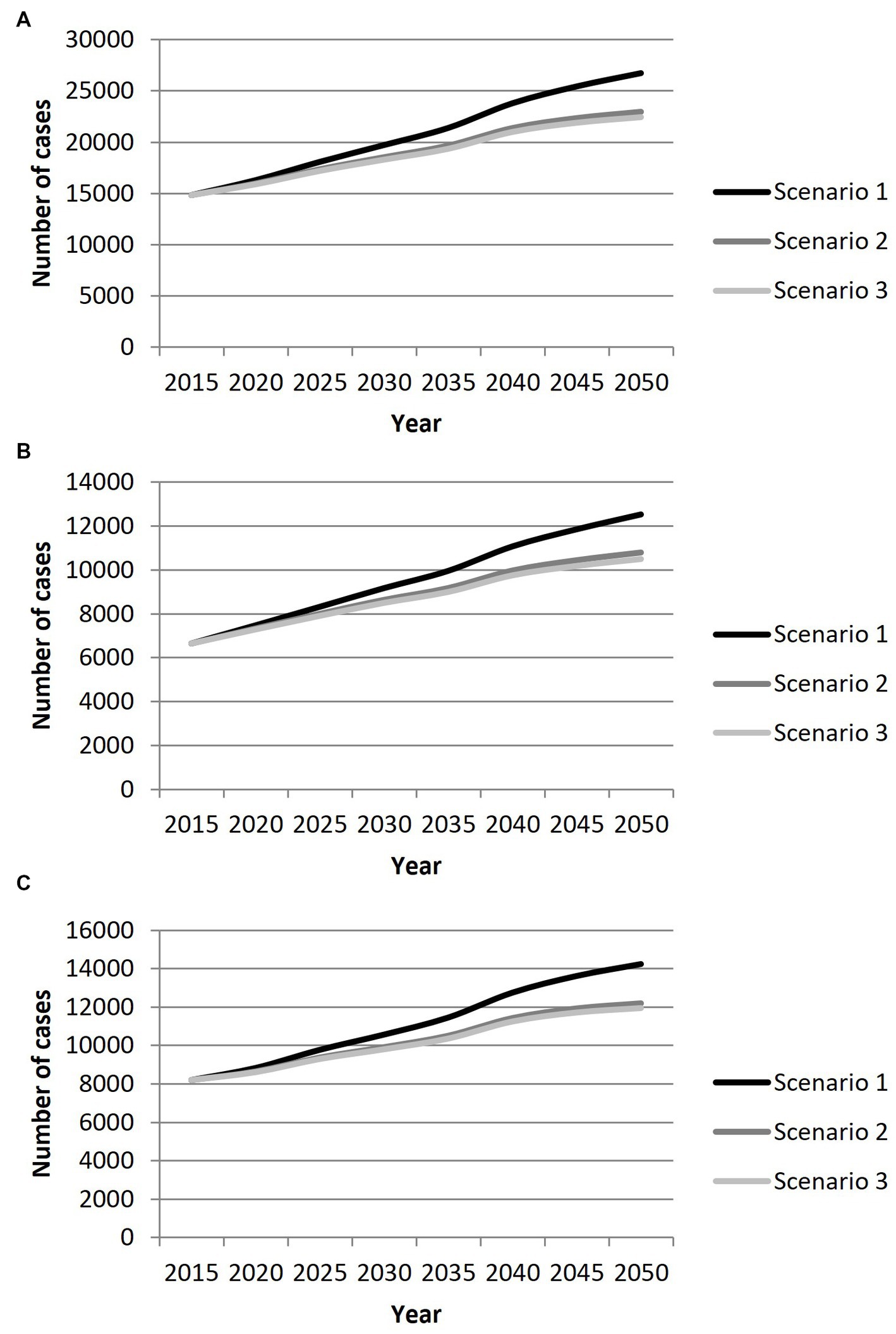
Figure 1. Projection of the number of cases of ischemic stroke with large vessel occlusion in France from 2015 to 2050 in men (A) women (B) and both (C) according to three scenarios: Scenario 1: stable age-and sex-specific incidence rates. Scenario 2: decrease in incidence rates of 0.5%/year in people over 65 years old. Scenario 3: decrease in incidence rates of 0.5%/year in overall population.
Due to an expected relative stable population < 50 years old in coming years and considering a stable incidence scenario, the number of cases of IS with LVO will not significantly change (−0.9% between 2015 and 2050) in this age group Figure 2. In case of a decrease in the incidence by 0.5%/year, we expect a decrease of cases by 16.8% in people <50 years old.
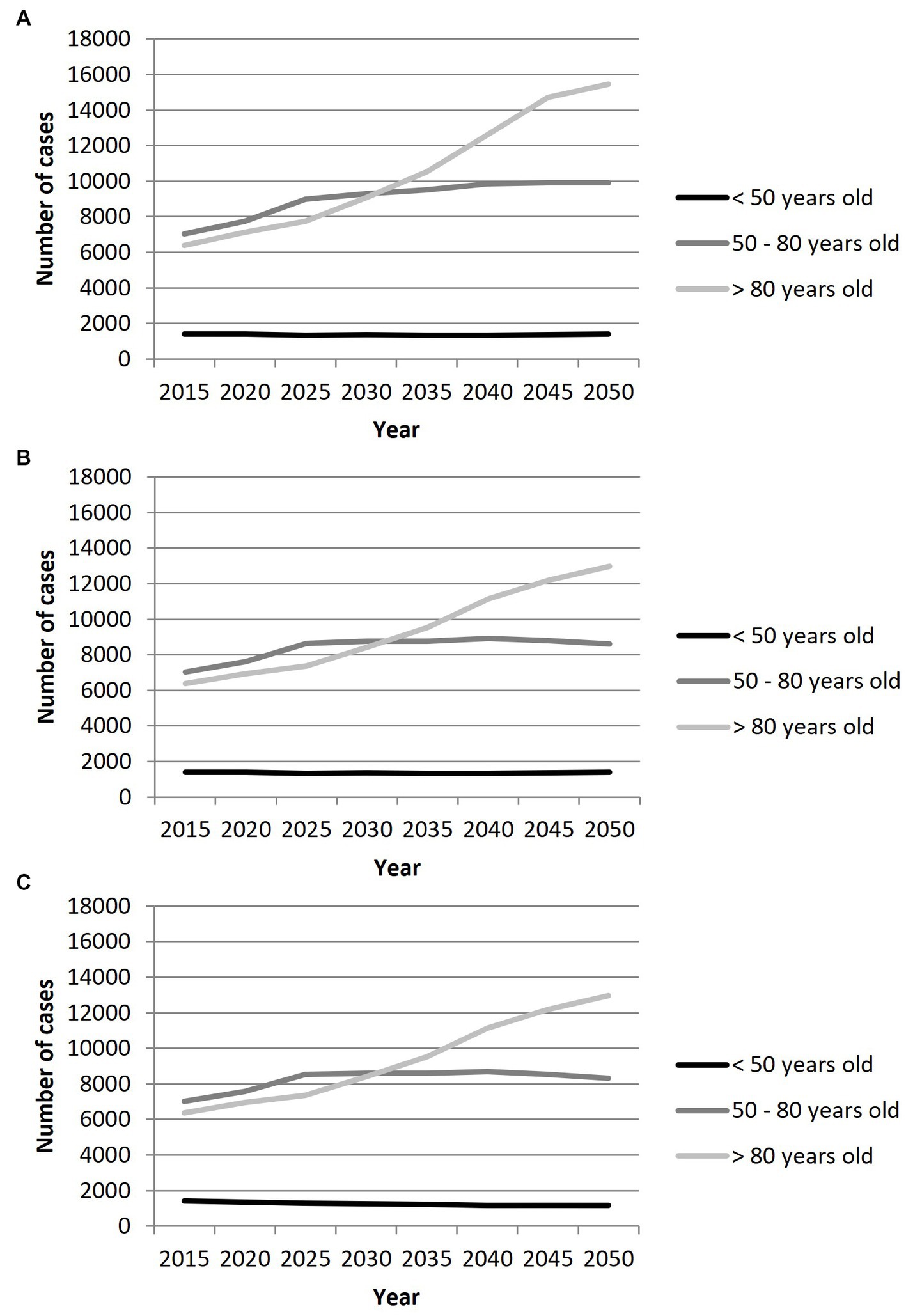
Figure 2. Projection of the number of cases of ischemic stroke with large vessel occlusion in France from 2015 to 2050 by age groups, according to three scenarios: (A) Scenario 1 with stable age-and sex-specific incidence rates; (B) Scenario 2 with a decrease in incidence rates of 0.5%/year in people over 65 years old; (C) Scenario 3 with a decrease in incidence rates of 0.5%/year in overall population.
Conversely, in the age group 50–80 years old, an increase in the number of cases by 41%, 23 and 18% according to the 3 incidence trends scenario, respectively, will be observed.
Finally, in individuals over 80 years, a steady increase in the number of cases of IS with LVO is expected throughout the study period. The increase is estimated to be by 142% considering a stable incidence scenario, and by 103% if the incidence decreases by 0.5%/year in this age group.
Considering, a stable or a decrease in the incidence in overall population, among IS patients with LVO, the proportion of individuals aged >80 years old will rise from 43% in 2015 to 57.7% in 2050, while that of individuals aged 50–80 years will decrease from 47.5 to 37.1%, and that of individuals <50 years old will decrease from 9.5 to 5.2% Figure 3. When considering a scenario of decreasing incidence by 0.5%/year in people >65 years old, the proportion of patients <50 years old years old will decrease from 9.5 to 6.1%, that of patients aged 50–80 years old will decrease from 47.5 to 37.5%, and that of patients >80 years old will increase from 43.0 to 56.4%.
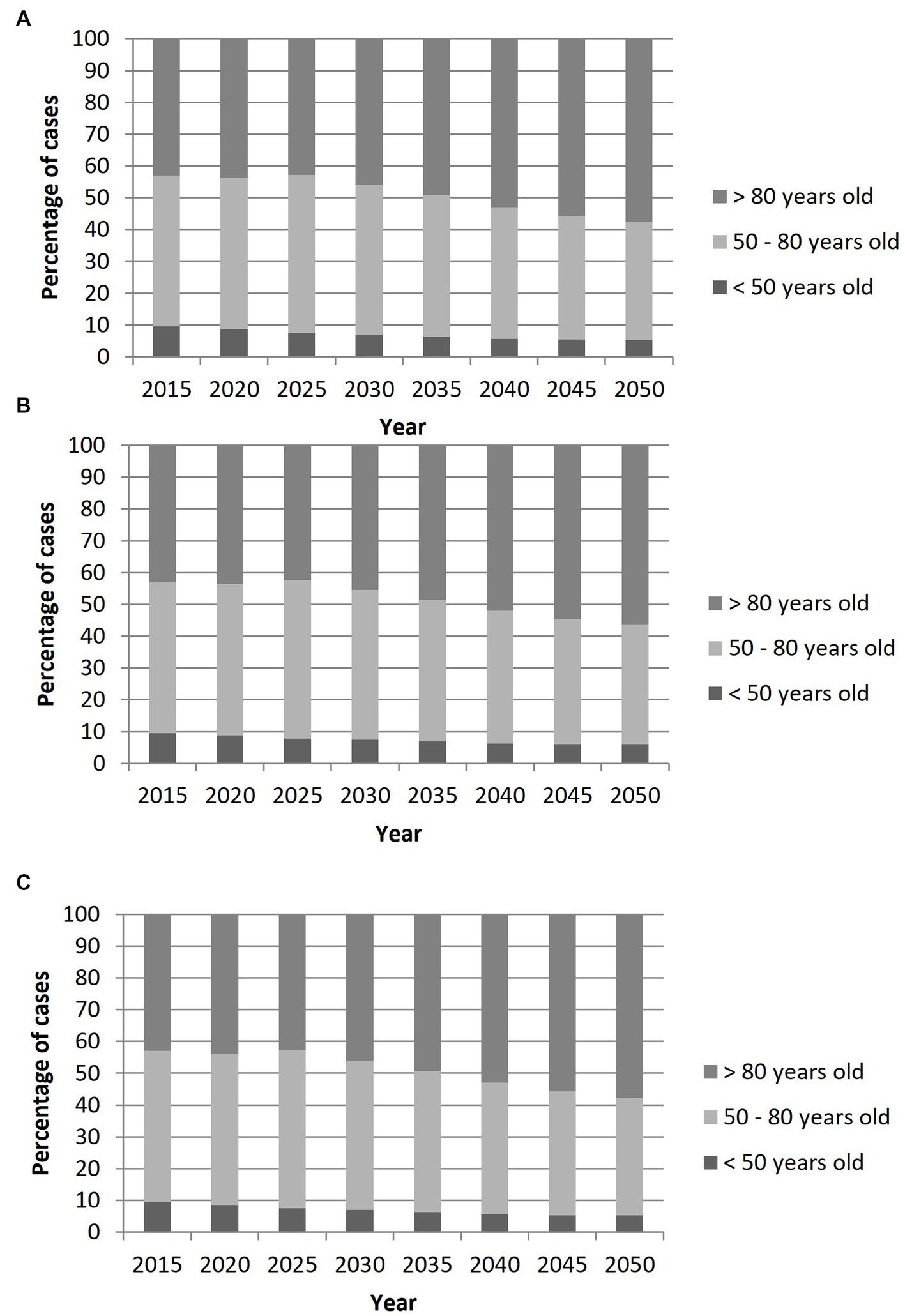
Figure 3. Projection of the age distribution of patients with ischemic stroke with large vessel occlusion in France from 2015 to 2050 according to three scenarios: (A) Scenario 1: stable age-and sex-specific incidences rates; (B) Scenario 2: decrease in incidence rates of 0.5%/year in people over 65 years old; (C) Scenario 3: decrease in incidence rates of 0.5%/year in overall population.
This study provides original information on nationwide projection of IS with LVO of the anterior circulation in coming years. In the absence of stroke registry covering whole France, these data are of importance to determine future needs for stroke care. Our findings point out a critical increase in the number of cases by 2050 due to the ongoing aging population. This increase will be mainly driven by a rise in the number of IS with LVO in people >80 years.
Our projections were made under the assumption of a stable standardized incidence by 2050, as observed in previous reports of the Dijon Stroke Registry (9). However, divergent findings were noted in other areas. For instance, a decrease by 28% in stroke incidence between the end of the 20th century and the beginning of the 21st century was reported in a meta-analysis including OXVASC study (10) and other European (11–22) and New Zealand (23, 24) population-based registries. Data from the Dijon Stroke Registry were included in this meta-analysis without decrease in the incidence in our population.
Similarly, the Global Burden of Disease (GBD) Study reported a decrease in age-standardised incidence of IS between 1990 and 2019. Therefore, we chose to report additional estimations according to two other scenarios based on an expected decrease in incidence rates (−0.5%/year in people over 65 years old, and −0.5%/year in overall population). Whatever the scenario considered, the projections remained globally unchanged, thus underlying that demographic changes will have a massive impact on the number of IS with LVO, and will overwhelm any improvement in stroke prevention. Of note, we only applied a maximum decrease in incidence of 0.5%/year, which is lower than the decrease reported by Li et al. (10) (−16% over the last 16 years) and projections of Wafa et al. (5) (−10% over 10 years). We chose this option because of specific causes of IS with LVO, i.e., a great frequency of cardioembolic source, especially atrial fibrillation (6). A review of population-and hospital-based studies showed that the recent decline in IS incidence was mostly driven by a decrease in lacunar stroke, whereas cardioembolic IS had increased by 2.4%/year (25), mainly because of a rise in the incidence of atrial fibrillation (26, 27). Therefore, we also proposed a model with no decrease in incidence in the age group under 65 years old, with data showing unchanged incidence in this age group since the beginning of the 21st century (17).
Recently, the Stroke Alliance for Europe anticipated a 34% increase in incident stroke events between 2015 and 2035 in Europe (28), which was consistent with a previous study from the Dijon Stroke Registry in which we estimated that according to demographic projections, the total number of annual stroke cases will increase by 55% between period 2009–2015 and year 2030 (29). Our present study adds to the literature by focusing on nationwide projection of cases of IS with LVO of the anterior circulation, which is of a great importance considering that such patients may be eligible for endovascular therapy, the achievement of which depends on a challenging care organization. Thanks to a systematic review of all arterial imaging exams by stroke-trained investigators, our estimates were based on observed cases of LVO of proximal occlusion, and not derived from proxies such as stroke severity. As others, we recently showed that clinical scales are not relevant enough to predict LVO in IS patients (30). To the best of our knowledge, this is the first time this approach has been used in a population-based study.
In addition, other studies reported the number of mechanical thrombectomy procedures using hospital database to approximate the incidence of IS with LVO (31, 32). Such a method underestimates the true burden of LVO given that it does not consider patients missed for a diagnosis of LVO, or who had no access to this treatment because of stroke care organization failure, or who were excluded from it for medical reasons.
Our results have major implications in both clinical practice and stroke care organization. Indeed, MT is a resource-intensive therapy, with a particular need for interventional neuroradiologists, thus limiting the development of new centers in a context of shortage of specialists. The expected rise in the number of IS with LVO threatens to saturate the existing TM-capable centers and to increase the need for medical transfers of patients. Therefore, the assessment of the number of strokes with proximal occlusion is crucial for the organization of the care pathway and the forecasting of resource needs in order to deploy them in the territories adequately. Then, IS with LVO are generally more severe and are associated with a poorer prognosis despite therapeutic advances, with many sequelae including cognitive or motor disabilities. This is particularly true for older patients, in whom the risk of institutionalization after stroke is high, raising the issue of the need for post-acute care facilities (33). This is all the more true since older patients will account for the vast majority of the increase in the total number of cases (29). It is therefore essential to foresee the weight that these subjects will represent in rehabilitation facilities, long stay units and retirement homes.
In our registry, we noted a stable age-standardized incidence of cerebrovascular disease with an increase in the number of cases in the past years (3). However, these observations need to be balanced. Indeed, we observed in our population of IS with LVO an over-representation of cardio-embolic stroke related to atrial fibrillation (AF) (6), whose prevalence is increasing (26). We cannot exclude that improvements in the diagnosis and treatment of AF may affect the future trends in the incidence of AF-related stroke.
The major strength of our study is the use for the first time of incidence rates obtained from a population-based registry to estimate the future number of cases of IS with LVO. Other studies have used estimations from databases to assess the annual number of MT (31, 32). Conversely, the aim of our study was to estimate the expected number of IS with LVO cases. However, not all these cases result in endovascular management. A study based on UK national registries estimate that approximately one third of IS with LVO are eligible for MT (31, 32). Moreover, the decision of MT takes into account various factors such advancing age, co-morbidities and impaired autonomy. These elements will have to be considered with the increase in the mean age of patients being managed for IS with LVO.
To conclude, knowledge of the future trends in the incidence of IS with LVO is a major issue to accurately anticipate dedicated resources needs. Our study demonstrated that a massive increase in IS with LVO is expected in the coming years, driven by an increasing number of patients.
The datasets presented in this article are not readily available because the data that support the findings of this study are available from the corresponding author, upon reasonable request. Requests to access the datasets should be directed to eWFubmljay5iZWpvdEBjaHUtZGlqb24uZnI=.
GD and YB contributed to the study conception and design. Data collection and analysis were performed by GD and YB. The first draft of the manuscript was written by GD and YB, and both authors commented on previous versions of the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by Santé Publique France, Institut National de la Santé et de la Recherche Médicale (INSERM), and Dijon University Hospital.
YB received honoraria for lectures or consulting fees from BMS, Pfizer, Medtronic, Amgen, Servier, and Novo-Nordisk, outside the submitted work.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Goyal, M, Menon, BK, van Zwam, WH, Dippel, DWJ, Mitchell, PJ, Demchuk, AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
2. Turc, G, Bhogal, P, Fischer, U, Khatri, P, Lobotesis, K, Mazighi, M, et al. European stroke organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical Thrombectomy in acute Ischaemic stroke endorsed by stroke Alliance for Europe (SAFE). Eur Stroke J. (2019) 4:6–12. doi: 10.1177/2396987319832140
3. Béjot, Y, Bailly, H, Durier, J, and Giroud, M. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. (2016) 45:e391–8. doi: 10.1016/j.lpm.2016.10.003
4. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
5. Wafa, HA, Wolfe, CDA, Emmett, E, Roth, GA, Johnson, CO, and Wang, Y. Burden of stroke in Europe: thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke. (2020) 51:2418–27. doi: 10.1161/STROKEAHA.120.029606
6. Duloquin, G, Graber, M, Garnier, L, Crespy, V, Comby, P-O, Baptiste, L, et al. Incidence of acute ischemic stroke with visible arterial occlusion: a population-based study (Dijon stroke registry). Stroke. (2020) 51:2122–30. doi: 10.1161/STROKEAHA.120.029949
7. Béjot, Y, Duloquin, G, Thomas, Q, Mohr, S, Garnier, L, Graber, M, et al. Temporal trends in the incidence of ischemic stroke in young adults: Dijon stroke registry. Neuroepidemiology. (2021) 55:239–44. doi: 10.1159/000516054
8. Available at: https://www.insee.fr/fr/statistiques/2496228.
9. Béjot, Y, Osseby, GV, Aboa-Eboulé, C, Durier, J, Lorgis, L, Cottin, Y, et al. Dijon’s vanishing lead with regard to low incidence of stroke. Eur J Neurol. (2009) 16:324–9. doi: 10.1111/j.1468-1331.2008.02415.x
10. Li, L, Scott, CA, and Rothwell, PM. Trends in stroke incidence in high-income countries in the 21st century. Stroke. (2020) 51:1372–80. doi: 10.1161/STROKEAHA.119.028484
11. Wolfe, CDA, Rudd, AG, Howard, R, Coshall, C, Stewart, J, Lawrence, E, et al. Incidence and case fatality rates of stroke subtypes in a multiethnic population: the South London stroke register. J Neurol Neurosurg Psychiatry. (2002) 72:211–6. doi: 10.1136/jnnp.72.2.211
12. Heuschmann, PU, Grieve, AP, Toschke, AM, Rudd, AG, and Wolfe, CDA. Ethnic group disparities in 10-year trends in stroke incidence and vascular risk factors: the South London stroke register (SLSR). Stroke. (2008) 39:2204–10. doi: 10.1161/STROKEAHA.107.507285
13. Kolominsky-Rabas, PL, Wiedmann, S, Weingärtner, M, Liman, TG, Endres, M, Schwab, S, et al. Time trends in incidence of pathological and etiological stroke subtypes during 16 years: the Erlangen stroke project. Neuroepidemiology. (2015) 44:24–9. doi: 10.1159/000371353
14. Correia, M, Magalhães, R, Felgueiras, R, Quintas, C, Guimarães, L, and Silva, MC. Changes in stroke incidence, outcome, and associated factors in Porto between 1998 and 2011. Int J Stroke. (2017) 12:169–79. doi: 10.1177/1747493016669846
15. Wolfe, CD, Giroud, M, Kolominsky-Rabas, P, Dundas, R, Lemesle, M, Heuschmann, P, et al. Variations in stroke incidence and survival in 3 areas of Europe. European registries of stroke (EROS) collaboration. Stroke. (2000) 31:2074–9. doi: 10.1161/01.str.31.9.2074
16. Béjot, Y, Daubail, B, Jacquin, A, Durier, J, Osseby, G-V, Rouaud, O, et al. Trends in the incidence of ischaemic stroke in young adults between 1985 and 2011: the Dijon stroke registry. J Neurol Neurosurg Psychiatry. (2014) 85:509–13. doi: 10.1136/jnnp-2013-306203
17. Aked, J, Delavaran, H, Norrving, B, and Lindgren, A. Temporal trends of stroke epidemiology in southern Sweden: a population-based study on stroke incidence and early case-fatality. Neuroepidemiology. (2018) 50:174–82. doi: 10.1159/000487948
18. Hallström, B, Jönsson, A-C, Nerbrand, C, Norrving, B, and Lindgren, A. Stroke incidence and survival in the beginning of the 21st century in southern Sweden: comparisons with the late 20th century and projections into the future. Stroke. (2008) 39:10–5. doi: 10.1161/STROKEAHA.107.491779
19. Johansson, B, Norrving, B, and Lindgren, A. Increased stroke incidence in Lund-Orup, Sweden, between 1983 to 1985 and 1993 to 1995. Stroke. (2000) 31:481–6. doi: 10.1161/01.str.31.2.481
20. Rothwell, PM, Coull, AJ, Giles, MF, Howard, SC, Silver, LE, Bull, LM, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford vascular study). Lancet. (2004) 363:1925–33. doi: 10.1016/S0140-6736(04)16405-2
21. Olindo, S, Chausson, N, Mejdoubi, M, Jeannin, S, Rosillette, K, Saint-Vil, M, et al. Trends in incidence and early outcomes in a Black Afro-Caribbean population from 1999 to 2012: Etude Réalisée en Martinique et Centrée sur l’Incidence des Accidents Vasculaires Cérébraux II Study. Stroke. (2014) 45:3367–73. doi: 10.1161/STROKEAHA.114.005930
22. Appelros, P. Secular trends of stroke epidemiology in Örebro, Sweden, 2017 compared to the trends in 1999: a population-based study. Cerebrovasc Dis. (2019) 48:149–56. doi: 10.1159/000504082
23. Feigin, VL, Krishnamurthi, RV, Barker-Collo, S, McPherson, KM, Barber, PA, Parag, V, et al. 30-year trends in stroke rates and outcome in Auckland, New Zealand (1981-2012): a multi-ethnic population-based series of studies. PLoS One. (2015) 10:e0134609. doi: 10.1371/journal.pone.0134609
24. Krishnamurthi, RV, Barker-Collo, S, Parag, V, Parmar, P, Witt, E, Jones, A, et al. Stroke incidence by major pathological type and ischemic subtypes in the Auckland regional community stroke studies. Stroke. (2018) 49:3–10. doi: 10.1161/STROKEAHA.117.019358
25. Ornello, R, Degan, D, Tiseo, C, Di Carmine, C, Perciballi, L, Pistoia, F, et al. Distribution and temporal trends from 1993 to 2015 of ischemic stroke subtypes. Stroke. (2018) 49:814–9. doi: 10.1161/STROKEAHA.117.020031
26. Kornej, J, Börschel, CS, Benjamin, EJ, and Schnabel, RB. Epidemiology of atrial fibrillation in the 21st century. Circ Res. (2020) 127:4–20. doi: 10.1161/CIRCRESAHA.120.316340
27. Wu, J, Nadarajah, R, Nakao, YM, Nakao, K, Wilkinson, C, Mamas, MA, et al. Temporal trends and patterns in atrial fibrillation incidence: a population-based study of 3·4 million individuals. Lancet Regional Health Europe. (2022) 17:100386. doi: 10.1016/j.lanepe.2022.100386
28. Available at: https://www.stroke.org.uk/sites/default/files/the_burden_of_stroke_in_europe_-_challenges_for_policy_makers.pdf.
29. Béjot, Y, Bailly, H, Graber, M, Garnier, L, Laville, A, Dubourget, L, et al. Impact of the ageing population on the burden of stroke: the Dijon stroke registry. Neuroepidemiology. (2019) 52:78–85. doi: 10.1159/000492820
30. Duloquin, G, Graber, M, Garnier, L, Mohr, S, Giroud, M, Vergely, C, et al. Assessment of clinical scales for detection of large vessel occlusion in ischemic stroke patients from the Dijon stroke registry. J Clin Med. (2021) 10:5893. doi: 10.3390/jcm10245893
31. McMeekin, P, White, P, James, MA, Price, CI, Flynn, D, and Ford, GA. Estimating the number of UK stroke patients eligible for endovascular thrombectomy. Eur Stroke J. (2017) 2:319–26. doi: 10.1177/2396987317733343
32. McMeekin, P, Flynn, D, James, M, Price, CI, Ford, GA, and White, P. Updating estimates of the number of UK stroke patients eligible for endovascular thrombectomy: incorporating recent evidence to facilitate service planning. Eur Stroke J. (2021) 6:349–56. doi: 10.1177/23969873211059471
Keywords: ischemic stroke, registries, epidemiology, large vessel occlusion, population-based studies
Citation: Duloquin G and Béjot Y (2023) Nationwide projections of ischemic stroke with large vessel occlusion of the anterior circulation by 2050: Dijon Stroke Registry. Front. Public Health. 11:1142134. doi: 10.3389/fpubh.2023.1142134
Received: 11 January 2023; Accepted: 09 May 2023;
Published: 25 May 2023.
Edited by:
Mei-Xue Dong, Renmin Hospital of Wuhan University, ChinaReviewed by:
Paolo Sciarrone, Gabriele Monasterio Tuscany Foundation (CNR), ItalyCopyright © 2023 Duloquin and Béjot. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yannick Béjot, eWFubmljay5iZWpvdEBjaHUtZGlqb24uZnI=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.