Abstract
Background:
Several studies have examined the effects of city-level meteorological conditions on the associations between meteorological factors and hand, foot, and mouth disease (HFMD) risk. However, evidence that city-level meteorological conditions modify air pollutant-HFMD associations is lacking.
Methods:
For each of the 17 cities in the Sichuan Basin, we obtained estimates of the relationship between exposures to multiple air pollutants and childhood HFMD risk by using a unified distributed lag nonlinear model (DLNM). Multivariate meta-regression models were used to identify the effects of city-level meteorological conditions as effect modifiers. Finally, we conducted subgroup analyses of age and sex to explore whether the modification effects varied in different subgroups.
Results:
The associations between PM2.5/CO/O3 and HFMD risk showed moderate or substantial heterogeneity among cities ( statistics: 48.5%, 53.1%, and 61.1%). Temperature conditions significantly modified the PM2.5-HFMD association, while relative humidity and rainfall modified the O3-HFMD association. Low temperatures enhanced the protective effect of PM2.5 exposure against HFMD risk [PM2.5 <32.7 μg/m3 or PM2.5 >100 μg/m3, at the 99th percentile: relative risk (RR) = 0.14, 95% CI: 0.03–0.60]. Low relative humidity increased the adverse effect of O3 exposure on HFMD risk (O3 >128.7 μg/m3, at the 99th percentile: RR = 2.58, 95% CI: 1.48–4.50). However, high rainfall decreased the risk of HFMD due to O3 exposure (O3: 14.1–41.4 μg/m3). In addition, the modification effects of temperature and relative humidity differed in the female and 3–5 years-old subgroups.
Conclusion:
Our findings revealed moderate or substantial heterogeneity in multiple air pollutant-HFMD relationships. Temperature, relative humidity, and rainfall modified the relationships between PM2.5 or O3 exposure and HFMD risk.
1. Introduction
Hand, foot, and mouth disease (HFMD), a widespread viral infectious disease, mainly affects children through enteroviruses (1–3), such as enterovirus 71 and coxsackievirus A16. HFMD may be transmitted via the fecal-oral route or respiratory droplets. Over the past few decades, many countries and regions, especially the Asia-Pacific region (4, 5), have experienced large HFMD outbreaks. Since 2008, HFMD has been listed as a notifiable Class C infectious disease in China. In 2019, the number of HFMD cases reached 1,918,830, and the incidence rate was 137.4 per 100,000 people, ranking second among all notifiable infectious diseases in China (6). The high incidence rate and lack of specific drug treatments indicate that HFMD still imposes a substantial public health burden in China.
Many studies have explored the environmental risk factors for HFMD. Meteorological factors, especially temperature and relative humidity, have been widely studied (7–12). With rapid increases in industrialization and urbanization, ambient air pollution has been exacerbated. Growing evidence indicates that air pollution may cause adverse health outcomes (13–15). For instance, Ibrahim et al. (16) found that exposure to fine particulate matter (diameter ≤2.5 μm; PM2.5) and SO2 increased the impacts of respiratory diseases in hospitalized children. Children under 5 years old are vulnerable to HFMD. As their lungs may still be developing and their immune defenses are immature, they are more likely to be adversely affected by exposure to air pollution (17–19). Therefore, the short-term exposure-response associations between air pollutants and pediatric HFMD risk has received increasing attention in recent years (20–22).
However, previous studies have indicated that the exposure-response relationships between air pollutants and HFMD had heterogeneity. For instance, Huang et al. (23) found that PM10 was not significantly related to HFMD morbidity. However, Peng et al. (20) found that extremely high or low concentrations of PM10 had adverse effects on HFMD. Furthermore, a seasonal analysis revealed that the effect of PM10 exposure on the relative risk (RR) of HFMD was significantly higher in the cold season (24). Regarding the O3-HFMD association, Gu et al. (25) found that O3 exposure was significantly associated with HFMD (RR = 2.12, 95% CI: 1.47–3.05), while Yan et al. (21) found that O3 exposure (>104 μg/m3) reduced HFMD risk. The heterogeneity of short-term associations may be due to the modification effects of meteorological conditions (12, 26–29). Previous studies have suggested that meteorological conditions may affect the relationship between air pollutant exposure and respiratory health. A study found that the relationship between chronic bronchitis and total suspended particulate matter (TSP) may be modified by humidity. Lower humidity may exacerbate the hazardous effects of TSP (30). Another study found that temperature may modify the effect of the air pollution index (API) on respiratory morbidity (31). Therefore, we predicted that meteorological conditions may also modify the relationships between air pollutant exposure and HFMD risk. Regarding the meteorological factor-HFMD associations, a previous study suggested that the diurnal temperature range modified the relationship between temperature and pediatric HFMD (32). Another study found that city-specific climate indicators, including temperature, sunshine duration, and air pressure, modified the relative humidity-HFMD association (27). However, to our knowledge, there is no evidence that meteorological conditions modify the air pollutant-HFMD associations.
The Sichuan Basin, a region with the fourth-highest air pollution in China, contains approximately 90% of the resident population of Sichuan Province (33). Located in the subtropical monsoon region, with deep mountain-basin topographic characteristics, the Sichuan Basin has a low average wind speed and a foggy and wet climate. These complex topographic and meteorological conditions make air stagnation more likely and prevent diffusion of air pollutants in the basin after excessive emission (33–36).
The objective of this study was to examine the modification effects of meteorological conditions as effect modifiers on air pollutant-HFMD associations. We adopted a multicity, unified distributed lag nonlinear model (DLNM)-based, two-stage time series study of 17 cities in the Sichuan Basin. In addition, since it is well known that meteorological factors are important environmental factors associated with HFMD, we simultaneously considered these meteorological factors to provide a more comprehensive understanding of HFMD risk in the Sichuan Basin.
2. Methods
2.1. Study area
The Sichuan Basin is in eastern Sichuan Province, which is located in southwestern China, with an area of approximately 160,000 square kilometers. We analyzed 17 prefecture-level cities in the Sichuan Basin, which is in the subtropical monsoon zone and has a humid climate. The meteorological conditions of cities in the Sichuan Basin were based on the latitudinal zonal climate, as the layered zonal climate varied (33, 37).
2.2. Data collection
Daily HFMD case counts of 17 cities from January 2015 to December 2017 were provided by the Sichuan Provincial Center for Disease Control and Prevention.1 This study analyzed HFMD cases in children aged 0–5 years. In the subgroup analysis of age, the cases were divided into three subgroups, age < 1 year, 1 ≤ age < 3 years, and 3 ≤ age < 6 years, to represent cases in infants, preschool children, and kindergarten children, respectively.
Daily meteorological data were extracted from the National Meteorological Science Data Center.2 The variables included daily average temperature (°C), daily average relative humidity (%), sunshine duration (hours), daily average wind speed (m/s), daily average air pressure (hPa), and daily average rainfall (mm). Daily air pollutant data were collected from the Sichuan Environmental Monitoring Center,3 including the daily average SO2 concentration (μg/m3), daily average NO2 (μg/m3), daily average PM10 (μg/m3), daily average PM2.5 (μg/m3), daily average CO (mg/m3), daily average O3 (μg/m3), and daily air quality index (AQI). A detailed description of the air quality station and meteorological monitoring station in the Sichuan Basin is provided in Supplementary Tables S1, S2. For the city-level meteorological conditions, we calculated the arithmetic average of the daily data of the meteorological variables (26, 27, 32) (including temperature, relative humidity, sunshine duration, wind speed, and rainfall) of each city in the study period (Supplementary Table S3).
2.3. Statistical analysis
2.3.1. Construction of a unified DLNM to obtain city-specific estimates
We used a DLNM in this study due to the nonlinearity and lag of HFMD surveillance data. Proposed by Gasparrini et al. (38–40), DLNMs can simultaneously consider nonlinear associations and lagged effects between environmental exposure and health outcomes. Currently, DLNMs are commonly used for environmental and epidemiological time series analysis (28, 41).
Spearman correlation analysis showed that PM10 concentrations, PM2.5 concentrations, and AQI values were highly correlated. Thus, PM2.5 concentrations were selected for further analysis. The city-specific time series HFMD case data were overdispersed (Supplementary Table S4), so we adopted a common DLNM based on a quasi-Poisson distribution (38, 42) to investigate the exposure-lag response relationships between meteorological factors, air pollutants, and HFMD case counts for each city. Referring to prior knowledge (8, 26) and the results of a systematic sensitivity analysis (Supplementary Text S1, Supplementary Figures S1–S7, and Supplementary Tables S5–S8), we determined the DLNM, which was constructed as follows:
where represents the HFMD case count on day ; is the intercept term; and is the examined variables of meteorological factors and air pollution, including temperature, relative humidity, wind speed, and concentrations of PM2.5, CO and O3. is the cross-basis function, which can simultaneously describe the relationship between the exposure-response dimension and the lag-response dimension between the explanatory variable and the dependent variable. The exposure dimension used the natural cubic spline (ns) function with two equal knots. The lag dimension also adopted the ns function with 3 degrees of freedom (). The lag period was defined as 0 to 14 days, which encompasses the incubation and infectious periods of HFMD (20, 22). The average incubation period of HFMD is usually defined as 3–5 days (43), and the disease usually ends within 7 to 10 days (44). contains the sunshine duration, rainfall, and concentrations of NO2 and SO2. Sunshine duration, NO2 and SO2 were controlled by calculating a simple moving average with a lag period of 0 to 14 days. Rainfall was determined by calculating the exponential moving average with a lag period of 0 to 14 days and adopting the ns function with 3 . The seasonality and long-term trend used an ns function with 8 to control annually. is an autoregressive term that converted the daily cases data to a logarithmic scale and incorporated the first and second lags; indicates the day of the week, and is the national holiday date.
2.3.2. Pooled city-specific estimates and exploration of the modification effects of city-level meteorological conditions by multivariate meta-regression models
We summed the lagged effects over 0–14 days to obtain the cumulative associations for each city. The overall cumulative exposure-response associations of the Sichuan Basin were obtained by pooling the city-specific estimates (39, 40). The Cochran Q test was performed to examine whether the heterogeneity of city-specific cumulative associations was statistically significant, and statistics were calculated to determine the proportion of heterogeneity in the total variation (45, 46). In this study, we determined the grade of heterogeneity by Cochrane’s evaluation criteria (47). Taking the intercept-only meta-regression model as a reference, multivariate meta-regression models were further conducted to analyze the modification effect of meteorological conditions. As meta-predictors, meteorological conditions were added to fit the meta-regression model individually. We selected the likelihood ratio (LR) test to evaluate the modification effect. Meteorological condition variables with p < 0.2 in the LR test were included in the subsequent multiple meta-predictor regression model as alternative variables. We fitted all candidate subsets in the models, and the best multiple meta-regression model was identified as the one with the lowest Akaike information criterion (AIC). AIC values reflect the goodness of fit of models. Moreover, ΔI2 was calculated to determine the proportion of the heterogeneity explained by the modifier. All of the statistical analyses in this study were performed in R software (4.0.3) using the dlnm and mvmeta packages, and statistical significance was tested as p < 0.05.
3. Results
3.1. Descriptive statistics of daily HFMD case counts
From January 1st, 2015 to December 31st, 2017, the total number of HFMD cases in 17 prefecture-level cities in the Sichuan Basin was 187,823. The time series distribution of HFMD case counts showed an effect of season. There were two peaks in HFMD case counts throughout the year. One peak was in April–July (summer), and the other was October–December (winter) (Figure 1).
Figure 1
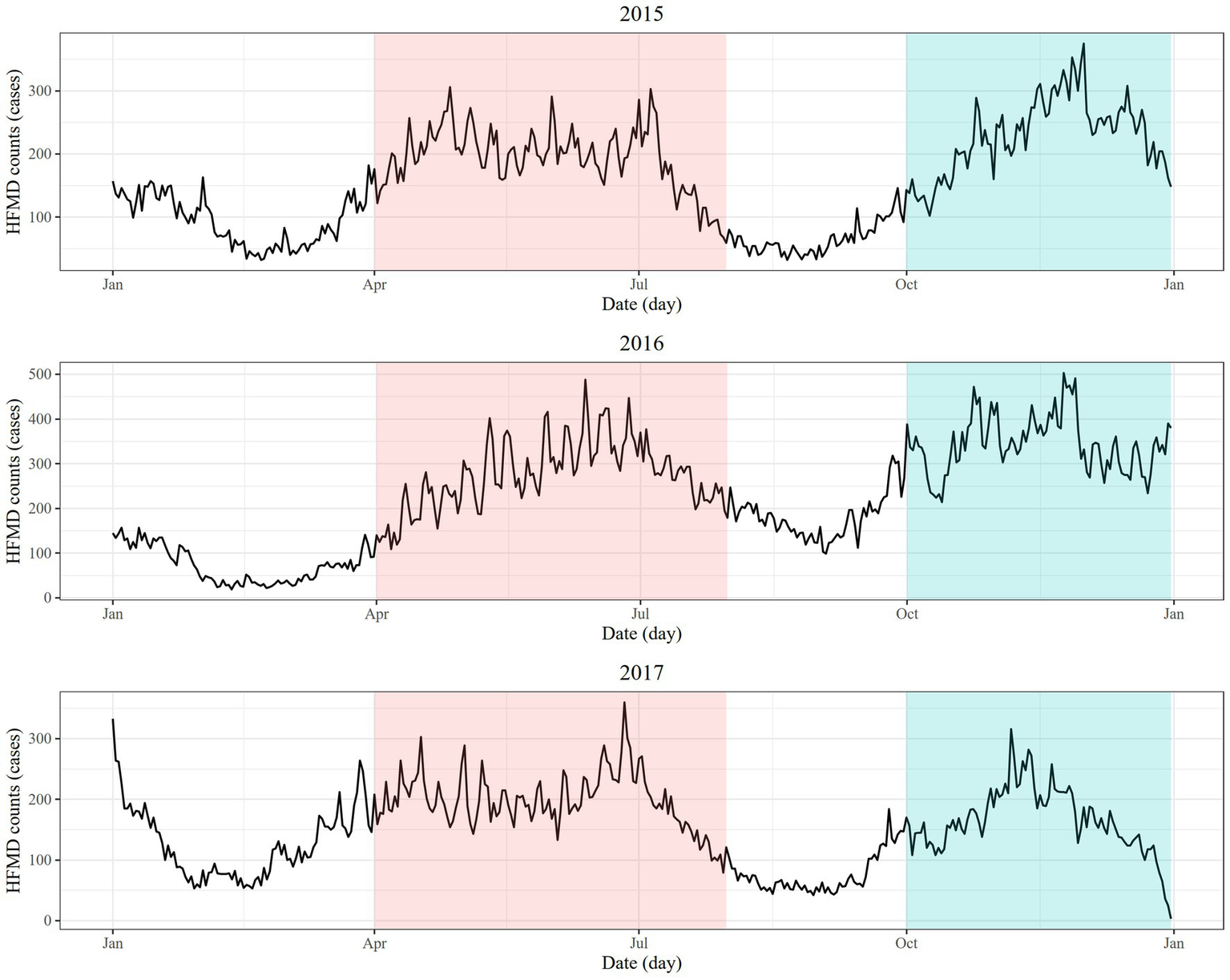
Daily time series of the number of HFMD cases in 2015, 2016, and 2017 (red shade: April-July, blue shade: October-December).
3.2. The heterogeneity of overall pooled estimates of the exposure-response relationships
Table 1 shows the heterogeneity results of the associations between the overall cumulative meteorological factors and air pollutants with HFMD risk. The exposure-response associations of all study variables had statistically significant heterogeneity. The proportions of heterogeneity (in terms of I2 values) in the temperature-HFMD, wind speed-HFMD, and relative humidity-HFMD associations were 31.3%, 34.9%, and 54.1%, respectively. The association between PM2.5 concentrations and HFMD risk showed moderate heterogeneity, with an value of 48.5%. The associations of CO and O3 concentrations with HFMD risk showed substantial heterogeneity, with values of 53.1% and 61.1%, respectively.
Table 1
| Variable | Cochran Q test | Model fit | Heterogeneity | Heterogeneity grade | ||
|---|---|---|---|---|---|---|
| Q | df | p | AIC | I 2(%) | (Cochrane’s evaluation criteria) | |
| Temperature | 69.85 | 48 | 0.021 | 134.89 | 31.3 | Moderate |
| Wind speed | 73.73 | 48 | 0.010 | 149.23 | 34.9 | Moderate |
| Relative humidity | 104.59 | 48 | <0.001 | 149.92 | 54.1 | Substantial |
| PM2.5 | 93.24 | 48 | <0.001 | 156.60 | 48.5 | Moderate |
| CO | 102.27 | 48 | <0.001 | 157.84 | 53.1 | Substantial |
| O3 | 123.35 | 48 | <0.001 | 150.48 | 61.1 | Substantial |
The heterogeneity results of the overall cumulative exposure-response associations.
3.3. Modification effects of meteorological conditions on the overall cumulative relationships among air pollutants, meteorological factors and HFMD
Table 2 shows significant modification effects of the meteorological conditions on air pollutant-HFMD associations. The ΔAICs of all models indicated that after adding the meta-predictors, the model fit improved. Temperature (p = 0.037) modified the PM2.5-HFMD association, with explaining 1% of the heterogeneity ( statistic). Relative humidity (p = 0.047) and rainfall (p = 0.028) individually modified the O3-HFMD association, and the ΔI2 values showed proportions of explained heterogeneity of 2.6% and 3.5%. The joint modification effects of relative humidity, wind speed, and rainfall on the O3-HFMD association explained more of the heterogeneity than any single effect modifier, explaining 11.2% of the heterogeneity.
Table 2
| Exposure | Modifier | LR test | Cochran Q test | Model fit | Heterogeneity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stats | df | p | Q | df | p | AIC | ΔAIC | I 2 | ΔI2 | ||
| Single meta-predictor model | |||||||||||
| Temperature | Reference | 69.85 | 48 | 0.021 | 134.89 | — | 31.3 | — | |||
| Temperature | 8.64 | 3 | 0.034 | 58.89 | 45 | 0.080 | 132.25 | −2.64 | 23.6 | −7.7 | |
| Wind speed | Reference | — | — | — | 73.73 | 48 | 0.010 | 149.23 | — | 34.9 | — |
| Relative humidity | 9.19 | 3 | 0.027 | 53.94 | 45 | 0.170 | 146.04 | −3.19 | 16.6 | −18.3 | |
| PM2.5 | Reference | — | — | — | 93.24 | 48 | <0.001 | 156.60 | — | 48.5 | — |
| Temperature | 8.49 | 3 | 0.037 | 85.79 | 45 | <0.001 | 154.11 | −2.49 | 47.5 | −1 | |
| O3 | Reference | — | — | — | 123.35 | 48 | <0.001 | 150.48 | — | 61.1 | — |
| Relative humidity | 7.97 | 3 | 0.047 | 108.55 | 45 | <0.001 | 148.52 | −1.96 | 58.5 | −2.6 | |
| Rainfall | 9.09 | 3 | 0.028 | 106.09 | 45 | <0.001 | 147.39 | −3.09 | 57.6 | −3.5 | |
| Multiple meta-predictors model | |||||||||||
| Temperature | Temperature + relative humidity | 14.85 | 6 | 0.021 | 51.02 | 42 | 0.16 | 132.03 | −2.86 | 17.7 | −13.6 |
| O3 | Relative humidity + wind speed + rainfall | 23.26 | 9 | 0.006 | 77.79 | 39 | <0.001 | 145.23 | −5.25 | 49.9 | −11.2 |
Significant meteorological condition modifiers and multivariate meta-regression model results.
In addition, meteorological conditions modified the meteorological factor-HFMD relationships. Temperature-HFMD and wind speed-HFMD associations were modified by temperature (p = 0.034) and relative humidity (p = 0.027). The results of ΔI2 showed proportions of explained heterogeneity of 7.7 and 18.3%, respectively. The joint modification effects of temperature and relative humidity on the temperature-HFMD association showed that 13.6% of heterogeneity was explained. Complete results of the modification effects of meteorological conditions on the meteorological factor/air pollutant-HFMD associations are described in Supplementary Tables S9–S14.
Using the pooled cumulative exposure-HFMD relationship curves as a reference, predicted relationship curves at the 10th and 90th percentiles of statistically significant meteorological conditions were drawn separately, as shown in Figure 2. Temperature, relative humidity, and rainfall modified the relationship between air pollutant exposures and HFMD risk. Temperature modified the PM2.5-HFMD association. Predicted at the 10th percentile (14.8°C), temperature significantly enhanced the protective effects of PM2.5 exposure against HFMD risk under high and low levels of PM2.5 concentrations (PM2.5 <32.7 μg/m3 or PM2.5 >100 μg/m3). At the 99th percentile of PM2.5 concentrations, the RR was 0.14 (95% CI: 0.03–0.60). The plot showed that the RR was decreasing, and the predicted curve became steeper. At the 90th percentile (18.6°C) of temperature, we found only a very small range of PM2.5 concentrations in which the predicted curve was statistically significant. For the modification effects of relative humidity on the O3-HFMD association, at the 10th percentile, relative humidity showed an enhanced effect on the right side, with the RR increasing quickly when the O3 concentration was higher than 129.7 μ/m3. At the 99th percentile of O3 concentrations, the RR was 2.58 (95% CI: 1.48–4.50). Rainfall also modified the O3-HFMD association. At the 90th percentile, rainfall significantly modified the O3-HFMD association at low O3 concentrations (14.1–41.4 μg/m3), enhancing the protective effect of O3. At the 5th percentile of O3 concentrations, the RR was 0.75 (95% CI: 0.56–0.99).
Figure 2
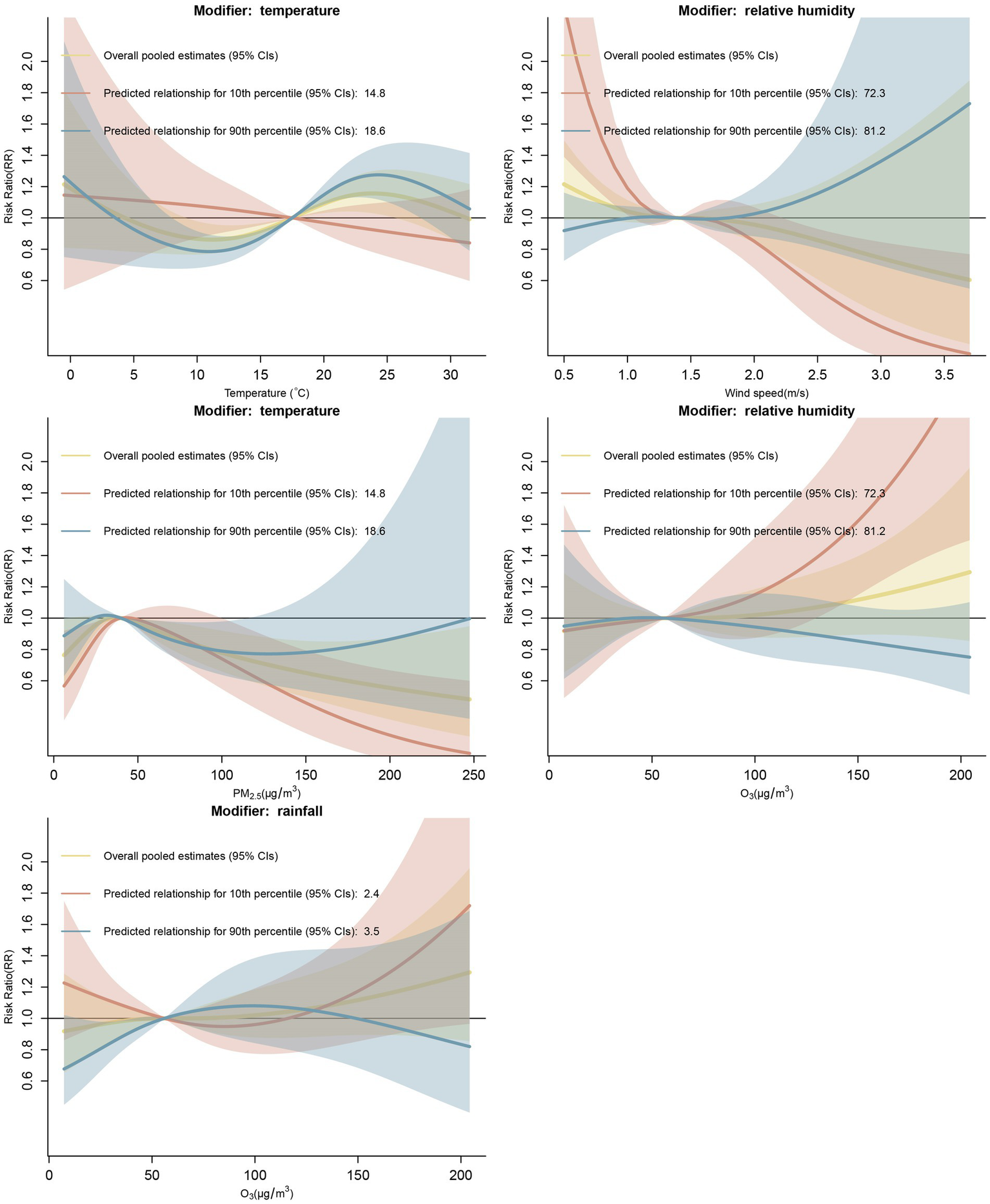
At the 10th and 90th percentiles, meteorological conditions modified the pooled cumulative exposure-HFMD associations (median value of the variables set as reference).
Figure 3 shows the results of subgroup analyses. We observed that temperature modified the PM2.5-HFMD association in the female subgroup. In the age subgroup analysis, we observed that relative humidity modified the O3-HFMD association in the 3–5 years-old subgroup at the 90th percentile, and a protective effect was found at high O3 concentrations, in contrast to other age subgroup analyses.
Figure 3
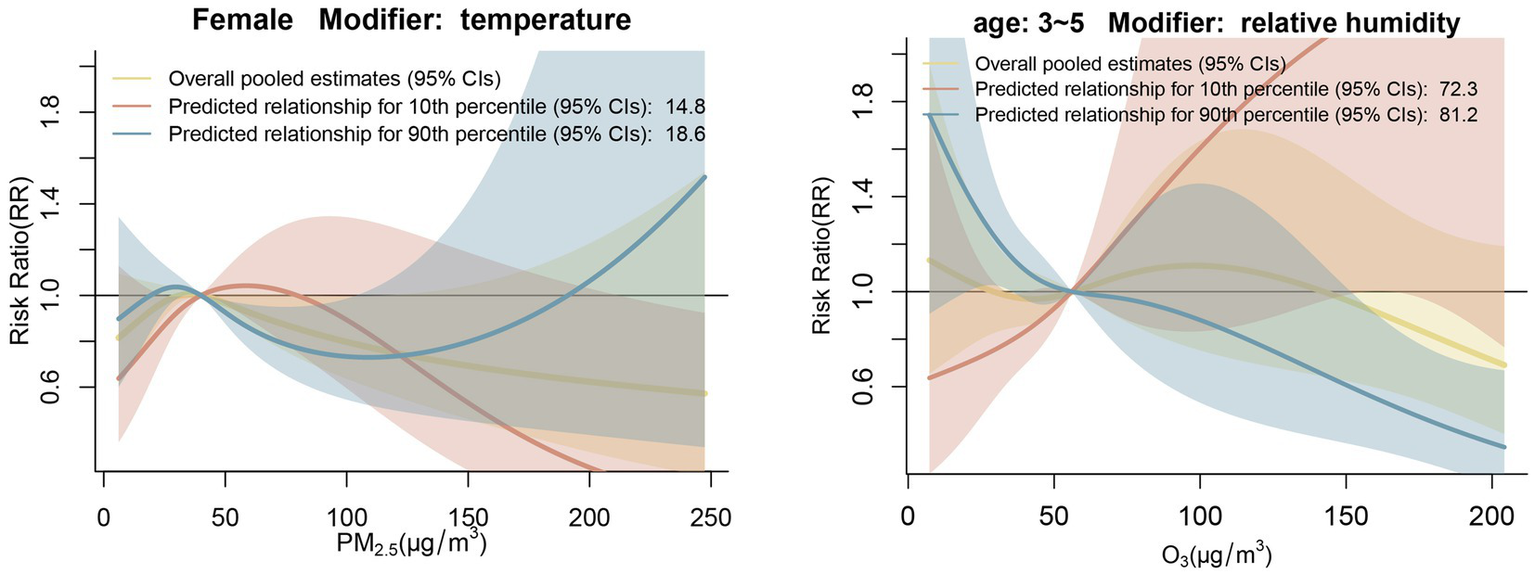
Subgroup analysis by gender and age At the 10th and 90th percentiles, meteorological conditions modified the pooled cumulative exposure-HFMD associations.
For the meteorological factor-HFMD associations, temperature and relative humidity were effect modifiers. At the 90th percentile (18.6°C), temperature significantly modified the temperature-HFMD association, with greater modification effects at the high-temperature level. The effect mainly changed the magnitude of the RR rather than the shape of the predicted curve. At the 10th percentile (72.3%), relative humidity significantly modified the wind speed-HFMD association. At a relatively high wind speed (>2.3 m/s), the association curve became steeper, and the curve slope decreased, which indicated a strong protective effect of wind speed against HFMD risk. However, at the left tail of the predicted curve, relative humidity increased the adverse effect of wind speed on HFMD risk. We observed that when the wind speed was 0.5 m/s, the RR was 2.36 (95% CI: 1.39–4.00).
4. Discussion
We began by exploring the heterogeneity of short-term associations between exposure to different air pollutants, including PM2.5, CO, and O3, and the number of HFMD cases in the Sichuan Basin. We found that these associations had moderate or substantial heterogeneity, with statistics of 48.5%, 53.1%, and 61.1% for PM2.5, CO, and O3, respectively. Second, we analyzed the modification effects of meteorological conditions on the air pollutant-HFMD associations. Overall, temperature significantly modified the PM2.5-HFMD association, while relative humidity and rainfall modified the O3-HFMD association. To our knowledge, this is the first study to explore the modification effects of meteorological conditions on air pollutant-HFMD associations.
There is some evidence of heterogeneity in the meteorological factor-HFMD associations (9, 27, 48, 49). For example, a study in mainland China found that 77.8% of the residual heterogeneity in the relative humidity-HFMD association was attributable to differences between cities (27). However, studies on the heterogeneity of multiple air pollutant-HFMD associations are limited. Our multicity study showed that the effects of PM2.5, CO, and O3 concentrations on HFMD risk exhibited moderate or substantial heterogeneity, which may provide a reference for future research.
For the PM2.5-HFMD associations, we found that the association curve exhibited an inverse “V” shape and that low and high PM2.5 concentrations exerted a protective effect against HFMD risk. For the modification effects, we concluded that low temperature modified and strengthened the PM2.5-HFMD association. In contrast, a study in northeast Asia found that extremely high temperatures may exacerbate the adverse effects of air pollutants on human health (50). Other studies have found that temperature modified the effect of particulate matter on influenza incidence and cardiorespiratory disease mortality (51–53), but the underlying mechanisms remain unclear. Similarly, evidence that temperature modifies the PM2.5-HFMD association is complicated, and still not yet clear. However, there are some plausible explanations for our findings. It is well known that low temperatures may restrict the survival and reproduction of viruses (9, 12, 54). Therefore, during the cold period, the activity of viruses may have been inhibited by low temperatures. Additionally, people would have less opportunity to inhale particulate matter containing viruses, especially at low PM2.5 concentrations. Experimental evidence indicated that particulate matter led to airway hyperresponsiveness and oxidative stress (55, 56). However, during the cold period with heavy PM2.5 pollution, guardians of children would pay attention to the forecasted air quality and keep their children at home. This behavior greatly reduced the risk of exposure to heavy PM2.5 pollution of vulnerable HFMD populations in a cold environment.
For the pooled O3-HFMD associations, we found substantial heterogeneity. We further analyzed the modification effect of meteorological conditions and found that relative humidity and rainfall modified this association. Remarkably, low relative humidity intensified the adverse effect of high O3 concentrations on HFMD risk. Leitte et al. (30) also found that dry air may increase the risk of air pollutant exposure for respiratory health since the respiratory airways of individuals seem to be protected by higher humidity. Compared with fog–haze weather mainly caused by PM2.5, O3 pollution may not attract much attention from parents, and children may engage in more outdoor activity on days with low relative humidity, which may have a higher human body comfort index than that on days with high relative humidity. Hence, owing to the immature host defense system and easy infection by respiratory pathogens (57), susceptible children may have a higher risk of infection. Furthermore, Yin et al. (58) found that for each 10 μ/m3 increase in O3 concentration, the estimated daily total mortality increased by 0.24%. Public health policymakers should devote more attention to specific meteorological conditions that aggravate the impact of high air pollutant concentrations on HFMD risk and develop targeted countermeasures. For example, during periods with severe ozone pollution and low relative humidity, programs to increase public awareness could be conducted in kindergartens, primary schools, etc. Children should be reminded to wear masks or reduce their outdoor activity in such conditions to reduce the health impacts of air pollution. From a sustainable development perspective, clean energy, such as nuclear and wind power, could be developed to reduce emissions from industries, vehicle exhaust, etc., and improve environmental quality (59). In this way, the influence of air pollution on HFMD risk may also be decreased.
In addition, we found that high rainfall conditions enhanced the protective effect of low O3 concentrations on HFMD risk. Heavy rainfall may restrict the outdoor activity of children, which may reduce exposure to O3 and further reduce the probability of contact between susceptible populations and infected children, thus decreasing the influence of O3 concentrations on HFMD risk. However, the exact mechanism by which rainfall conditions modify the O3-HFMD association is not clear and merits further study.
For the CO-HFMD association, although there was substantial heterogeneity among regions, we did not identify significant modification effects of meteorological conditions. The heterogeneity of the CO-HFMD association may be caused by other factors besides meteorological conditions, such as geographical factors.
This is the first study to explore the modification effect of city-level meteorological conditions on air pollutant-HFMD associations, expanding our understanding of the effect of air pollution on HFMD risk. Our findings have practical implications in two aspects. First, in the development of public health policies, our findings suggest that meteorological conditions and air pollutants jointly affected the incidence of HFMD. For instance, to mitigate the harmful effects of O3 concentrations on the incidence of HFMD, different policies should be implemented in the rainy and dry seasons. Second, in the development of individual-level interventions, our study can serve as a reference. Children should adopt healthy hygiene habits, such as washing their hands before meals and after going to the bathroom. Parents or guardians should take care to reduce children’s outdoor activities during HFMD outbreaks. In addition, it is essential to check the weather forecast and air quality before going outside.
However, some limitations should be acknowledged in our study. First, this is an ecological study. Due to the characteristics of our study design, our findings cannot be used to prove causality. Additionally, we did not consider spatial correlations in our study. This issue will be considered in further research.
5. Conclusion
Our findings suggest that meteorological conditions modified the air pollutant-HFMD associations in the Sichuan Basin. Specifically, temperature, relative humidity, and rainfall partly explained heterogeneity in the associations of PM2.5 or O3 concentrations with HFMD risk. The complex interaction between meteorological conditions and air pollution indicates that it is necessary to consider the joint effects of these environmental factors to obtain more accurate insights into HFMD risk. Our findings could inform the development of effective regional public health strategies for the prevention and control of HFMD.
Funding
This work was supported by the National Natural Science Foundation of China (Grant nos. 81872713 and 81803332), the Sichuan Science and Technology Program (Grant nos. 2021YFS0181 and 2022YFS0641), and Chongqing Science and Technology Program (Grant no. cstc2020jscx-cylhX0003; URL: http://kjj.cq.gov.cn/).
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The datasets presented in this article are not readily available because the datasets generated and/or analyzed in this study are available from Sichuan Center for Disease Control and Prevention. The authors used the data for this current study under a license from the Sichuan CDC, so the data cannot be shared publicly. Requests to access the datasets should be directed to https://www.sccdc.cn/.
Ethics statement
Our study was carried out in accordance with relevant guidelines and regulations and approved by the Institutional Review Board of the School of Public Health, Sichuan University. The daily HFMD data used in this current study were aggregated at the city level by counts, so no confidential information was involved in this study, and the study was exempt from ethical approval procedures.
Author contributions
WC, YM, and TS designed the study. CY, TZ, and HZ collected the data. WC, CL, and XG performed the analysis and interpreted the results. WC, YM, YZ, and FY coordinated and drafted the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1140639/full#supplementary-material
Footnotes
References
1.
Xing W Liao Q Viboud C Zhang J Sun J Wu JT et al . Hand, foot, and mouth disease in China, 2008–12: an epidemiological study. Lancet Infect Dis. (2014) 14:308–18. doi: 10.1016/S1473-3099(13)70342-6
2.
Zhu F Xu W Xia J Liang Z Liu Y Zhang X et al . Efficacy, safety, and immunogenicity of an enterovirus 71 vaccine in China. N Engl J Med. (2014) 370:818–28. doi: 10.1056/NEJMoa1304923
3.
Aswathyraj S Arunkumar G Alidjinou EK Hober D . Hand, foot and mouth disease (HFMD): emerging epidemiology and the need for a vaccine strategy. Med Microbiol Immunol. (2016) 205:397–407. doi: 10.1007/s00430-016-0465-y
4.
Chan LG Parashar UD Lye MS Ong FGL Zaki SR Alexander JP et al . Deaths of children during an outbreak of hand, foot, and mouth disease in Sarawak, Malaysia: clinical and pathological characteristics of the disease. Clin Infect Dis. (2000) 31:678–83. doi: 10.1086/314032
5.
Van Tu P Thao NTT Perera D Huu TK Tien NTK Thuong TC et al . Epidemiologic and virologic investigation of hand, foot, and mouth disease, southern Vietnam, 2005. Emerg Infect Dis. (2007) 13:1733–41. doi: 10.3201/eid1311.070632
6.
Overview of the National Epidemic of Notifiable Infectious Diseases in 2019: National Bureau of Disease Control and Prevention; (2020) Available at: http://www.nhc.gov.cn/jkj/s3578/202004/b1519e1bc1a944fc8ec176db600f68d1.shtml (Accessed January 7, 2023).
7.
Qi H Chen Y Xu D Su H Zhan L Xu Z et al . Impact of meteorological factors on the incidence of childhood hand, foot, and mouth disease (HFMD) analyzed by DLNMs-based time series approach. Infect Dis Poverty. (2018) 7:7. doi: 10.1186/s40249-018-0388-5
8.
Zhu L Wang X Guo Y Xu J Xue F Liu Y . Assessment of temperature effect on childhood hand, foot and mouth disease incidence (0–5 years) and associated effect modifiers: a 17 cities study in Shandong Province, China, 2007–2012. Sci Total Environ. (2016) 551–552:452–9. doi: 10.1016/j.scitotenv.2016.01.173
9.
Xu Z Hu W Jiao K Ren C Jiang B Ma W . The effect of temperature on childhood hand, foot and mouth disease in Guangdong Province, China, 2010–2013: a multicity study. BMC Infect Dis. (2019) 19:969. doi: 10.1186/s12879-019-4594-y
10.
Zhang Z Xie X Chen X Li Y Lu Y Mei S et al . Short-term effects of meteorological factors on hand, foot and mouth disease among children in Shenzhen, China: non-linearity, threshold and interaction. Sci Total Environ. (2016) 539:576–82. doi: 10.1016/j.scitotenv.2015.09.027
11.
Hao J Yang Z Yang W Huang S Tian L Zhu Z et al . Impact of ambient temperature and relative humidity on the incidence of hand-foot-mouth disease in Wuhan, China. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17020428
12.
Cheng Q Bai L Zhang Y Zhang H Wang S Xie M et al . Ambient temperature, humidity and hand, foot, and mouth disease: a systematic review and meta-analysis. Sci Total Environ. (2018) 625:828–36. doi: 10.1016/j.scitotenv.2018.01.006
13.
Doiron D de Hoogh K Probst-Hensch N Fortier I Cai Y De Matteis S et al . Air pollution, lung function and COPD: results from the population-based UK Biobank study. Eur Respir J. (2019) 54:1802140. doi: 10.1183/13993003.02140-2018
14.
Ye X Peng L Kan H Wang W Geng F Mu Z et al . Acute effects of particulate air pollution on the incidence of coronary heart disease in Shanghai, China. PLoS One. (2016) 11:e0151119. doi: 10.1371/journal.pone.0151119
15.
Lu X Yuan D Chen Y Fung JCH . Impacts of urbanization and long-term meteorological variations on global PM2.5 and its associated health burden. Environ Pollut. (2021) 270:116003. doi: 10.1016/j.envpol.2020.116003
16.
Ibrahim MF Hod R Tajudin MABA Mahiyuddin WRW Nawi AM Sahani M . Children’s exposure to air pollution in a natural gas industrial area and their risk of hospital admission for respiratory diseases. Environ Res. (2022) 210:112966. doi: 10.1016/j.envres.2022.112966
17.
Liu SL Pan H Liu P Amer S Chan TC Zhan J et al . Comparative epidemiology and virology of fatal and nonfatal cases of hand, foot and mouth disease in mainland China from 2008 to 2014. Rev Med Virol. (2015) 25:115–28. doi: 10.1002/rmv.1827
18.
Samoli E Nastos PT Paliatsos AG Katsouyanni K Priftis KN . Acute effects of air pollution on pediatric asthma exacerbation: evidence of association and effect modification. Environ Res. (2011) 111:418–24. doi: 10.1016/j.envres.2011.01.014
19.
Atkinson RW Anderson HR Strachan DP Bland JM Bremner SA Ponce de Leon A . Short-term associations between outdoor air pollution and visits to accident and emergency departments in London for respiratory complaints. Eur Respir J. (1999) 13:257–65. doi: 10.1183/09031936.99.13225799
20.
Peng H Chen Z Cai L Liao J Zheng K Li S et al . Relationship between meteorological factors, air pollutants and hand, foot and mouth disease from 2014 to 2020. BMC Public Health. (2022) 22:998. doi: 10.1186/s12889-022-13365-9
21.
Yan S Wei L Duan Y Li H Liao Y Lv Q et al . Short-term effects of meteorological factors and air pollutants on hand, foot and mouth disease among children in Shenzhen, China, 2009–2017. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16193639
22.
Yu G Li Y Cai J Yu D Tang J Zhai W et al . Short-term effects of meteorological factors and air pollution on childhood hand-foot-mouth disease in Guilin, China. Sci Total Environ. (2019) 646:460–70. doi: 10.1016/j.scitotenv.2018.07.329
23.
Huang R Bian G He T Chen L Xu G . Effects of meteorological parameters and PM10 on the incidence of hand, foot, and mouth disease in children in China. Int J Environ Res Public Health. (2016) 13. doi: 10.3390/ijerph13050481
24.
Yang Z Hao J Huang S Yang W Zhu Z Tian L et al . Acute effects of air pollution on the incidence of hand, foot, and mouth disease in Wuhan, China. Atmos Environ. (2020) 225:117358. doi: 10.1016/j.atmosenv.2020.117358
25.
Gu S Li D Lu B Huang R Xu G . Associations between ambient air pollution and daily incidence of pediatric hand, foot and mouth disease in Ningbo, 2014–2016: a distributed lag nonlinear model. Epidemiol Infect. (2020) 148:e46. doi: 10.1017/S0950268820000321
26.
Xiao X Gasparrini A Huang J Liao Q Liu F Yin F et al . The exposure-response relationship between temperature and childhood hand, foot and mouth disease: a multicity study from mainland China. Environ Int. (2017) 100:102–9. doi: 10.1016/j.envint.2016.11.021
27.
Bo Z Ma Y Chang Z Zhang T Liu F Zhao X et al . The spatial heterogeneity of the associations between relative humidity and pediatric hand, foot and mouth disease: evidence from a nation-wide multicity study from mainland China. Sci Total Environ. (2020) 707:136103. doi: 10.1016/j.scitotenv.2019.136103
28.
Qi H Li Y Zhang J Chen Y Guo Y Xiao S et al . Quantifying the risk of hand, foot, and mouth disease (HFMD) attributable to meteorological factors in East China: a time series modelling study. Sci Total Environ. (2020) 728:138548. doi: 10.1016/j.scitotenv.2020.138548
29.
Leone M D’Ippoliti D De Sario M Analitis A Menne B Katsouyanni K et al . A time series study on the effects of heat on mortality and evaluation of heterogeneity into European and eastern-southern Mediterranean cities: results of EU CIRCE project. Environ Health. (2013) 12:55. doi: 10.1186/1476-069X-12-55
30.
Leitte AM Petrescu C Franck U Richter M Suciu O Ionovici R et al . Respiratory health, effects of ambient air pollution and its modification by air humidity in Drobeta-Turnu Severin, Romania. Sci Total Environ. (2009) 407:4004–11. doi: 10.1016/j.scitotenv.2009.02.042
31.
Song X Jiang L Wang S Tian J Yang K Wang X et al . The impact of main air pollutants on respiratory emergency department visits and the modification effects of temperature in Beijing, China. Environ Sci Pollut Res Int. (2021) 28:6990–7000. doi: 10.1007/s11356-020-10949-z
32.
Hu Y Liu F Zhao X Ma Y Lan T Yang F et al . The modification effect of the diurnal temperature range on the exposure-response relationship between temperature and pediatric hand, foot and mouth disease. Sci Total Environ. (2020) 722:137921. doi: 10.1016/j.scitotenv.2020.137921
33.
Ning G Wang S Ma M Ni C Shang Z Wang J et al . Characteristics of air pollution in different zones of Sichuan Basin, China. Sci Total Environ. (2018) 612:975–84. doi: 10.1016/j.scitotenv.2017.08.205
34.
Li Y Chen Q Zhao H Wang L Tao R . Variations in PM10, PM2.5 and PM1.0 in an urban area of the Sichuan Basin and their relation to meteorological factors. Atmosphere. (2015) 6:150–63. doi: 10.3390/atmos6010150
35.
Chen Y Xie S . Temporal and spatial visibility trends in the Sichuan Basin, China, 1973 to 2010. Atmos Res. (2012) 112:25–34. doi: 10.1016/j.atmosres.2012.04.009
36.
Chen Y Xie S Luo B Zhai C . Characteristics and origins of carbonaceous aerosol in the Sichuan Basin, China. Atmos Environ. (2014) 94:215–23. doi: 10.1016/j.atmosenv.2014.05.037
37.
Li X Hussain SA Sobri S Md Said MS . Overviewing the air quality models on air pollution in Sichuan Basin, China. Chemosphere. (2021) 271:129502. doi: 10.1016/j.chemosphere.2020.129502
38.
Gasparrini A Armstrong B Kenward MG . Distributed lag non-linear models. Stat Med. (2010) 29:2224–34. doi: 10.1002/sim.3940
39.
Gasparrini A Armstrong B Kenward MG . Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med. (2012) 31:3821–39. doi: 10.1002/sim.5471
40.
Gasparrini A Armstrong B . Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med Res Methodol. (2013) 13:1. doi: 10.1186/1471-2288-13-1
41.
Zhao R Gao Q Hao Q Wang S Zhang Y Li H et al . The exposure-response association between humidex and bacillary dysentery: a two-stage time series analysis of 316 cities in mainland China. Sci Total Environ. (2021) 797:148840. doi: 10.1016/j.scitotenv.2021.148840
42.
Gasparrini A . Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. (2011) 43:1–20.
43.
Esposito S Principi N . Hand, foot and mouth disease: current knowledge on clinical manifestations, epidemiology, aetiology and prevention. Eur J Clin Microbiol Infect Dis. (2018) 37:391–8. doi: 10.1007/s10096-018-3206-x
44.
Cox B Levent F . Hand, foot, and mouth disease. JAMA. (2018) 320:2492. doi: 10.1001/jama.2018.17288
45.
Fan C Liu F Zhao X Ma Y Yang F Chang Z et al . An alternative comprehensive index to quantify the interactive effect of temperature and relative humidity on hand, foot and mouth disease: a two-stage time series study including 143 cities in mainland China. Sci Total Environ. (2020) 740:140106. doi: 10.1016/j.scitotenv.2020.140106
46.
Gasparrini A Guo Y Hashizume M Kinney PL Petkova EP Lavigne E et al . Temporal variation in heat-mortality associations: a multicountry study. Environ Health Perspect. (2015) 123:1200–7. doi: 10.1289/ehp.1409070
47.
Higgins J Thomas J Chandler J Cumpston M Li T Page M et al eds. Cochrane handbook for systematic reviews of interventions version 6.3Cochrane (2022). Available at: www.training.cochrane.org/handbook
48.
Yi X Chang Z Zhao X Ma Y Liu F Xiao X . The temporal characteristics of the lag-response relationship and related key time points between ambient temperature and hand, foot and mouth disease: a multicity study from mainland China. Sci Total Environ. (2020) 749:141679. doi: 10.1016/j.scitotenv.2020.141679
49.
Luo C Qian J Liu Y Lv Q Ma Y Yin F . Long-term air pollution levels modify the relationships between short-term exposure to meteorological factors, air pollution and the incidence of hand, foot and mouth disease in children: a DLNM-based multicity time series study in Sichuan Province, China. BMC Public Health. (2022) 22:1484. doi: 10.1186/s12889-022-13890-7
50.
Lee W Choi HM Kim D Honda Y Leon Guo YL Kim H . Synergic effect between high temperature and air pollution on mortality in Northeast Asia. Environ Res. (2019) 178:108735. doi: 10.1016/j.envres.2019.108735
51.
Ren C Tong S . Temperature modifies the health effects of particulate matter in Brisbane, Australia. Int J Biometeorol. (2006) 51:87–96. doi: 10.1007/s00484-006-0054-7
52.
Meng X Zhang YH Zhao ZH Duan XL Xu XH Kan HD . Temperature modifies the acute effect of particulate air pollution on mortality in eight Chinese cities. Sci Total Environ. (2012) 435-436:215–21. doi: 10.1016/j.scitotenv.2012.07.008
53.
Zhang R Meng Y Song H Niu R Wang Y Li Y et al . The modification effect of temperature on the relationship between air pollutants and daily incidence of influenza in Ningbo, China. Respir Res. (2021) 22:153. doi: 10.1186/s12931-021-01744-6
54.
Zhu L Yuan Z Wang X Li J Wang L Liu Y et al . The impact of ambient temperature on childhood HFMD incidence in inland and coastal area: a two-city study in Shandong Province, China. Int J Environ Res Public Health. (2015) 12:8691–704. doi: 10.3390/ijerph120808691
55.
Guarnieri M Balmes JR . Outdoor air pollution and asthma. Lancet. (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
56.
Stanek LW Brown JS Stanek J Gift J Costa DL . Air pollution toxicology—a brief review of the role of the science in shaping the current understanding of air pollution health risks. Toxicol Sci. (2011) 120:S8–S27. doi: 10.1093/toxsci/kfq367
57.
Li Q Wang HJ Song Y Ma J Song JY Guo YM . Association between children’s forced vital capacity and long-term exposure to local ambient temperature in China: a national cross-sectional survey. Sci Total Environ. (2016) 557-558:880–7. doi: 10.1016/j.scitotenv.2016.02.135
58.
Yin P Chen R Wang L Meng X Liu C Niu Y et al . Ambient ozone pollution and daily mortality: a nationwide study in 272 Chinese cities. Environ Health Perspect. (2017) 125:117006. doi: 10.1289/EHP1849
59.
Pata UK Samour A . Do renewable and nuclear energy enhance environmental quality in France? A new EKC approach with the load capacity factor. Prog Nucl Energy. (2022) 149:104249. doi: 10.1016/j.pnucene.2022.104249
Summary
Keywords
meteorological conditions, air pollution-HFMD associations, modification effects, air pollution, two-stage analysis
Citation
Cai W, Luo C, Geng X, Zha Y, Zhang T, Zhang H, Yang C, Yin F, Ma Y and Shui T (2023) City-level meteorological conditions modify the relationships between exposure to multiple air pollutants and the risk of pediatric hand, foot, and mouth disease in the Sichuan Basin, China. Front. Public Health 11:1140639. doi: 10.3389/fpubh.2023.1140639
Received
10 January 2023
Accepted
26 June 2023
Published
11 July 2023
Volume
11 - 2023
Edited by
Mohsen Saeedi, University Canada West, Canada
Reviewed by
Zhongjun Shao, Air Force Medical University, China; Jianpeng Wang, Central South University, China; Worradorn Phairuang, Kanazawa University, Japan; Ahmed Samour, Near East University, Cyprus
Updates
Copyright
© 2023 Cai, Luo, Geng, Zha, Zhang, Zhang, Yang, Yin, Ma and Shui.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Ma, gordonrozen@scu.edu.cnTiejun Shui, shuitiejunynjkedu@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.