
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 14 March 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1139832
This article is part of the Research TopicNeonatal Sepsis: Current Insights and ChallengesView all 11 articles
Background: Neonatal infections, especially neonatal sepsis, are one of the major causes of incidence and mortality in pediatrics. However, the global burden of neonatal sepsis and other neonatal infections (NSNIs) remains unclear.
Methods: From the 2019 global disease burden study, we collected annual incident cases, deaths, age-standardized incidence rates (ASIRs), and age-standardized deaths rates (ASDRs) of NSNIs in the past 30 years. Analysis indicators included the percentage of relative changes in incident cases and deaths, and the estimated annual percentage changes (EAPCs) of ASIRs and ASDRs. Correlations were assessed between the EAPCs of ASIRs and ASDRs and social evaluation indicators, including sociodemographic index (SDI) and universal health coverage index (UHCI).
Results: Globally, the number of incident cases of NSNIs grew by 12.79% per year, and the number of deaths dropped by 12.93% per year. During this period, global ASIR of NSNIs increased by 46% annually on average, while ASDR decreased by 53% annually on average. The ASIR and ASDR of female NSNIs were consistently lower than that of male NSNIs. The EAPC of female ASIR was 0.61, nearly twice that of male ASIR, and female ASIR was growing rapidly. The same declining trends of ASDR were noted in males and females. The ASIR of NSNIs in high-SDI regions grew by an average of 14% annually from 1990 to 2019. Except for high-SDI regions, the ASIRs of other 4 SDI regions maintained a rising trend at a high level, and were improved in the past 10 years. The ASDRs of all 5 SDI regions generally showed a downward trend. The region with the highest ASIR of NSNIs was Andean Latin America, and Western Sub-Saharan Africa had the highest mortality. We found a negative correlation between EAPCs of ASDRs and UHCI in 2019.
Conclusion: The global health situation was still not optimal. The incidence of NSNIs remained high, and continues to rise. The mortality of NSNIs has decreased, especially in the countries/territories with high UHCI. Therefore, it is crucial to improve the overall awareness and management of NSNIs, and take interventions for NSNIs worldwide.
Neonatal infections refer to the disease caused by the infection of pathogenic microorganisms (bacterial, viral, or fungal) in newborns, including neonatal sepsis, neonatal pneumonia and other neonatal infections, the most common pathogens of which include group B Streptococcus (GBS), Escherichia coli, and herpes simplex virus (HSV) (1, 2). In the past decades, the mechanism of neonatal susceptibility to infection has been extensively studied. Neonatal immature immunity has been implicated for the higher neonatal infection rate (3). Preterm infants, compared with term infants, showed more immature immune responses and had a higher risk of infection (1, 4, 5). Another risk factor was neonatal environmental exposure, such as the maternal history of exposure to infectious diseases and bacterial colonization (6, 7).
Neonatal infections, especially neonatal sepsis, are one of the major causes of incidence and mortality in pediatrics (2). In 2015, 600,000 of newborns died of infection worldwide (8). The 2016 Global Burden of Disease Study illustrated that neonatal sepsis and other neonatal infections (NSNIs) ranked third in neonatal deaths (243,000 deaths per year), and also ranked at the forefront of years of lost life across all age groups (9). It was reported that South Asia and Sub-Saharan Africa had the highest burden of neonatal sepsis, and the total incidence of culture-positive sepsis reported by South Asian hospitals was 15.8 per 1,000 live births (10). This was about 2–4 times higher than the rate reported in the United Kingdom and the United States (1, 11). To reduce the incidence and mortality of NSNIs, measures should be taken based on national and regional incidence and mortality data for NSNIs and related factors.
As far as we know, there is no detailed and systematic study to illustrate the incidence and mortality of NSNIs, and the relationship with national socio-economic status and medical health level. Therefore, we collected Global Burden of Disease 2019 data to assess the global incidence and mortality characteristics of NSNIs and the relationship with national socio-economic status and medical health level, so as to provide a more comprehensive view for the development of global and regional interventions to prevent and control NSNIs health care policies.
The GBD 2019 study performed an all-round epidemiological assessment of 369 diseases and injuries (by age and sex) in 204 countries and territories worldwide in the past 30 years (12). The details of the GBD study have been reported before (12–14). The specific protocols are available in the GBD website (https://www.healthdata.org/gbd/about/protocol).
From the Global Health Data Exchange (GHDx) query tool, we collected annual incident cases, deaths, age-standardized incidence rates (ASIRs), and age-standardized deaths (ASDRs) of NSNIs in the past 30 years. A total of 204 countries and territories were included, which were divided into 5 sociodemographic index (SDI) regions and 21 GBD regions.
The SDI can quantitatively reveal the development status of the country/territory, and it is obtained by comprehensive evaluation of the overall fertility rates of women under the age of 25, the average education level of women aged 15 and above, and the per capita income (15). The SDI values range from 0 to 1. The smaller the SDI, the lower the level of sociodemographic development. The SDIs are provided in the GHDx. The SDIs of 204 countries and territories in 2019 (SDI 2019) are used for subsequent analyses.
Universal health coverage (UHC) refers to the access of all people to the quality health services they need without experiencing financial hardship (16). The UHCI comprises 23 indicators, of which 4 are used to measure intervention coverage, and 19 are based on mortality to measure the quality of care obtained (16). The UHCI is scored on a scale of 0 (less developed) to 100 (most developed). The UHCIs are provided in the GHDx. The UHCIs of 204 countries and territories in 2019 (UHCI 2019) are used for subsequent analyses.
Analysis indicators included the percentage of relative changes in incident cases and deaths, and the estimated annual percentage changes (EAPCs) of ASIRs and ASDRs to characterize the trends in the incidence and mortality of NSNIs. The percentage of relative change in the number of incidents cases and deaths was calculated as reported (17). The formulas for ASIR and ASDR have been described previously (18, 19). EAPC is a measure that reflects trends in the age-standardized rate (ASR) in a certain interval, and its calculation method was described before (20). The EAPC and lower boundary of 95% confidence interval (CI) both >0 indicated an upward trend. Conversely, when both the EAPC and the upper boundary of the 95% CI were lower than 0, ASR showed a downward trend.
In addition, the correlations between the EAPCs of ASIRs and ASDRs and social evaluation indicators (SDI 2019; UHCI 2019) were assessed by Pearson correlation analysis in 204 countries and territories to identify potential factors affecting EAPCs. All analyses were conducted using in R (version 4.1.2). The threshold value of P is 0.05.
On a global scale, the number of incident cases of NSNIs showed a rise of 12.79% (5.59 million in 1990 to 6.31 million in 2019), and the number of deaths of NSNIs declined by 12.93% (260,000 in 1990 to 227,000 in 2019) (Table 1). In males, the number of global incident cases of NSNIs grew by 10.09% annually, and the number of deaths dropped by 12.54% annually. In females, the number of global incident cases of NSNIs grew by 19.52% annually, and the number of deaths dropped by 11.13% annually. After age standardization, the ASIR of NSNIs ascended [EAPC = 0.46 (95% CI, 0.43 to 0.48)] from 85.21 per 100,000 in 1990 to 97.43 per 100,000 in 2019 (Table 2), and the ASDR of NSNIs declined over this period by an average of 0.53 per year (95% CI, −0.72 to −0.35; from 3.97 per 100,000 in 1990 to 3.50 per 100,000 in 2019; Table 2). Overall, the ASIR showed an increasing trend year by year worldwide, with similar trend in males and females, and the ASIR of females was lower than that of males (Figure 1A). It can be noted that the ASIR of male NSNIs (ASIR: 99.74 per 100,000) was higher than that of females (ASIR: 94.96 per 100,000) in 2019 (Table 2). The EAPC of female ASIR was 0.61, nearly twice that of male ASIR, indicating that female ASIR increased rapidly. From 1990 to 2019, the global ASDR initially rose, plateaued between 1999 and 2005, and then declined (Figure 1B). The trend was the same for males and females, with males having higher ASDR than females (Figure 1B).
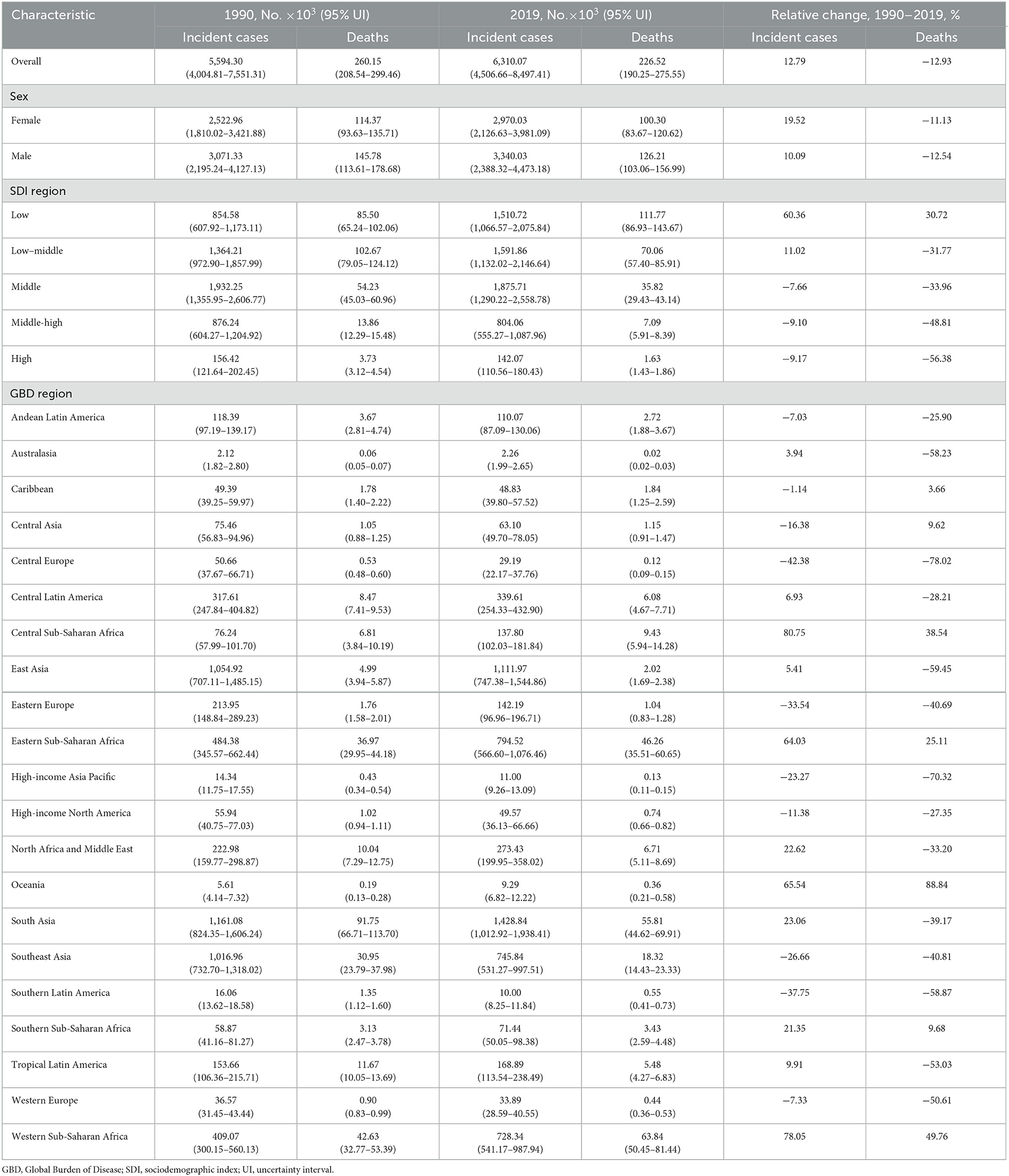
Table 1. Incident cases and deaths of NSNIs in 1990 and 2019 and their change trends from 1990 to 2019.
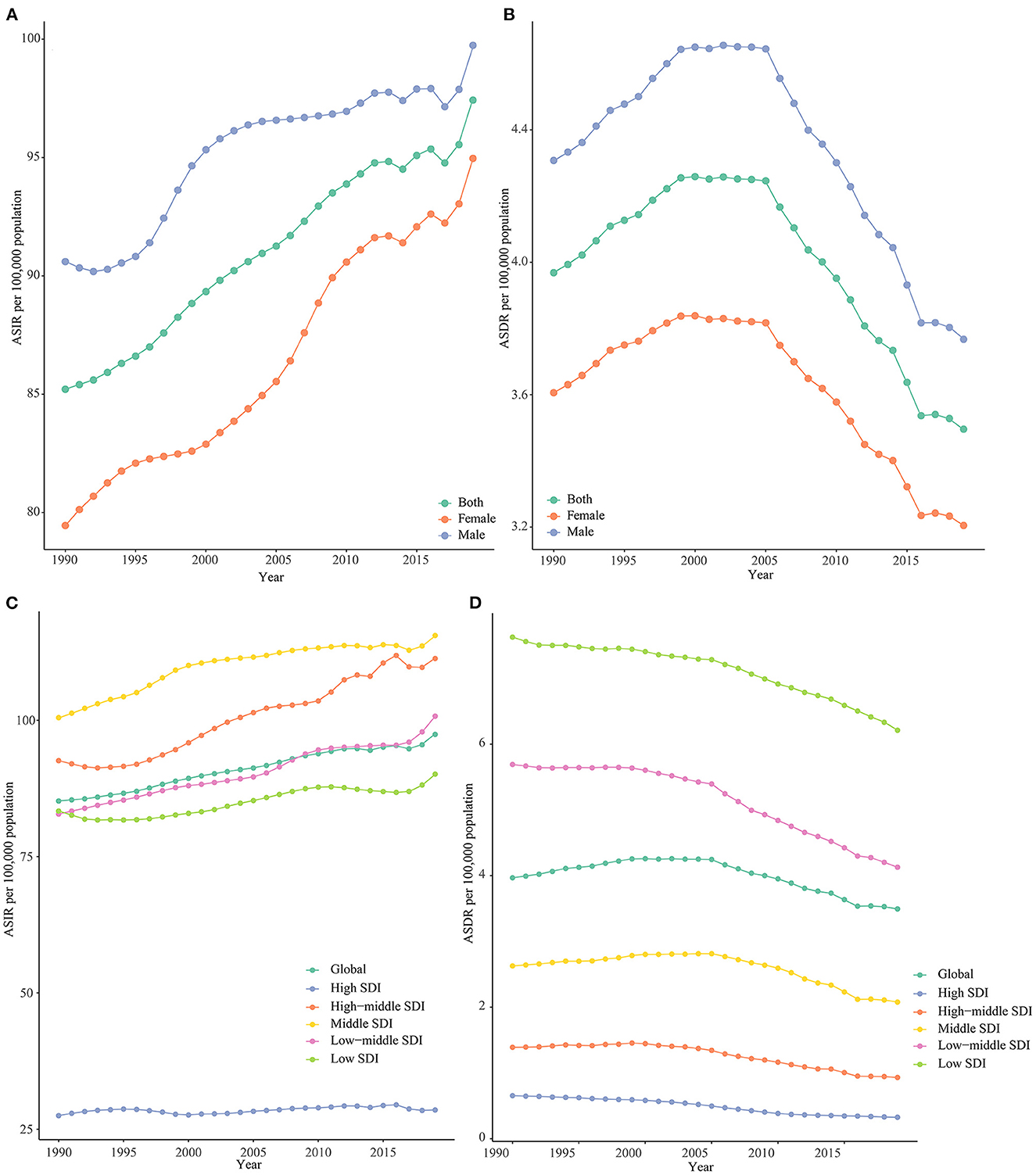
Figure 1. Trends of global ASIRs (A) and ASDRs (B) by gender and global ASIRs (C) and ASDRs (D) by SDIs from 1990 to 2019.
In high-SDI regions, the number of incident cases of NSNIs decreased by 9.17%, and the number of deaths of NSNIs decreased by 56.38% from 1990 to 2019 (Table 1). The ASIR of NSNIs during this period increased [EAPC = 0.14 (95% CI, 0.07 to 0.20)] from 27.50 per 100,000 in 1990 to 28.54 per 100,000 in 2019, and the ASDR declined [EAPC = −2.77 (95% CI, −2.98 to −2.55)] from 0.65 per 100,000 in 1990 to 0.33 per 100,000 in 2019 (Table 2). The ASIRs of other 4 SDI regions all maintained a rising trend at a high level except for high-SDI regions, and there were heterogeneous trends between ASIRs and SDIs, for example, the ASIR of middle-SDI regions was not lower than that of low-SDI regions (Table 2, Figure 1C, Supplementary Figure 1A). The ASDR in all 5 SDI regions showed a downward trend on the whole, and the higher the SDI, the smaller the ASDR (Table 2, Figure 1D, Supplementary Figure 1B).
Among the 21 GBD regions, the number of incident cases increased in 10 regions and decreased in 11 regions; the number of deaths increased in seven regions and decreased in 14 regions (Table 1). The regions where both incident cases and deaths were increasing were Southern Sub-Saharan Africa, Eastern Sub-Saharan Africa, Western Sub-Saharan Africa, Central Sub-Saharan Africa, and Oceania (Table 1). The largest increase in incident cases was in Central Sub-Saharan Africa (relative change = 80.75%), and in deaths in Oceania (relative change = 88.84%; Table 1). Besides, the number of incident cases (relative change = −42.38%) presented the most rapid decline in Central Europe, as did the number of deaths (relative change = −78.02%; Table 1). The region with the highest incidence of NSNIs was Andean Latin America (2019 ASIR: 174.90 per 100,000), and Central Latin America ranked second (2019 ASIR: 160.76 per 100,000) (Table 2). In terms of NSNIs mortality, the threat was most severe in Western Sub-Saharan Africa (2019 ASDR: 8.18 per 100,000), and Eastern Sub-Saharan Africa ranked second (2019 ASDR: 6.88 per 100,000; Table 2). The ASIRs decreased in 10 regions, most notably in Southern Latin America [EAPC = −1.71 (95% CI −1.85 to −1.57)]; the ASIRs of 9 regions had an increasing trend, with East Asia showing highest increasing trend [EAPC = 2.16 (95% CI 2.03 to 2.27); Table 2, Figure 2A]. The ASIRs of Western Europe and High-income Asia Pacific remained stable (Table 2, Figure 2A). The ASDR generally showed a downward trend, with only three regions showing an upward trend, including Central Asia, Southern Sub-Saharan Africa, and the Caribbean (Table 2, Figure 2B). The largest decrease in ASDR was noted in Central Europe (Table 2, Figure 2B).

Figure 2. Estimated annual percentage changes (EAPCs) of ASIRs and ASDRs in NSNIs at the regional levels. (A) EAPCs of ASIRs from 1990 to 2019; (B) EAPCs of ASDRs from 1990 to 2019; (C) EAPCs of ASIRs from 2010 to 2019; (D) EAPCs of ASDRs from 2010 to 2019.
In order to show the recent changes in the ASIRs and ASDRs of NSNIs, we obtained data from the past 10 years (2010–2019; Supplementary Table 1). In recent 10 years, the ASIRs in regions with high-middle and low-middle SDI were still on the rise, while those in regions with high SDI, middle SDI and low SDI tended to be stable and improved compared with the overall trend (the ASIRs of all SDI regions were on the rise from 1990 to 2019; Figures 2A, C). The short-term and long-term trends of ASDRs in the 5 SDI regions were the same, showing a downward trend (Figures 2B, D). In the 21 GBD regions, East and South Asia remained the top 2 in the rapid growth of ASIRs, while Central Europe and Southern Latin America maintained a continuous decline of ASIRs (Figure 2C). Central Latin America, Eastern Sub-Saharan Africa, Tropical Latin America and Caribbean performed well. While the overall ASIRs (1990–2019) showed an upward trend, effective measures were taken in the past 10 years to successfully curb the upward trend of ASIRs, showing a downward trend (Figures 2A, C). In Southern Sub-Saharan Africa, ASIR stopped growing and remained stable over the past decade (Figure 2C). The ASDRs declined in all 21 GBD regions from 2010 to 2019, indicating that infant death caused by NSNIs has attracted attention in some regions where ASDR was still growing (Figure 2D).
Among 204 countries and territories, China (1.11 million) and India (0.75 million) ranked the top 2 in the number of incident cases of NSNIs in 2019, accounting for about 29% of the number of global incident cases (6.31 million; Supplementary Table 2). The countries with the highest number of deaths were India (36,900) and Nigeria (27,200), accounting for 28% of the number of global deaths (226,500; Supplementary Table 2).
Northern Macedonia exhibited the largest increase in incident cases of NSNIs (300.45%), followed by Afghanistan (241.37%; Supplementary Table 3, Figure 3A). Mauritius had the largest ASIR (244.26 per 100,000), followed by Bangladesh (231.66 per 100,000), and Dominican Republic (230.71 per 100,000; Supplementary Table 2, Figure 3B). The ASIRs of 101 countries or territories showed an upward trend, of which North Macedonia had the largest increase [EAPC = 8.41 (95% CI, 7.72 to 9.10); Supplementary Table 4, Figure 3C]. The ASIRs of 93 countries or territories were considered to show a downward trend, with the largest decline in Serbia [EAPC = −4.76 (95% CI, −5.25 to −4.26)], followed by Poland [EAPC = −4.47 [95% CI, −5.36 to −3.58); Supplementary Table 4, Figure 3C]. The ASIRs of 25 countries or territories, including Denmark, Norway, and Greenland, remained stable (Supplementary Table 4).
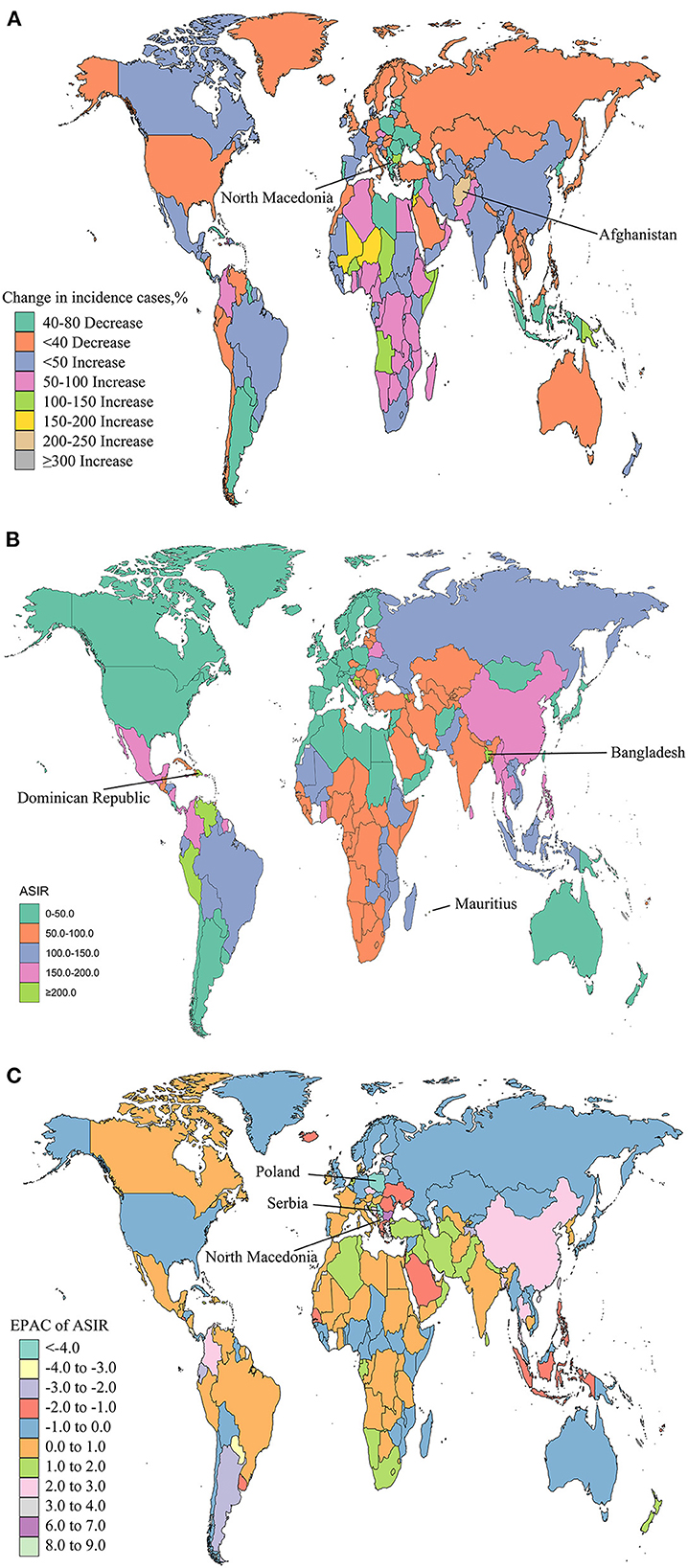
Figure 3. Global trends in the incidence of NSNIs in 204 countries and territories. The percentage of relative change in incident cases of NSNIs between 1990 and 2019 (A), age-standardized incidence rates (ASIRs) of NSNIs in 2019 (B), and estimated annual percentage changes (EAPCs) of ASIRs of NSNIs from 1990 to 2019 (C) were shown.
North Macedonia (227.49%) had the largest increase in deaths of NSNIs, followed by Bulgaria (216.90%), and Afghanistan (196.38%; Supplementary Table 3, Figure 4A). In 2019, Mali (ASDR: 14.11 per 100,000) and Ghana (ASDR: 10.14 per 100,000) showed the highest ASDR (Supplementary Table 2, Figure 4B). The ASDRs were on the rise among the 38 countries or territories, with the largest increase in North Macedonia [EAPC = 9.31 (95% CI, 7.81 to −10.83); Supplementary Table 4, Figure 4C]. The ASDRs of 153 countries or territories declined, with the greatest reduction in Serbia [EAPC = −8.66 (95%CI, −9.83 to −7.47)], followed by Greece [EAPC = −7.41 (95% CI, −9.32 to −5.46); Supplementary Table 4, Figure 4C]. The ASDR remained stable in 13 countries or territories, including Yemen, Somalia, and Belize (Supplementary Table 4).
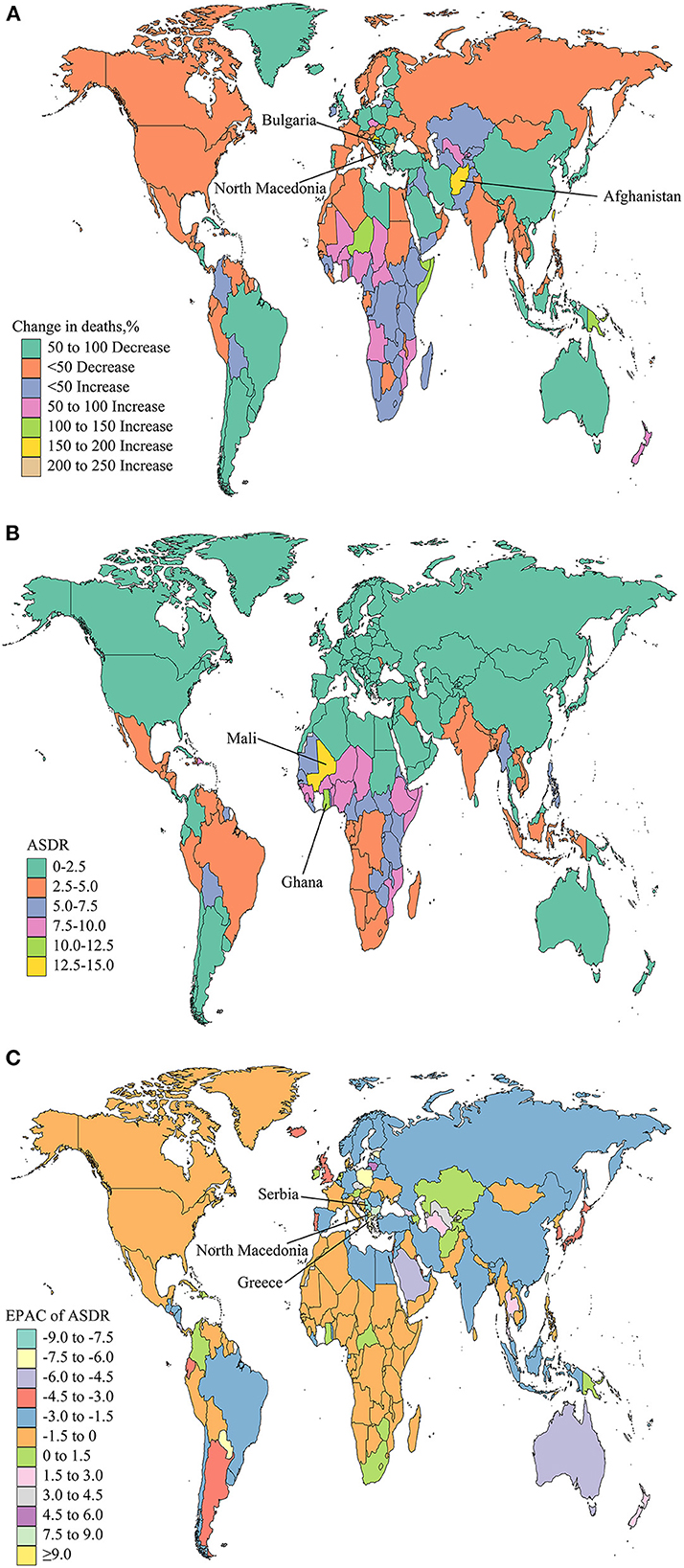
Figure 4. Global trends in the deaths of NSNIs in 204 countries and territories. The percentage of relative change in deaths of NSNIs between 1990 and 2019 (A), age-standardized deaths rates (ASDRs) of NSNIs in 2019 (B), and estimated annual percentage changes (EAPCs) of ASDRs of NSNIs from 1990 to 2019 (C) were shown.
To show the effect of recent interventions, we analyzed the changes of ASIRs and ASDRs in 204 countries and territories from 2010 to 2019. The ASIRs of 74 countries or territories showed an upward trend, with the largest increase in Singapore [EAPC = 4.08 (95% CI, 3.92 to 4.24); Supplementary Table 4, Supplementary Figure 2A]. The ASIRs of 92 countries or territories were in a downward trend, with the largest decline in Estonia [EAPC = −6.21 (95% CI, −7.09 to −5.33)], followed by Serbia [EAPC = −5.22 (95% CI, −6.14 to −4.29)] and Poland [EAPC = −5.03 (95% CI, −6.32 to −3.73); Supplementary Table 4, Supplementary Figure 2A]. The ASIRs of 38 countries or territories remained stable, such as Canada and Finland (Supplementary Table 4). The ASDRs of eight countries or territories had a downward trend, and Mauritius had the largest increase [EAPC = 2.98 (95% CI, 1.23 to 4.77)], followed by Austria, Greenland and Singapore (Supplementary Table 4, Supplementary Figure 2B). The ASDRs of 177 countries or territories decreased, of which Estonia experienced the largest decline [EAPC = −7.70 (95% CI, −11.61 to −3.62)], followed by Cyrus [EAPC = −7.22 (95% CI, −8.75 to −5.67); Supplementary Table 4, Supplementary Figure 2B]. The ASDRs remained stable in 19 countries or territories, such as Sweden, France and Greece (Supplementary Table 4). Compared with the data of the past 30 years, the ASIRs and ASDRs of NSNIs in some countries and territories were under control from 2010 to 2019.
The EAPCs of ASIRs and ASDRs of NSNIs in 2019 were not correlated with SDI (p > 0.05; Figures 5A, B). The EAPCs of ASIRs of NSNIs in 2019 were not correlated with UHCI (P > 0.05; Figure 5C), while the EAPCs of ASDRs of NSNIs in 2019 was significantly negatively correlated with UHCI (cor = −0.18; P = 0.009; Figure 5D).
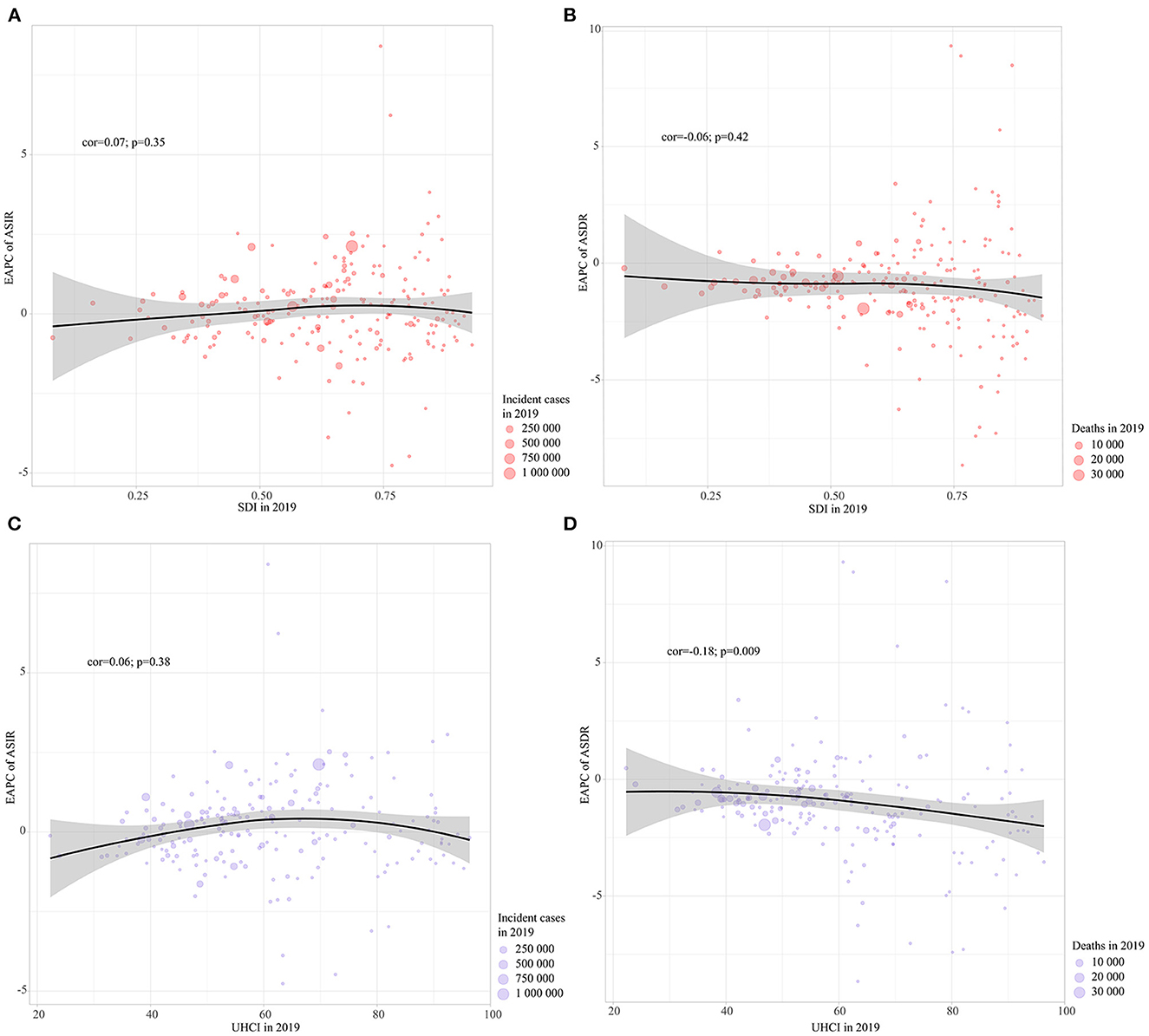
Figure 5. Pearson correlation was analyzed between EAPCs of ASIRs and ASDRs in NSNIs from 1990 to 2019 and SDI and UHCI in 2019 at the country and territorial levels. (A) SDI in 2019 and EAPC of ASIR; (B) SDI in 2019 and EAPC of ASDR; (C) UHCI in 2019 and EAPC of ASIR; (D) UHCI in 2019 and EAPC of ASDR. The incident cases and deaths of NSNIs from 204 countries and territories in 2019 are represented by circles. The size of the circles increased with the incident cases or deaths of NSNIs. Correlation coefficient, cor.
To the best of our knowledge, we for the first time comprehensively assessed global and regional long-term and short-term characteristics in incidence and mortality of NSNIs. In this study, we found that the number of incident cases of NSNIs in the world grew by 12.79% per year, and the number of deaths dropped by 12.93% per year from 1990 to 2019. During this period, global ASIR of NSNIs increased by 46% annually on average, while ASDR decreased by 53% annually on average. The ASIR and ASDR of female NSNIs were consistently lower than that of male NSNIs. The EAPC of female ASIR was 0.61, nearly twice that of male ASIR, and female ASIR was growing rapidly. The same declining trends of ASDR were noted in males and females. For SDI regions, the ASIR of NSNIs in high-SDI regions grew by an average of 14% annually from 1990 to 2019. Except for high-SDI regions, the ASIRs in other 4 SDI regions maintained a rising trend at a high level. The ASDRs of all 5 SDI regions generally showed a downward trend. The largest decline was in the high-SDI regions. The highest ASIR of NSNIs was in Andean Latin America (ASIR in 2019: 174.90 per 100,000), and the highest mortality of NSNIs was in Western Sub-Saharan Africa (ASDR in 2019: 8.18 per 100,000). From 2010 to 2019, the burden of NSNIs in several regions where the ASIRs or ASDRs were rising were under control. We found a negative correlation between EAPCs of ASDRs and UHCI in 2019.
NSNIs are one of the major causes of 2.6 million newborn deaths worldwide every year (21). It is necessary and significant to improve the current situation of NSNIs. We need to better understand the characteristics of NSNIs, and actively enhance newborn care. In this study, we found that the global incidence of NSNIs showed rapid growth, and the mortality was generally declining. The incidence and mortality of males and females were in line with global trends. The incidence and mortality of NSNIs in females were lower than in males. The continuous increase in global incidence of NSNIs may indicate that the global health environment still needs to be improved. However, the decline of global mortality of NSNIs in the short term showed that the current maternal and newborn health care has achieved positive results (22).
We found that in high SDI regions, the ASIR showed the lowest increase, while the ASDR exhibited the highest decline. In other 4 SDI regions, we found no relationship between ASIR and SDI levels. For example, the ASIR in the middle-SDI regions was higher than that in the low-SDI regions. The ASDRs of all 5 SDI regions were generally decreasing, and the higher the SDI, the smaller the ASDR. This finding indicated that NSNIs had a high ASIRs and was growing rapidly, and the mortality of NSNIs was related to the educational level and economic level of the SDI regions. Although the ASIRs of Western Sub-Saharan Africa and Eastern Sub-Saharan Africa were not the highest (the highest was Andean Latin America and Central Latin America), the ASDRs were the highest. Consistent with our findings, Sub-Saharan Africa topped the list for the mortality of NSNIs (23). One possible reason was the high antimicrobial resistance of pathogens in Sub-Saharan Africa, and the efficacy of treatment was reduced (24). Ranjeva et al. evaluated the public health burden and economic pressure caused by neonatal sepsis in Sub-Saharan Africa, and believed that it was necessary to provide reasonable and appropriate health care for neonatal infections (25).
The high incidence and its high growth rate of NSNIs may indicate that infants are generally susceptible to pathogens and their infection capacity is increasing. The death of NSNIs may be related to the lack of timely diagnosis and treatment, and antibiotic resistance (26, 27). Our findings illustrated that the mortality of NSNIs was relatively high in low- and middle-income countries. Families and health workers in low- and middle-income countries lack relevant knowledge and training to identify the early stage of infections, and the corresponding laboratory equipment is only available in hospitals, delaying the time of treatment (27, 28). In addition, many people in low- and middle-income countries may not go to hospitals due to financial hardship, or may not have access to medical care. It was estimated that there were 8 million curable deaths in 2015, of which 96% occurred in low- and middle-income countries (29). A study estimated the quality of care in 81 low- and middle-income countries, and when high-quality care was provided, it was believed that neonatal mortality would be reduced by 28% (30). UHCI is an indicator reflecting health coverage and nursing quality (16). Efforts to improve UHC can overcome these issues and promote health equity. From our results, it was observed that the UHCI was negatively correlated with the trend of ASDRs, that is, when the level of UHCI was high, the ASDR was generally in a downward trend. This was consistent with previous report (31). There is no doubt that the use of antibiotics is crucial to the treatment of infections. It is known that there is a clear correlation between antibiotic use and antibiotic resistance, and antibiotic resistance has become a persistent global health threat (32, 33). On the one hand, there is the misuse of antibiotics and population-level resistance in low- and middle-income countries (34). On the other hand, low- and middle-income countries showed high resistance to antibiotics recommended by World Health Organization (WHO) (35). These are not conducive to neonatal outcomes. Therefore, we need to improve the overall awareness, timely diagnosis and management of NSNIs.
Finally, special attention should be paid to countries or territories where ASDR is still growing, including Mauritius, Austria, and Greenland (Supplementary Table 4). In these countries and territories with ASDR on the rise, it was imperative to accelerate the promotion of universal health coverage and strengthen antibiotic management.
This study fills a gap in this area by providing the first comprehensive assessment of global and regional long-term and short-term characteristics of incidence and mortality of NSNIs, and the relationship with socioeconomic status and medical health level. However, we should recognize several limitations. First of all, the quality of the data limited our accurate description of the results. The possible bias made the results less robust. Second, the causes of NSNIs were notoriously complex. There was no specific pathogen infection data in the GBD study, so we could not estimate the contribution of different causes.
To sum up, the ASIR of global NSNIs gradually increased and the ASDR gradually declined from 1990 to 2019. In addition, the ASIR and ASDR of males were higher than those of females. Except for high-SDI regions, the ASIRs of other 4 SDI regions remained at a high level in this period. The ASDRs declined in all SDI regions. The ASDRs in Western Sub-Saharan Africa and Eastern Sub-Saharan Africa were the highest. The ASDRs were still growing in some countries and territories. Therefore, it is essential to improve the overall awareness and management of NSNIs, and reduce the morbidity and mortality of NSNIs worldwide.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
KQ: project design. JL: data curation, analysis, and manuscript writing. LS: manuscript revision. All authors read and approved the final manuscript.
This study was funded by including the National Key R&D Program of China (Grant No. 2018YFA0108401).
We thank Shaozhe Cai, Jiawei Liu, and Ruimin Chi for their help in this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1139832/full#supplementary-material
1. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. (2017) 390:1770–80. doi: 10.1016/S0140-6736(17)31002-4
3. Levy O. Innate immunity of the newborn: Basic mechanisms and clinical correlates. Nat Rev Immunol. (2007) 7:379–90. doi: 10.1038/nri2075
4. Borghesi A, Stronati M, Castagnoli R, Ioimo I, Achille C, Manzoni P, et al. Novel approaches to the study of neonatal infections. Am J Perinatol. (2018) 35:570–4. doi: 10.1055/s-0038-1639360
5. Berardi A, Rossi C, Lugli L, Creti R, Reggiani MLB, Lanari M, et al. Group B streptococcus late-onset disease: 2003-2010. Pediatrics. (2013) 131:e361–8. doi: 10.1542/peds.2012-1231
6. Berardi A, Rossi C, Creti R, China M, Gherardi G, Venturelli C, et al. Group B streptococcal colonization in 160 mother-baby pairs: A prospective cohort study. J Pediatr. (2013) 163:1099–04.e1. doi: 10.1016/j.jpeds.2013.05.064
7. Pylipow M, Gaddis M, Kinney JS. Selective intrapartum prophylaxis for group B streptococcus colonization: Management and outcome of newborns. Pediatrics. (1994) 93:631–5. doi: 10.1542/peds.93.4.631
8. Lawn JE, Blencowe H, Oza S, You D, Lee ACC, Waiswa P, et al. Every Newborn: Progress, priorities, and potential beyond survival. Lancet. (2014) 384:189–205. doi: 10.1016/S0140-6736(14)60496-7
9. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
10. Chaurasia S, Sivanandan S, Agarwal R, Ellis S, Sharland M, Sankar MJ. Neonatal sepsis in South Asia: Huge burden and spiralling antimicrobial resistance. Br Med J. (2019) 364:k5314. doi: 10.1136/bmj.k5314
11. Vergnano S, Menson E, Kennea N, Embleton N, Russell AB, Watts T, et al. Neonatal infections in England: The NeonIN surveillance network. Archiv Dis Childh. (2011) 96:178798. doi: 10.1136/adc.2009.178798
12. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
13. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
14. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
15. GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1684–735. doi: 10.1016/S0140-6736(18)31891-9
16. GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1250–84. doi: 10.1016/S0140-6736(20)30750-9
17. Cao G, Liu J, Liu M. Global, regional, and national incidence and mortality of neonatal preterm birth, 1990-2019. J Am Med Assoc Pediatr. (2022) 176:787–96. doi: 10.1001/jamapediatrics.2022.1622
18. Gao S, Yang W-S, Bray F, Va P, Zhang W, Gao J, et al. Declining rates of hepatocellular carcinoma in urban Shanghai: Incidence trends in 1976-2005. Eur J Epidemiol. (2012) 27:39–46. doi: 10.1007/s10654-011-9636-8
19. Dhillon PK, Yeole BB, Dikshit R, Kurkure AP, Bray F. Trends in breast, ovarian and cervical cancer incidence in Mumbai, India over a 30-year period, 1976-2005: An age-period-cohort analysis. Br J Cancer. (2011) 105:723–30. doi: 10.1038/bjc.2011.301
20. Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. (2019) 70:674–83. doi: 10.1016/j.jhep.2018.12.001
21. Khan AM, Morris SK, Bhutta ZA. Neonatal and perinatal infections. Pediatr Clin North Am. (2017) 64:785–98. doi: 10.1016/j.pcl.2017.03.008
22. Countdown to 2030 Collaboration. Countdown to 2030: Tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet. (2018) 391:1538–48. doi: 10.1016/S0140-6736(18)30104-1
23. Lawn JE, Cousens S, Zupan J. Four million neonatal deaths: When? where? why? Lancet. (2005) 365:891–900. doi: 10.1016/S0140-6736(05)71048-5
24. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. (2022) 399:629–55. doi: 10.1016/S0140-6736(21)02724-0
25. Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. Br Med J Glob Health. (2018) 3:e000347. doi: 10.1136/bmjgh-2017-000347
26. Akova M. Epidemiology of antimicrobial resistance in bloodstream infections. Virulence. (2016) 7:252–66. doi: 10.1080/21505594.2016.1159366
27. Huynh B-T, Padget M, Garin B, Delarocque-Astagneau E, Guillemot D. Bacterial neonatal sepsis and antibiotic resistance in low-income countries. Lancet. (2016) 387:533–4. doi: 10.1016/S0140-6736(16)00220-8
28. Doherty T, Tran N, Sanders D, Dalglish SL, Hipgrave D, Rasanathan K, et al. Role of district health management teams in child health strategies. Br Med J. (2018) 362:k2823. doi: 10.1136/bmj.k2823
29. Alkire BC, Peters AW, Shrime MG, Meara JG. The economic consequences of mortality amenable to high-quality health care in low- and middle-income countries. Health Affairs. (2018) 37:988–96. doi: 10.1377/hlthaff.2017.1233
30. Chou VB, Walker N, Kanyangarara M. Estimating the global impact of poor quality of care on maternal and neonatal outcomes in 81 low- and middle-income countries: A modeling study. PLoS Med. (2019) 16:e1002990. doi: 10.1371/journal.pmed.1002990
31. Verrecchia R, Thompson R, Yates R. Universal Health Coverage and public health: A truly sustainable approach. Lancet Public Health. (2019) 4:e10–1. doi: 10.1016/S2468-2667(18)30264-0
32. Frieri M, Kumar K, Boutin A. Antibiotic resistance. J Infect Public Health. (2017) 10:369–78. doi: 10.1016/j.jiph.2016.08.007
33. Gyssens IC. Antibiotic policy. Int J Antimicrob Agents. (2011) 38(Suppl.):11–20. doi: 10.1016/j.ijantimicag.2011.09.002
34. Mendelson M, Røttingen J-A, Gopinathan U, Hamer DH, Wertheim H, Basnyat B, et al. Maximising access to achieve appropriate human antimicrobial use in low-income and middle-income countries. Lancet. (2016) 387:188–98. doi: 10.1016/S0140-6736(15)00547-4
35. Thomson KM, Dyer C, Liu F, Sands K, Portal E, Carvalho MJ, et al. Effects of antibiotic resistance, drug target attainment, bacterial pathogenicity and virulence, and antibiotic access and affordability on outcomes in neonatal sepsis: An international microbiology and drug evaluation prospective substudy (BARNARDS). Lancet Infect Dis. (2021) 21:1677–88. doi: 10.1016/S1473-3099(21)00050-5
Keywords: neonatal sepsis and other neonatal infections, global burden disease, incidence, mortality, global trend
Citation: Li J, Shen L and Qian K (2023) Global, regional, and national incidence and mortality of neonatal sepsis and other neonatal infections, 1990–2019. Front. Public Health 11:1139832. doi: 10.3389/fpubh.2023.1139832
Received: 07 January 2023; Accepted: 22 February 2023;
Published: 14 March 2023.
Edited by:
Rozeta Sokou, Nikaia General Hospital “Aghios Panteleimon”, GreeceReviewed by:
Evangelia-Filothei Tavoulari, General Hospital Nice Piraeus Saint Panteleimon, GreeceCopyright © 2023 Li, Shen and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kun Qian, a3VucWlhbkB0amgudGptdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.