- 1Department of Psychiatry, The First Hospital of Hebei Medical University, Shijiazhuang, China
- 2Mental Health Center, Hebei Medical University, Shijiazhuang, China
- 3Clinical Medical Research Center for Psychiatric and Psychological Disorders of Hebei Province, Shijiazhuang, China
- 4Saudi Arabia Neuroscience Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Objective: To examine the role of night shift work on the risk of metabolic syndrome (MetS) in adults suffered from earthquakes prenatally or as infants and to analyse the effect of stress on factors that influence MetS in this population.
Methods: We included 870 subjects from 2014 to 2015. All subjects work as miners for the Kailuan Mining Group and were born were living in Tangshan. Participants were classified into two groups on basis of their work schedules: day shift and night shift. They were further classified into the prenatal exposure group, the infancy exposure group, and the control group based on their age during the Tangshan earthquake. This study was conducted 38 years after the earthquake. Participants’ general demographic data, smoking and drinking habits, as well as work schedules were collected. All participants’ sleep status was assessed with the Pittsburgh Sleep Quality Index. The measurement of all subjects’ waist circumference and blood pressure was made, and triglycerides, fasting blood glucose, high-density lipoproteins, and low-density lipoproteins were measured by collecting blood samples. The definition of MetS was made after the guidelines for preventing and controlling type 2 diabetes in China (2017 Edition).
Results: A total of 187 (21.5%) workers were determined to have MetS. The incidence of MetS was greatly higher in night shift workers who were exposed to an earthquake during infancy than in day shift workers (χ2 = 8.053, p = 0.005). A multivariate logistic regression analysis displayed male participants had a higher risk develop MetS than female participants (p = 0.042, OR = 0.368, 95% CI = 0.140, 0.965). Current smokers (p = 0.030, OR = 1.520, 95%CI = 1.042, 2.218) and participants who sleep fewer than 7 h per night (p = 0.015, OR = 1.638, 95%CI = 1.101, 2.437) had a higher risk of MetS. Prenatal earthquake stress was also a risk element for MetS (p = 0.012, OR = 1.644, 95%CI = 1.115, 2.423).
Conclusion: The risk of MetS is significantly higher in night shift workers exposed to earthquake stress during infancy than day shift workers. Earthquake exposure during pregnancy is an independent risk factor for MetS. Smoking and sleeping less than 7 h have a higher risk of MetS than the control group.
1. Introduction
Metabolic syndrome (MetS) is defined as a pathologic condition with the characteristics such as abdominal obesity, insulin resistance, hypertension, and hyperlipidaemia by the WHO. These factors are correlated with a higher risk of type 2 diabetes, cardiovascular disease, and mortality. MetS is estimated to affect about 25% of the global population (1). More importantly, MetS -related disorders account for two-thirds of deaths caused globally by non-communicable diseases (NCDs) (2). In these years, it has been estimated that the prevalence of MetS among adults in the US is at around 34.7% (3). The prevalence of MetS among younger individuals (aged 20–39 years) has recently increased significantly (from 16.2 to 21.3%)—especially among older individuals between 2011 and 2016 (3). More than 4/5 of adults had at least one abnormal MetS component in China (4). Individuals who are younger when they first develop MetS show a higher risk of also developing cardiovascular disease (5).
Both genetic and environmental elements such as the in the utero environment, exert significant effects on the growth of MetS. Several studies have found that the risk of MetS increases following stress in early life (6, 7). The Dutch Famine Birth Cohort Study found that the children born to women who suffered famine during pregnancy are more likely to have several symptoms of MetS including insulin resistance, dyslipidaemia, obesity, and hypertension (8). Men exposed to two or more psychosocial traumatic events and women exposed to one psychosocial traumatic event have a higher risk of MetS than individuals who are not exposed to trauma (9). Doom and colleagues (10) found that a worse psychosocial environment during infancy is associated with higher blood pressure, a higher risk of biomarkers related to MetS (greater triglycerides and cholesterol), and a higher risk of MetS in adolescence.
The assumption that factors during early life (preadult), such as exposure to famine, may exert an effect on the pathophysiology of metabolic diseases in adulthood has attracted basic study interest especially in the last two decades (11, 12). Our previous research on earthquake stress found that earthquake stress is an independent risk factor with long-term impacts on diabetes incidence (13). Our previous research also showed that earthquake exposure during infancy is a great independent risk element for hypertension (14). Previous studies on earthquakes and health have been short-term follow-up studies, and no studies have investigated early life earthquake exposure to MetS in adulthood (15, 16). This study base on our previous research to investigated the effect of earthquake stress in MetS in adulthood after 38 years of maternal and fetal exposure to earthquake stress.
Lifestyle factors such as sleep disturbance, daily calorie intake, alcohol consumption, and smoking are related to the risk of MetS (4, 17). Humans spend approximately one-third of our lives sleeping. Sleep plays a crucial role in the body’s energy metabolism. Previous studies have shown that sleep disorders are closely related to metabolic disorders (17). Sleep deprivation has been linked to an increased risk of cardiovascular disease,such as hypertension, obesity, coronary artery disease, and stroke—these are all associated with morbidity and mortality (18). In addition, night shift work is correlated with a higher risk of MetS and high waist circumference versus daytime work (19). Men who work a permanent night shift show a higher risk of MetS than those with permanent day work, and this association could be mediated by visceral obesity (20). Therefore, this study explores whether night shift work or abnormal sleep duration in adulthood increases the risk of MetS in individuals born before or after the Tangshan earthquake.
2. Subjects and methods
2.1. Subjects
This research recruited miners from Tangshan, China who work for the Kailuan Mining Group. The workers change shifts at 8:00 AM and midnight; hence, participants were classified into the day shift (from 8:00 AM to 24:00) and the night shift (from 24:00 to 8:00 AM the next day).
Participants were classified into three earthquake exposure groups. The infancy exposure group includes participants born between July 29, 1975 and April 28, 1976; they were aged three to 12 months when the Tangshan earthquake happened. The prenatal exposure group includes participants born between July 29, 1976 and April 28, 1977; these subjects experienced the earthquake prenatally. The control/no exposure group includes participants who were born between July 29, 1977 and April 28, 1978 or one to 1.9 years after the earthquake. All participants had lived in Tangshan since birth and agreed to participate in the study. Individuals whose mothers had infections, hypertension, epilepsy or seizures, diabetes, thyroid disease, or coronary heart disease during pregnancy were excluded. Individuals whose mothers experienced other traumatic events apart from the earthquake during pregnancy were excluded.
2.2. Subject evaluation
Participants received a standardized interview including demographics; smoking and drinking history; history of arterial hypertension, diabetes mellitus, and hyperlipidaemia; and the participants’ mothers’ conditions during pregnancy. Specially trained physicians made the interview and all examinations. Participants were classified into three groups according to smoking status: never smoked, ex-smoker, and current smoker. They were also divided into three groups according to drinking status: never drinks, ex-drinker, and current drinker. The Childhood Trauma Questionnaire (CTQ) and the Life Event Scale (LES) were adopted to assess traumatic events. Childhood trauma was defined as a CTQ score of 26 points or higher. An LES score of 32 or higher indicated a traumatic event in adulthood.
2.3. Physical measurements
The blood pressure of the right brachial artery was measured using a corrected mercury sphygmomanometer. Smoking, tea, and coffee were forbidden before this measurement, and workers sat quietly for 15 min before measure blood pressure. Three measurements were made consecutively at 1–2 min intervals, and the results were averaged. The evaluation of waist was as the body circumference midway between the lowest rib and the iliac crest as measured parallel to the floor with an inelastic tape 1measure without compressing the body tissue were made. The recording of measurements was made in centimetres with a sensitivity of 0.1 cm. The measurement of hip circumference was made similarly at the widest part of the hip.
2.4. Biochemical measurements
Blood was drawn between 7:00 AM and 9:00 AM on the same day as the physical examination. Blood was taken from the cubital vein of fasting subjects and placed in EDTA vacuum tubes. The 10-min centrifugal of samples was made at 3000 g at room temperature, and the collection of supernatants was performed. Fasting plasma glucose (FPG), triglycerides, low-density lipoprotein cholesterol (LDL-C), total cholesterol, and high-density lipoprotein cholesterol (HDL-C) were then measured. An oxidase approach was adopted to measure total cholesterol and triglycerides.
The definition of MetS was according to the guidelines for preventing and controlling type 2 diabetes in China (2017 Edition) (21). People with three or more of the following were diagnosed with MetS: (1) Abdominal obesity:the presence of central obesity (waist circumference ≥ 90 cm for men or ≥ 85 cm for women). (2) Hyperglycemia: fasting blood glucose ≥6.1 mmol/L or blood glucose ≥7.8 mmol/L 2 h after glucose load and/or diagnosed treated with diabetes. (3) Hypertension: SBP ≥130 mmHg or DBP ≥ 85 mmHg or treated with medication for hypertension. (4) Fasting triglyceride (TG) ≥ 1.70 mmol/L. (5) Fasting high-density lipoprotein cholesterol (HDL-C) < 1.04 mmol/L.
2.5. Sleep evaluation
The quality and duration of participants’ sleep were measured with the Pittsburgh Sleep Quality Index (PSQI). The PSQI consists of 7 subscales: the score ranges from 0 to 3 for each. Thus, the total points can vary from 0 to 21; a higher point represents poorer sleep quality. In this study, a PQSI score over seven is considered to indicate a sleep disorder.
2.6. Statistical analyses
SPSS 23.0 was adopted for all statistical analyses. The expression of measurement data was made using the mean and standard deviation (SD). Continuous variables for the three groups were compared with One-Way-ANOVA. Categorical variables for the three groups were compared with Chi-squared tests. Multivariate logistic regressions were used to identify factors that influence MetS. A two-sided value of p greater than 0.05 was of statistical significance.
3. Results
3.1. Demographic and baseline characteristics of three groups
Employees of the Kailuan Mining Group were scanned; 928 individuals satisfied the inclusion standards and agreed to take part in the research, and 58 additional individuals were excluded after the participants completed the questionnaire and the PSQI. Ten individuals were excluded because of missing data on sleep and earthquake exposure; 17 were excluded due to prenatal exposure to other stress; and 31 withdrew from the study because they chose not to undergo blood sample collection. There were 870 participants included in the analyses.
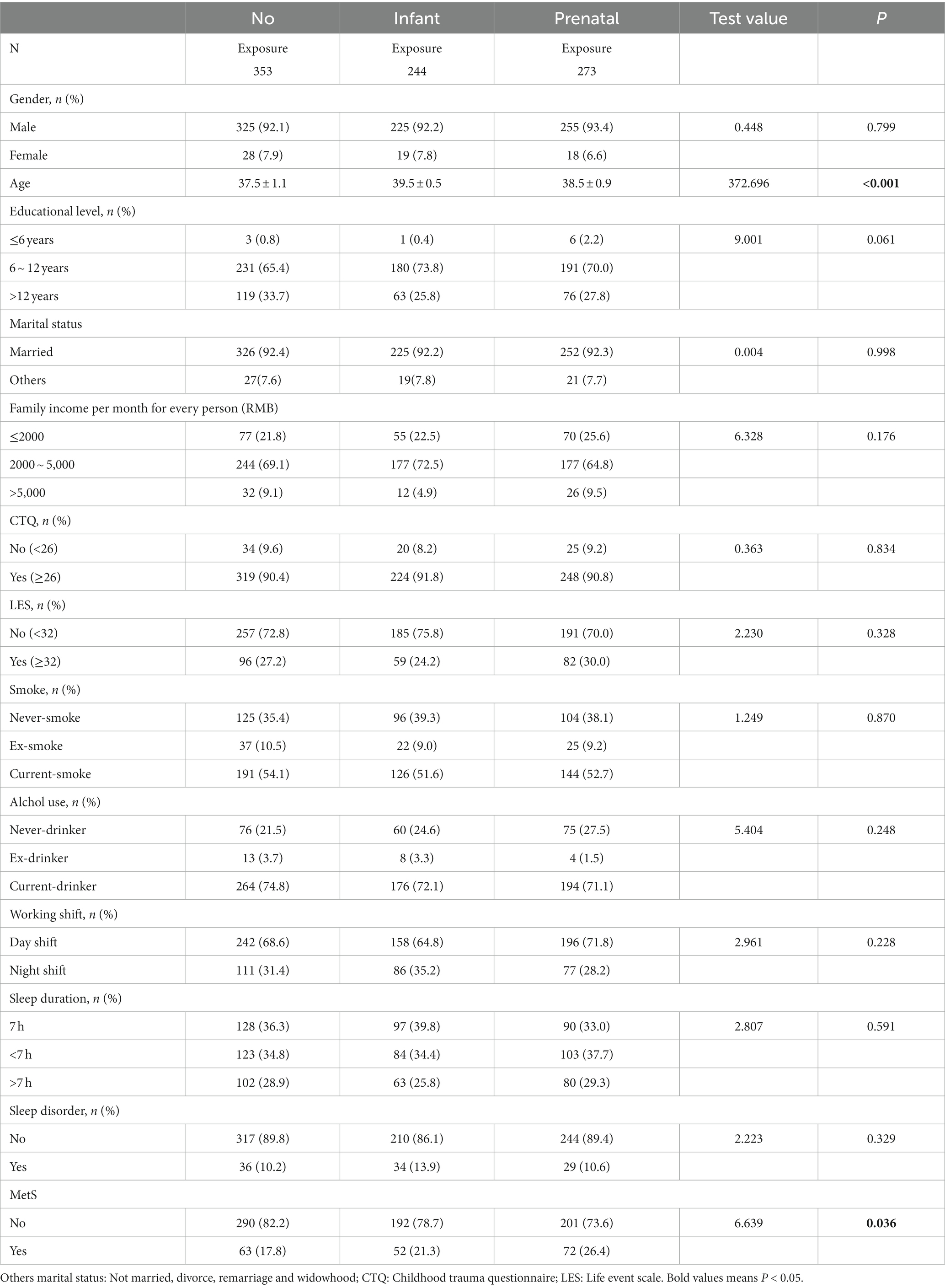
Of the 870 participants, 273 workers who experienced the earthquake as fetuses, 244 workers who experienced the earthquake as infants and 353 workers who did not experience the earthquake (Table 1). 187 (21.5%) met the diagnostic criteria for MetS. MetS was greatly more common in infancy exposure group (21.3%) and prenatal exposure group (26.4%; Table 1) than no exposure group (17.8%,χ2 = 6.639, p = 0.036). There was a statistical difference in age among the three groups (F = 372.696,P<0.001; Table 1).
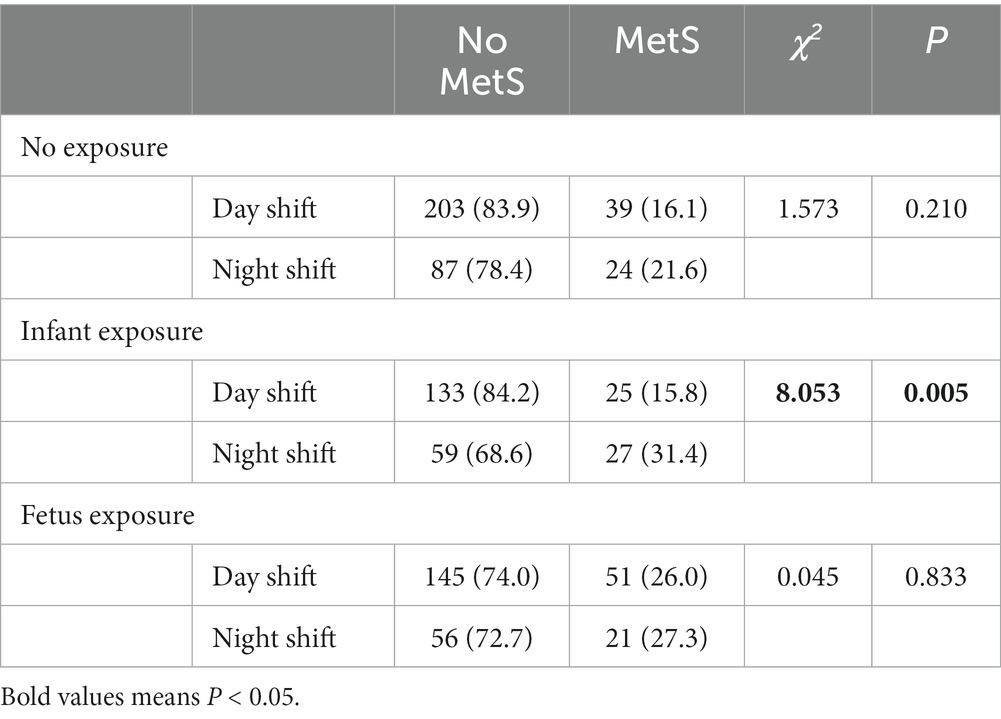
3.2. Mets incidence in earthquake exposure groups and in day vs. night shift workers in all three exposure groups
All subjects were grouped by earthquake exposure, and the groups were compared. Among workers in the infant-exposure group, night shift workers had a higher risk of MetS than day shift workers (31.4% vs. 15.8%, p = 0.005; Table 2). In the unexposed group (21.6% vs. 16.1%, p = 0.210) and the prenatal exposure group (27.3% vs. 26.0%, p = 0.833 Table 2), night shift workers had slightly higher rates of MetS than day shift workers.
3.3. Multivariate logistic regression analysis of MetS risk factors
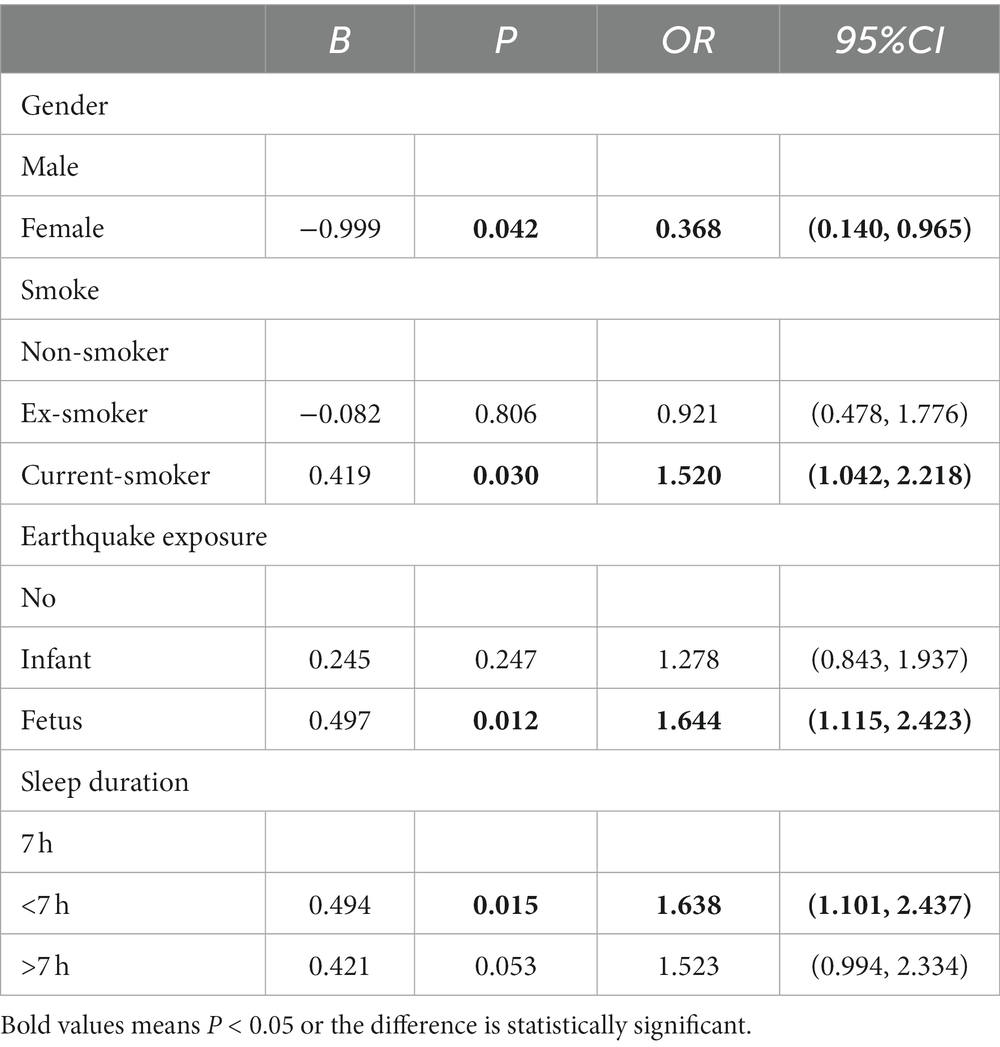
Participant groups were compared using a multivariate logistic regression analysis with or without MetS as the dependent variable. Factors that including gender, smoking and alcohol status, sleep duration, sleep disorder,working shift and earthquake exposure were used as independent variables.
The multivariate analysis showed that male participants had a higher risk develop MetS than female participants (p = 0.042, OR = 0.368, 95% CI = 0.140, 0.965; Table 3). Current smokers showed a higher risk (p = 0.030, OR = 1.520, 95%CI = 1.042, 2.218; Table 2) of MetS. Participants who sleep fewer than 7 hours (p = 0.015, OR = 1.638, 95%CI = 1.101, 2.437; Table 3) also showed a higher risk of MetS. Prenatal earthquake exposure was also correlated with an increased risk of MetS (p = 0.012, OR = 1.644, 95%CI = 1.115, 2.423; Table 3).
4. Discussion
On July 28, 1976, a 7.8-magnitude earthquake struck Tangshan, China, instantly destroyed the entire city. The loss of traffic infrastructure, telecommunications, power, and water supply led to 242,000 deaths as well as serious injury to 164,000 residents. Fetuses and infants exposed to earthquakes are affected not only by the direct stress of the earthquake, but also by water and power outages, food shortages, and changes in living conditions after the earthquake. We found here that miners who were exposed to earthquake stress prenatally had a significantly higher risk of MetS. This may be related to the lack and imbalance of maternal nutrition after the earthquake. Animal research has shed light on the fundamental underlying mechanisms that the imbalance of specific amino acids and other nutrients could be the decisive factor in programming of MetS-related phenotypes (22). Additionally, deficiencies of micronutrients in pregnant mother rats, such as calcium, zinc and vitamin D, are linked to offspring MetS (22). Furthermore, prenatal stress may lead to abnormal methylation levels of genes associated with important pathways of embryogenesis in the placenta, possibly affecting fetal development, as well as the peripheral tissues of the mother and baby (23). Both animal and human studies have confirmed that epigenetic mechanisms are important modulators of the susceptibility of offspring exposed to stressors during pregnancy to chronic diseases, especially metabolic diseases (24, 25). The result of this study conforms to the findings of the Dutch Famine Birth Cohort Study, which observed that kids of pregnant women exposed to famine presented with various characteristics of MetS including obesity, dyslipidaemia, hypertension, and insulin resistance (8). However, previous studies on this topic have only examined one or a few characteristics of MetS. Here, we focus on subjects who clearly meet the MetS diagnosis criteria.
More importantly, our findings suggest that workers exposed to earthquake stress during infancy have a greatly higher risk of MetS, and this risk increases further for those who work night shifts. Wang and colleagues observed that exposure to the Great Chinese famine during infancy was correlated with an increased risk of MetS in adults in their 50s (12). Importantly, our subjects are younger (38 to mid-40s) than those examined by Wang and colleagues. Bayon and colleagues found that men working on permanent night shifts show a higher risk of MetS than those with permanent day work (20). Another inconsistent found that night shift work, and sleep duration per night and day had no association with the higher odds of having MetS (26). It is important to note that previous studies have focused on only one factor (early life adversity or adult sleep conditions) that may influence the risk of developing MetS. Specifically, our findings confirm that individuals exposed in infancy are more susceptible to MetS - especially if they experience sleep rhythm disturbances in adulthood.
The mechanism linking early-life exposure to environmental stress and MetS risk is poorly understood. However,compelling evidence shows that infancy are windows of particular sensibility to environmental clues which influence lifelong trajectories of health and disease (27). Early-life stress may cause a blunted cortisol response to social stress in later life, moreover, that the long-term adverse effects of early life stress may reach peak levels in adults (28). Furthermore,night shift work disrupted diurnal changes in hypothalamic–pituitary–adrenal (HPA) axis activity associated with cortisol arousal response (29). Continuous maladaptation of the HPA axis leads to various stress disorders such as MetS, hypertension, and diabetes mellitus (30). Previous animal research has displayed a link between early life stress and chronic cardiorenal metabolic pathologies including alterations to organ weight, affective state, and metabolites and/or metabolic paths (31). These conditions are further associated with adverse mental health results and metabolic illnesses including insulin resistance, cardiorenal syndrome, diabetes, and obesity (31).
As a microbial ecosystem, the gut microbiota exerts a significant effect on human health. The composition and function of the human gut microbiota develop over the first years of life, and a strong microbial population is established by age two (32). The gut microbiota encounters several perturbators in individuals who experience trauma during this period, e.g., unhealthy diet or drug exposure (33). If the microbiota cannot oppose these attacks, then a permanent variation happens, resulting in a new balance of microorganisms. This new balance may not be healthy, thus creating a condition called dysbiosis. In addition, it is unlikely that the negative impact of poor nutrition in early life is eliminated by healthy lifestyle elements during adulthood (34). Further research is required to identify the exact mechanisms underlying this association.
Female is a protective factor for MetS in our sample, consistent with other study. As shown in recent results demonstrated that males (6.1%) have nearly twice the prevalence of young-onset MetS compared with females (3.5%) (35). Compared with their study, our study had a higher incidence of MetS. On one hand is because the differences in diagnostic criteria of MetS and on other hand is because their study subjects were relatively young (between 18 and 40 years old). In our sample,females were less likely to work night shift than males (7.7% vs. 33.4%, χ2 = 18.446, P<0.001). Females were also less likely to smoke than males (1.5% vs. 57.8%, χ2 = 102.126, P<0.001).
More importantly, our findings suggest that workers who slept fewer than 7 h were more likely to develop MetS than those who slept 7 h. Previous studies showed that inadequate sleep is a risk element for obesity and diabetes (36). During sleep, the body restores and replenishes energy. Adipokines may exert an effect on mediating the close connection between sleep disorders and systemic metabolic disorders (17). As an adipocyte-derived peptide and a regulator of food intake and energy expenditure, Leptin is related to short sleep duration in the pathophysiology of obesity and accordingly type 2 diabetes (37). The growth of ghrelin levels after sleep loss has been determined in follow-up research (38). Ghrelin is a hormone generated in the oxyntic glands of the stomach and plays an orexigenic role. Hanlon and colleagues studied subjects who slept for only 4.5 h for four nights and found peak midday levels of the most abundant circulating endocannabinoid (eCB), 2-arachidonoylglycerol (2-AG), were elevated in a 24-h profile versus subjects who slept 8.5 h (39). Subjects with restricted sleep also experienced growing hunger and appetite and a reduced capacity of inhibiting snack intake (39). Inadequate sleep may increase the risk of MetS by causing changes in the amount and rhythm of these appetite-regulating hormones.
Consistent with previous studies, we found that current smokers had a higher risk of MetS. It was more likely that smokers show high insulin resistance than their non-smoking counterparts, and smoking cessation may protect against insulin resistance (40). A large sample study on alcohol consumption and MetS in South Korea found that, compared to complete abstinence, drinking less than 7 g/d reduced the risk of MetS, and drinking more than 7.1 g/d grew the risk of MetS (41). We found no relationship between alcohol consumption and MetS probably because we did not divide current drinkers into light and heavy drinkers.
5. Limitations
Other factors that were not included here such as diet and exercise may confound our analysis. These factors were excluded due to the difficulty of performing quantitative analyses on these confounding factors. The sex ratio of men and women in the current sample is unbalanced. Most subjects (92.5%) in this study were male. It is importantly that we corrected for sex as a confounding factor in multifactorial logistic regression (Table 3).
6. Conclusions and future research
Our results show that the risk of MetS is significantly higher in night shift workers exposed to earthquake stress during infancy than day shift workers. We also show that the presence of MetS was significantly higher in males than in females. Earthquake exposure during pregnancy is an independent risk factor for MetS. Smoking and sleeping less than 7 h have a higher risk of MetS than the control group. Future research should use larger sample size to explore hormonal indicators related to early-life stress such as HPA axis-related hormones as well as and biological markers related to the MetS such as orexin, which has been shown to be related to both the MetS and stress in recent studies. Thus, it is important to further investigate the effect of orexin on early-life stress and MetS in adulthood.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Hospital of Hebei Medical University (No 2014005). The patients/participants provided their written informed consent to participate in this study.
Author contributions
XW and NL designed the paper. NL, RW, PH, WL, XZ, and YG performed the experiment. LW, MS, and CA analyzed the data. NL wrote the manuscript. XW, RW, and SB reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the S&T Program of Hebei (SG2021189), Project of Clinical Medical Research Center for Psychiatric and Psychological Disorders of Hebei Province (199776245D), Provincial Science and Technology Program of Hebei Province (21377711D), Hebei Medical University Clinical Research Innovation Team (2022LCTD-A1) and Introduce Foreign Intellectual Projects of Finance Department in Hebei Province (YZ202204). Medical Research Projects from Health Commission of Hebei Province (20210418).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Saklayen, MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. (2018) 20:12. doi: 10.1007/s11906-018-0812-z
2. Zarocostas, J. Need to increase focus on non-communicable diseases in global health, says WHO. BMJ. (2010) 341:c7065. doi: 10.1136/bmj.c7065
3. Hirode, G, and Wong, RJ. Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. JAMA. (2020) 323:2526–8. doi: 10.1001/jama.2020.4501
4. Yao, F, Bo, Y, Zhao, L, Li, Y, Ju, L, Fang, H, et al. Prevalence and influencing factors of metabolic syndrome among adults in China from 2015 to 2017. Nutrients. (2021) 13:4475 doi: 10.3390/nu13124475
5. Huang, Z, Wang, X, Ding, X, Cai, Z, Li, W, Chen, Z, et al. Association of age of metabolic syndrome onset with cardiovascular diseases: the Kailuan study. Front Endocrinol. (2022) 13:857985. doi: 10.3389/fendo.2022.857985
6. Godoy, LC, Frankfurter, C, Cooper, M, Lay, C, Maunder, R, and Farkouh, ME. Association of adverse childhood experiences with cardiovascular disease later in life: a review. JAMA Cardiol. (2021) 6:228–35. doi: 10.1001/jamacardio.2020.6050
7. Burgueño, AL, Juarez, YR, Genaro, AM, and Tellechea, ML. Systematic review and meta-analysis on the relationship between prenatal stress and metabolic syndrome intermediate phenotypes. Int J Obes. (2020) 44:1–12. doi: 10.1038/s41366-019-0423-z
8. Schulz, LC. The Dutch hunger winter and the developmental origins of health and disease. Proc Natl Acad Sci. (2010) 107:16757–8. doi: 10.1073/pnas.1012911107
9. Delpierre, C, Fantin, R, Barboza-Solis, C, Lepage, B, Darnaudéry, M, and Kelly-Irving, M. The early life nutritional environment and early life stress as potential pathways towards the metabolic syndrome in mid-life? A lifecourse analysis using the 1958 British birth cohort. BMC Public Health. (2016) 16:815. doi: 10.1186/s12889-016-3484-0
10. Doom, JR, Reid, BM, Blanco, E, Burrows, R, Lozoff, B, and Gahagan, S. Infant psychosocial environment predicts adolescent Cardiometabolic risk: a prospective study. J Pediatr. (2019) 209:85–91.e1. doi: 10.1016/j.jpeds.2019.01.058
11. Li, C, Tobi, EW, Heijmans, BT, and Lumey, LH. The effect of the Chinese famine on type 2 diabetes mellitus epidemics. Nat Rev Endocrinol. (2019) 15:313–4. doi: 10.1038/s41574-019-0195-5
12. Wang, Z, Zou, Z, Wang, S, Yang, Z, and Ma, J. Chinese famine exposure in infancy and metabolic syndrome in adulthood: results from the China health and retirement longitudinal study. Eur J Clin Nutr. (2019) 73:724–32. doi: 10.1038/s41430-018-0211-1
13. An, C, Zhang, Y, Yu, L, Li, N, Song, M, Wang, L, et al. Long-term impact of earthquake stress on fasting glucose control and diabetes prevalence among Chinese adults of Tangshan. Int J Clin Exp Med. (2014) 7:4441–7.
14. Li, N, Yu, LL, Zhao, XC, Song, M, Wang, L, Gao, YY, et al. Perinatal exposure to earthquake stress increases the risks of hypertension and diabetes in subsequent adult life: a cross-sectional study. J Clin Hypertens. (2020) 22:2354–60. doi: 10.1111/jch.14083
15. Mavrouli, M, Mavroulis, S, Lekkas, E, and Tsakris, A. The impact of earthquakes on public health: a narrative review of infectious diseases in the post-disaster period aiming to disaster risk reduction. Microorganisms. (2023) 11:419 doi: 10.3390/microorganisms11020419
16. Takahashi, S, Yonekura, Y, Tanno, K, Shimoda, H, Sakata, K, Ogawa, A, et al. Increased incidence of metabolic syndrome among older survivors relocated to temporary housing after the 2011 great East Japan earthquake & tsunami. Metabol Open. (2020) 7:100042. doi: 10.1016/j.metop.2020.100042
17. Wei, Z, Chen, Y, and Upender, RP. Sleep disturbance and metabolic dysfunction: the roles of Adipokines. Int J Mol Sci. (2022) 23:1706. doi: 10.3390/ijms23031706
18. Primack, C. Obesity and sleep. Nurs Clin North Am. (2021) 56:565–72. doi: 10.1016/j.cnur.2021.07.012
19. Cheng, WJ, Liu, CS, Hu, KC, Cheng, YF, Karhula, K, and Härmä, M. Night shift work and the risk of metabolic syndrome: findings from an 8-year hospital cohort. PLoS One. (2021) 16:e0261349. doi: 10.1371/journal.pone.0261349
20. Bayon, V, Berger, M, Solelhac, G, Haba-Rubio, J, Marques-Vidal, P, Strippoli, MP, et al. Impact of night and shift work on metabolic syndrome and its components: a cross-sectional study in an active middle-to-older-aged population-based sample. BMJ Open. (2022) 12:e053591. doi: 10.1136/bmjopen-2021-053591
21. Yang, W. Guidelines for the prevention and control of type 2 diabetes in China (2017 edition). Chin J Pract Intern Med. (2018) 38:5–14.
22. Hsu, CN, Hou, CY, Hsu, WH, and Tain, YL. Early-life origins of metabolic syndrome: mechanisms and preventive aspects. Int J Mol Sci. (2021) 22:11872 doi: 10.3390/ijms222111872
23. Stoccoro, A, Nicolì, V, Coppedè, F, Grossi, E, Fedrizzi, G, Menotta, S, et al. Prenatal environmental stressors and DNA methylation levels in placenta and peripheral tissues of mothers and neonates evaluated by applying artificial neural networks. Genes. (2023) 14:836 doi: 10.3390/genes14040836
24. Possamai-Della, T, Cararo, JH, Aguiar-Geraldo, JM, Peper-Nascimento, J, Zugno, AI, Fries, GR, et al. Prenatal stress induces long-term behavioral sex-dependent changes in rats offspring: the role of the HPA axis and epigenetics. [published online ahead of print]. Mol Neurobiol. (2023). doi: 10.1007/s12035-023-03348-1
25. Grilo, LF, Tocantins, C, Diniz, MS, Gomes, RM, Oliveira, PJ, Matafome, P, et al. Metabolic disease programming: from mitochondria to epigenetics, glucocorticoid signalling and beyond. Eur J Clin Investig. (2021) 51:e13625. doi: 10.1111/eci.13625
26. Kazemi, M, Khalili, P, Kazemi, M, Hasani, H, Sadeghi, M, and Jamali, Z. Investigation of the relationship between sleep-related parameters and metabolic syndrome (MetS) among youths in the southeast of Iran. Diabetol Metab Syndr. (2023) 15:91. doi: 10.1186/s13098-023-01072-3
27. Nobile, S, Di Sipio Morgia, C, and Vento, G. Perinatal origins of adult disease and opportunities for health promotion: a narrative review. J Pers Med. (2022) 12:157 doi: 10.3390/jpm12020157
28. Bunea, IM, Szentágotai-Tătar, A, and Miu, AC. Early-life adversity and cortisol response to social stress: a meta-analysis. Transl Psychiatry. (2017) 7:1274. doi: 10.1038/s41398-017-0032-3
29. Ljevak, I, Vasilj, I, Lesko, J, Neuberg, M, Perić, O, and Ćurlin, M. The impact of shift work on the metabolism and circadian rhythm in nurses and medical technicians. Acta Clin Croat. (2022) 60:476–82. doi: 10.20471/acc.2021.60.03.19
30. O'Connor, DB, Thayer, JF, and Vedhara, K. Stress and health: a review of psychobiological processes. Annu Rev Psychol. (2021) 72:663–88. doi: 10.1146/annurev-psych-062520-122331
31. Poplawski, J, Radmilovic, A, Montina, TD, and Metz, GAS. Cardiorenal metabolic biomarkers link early life stress to risk of non-communicable diseases and adverse mental health outcomes. Sci Rep. (2020) 10:13295. doi: 10.1038/s41598-020-69866-3
32. Yatsunenko, T, Rey, FE, Manary, MJ, Trehan, I, Dominguez-Bello, MG, Contreras, M, et al. Human gut microbiome viewed across age and geography. Nature. (2012) 486:222–7. doi: 10.1038/nature11053
33. Cristofori, F, Dargenio, VN, Dargenio, C, Miniello, VL, Barone, M, and Francavilla, R. Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body. Front Immunol. (2021) 12:578386. doi: 10.3389/fimmu.2021.578386
34. Du, R, Zheng, R, Xu, Y, Zhu, Y, Yu, X, Li, M, et al. Early-life famine exposure and risk of cardiovascular diseases in later life: findings from the reaction study. J Am Heart Assoc. (2020) 9:e014175. doi: 10.1161/jaha.119.014175
35. Boisvenue, JJ, Oliva, CU, Manca, DP, Johnson, JA, and Yeung, RO. Identifying sex-specific differences in young-onset metabolic syndrome using primary care electronic Medical record. Metab Syndr Relat Disord. (2023) 21:133–40. doi: 10.1089/met.2022.0065
36. Reutrakul, S, and Van Cauter, E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. (2018) 84:56–66. doi: 10.1016/j.metabol.2018.02.010
37. Mosavat, M, Mirsanjari, M, Arabiat, D, Smyth, A, and Whitehead, L. The role of sleep curtailment on leptin levels in obesity and diabetes mellitus. Obes Facts. (2021) 14:214–21. doi: 10.1159/000514095
38. van Egmond, LT, Meth, EMS, Engström, J, Ilemosoglou, M, Keller, JA, Vogel, H, et al. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: a laboratory study. Obesity. (2022) 31:635–41. doi: 10.1002/oby.23616
39. Hanlon, EC, Tasali, E, Leproult, R, Stuhr, KL, Doncheck, E, de Wit, H, et al. Sleep restriction enhances the daily rhythm of circulating levels of endocannabinoid 2-Arachidonoylglycerol. Sleep. (2016) 39:653–64. doi: 10.5665/sleep.5546
40. Cho, SH, Jeong, SH, Shin, J, Park, S, and Jang, SI. Short-term smoking increases the risk of insulin resistance. Sci Rep. (2022) 12:3550. doi: 10.1038/s41598-022-07626-1
Keywords: pregnancy, infancy, earthquake stress, metabolic syndrome, night shift work, adulthood
Citation: Li N, Wang R, Hu P, Lu W, Zhao X, Wang L, Song M, Gao Y, An C, Bashir S and Wang X (2023) Effect of night shift work on metabolic syndrome in adults who suffered from earthquake stress in early life. Front. Public Health. 11:1139113. doi: 10.3389/fpubh.2023.1139113
Edited by:
Olga Pivovarova-Ramich, German Institute of Human Nutrition Potsdam-Rehbruecke (DIfE), GermanyReviewed by:
Man Guo, The Affiliated Hospital of Southwest Medical University, ChinaSteven K. Malin, Rutgers, The State University of New Jersey, United States
Copyright © 2023 Li, Wang, Hu, Lu, Zhao, Wang, Song, Gao, An, Bashir and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xueyi Wang, eWR5eXd4eUAxNjMuY29t
†These authors have contributed equally to this work
 Na Li
Na Li Ran Wang
Ran Wang Peihua Hu1,2,3
Peihua Hu1,2,3 Lan Wang
Lan Wang