- 1School of Public Health and Women’s Hospital, Zhejiang University School of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
- 2School of Public Health, Zhejiang University School of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
- 3Department of Orthopedic Surgery, The Forth Affiliated Hospital, International Institutes of Medicine, Zhejiang University School of Medicine, Yiwu, Zhejiang, China
- 4School of Public Health, Hangzhou Medical College, Hangzhou, Zhejiang, China
Background: Self-rated health (SRH), interviewer-rated health (IRH), and objective health reflect the overall health status from different aspects. This study aimed to investigate the associations of SRH, IRH, and objective health with mortality among Chinese older adults.
Methods: This study used data from the 2008 (baseline), 2011, 2014 and 2018 waves of the Chinese Longitudinal Healthy Longevity Survey. SRH and IRH were evaluated by questionnaire. Objective health was evaluated by the Chinese multimorbidity-weighted index (CMWI), which incorporated 14 diagnosed chronic diseases. SRH, IRH, and CMWI were assessed as: (1) baseline levels; (2) longitudinal changes by subtracting the values obtained in 2008 from the corresponding values in 2014; (3) trajectories by Group-Based Trajectory Modeling, respectively. The Cox proportional hazards model was used to explore the associations of baseline SRH, IRH, and CMWI, their changes, and trajectories with mortality.
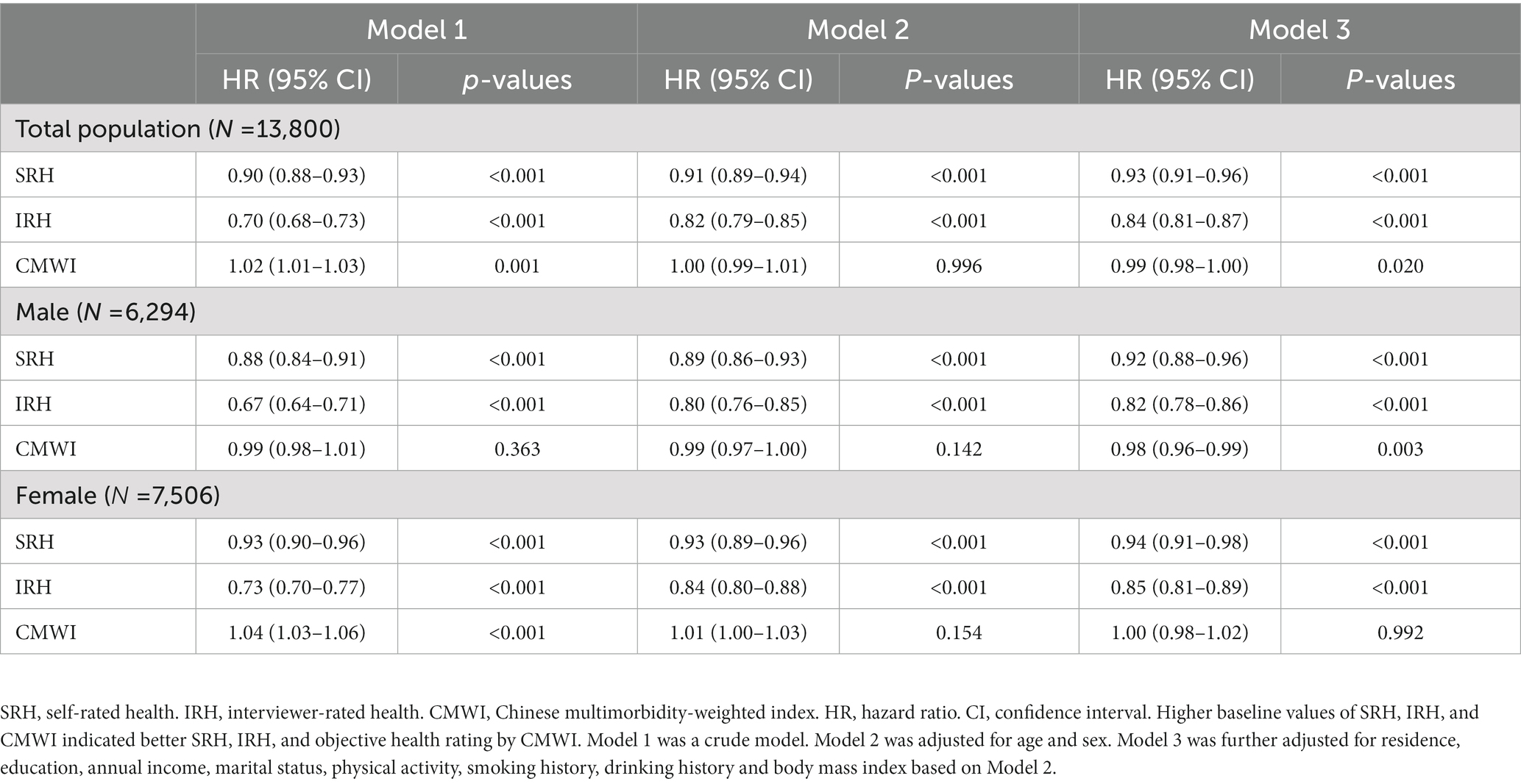
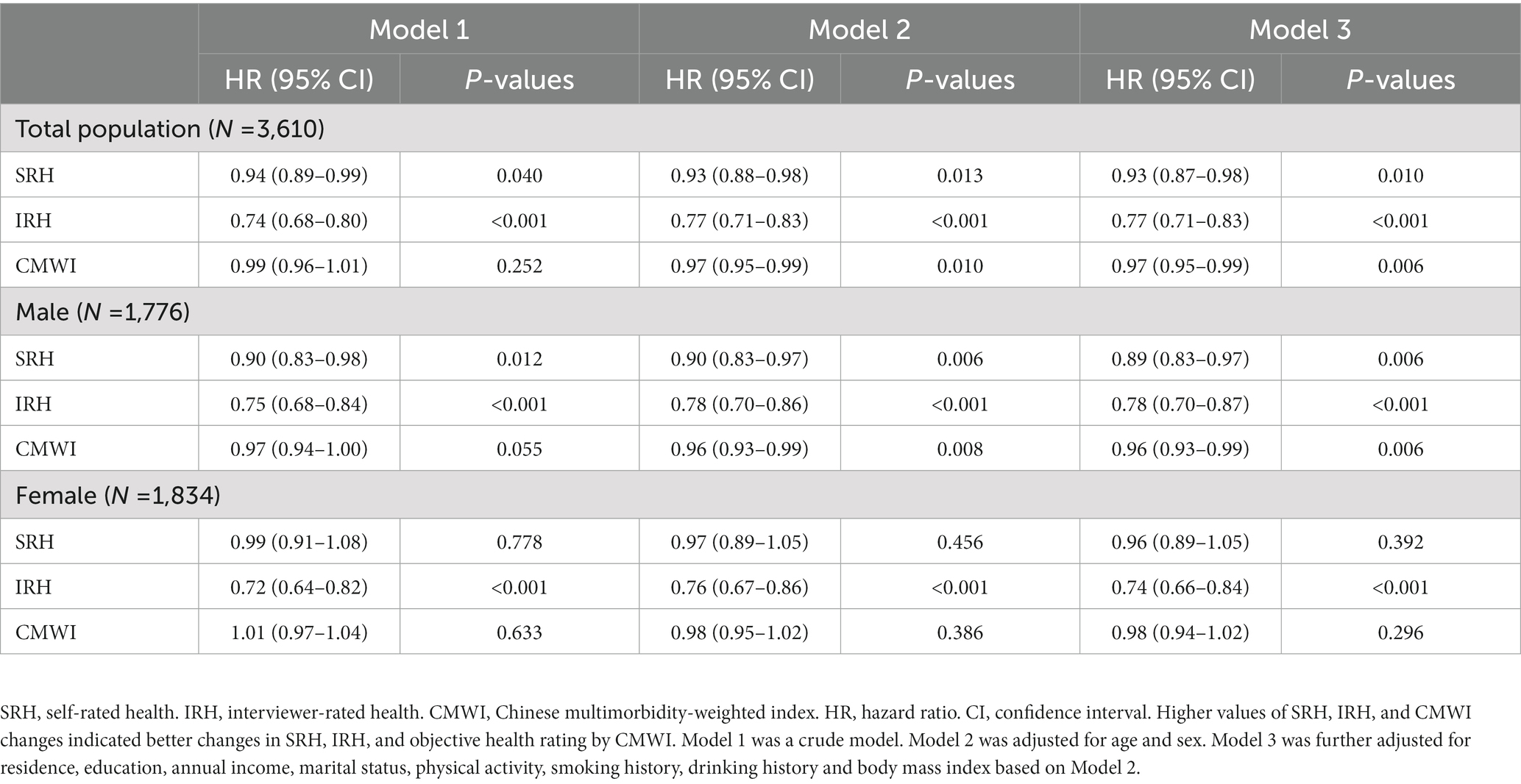
Results: A total of 13,800 participants were included at baseline (2008). The baseline SRH ([hazard ratio] 0.93, [95% confidence interval] 0.91–0.96), IRH (0.84, 0.81–0.87), and CMWI (0.99, 0.98–1.00) in 2008 were significantly associated with 10-year mortality (2008 to 2018). Among 3,610 participants, the changes of SRH (0.93, 0.87–0.98), IRH (0.77, 0.71–0.83), and CMWI (0.97, 0.95–0.99) from 2008 to 2014 were significantly associated with 4-year mortality (2014–2018). The trajectories were divided into “high SRH/IRH/CMWI” and “low and declining SRH/IRH/CMWI.” Compared with “low and declining SRH/IRH/CMWI,” “high SRH” (0.58, 0.48–0.70), “high IRH” (0.66, 0.55–0.80), and “high CMWI” (0.74, 0.61–0.89) from 2008 to 2014 were significantly associated with 4-year mortality (2014–2018).
Conclusion: Baseline SRH, IRH, and CMWI, their changes and trajectories are all associated with mortality in Chinese older adults. It is possibly necessary to promote the use of cost-effective indicators in primary medical institutions to improve the health management of the older adults.
Introduction
With the declining fertility rate and the development of modern medical care, the aging process in China accelerates (1). According to the Seventh National Population Census of the People’s Republic of China, in 2020, the people aged 60 and above, 65 and above accounted for 18.70 and 13.50% of the total Chinese population, respectively (2). It is projected that by 2050, the proportion of people aged 65 and above will increase to 26.9% of the total Chinese population (3). Meanwhile, as the prevalence of chronic diseases among the older adults continues to grow, the associated burden on public health and socioeconomic development becomes more severe (4). Hence, cost-effective health indicators for the older adults are expected to help public health institutions identify high-risk groups and allocate resources effectively to improve health management in an aging society.
In recent years, simplified indicators of health status have gained attention from researchers. One such indicator is Self-Rated Health (SRH), which measures respondents’ own evaluation of their health status, and encompasses physical health, mental health, and social participation simultaneously (5, 6). Previous studies have confirmed the reliability of SRH in predicting overall health (7), and the World Health Organization (WHO) has recommended SRH as a cost-effective and reliable surrogate indicator of health status (8). However, SRH may exhibit disparities among individuals due to a set of cognitive factors, such as different understanding of health. Interviewer-Rated Health (IRH) addresses this limitation by enabling interviewers to evaluate respondent’s health status during interviews (9). Interviewers often have a more comprehensive and objective perception of health than respondents themselves, and thus IRH can provide supplemental information to SRH, such as respondents’ living environments and lifestyle habits (9). However, these subjective health indicators may lack specificity and pose challenges in ensuring the accuracy of information, particularly when they are used to determine eligibility for further care resources (10). In contrast to subjective health, objective health refers to the health status of respondents characterized by objectively measured biochemical or functional indicators. Recently, the Chinese multimorbidity-weighted index (CMWI) has been proposed as an objective health evaluation index that can quantify the burden of multimorbidity among Chinese older adults through routinely physical examinations at the community health care center (11).
Previous studies have illustrated that poor subjective and objective health were associated with an increased risk of mortality in older adults (12–18). A study involving 373,761 participants from the UK Biobank investigated the associations of different combinations of SRH and objective health status with all-cause mortality, and found that individuals with concordant favorable SRH and health status had the lowest hazard of mortality, while those with concordant unfavorable SRH and health status had the highest hazard of mortality, and those with discordant SRH and health status had intermediate hazards of mortality (19). However, studies also indicated that health status is dynamic and can change over a long follow-up period (20). Some studies have explored the associations of the change and trajectory of SRH with mortality, but the findings have been inconsistent (21–24). For instance, the Lifelines Cohort Study suggested that older adults individuals with a stable poor SRH trajectory often had unfavorable health status (21). While another study with 3,129 participants indicated no significant associations between SRH trajectories and mortality (24). Besides, it remains unclear whether changes and trajectories of IRH and CMWI over time are associated with mortality.
To fill this research gap, we aimed to investigate (1) the association of baseline SRH, IRH, and CMWI with mortality; (2) the association of changes of SRH, IRH, and CMWI (the values of SRH, IRH, and CMWI in 2014 minus the values in 2008) with mortality; (3) the association of trajectories of SRH, IRH, and CMWI (constructed by the values of SRH, IRH, and CMWI in 2008, 2011, and 2014) with mortality.
Methods
Study design and participants
The data used in this study came from the 2008, 2011, 2014, and 2018 waves of the Chinese Longitudinal Healthy Longevity Survey (CLHLS), an ongoing and national prospective cohort study of community-dwelling Chinese older adults, which aims to investigate factors related to health and longevity. Details of the CLHLS have been reported elsewhere (25–28). The baseline survey in 2008 consisted of face-to-face questionnaire interviews (including sociodemographic, SRH, IRH, medication history and medical history), physical measurements (including blood pressure, height and weight), and blood sample collection. Standard procedures were followed by well-trained examiners (27).
The CLHLS was approved by The Research Ethics Committees of Peking University (IRB00001052-13074) and Duke University Health System’s Institutional Review Board. Informed consent was obtained from all respondents or their proxy respondents.
Measures
SRH
SRH was defined using the following question, “How do you rate your health at present?” Responses to this question were graded with options of “very good,” “good,” “fair,” “poor,” “very poor,” and “unable to answer.” We combined “poor” and “very poor” considering small frequencies, and recorded “unable to answer” as “missing” in the analysis. The categories of “poor/very poor,” “fair,” “good,” and “very good” were assigned 1–4 points in turn.
IRH
IRH was defined using the question, “how does the older adults look?” to rate the respondent’s overall health by interviewers during each wave. The options, including “moderately or severely ill,” “slightly ill,” “relative healthy,” or “healthy,” were given 1–4 points in turn.
CMWI
The development process of CMWI has been described in detail elsewhere (11). Briefly, CMWI was developed using physical functioning (PF) as the outcome variable and 14 chronic diseases as predictors, based on data from the China health and retirement longitudinal study. A linear mixed model was used to quantify the weights of each disease in the multimorbidity burden. The effect of each chronic disease on PF was measured with the relevant regression coefficient after adjusting for age, sex and other chronic diseases, and the absolute value of which was denoted as the weight of the disease. For the calculation of CMWI, the following 14 chronic diseases were assigned a score (X1 to X14) of 1 (yes) or 0 (no) depending on whether the participant had a disease: stroke, memory-related diseases (dementia and Parkinson’s disease), cancer or malignant tumor, asthma, arthritis or rheumatism, emotional, nervous or psychiatric problems, heart disease, chronic lung diseases, hypertension, kidney disease, diabetes or high blood sugar, stomach or other digestive disease, dyslipidemia and liver disease.
Blood pressure was measured two times at a 1-min interval. The average of the two measurements was calculated to the nearest 1 mmHg for analysis. Hypertension was defined as: (1) systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, and/or (2) self-reported having been diagnosed with hypertension, and/or (3) being treated for hypertension. A 5 mL fasting venous blood sample was collected in heparin anticoagulant vacuum tubes by veteran medical staff. The local Center for Disease Control and Prevention was in charge of routine blood and urine testing. The samples were then transported to Beijing using the specific transport boxes. The central laboratory at Capital Medical University analyzed the samples and tested indicators including four items of blood lipid tests (triglyceride, total cholesterol, high density lipoprotein cholesterol, low density lipoprotein cholesterol) and blood glucose. Diabetes and high blood sugar were defined as: (1) fasting blood glucose >6.1 mmoL/L, and/or (2) self-reported having been diagnosed with diabetes, and/or (3) being treated for diabetes. Dyslipidemia was defined as: (1) triglyceride >1.71 mmoL/L, and/or (2) total cholesterol >5.18 mmoL/L, and/or (3) high-density lipoprotein <1.04 mmoL/L, and/or (4) low-density lipoprotein >3.10 mmol/, and/or (5) self-reported dyslipidemia, and/or (6) being treated for dyslipidemia. Other diseases were defined as self-reported having been diagnosed by doctors and/or being treated for corresponding diseases. The value of CMWI was calculated using the following formula (11):
where Xi referred to the score of 1 (yes) or 0 (no) depending on whether the participant had the following 14 diseases: stroke, memory-related diseases (dementia and Parkinson’s disease), cancer or malignant tumor, asthma, arthritis or rheumatism, emotional, nervous or psychiatric problems, heart disease, chronic lung diseases, hypertension, kidney disease, diabetes or high blood sugar, stomach or other digestive disease, dyslipidemia, and liver disease.
Death
The participant’s survival status and/or date of death was collected during the follow-up (2011, 2014, and 2018). The death of the participants was confirmed and determined by a close family member or a doctor.
Covariates
Covariates included socio-demographic characteristics (e.g., age, sex, residence, education, annual income, marital status, physical activity, smoking, and drinking history) and body mass index (BMI). Age was defined as continuous variables. Residence was classified as rural and urban. Education was divided into illiteracy, primary education, and middle school or above. Annual income had three categories: CNY 0–29,999, CNY 30,000–59,999, and > CNY 60,000. Marital status included married or cohabitation, and unmarried or widowed. Physical activity was divided as no and yes. Smoking history was classified as never smoking and ever smoking (including current smoking). Similarly, drinking history was classified as never drinking and ever drinking (including current drinking). BMI (kg/m2) was calculated as weight (kg) divided by the square of height (m), which was further analyzed as a continuous variable.
Statistical analysis
The baseline characteristics were described as the mean with standard deviation (SD) for normally distributed continuous variables, the median with interquartile range (IQR) for nonnormally distributed continuous variables, and numbers with percentage (%) for categorical variables. Wilcoxon rank-sum tests for continuous variables and Chi-square tests for categorical variables were used to evaluate the differences between participants who have died and who survived or lost to follow-up. Three analyses were conducted:
First, a multivariable Cox proportional hazards model with hazard ratios (HRs) and 95% confidence intervals (CIs) with the follow-up time in years as the time scale was used to explore the associations of baseline SRH, IRH, and CMWI (2018) as continuous variables with 10-year mortality (2008–2018). Model 1 was unadjusted; Model 2 was adjusted for age and sex; Model 3 was further adjusted for residence, education, annual income, marital status, physical activity, smoking history, drinking history, and BMI based on model 2. Sensitive analyses were also conducted to investigate the associations of SRH and IRH as categorical variables with 10-year mortality as a robustness check. Since the associations between SRH, IRH, CMWI and mortality may be different between males and females, the sex-stratified multivariable logistic regression was conducted as well (29).
Second, the multivariable Cox proportional hazards model was used to explore the associations between the changes of SRH, IRH, CMWI (2008–2014) and the 4-year mortality (2014–2018). The changes of SRH, IRH, and CMWI were defined as the values in 2014 minus the values in 2008. Improvements of health were those that had a change value larger than zero. All models and adjustments were consistent with those above.
Third, the trajectories of SRH, IRH, and CMWI in 2008, 2011, and 2014 were plotted and grouped using Group-Based Trajectory Modeling (GBTM). GBTM can divide the whole population into individual clusters with similar trajectories according to the trajectory of a certain feature over time (30). By comparing the Akaike information criterion (AIC) and Bayesian information criterion (BIC), the model with the lowest AIC and BIC values was selected as the model with the highest fit level. A multivariable Cox proportional hazards model was used to explore the associations between the trajectories of SRH, IRH, and CMWI (2008–2014) with 4-year mortality (2014–2018). All adjustments were consistent with that in above mentioned models.
The baseline levels and longitudinal changes of SRH, IRH, and CMWI were considered as continuous variables, while their trajectories were considered as nominal variables. All analyses were performed using SAS statistical software (version 9.4; SAS Institute Inc., Cary, NC, United States). p-value <0.05 was considered statistically significant.
Results
Selection of study participants
Of 16,954 participants in the 2008 wave of the CLHLS, 13,800 participants were included in the analyses of the associations between baseline indicators (SRH, IRH, or CMWI in 2008) and subsequent 10-year mortality (2008–2018), while 3,154 participants who had missing data on socio-demographic characteristics, BMI, SRH, IRH or CMWI were excluded. Then, those who died, lost to follow-up, or had missing data on SRH, IRH, or CMWI in 2014 were excluded, leaving 3,610 participants in the analyses of the associations between changes of indicators (SRH, IRH, or CMWI from 2008 to 2014) and subsequent 4-year mortality (2014–2018). Finally, since GBTM required at least three times of measurements on SRH, IRH, and CMWI, a total of 2,594 participants were included in the analyses of the associations between trajectories of indicators (SRH, IRH, or CMWI from 2008 to 2014) and subsequent 4-year mortality (2004–2018), after excluding participants who had missing data on SRH, IRH, or CMWI in 2011 (Figure 1) (31).
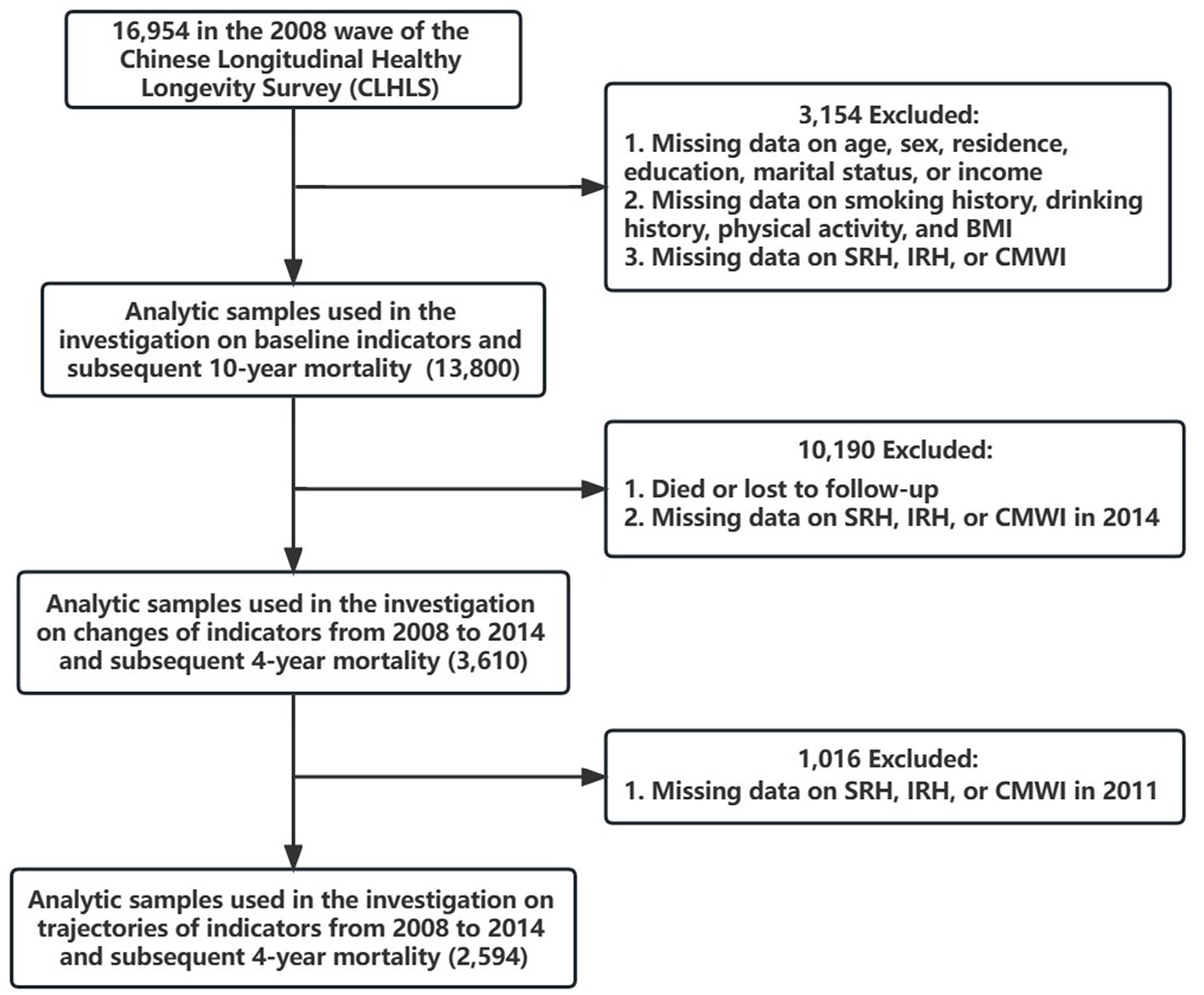
Figure 1. Flow chart. BMI, body mass index. SRH, self-rated health. IRH, interviewer-rated health. CMWI, Chinese multimorbidity-weighted index.
Baseline SRH, IRH, and CMWI with 10-year mortality
The baseline characteristics of participants included in analyses of baseline SRH, IRH, and CMWI (2008) with 10-year mortality (2008–2018) are shown in Supplementary Table S1. Compared with participants who survived or lost to follow-up within 10 years, the older adults who died were older, with lower education level, lower annual income, smaller BMI, less physical activity. They were more likely to be in rural areas, be married or cohabitation. They also had significantly differences in SRH, IRH, and CMWI (all p < 0.05).
The multivariable Cox proportional hazards model showed that higher baseline SRH (HR 0.93, 95% CI 0.91–0.96), IRH (HR 0.84, 95% CI 0.81–0.87), and CMWI (HR 0.99, 95% CI 0.98–1.00) were significantly associated with lower 10-year mortality (Table 1). The results in sensitive analyses revealed consistent patterns with the main results (Supplementary Table S2). The results in males and females are also shown in Table 1. The association between CMWI (2008) and subsequent 10-year mortality (2008–2018) was not significant in females (HR 1.00, 95% CI 0.98–1.02).
Changes of SRH, IRH, and CMWI with 4-year mortality
Since there was a considerable loss of participants after the exclusions (n = 10,190), we compared characteristics of study participants and excluded participants in the changes of SRH, IRH, and CMWI with 4-year mortality (Supplementary Table S3). Supplementary Table S4 shows that in analyses of changes of SRH, IRH, and CMWI (2008–2014) with 4-year mortality (2014–2018), 3,610 participants were included, in which 928 participants died (median age 84.0 [IQR 77.0–90.0]) and 2,682 participants survived or were lost to follow-up (median age 74.0 [IQR 69.0–81.0]). The older adults who died had significantly lower baseline SRH and IRH (all p < 0.05).
The results in Table 2 showed that participants with better changes of SRH (HR 0.93, 95% CI 0.87–0.98), IRH (HR 0.77, 95% CI 0.71–0.83), and CMWI (HR 0.97, 95% CI 0.95–0.99) showed significantly lower 4-year mortality. When stratified by sex, the results were similar in males, but in females, only the change of IRH was significantly associated with 4-year mortality (HR 0.74, 95% CI 0.66–0.84).
Trajectories of SRH, IRH, and CMWI with 4-year mortality
The baseline characteristics of participants included in analyses on the trajectory of predictors and 4-year mortality from 2014 to 2018 was shown in Supplementary Table S5. Compared with participants who survived or were lost to follow-up within 4 years, the older adults who died had significantly lower SRH and IRH (all p < 0.05). Supplementary Table S6 indicated that when trajectories were divided into 2, the models of SRH, IRH, and CMWI had the lowest AIC and BIC values (AIC = −11345.1, BIC = −11368.5 for the trajectory of SRH; AIC = −8887.4, BIC = −8910.8 for the trajectory of IRH; AIC = −16987.7, BIC = −17011.1 for the trajectory of CMWI). Supplementary Figure S1 showed the trajectories of SRH, IRH, and CMWI, respectively. The higher SRH, IRH, and CMWI trajectories were named “high SRH/IRH/CMWI,” and the others were named “low and declining SRH/IRH/CMWI.”
Taking “low and declining SRH/IRH/CMWI” as the reference, we found that high SRH (HR 0.58, 95% CI 0.48–0.70), high IRH (HR 0.66, 95% CI 0.55–0.80), and high CMWI (HR 0.74, 95% CI 0.61–0.89) were associated with lower 4-year mortality (Table 3). However, the association between the trajectory of CMWI and 4-year mortality was not significant in females (HR 0.76, 95% CI 0.57–1.02).
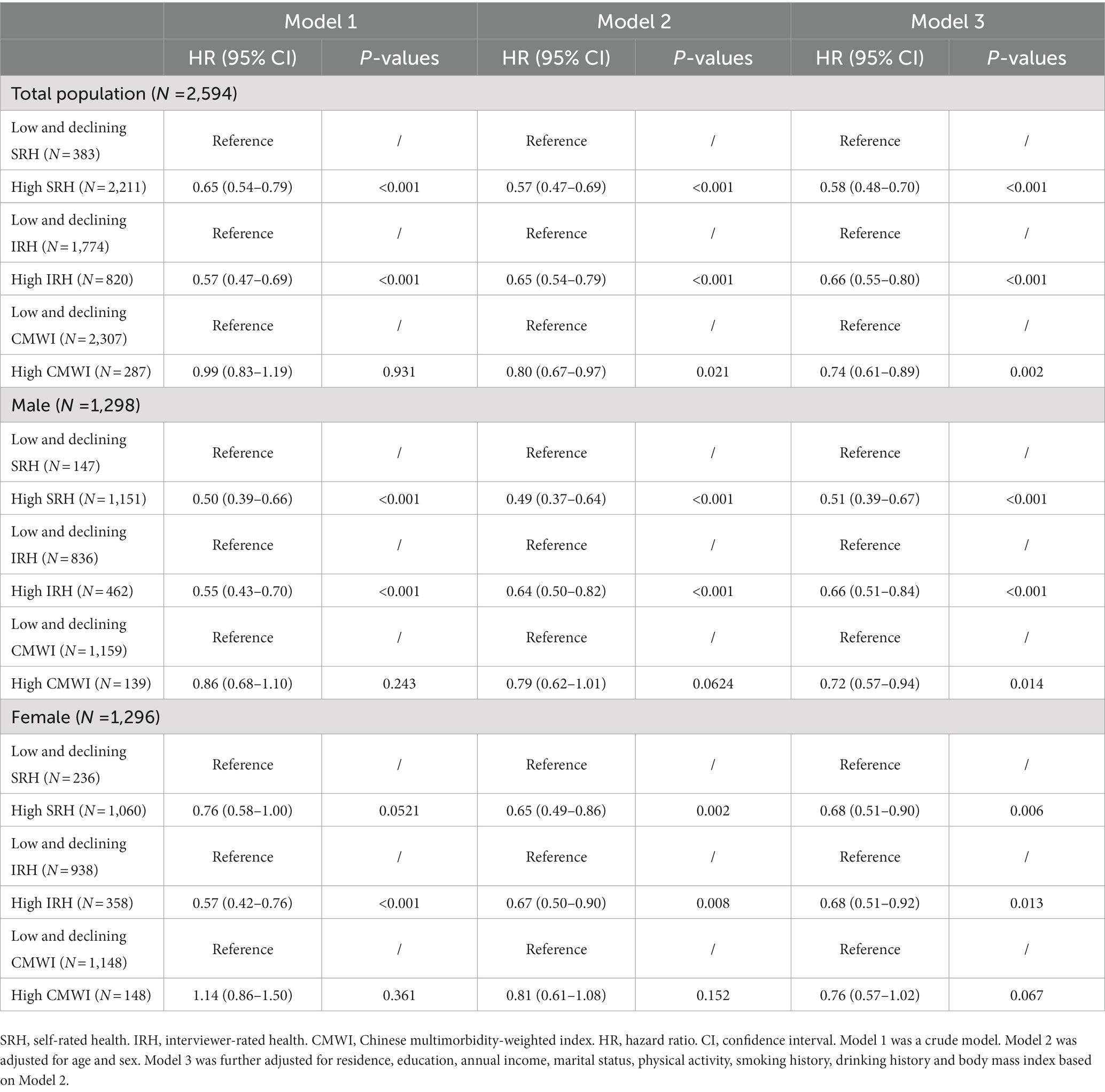
Table 3. Trajectories of SRH, IRH, and CMWI from 2008 to 2014 with 4-year mortality from 2014 to 2018.
Discussion
Our study found that baseline SRH, IRH, and CMWI were all negatively associated with 10-year mortality in Chinese older adults. Better changes and trajectories of SRH, IRH, and CMWI were also significantly associated with lower 4-year mortality in Chinese older adults.
Previous studies have revealed the negative associations of baseline SRH, IRH, and objective health with mortality, which were in line with our results (11, 16, 29, 32, 33). First, SRH is a subjective assessment based on objective health status (34), therefore serves as a statistical indicator with a condensed overview of physical information (5). Second, compared to objective indicators of health, SRH might capture the burden of subclinical conditions, such as high blood pressure, early stages of diabetes, and preclinical forms of cancer (35). Third, poor SRH sometimes mirrors mental stress, which can lead to elevations in serum proinflammatory cytokines (36–38). Inflammation is associated with symptoms of sickness behavior, such as lethargy, decreased appetite, and behavioral withdrawal, which in turn will have an impact on SRH (39). Additionally, the dysregulation of inflammation leads to the development of illnesses and raises the risk of mortality in older adults (40–42). Consequently, elevated levels of circulating inflammatory markers contribute to both a decrease in SRH and an increase in mortality risk (43).
Some recent studies reported that IRH is a better indicator of mortality than SRH, and investigated the potential mechanisms underlying the association. For instance, using data from CLHLS, Feng et al. found that the association between IRH and mortality remained significant even after adjusting for SRH (7). Similarly, Todd M A and Goldman N used an older adults cohort in Taiwan to compare the predictive power of SRH, IRH, and health ratings from physicians on 5-year mortality, and revealed that IRH was the most accurate predictor (16). Several reasons have been put forward to explain why IRH may be a better predictor of mortality than SRH. First, when evaluating SRH, respondents may underestimate health-related behaviors and functional limitations (44), whereas interviewers who assess IRH can weigh and integrate individual information more effectively (45). Moreover, interviewers may be able to capture unmeasured health information that SRH lacks through on-site observations, such as respondents’ appearance and living situation. Second, in CLHLS, the rating process is done immediately following the interviewer’s completion of data collection, therefore IRH incorporates detailed information about the participants overall health, including their SRH. Third, trained interviewers can maintain a consistent and relatively objective evaluation standard when investigating multiple respondents, avoiding personal biases to some extent. Furthermore, interviewers generally have higher educational attainment than the respondents, which could help them accurately summarize information during the interview and provide a more accurate assessment of the respondent’s health conditions (7, 16, 44). Incorporating both self-rated and interviewer-rated health could provide a more complete understanding of a person’s health status.
Previous studies produced contradictory results of gender differences in the association between SRH and mortality (46). Our results indicate that SRH was associated with mortality in male. In females, however, there was no association between the change of SRH and mortality. These sex differences in the associations between subjective health indicators and mortality may result from the different health self-perceptions, which means the meaning of “health” differs between sexes (46). Also, the covariates may be different between males and females. Besides, it is noteworthy that sex-stratified analyses showed that compared to male, the association between CMWI and mortality was not significant in females, which was consistent with result from Wuorela et al. (47). One explanation could be that although women have poorer health status, they can tolerate more frailty than men. It could also result from biological and social factors (48, 49).
Multimorbidity, defined as the presence of two or more chronic diseases in the same individual, reflects worse health status and is associated with mortality (50). Previous study has shown that CMWI is a superior predictor of mortality among the Chinese older adults compared to other multimorbidity indexes, as its disease weights were tailored to the Chinese middle-aged and older community-dwelling adults (11). When stratified by sex, we found that baseline CMWI, together with its change and trajectory was not associated with subsequent mortality in female. This may be due to several limitations. First, mental function was not considered in the development and validation of CMWI due to limited mental health measures. This may result in information bias, as there are sex-differences in mental health conditions. Second, the collection of information on chronic diseases were largely gathered by self-report, which may lead to reporting bias. Third, the burden of multimorbidity may have been underestimated because the severity of the disease was not taken into account while calculating CMWI. Thus, further studies are needed to investigate the sex-specific factors behind CMWI and explore a more universally applicable indicator of mortality for both males and females.
Previous studies have investigated the association between changes and trajectories in SRH and mortality, but the results have not been consistent. For instance, the Women’s Health and Aging Study suggested that change in SRH was a stronger indicator of mortality than baseline SRH (23). While another study found that SRH trajectories did not have a significant, direct impact on mortality (24). The inconsistent findings might stem from variations in investigation date, sample size, studying setting, and other factors. Our study confirmed significant associations of changes and trajectories in SRH with mortality, and further indicated that the changes and trajectories of IRH and CMWI were also associated with mortality in Chinese older adults. These indicators are dynamic and change over time during the follow-up period (46, 51). Neglecting to assess SRH as a dynamic indicator may lead to a misinterpretation of the association between SRH and mortality (52). One study revealed that baseline SRH was only associated with 4-year mortality, but not with 9-year mortality among old female (53). A research also indicated that poor baseline SRH was associated with higher risk of 10-year mortality, but no longer with 18-year mortality in older male (38). Idler and Benyamini proposed the trajectory hypothesis, which suggested that people incorporated changes in prior health status into their current health evaluations, and that poor SRH indicated assessments of their future decline or death (24, 29). Since the changes and trajectories are originated from different interview points, their evaluation often involve all the information of multiple time points. Besides, changes in other information such as socioeconomics factors, which are not included in the questionnaire can be reflected in the changes and trajectories of indicators (7). Therefore, the changes and trajectories of indicators contain a wider range of information than baseline.
Numerous studies have explored a range of mortality indicators, such as multimorbidity-weighted index and the Elixhauser comorbidity index. However, their widespread use in densely populated developing countries like China is challenging due to their high cost and implementation complexity (11). Besides, previous studies have also shown that the combination of subjective and objective health indicators could provide a simple measure for risk classification (19). Our study highlights the applicability of SRH, IRH, and CMWI, particularly in geriatric health-related studies. Because SRH, IRH, and CMWI are easy to use and cost-effective, it is realistic to popularize them in grassroots communities and rural areas in China, and conducive to the government’s preliminary understanding of the health status of the local older adults. Formulating a more appropriate health promotion plan for the older adults can promote the healthy aging construction of Chinese society.
Strengths and limitations
To the best of our knowledge, this study was the first prospective cohort study to comprehensively explore the association of baseline SRH, IRH, and CMWI, their changes and trajectories with subsequent mortality in Chinese older adults. Moreover, with the national sample, the CLHLS represented community-based older adults from 22 Chinese provinces, ensuring that our findings were reliable and generalizable.
This study had several limitations. First, we merged “poor” and “very poor” SRH due to the limitations of sample size, which may lead to information bias. Also, since we used the continuous forms of SRH and IRH, the results of baseline values and changes of SRH and IRH with mortality might be difficult to interpret. However, the sample sizes in some groups were relatively small when considering SRH and IRH as categorial variables. We have conducted sensitive analyses to investigate the associations of SRH and IRH as categorical variables with 10-year mortality. The results were consistent with the main findings, supporting the robustness of our approach. Second, the number of participants included in the analysis of the trajectory was relatively small, thus, the trajectory of IRH was not smooth enough. However, this limitation did not influence the association between trajectories of indicators and mortality. Further studies are needed in a larger population. Third, some of the covariates, such as physical activity and smoking history, were lacking more detailed data in the questionnaire of CLHLS, which may result in potential residual confounding in the associations. Finally, some potential covariates, such as type of work, social participation, may have been neglected in the adjustment.
Conclusion
SRH, IRH, and CMWI are practical and accurate indicators of mortality in the Chinese older adults. More researches are required to promote the application and generalization of cost-effective indicators in the field of health assessment and monitoring among Chinese older adults.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
PS designed the study. ZR and SS managed and analyzed the data. SS and SC prepared the first draft. SS, JC, SC, KT, SL, WS, LH, and QY reviewed and edited the manuscript, with comments from PS. All authors involved in revising the manuscript, had full access to the data, and gave final approval of the submitted versions.
Funding
Data used for this research was provided by the study entitled “Chinese Longitudinal Healthy Longevity Survey” (CLHLS) managed by the Center for Healthy Aging and Development Studies, Peking University. CLHLS was supported by funds from the U.S. National Institutes on Aging (NIA), China Natural Science Foundation, China Social Science Foundation, and UNFPA. The study sponsors had no role in the study design, analysis, interpretation of data, writing of the report, or in the decision to submit the paper for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1137527/full#supplementary-material
References
1. Liangchu, Y. Research on fertility policy to cope with the challenge of population aging. Soc Sec Stud. (2021) 78, 05:39–48. doi: 10.3969/j.issn.1674-4802.2021.05.004
2. Tu, WJ, Zeng, X, and Liu, Q. Aging tsunami coming: the main finding from China’s seventh national population census. Aging Clin Exp Res. (2022) 34:1159–63. doi: 10.1007/s40520-021-02017-4
3. Fang, EF, Scheibye-Knudsen, M, Jahn, HJ, Li, J, Ling, L, Guo, H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
4. Guixin, W. Future challenges and coping strategies of population ageing in China. Governance. (2022) 10:50–6.
5. Jylhä, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. (2009) 69:307–16. doi: 10.1016/j.socscimed.2009.05.013
6. Mossey, JM, and Shapiro, EJAJOPH. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. (1982) 72:800–8. doi: 10.2105/AJPH.72.8.800
7. Feng, Q, Zhu, H, Zhen, Z, and Gu, D. Self-rated health, interviewer-rated health, and their predictive powers on mortality in old age. J Gerontol B Psychol Sci Soc Sci. (2016) 71:538–50. doi: 10.1093/geronb/gbu186
8. De Bruin, A. Health interview surveys: towards international harmonization of methods and instruments. WHO Reg Publ Eur Ser. (1996) 58:1–161.
9. Zhu, H, Feng, Q, and Gu, DJIJOPS. Self-rated health and interviewer-rated health: differentials in predictive power for mortality among subgroups of Chinese elders. Int J Popul Stud. (2017) 2:74–91. doi: 10.18063/IJPS.2016.02.007
10. Lima-Costa, MF, Cesar, CC, Chor, D, and Proietti, FA. Self-rated health compared with objectively measured health status as a tool for mortality risk screening in older adults: 10-year follow-up of the Bambuí cohort study of aging. Am J Epidemiol. (2012) 175:228–35. doi: 10.1093/aje/kwr290
11. Hu, WH, Liu, YY, Yang, CH, Zhou, T, Yang, C, Lai, YS, et al. Developing and validating a Chinese multimorbidity-weighted index for middle-aged and older community-dwelling individuals. Age Ageing. (2022) 51:afab274. doi: 10.1093/ageing/afab274
12. Garbarski, D, Schaeffer, NC, and Dykema, J. Interviewers’ ratings of respondents’ health: predictors and association with mortality. J Gerontol B Psychol Sci Soc Sci. (2019) 74:1213–21. doi: 10.1093/geronb/gbx146
13. Idler, EL, Benyamini, YJJOH, and Behavior, S. Self-rated health and mortality: a review of twenty-seven community studies. J. Health Soc. Behav. (1997) 38:21–37.
14. Idler, EL, and Kasl, S. Health perceptions and survival: do global evaluations of health status really predict mortality? J Gerontol. (1991) 46:S55–65. doi: 10.1093/geronj/46.2.S55
15. Miller, AC, O’reilly, D, Kee, F, Cruise, S, and Young, I. Multimorbidity, activity limitation and self-reported health all predict mortality risk, but better measures were required. J Clin Epidemiol. (2022) 144:144–62. doi: 10.1016/j.jclinepi.2021.12.010
16. Todd, MA, and Goldman, N. Do interviewer and physician health ratings predict mortality? A comparison with self-rated health. Epidemiology. (2013) 24:913–20. doi: 10.1097/EDE.0b013e3182a713a8
17. Valanis, BG, and Yeaworth, RJRIN, Health. Ratings of physical and mental health in the older bereaved. Res Nurs Health. (1982) 5:137–46. doi: 10.1002/nur.4770050305
18. Yuzhi, L, and Qiang, L. The relationship between self-rated health and mortality risk of the Chinese oldest old. Chin J Popul Sci. (2004) 04:30–37+81. doi: 10.3969/j.issn.1000-7881.2004.04.004
19. Mutz, J, and Lewis, CM. Cross-classification between self-rated health and health status: longitudinal analyses of all-cause mortality and leading causes of death in the UK. Sci Rep. (2022) 12:459. doi: 10.1038/s41598-021-04016-x
20. Fayers, PM, and Sprangers, MAG. Understanding self-rated Health. Lancet. (2002) 359:187–8. doi: 10.1016/S0140-6736(02)07466-4
21. Feenstra, M, Van Munster, BC, Macneil Vroomen, JL, De Rooij, SE, and Smidt, N. Trajectories of self-rated health in an older general population and their determinants: the lifelines cohort study. BMJ Open. (2020) 10:E035012. doi: 10.1136/bmjopen-2019-035012
22. Ferraro, KF, and Kelley-Moore, JA. Self-rated health and mortality among black and white adults: examining the dynamic evaluation thesis. J Gerontol B Psychol Sci Soc Sci. (2001) 56:S195–205. doi: 10.1093/geronb/56.4.S195
23. Han, B, Phillips, C, Ferrucci, L, Bandeen-Roche, K, Jylha, M, Kasper, J, et al. Change in self-rated health and mortality among community-dwelling disabled older women. Gerontologist. (2005) 45:216–21. doi: 10.1093/geront/45.2.216
24. Miller, TR, and Wolinsky, FD. Self-rated health trajectories and mortality among older adults. J Gerontol B Psychol Sci Soc Sci. (2007) 62:S22–7. doi: 10.1093/geronb/62.1.S22
25. Lv, X, Li, W, Ma, Y, Chen, H, Zeng, Y, Yu, X, et al. Cognitive decline and mortality among community-dwelling Chinese older people. BMC Med. (2019) 17:63. doi: 10.1186/s12916-019-1295-8
26. Lv, YB, Gao, X, Yin, ZX, Chen, HS, Luo, JS, Brasher, MS, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ. (2018) 361:K2158. doi: 10.1136/bmj.k2158
27. Zeng, Y. Towards deeper research and better policy for healthy aging --using the unique data of Chinese longitudinal healthy longevity survey. China Econo J. (2012) 5:131–49. doi: 10.1080/17538963.2013.764677
28. Zeng, Y, Feng, Q, Hesketh, T, Christensen, K, and Vaupel, JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. (2017) 389:1619–29. doi: 10.1016/S0140-6736(17)30548-2
29. Benyamini, Y, and Idler, ELJROA. Community studies reporting association between self-rated health and mortality: additional studies, 1995 to 1998. Res. Aging. (1999) 21:392–401. doi: 10.1177/0164027599213002
30. Feldman, B, Shen, J, Chen, C, Shi, J, and Xiang, H. Perceived health after adult traumatic brain injury: a Group-Based Trajectory Modeling (GBTM) analysis. Brain Inj. (2020) 34:741–50. doi: 10.1080/02699052.2020.1753111
31. Nguena Nguefack, HL, Pagé, MG, Katz, J, Choinière, M, Vanasse, A, Dorais, M, et al. Trajectory modelling techniques useful to epidemiological research: a comparative narrative review of approaches. Clin Epidemiol. (2020) 12:1205–22. doi: 10.2147/CLEP.S265287
32. Larsson, D, Hemmingsson, T, Allebeck, P, and Lundberg, I. Self-rated health and mortality among young men: what is the relation and how may it be explained? Scand J Public Health. (2002) 30:259–66. doi: 10.1080/14034940210133997
33. Moreno, X, Huerta, M, and Albala, C. Global self-rated health and mortality in older people. Gac Sanit. (2014) 28:246–52. doi: 10.1016/j.gaceta.2013.07.006
34. Fan, Y, and He, D. Self-rated health, socioeconomic status and all-cause mortality in Chinese middle-aged and elderly adults. Sci Rep. (2022) 12:1–8. doi: 10.1038/s41598-022-13502-9
35. Benyamini, Y. Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychol Health. (2011) 26:1407–13. doi: 10.1080/08870446.2011.621703
36. Benyamini, Y, Idler, EL, Leventhal, H, Leventhal, EAJTJOGSBPS, and Sciences, S. Positive affect and function as influences on self-assessments of health: expanding our view beyond illness and disability. J Gerontol B Psychol Sci Soc Sci. (2000) 55:P107–16. doi: 10.1093/geronb/55.2.P107
37. Brumpton, BM, Leivseth, L, Romundstad, PR, Langhammer, A, Chen, Y, Camargo, CA Jr, et al. The joint association of anxiety, depression and obesity with incident asthma in adults: the hunt study. Int J Epidemiol. (2013) 42:1455–63. doi: 10.1093/ije/dyt151
38. Lyyra, T-M, Heikkinen, E, Lyyra, A-L, and Jylhä, M. Self-rated health and mortality: could clinical and performance-based measures of health and functioning explain the association? Arch Gerontol Geriatr. (2006) 42:277–88. doi: 10.1016/j.archger.2005.08.001
39. Dantzer, R, and Kelley, KW. Twenty years of research on cytokine-induced sickness behavior. Brain Behav Immun. (2007) 21:153–60. doi: 10.1016/j.bbi.2006.09.006
40. Allin, KH, Bojesen, SE, and Nordestgaard, BG. Baseline C-reactive protein is associated with incident cancer and survival in patients with cancer. J Clin Oncol. (2009) 27:2217–24. doi: 10.1200/JCO.2008.19.8440
41. Black, PH. Stress and the inflammatory response: a review of neurogenic inflammation. Brain Behav Immun. (2002) 16:622–53. doi: 10.1016/S0889-1591(02)00021-1
42. Roubenoff, R, Parise, H, Payette, HA, Abad, LW, D’agostino, R, Jacques, PF, et al. Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham Heart Study. Am J Med. (2003) 115:429–35. doi: 10.1016/j.amjmed.2003.05.001
43. Christian, LM, Glaser, R, Porter, K, Malarkey, WB, Beversdorf, D, and Kiecolt-Glaser, JK. Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology. (2011) 36:1495–504. doi: 10.1016/j.psyneuen.2011.04.003
44. Smith, KV, and Goldman, N. Measuring health status: self-, interviewer, and physician reports of overall health. J Aging Health. (2011) 23:242–66. doi: 10.1177/0898264310383421
45. Brissette, I, Leventhal, H, and Leventhal, EA. Observer ratings of health and sickness: can other people tell us anything about our health that we don’t already know? Health Psychol. (2003) 22:471–8. doi: 10.1037/0278-6133.22.5.471
46. Lyyra, T-M, Leskinen, E, Jylhä, M, and Heikkinen, E. Self-rated health and mortality in older men and women: a time-dependent covariate analysis. Arch Gerontol Geriatr. (2009) 48:14–8. doi: 10.1016/j.archger.2007.09.004
47. Wuorela, M, Lavonius, S, Salminen, M, Vahlberg, T, Viitanen, M, and Viikari, L. Self-rated health and objective health status as predictors of all-cause mortality among older people: a prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. (2020) 20:120. doi: 10.1186/s12877-020-01516-9
48. Gordon, EH, Peel, NM, Samanta, M, Theou, O, Howlett, SE, and Hubbard, RE. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. (2017) 89:30–40. doi: 10.1016/j.exger.2016.12.021
49. Mutz, J, Roscoe, CJ, and Lewis, CM. Exploring health in the UK Biobank: associations with sociodemographic characteristics, psychosocial factors, lifestyle and environmental exposures. BMC Med. (2021) 19:240. doi: 10.1186/s12916-021-02097-z
50. Rizzuto, D, Melis, RJ, Angleman, S, Qiu, C, and Marengoni, A. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. (2017) 65:1056–60. doi: 10.1111/jgs.14868
51. Strawbridge, WJ, and Wallhagen, MI. Self-rated health and mortality over three decades: results from a time-dependent covariate analysis. Res Aging. (1999) 21:402–16.
52. Nery Guimarães, JM, Chor, D, Werneck, GL, Carvalho, MS, Coeli, CM, Lopes, CS, et al. Association between self-rated health and mortality: 10 years follow-up to the Pró-Saúde cohort study. BMC Public Health. (2012) 12:1–10. doi: 10.1186/1471-2458-12-676
Keywords: self-rated health, interviewer-rated health, the multimorbidity-weighted index, Chinese older adults, mortality
Citation: Shan S, Cao J, Tang K, Cheng S, Ren Z, Li S, Sun W, Hou L, Yi Q, Chen D and Song P (2023) Self-rated health, interviewer-rated health, and objective health, their changes and trajectories over time, and the risk of mortality in Chinese adults. Front. Public Health. 11:1137527. doi: 10.3389/fpubh.2023.1137527
Edited by:
Angelo d’Errico, Azienda Sanitaria Locale TO3, ItalyReviewed by:
Qiong Meng, Kunming Medical University, ChinaErvin Toci, University of Medicine, Tirana, Albania
Julian Mutz, King’s College London, United Kingdom
Copyright © 2023 Shan, Cao, Tang, Cheng, Ren, Li, Sun, Hou, Yi, Chen and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dingwan Chen, Y2hlbmR3QGhtYy5lZHUuY24=; Peige Song, cGVpZ2Vzb25nQHpqdS5lZHUuY24=
 Shiyi Shan1
Shiyi Shan1 Siqing Cheng
Siqing Cheng Ziyang Ren
Ziyang Ren Qian Yi
Qian Yi Peige Song
Peige Song