- 1West China School of Nursing, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 2Center for Interdisciplinary Research on AIDS (CIRA), Yale University, New Haven, CT, United States
- 3School of Nursing, Yale University, New Haven, CT, United States
Purpose: This study aimed to explore health-related quality of life (HRQoL) and its associated factors among people living with HIV/AIDS (PLWH) in Sichuan, China.
Methods: A total of 401 PLWH were recruited from the city of Panzhihua between August 2018 and January 2019. Demographic characteristics and disease-related data were collected by self-administered questionnaires and medical system records. Health-related quality of life (HRQoL) was measured by the medical outcome study HIV health survey (MOS-HIV), which measured ten subdimensions and two summarized dimensions, the physical health summary score (PHS) and the mental health summary score (MHS). Logistic regression models were used to explore the variables independently associated with quality of life.
Results: The PHS and MHS measured by MOS-HIV were 53.66 ± 6.80 and 51.31 ± 7.66, respectively. Younger age, higher educational level, no methadone use, higher CD4 lymphocyte counts, less symptom counts and heathy BMI significantly were associated with higher HRQOL in the univariate χ2-test analysis. Education level was found to have a significant influence on patients' quality of life, both in physical health (P = 0.022) and mental health (P = 0.002) dimensions. Younger age (P = 0.032), higher CD4 lymphocyte counts (P = 0.007), less symptom counts (P < 0.001) and health BMI level (P < 0.001) were positively related to the PHS of quality of life in the multivariable logistic regression model.
Conclusion: The HRQoL of PLWH in Sinchuan Province was relatively low. Age, educational level, methadone use, CD4 lymphocyte counts, symptom counts and BMI were positively related to quality of life. This study indicates that health caregivers should pay more attention to comorbidity issues and mental health in PLWH, especially for those with lower education levels, unhealthy body mass index, more symptomatic presentation and older age.
Introduction
The human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) pandemic is a serious global challenge (1). According to the Joint United Nations Program on HIV/AIDS (UNAIDS), there were 37.7 (30.2–45.1) million people living with HIV/AIDS (PLWH), and 36.3 (27.2–47.8) million people died from AIDS-related illnesses worldwide by the end of 2021 (1). In China, there are 1.147 million people living with HIV/AIDS (2).
The government of China has implemented the “Four Free and One Care” policy since 2003 in response to the HIV/AIDS epidemic (3). It is well known that one of the “Four Free” was to provide free highly active antiretroviral therapy (HAART) for all PLWH who meet the criteria for antiviral treatment. They can obtain free antiviral medication and health counseling every 3 months at the outpatient department of the infectious disease hospital or a general hospital with an infectious disease department. Thanks to the development of clinical treatment techniques and HAART, AIDS has transformed from a fatal infectious disease to a manageable chronic illness (4). The use of HAART in PLWH has substantially decreased the morbidity and lethality caused by HIV/AIDS symptoms (5), boosted their immune system (6), and improved their health-related quality of life (HRQoL) (7). A new “beyond viral suppression” model suggested adding a “fourth 95” to the UNAIDS' 95–95–95 target to ensure that 95% of PLWH with suppression have good HRQoL (8–10).
HRQoL is a multidimensional concept that includes dimensions such as physical health, psychological health, social functioning, and perception of general health (11). It emphasizes the importance of an overall subjective feeling of wellbeing pertaining to aspects of morale, happiness and satisfaction. Changes in HRQoL, including functional status and personal perceptions, may last throughout the rest of the PLWH's life (12).
Many previous studies around the world have proven that social problems such as cultural beliefs (13), sociodemographic characteristics (14, 15), socioeconomic characteristics (15–17), presence of comorbidities (18), stage of the disease (19), psychological (20), and clinical factors (18) can affect HRQoL among PLWH. Furthermore, alcohol drinking (18), depression (21), and spiritual belief in their disease and medication can also affect the mental and physical aspects of HRQoL (20, 22). Although the HRQoL of PLWH has significantly improved after treatment with HAART (9), drug-related side effects (15), poor adherence to HAART (18), and irregular medical follow-up have impaired HRQoL (15).
Many studies (20, 23–25) have explored the determinants of HRQoL in PLWH in China and found that older age, single, unemployment, low education, living in rural areas, and low CD4+ cell count are associated with low HRQoL among PLWH in China. Sichuan Province has one of the highest incidences of HIV/AIDS in China (26). Since the first AIDS case was reported in Sichuan in 1991, the province has reported more than 110,000 surviving HIV infections/patients as of 2017 (ranking first in China), with a 0.13% survival rate (ranking fourth in China). The number of new cases in the province continues to grow, ranking first in China for five consecutive years (27). However, there was a scarcity of studies reporting the HRQoL of PLWH. In the literature, several instruments, including the Medical Outcomes Study 36-item short-form health survey (28), 12-item short-form health survey (29), Medical Outcomes Study HIV Health Survey (MOS-HIV) and World Health Organization quality of life (WHOQOL)-BREF (30), have been used to evaluate the HRQoL of PLWH, but MOS-HIV is the most widely used measurement to assess HRQoL for PLWH with well-established psychometric properties (31).
Knowing the determinants of HRQoL would enable PLWH, their families, healthcare providers and policy makers to develop relevant and holistic interventions to improve the general wellbeing and overall HRQoL of PLWH (32). In particular, HRQoL in PLWH is critical for monitoring the impact of drug therapy on disease progression (33). Thus, the aim of this study was to investigate HRQoL status and associated factors in PLWH by using the MOS-HIV.
Methods
Study design and participants
This was a cross-sectional study conducted from August 2018 to January 2019 in Panzhihua city, Sichuan Province, China. HRQoL was used as the main indicator, and the sample content was designed to be 328 with reference to the relevant literature and the mean survey formula. The required sample size was finally determined to be 410 cases because 20% of invalid questionnaires were considered. Regarding the sites for conducting the sampling, 2 districts or counties in Panzhihua were randomly selected to conduct the survey. Finally, Renhe District and Miyi County were chosen. The researcher inquired about the number of PLWH in different districts or counties of Panzhihua City in that year to calculate the relative proportion to determine the sample size assigned to the two sites. And the convenient sampling sites were selected as the Fourth People's Hospital of Renhe District and the People's Hospital of Miyi County in Panzhihua City, respectively, both of which were designated as PLWH getting free medications, testing and consulting. Participants were recruited through convenience sampling. The inclusion criteria of participants were (1) HIV seropositivity, (2) age older than 17 years, (3) willing to fill out the study questionnaire. People with mental illness or cognitive impairment were excluded.
Ethical considerations
The study was approved by the West China Hospital Medical Ethics Committee (study ID#: 20170430). The objectives and procedures of the study were verbally explained to participants. Before the study, participants signed written informed consent.
Data collection
All data were collected through paper questionnaires. First, the investigators received training about the administration of the questionnaires. Second, all participants were informed of the purpose, content and potential risks of the study before the investigation. Participants independently completed the anonymous questionnaires. If the participants had difficulty understanding or reading the questionnaire, the investigators explained it in detail and recorded the answer if inquired. After the questionnaire was completed by participants recruited by the local CDC, the investigators immediately completed the questionnaire in person to verify whether the respondent had answered all the questions. If the patient refused to answer and the incomplete part of the questionnaire was >20%, the questionnaire was discarded. Each participant was paid ¥50 (equivalent to $7) as compensation for transportation.
Measurements
Sociodemographic characteristics
Sociodemographic characteristics included sex, age, ethnicity, educational level, marital status, religion, sexual orientation, religious beliefs, occupation, alcohol consumption, residence, smoking habits, drinking habits, BMI and per capita monthly household income. In this study, age was divided into three groups: young adults aged 18–45 years, middle-aged adults aged 45–60 years and elderly adults aged 65 years and above. Participants were classified into 4 categories according to the weight determination criteria for Chinese adults published by the National Health and Wellness Commission Participations, which were underweight (<18.5), healthy weight (18.5–24.9), overweight (25–27.9), and obese (≥28).
Disease-related characteristics
We chose methadone use, infection route, disclosure status, CD4 cell count, symptom counts, duration since HIV diagnosis, duration of treatment, viral load and the 30 most common symptoms for now according to the literature review and clinical experience. Years since HIV diagnosis, duration of treatment, CD4 cell count and viral load from database and clinic records. Disclosure status, infection route, and symptoms were obtained through patient self-reporting. If there were missing data in the database or clinic records, the investigator asked the patient for relevant information.
Health-related quality of life
HRQoL was assessed by the Medical Outcomes Study HIV Survey (MOS-HIV), which is a brief, comprehensive measure of health-related quality of life used extensively in HIV/AIDS (33). It consists of 35 items and measures 10 dimensions, including general health, physical function, role function, social function, cognitive function, pain, mental health, energy/fatigue, health distress, and quality of life. Of these 10 domains, 8 were multi-item and 2 (Social Function and Quality of Life) consisted of a single item. Ten subdimension scores and two summary dimensions (physical health summary score, PHS and mental health summary score, MHS) were obtained by adding the raw item scores of the respective scales and then transforming them into a 0–100 scale, with higher scores indicating better functioning and wellbeing. The simplified Chinese version of the MOS-HIV questionnaire has been reported to have good validity and reliability (34, 35). The Cronbach's α of the PHS and MHS scales was 0.87 and 0.89, respectively. The Cronbach's α for individual dimensions was >0.70 (34).
Statistical analyses
Data were inputted by two researchers through EpiData 3.1, and all statistical analyses were performed using SPSS 24.0. A P-value of <0.05 was considered statistically significant. Descriptive statistics analysis was performed by mean ± standard deviation (SD) and median, interquartile range (IQR), frequency, and constituent ratio, as appropriate. We divided PHS and MHS scores into dichotomous variables by 50, in which scores above or below 50 can be considered better or worse HRQoL (36). Univariate analysis χ2-test for categorical data and Spearman's correlation for continuous data were performed to examine the quality of life of PLWH with different demographic characteristics and disease-related characteristics. Intragroup comparisons for multiple categorical variables were also performed by Fisher's exact test. Binary logistic regression analysis was conducted to explore factors associated with HRQoL in PLWH. Because there is no universal consensus in choosing predictor variables in a multivariable logistic regression analysis, we included all the variables with P ≤ 0.2 in the univariate analysis and all clinically significant variables regardless of their P-values, based on the literature evidence. The Hosmer–Lemeshow goodness-of-fit statistic with a P-value > 0.05 was considered a well-fitting regression model, and the percentage of the variability predicted by the model was explained by the Nagelkerke R2.
Results
Sociodemographic and disease-related characteristics of participants
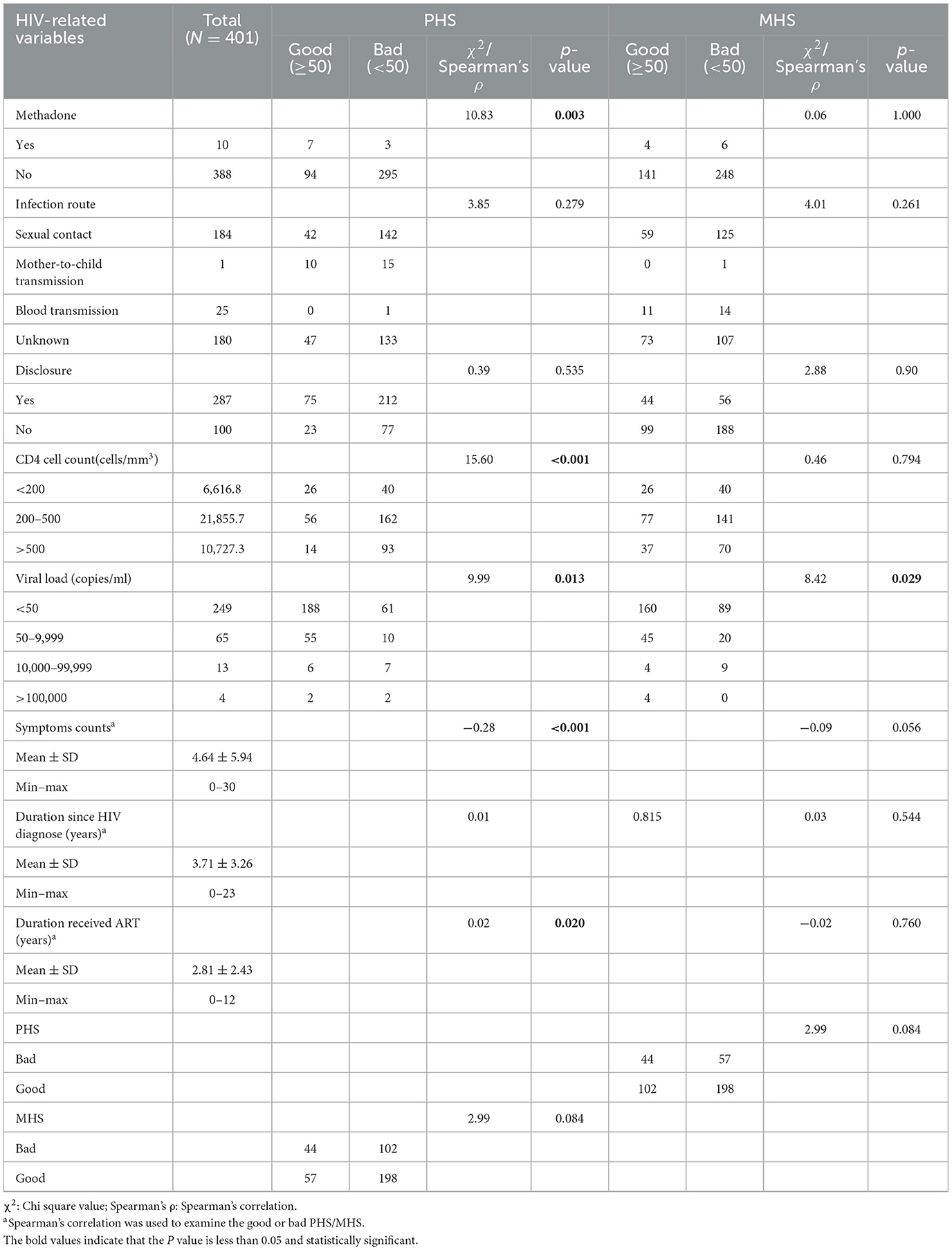
Finally, 410 participants were enrolled in the study. However, A total of 9 questionnaires with missing values >20% were excluded, and the final number of valid questionnaires collected was 401. Among the participants, 64.7% (n = 258) were male and 35.2% (n = 141) were female. Their mean (SD) age was 50.02 (15.06) years. Most participants were of Han ethnicity (n = 340, 85.4%), married (n = 227, 58.2%), and employed (n = 304, 76.9%). Nearly half of the participants were living in rural areas (n = 209, 53.3%). The sociodemographic characteristics of the participants and the HRQoL in different groups are presented in Table 1.
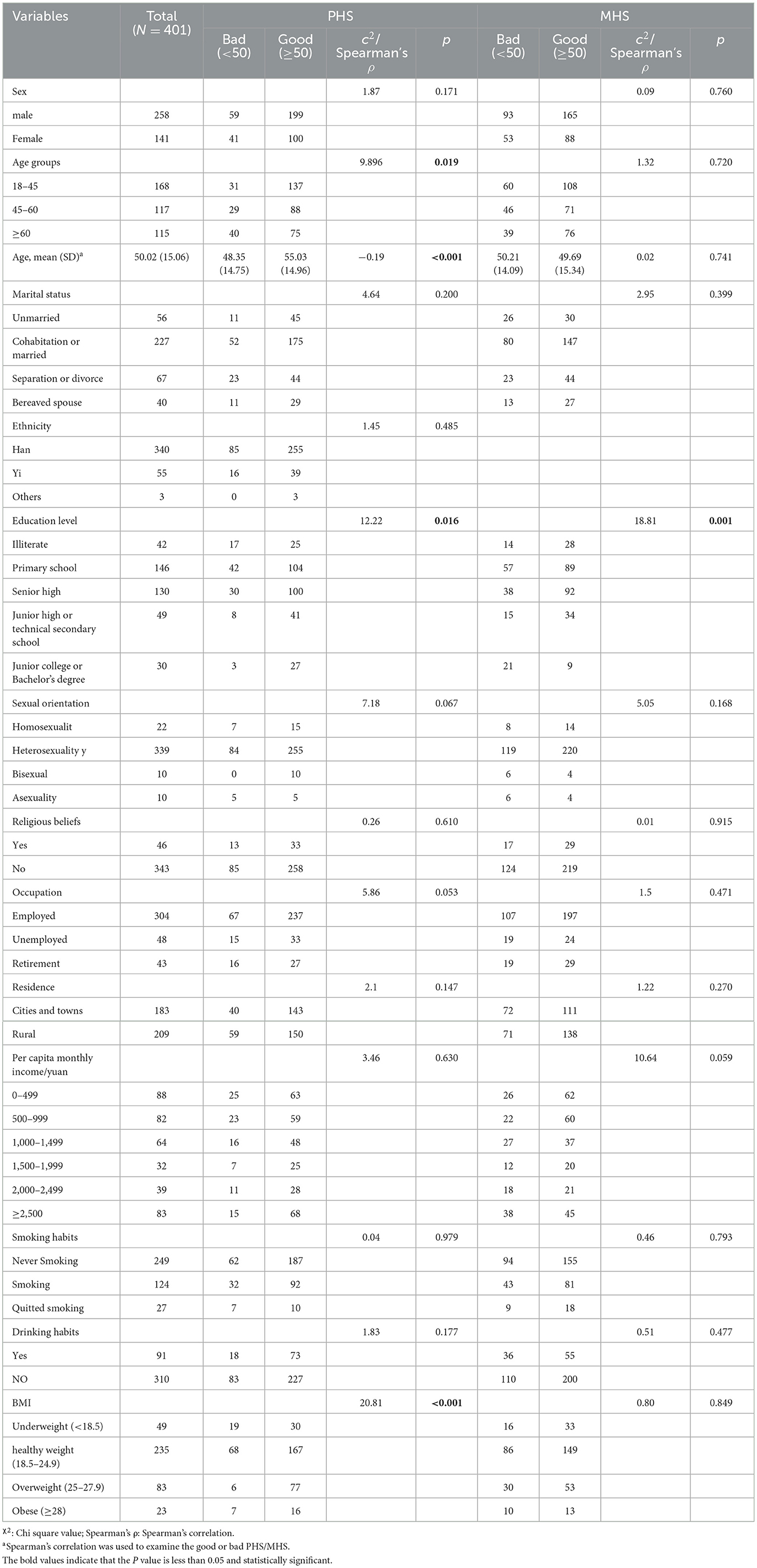
Table 1. The socio-demographic of total samples, good or bad PHS/MHS groups of people living with HIV/AIDS (PLWH) (N = 401).
HIV-related variables
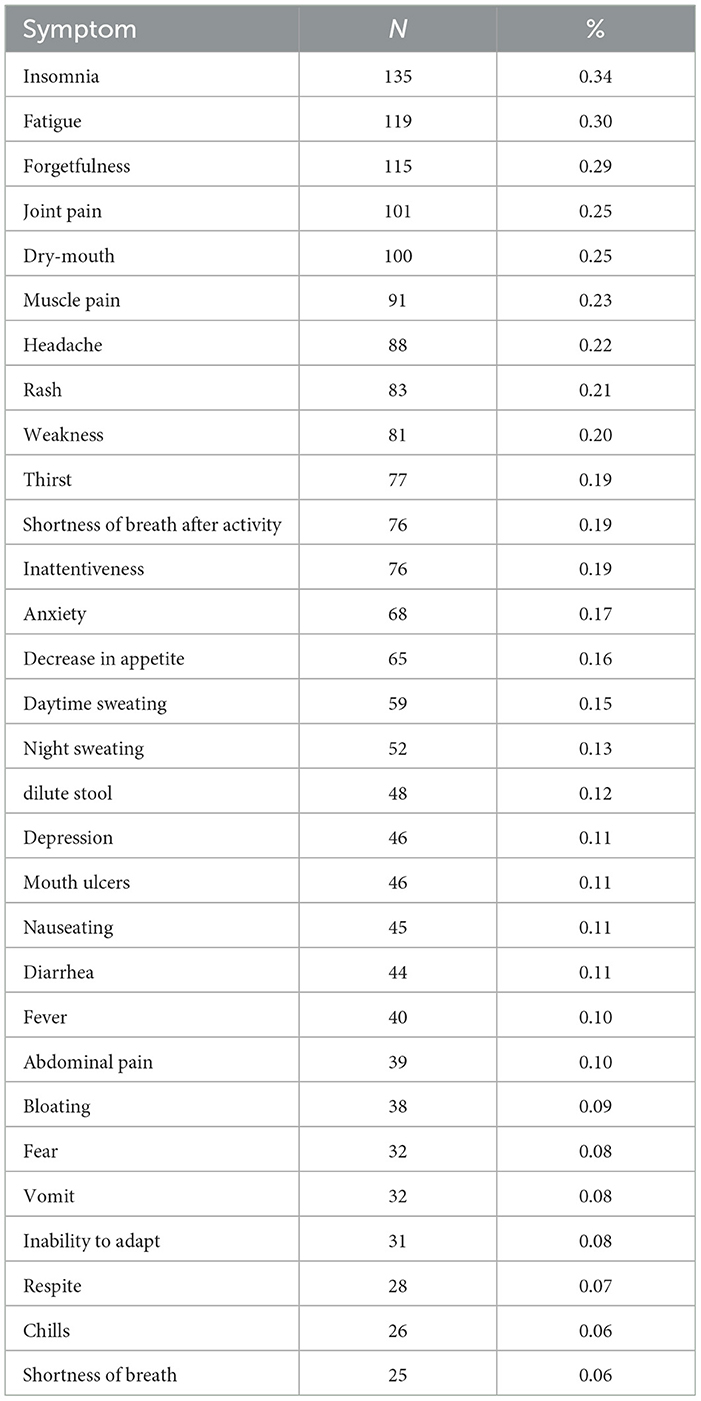
The mean duration after being diagnosed with HIV was 3.7 (SD = 3.3) years, ranging from 1 month to 30 years. All participants received ART with an average duration of 2.8 (SD = 2.4) years. Most of the participants' (n = 284, 72.6%) immune systems were weakened by HIV, while more than half of the patients had viral suppression (n = 249, 75.2%) and disclosed the HIV-infected condition (n = 287, 74.1%). The most common form of infection was sexual contact (n = 184, 47.1%). Most participants reported that they had more than one symptom, and only 14.5% (n = 58) of people indicated that they were not bothered by HIV-related symptoms (Table 2).
Symptoms
The majority of participants suffered fewer than 10 symptoms (Table 2). The top 5 symptoms reported by patients were insomnia (32.90%), fatigue (29.00%), forgetfulness (28.10%), joint pain (24.60%) and dry mouth (24.40%). Most participants' symptoms were light (Table 3). The least reported symptom was mouth ulcers. We found that anxiety and depression were not the most frequent symptoms among PLWH. In this study, the number of patients who reported having symptoms of anxiety and depression was 68 (16.6%) and 46 (11.3%), respectively.
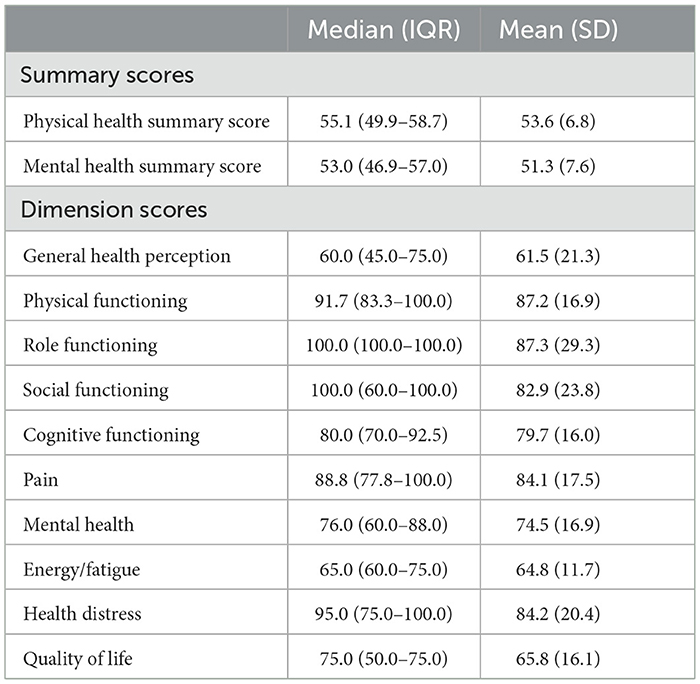
HRQoL of participants
The Cronbach's α coefficient for the MOS-HIV in this study was 0.659. According to the questionnaire, the HRQoL of the participants in terms of PHS, MHS and 10-dimensional scores are presented in Table 4. The mean physical health summary (PHS) and mental health summary (MHS) scores were 53.66 (6.81) and 51.31 (7.66), respectively, and there were 300 (74.8%) participants with good PHS and 255 (63.6%) participants with good MHS based on the standardized mean score of 50 (36). Of the 10 dimensions, the highest mean was found in the role functioning dimension (87.39 ± 29.37), while the lowest mean was found in the general health perceptions subscale (61.51 ± 21.37). There was no significant correlation between PHS and MHS (Spearman's correlation = 0.20; P = 0.017) and no significant correlation between PHS and MHS rank material, which was divided by 50 to be considered a good or poor health situation (Pearson chi-square = 2.99, P = 0.084).
Factors associated with HRQoL
In the univariate analysis (Tables 1, 2), the PHS was significantly higher in participants who were younger (p = 0.036), had better education (p = 0.005), had fewer symptoms of HIV (p < 0.001), had a CD4 level >500cells/mm3 (p = 0.004), had a viral load <10,000 copies/ml, did not use methadone (p = 0.001) and had a BMI between 18.5 and 27.9 (p < 0.001). Significantly higher MHS scores were reported by people with higher education levels (p = 0.001) and fewer symptoms. However, there was no correlation between disclosure, sex, sexual orientation and HRQoL score.
The association of the predictor variables with the PHS and MHS categories were explored using multivariate analysis and multivariable logistic regression analyses and are presented in Table 5.
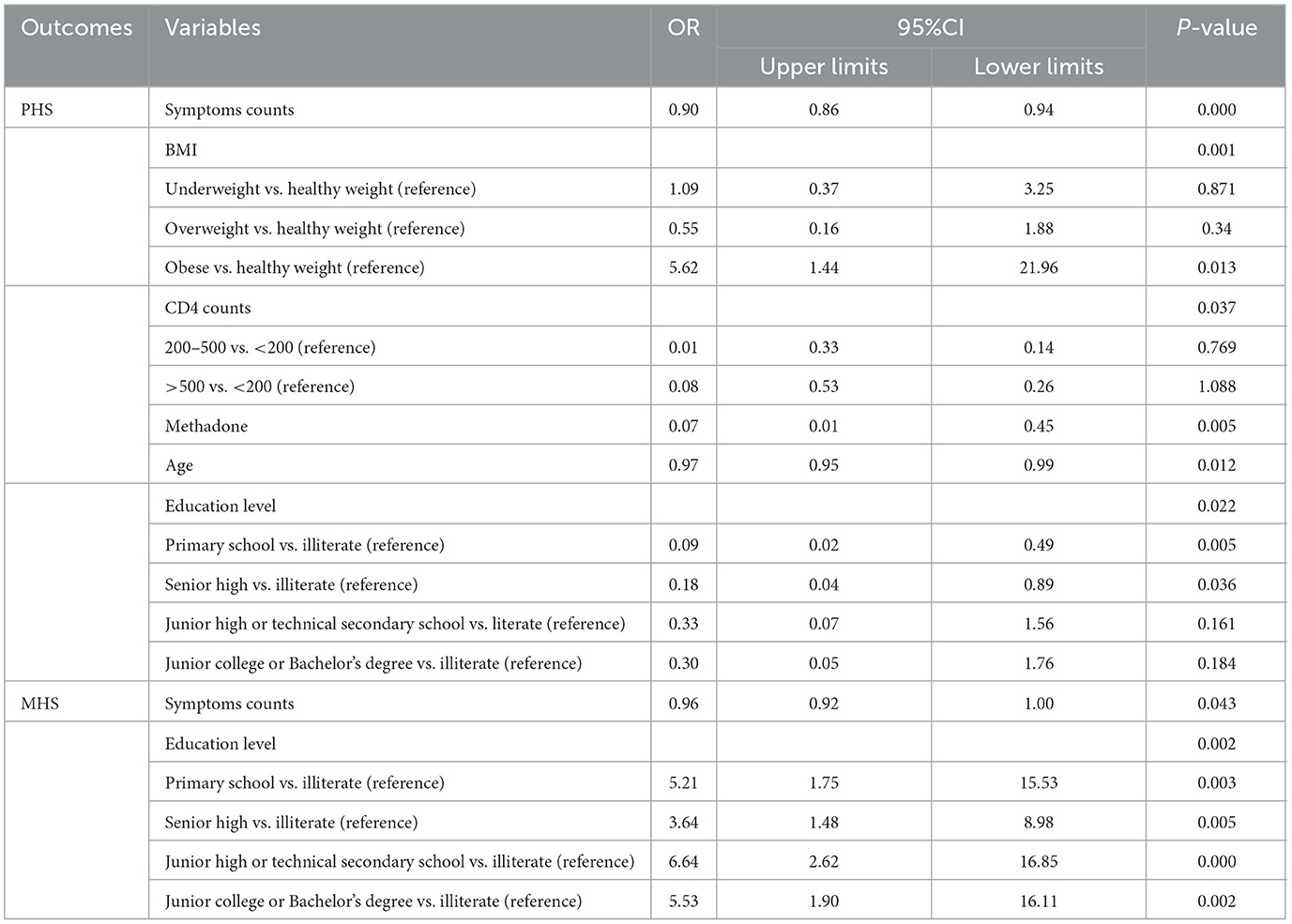
Table 5. Factors associated with health-related quality of life in the multivariable logistic regression (N = 401).
Only educational level and symptom counts were both significant in PHS and MHS in the univariable analysis and multivariable logistic regression analyses. However, there was no significant correlation between PHS and MHS by Spearman's correlation or χ2-test. Youth population, higher education, health BMI level, CD4 level ≥500 cells/mm3, fewer symptoms, not using methadone and shorter time receiving ART were associated with good PHS in the univariable analysis, whereas only education level and symptom counts were associated with MHS. Some variables significantly associated with PHS and MHS in the univariate analyses were not significant in the multivariable models (Table 4). The Hosmer–Lemeshow goodness-offit test p-values were 0.628 and 1 for the PHS and MHS models constructed, respectively, suggestive of well-fitting models. It is assumed that 33.2% of the variability in the PHS (Nagelkerke R2 = 0.33) and 7% of the variability in the MHS (Nagelkerke R2 = 0.07) is explained by these models.
Discussion
The results of the study showed that the total physical health score (PHS) and mental health score (MHS) of HIV/AIDS in Sichuan Province were 53.6 ± 6.8 and 51.3 ± 7.7, which were higher than those in previous studies surveyed in other areas of China (37–40). The reason may be that some time has passed since the previous studies were conducted. The impact of this illness on their quality of life is substantially lower than a few years ago because of the significant improvement in mortality and morbidity in PLWH with the implementation of ART (21). With the implementation of the “Four Free and One Care” policy, PLWH do not need to pay for medications, testing and counseling, can even obtain relief money from the government. Antiviral treatment and the four-free care policy help PLWH in poor areas of China receive better treatment, which helps to control disease and improve their quality of life.
The dimensions that scored higher were role function, physical function and health distress, which is similar to other studies (21, 41, 42). This is probably because HIV/AIDS can be controlled like any other chronic disease with the implementation of ART (41). The rate of severe illness decreased, and patients did not suffer significant impairment in physical or social functioning. The participants reported lower scores in the quality of life, energy/fatigue and general health perception dimensions, consistent with the results of previous studies (21, 41, 43). The lowest mean score was 61.52 for general health perception. The highest score in the energy/fatigue dimension is 95, and only in this dimension did no patient report a full score, 100. This result indicated that HIV-infected peoples' quality of life was still impaired and that each participant's energy was affected to varying degrees. Fatigue is the second most common symptom, with a 29% reporting rate. The causes of fatigue are complex. The disease itself, comorbidities, drug effects and even psychological factors may cause fatigue (41, 44, 45). We suggest that fatigue management and self-perception of health promotion are areas that need further attention for researchers.
The study revealed that education level was significantly associated with both the PHS and MHS of PLWH. The vast majority (80.1%) of participants in our study had only received a junior high school education or less. A further 10.5% were illiterate. Consistent with the findings of previous studies (42, 46, 47), educational level was a protective factor of HRQoL. Moreover, having no formal education is a barrier to accessing health services and increasing PLWH vulnerability (48). This result was also confirmed in this study, even if PLWH with primary education had a much lower risk of low quality of life than illiterate PLWH. The impact of education level on PLWH is multifaceted. It plays an important role in the spread and prevalence of HIV (49) and is more likely to lead to risky sexual behavior (50). Well-educated PLWH were more likely to show good knowledge, positive attitudes toward HIV/AIDS (48) and good social support (47) and cognitive level (42, 46), which leads to better self-management and health outcomes. Although education level is difficult to change, we recommend that more health information and education be provided through brochures, bulletin boards, and public online platforms. More tailored patient education should be conducted during the patient's hospitalization and at follow-up visits.
Symptoms of HIV have also been reported to be associated with HRQoL in many previous studies (22, 32, 51, 52), and more serious complications can lead to poor quality of life. In our study, we found that the number of symptoms was a risk factor for HRQoL, both in PHS and MHS. The most common symptoms reported by the participants in our study were sleep disturbances, fatigue, forgetfulness, joint pain and dry mouth. Sleep disturbances, fatigue, and forgetfulness have received extensive attention in previous studies (35, 53, 54). There are many factors that influence the symptoms, including the impact of AIDS on the immune system (53, 54), the adverse effects of medication (35, 55, 56) and psychosocial factors (45, 55, 57). Many studies have revealed that joint pain (58–62) and xerostomia are also common symptoms in PLWH (63, 64). In a cross-sectional survey of 195 PLWH conducted in Brazil, 40% of patients reported dry mouth symptoms (63). In a cross-sectional survey of 312 PLWH conducted in Italy, 34% reported joint pain (65). They have all been shown to have a negative impact on the QOL of PLWH (63, 65, 66). Possible causes are joint pain and salivary gland hypofunction due to ART (59, 64, 67). It has also been suggested that joint pain may be related to inflammatory responses mediated by inflammatory factors, but the exact mechanisms need to be further elucidated (68). This suggests that we need to include a full range of physical, psychological, and social care in future studies to reduce the impact of symptoms on the quality of life of PLWH and implement proven effective interventions in health services. Meanwhile, PLWH's joint pain and dry mouth need more attention by researchers and medical services team members.
Age was an independent risk factor that was significantly associated with the physical health of PLWH, which was similar to other studies (69, 70) but different from George's research (21). It may be that older PLWH experience a greater burden of age-related comorbidities, poorer social determinants of health and even ageism (71). Murzin's team (71) showed that ageism transcended multiple interactions and environments from dating to healthcare and community services to society because of social determinants, health provider issues and structural challenges. Therefore, we suggest that the government should pay more attention to older people, especially in the advent of an aging society.
This study showed a significant relationship between HRQoL PHS and CD4 lymphocyte counts. As CD4 lymphocyte counts increased, physical HRQoL improved. The findings were consistent with the results of other studies (31, 72, 73). A few studies have reported that lower CD4 counts may affect physical health (74–76). CD4+ cell count is an indicator of clinical progression and can reflect the impact of therapeutic efforts. Because of the “Four Frees and One Care” Policy, all HIV/AIDS patients in China can receive free ART in China. However, a relatively low CD4+ cell count of participants was also found in our study. This suggests that strategies to enhance medication adherence may be needed.
BMI is considered to be an important factor associated with patients' quality of life. In our study, both malnutrition and obesity may have contributed to the impairment of physical health. This is consistent with previous studies (77, 78), and some studies showed that obesity or malnutrition affects adult PLWH muscle strength (79) and the risk of frailty (80, 81) and comorbidities in PLWH followed up for 12 years (78). Even, BMI can be a predictor tool for death risk in Ethiopian adults living with HIV on ART (82). However, it is noteworthy that the PHS scores of the overweight group were the highest, even exceeding the healthy BMI level. Obesity may be due to a lack of physical activity and poor lifestyle (21), while underweight may be associated with disease consumption (77). We need more research to reveal whether the burden of being overweight will or will not affect patients' psychosocial functioning and how it could happen.
In addition, only 75.2% of participants in this study achieved viral suppression, which is much lower than the 92.4% in Beijing (78) but close to the figure for Liangshan, Sichuan (79). This may be attributed to the relatively short duration of HIV diagnosis and antiretroviral treatment in most of our participates. In addition, the comparison of data from two districts in China also illustrates the large differences in treatment effectiveness between regions. In particular, there is the largest base of HIV-infected patients in Sichuan Province. To achieve the “95 95 95” targets, there is a greater need for more targeted programs in less economically developed regions to explore critical influencing factors and efficient management interventions. Rationalize the allocation of limited resources to the whole process of HIV/AIDS management.
Although some studies have shown that women with HIV/AIDS have a higher quality of life than men (80, 81), we did not find any differences in quality of life between male and female HIV/AIDS patients. The difference might be due to the study population, sampling method, and measurement tools used to assess HRQoL among studies. A cross-sectional study of sex differences in quality of life among PLWH found that total physical health scores and mental health scores among PLWH were not statistically significant by sex (82).
Disclosure of HIV infection in this study was 71.6%, higher than other studies (21, 83). The majority of participants chose to disclose to their spouses (58.9%) and children (46.7%), and a small proportion disclosed the disease to parents (19.6%) and friends (7.4%). This may be one of the reasons why the MHS score in this study was higher than that in other studies.
One thing that should not be overlooked in our study is that PLWH explain only 7% of the PHS, and only two factors are included in the final multivariate regression. The reason may be that the sample was a general adult PLWH population with higher psychological scores than those reported in other literature (84, 85), and fewer people reported anxiety (17%) and depression (11%) among the symptom questionnaires, which indicates a relatively high level of mental health in this study sample. Second, nearly half of the PLWH in this sample had received only primary education and below, and their cognitive level of mental health might not be sufficient (86). Last, previous studies have shown that disclosure, sexual orientation and other factors have a significant impact on the mental health of PLWH (87), the level of disclosure in this sample population is higher than that in previous studies (21, 83), and the sexual orientation is mostly heterosexual. It would be easier to tap into special populations such as men who have sex with men (MSM), sexual service providers or adolescent groups to identify the relevant influencing factors.
There were limitations in our study that should be acknowledged. First, it is a population with a relatively recent history of antiretroviral treatment but with many symptoms that seem more related to treatments used in the past. However, the type of treatment and regimens used are not available. We were unable to analyze whether the patient-reported symptom presentation was related. Second, the study was conducted in a single city in Sichuan. Future studies need to be conducted in other Sichuan provinces and even nationwide to verify whether there are differences in PLWH quality of life across geographic areas. Third, we could not determine the exact causality between HRQoL and the related factors due to the cross-sectional design. Therefore, there is a need for longitudinal research and multicenter studies to confirm our findings and explore their causality.
Conclusion
In conclusion, the HRQoL of PLWH in Panzhihua improved compared to previous studies. Alleviating symptoms of HIV and preventing comorbidities, especially insomnia and fatigue, are important for patient life treatment. We recommend that further research should be conducted to explore factors affecting quality of life so that we can develop more comprehensive interventions to prevent HIV/AIDS. Moreover, more care and support should be given to patients, especially for those with lower educational attainment, unhealthy body mass index, more symptomatic presentation and older age.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Sichuan University Medical Ethics Committee. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HZ: writing manuscripts and data processing. FW: data entry and writing manuscript. YS, ZN, and HC: draft touch-ups and guidance on writing. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by Sichuan Province Provincial Financial Subsidy Major Diseases Prevention and Control Project [Sichuan Health Office (2017) No.70; PI: HC] and Science & Technology Department of Sichuan Province Program (2023YFS0045).
Acknowledgments
The authors thank the Panzhihua Center for Disease Control and Prevention (CDC) for helping with the collection of clinical data and all the participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. AIDSinfo|UNAIDS. Global Data on HIV Epidemiology and Response. Geneva: WHO (2022). Available online at: https://aidsinfo.unaids.org/ (accessed November 9, 2022).
2. Gan X, Zhao D, Zhao Y, Ma Y, Wu Y, Dou Z. Progress on national antiretroviral treatment program during 2003–2021 in China. Chin J AIDS STD. (2022) 21:642–6. doi: 10.13419/j.cnki.aids.2022.06.04
3. The State Council of the People's Republic of China. Regulation on the Prevention and Treatment of HIV/AIDS. Decree of the State Council of the People's Republic of China No 457. Beijing: The State Council of the People's Republic of China (2006). Available online at: http://www.gov.cn/node_12372/content_456866.htm (accessed December 1, 2022).
4. Kanters S, Vitoria M, Doherty M, Socias ME, Ford N, Forrest JI, et al. Comparative efficacy and safety of first-line antiretroviral therapy for the treatment of HIV infection: a systematic review and network meta-analysis. Lancet HIV. (2016) 3:e510–20. doi: 10.1016/S2352-3018(16)30091-1
5. Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med. (1998) 338:853–60. doi: 10.1056/NEJM199803263381301
6. Ofotokun I, Titanji K, Vunnava A, Roser-Page S, Vikulina T, Villinger F, et al. Antiretroviral therapy induces a rapid increase in bone resorption that is positively associated with the magnitude of immune reconstitution in HIV infection. AIDS. (2016) 30:405–14. doi: 10.1097/QAD.0000000000000918
7. Castro R, De Boni RB, Luz PM, Velasque L, Lopes LV, Medina-Lara A, et al. Health-related quality of life assessment among people living with HIV in Rio de Janeiro, Brazil: a cross-sectional study. Qual Life Res Int J Qual Life Aspects Treatment Care Rehabil. (2019) 28:1035–45. doi: 10.1007/s11136-018-2044-8
8. Frescura L, Godfrey-Faussett P, Feizzadeh AA, El-Sadr W, Syarif O, Ghys PD. Achieving the 95 95 95 targets for all: a pathway to ending AIDS. PLoS ONE. (2022) 17:e0272405. doi: 10.1371/journal.pone.0272405
9. Lazarus JV, Safreed-Harmon K, Barton SE, Costagliola D, Dedes N, Del Amo Valero J, et al. Beyond viral suppression of HIV: the new quality of life frontier. BMC Med. (2016) 14:94. doi: 10.1186/s12916-016-0640-4
10. Cho H, Jiang Y, Li X, Deming M. The relationship between self-reported viral load suppression and quality of life among people living with HIV in South Carolina. AIDS Care. (2020) 32:1198–205. doi: 10.1080/09540121.2019.1698706
11. Ashing-Giwa KT. The contextual model of HRQoL: a paradigm for expanding the HRQoL framework. Qual Life Res. (2005) 14:297–307. doi: 10.1007/s11136-004-0729-7
12. Cardona-Arias J, Peláez-Vanegas L, López-Saldarriaga J, Duque-Molina M, Leal-Álvarez O. Health related quality of life in adults with HIV/AIDS in Colombia. Biomedica. (2011) 31:532–44. doi: 10.7705/biomedica.v31i4.422
13. da Costa TL, de Oliveira DC, Gomes AM, Formozo GA. Quality of life and people living with AIDS: relationship with sociodemographic and health aspects. Rev Lat Am Enfermagem. (2014) 22:582–90. doi: 10.1590/0104-1169.3350.2455
14. Tran BX, Nguyen LT, Do CD, Nguyen QL, Maher RM. Associations between alcohol use disorders and adherence to antiretroviral treatment and quality of life amongst people living with HIV/AIDS. BMC Public Health. (2014) 14:27. doi: 10.1186/1471-2458-14-27
15. Campsmith ML, Nakashima AK, Davidson AJ. Self-reported health-related quality of life in persons with HIV infection: results from a multi-site interview project. Health Qual Life Outcomes. (2003) 1:12. doi: 10.1186/1477-7525-1-12
16. Rourke SB, Bekele T, Tucker R, Greene S, Sobota M, Koornstra J, et al. Housing characteristics and their influence on health-related quality of life in persons living with HIV in Ontario, Canada: results from the positive spaces, healthy places study. AIDS Behav. (2012) 16:2361–73. doi: 10.1007/s10461-012-0284-0
17. Imam MH, Karim MR, Ferdous C, Akhter S. Health related quality of life among the people living with HIV. Bangl Med Res Counc Bull. (2011) 37:1–6. doi: 10.3329/bmrcb.v37i1.7791
18. Miners A, Phillips A, Kreif N, Rodger A, Speakman A, Fisher M, et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV. (2014) 1:e32–40. doi: 10.1016/S2352-3018(14)70018-9
19. Nojomi M, Anbary K, Ranjbar M. Health-related quality of life in patients with HIV/AIDS. Arch Iran Med. (2008) 11:608–12.
20. Sun W, Wu M, Qu P, Lu C, Wang L. Quality of life of people living with HIV/AIDS under the new epidemic characteristics in China and the associated factors. PLoS ONE. (2013) 8:e64562. doi: 10.1371/journal.pone.0064562
21. George S, Bergin C, Clarke S, Courtney G, Codd MB. Health-related quality of life and associated factors in people with HIV: an Irish cohort study. Health Qual Life Outcomes. (2016) 14:115. doi: 10.1186/s12955-016-0517-4
22. Briongos-Figuero LS, Bachiller-Luque P, Palacios-Martan T, De Luis-Romcn D, Eiros-Bouza JM. Depression and health related quality of life among HIV-infected people. Eur Rev Med Pharmacol Sci. (2011) 15:855–62.
23. Ming Z, Prybylski D, Cheng F, Airawanwat R, Zhu Q, Liu W, et al. Two-year prospective cohort study on quality of life outcomes among people living with HIV after initiation of antiretroviral therapy in Guangxi, China. J Assoc Nurses AIDS Care. (2014) 25:603–13. doi: 10.1016/j.jana.2014.04.003
24. Hou WL, Chen CE, Liu HY, Lai YY, Lee HC, Lee NY, et al. Mediating effects of social support on depression and quality of life among patients with HIV infection in Taiwan. AIDS Care. (2014) 26:996–1003. doi: 10.1080/09540121.2013.873764
25. Wang H, Zhou J, Huang L, Li X, Fennie KP, Williams AB. Effects of nurse-delivered home visits combined with telephone calls on medication adherence and quality of life in HIV-infected heroin users in Hunan of China. J Clin Nurs. (2010) 19:380–8. doi: 10.1111/j.1365-2702.2009.03048.x
26. Wang ZW, Liu HJ, Ying W. Spatial distribution and clustering characteristics of AIDS epidemic in China, 2005–2017. Chin J Public Health. (2019) 35:1593–7. doi: 10.11847/zgggws1124457
27. Feng L, Xie R-X, Zhang L, Li Y, Yang Y, Zhao L, et al. Win the battle of AIDS prevention and rally to set sail again: measures and achievements of HIV/AIDS prevention in Sichuan Province. Mod Prevent Med. (2022) 49:3649–54. doi: 10.20043/j.cnki.MPM.202209900
28. Ware JE. SF-36 health survey update. Spine. (2000) 25:3130–9. doi: 10.1097/00007632-200012150-00008
30. The World Health Organization. WHOQOL: Files. WHOQOL: Measuring Quality of Life. Geneva: WHO (2004). Available online at: https://www.who.int/tools/whoqol/whoqol-bref (accessed November 9, 2022).
31. Cooper V, Clatworthy J, Harding R, Whetham J. Measuring quality of life among people living with HIV: a systematic review of reviews. Health Qual Life Outcomes. (2017) 15:220. doi: 10.1186/s12955-017-0778-6
32. Degroote S, Vogelaers D, Vandijck DM. What determines health-related quality of life among people living with HIV: an updated review of the literature. Arch Public Health. (2014) 72:40. doi: 10.1186/2049-3258-72-40
33. Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the medical outcomes study HIV health survey (MOS-HIV). Qual Life Res Int J Qual Life Aspects Treatment Care Rehabil. (1997) 6:481–93.
34. Liu J, Zhu Y, Qu B. Reliability and validity of the Chinese version of the medical outcomes study HIV health survey (MOS-HIV) in people living with HIV/AIDS (PLWHA) in China. PLoS ONE. (2018) 13:e0201177. doi: 10.1371/journal.pone.0201177
35. Huang Y, Luo D, Chen X, Zhang D, Huang Z, Xiao S. Role of psychosocial status in predicting health-related quality of life at 1-year follow-up among newly diagnosed people living with HIV. PLoS ONE. (2019) 14:e0224322. doi: 10.1371/journal.pone.0224322
36. Shahriar J, Delate T, Hays RD, Coons SJ. Commentary on using the SF-36 or MOS-HIV in studies of persons with HIV disease. Health Qual Life Outcomes. (2003) 1:25. doi: 10.1186/1477-7525-1-25
37. Wu LP, Liu LF, Hu JL. Investigation on quality of life among HIV infection/AIDS patients in Huai an City and analysis on influencing factors. Occup Health. (2014) 30:2412–5. doi: 10.13329/j.cnki.zyyjk.2014.17.075
38. Xie F, Zheng H, Huang L, Yuan Z, Lu Y. Social capital associated with quality of life among people living with HIV/AIDS in Nanchang, China. Int J Environ Res Public Health. (2019) 16:276. doi: 10.3390/ijerph16020276
39. Lan GL, Yuan ZK, Clements-Nolle KD, Cook A, Yuan LL, Xu QY, et al. Social capital and quality of life among people living with HIV/AIDS in Southeast China. Asia Pac J Public Health. (2016) 28:325–35. doi: 10.1177/1010539516641490
40. Ke£ ZX. Quality of life and its influencing factors among people living with HIV/AIDS in Hangzhou City. Prev Med. (2022) 34:27–32.
41. Michel M, Wahl A, Anders M, Alqahtani SA, Kremer WM, Galle PR, et al. Significant liver fibrosis is a predictor of poor health-related quality of life in people living with HIV. Qual Life Res. (2022) 32:401–11. doi: 10.1007/s11136-022-03232-w
42. Aurpibul L, Sripan P, Tangmunkongvorakul A, Chaikan W, Sarachai S, Srithanaviboonchai K. Neurocognitive performance and quality of life of older adults with HIV on antiretroviral treatment in Northern Thailand. J Int AIDS Soc. (2022) 25:e25983. doi: 10.1002/jia2.25983
43. Ion A, Cai W, Elston D, Pullenayegum E, Smaill F, Smieja M, et al. comparison of the MOS-HIV and SF-12v2 for measuring health-related quality of life of men and women living with HIV/AIDS. AIDS Res Ther. (2011) 8:5. doi: 10.1186/1742-6405-8-5
44. Ter Haar AM, der Vlist MMN, Van den Hof M, Nijhof SL, van Litsenburg RRL, Oostrom KJ, et al. Fatigue in children and adolescents perinatally infected with human immunodeficiency virus: an observational study. BMC Pediatr. (2021) 21:519. doi: 10.1186/s12887-021-02977-6
45. Voss JG, Barroso J, Wang T, A. critical review of symptom management nursing science on HIV-related fatigue and sleep disturbance. Int J Environ Res Public Health. (2021) 18:10685. doi: 10.3390/ijerph182010685
46. Zenebe Y, Necho M, Yimam W, Akele B. Worldwide occurrence of HIV-associated neurocognitive disorders and its associated factors: a systematic review and meta-analysis. Front Psychiatry. (2022) 13:814362. doi: 10.3389/fpsyt.2022.814362
47. Mutabazi-Mwesigire D, Katamba A, Martin F, Seeley J, Wu AW. Factors that affect quality of life among people living with HIV attending an urban clinic in Uganda: a cohort study. PLoS ONE. (2015) 10:e0126810. doi: 10.1371/journal.pone.0126810
48. Virdausi FD, Efendi F, Kusumaningrum T, Adnani QES, McKenna L, Ramadhan K, et al. Socio-economic and demographic factors associated with knowledge and attitude of HIV/AIDS among women aged 15–49 years old in Indonesia. Healthcare. (2022) 10:1545. doi: 10.3390/healthcare10081545
49. Azevedo WS, Santos EPD, Pedreira NP, Dantas LB, Nascimento VGC, Dias GAR, et al. Prevalence and vulnerability factors associated with HIV and syphilis in older people from subnormal agglomerate, Brazilian Amazon. Trop Med Infect Dis. (2022) 7:332. doi: 10.3390/tropicalmed7110332
50. Diress G, Adane S, Linger M, Merchaw A, Mengist B. Individual and community-level determinates of risky sexual behaviors among sexually active unmarried men: a multilevel analysis of 2016 Ethiopian demographic and health survey. PLoS ONE. (2022) 17:83. doi: 10.1371/journal.pone.0270083
51. Surah S, Adams R, Townsend L, Reynolds I, Kinahan JC, Keating S, et al. Health-related quality of life of HIV-infected intravenous drug users. Int J STD AIDS. (2013) 24:867–74. doi: 10.1177/0956462413486454
52. Perez IR, Olry de Labry Lima A, del Castillo LS, Bano JR, Ruz MAL, del Arco Jimenez A. No differences in quality of life between men and women undergoing HIV antiretroviral treatment Impact of demographic, clinical and psychosocial factors. AIDS Care. (2009) 21:943–52. doi: 10.1080/09540120802612840
53. O'Brien KE, Riddell NE, Gómez-Olivé FX, Rae DE, Scheuermaier K, von Schantz M. Sleep disturbances in HIV infection and their biological basis. Sleep Med Rev. (2022) 65:101571. doi: 10.1016/j.smrv.2021.101571
54. Zuñiga JA, Harrison ML, Henneghan A, García AA, Kesler S. Biomarkers panels can predict fatigue, depression and pain in persons living with HIV: a pilot study. Appl Nurs Res. (2020) 52:151224. doi: 10.1016/j.apnr.2019.151224
55. Jong E, Oudhoff LA, Epskamp C, Wagener MN, van Duijn M, Fischer S, et al. Predictors and treatment strategies of HIV-related fatigue in the combined antiretroviral therapy era. AIDS. (2010) 24:1387–405. doi: 10.1097/QAD.0b013e328339d004
56. Shikuma CM, Kohorn L, Paul R, Chow DC, Kallianpur KJ, Walker M, et al. Sleep and neuropsychological performance in HIV+ subjects on efavirenz-based therapy and response to switch in therapy. HIV Clin Trials. (2018) 19:139–47. doi: 10.1080/15284336.2018.1511348
57. Barroso J, Voss JG. Fatigue in HIV and AIDS: an analysis of evidence. J Assoc Nurses AIDS Care. (2013) 24:S5–14. doi: 10.1016/j.jana.2012.07.003
58. Wilson NL, Azuero A, Vance DE, Richman JS, Moneyham LD, Raper JL, et al. Identifying symptom patterns in people living with HIV disease. J Assoc Nurses AIDS Care. (2016) 27:121–32. doi: 10.1016/j.jana.2015.11.009
59. Moens K, Siegert RJ, Taylor S, Namisango E, Harding R, ENCOMPASS, EURO IMPACT. Symptom clusters in people living with HIV attending five palliative care facilities in two sub-Saharan African countries: a hierarchical cluster analysis. PLoS ONE. (2015) 10:e0126554. doi: 10.1371/journal.pone.0126554
60. Boyer V, Vilotitch A, Marcellin F, Demoulin B, Dray-Spira R, Spire B, et al. Self-reported bothersome symptoms across different socioepidemiological groups of people living with HIV attending French hospitals: results from the ANRS-VESPA2 survey. J Pain Symptom Manage. (2017) 54:110–9. doi: 10.1016/j.jpainsymman.2017.03.010
61. Zhu Z, Zhao R, Hu Y. Symptom clusters in people living with HIV: a systematic review. J Pain Symptom Manage. (2019) 58:115–33. doi: 10.1016/j.jpainsymman.2019.03.018
62. Zuniga JA, Bose E, Park J, Lapiz-Bluhm MD, García AA. Diabetes changes symptoms cluster patterns in persons living with HIV. J Assoc Nurses AIDS Care. (2017) 28:888–96. doi: 10.1016/j.jana.2017.07.004
63. Busato IMS, Thomaz M, Toda AI, Alanis DGP, França BHS, de Lima AAS, et al. Prevalence and impact of xerostomia on the quality of life of people living with HIV/AIDS from Brazil. Spec Care Dentist. (2013) 33:128–32. doi: 10.1111/j.1754-4505.2012.00290.x
64. Macedo N, Baggio G, Henn I, Santos J, Batista T, Ignácio S, et al. Oral conditions and salivary analysis in HIV-uninfected subjects using preexposure prophylaxis. Med Oral Patol Oral Cir Bucal. (2022) 27:e265–73. doi: 10.4317/medoral.25140
65. Di Gennaro F, Lattanzio R, Falanga C, Negri S, Papagni R, Novara R, et al. Low-wage agricultural migrant workers in Apulian Ghettos, Italy: general health conditions assessment and HIV screening. Trop Med Infect Dis. (2021) 6:184. doi: 10.3390/tropicalmed6040184
66. Umniyati H, Noviani RP, Masriadi S. Determine relationship between xerostomia and quality of life of HIV person's living in prison. J Int Soc Prev Community Dent. (2022) 12:360–4. doi: 10.4103/jispcd.JISPCD_229_21
67. Navazesh M, Mulligan R, Karim R, Mack WJ, Ram S, Seirawan H, et al. Effect of HAART on salivary gland function in the Women's Interagency HIV Study (WIHS). Oral Dis. (2009) 15:52–60. doi: 10.1111/j.1601-0825.2008.01456.x
68. Schnall R, Jia H, Reame N. Association between HIV symptom burden and inflammatory cytokines: an analysis by sex and menopause stage. J Womens Health. (2020) 29:119–27. doi: 10.1089/jwh.2019.7749
69. Feng SY, Shao B, Song B. Analysis of life quality of major HIV infected people in Harbin and its influencing factors. J Harbin Med Univ. (2017) 51:78–86.
70. Sun Y, Xue Z, Xuan Y. Quality of life and influencing factors of long-term survival of HIV/AIDS patients in Henan province. Chin J AIDS STD. (2019) 25:115–8.
71. Murzin K, Racz E, Behrens DM, Conway T, Da Silva G, Fitzpatrick E, et al. “We can hardly even do it nowadays. So, what's going to happen in 5 years from now, 10 years from now?” The health and community care and support needs and preferences of older people living with HIV in Ontario, Canada: a qualitative study. J Int AIDS Soc. (2022) 25:e25978. doi: 10.1002/jia2.25978
72. Zhang X, Chen J, Xu K. Quality of life and its influencing factors among people living with HIV/AIDS in Hangzhou City. Prev Med. (2022) 34:27–32. doi: 10.19485/j.cnki.issn2096-5087.2022.01.006
73. Emuren L, Welles S, Macalino G, Evans AA, Polansky M, Ganesan A, et al. Predictors of health-related quality of life among military HIV-infected individuals. Qual Life Res. (2020) 29:1855–69. doi: 10.1007/s11136-020-02441-5
74. Afrashteh S, Fararouei M, Ghaem H, Aryaie M. Factors associated with baseline CD4 cell counts and advanced HIV disease among male and female HIV-positive patients in Iran: a retrospective cohort study. J Trop Med. (2022) 2022:8423347. doi: 10.1155/2022/8423347
75. Armon Armon C;, Lichtenstein K; The associations among coping nadir CD4+ T-cell count and and non-HIV-related variables with health-related quality of life among an ambulatory HIV-positive patient population. Qual Life Res. (2012) 21:993–1003. doi: 10.1007/s11136-011-0017-2
76. Protopopescu C, Marcellin F, Spire B, Prau M, Verdon R, Peyramond D, et al. Health-related quality of life in HIV-1-infected patients on HAART: a 5-years longitudinal analysis accounting for dropout in the APROCO-COPILOTE cohort (ANRS CO-8). Qual Life Res Int J Qual Life Aspects Treatment Care Rehabil. (2007) 16:577–91. doi: 10.1007/s11136-006-9151-7
77. Alebel A, Sibbritt D, Petrucka P, Demant D. Association between body mass index variation and early mortality among 834 ethiopian adults living with HIV on ART: a joint modelling approach. Infect Dis Ther. (2022) 22:1–18. doi: 10.1007/s40121-022-00726-5
78. Liu Y, Hao Y, Xiao J, Wu L, Liang H, Han J, et al. Trends in rates and causes of hospitalization among people living with HIV in the antiretroviral therapy era: a retrospective cohort study in China, 2008–2020. Front Public Health. (2022) 10:1000942. doi: 10.3389/fpubh.2022.1000942
79. Che S, Huang Y, Zeng Y, Yang W, Ren J, Zhang Q, et al. Analysis of the effect and influencing factors of antiviral treatment among HIV/AIDS patients in Liangshan prefecture from 2010 to 2019. Prevent Med Inform. (2022) 38:1321–8.
80. Dong X, Peng L, Zhang S, Li Y, Cai W, Wang H, et al. Quality of life and related factors among people living with HIV/AIDS in Guangdong province. Chin J Epidemiol. (2014) 35:40–4.
81. Sui DD, Lin P, Chen SH. Quality of life of 179 patients infected with HIV. South China J Prev Med. (2015) 41:117–23. doi: 10.13217/j.scjpm.2015.0117
82. van der Kop ML, Muhula S, Patel A, Thabane L, Awiti P, Kyomuhangi L, et al. Gender differences in health-related quality of life at the time of a positive HIV test: a cross-sectional study in a resource-poor, high prevalence setting in?Nairobi, Kenya. AIDS Care. (2018) 30:493–9. doi: 10.1080/09540121.2017.1417970
83. Rayanakorn A, Ong-Artborirak P, Ademi Z, Chariyalertsak S. Predictors of stigma and health-related quality of life among people living with HIV in Northern Thailand. AIDS Patient Care STDS. (2022) 36:186–93. doi: 10.1089/apc.2022.0035
84. Wang P, Gao J-Y, Zhou H-J, Wu J, Wang Y. Health-related quality of life of Chinese AIDS patients: a multi-region study. Qual Life Res. (2022) 22:1–10. doi: 10.1007/s11136-022-03299-5
85. Kall M, Fresán U, Guy D, Brown G, Burgui C, Castilla J, et al. Quality of life in people living with HIV in Romania and Spain. BMC Infect Dis. (2021) 21:898. doi: 10.1186/s12879-021-06567-w
86. Xu X, Zhou Y, Su D, Dang Y, Zhang X. Does education influence life-course depression in middle-aged and elderly in China? Evidence from the China health and retirement longitudinal study (CHARLS). Int J Environ Res Public Health. (2023) 20:1256. doi: 10.3390/ijerph20021256
Keywords: HIV, health-related quality of life, China, influencing factors, cross-sectional study
Citation: Zhong H, Wei FL, Song YQ, Chen H and Ni Z (2023) Health-related quality of life and associated factors among people living with HIV/AIDS in Sichuan, China: A cross-sectional study. Front. Public Health 11:1133657. doi: 10.3389/fpubh.2023.1133657
Received: 29 December 2022; Accepted: 20 February 2023;
Published: 13 March 2023.
Edited by:
Diego Ripamonti, Papa Giovanni XXIII Hospital, ItalyReviewed by:
Wei Ma, School of Public Health, Shandong University, ChinaAntonella Cingolani, Catholic University, Italy
Linda Aurpibul, Chiang Mai University, Thailand
Copyright © 2023 Zhong, Wei, Song, Chen and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Chen, MTM2NjEwOTg3OEBxcS5jb20=
 Hua Zhong
Hua Zhong Fuling Wei
Fuling Wei Yuqing Song1
Yuqing Song1 Hong Chen
Hong Chen Zhao Ni
Zhao Ni