- 1School of Nursing, Shaanxi University of Chinese Medicine, Xianyang, Shaanxi, China
- 2Department of Nursing, Affiliated Hospital of Shaanxi University of Chinese Medicine, Xianyang, Shaanxi, China
Background: To investigate the depression, anxiety and somnipathy situation occurred in the nucleic acid collection staff during the closed-loop management period of COVID-19. And try to understand the influencing factors of related psychological status.
Methods: A cross-sectional study of 1,014 nucleic acid collection staff from seven Chinese hospitals was conducted. Various investigation methods were involved in the questionnaires to collect data, including 12-items self-made questionnaire survey of basic demographic information, 9-items patient health questionnaire depression scale (PHQ-9), 7-items generalized anxiety disorder scale (GAD-7) and Pittsburgh sleep quality index (PSQI). Data analysis was performed using SPSS version 26.0 and Excel software. Mann-Whitney U-test, Chi-square test, correlation analysis, mono-factor analysis and binary logistic regression were applied accordingly for further analysis.
Results: The positive rate of depression, anxiety and sleep disorder of 1,014 nucleic acid collectors under closed-loop management were 33.5, 27.2, and 50.1%, respectively. Depression was significantly positively correlated with anxiety and sleep (P < 0.05). The scores of depression scale were positively correlated with the age and the fear for infection (r = 0.106, 0.218, both P < 0.05); The scores of anxiety scale were also positively correlated with the age and the fear for infection (r = 0.124, 0.225, both P < 0.05); The length of service, collection time and the degree of worry about infection and was positively correlated with the score of sleep scale (r = 0.077, 0.074, 0.195, both P < 0.05); Education level had a significant negative association with PHQ-9, GAD-7 and PSQI (r = −0.167,−0.172, both P < 0.05). Binary logistic regression analysis showed that age, technical title, education level, collection time, collection frequency, collection location, fear for infection and external environment were important influencing factors of depression, anxiety and sleep disorders.
Conclusion: The results of this study suggested that when carrying out nucleic acid collection mission, managers should intervene to optimize the collection location, control the duration of each collection mission, replace the collection staff in time and pay close attention to the psychological state of the collection staff.
1. Introduction
A novel coronavirus disease (COVID-19), caused by Coronavirus type 2 (SARS-CoV-2) emerged in Wuhan, China in December 2019, has become the third coronavirus in the past 20 years since the outbreak of severe acute respiratory syndrome coronavirus (SARS-CoV) in 2002 and the Middle East outbreak of respiratory syndrome coronavirus (MERS-CoV) in 2012. With rapidly spread all over the world and concomitant mortality burden, the COVID-19 outbreak represents a global public health issue which unseen in the last century (1–4). So far, the world has been witnessed four waves of viruses: Alpha variant (B.1.1.7), Beta variant (B.1.351), Gamma variant (P.1) and Delta variant (B.1.617.2). However, the new strain, Omicron (B.1.1.529), was discovered for the first time in South Africa in November 2021 (5). This strain has the characteristics of fast transmission, strong infectivity, high pathogenicity and short incubation period (6). Therefore, we need more rapid and immediate responses in healthcare to avoid more infections.
In December 2021, a case of localized Omicron variant occurred in Xi'an, Shaanxi. There were 2,080 new cases of coronavirus pneumonia confirmed within 40 days, the largest local outbreak in a megacity since the Wuhan outbreak (7). According to the COVID-19 Diagnostic Guide issued by China and related research, a positive real-time reverse transcription polymerase chain reaction (RT-PCR) test is considered the main criterion for the diagnosis of COVID-19 (8, 9). Nucleic acid collectors are one of the important pillars during the pandemic and play a key role during the pandemic.
In order to prevent the further spread of the epidemic, the medical institutions actively arranged nucleic acid collection teams to carry out wide range nucleic acid sampling throughout the city and closed-loop management for nucleic acid collection employees in accordance with the local epidemic prevention and control procedures. Closed-loop management is a management method formed by integrated information system, closed-loop system, management control and management closure principle. It can be effectively used in epidemic prevention and control (10). Point-to-point management allowed for closed-loop hospital locations, closed-loop roadways, closed-loop lodging sites, closed-loop epidemics and closed-loop patient status (hospital to hotel accommodation sites, hospital to quarantine sites).
During the sampling period, due to the large population of Xi'an, the sampling workload is extremely heavy, and the maximum sample size can reach 8.92 million people per day. The nucleic acid collectors need to start the preparation work at 3 am every day. The sampling site conditions are rudimentary, most of them are mobile sampling points which are temporarily constructed outdoors. And the weather is cold during the epidemic, the protective suits are too thin to keep warm. The working hours are also uncertain, most people work more than 8 h a day. Due to strict protection requirements, medical staff can barely drink water when sampling, and it is inconvenient to go to the toilet. All these factors may cause high work pressure on both physical and mental aspects among nucleic acid collectors.
Previous studies have found that frontline workers are prone to a range of psychological problems, including fear, depression, anxiety, post-traumatic stress symptoms and insomnia during high-risk and stressful situations during the pandemic (11–13). For example, a large proportion of healthcare workers battling SARS suffer from depression, anxiety and sleep problems (14, 15). Recent studies have shown that health workers have higher psychological problems during COVID-19 than in past epidemics (16). Several studies have shown that physical, emotional, and mental health can all be impaired by overwork (17–20). The potential negative psychological impact is not only detrimental to the growth of medical staff, but also may reduce effective response to emergencies (11, 21).
At present, there have been many investigations on the anxiety and depression of medical staff in the fight against the epidemic. But during the strict closed-loop management, nucleic acid collectors face great physical and mental challenges, and there are few studies on the impact of such management methods on psychological state. The purpose of this paper was to conduct a preliminary psychological evaluation of nucleic acid collectors who participated in closed-loop management during the Omicron epidemic in Xi'an, and analyze the influencing factors to provide a scientific basis for later psychological recovery.
2. Method
2.1. Setting and sampling
This survey based on convenience sampling was conducted for medical personnel for nucleic acid collection during closed-loop management in 7 Grade III Grade A hospitals in Shaanxi Province from March 25 to April 18, 2022. To facilitate the sample collection, all personnel participated in nucleic acid collection-related training, informed consent and voluntary participation in this study. Thompson's study suggested a sample size of 10–15 times the questionnaire items for the structural equation model (22). Forty seven items made up the self-administered questionnaire, which had a total sample size of 705 participants. Due to incomplete questionnaires, the sample size was increased by 20% to a total of 846; nevertheless, the final sample size was 1,028 individuals.
2.2. Ethical approval
All personnel volunteered to participate in this study and were allowed to withdraw during the process. The electronic information submitted was anonymous and only researchers had access to the data. The Ethics Committee of the Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine, Shaanxi Province, China approved this study (Ethical number:2022-0516).
2.3. Data collection
Wenjuanxing, an online crowdsourcing platform on the Chinese mainland, was used to make the questionnaire because of the outbreak. It was then sent to the WeChat group, which is a public social networking tool in China, for the staff who collect nucleic acids. The WeChat group was informed of the objective and importance of this survey and one response is allowed from a given IP address. After the questionnaire had been reviewed and examined by two quality controllers, the entire survey results were collected from the questionnaire star platform. Those who chose the same option in questionnaires and those who missed >10% of items were excluded. After filtering, 1,014 questionnaires were included in the subsequent analysis with a response rate of 98.64%.
2.4. Measurements
The survey consisted of the following four parts: Sociodemographic data, Patient health questionnaire-9 (PHQ-9), Generalized anxiety disorder 7-item (GAD-7) Scale and Pittsburgh sleep quality index (PSQI).
2.4.1. Demographic information of survey respondents
A self-administered general data questionnaire was used, mainly including gender, age, occupation, years of work, education level, technical title, nucleic acid collection attendance frequency in the past 3 months (hereinafter referred to as “collection frequency”), continuous collection time per attendance (hereinafter referred to as “collection time”), a regular presence at the site of nucleic acid collection (hereinafter referred to as “collection place”), and whether external environmental factors (winter, summer, rain, wind) affect nucleic acid collection (hereinafter referred to as “external environment”). The degree of concern about infection is hereinafter referred to as “the degree of concern.”
2.4.2. Patient health questionnaire-9 (PHQ-9)
The Chinese Patient Health Questionnaire-9 (PHQ-9), a self-measuring reporting method used to assess the severity of depression, is widely used as an open screening tool for depression in different healthcare and community environments (23). PHQ-9 is composed of 9 items, with a Likert score of 4, divided into scores of 0 (none at all), 1 (a few days), 2 (most of the time), and 3 (almost every day), for a total score of 27 points. The higher the score, the more severe the depression. Scoring criteria: no depression (0~4), mild depression (5~9), moderate depression (10~14), severe depression (15~27). The psychometric characteristics of the PHQ-9 are reliable to measure depression allied with clinical features with strong consistency (Cronbach's alpha = 0.86) (24). The study concluded that a score of 10 was the optimal threshold for PHQ-9 with a sensitivity of 92.8% and specificity of 95.7% (25). Therefore, a score of 10 on the PHQ-9 questionnaire indicated the presence of depression.
2.4.3. Generalized anxiety disorder 7-item (GAD-7) scale
The generalized anxiety scale, developed by Spitzer et al. (26) in 2006 to identify anxiety disorders with optimal reliability and validity, assesses the severity of anxiety symptoms over 2 weeks. GAD-7 is composed of seven items, with a Likert score of 4, divided into scores of 0 (none at all), 1 (a few days), 2 (most of the time), and 3 (almost every day), for a total score of 21 points. The higher the score, the more severe the anxiety suppression. Scoring criteria were no anxiety (0~4), mild anxiety (5~9), moderate anxiety (10~14), and severe anxiety (15~21). On the other hand, the psychometric characteristics of the GAD-7 are also reliable to measure anxiety allied with clinical features with strong consistency (Cronbach's alpha = 0.92) and good test-retest reliability (r = 0.88) (26). In this questionnaire, people with GAD-7 score ≥10 were very likely suffering anxiety, a score of 10 was considered the optimal cut-off value for the GAD-7 with a sensitivity of 89% and specificity of 82% (27).
2.4.4. Pittsburgh sleep quality index, PSQI
This scale was compiled by Buysse et al. (28) and translated into Chinese (29) to evaluate the sleep quality. The scale can evaluate the sleep situation of nearly a month and contains 18 items and 7 dimensions, including sleep quality, time to sleep, sleep time, sleep efficiency, sleep disorder, hypnotics and daytime dysfunction. The responses to the items are weighted on a scoring scale between 0 and 3. The total PSQI score is from 0 to 21 points. The seven component scores are then summed to yield a global PSQI score, which has a range of 0–21, higher scores indicate worse sleep quality. The scoring criteria were normal sleep quality (0~5), mild sleep disorder (6~10), moderate sleep disorder (11~15), and severe sleep disorder (16~21). The PSQI has internal uniformity and a reliability coefficient (Cronbach's alpha) of 0.90 for its seven components, the overall PSQI global score correlation coefficient for test-retest reliability was 0.87 (30). When PSQI is applied in different populations, in order to achieve better screening effect, it is necessary to adjust the judgment cut-off. Applying PSQI ≥ 7 as a reference value for sleep quality problems in Chinese adults (31, 32).
2.5. Data analysis
The collected data were analyzed using SPSS version 26 and Excel software. The distribution of PHQ-9, GAD-7, and PSQI scores in the general population did not adhere to a normal distribution, according to a first evaluation of the measured data's normality. The median and quartile were used to represent M (P25, P75), and the non-parametric rank sum test (Mann Witney U) was employed for intergroup comparison, and count data were expressed as ratio or composition ratio (%). Second, the differences between groups were compared using the Chi-square test (χ2), and all of the variables' correlations were determined using Pearson's correlation coefficients. Third, monofantor analysis and binary logistic regression were used to analyze the influencing factors of depression, anxiety and sleep disorder. The OR value and 95% CI were calculated, with P-values < 0.05 being regarded as statistically significant (2-sided tests).
3. Results
3.1. General participant characteristics
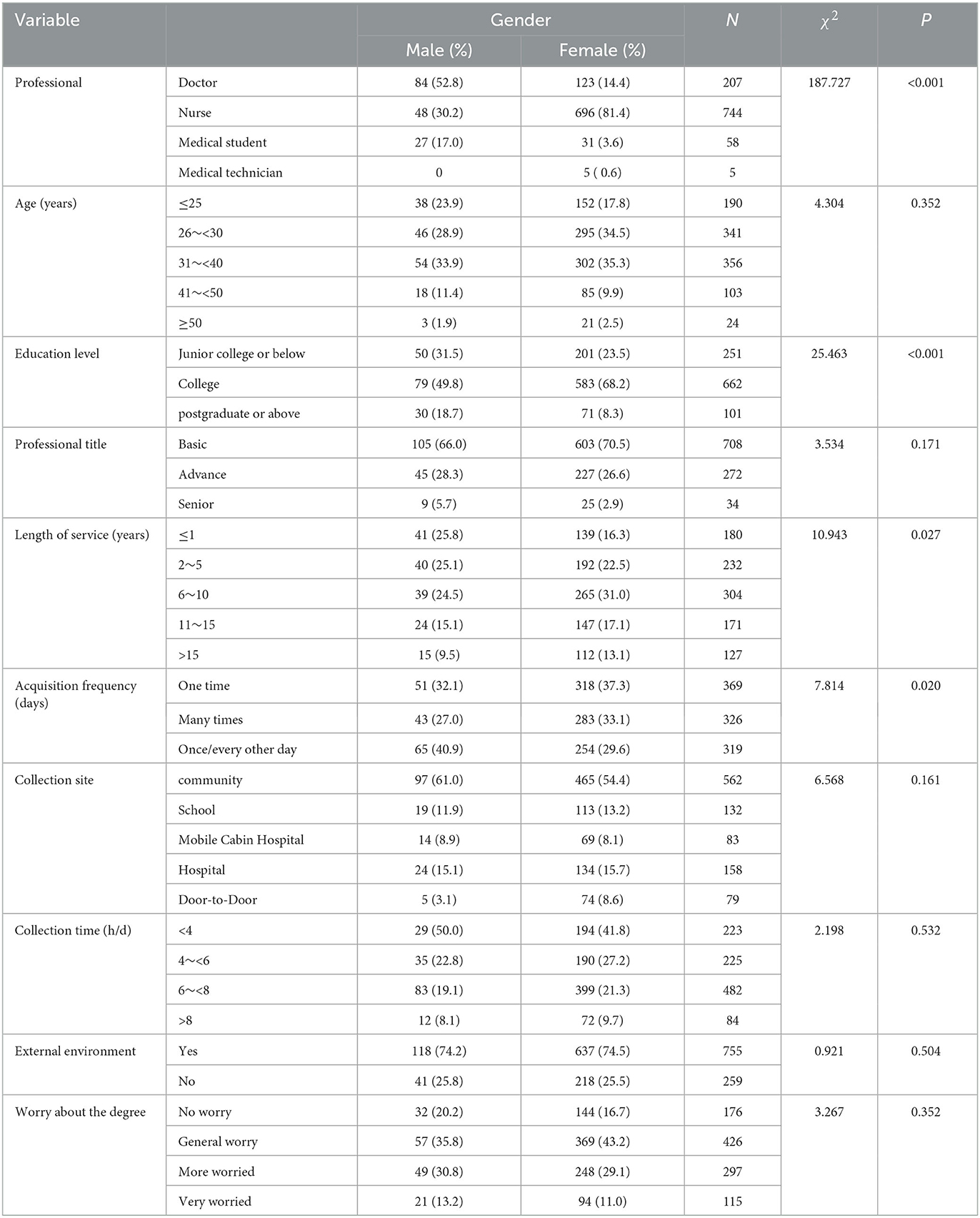
The demographic and work-related characteristics and scores of 1,014 nucleic acid collections are shown in Table 1. Demographic data analysis by gender showed that 84.3% of the 1,014 participants were female; 73.4% were nurses; 35.1% were 31–40 years old; 66.2% were undergraduates; junior professional titles accounted for the majority, 69.8%; the participants acquired once per day (36.4%); 55.4% were community-based; the acquisition time was 6–8 h per day, accounting for 47.5%; 74.5% would be influenced by the external environment; and 42.0% were generally concerned about infection.
3.2. Score and prevalence of PHQ-9, GAD-7 and PSQI
PHQ-9, GAD-7 and PSQI of the nucleic acid collectors were statistically analyzed by sex. The results showed that the median M (P25, P75) score of PHQ-9 was 7 (1, 17) for males and 6 (2, 14) for females; GAD-7: 4 (0, 13) for males and 3 (0, 11) for females; PSQI was 6 (3, 8) for males and 7 (4, 9) for females. The positive rates of depression, anxiety and sleep disorders among nucleic acid collectors were 33.5, 27.2, and 50.1%, respectively; there was a significant difference between male and female groups in sleep disorder (P < 0.05) (Table 2).

Table 2. Positive rate of depression, anxiety and sleep disorders among 1,014 nucleic acid collectors under closed-loop management [N = 1,014(%)].
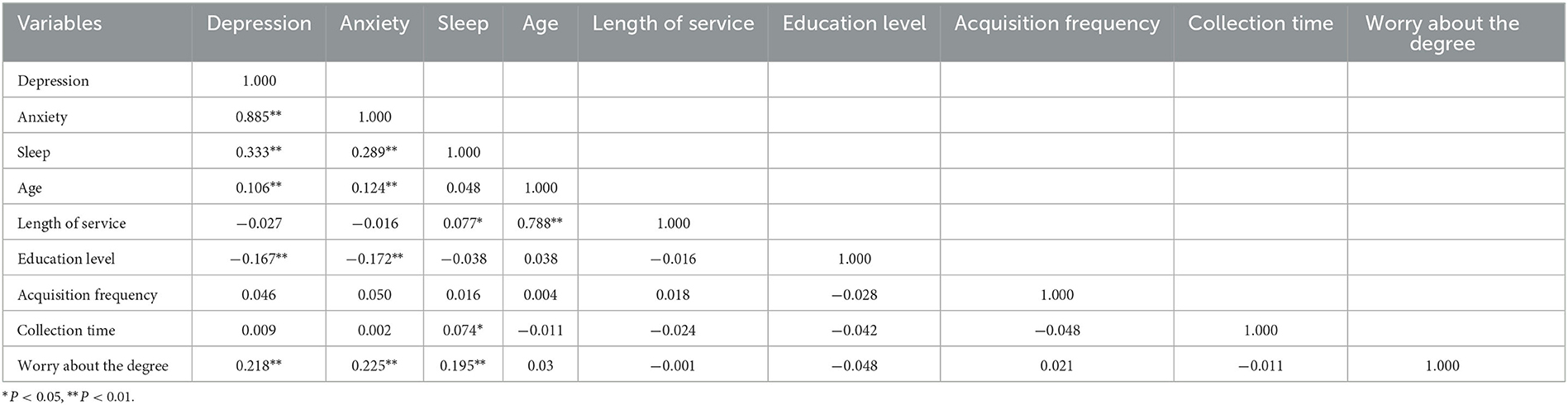
3.3. Correlation analysis of depression, anxiety and sleep quality
PHQ-9, GAD-7, and PSQI were found to be positively correlated (P < 0.05) in a correlation analysis. Age and fear for infection were positively correlated with depression and anxiety scores (P < 0.05). Years of work, collection time and fear for infection were positively correlated with sleep disorder scores (P < 0.05). Notably, education level had a significant negative association with PHQ-9, GAD-7 and PSQI (P < 0.05), as can be found in Table 3.
3.4. Monofactor analysis
Monofactor analysis revealed significant differences between the type of personnel, age, education level, technical title, collection time, collection frequency, collection location, external environment and worry level and the positive rate of depression and anxiety (all P < 0.05). There were statistically significant differences between the positive rate of sleep disorders and different education levels, collection frequency, external environment and worry level (all P < 0.05), as indicated in Table 4.
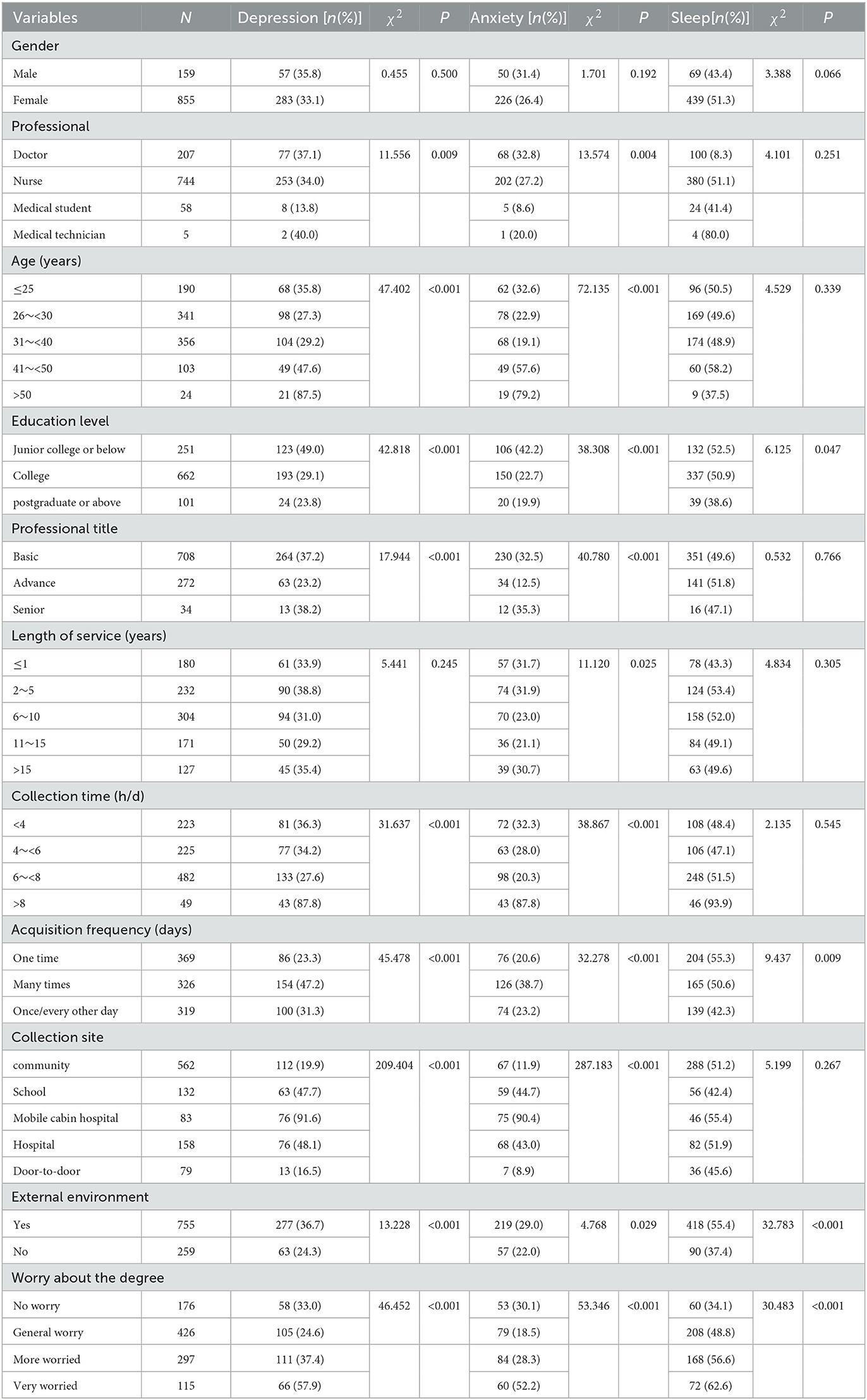
Table 4. Monofactor analysis of depression, anxiety and sleep disorder in 1,014 nucleic acid collectors under closed-loop management [N = 1,014(%)].
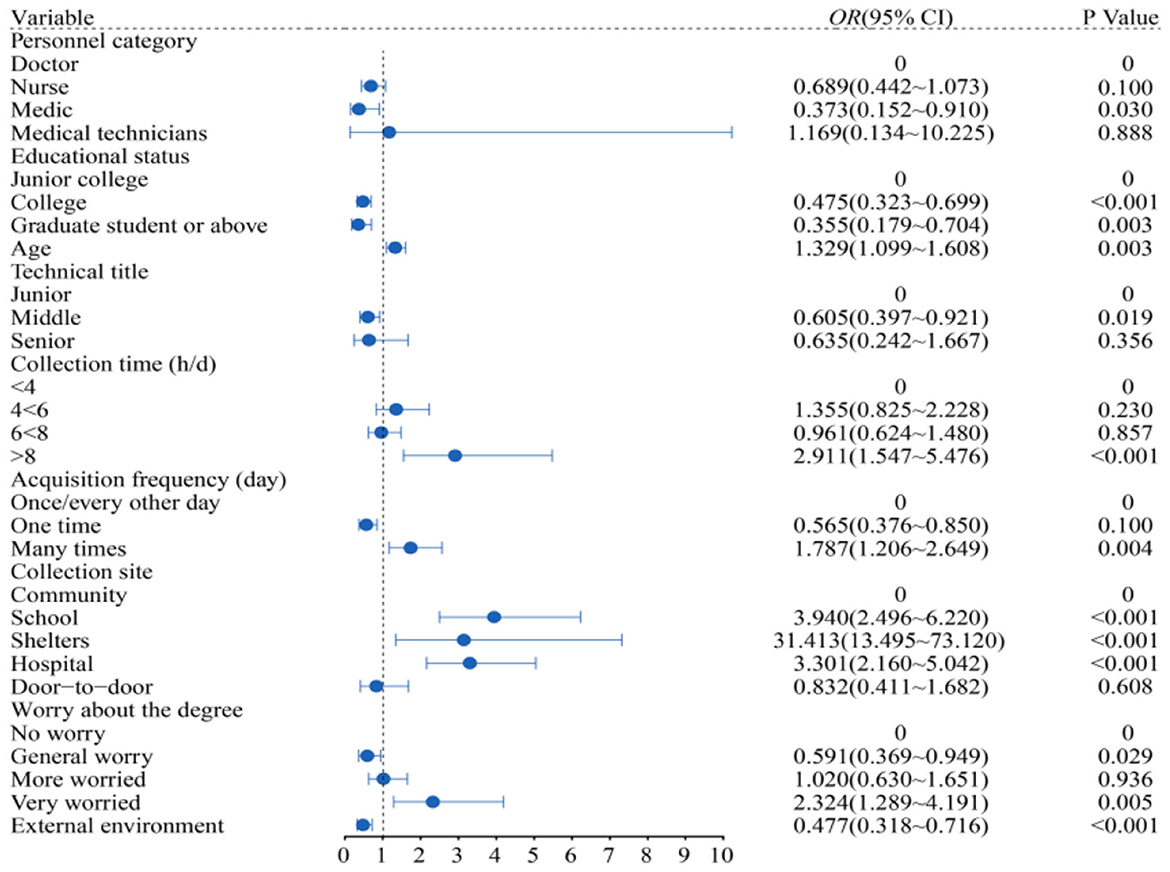
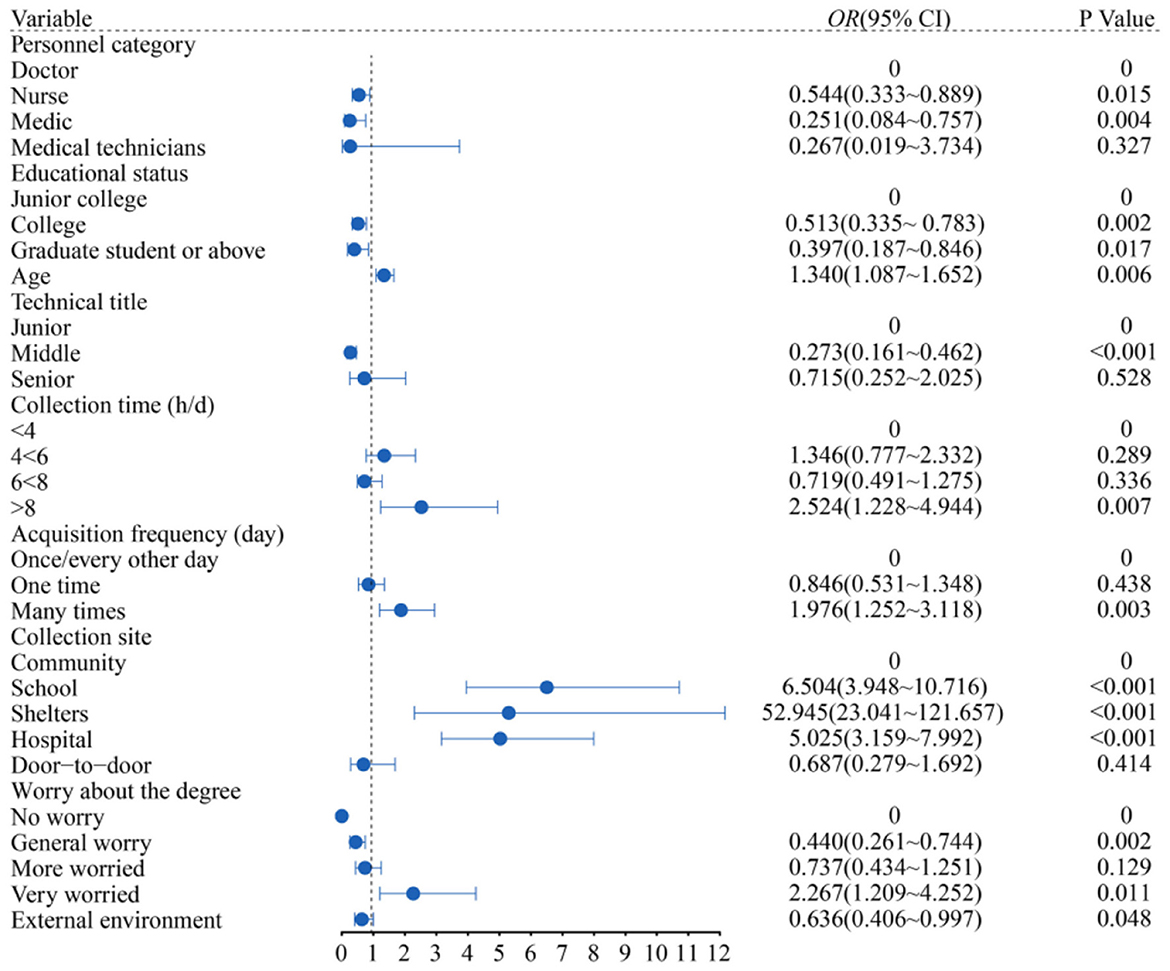
3.5. Binary logistic regression
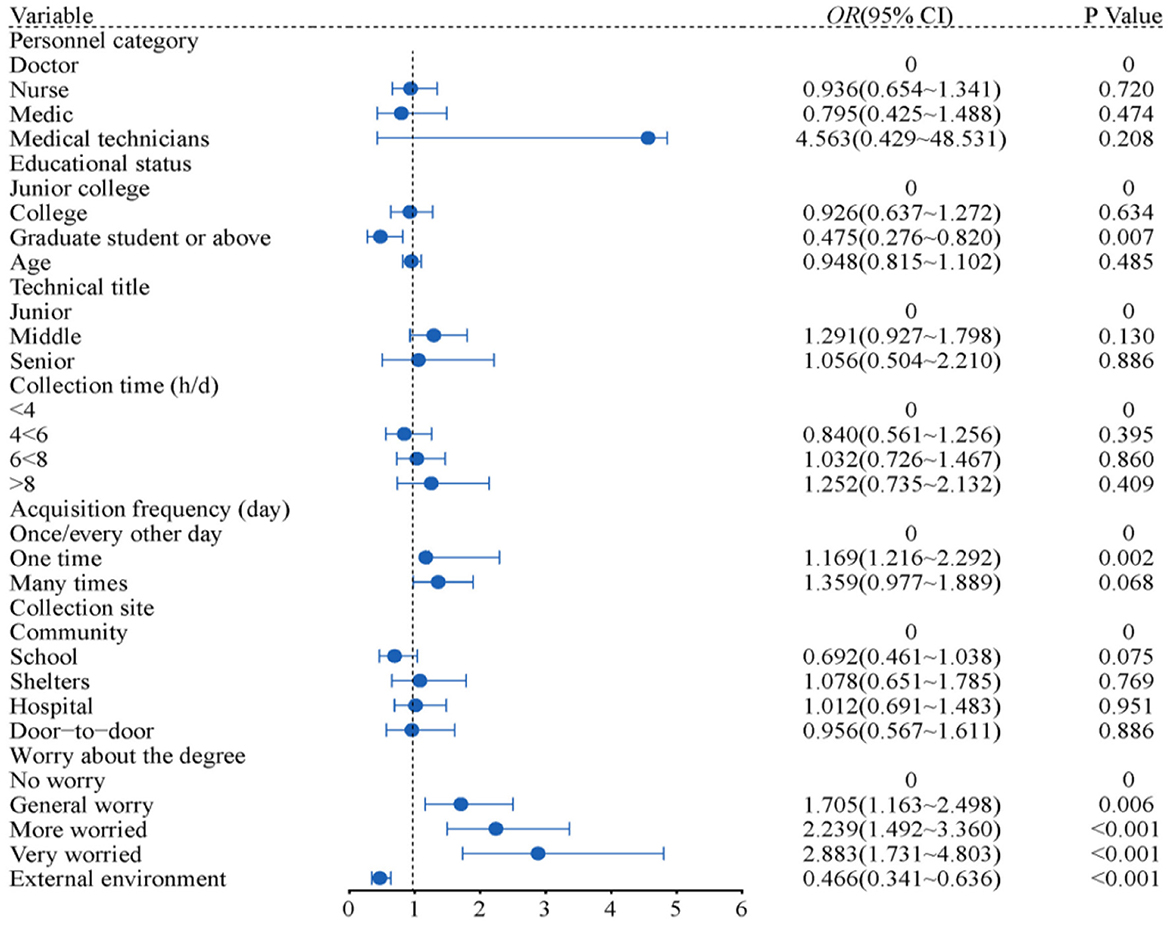
The following independent variables were included in the binary logistic regression model with whether depression, anxiety and sleep were abnormal as dependent variables (values of 1 for yes and 0 for no). Each variable was based on “0.” The reference group was assigned to the category of medical personnel (0 for doctors), education level (0 for junior college students), technical title (0 for junior students), collection time (0 for < 4 h/day), collection frequency (0 for once/every other day), and collection location (0 for communities), Worry level (no worry is 0).
3.5.1. Overall fit of the model
The goodness-of-fit of this paper focused on the H-L index to test the goodness-of-fit of the logistic model. When the significance is >0.05, it indicates that the model fits well, and when the significance is < 0.05, it suggests that the model fits poorly, and the model test results are shown in Table 5.
3.5.2. Binary logistic model results
Figure 1 depicts the depression of medical students as being 0.373 times lower than that of doctors (95% CI: 0.152 to 0.910); education level is the protective factor for depression. Undergraduate and graduate students with higher education backgrounds had 0.475 times lower depression levels compared to undergraduates (95% CI: 0.323 to 0.699); 1.329 times higher depression prevalence per additional age unit (95% CI: 1.099 to 1.608); and 0.605 times lower intermediate levels compared to junior level (95% CI: 0.397 to 0.921); the longer the collection time, the higher the depressive mood. The risk of depressive mood of those who collected more than 8 h per day was 2.911 times higher than that of those who collected 4 h per day (95% CI: 1.547 to 5.476); the number of people with multiple collection times/day was 1.787 times that of people with one collection every other day (95% CI: 1.206 to 2.649); The people in the mobile cabin hospital were the most depressed, 31.413 times as many as those in the community (95% CI: 13.495 to 73.120); 2.324 times (95% CI: 1.289 to 4.191) of those who were very worried about infection than those who were not; the external environment could affect the depression of the collectors (95% CI: 0.318 to 0.716) (All P < 0.05).
Figure 2 depicts the anxiety of nurses as being 0.544 times lower than that of doctors (95% CI: 0.333 to 0.889), and that of medical students was 0.251 times lower than that of doctors (95% CI: 0.084 to 0.757); the degree of education was a protective factor of anxiety. Compared with college students, the anxiety of undergraduates and postgraduates with higher education is 0.513 times lower (95% CI: 0.335 to 0.783); the incidence of anxiety increased 1.340 times (95% CI: 1.087 to 1.652) with the increase in age; Compared with primary professional titles, intermediate professional titles decreased by 0.237 times (95% CI: 0.161 to 0.462); The longer the collection time, the greater the inhibition of anxiety was. The risk of depression was 2.542 times (95% CI: 1.228 to 4.944) higher for those who collected more than 8 h a day than those for collected 4 h a day; the number of people with multiple collection times/day was 1.976 times that of people with one collection every other day (95% CI: 1.252 to 3.118); people in mobile cabin hospital were the most anxious, 52.945 times as much as those in the community (95% CI: 23.041 to 121.657); 2.267 times (95% CI: 1.209 to 4.252) of those who were very worried about infection than those who were not; the external environment affected the anxiety of the collectors (95% CI: 0.406 to 0.997) (All P < 0.05).
Figure 3 depicts that education level is the protective factor for sleep disorder. Compared with college students, the sleep disorder of postgraduates and above decreased by 0.475 times (95% CI: 0.276–0.820); The personnel who collected once a day were 1.169 times as many as those who collected once every other day (95% CI: 1.216 to 2.292); People who were very worried about infection were 2.883 times more likely to have sleep disorders than others (95% CI: 1.731 to 4.803); The external environment can affect the sleep of the collector (95% CI 0.341 to 0.636) (All P < 0.05).
4. Discussion
This study analyzed the psychological status of 1,014 nucleic acid collection staff in Shaanxi Province under closed-loop management through monofactor and binary logistic regression models. And the research found a high proportion of nucleic acid collectors with depression, anxiety and sleep disorders during closed-loop management. Age, technical title, education level, collection time, collection frequency, collection location, fear for infection and external environment also affected the psychological state. The PHQ-9, GAD-7 and PSQI used in this study are mainly used for clinical screening for depression, generalized anxiety disorders and sleep disorders. When PHQ-9 and GAD-7 scores ≥ 10 points, PSQI ≥ 7 points, usually considered that the patients may have depressed mood, anxiety or sleep disorder problems and need further diagnosis (25, 26).
First, the incidence of depression, anxiety and sleep disorders among nucleic acid collection personnel throughout the closed-loop management period were 33.5, 27.2, and 50.1%, respectively. Previous research showed that during the epidemic, 14.3% of clinical doctors and nurses suffered from depression, 11.2% from anxiety (33), and 61.67% (34) from sleep disorders. During the non-epidemic period, the incidence of depression, anxiety and sleep disorders of medical staff were 1.98%, 6.52% (35), and 39.2% (36), respectively. Moreover, compared with more research data from other countries on the incidence of depression, anxiety and sleep disorders among medical personnel during the COVID-19 pandemic. The incidence of depression, anxiety and sleep disorders were 36, 34, and 52%, respectively in Spanish medical personnel (37); 37, 23, and 34% in Latin America (38); 55, 51, and 28% in Africa (39); 34%, 46% (40), and 40% (41) in Eastern Europe. And the prevalence of depression, anxiety and sleep disorders among health-care workers in south-east Asia were generally lower than other regions during the pandemic, which were 14, 23, and 18% (42), respectively. Therefore, the prevalence of mental health symptoms during the COVID-19 pandemic is not homogeneous across different regions. Compared with the results in this study, the incidence of depression and anxiety in above countries are much higher. On the one hand, different research tools may lead to differences results. On the other hand, since the COVID-19 outbreak, the world has experienced many waves of the epidemic, medical staff's mental state is also different from the beginning. Moreover, the different incidence of depression, anxiety and sleep disorders between different countries are more likely related to region, cultural and political factors. For instance, African health-care workers have the highest rates of depression and anxiety in these countries, and it may be that in economically underdeveloped areas, the incidence of infectious diseases is high, health facilities are poor and mental health receives less attention (39). These are likely to lead to an increase in the incidence of depression and anxiety in health-care workers. On the contrary, the incidence of sleep disorders among nucleic acid collection personnel in this study is higher than in other countries. It was hypothesized that researchers and nucleic acid collectors were engaged in long-term epidemic prevention, which leading to high mental stress and heavy workload. In addition, frequent shifts, lack of sleep also increased the risk of infection during closed-loop management. The sudden outburst of this highly infectious disease and the containment measures such as quarantine and social distancing have posed immense pressure on the work and life of the health-care workers (43). This could lead to an increased incidence of sleep disorders among the nucleic acid collection staff.
Second, this study examined the correlation between the research variables among the nucleic acid collection staff. The higher the score on the depression and anxiety scale, the higher the total score of sleep disorder, indicating that medical staff sleep quality is poor. At the same time, when the sleep disorder score increased, the occurrence of depression and anxiety increased. The age of the nucleic acid collection staff was positively related to depression and anxiety, indicating that the older the patient, the more likely he or she was to suffer from depression and anxiety, the present study findings are in line with other reports (35, 44). Younger adults, however, appear to be more susceptible to sleeplessness and anxiety, according to Wang et al. (45). The discrepancy may be caused by older medical staff members' worse health state in terms of nucleic acid collection and their decreased tolerance and capacity to adjust to cold and demanding work situations compared to those under the age of 40. Depression, anxiety and sleep disorders were negatively correlated with education level, that is, the higher the education level, the lower the incidence of depression, anxiety and sleep disorders. Among people suffering from serious physical health problems, those with higher education were less likely to experience symptoms of depression and anxiety than those with lower education. Higher levels of education help to regulate the relationship between psychological and stress responses, thus reducing the occurrence of depression and anxiety (46, 47). The findings showed that fear for infection was positively associated with depression, anxiety and sleep disorders, which was because the outbreak of COVID-19 is the largest public health emergency in China in the past decade (48). At the same time, the developing Omicron variant has a high incidence and expands quickly (49). In the short term, there were many more confirmed cases in Xi'an, which can add to their psychological strain.
By analyzing data from a binary logistic regression model, we discovered greater positive rates of depression and anxiety among the mobile cabin hospital collecting staff than at other collection locations in the current research. The results of the analysis revealed that the collection personnel had extended direct contact with the sampled subjects (positive patients) and that this increased both parties' risks of infection or cross-infection compared to those in the community or schools. According to other research, medical professionals working in high-risk situations are more likely to experience depression, anxiety, and sleep difficulties as well as higher levels of “fear about infection” than those working in low-risk conditions (50). Similar to door-to-door nucleic acid collection, floor-by-floor sampling by medical professionals raises the risk of aberrant psychological situations under heavy load and external environmental effects. As evidenced by the frequency and duration of nucleic acid collection, the intensity of nucleic acid collection is relatively high and overload is more common. Among them, 79.1% were overloaded. Previous research has shown that prolonged and intensive work tends to worsen medical personnel's mental health (51). In addition, the heavy workload may make medical staff more susceptible to illness and the shifts in the outside environment will have an impact on collectors' attitudes. Previous studies have shown that the weather to some extent affects the psychological two important factors are the season and outdoor time (52). In January, the temperature outdoor Xi'an was relatively low, and the collecting staff worked longer in the low-temperature environment, which was more likely to lead to negative emotions than the more comfortable indoor environment.
5. Conclusion
The public was poorly informed about the mental health implications of the SARS pandemic when it first appeared in China, and those who need it did not receive any specific psychological support. In public health emergencies, the intensity and duration of medical staff increases, the risk of infection increases, and they face greater physical strength and mental stress, which leads to the occurrence of depression and anxiety, which is seriously affected sleep quality (53, 54). Staff members who performing nucleic acid collection always get physically and mentally exhausted during a protracted period of epidemic preparation, particularly during line-points closed-loop management. The suggestions are as follows. First, the staff can engage in appropriate physical exercise during closed-loop management to reduce psychological stress and relieve psychological tension. Second, relevant management departments should strengthen human resources to improve detection efficiency, optimize nucleic acid collection process, reduce the workload of nucleic acid collection staff, and improve the working environment for nucleic acid collection. Finally, the mental health status of nucleic acid collection medical staff should be investigated regularly and corresponding psychological assistance measures should be taken to alleviate depression, anxiety and sleep disorders of nucleic acid collection personnel under closed-loop management.
6. Limitations
There are some limitations in this study. First, we used a practical sample strategy based on an online questionnaire survey, which made our sampling dependent on the online network environment and potentially prone to selection bias. Second, it has a cross-sectional design which limits the ability to interpret the causal relationships between the different variables in this study. The association and causality can be more accurately determined in randomized prospective research. Finally, since the scope of our study was restricted to Shaanxi Province and the sample size was modest, a bigger sample size is required for the validation of our findings.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The Ethics Committee of the Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine, Shaanxi Province, China approved this study (Ethical number: 2022-0516). The patients/participants provided their written informed consent to participate in this study.
Author contributions
MS implemented this study and was responsible for data collection and analysis and writing. XL, JY, and YK took part in the process of data collection. XH and ZL provided assistance in reviewing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Advantages and Interdisciplinary Support Program of Shaanxi University of Traditional Chinese Medicine (No. 2022XKZC05).
Acknowledgments
The authors want to thank all the physicians and nurses who participated and all the teachers and students who assisted in distributing questionnaires to the subjects and in undertaking data collection for the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. MunsterVJ, Koopmans M, Doremalen N, Riel D, Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. (2020) 382:692–4. doi: 10.1056/NEJMp2000929
2. Jamebozorgi MH, Karamoozian A, Bardsiri TI, Sheikhbardsiri H. Nurses burnout, resilience, and its association with socio-demographic factors during COVID-19 pandemic. Front Psychiatry. (2022) 12:803506. doi: 10.3389/fpsyt.2021.803506
3. Pfaller L. Theorizing the virus: abjection and the COVID-19 pandemic. Int JSociol Soc Policy. (2020) 40:821–9. doi: 10.1108/IJSSP-06-2020-0243
4. Safi-Keykaleh M, Aliakbari F, Safarpour H, Safari M, Tahernejad A, Sheikhbardsiri H, et al. Prevalence of postpartum depression in women amid the COVID-19 pandemic: a systematic review and meta-analysis. Int J Gynaecol Obstet. (2022) 157:240–7. doi: 10.1002/ijgo.14129
5. El-Shabasy RM, Nayel MA, Taher MM, Abdelmonem R, Shoueir KR, Kenawy ER. Three waves changes, new variant strains, and vaccination effect against COVID-19 pandemic. Int J Biol Macromol. (2022) 204:161–8. doi: 10.1016/j.ijbiomac.2022.01.118
6. He X, Hong W, Pan X, Lu G, Wei X. SARS-CoV-2 Omicron variant: Characteristics and prevention. Med Comm. (2020). 2:838–45. doi: 10.1002/mco2.110
7. Chinese Center for Disease Control and Prevention. (2022). Available online at: https://www.chin-acdc.cn/ (accessed June 28, 2022).
8. General Office of National Health Committee. Office of State Ad-ministration of Traditional Chinese Medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (Trial Version 9). (2022). Available online at: https://mp.weixin.qq.com/s/ngOikj7jrsa1yOksv-Bv3Q/ (accessed June28, 2022).
9. Jin Y-H, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. (2020) 7:4. doi: 10.1186/s40779-020-0233-6
10. Bai DS, Geng P, Wang ZD, Wang XL, Xu GR, Ye Q, et al. Practice and experience of regional medical center entrance linkage and closed-loop management under the wartime situation of the COVID-19 in China. Ann Transl Med. (2022) 10:112. doi: 10.21037/atm-22-61
11. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:43. doi: 10.1007/s11920-020-01166-z
12. Schenk EJ, Yuan J, Martel LD, Shi GQ, Han K, Gao X. Risk factors for long-term post-traumatic stress disorder among medical rescue workers appointed to the 2008 Wenchuan earthquake response in China. Disasters. (2017) 41:788–802. doi: 10.1111/disa.12222
13. Sheikhbardsiri H, Afshar PJ, Baniasadi H, Farokhzadian J. Workplace violence against prehospital paramedic personnel (City and Road) and factors related to this type of violence in Iran. J Interpers Violence. (2022) 37:NP11683–98. doi: 10.1177/0886260520967127
14. Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh W, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. (2004) 185:127–33. doi: 10.1192/bjp.185.2.127
15. Chen R, Chou KR, Huang YJ, Wang TS, Liu Y, Ho Y. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
16. Dong Z-Q, Ma J, Hao Y-N, Shen X-L, Liu F, Gao Y, et al. The social psychological impact of the COVID-19 epidemic on medical staff in China: a cross-sectional study. Eur Psychiatry. (2020) 63:e65. doi: 10.1192/j.eurpsy.2020.59
17. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
18. Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. (2020) 133:110102. doi: 10.1016/j.jpsychores.2020.110102
19. Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the coronavirus disease 2019 epidemic in China. Brain Behav Immun. (2020) 88:60–5. doi: 10.1016/j.bbi.2020.06.002
20. Sheikhbardsiri H, Khademipour G, Davarani ER, Tavan A, Amiri H, Sahebi A. Response capability of hospitals to an incident caused by mass gatherings in southeast Iran. Injury. (2022) 53:1722–6. doi: 10.1016/j.injury.2021.12.055
21. Aminizadeh M, Saberinia A, Salahi S, Sarhadi M, Jangipour Afshar P, Sheikhbardsiri H. Quality of working life and organizational commitment of Iranian pre-hospital paramedic employees during the 2019 novel coronavirus outbreak. Int J Healthc Manag. (2021) 15:36–44. doi: 10.1080/20479700.2020.1836734
22. Thompson B. Ten commandments of structural equation modeling. In:Grimm LG, Yarnold PR, , editors. Reading and Understanding MORE Mu-ltivariate Statistics. American Psychological Association. (2000) p. 261–83.
23. Yin L, Teklu S, Pham H, Li R, Tahir P, Garcia ME. Validity of the Chinese language patient health questionnaire 2 and 9: a systematic review. Health Equity. (2022) 6:574–94. doi: 10.1089/heq.2022.0030
24. Kocalevent RD, Hinz A, Brähler E. Standardization of the depressinscreener patient health questionnaire (PHQ-9) in the general population. Gen Hospital Psychiat, J. (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
25. Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. (2021) 279:473–83. doi: 10.1016/j.jad.2020.09.131
26. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
27. Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. (2016) 39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005
28. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
29. Zhang C, Zhang H, Zhao M, Li Z, Cook CE, Buysse DJ, et al. Reliability, validity, and factor structure of Pittsburgh sleep quality index in community-based centenarians. Front Psychiatry. (2020) 11:573530. doi: 10.3389/fpsyt.2020.573530
30. Zhang HH, Zhao YJ, Wang C, Zhang Q, Yu HY, Cheung T, et al. Depression and its relationship with quality of life in frontline psychiatric clinicians during the COVID-19 pandemic in China: a national survey. Int J Biol Sci. (2021) 17:683–8. doi: 10.7150/ijbs.56037
31. Farah NM, Saw Yee T, Mohd Rasdi HF. Self-Reported sleep qual-ity using the Malay version of the Pittsburgh sleep quality index (PSQI-M) in Malaysian adults. Int J Environ Res Public Health. (2019) 16:47–50. doi: 10.3390/ijerph16234750
32. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. (2020) 26:e923549. doi: 10.12659/MSM.923549
33. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
34. Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. (2020) 26:e924085. doi: 10.12659/MSMBR.924085
35. Huang CL, Weng SF, Wang JJ, Hsu YW, Wu MP. Risks of treat-ed insomnia, anxiety, and depression in health care-seeking physicians: a nationwide population-based study. Medicine. (2015) 94:e1323. doi: 10.1097/MD.0000000000001323
36. Qiu D, Yu Y, Li R-Q, Li Y-L, Xiao S-Y. Prevalence of sleep distu-rbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med J. (2020) 67:258–66. doi: 10.1016/j.sleep.2019.01.047
37. Zhang SX, Chen RZ, Xu W, Yin A, Dong RK, Chen BZ, et al. A systematic reviewand meta-analysis of symptoms of anxiety, depression, and insomnia in Spain in the COVID-19 crisis. Int J Environ Res Public Health. (2022) 19:1018. doi: 10.3390/ijerph19021018
38. Zhang SX, Batra K, Xu W, Liu T, Dong RK, Yin A, et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America – a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2022) 31:e23. doi: 10.1017/S2045796021000767
39. Chen J, Farah N, Dong RK, Chen RZ, Xu W, Yin J, et al. Mental health during the COVID-19 crisis in Africa: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:10604. doi: 10.3390/ijerph182010604
40. Zhang SX, Miller SO, Xu W, Yin A, Chen BZ, Delios A, et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur J Psychotraumatol. (2022) 13:2000132. doi: 10.1080/20008198.2021.2000132
41. Krupa S, Filip D, Medrzycka-Dabrowska W, Lewandowska K, Witt P, Ozga D. Sleep disorders among nurses and other health care workers in Poland during the COVID-19 pandemic. Appl Nurs Res. (2021) 59:151412. doi: 10.1016/j.apnr.2021.151412
42. Pappa S, Chen J, Barnett J, Chang A, Dong RK, Xu W, et al. A systematic review and meta-analysis of the mental health symptoms during the Covid-19 pandemic in Southeast Asia. Psychiatry Clin Neurosci. (2022) 76:41–50. doi: 10.1111/pcn.13306
43. Chen X, Chen J, Zhang M, Dong RK Li J, Dong Z, et al. Meta-regression on the heterogenous factors contributing to the prevalence of mental health symptoms during the COVID-19 crisis among healthcare workers. Front Psychiatry. (2022) 13:833865. doi: 10.3389/fpsyt.2022.833865
44. Heidarijamebozorgi M, Jafari H, Sadeghi R, Sheikhbardsiri H, Kargar M, Amiri Gharaghani M. The prevalence of depression, anxiety, and stress among nurses during the coronavirus disease 2019: a comparison between nurses in the frontline and the second line of care delivery. Nurs Midwifery Stud. (2021) 10:188–93. doi: 10.4103/nms.nms_103_20
45. Wang LQ, Zhang M, Liu GM, Nan SY, Li T, Xu L, et al. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatr Res. (2020) 129:198–205. doi: 10.1016/j.jpsychires.2020.07.008
46. Di Novi C, Leporatti L, Montefiori M. The role of education in psychological response to adverse health shocks. Health Policy. (2021) 125:643–50. doi: 10.1016/j.healthpol.2021.02.006
47. Hashmi R, Alam K, Gow J. Socioeconomic inequalities in mental health in Australia: explaining life shock exposure. Health Policy. (2020) 124:97–105. doi: 10.1016/j.healthpol.2019.10.011
48. Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci J. (2012) 66:353–60. doi: 10.1111/j.1440-1819.2012.02336.x
49. Ren SY, Wang WB, Gao RD, Zhou AM. Omicron variant (B.1.1.529) of SARS-CoV-2: mutation, infectivity, transmission, and vaccine resistance. World J Clin Cases. (2022) 10:1–11. doi: 10.12998/wjcc.v10.i1.1
50. Koh D, Lim MK, Chia SE, Ko SM, Qian F, Ng V, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med Care. (2005) 43:676–82. doi: 10.1097/01.mlr.0000167181.36730.cc
51. Abarghouei MR, Sorbi MH, Abarghouei M, Bidaki R, Yazdanpoor S. A study of job stress and burnout and related factors in the hospital personnel of Iran. Electron Physician. (2016) 8:2625–32. doi: 10.19082/2625
52. Keller MC, Fredrickson BL, Ybarra O, Côté S, Johnson K, Mikels J, et al. A warm heart and a clear head. The contingent effects of weather on mood and cognition. Psychol Sci. (2005) 16:724–31. doi: 10.1111/j.1467-9280.2005.01602.x
53. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. (2007) 52:241–7. doi: 10.1177/070674370705200406
Keywords: COVID-19, closed-loop management, RT-PCR test, nucleic acid collection, psychological status, influencing factors
Citation: Sun M, Li X, Yao J, Huang X, Kang Y and Li Z (2023) Psychological status of medical staff dedicated to nucleic acid collection in COVID-19 epidemic during closed-loop management: A cross-sectional study. Front. Public Health 11:1131971. doi: 10.3389/fpubh.2023.1131971
Received: 26 December 2022; Accepted: 21 February 2023;
Published: 10 March 2023.
Edited by:
Stephen X. Zhang, University of Adelaide, AustraliaReviewed by:
Roel Van Overmeire, Vrije University Brussels, BelgiumHojjat Farahmandnia, Kerman University of Medical Sciences, Iran
Copyright © 2023 Sun, Li, Yao, Huang, Kang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaowei Li, bGl4aWFvd2Vpd2RAMTI2LmNvbQ==
 Mingzhu Sun
Mingzhu Sun Xiaowei Li
Xiaowei Li Jie Yao1
Jie Yao1