- 1Addiction Science Center, College of Public Health, East Tennessee State University, Johnson City, TN, United States
- 2College of Public Health, East Tennessee State University, Johnson City, TN, United States
- 3Institute of Agriculture, University of Tennessee, Knoxville, Knoxville, TN, United States
Background: The U.S. has experienced exponential growth in overdose fatalities over the past four decades and more than 22 million people are currently living with a substance use disorder (SUD). While great strides have been made in advancing the science of SUD prevention and treatment, proven programs and interventions are not commonly disseminated at scale in impacted communities. The U.S. Cooperative Extension System (Extension) has been recognized as a valued partner in addressing SUD in communities. Federal funding supporting Extension's response to the opioid epidemic reached $35 million in 2021 primarily through two grant programs: the United States Department of Agriculture's (USDA) Rural Health and Safety Education program; and the Substance Abuse and Mental Health Services Administration (SAMHSA) Rural Opioid Technical Assistance (ROTA) grants. The primary objective of this scoping review was to identify the range of Extension activities aimed at mediating substance misuse.
Methods: Authors utilized the PRISMA-SCR model to complete this scoping review. Due to the nature of Extension work and the expectation that few activities would be cited in the peer-reviewed literature, the scoping review included a search of peer-reviewed databases, Extension websites for each state and U.S. territory, and the utilization of a web search engine. Upon initial analysis of records returned, authors noted a discrepancy between results returned and the number of states receiving ROTA grants. Thus, authors supplemented the PRISMA-SCR review protocol with a systematic procedure for investigating ROTA funded activities not readily apparent in the peer-reviewed or grey literature.
Results: A total of 87 records met inclusion criteria. Findings included seven peer-reviewed articles and 80 results from the grey literature. An additional 11 ROTA grantees responded to requests for information regarding state level activities.
Conclusions: Nationwide, Extension has scaled multiple efforts to address SUD operating through a loose confederation of organizations connected to the land-grant system. Most activities are funded by federal grants and focus on state-sponsored training and resource sharing. The volume of effort is significant, however, implementation at the community-level has been slow. Significant opportunities exist for local adoption of evidence-based practices aimed at mitigating SUD.
Introduction
Overdose fatalities in the U.S. have continued to rise over the past four decades (1). Substance use and misuse are contributing to an escalating burden of disease leading to premature death and disability (2) and a host of other associated harms including childhood and family trauma (3), excessive health care costs (4), and justice system involvement (5). An estimated 174 people die each day in the U.S. from a drug-related overdose (1) and more than 22 million people are currently living with a substance use disorder (SUD) (6). In April of 2021, in the midst of the COVID-19 pandemic, the U.S. surpassed 100,000 drug-related deaths in a 12-month period for the first time in history (7).
Concurrent to these year-on-year increases in overdose fatality, numerous advances have been made in the science of SUD prevention and treatment. Unfortunately, many of these proven programs and interventions are not disseminated to scale in impacted communities to counter the mounting burden of disease. Cited barriers to the dissemination of evidence-based programs and policies include poor translation and clarity of scientific studies (8), perceived patient factors, limited community-level referral sources (9), stigma, and other systemic barriers (10). Moreover, communities most affected by SUD, such as those in rural areas or the Appalachian region, may also be communities with limited resources, and thus, the effective dissemination and implementation of preventative interventions may prove more challenging.
The Cooperative Extension System (Extension) is part of the land grant university system in the United States. Extension is a nationwide network of local offices affiliated with and partially supported by land grant institutions with offices in or near most U.S. counties (11). Local Extension offices house teams of educators who offer educational outreach and programs in several areas, including agriculture and natural resources, 4-H and youth development, family and consumer sciences, and community economic development. Extension efforts are informed by local priorities and needs and shaped by programmatic resources available from the sponsoring land grant institution. Extension personnel serve as vital partners across multiple community-based efforts and more recently have been recognized as valued partners in addressing SUD and related issues impacting families and communities (12). To that end, the Extension Opioid Crisis Response Workgroup was formed in February 2018 at the recommendation of the Extension Committee on Organization and Policy and following the declaration of the opioid crisis as a national public health emergency in 2017 (13). The purpose of this group was to identify and organize resources to help Extension play a clear and intentional role in addressing the opioid crisis and general behavioral health challenges (14). Moreover, a 2018 survey of national Extension leaders indicated that an overwhelming majority agreed that Extension should play a role in reducing opioid misuse and overdose in their respective states, but <24% agreed their Extension System had capacity to respond to the epidemic (14).
Federal funding supporting Extension's response to the opioid epidemic exceeded $35 million between 2017 and 2021 (15, 16). This funding originated primarily through the United States Department of Agriculture's (USDA) Rural Health and Safety Education program and the Substance Abuse and Mental Health Services Administration (SAMHSA) Rural Opioid Technical Assistance (ROTA) grants. Additional funding was also provided through USDA's Children, Youth and Families at Risk grant program (17). For nearly 6 years, Federal funding has prioritized Extension projects and trainings that address the opioid crisis, however, the full scope of this work and related outcomes is unknown.
The primary objective of this scoping review was to identify the full range of Extension activities aimed at mediating opioid and substance misuse from 2016–2022. Furthermore, the review may help to elucidate opportunities for the expansion of existing programs and assets or fill gaps and implement programs in areas that are not currently working in this space, specifically, those in rural communities and those most impacted by SUD.
Materials and methods
Study design and search strategy
This scoping review was conducted from February through July of 2022 and was informed by the PRISMA-SCR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) model (18). Due to the nature of Extension work, authors anticipated that few activities would be cited in the traditional peer-reviewed literature, thus, the review included searches within peer-reviewed databases and within one standard web search engine. First, authors used combinations of the following search terms to query the peer-reviewed literature via PubMed, EBSCOhost, ProQuest, Elsevier, and JSTOR: opioid, cooperative extension, drug, substance, and substance abuse. Authors also utilized the OneSearch platform hosted by the East Tennessee State University's Sherrod Library to expand the search to additional databases. Additional filters applied during the search included: (1) peer-reviewed, (2) full article, and (3) 2016 and newer.
Following a search of the peer-reviewed literature, authors queried Extension websites for each state and U.S. territory and utilized the Google search engine using combinations of the following key terms: opioid, cooperative extension, drug, substance, and substance abuse. Additional filters included records that were written in English and published between 2016 and 2022. Upon conclusion of the initial search and saturation of the traditional literature and web findings, a preliminary review of records excluded duplicates and records or titles that were not connected to Cooperative Extension and/or were not focused on SUD or opioid related topics. In this preliminary review, records were included only if they met all of the following criteria: (1) connection to Extension work; (2) focus on programs or activities designed to mediate opioid or substance misuse; (3) written in English; (4) and published between the years of 2016 and 2022. Each included record was then documented in an Excel spreadsheet and sorted into two categories: peer-reviewed and web results. Authors then classified the web results as press releases, news articles, Extension blogs or feeds, impact statements, and online videos or online training series, and defined these records for the purposes of this review as “grey literature” (19).
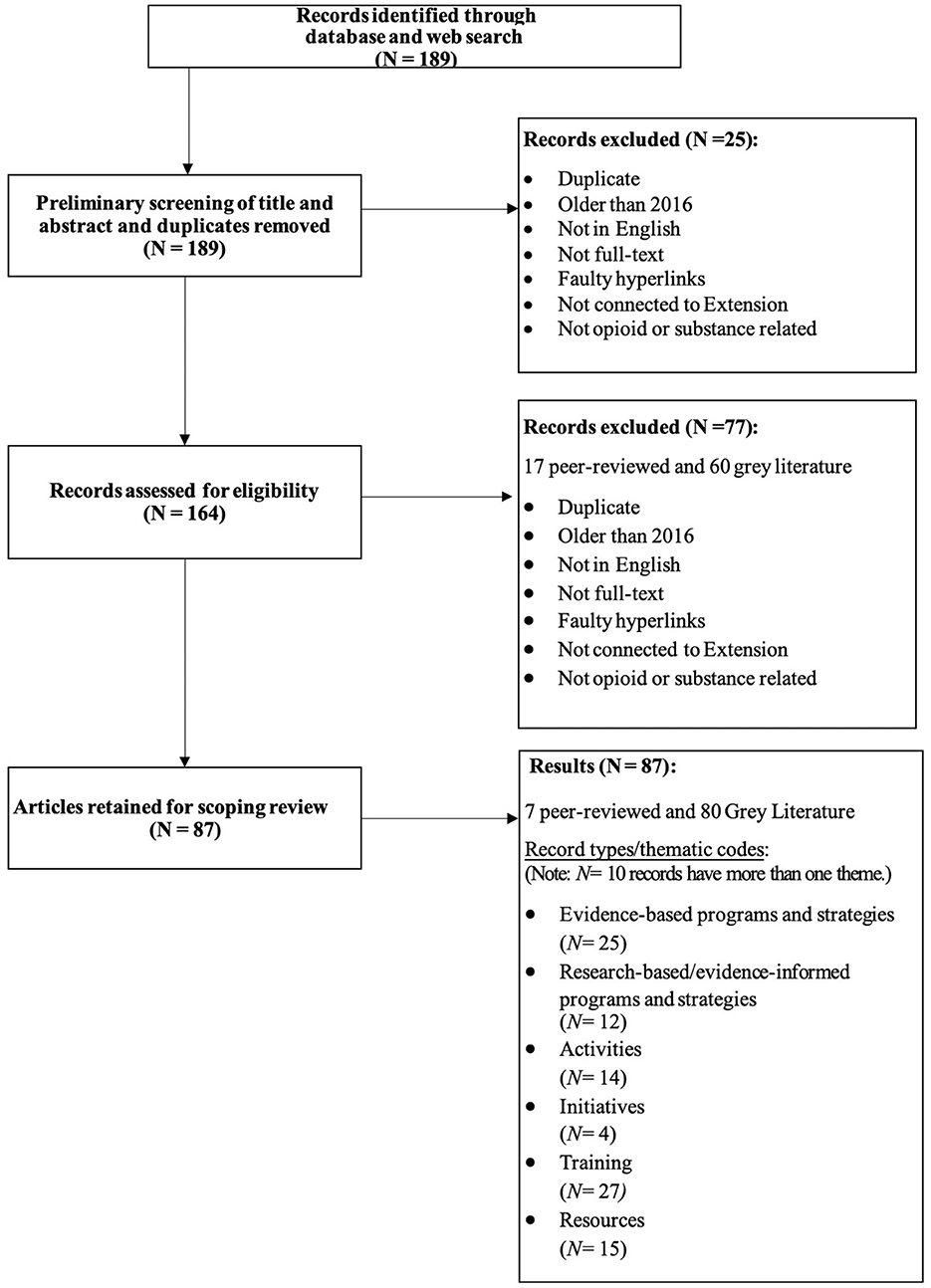
A pair of reviewers then conducted a critical analysis of each record to ensure that each still met the inclusion criteria. Reviewers also began coding records into themes or result “types.” The reviewing team met on three separate occasions to discuss discrepancies in the thematic codes and any newly excluded results. The Excel spreadsheet was updated following each meeting. Upon the third review, a final set of six themes was established for the grey literature and included: evidence-based programs and strategies, research-based and evidence-informed programs and strategies, activities, initiatives, training, and resources. Figure 1 illustrates the comprehensive review process.
Supplemental analysis
Upon conclusion of the records review process, the authors identified a notable discrepancy in the number of records returned as compared to the number of states that received opioid focused grant funds. Twenty-three states received ROTA funding during the years 2016-2022, however, only 9 records identified this funding explicitly via the PRIMSA-SCR informed scoping review process. Thus, the authors agreed to supplement the PRISMA-SCR protocol with a systematic post-hoc procedure for investigating ROTA funded activities not readily apparent in the peer-reviewed or grey literature and to identify the full range of Extension activities aimed at mediating opioid and/or substance misuse. The authors developed a standard email inquiry and interview guide and then contacted all ROTA-funded state project directors with a request for a brief telephone interview to confirm project activities and scope utilizing a pre-defined set of questions.
Results
The initial search of the peer-reviewed and grey literature resulted in 189 returned records. Following a preliminary review to identify duplicates and titles that did not meet inclusion criteria, 25 records were excluded, and 164 records were retained (22 peer-reviewed and 142 web/grey literature). The next stage in the process included a critical appraisal of each remaining record by two of this paper's authors. This phase included three iterations of review and thematic coding of each record by type. An additional 77 records that did not meet inclusion criteria were removed in this phase of the review. Upon completion of the full review process, final results included 87 records (80 web/grey literature and 7 peer-reviewed). Moreover, ten (9) records found in the grey literature search overlapped across multiple themes.
Peer-reviewed results
The seven peer-reviewed articles included were thematically categorized as: (1) Conceptual-System - focused on the Cooperative Extension System, capacity, and potential as it applies to SUD prevention, education, or behavioral health; (2) Interventions - described evidence-based interventions, approaches, or results; and (3) Coalitions- focused on coalition-based approaches and support; (4) Needs Assessment; and (5) Supplemental.
Two of the seven peer-reviewed results were coded as Conceptual-System. The first provided a conceptual framework for Extension's response to the opioid crisis with examples of Extension professionals as public health agents bringing practical, evidence-based solutions to communities to combat increases in poly-substance use (20). The second provided a framework for science-driven behavioral health translation to more effectively address substance misuse through the Extension system (21).
Two results were coded as Interventions. One record focused on the evidence-based PROSPER system (PROmoting School-Community-University Partnerships to Enhance Resilience created for implementation through Cooperative Extension (22). A second article described a multi-state education and outreach effort including opioid misuse prevention programming in rural communities (23).
A fifth record from the traditional literature focused on coalition-based approaches as a promising approach for addressing disparities in rural health such as substance misuse (24). The sixth record was categorized as a Needs Assessment and described community-focused needs assessment conducted as part of the PROMISE (Preventing Opioid Misuse in the SouthEast) initiative (25). The final peer-reviewed article was deemed Supplemental and included in this review due to the broad focus on 4-H Healthy Living programs, which are widely implemented through Extension across the U.S. This article described an evaluation study reviewing 32 promising health-related positive youth development programs, some of which included prevention of alcohol, tobacco and other drug use (26).
Grey literature results
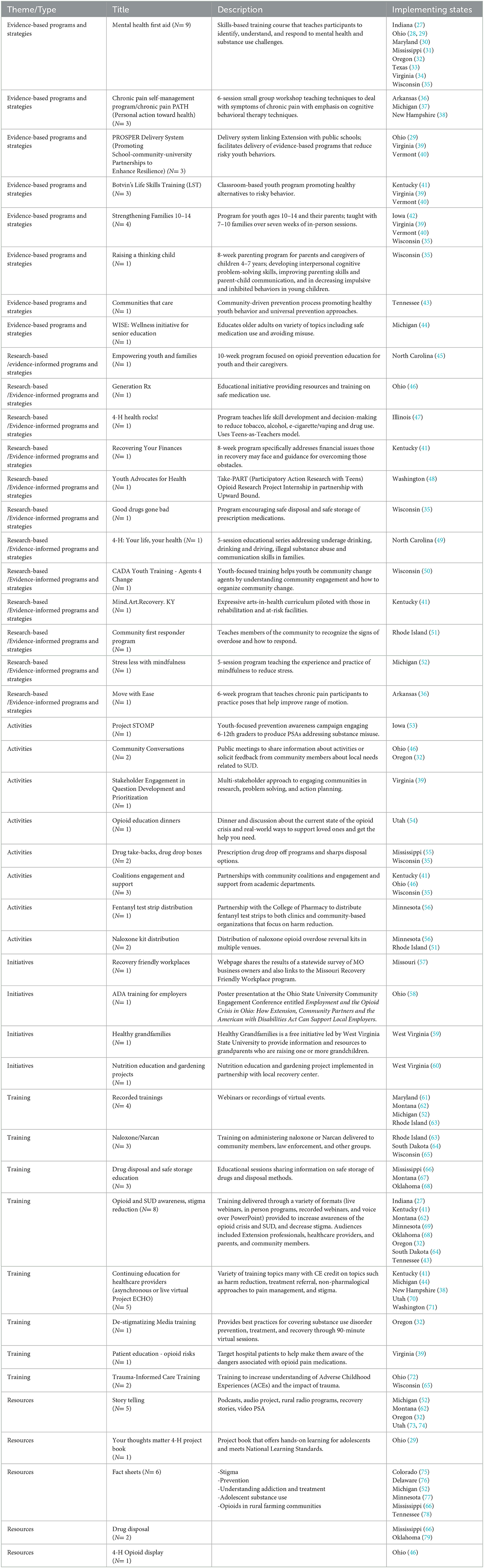
A total of 80 records were included in the grey literature results. Sources meeting inclusion criteria were representative of Extension in nearly every state except Arizona, Connecticut, Maine, New Jersey, and South Carolina. Authors categorized the grey literature into six coded themes: Evidence-based Programs and Strategies, Research-based and Evidence-Informed Programs, and Strategies. Activities, Initiatives, Training, and Resources. Most states' opioid response activities included a combination of efforts across categories. The paragraphs below summarize findings by thematic code. Table 1 contains a more detailed description of each result including states implementing and all related citations.
Evidence-based programs and strategies
The PRISMA-SCR informed search located eight evidence-based programs/strategies being implemented through the Extension system to address aspects of opioid misuse. Records for eight states implementing Mental Health First Aid were found. States implementing the PROSPER (PROmoting School-community-university Partnerships to Enhance Resilience) model also implemented two evidence-based programs as part of the PROSPER delivery system, one youth- and one family-focused program. Most often Botvin's Life Skills Training and Strengthening Families 10-14 were paired in PROSPER states. Several states offered chronic pain programs including Chronic Pain PATH and the Chronic Pain Self-Management Program, reaching underserved adults in rural areas.
Research-based and evidence-informed programs and strategies
The grey literature also returned 14 research-based and evidence-informed programs implemented through Extension. Programs ranged from multi-week, multi-session education programs for youth and families to training community members in opioid overdose response. Content included nutrition education, financial management, and physical activity. Some incorporated community engagement approaches, while others focused primarily on increasing knowledge or awareness.
Activities
Search results also demonstrated a range of activities that have been implemented through Extension in the U.S., including naloxone kit and fentanyl test strip distribution, awareness-raising community dinners and other community forums, and support for coalition-engaged approaches. Activities are sometimes paired with other educational strategies, like providing training on naloxone use prior to providing naloxone kits. Activities are often conducted with partner organizations (e.g., drug takeback events or drop box placement in collaboration with law enforcement).
Initiatives
The scoping review process yielded two records specifically focused on the workplace. The Recovery Friendly Workplaces initiative implemented in one state helps employers support people affected by SUD and those in recovery. This initiative focuses on creating a workplace culture that promotes employee safety, and health and wellbeing while reducing stigma and providing recovery resources. Another state's initiative focused on employer training dedicated to the Americans with Disabilities Act, including protections for those in recovery. Moreover, this review found several projects offering existing subject-matter expertise and resources to those in recovery and their families through local organization partnerships. Two states conducted nutrition education and implemented gardening projects in partnership with local recovery centers. Finally, as parenting and family life education are traditional areas of Extension outreach, the Healthy Grandfamilies initiative extends this focus to include the provision of information and resources to grandparents who are raising one or more grandchild due to a family members' challenges with substance use disorder.
Training
Results in this category indicated that training was provided on a range of topics with varied target audiences using synchronous, asynchronous, and hybrid methods. Training topics included administering naloxone to community members, law enforcement, and other groups. SUD and opioid awareness topics, including stigma reduction, were also delivered through a variety of formats (live webinars, in person programs, recorded webinars). Audiences included Extension professionals, healthcare providers, parents, and community members. Some states provided continuing education for healthcare providers, both asynchronously and through live virtual sessions utilizing Project ECHO. Training topics included trauma-informed care and other more targeted training, such as a De-stigmatizing Media Training that provides best practices for covering SUD prevention, treatment and recovery. Finally, one state's patient education program addresses opioid risk and provides additional education sessions on safe storage and disposal of drugs.
Resources
A number of states produced a range of educational resources to raise awareness and reduce stigma. Several educational video series offered introductory information about substance use for the public, and other resources included personal stories of people impacted by substance misuse. Recovery resources were also provided including podcasts, audio recordings, videos, and one rural radio program. Web and print publications covered topics including prevention, stigma, understanding addiction and treatment, adolescent substance use, and opioids in farming communities. Some resources supplemented training topics such as prescription drug disposal or resources aimed at youth audiences such as displays and 4-H project books. Social media marketing messages were also developed and included in one statewide campaign.
Supplementary findings from grantee interviews
As discussed previously, the authors of this paper universally agreed that the nine records returned via the PRISMA-SCR search process were insufficient to illustrate the contributions of the 23 states funded by ROTA grants during the six-year time frame for this search. Eleven states responded to the request for interview and the grant program director, or a designee, participated in a 30-min interview by phone or Zoom to answer the pre-defined list of questions. Responses frequently aligned with the six previously identified grey literature themes. The following responses were consistent with the evidence-based programs and strategies theme: Question, Persuade, Refer in Oregon; WeCOPE (Connecting with Our Positive Emotions) in Wisconsin, and CRAFT: Community Reinforcement and Family Training in South Dakota. Virginia also implemented two evidence-based programs: Botvin's Life Skills Training Parent Program and Too Good for Drugs, a universal K-12 prevention education program. Research-based/evidence-informed programs found via the supplementary interview process included RELAX: Alternatives to Anger in Michigan, and Learning to Breathe, a mindfulness curriculum for youth, in Wisconsin.
A unique approach implemented in Oklahoma included partnerships with rural fire departments for naloxone education and distribution and aligned with the Initiatives theme. This state relied upon coalition engagement and hired field faculty specifically dedicated to opioid response. A Virginia initiative included hiring regional coordinators to work with coalitions in multiple counties. Several interviewees revealed that their project approaches evolved over time when new data became available thereby informing improvements to their funded strategies. ROTA project interviewees also described newly developed Training tools, such as Montana's Prescription Opioid Toolkit, a 5-module packaged curriculum for Extension field agents use in communities.
Discussion
This scoping review is the first, to our knowledge, to compile efforts of the U.S. land-grant university Extension system to address the opioid crisis. The results offered in this PRISMA-SCR informed review (18) highlight a ramp-up of Extension activities following the 2016 shift in federal funding priorities. However, continued and expanded engagement of Extension personnel is still warranted given the far-reaching impacts of the opioid epidemic and ongoing challenges of SUD and overdose fatality for families and communities. Expanded engagement may be particularly impactful in rural areas disproportionately affected by SUD and where Extension may serve as an active partner in agricultural activity, and thus, may have increased credibility when engaging in community-based SUD initiatives.
University-generated publicity announcing federal grant awards represented a large proportion of the grey literature sources identifying opioid related Extension activities. This information underscores the critical role of federal funding priorities in driving the initiation or expansion of SUD related prevention and recovery activities in many states. Authors are unable to speculate whether states would have pursued the same volume of activities absent external funding support, and to our knowledge, there no studies investigating this topic. Given Extension's limited capacity and resources to address SUD prior to funding availability, it seems unlikely this range of activities would have occurred. The combination of funded activities involving both mental health and SUD illustrates how specific states repurposed or reframed existing programs and traditional Extension content (e.g., stress coping, mindfulness, parenting) to reach new audiences. This approach was likely influenced by evolving ROTA funding requirements which required integration of mental health and SUD.
Few partnerships between Extension and non-Extension community partners were identified in the initial scoping review process. However, findings gleaned through supplemental interviews with ROTA grantees confirmed collaborative efforts and state/regional agency partnerships in opioid response. For example, a social marketing project developed and tested through an Extension partnership with other university academic units primed a larger campaign disseminated by a state agency. This social marketing content originated through Extension effort but would have been unidentified using PRISMA-SCR methods. Collaboration, while essential to opioid response efforts, may have made identifying Extension contributions more difficult. This, however, is probably a necessary by-product of true collaboration where accomplishing the work is more important than naming the headlining or sponsor agency.
Moreover, interviews with ROTA grantees provided context for opioid-focused activities that could not have been obtained through traditional scoping review methods. For example, partnerships with state agencies and community organizations not apparent through grant award announcements and project websites were vital to understanding overall project implementation. These interviews also provided information on implementation processes and barriers beyond the scope of this review but worthy of further exploration. Many interviewees found it difficult to attribute specific activities to a particular funding source or funding period. A series of prerequisite grant funding determined state's initial eligibility for ROTA funding; thus, interrelated grant funded activities were inherent. Work under these funding sources intersected and became interwoven, suggesting movement toward institutionalizing opioid and SUD related activities as opposed to simply adhering to grant timelines and objectives. Implementation of opioid-focused activities that was not required by grant funding also suggests increased acceptance of Extension's role in opioid misuse prevention and other SUD related topics.
Extension is typically located in Colleges of Agriculture within land grant universities. This traditional organizational structure and related subject-matter expertise of the Extension-affiliated faculty specialists may limit the capacity to support work occurring locally. This structure may also hamper visibility of activities addressing SUD by making efforts harder to recognize within the larger university system. A concentrated effort by Federal funding entities to develop formal dissemination strategies for grant-funded outcomes at the local level could address this challenge. This search found limited but intentional linkages between multiple academic units working to impact SUD. Such approaches bridged pharmacy, social work, nursing, and behavioral science disciplines to enhance activities beyond Extension's traditional subject matter focus and thereby potentially expanding overall impact at the organizational and systems levels. Finally, partnerships with external entities, such as state agencies and state or local non-profit organizations, appeared to broaden the reach of Extension activities, thereby strengthening the collective response of the Extension System to the opioid crisis.
Limitations
The PRIMSA-SCR method created a foundation from which to initiate the scoping review, however, it was insufficient to achieve the author's goals, thus requiring the adoption of supplemental methodology (e.g., state-level interviews) to identify the range of Extension activities aimed at mediating substance misuse. Moreover, the inclusion criteria for this search, while appropriate given the focus of this scoping review, may have excluded relevant results broadly related to SUD. Initial shifts in federal funding priorities for Extension specifically related to the opioid crisis, thus, authors may have prioritized data sources specific to opioid misuse. Records returned limited grey literature results beyond those described in the initial funding announcements. However, direct contact with ROTA grantees revealed a range of activities and resources. Thus, a key limitation in our search may be characteristic of the organization of focus (Extension) whereby associated strategies for promotion and marketing may result in infrequent website updates and lack of keywords for search engine optimization. Further limitations are also inherent within the U.S. Extension System. For example, publication in peer-reviewed journals, while standard for disseminating knowledge in academia, is less common among Extension professionals, particularly those focused on local implementation. Furthermore, time parameters for the search may have limited search returns and these results can only be considered current through July 2022. Time needed to produce results, COVID-19 implementation delays, and long wait times for peer-reviewed publication may also explain why few traditional journal articles were found.
Finally, the search methods utilized in this review may have unintentionally excluded efforts of historically black and Native American tribally controlled land-grant institutions. Federal legislation established or extended land-grant status to these institutions in 1890 and 1994, respectively, and they share the Extension mission (80). While selected cooperative activities between land-grant universities were found, particularly in states with tribal colleges, we acknowledge that results may not be fully representative of all work occurring, particularly through institutions with university names not including, “cooperative extension,” or other specified search terms.
Conclusions
This is, to our knowledge, the first review of its kind to provide a snapshot of Extension's efforts to address the opioid and SUD crisis in the U.S. While these results may not include every Extension activity that occurred during the specified time frame, Extension has significantly increased efforts to address the opioid crisis and related challenges operating through a loose confederation of organizations that are part of the land-grant system. Numerous training activities, resources, and toolkits have been developed at the state level through funding by federal grant dollars. The volume of effort is significant. Continued efforts and expanded partnerships, particularly for community-level work, are needed to combat the ongoing epidemic of opioid and substance misuse across the country.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AH contributed to the conception and design of the study, reviewed and coded all search results, assisted with writing the introduction, constructed Table 1 and edited Figure 1, inserted all citations, and was responsible for combining, and proofreading all sections of the manuscript. KR conducted the initial web and peer-reviewed literature search, built the excel file for co-authors to review, prepared Figure 1, and assisted with writing results. LW was the Principal Investigator of the Rural Health and Safety Education project (grant no. 2019-46100-30276) from the USDA that funded this work, contributed to the conception and design of the study, reviewed and coded all search results, assisted with writing the introduction, assisted with compiling the results, drafted the discussion, and conclusion sections. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by Rural Health and Safety Education (grant no. 2019-46100-30276) from the USDA National Institute of Food and Agriculture.
Acknowledgments
The authors would like to express our gratitude to Elizabeth Childress, QMHP, RPRS, CPRS VA, and PRSS TN. Elizabeth assisted with the colossal task of initiating all citations in the online citation management system and preparing the final draft of Figure 1.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. (2018) 21:361. doi: 10.1126/science.aau1184
2. Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, White WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug Alcohol Depend. (2017) 181:162–9. doi: 10.1016/j.drugalcdep.2017.09.028
3. Giano Z, Wheeler DL, Hubach RD. The frequencies and disparities of adverse childhood experiences in the US. BMC Public Health. (2020) 1:1327. doi: 10.1186/s12889-020-09411-z
4. Ashford R, Brown AM, Ryding R, Curtis B. Building recovery ready communities: the recovery ready ecosystem model and community framework. Addict Res Theory. (2019) 1:11. doi: 10.1080/16066359.2019.1571191
5. Moore KE, Oberleitner L, Pittman BP, Roberts W, Verplaetse TL, Hacker RL, et al. The prevalence of substance use disorders among community-based adults with legal problems in the US. Addict Res Theory. (2020) 28:165–72. doi: 10.1080/16066359.2019.1613524
6. Substance Abuse Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration (2019). Retrieved from: https://www.samhsa.gov/data/
7. Centers for Disease Control and Prevention National Center for Health Statistics. Drug Overdose Deaths in the U.S. Top 100,000 Annually. (2021). Available online at: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm (accessed June 17, 2022).
8. Correa VC, Lugo-Agudelo LH, Aguirre-Acevedo DC, Contreras JAP, Borrero AMP, Patiño-Lugo DF, et al. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: a systematic metareview. Health Res Policy Syst. (2020) 18:74. doi: 10.1186/s12961-020-00588-8
9. Lowenstein M, Kilaru A, Perrone J, Hemmons J, Abdel-Rahman D, Meisel ZF, et al. Barriers and facilitators for emergency department initiation of buprenorphine: a physician survey. Am J Emerg Med. (2019) 37:1787–90. doi: 10.1016/j.ajem.2019.02.025
10. Grella CE, Ostile E, Scott CK, Dennis M, Carnavale J. A scoping review of barriers and facilitators to implementation of medications for treatment of opioid use disorder within the criminal justice system. Int J Drug Policy. (2020) 81:102768. doi: 10.1016/j.drugpo.2020.102768
11. USDA National Institute of Food and Agriculture. Cooperative Extension System. Available online at: https://www.nifa.usda.gov/about-nifa/how-we-work/extension/cooperative-extension-system (accessed December 10, 2022).
12. Office of National Drug Control Policy. Rural Community Action Guide: Building Stronger, Healthy, Drug-Free Rural Communities. (2020). Available online at: https://www.usda.gov/sites/default/files/documents/rural-community-action-guide.pdf (accessed December 10, 2022).
13. Alexander LM, Keahey D, Dixon K. Opioid use disorder: a public health emergency. JAAPA. (2018) 31:10. doi: 10.1097/01.JAA.0000545072.09344.ee
14. Washburn LT, Franck KL, Upendram S, Yenerall JN. Cooperative extension professionals' knowledge and attitudes toward the opioid epidemic: implications for capacity development and outreach. Front Psychiatry. (2022) 1795. doi: 10.3389/fpsyt.2022.958335
15. United States Department of Agriculture. Current Research Information System (CRIS) (2022). Available online at: https://cris.nifa.usda.gov (accessed December 10, 2022).
16. Substance Abuse and Mental Health Services Administration. Rural Opioids Technical Assistance Grants Notice of Funding Opportunity. (2018). Available online at: https://www.samhsa.gov/grants/grant-announcements/ti-19-010
17. USDA National Institute of Food and Agriculture. Children, Youth and Families at Risk (CYFAR). Available online at: https://www.nifa.usda.gov/grants/programs/4-h-positive-youth-development/4-h-access-equity-opportunity/children-youth-families-risk-cyfar (accessed December 10, 2022).
18. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
19. Kamei F, Pinto G, Wiese I, Ribeiro M, Soares S. What evidence we would miss if we do not use grey literature? in Proceedings of the 15th ACM/IEEE International Symposium on Empirical Software Engineering and Measurement (ESEM). (2021). p. 1–11.
20. Bowie M. A Conceptual Model for Cooperative Extension Professionals as Public Health Change Agents: Three Essays on the Cooperative Extension Program, the Opioid Epidemic, and Substance Use Disorder Needs of Rural Georgia: University of Georgia. (2020). Available online at: https://marylandrota.org/wp-content/uploads/2021/04/1.3-SPR-Poster.pdf
21. Spoth R, Franz N, Brennan A. Strengthening the power of evidence-based prevention in cooperative extension: a capacity-building framework for translation science-driven behavioral health. Proc Child Youth Care Forum. (2021). doi: 10.1007/s10566-020-09559-0
22. Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Trudeau L, et al. delivery of universal preventive interventions with young adolescents: long-term effects on emerging adult substance misuse and associated risk behaviors. Psychol Med. (2017) 47:2246–59. doi: 10.1017/S0033291717000691
23. Hoffman MS, Ramsay-Seaner K, Letcher A, Heckmann C. Collaboration is key: Implications for successful rural opioid misuse prevention programming. J Rural Mental Health. (2021) 45:198. doi: 10.1037/rmh0000184
24. Ken-Opurum J, Lynch K, Vandergraff D, Miller DK, Savaiano DA. A mixed-methods evaluation using effectiveness perception surveys, social network analysis, and county-level health statistics: a pilot study of eight rural Indiana community health coalitions. Eval Program Plann. (2019) 77:101709. doi: 10.1016/j.evalprogplan.2019.101709
25. Steen JK, Robertson MN, Seitz H, Downey L, Hardman A, Buys D. Addressing the Opioid Epidemic: Defining Cooperative Extension's Role. J Ext. (2021) 57:10.
26. Peterson DJ, Downey LH, Leatherman J. Informing youth health and well-being programs: a national 4-H healthy living evaluation study. J Youth Dev. (2018) 13:212–36. doi: 10.5195/jyd.2018.605
27. Purdue University Extension. Purdue Extension Offers A Substance Use Education Video Series. (2022). Available online at: https://extension.purdue.edu/opioids/ (accessed December 10, 2022).
28. Ohio State University Extension College of Food and Environmental Sciences. Opioid Epidemic in Ohio – Extension in Action. (2022). Available online at: https://extension.osu.edu/about/resources/opioid-epidemic-ohio-%E2%80%93-extension-action#:~:text=Ohio%20is%20considered%20%22ground%20zero,prevention%20of%20opioid%20abuse%20statewide (accessed December 10, 2022).
29. Dellifield J. Utilizing Cooperative Extension to Leverage Effective Community Education. Proceedings of the American Public Health Association Conference; 2019. Philadelphia, PA (2022). Available online at: https://apha.confex.com/apha/2019/meetingapp.cgi/Session/58309
30. Kim J, Hurtado GA, Munoz B J, Randolph S, Bonilla L. Increasing Rural Capacity to Identify, Respond to, and Address Opioid-related Needs for Prevention through Extension Research and Outreach. University of Maryland Extension. (2021).
31. Mississippi State Extension. Mental Health First Aid. (2022). Available online at: http://extension.msstate.edu/health/the-promise-initiative/mental-health-first-aid (accessed December 10, 2022).
32. Oregon State University. Coast to Forest: Building on Community Strengths to Promote Mental Health and Reduce Opioid Abuse in Rural Oregon. (2020). Available online at: https://health.oregonstate.edu/extension/fch/coast-to-forest (accessed December 10, 2022).
33. Mahadevan L. Mental Health First Aid Research in Rural Texas. Mental Health News. (2022). Available online at: https://www.openaccessgovernment.org/mental-health-first-aid-rural-areastrauma-informed/131293/ (Accessed July, 2022).
34. Virginia Cooperative Extension. Opioid Prevention. (2022). Available online at: https://ext.vt.edu/food-health/opioid-prevention.html2022 (accessed December 10, 2022).
35. University of Wisconsin-Madison Extension. UW-Madison Division of Extension Receives $500,000 Grant to Address Opioid Issues. (2020). Available online at: https://fyi.extension.wisc.edu/news/2020/08/13/uw-madison-division-of-extension-receives-500000-grant-to-address-opioid-issues/ (accessed December 10, 2022).
36. US Fed News Service. Garrison Moon in HESC Leading Group in 2 USDA Funded Health Projects. (2017). Available online at: https://www.proquest.com/docview/1975626871/E5070349E54D491FPQ/13?accountid=10771&forcedol=true&parentSessionId=3WWnXfwbdSAFSojL3qCk8eTro6djB3VSP6Jn96VM8s4%3D (accessed December 10, 2022).
37. McKendry B. MSU Research Team Wins Grant to Help Rural Communities Deal With Opioid Crisis. (2020). Available online at: https://www.canr.msu.edu/news/msu-research-team-wins-grant-to-help-rural-communities-deal-with-opioid-crisis (accessed December 10, 2022).
38. Ray R. UNH Receives Nearly a Million Dollars to Help Fight the Opioid Epidemic. University of New Hampshire Media Relations Newsroom. (2020). Available online at: https://www.unh.edu/unhtoday/news/release/2020/08/13/unh-receives-nearly-million-dollars-help-fight-opioid-epidemic
39. Painter A. Virginia Cooperative Extension forms Key Partnerships to Tackle the State's Opioid Epidemic. (2018). Available online at: https://vtx.vt.edu/articles/2018/07/cals-opioid.html (accessed December 10, 2022).
40. University of Vermont Extension. UVM Cultivating Healthy Communities. (2022). Available online at: https://www.uvm.edu/extension/prosper_programs (accessed December 10, 2022).
41. Pratt K. Grant will help UK Extension Expand Opioid Prevention and Recovery Efforts. College News. (2019). Available online at: https://news.ca.uky.edu/article/grant-will-help-uk-extension-expand-opioid-prevention-and-recovery-efforts
42. Iowa State University Extension Outreach. Strengthening Families Program: For Parents and Youth 10-14 Web: Iowa State University. Available online at: https://www.extension.iastate.edu/sfp10-14/ (accessed December 10, 2022).
43. University of Tennessee Institute of Agriculture. New Approach to Combat Opioid Crisis in Rural Tennessee. (2020). Available online at: https://utianews.tennessee.edu/new-approach-to-combat-opioid-crisis-in-rural-tennessee/ (accessed December 10, 2022).
44. Michigan State University Extension. Combating the Opioid Crisis through Outreach and Edcucation. (2020). Available online at: https://www.canr.msu.edu/resources/combating-the-opioid-crisis-through-outreach-and-education (accessed December 10, 2022).
45. Murray D. NC Empowering Youth and Families Program (EYFP). Available online at: https://carteret.ces.ncsu.edu/2021/03/nc-empowering-youth-and-families-program-eyfp/ (accessed December 10, 2022).
46. Ohio State University Extension College of Food Agricultural and Environmental Sciences. Opioid Epidemic in Ohio – Extension in Action. (2022). Available online at: ttps://extension.osu.edu/about/resources/opioid-epidemic-ohio-%E2%80%93-extension-action#:~:$\sim$text=Ohio%20is%20considered%20%22ground%20zero,prevention%20of%20opioid%20abuse%20statewide (accessed December 10, 2022).
47. Illinois Extension College of Agricultural Consumer & Environmental Sciences. 2017 Impact Report. University of Illinois Extension. (2018).
48. Washington State University Extension. Take-PART (Participatory Action Research with Teens) Opioid Research Project Internship. Available online at: https://extension.wsu.edu/clallam/4h/youth-advocates-for-health-ya4-h/ (accessed December 10, 2022).
49. Manning J. Your Life–Your Health Programming Availability. (2018). Available online at: https://wilson.ces.ncsu.edu/2017/11/your-life-your-health/ (accessed December 10, 2022).
50. Extension Monroe County. Agents 4 Change. Available online at: https://monroe.extension.wisc.edu/4-h-youth-development/agents-4-change/ (accessed December 10, 2022).
51. University of Rhode Island. URI to Offer Opioid Education, Training to Rural Communities. (2020). Available online at: https://www.uri.edu/news/2020/02/uri-to-offer-opioid-education-training-to-rural-communities/ (accessed December 10, 2022).
52. Michigan State University. Farm Stress and Opioid Misuse Awareness. Available online at: https://www.canr.msu.edu/resources/farm-stress-and-opioid-misuse-awareness (accessed December 10, 2022).
53. Iowa State University Prosper Rx. Project STOMP is a new initiative just for ISU County Extension & Outreach Staff brought to you by the PROSPER Rx Team. (2021). Available online at: https://prosper-rx.ppsi.iastate.edu/project-stomp (accessed December 10, 2022).
54. Utah State University. Community Opioid Education Dinner - Green River. (2022). Available online at: https://www.usu.edu/calendar/?id=78789 (accessed December 10, 2022).
55. Mississippi State University Extension. PROMISE:Preventing Opioid Misuse in the Southeast. (2020). Available online at: http://extension.msstate.edu/the-promise-initiative (accessed December 10, 2022).
56. University of Minnesota Extension. With drug overdoses skyrocketing, Extension and the College of Pharmacy partner in rural Minnesota to reduce harms. Extension and the College of Pharmacy Combat the Opioid Crisis. (2021). Available online at: https://extension.umn.edu/family-news/-extension-pharmacy-combat-opioid-crisis (accessed December 10, 2022).
57. Extension University of Missouri. Statewide Survey Shows that Drugs Affect 70% of Missouri Employers. (2021). Available online at: https://extension.missouri.edu/news/statewide-survey-shows-that-drugs-affect-70-of-missouri-employers-5455 (accessed December 10, 2022).
58. Akgerman L, Apaliyah G. Employment and the Opioid Crisis in Ohio: How Extension, Community Partners and the Americans with Disabilities Act Can Support Local Employers. In: Proceedings of the Community Engagement Conference. Columbus, Ohio. (2018). p. 24–5.
59. West Virginia State University Extension Service. Healthy Grandfamlies. Available online at: http://healthygrandfamilies.com/about/ (accessed December 10, 2022).
60. West Virginia University Extension. WVU Extension Service joins Marie's House in the Battle Against the Opioid Epidemic. (2019). Available online at: https://extension.wvu.edu/news/2019/09/25/wvu-extension-service-joins-marie-s-house-in-the-battle-against-the-opioid-epidemic (accessed December 10, 2022).
61. Maryland ROPTA. Introducing MarylandROPTA. (2021). Available online at: https://marylandropta.org/about/ (accessed December 10, 2022).
62. Montana State University Extension. Opioid Public Service Announcements [Videos] (2020). Available online at: https://www.montana.edu/extension/health/opioid_pubic_service_announcement_videos.html (accessed December 10, 2022).
63. University of Rhode Island. Learn how to reverse and overdose. Become a Community First Responder with our Ten Minute Certification Module and Receive Free Narcan. Available online at: https://web.uri.edu/cfrp/ (accessed December 10, 2022).
64. South Dakota State University Extension. Strengthening the Heartland. Available online at: https://extension.sdstate.edu/tags/strengthening-heartland (accessed December 10, 2022).
65. University of Winsconsin-Madison Extension. EXTENSION'S Role in Addressing Wisconsin's Opioid Crisis (2019). Available online at: https://extension.wisc.edu/files/2019/03/Extension-OpioidResponseOverview.pdf (accessed December 10, 2022).
66. Mississippi State University Extension. You Have the Power to Prevent Opioid Addiction. (2019). Available online at: http://extension.msstate.edu/publications/you-have-the-power-prevent-opioid-addiction (accessed December 10, 2022).
67. Cantrell A. MSU Extension Researchers Receive Grants for Projects Aimed to Address Prescription Opioid Misuse. (2019). Available online at: https://www.montana.edu/news/18650/msu-extension-researchers-receive-grants-for-projects-aimed-to-address-prescription-opioid-misuse (accessed December 10, 2022).
68. Oklahoma State University Extension. Tulsa County Family and Consumer Sciences. (2022). Available online at: https://extension.okstate.edu/county/tulsa/family-and-consumer-sciences.html (accessed December 10, 2022).
69. University of Minnesota Extension Family Development. Community Solutions to the Opioid Crisis. YouTube. (2020). Available online at: https://www.youtube.com/playlist?list=PL-JlTnitjANGcEE6eCT6p349OGvBtPqtL (accessed December 10, 2022).
70. Weibe A. Utah State University HEART Team Solidifies Vision, Reinforces Project Planning at Impact Collaborative Summit. (2019). Available online at: https://extension.org/2019/07/24/utah-state-university-heart-team-solidifies-vision-reinforces-project-planning-at-impact-collaborative-summit/ (accessed December 10, 2022).
71. Haskins T, Hartman A. Webinar: Assessment of Opioid Misuse Risk Among Farmers in the Clinical Setting. Washington State University (2021).
72. Stewart G. Ohio State University Extension offers Trauma-Informed Care Training for Noble County. (2020). Available online at: https://noble.osu.edu/news/ohio-state-university-extension-offers-trauma-informed-care-training-noble-county (accessed December 10, 2022).
73. Utah State University Office of Health Equity and Community Engagement. Tribal and Rural Opioid Initiative. Available online at: https://extension.usu.edu/healthwellness/healthequity/troi/index (accessed December 10, 2022).
74. Utah State University Office of Health Equity Community Engagement. Debunked [Podcast]. Available online at: https://extension.usu.edu/healthwellness/healthequity/ (accessed December 10, 2022).
75. Matheson JL, McGrath R.T. Adolescent Alcohol and Other Drug Abuse Quick Facts Colorado State University Extension Website. (2012) [Fact Sheet]. Available online at: https://extension.colostate.edu/topic-areas/family-home-consumer/adolescent-alcohol-and-other-drug-abuse-10-216/ (accessed December 10, 2022).
76. Nelson PT. Prevention Pays in Families Matter! A Series for Parents of School-Age Youth Newark, DE: University of Delware Cooperative Extension. (2012). Available online at: https://www.udel.edu/academics/colleges/canr/cooperative-extension/fact-sheets/prevention-pays/ (accessed December 10, 2022).
77. Palombi L, Hager K. Understanding opioid addiction and treatment. University of Minnesota Extension (2020). Available online at: https://extension.umn.edu/mental-well-being/understanding-opioid-addiction-and-treatment (accessed December 10, 2022).
78. Kennedy LE. Understanding opioids without the stigma. In: Extension TSUC, editor. Web: Tennessee State University Cooperative Extension Department of Human Sciences College of Agriculture. (2019). Available online at: https://www.tnstate.edu/extension/documents/understanding%20opioids%20without%20the%20stigma.pdf (accessed December 10, 2022).
79. Borsuah K, Whitacre B. Drug Disposal Options for Rural Communities. Oklahoma State University Extension. (2020). Available online at: https://extension.okstate.edu/fact-sheets/drug-disposal-options-for-rural-communities.html (accessed December 10, 2022).
Keywords: substance abuse, cooperative extension, drug abuse, opioid, prevention
Citation: Hagaman A, Roark K and Washburn LT (2023) U.S. Cooperative Extension's response to substance misuse: A scoping review. Front. Public Health 11:1127813. doi: 10.3389/fpubh.2023.1127813
Received: 20 December 2022; Accepted: 23 January 2023;
Published: 17 February 2023.
Edited by:
Allen C. Meadors, Independent Researcher, Seven Lakes, NC, United StatesReviewed by:
Robert J. Wellman, UMass Chan Medical School, United StatesBricca Sweet, Ed-LBEX, United States
Anne Iaccopucci, University of California Agriculture and Natural Resources, United States
Copyright © 2023 Hagaman, Roark and Washburn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angela Hagaman,  hagaman@etsu.edu
hagaman@etsu.edu
 Angela Hagaman
Angela Hagaman