
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 17 April 2023
Sec. Digital Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1121563
This article is part of the Research Topic Future Trends and Directions of using mHealth Strategies to Prevent and Treat Cardiovascular Diseases View all 5 articles
Background: Individual’s adaptation following acute myocardial infarction (AMI) and low attendance of whole-course cardiac rehabilitation (CR) are significant issues. For optimal health post AMI, an integrated CR program aiming at individual’s adaptive behaviors is imperative for improving the CR efficiency and patients’ outcomes. This study aims to develop theory-guided interventions to increase CR attendance and adaptation level of patients post-AMI.
Methods: This study was conducted in a tertiary hospital from July 2021 to September 2022 in Shanghai China. Guided by the theory of adaptation to chronic illness (ACI theory), the study followed the Intervention mapping (IM) framework to develop the interventions for CR program. Four phases included: (1) needs assessment of patients and facilitators using a cross-sectional study and semi-structured, in-depth interviews, (2) identification of implementation outcomes and performance objectives, (3) selection of theoretical methods to explain the mechanism of patients’ adaptive behaviors and to use for behavior change, and (4) development of implementation protocol from the results of the previous phases.
Results: A total of 226 AMI patient-caregivers paired samples were eligible for the data analysis, 30 AMI patients participated in the qualitative inquiry, 16 experts in the CR field evaluated the implementation protocol, and 8 AMI patients commented on the practical interventions. Following the IM framework, an integrated cardiac rehabilitation program using mHealth strategies was developed for AMI patients to facilitate CR attendance and completion, to improve their adaptation level and health outcomes.
Conclusion: Using the IM framework and ACI theory, an integrated CR program was developed to help guide the behavior change and improve adaptation among AMI patients. The preliminary findings suggest that further intervention in enhancing the combination of three-stage CR is required. A feasibility study will be conducted to assess the acceptability and effectiveness of this generated CR intervention.
Cardiac rehabilitation (CR), as 1A-class evidence proposed by multinational guidelines, can improve patients’ cardiopulmonary function and quality of life, and reduce hospital readmission and cardiovascular mortality (1–4). A component of Acute Myocardial Infarction (AMI) treatment is CR program which includes three phases defined as clinical, outpatient, and post-cardiac rehab. According to Million Hearts Cardiac Rehabilitation Collaborative, a 70% participation rate of CR was expected to be achieved by 2022 (5). Analytical data demonstrated a huge gap showing low rates with 24.4% participation rate (7.1% for AMI event) among Medicare beneficiaries in United States (6), 7.05% of AMI patients attending the CR after discharge in China (7), and 1.5% of AMI patients undertaking CR during outpatient treatment in Korea (8). Despite the benefits of CR, CR participation rates remain suboptimal worldwide (4), and thus effective strategies are required (9).
CR is a comprehensive intervention including the optimal use of medication, physical exercise, lifestyle modifications, psychosocial health, and regular follow-up education (10). Outcome measures and performance within CR have been audited in Sweden and United Kingdom demonstrating high-quality CR programs in these countries (10, 11). However, a national survey conducted in 2016 about CR programs in China (12), reported that the estimated prevalence of CR services in China was 24.4% among tertiary hospitals and estimated availability of CR programs was 2.2 per 100 million people. Little is known about the embedding of three CR phases. Redesigning the CR program at an institutional level and improving CR attendance and completion at an individual level has the potential to impact healthcare resources and outcomes and requires further exploration.
Interventions on the different CR phases provide an effective pathway to improve the CR participation and outcomes, but require significant institutional support, multidisciplinary team, and robust referral system for patients (4, 10, 13, 14). Previous studies have demonstrated that CR programs need to be designed and adapted as patient demographics vary and health needs of attendees have expanded across different CR phases (15–17). With current studies mainly focusing on one specific phase of CR, strategies for promoting CR program processes are needed to maintain systematic rehabilitation during health transitions of different contexts. A large-scale trail named Yoga-CaRe program for AMI patients was conducted in India and the United Kingdom to evaluate the effectiveness of four-phase CR program (inpatient care, two-session outpatient care, and long-term home care). The 6 month interventions of Yoga-CaRe program were delivered via a booklet, DVD materials, in-person education, and telephonic visits and showed satisfactory results on self-report health and return to pre-infarct activities (18). Evidence for designing and mechanism explanations of transitions among four phases are mainly based on the reviews of literature and consultations of CR experts and Yoga experts lacking patients’ involvement and implementation planning group which are important factors for increasing CR enrollment and completion (9).
Numerous studies showed that mHealth or eHealth strategies using digital technologies were useful in CR programs (19), such as SMS messages, telephonic follow-up (20), social media platforms (21, 22), and smartphone applications (23). As a result of the COVID-19 pandemic, inpatient and centered-based CR programs were limited and inaccessible to patients. Home-based CR has been viewed as a priority to promote an efficient integration in the CR program process with the use of remote monitoring device to support AMI patients (6, 16). Patients’ perceptions of CR and their needs, patients’ preference to mHealth use, experts’ recommendations, and contextual factors are core elements of a personalized CR program, and these challenges need to be considered in the development and implementation of interventions in CR.
Moreover, individual adaptation of a CR program can be a complicated integration of internal and external environment resources and information processing which leads to regain a balance between illness and life (24). Within the CR program, patients have to cope and adapt post AMI (25). The level of adaptation represents the capacity of an AMI patient to address the tasks of rehabilitation, to mitigate the side effects of illness on their lives, and to use the available resources (4, 6). Adaptation is a dynamic and nonlinear process for AMI patients, that is, associated with self-regulation and constant learning to extend the competency of health management (26). It manifests in connections with personal socio-demographics, cognitive processing, relationships with healthcare professionals, and the behavioral reactions to their specific health issues. Investigating adaptation in post AMI patients within CR program with interpersonal-tailored interventions and health behaviors change is needed to determine its efficacy.
Theory-guided implementation is foundational in providing the framework for the development of systematic CR program and for interventional efforts of increasing CR enrolment, adherence, and completion (9). The approach of Intervention mapping (IM) emphasizing an inclusion of a theory basis and evidence has been used to develop, implement, and evaluate interventions about health promotion and behavior change (27, 28). The IM framework which adopts an ecological perspective and system thoughts on the individuals, is consistent with the philosophical statement of adaptation concept describing individuals as adaptive systems. Environmental stimuli (i.e., individual characteristics; and social, cultural, and economical factors) should be assessed before promotion of behavior change. To the best of our knowledge, there are no reported studies using IM framework with the combination of adaptation theory to develop individual-level health interventions likely to improve the rate of CR attendance and completion.
This study aims to describe the development of CR program interventions following the IM framework using patients’ experience of adaptation processing and experts’ recommendations with the objectives of increasing CR attendance and improving individuals’ adaptation level in the post-AMI period. The results from this study could be used to examine and redesign the transitions of cardiac rehabilitation and improve the efficiency of hospital-community-home service in the future.
This study was conducted in a tertiary hospital from July 2021 to September 2022 in Shanghai China. The CR intervention program was led by an interprofessional research team equipped from medicine, nursing and primary care from universities and the affiliated hospital. The scale of the project was considered regionally within the Shanghai City with a cohort of AMI patients recruited prior to their discharge. This study identified AMI patients who were: (1) aged 18 years or older, (2) diagnosed as first-time AMI and survived, (3) received PCI treatment, and (4) willing to participate and contribute to interventions development. The exclusion criteria were: (1) transition to long-term nursing home and (2) cognitive impairment. The three phases of CR program included in-hospital CR in the cardiac care unit (CCU), center-based CR in the cardiac rehabilitation center (CRC), and center-guided home-bases CR in the patient’s home.
The study was approved by the ethics committee of the university affiliated hospital (No. KY2021-098-B). Participants were informed of the study design and provided written consent. Participants were informed that their data were confidential and beneficial to their follow-up rehabilitation. This study adhered to the principles of the Declaration of Helsinki.
IM is a robust framework (28), which allows integration of theories and contexts to develop implementation interventions (29), and it was used to guide the study design. To guide our work in the development of CR program, the conceptual framework of Roy’s adaptation theory (24) and middle-range theory of adaptation to chronic illness (ACI theory) (26) were followed, in which adaptation is a process and an outcome of integration of internal and external environments. Thus, we followed the IM framework to develop the CR program and related interventions within the ACI theory. Four phases included (shown in Figure 1), after that, the 5th and 6th phases will proceed at a regional level.
The phase of needs assessment comprised four steps.
Step 1. Establishing an implementing planning group: core members of the research team liaised with key stakeholders at institutional and individual levels. First, following the standard CR three stages, the contextual factors for intervention implementation were agreed, including the CCU, CRC, home environments, transition measures, and COVID-19 policies. Institutional members involved in CR program were identified and categorized to be CCU group, CRC group, and follow-up group, including physicians and nurses with expertise in cardiac rehabilitation and self-management. Secondly, a purposeful inclusion of experts was undertaken based on personal collaborative network. University-level researchers with expertise in health behavior change and mobile health technology were selected. Two researchers led the 10-member implementation planning group and organized meetings of initial brainstorm and following discussion. Using the approaches of open-ended questions and group voting, qualitative records and quantitative data were analyzed.
Step 2. Literature reviews: The needs assessment started with a literature review on an exploration of adaptation in chronic care (30) and electronic health interventions on lifestyle modification (31). Additionally, a scoping review about the coping strategies enacted by cardiac patients was conducted, and with the extraction of influencing factors related to coping capacity (unpublished). Using the keywords of coping and coronary heart disease, English databases Web of Science, PubMed, CINAHL, Cochrane Library, and Embase, and Chinese databases Wan Fang, China National Knowledge Infrastructure, and China Biomed were searched. An initial 2,882 abstracts were screened and 259 full text manuscript were read. According to coping concept defined by Lazarus and Folkman, inclusion criteria were describing coping mechanism and coping behaviors on cardiac outcomes among adult population, primary studies, and English or Chinese language. After excluding reviews, conference abstracts, and other language papers, 18 articles were included for analysis. Moreover, searches of interventional studies that integrated different phases within CR programs and aimed to increase CR attendance or CR completion were made in the initial study. The literature review provided an overview of the core elements related to CR program process at different level of environments (institutional, individual, and interpersonal factors). With a summative review of previous study findings, the attitudes toward general self-management (32) and the adaptive coping strategies of Chinese cardiovascular patients (33, 34) were extracted into the consideration of individual factors.
Step 3. Assessing patients’ and caregivers’ needs: From July 2021, a cross-sectional study investigating AMI patients and their caregivers was conducted using a convenient sample in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. This part of study was to assess patients’ and caregivers’ readiness to return home from hospital following acute care hospitalization. In addition to collecting patients’ socio-demographic information, valid and culture-adapted scales with authors’ permissions were used, including Scale of Systemic Family Dynamics (SSFD) (35), Readiness for Hospital Discharge Scale (RHDS) (36), and Quality of Discharge Teaching Scale (QDTS) (37). Bedside nurses at CCU were trained to collect the questionnaire data. Finally, 240 patient-caregiver paired samples were enrolled for the survey of the discharge readiness, determinants of adaptation to illness status, and perceived family function (unpublished results).
Step 4. Exploring patients’ perceptions and experiences of CR: To have a better understanding of the factors influencing the partial or full implementation of this CR program, sub-sequential qualitative data collected from interviews were made by two principal researchers (one was PhD qualified researcher and expert in qualitative study; the other was clinical nursing specialist with abundant experience). From the perspectives of the patients, we explored patients’ adaptive coping strategies for long-term CR and needs related to CR program (i.e., mobile health experiences and challenges, acceptance of clinic follow-up alternatives). Additionally, the barriers and facilitators to implementation of integrated interventions were elucidated. Participants who met the inclusion criteria of adaptive coping (defined by hospital-based CR attendance rate, regular clinical visits, and meeting goals of guideline-recommended CR targets and levels) were approached and recruited. Using a convenient sample, 30 AMI patients were recruited by a CCU nurse and a CRC therapist. The interview guides were developed according to the findings of step 3 and the clinical experience of the researchers. Each participant participated in a face-to-face audiotaped interview lasting approximately 40–80 min. Eleven AMI patients expressed their attitudes and motivation toward CR program in hospital pre-discharge and 19 AMI patients who achieved their goal of centered-based CR shared their experiences of developing adaptive coping strategies (unpublished). The study design was performed aligning with the standards for Reporting Qualitative Research (SRQR).
Based on the logical model of needs assessment (Phase one), we decided to formulate program streams for patients and CR implementation separately following the culturally tailored guidelines and using the approach of the research team. The goals of the program would not only focus on promoting the integration of internal and external environments of an individual, but also on bringing AMI patients in contact with healthcare professionals thereby extending their usage of CR programs and their capacity of adaptation. Seven researchers with expertise in clinical practice, interventional studies, and theory-testing research within the field of cardiovascular had discussions on performance objectives at the practical and theoretical level. With the findings of need assessment, the performance objectives were adjusted. The general performance objectives would be evaluated by improved capacity of adaptation processing and better quality of life.
Concept of adaptation demonstrates the idea of philosophical states describing the relationship of the person and environment (24). Using the conceptual-theoretical-empirical framework (38), the process of adaptation was deconstructed based on the empirical evidence. Within the context of chronic health conditions, ACI theory describing the mechanism of patients’ adaptive behaviors (26) was used to guide selection of the theoretical methods for developing interventions belonging to this integrated CR program. Additionally, corresponding to KoK’ taxonomy (39), selection of behavioral change methods for our CR program was performed by reviewing the relevant literature. Referring to practical applications (39) (herein for practice use in ways that fit the AMI patients and the context in CCU and CRC), inductive analysis was performed based on patients’ experience and perspectives to condense the meaning of theoretical methods. Discussions with the research team took place for clarification of the theoretical methods and practical applications and all queries resolved.
Chinese guidelines of cardiac rehabilitation with cultural adaptation of the guidelines from ESC, AHA, and ACC were followed and reviewed several times considering the real-world context. Completion of the above phases, implementation planning group and implementors from CRC had a detailed discussion about the practical applications and intervention delivery. Iterative updates on the list of behavior change methods and practical applications were embedded. Meanwhile, all relevant materials were reviewed again by two principal researchers and synthetized as initial version of implementation protocol, then intervention contents were sent to 16 experts with different academic backgrounds within the cardiovascular field via email and instant communication application. The Delphi expert panel consisted of cardiac specialist physicians, cardiac specialist nurses, behavioral intervention experts, physical rehabilitation therapists, and methodological experts (40). All experts reviewed and evaluated the feasibility of the intervention procedures and corresponding outcome indexes independently. Based on experts’ feedback, we revised the intervention content and confirmed the content with the group. Apart from measuring adaptive capacity and discharge readiness at baseline, process indicators related to health transitions were included (i.e., each phase of CR enrollment rate and attendance rate, and follow-up frequency) for evaluating the adaptation processing. What’s more, meetings to discuss the interactions of remote device use and patients’ data feedback were held. Further modifications of implementation protocol were made and supported by technological companies. Eight AMI patients were invited to comment on the implementation protocol for the sub-sequential trial study. The implementation protocol was then revised (intervention change components, behavior change methods, and practical applications).
Mixed-method approaches were performed and varied in different study stages according to the research questions (see Figure 1). All involved investigators were trained for different parts of study accordingly. Within the IM framework and ACI theory, integration was made by combining quantitative and qualitative data. Quantitative data were collected from a cross-sectional study and other statistic-based judgments by trained clinical nurses. Qualitative data were original from semi-structured interviews for describing patients’ experiences and exploring individual’s perspective on why and what interventions should be included and how implementation should be conducted. Additionally, integration of cultural specificity and evidence translations for real-world practices were considered using implementation planning group and Delphi experts.
The raw data were transferred into digital version by trained nursing students. The collected data were managed using Excel spreadsheet and Word file. For the rigor of quantitative data, clinical nurses checked the questionnaires, and a well-trained nurse intern undertook a check of the digital data. The sample size was estimated using the G-power 3.1 and for the next-step empirical study. According to the data from a 6-month behavior change program for heart failure patients, an effect size (Cohen’s d = 0.54, r = 0.26) was determined by the difference in scores of adaptation evaluation (38). The sample size of 182 participants would be adequate to achieve a 95% power at 0.54 effect size at a 5% level of significance with the T-test method. SPSS 28.0 software was used to calculate for a baseline description of patients’ needs. All raw scores of scales were transferred into standard scores to make comparations. Descriptive analysis was performed to determine the mean and standard deviation (SD) for continuous variables and frequency/percentages for categorical variables. Regarding the qualitative data, all interviews and group discussions were recoded using a professional recording device and transcribed and reviewed, and then analyzed via the NVivo 12.0 plus software. The themes of the interview were used as coding categories under the umbrella of theory concepts with a deductive view. Meanwhile, an inductive content analysis was performed to compensate patients’ feelings, perceptions, and expectations in the perspectives of intervention implementation.
This section describes the results from the phases synthesized using the results of needs assessment, implementation outcomes and behavior objectives, the theoretical methods and strategies, and implementation protocol.
A total of 226 patient-caregiver paired samples were analyzed. They were mean age 62.09 years (SD 12.57) male (80.5%), Han nationality (97.8%), married (88.1%), no religion (86.7%), retired status (58.0%), and with health insurance (81.0%). Among 226 caregivers, the relationships with AMI patients varied with 48.7% couples, 45.10% parents and children, 3.5% siblings, 1.3% grandparents and grandsons, and 1.3% friends.
All members in the implementation planning group reached an agreement that a well-designed, patient-centered, caregiver-involved, and multidisciplinary-led CR program should be developed to improve the attendance and completion of CR program. Figure 2 demonstrates the determinants of CR behaviors of AMI patients and conceptualizes a logic model of individual adaptation for potential interventions to focus on and then to address patients’ needs, which were derived from theory concepts, empirical evidence, and practical knowledge. This framework proposes a statement that incorporates institutional, interpersonal, and individual factors that includes different levels of resources and that will impact on AMI patient’s cognition and regulation. These components will then lead to the output of behaviors and changes in health outcomes.
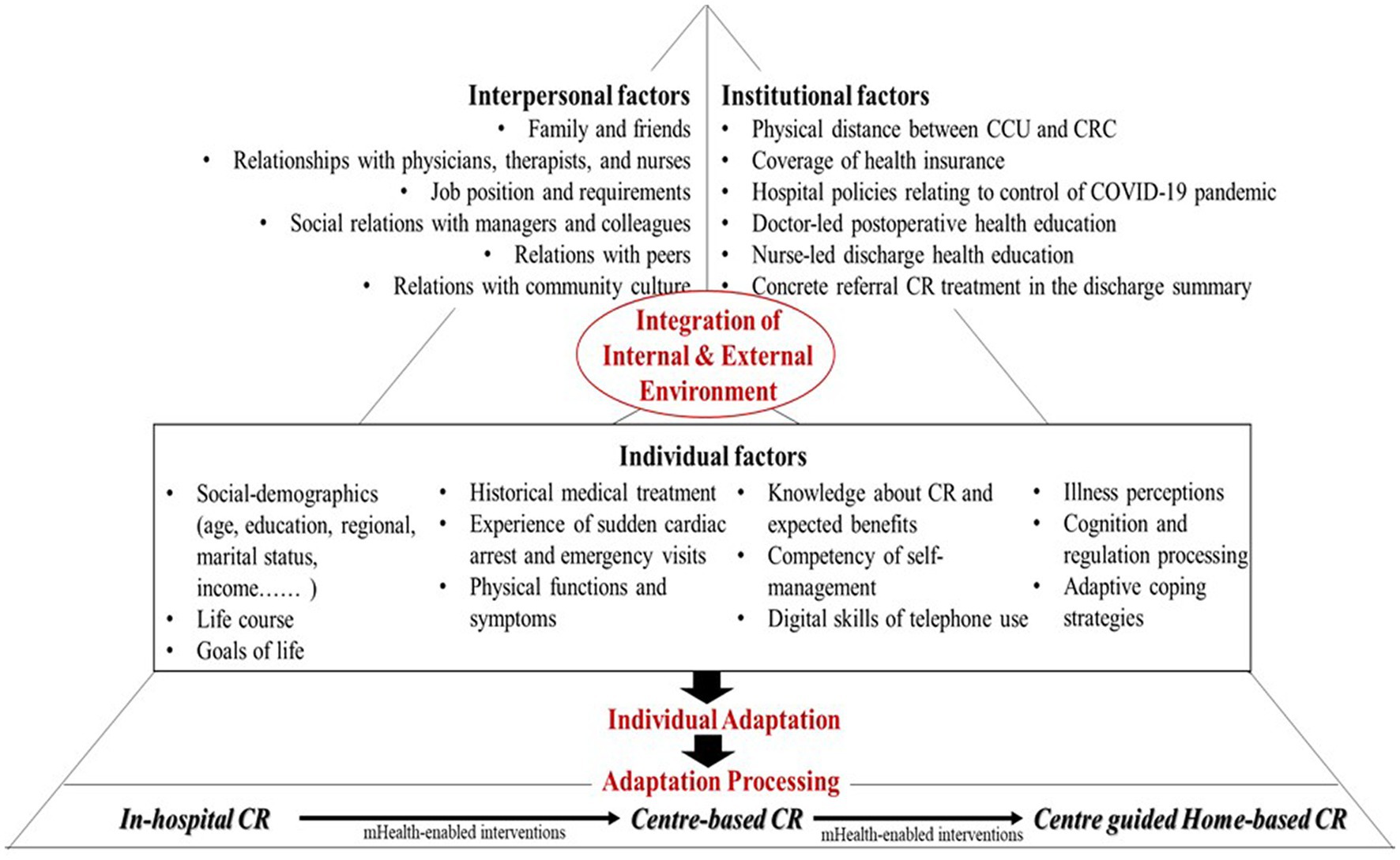
Figure 2. The logic model describing the institutional, interpersonal, and individual determinants for CR health behaviors.
Institutional factors. Combining literature review findings and previous results from a retrospective study investigating the CR attendance (7), institutional factors were identified. These included physical distance between CCU and CRC, coverage of health insurance, hospital policies relating to control of COVID-19 pandemic, doctor-led postoperative health education, nurse-led discharge health education, and concrete referral CR treatment in the discharge summary.
Individual factors. As shown in Table 1, the assessment of discharge readiness of patients and caregivers was performed in the time point of transition from the in-hospital CR to center-based CR. Findings from quantitative data showed that patients and their caregivers with different social demographics, history medical treatment, and physical symptom resulted in varied discharge readiness, and AMI patients reported sub-optimal patient education discharge information. Findings from the sub-sequential qualitative interviews revealed that AMI patients demonstrated a willingness to attend CR programs. With clear life goals and motivations for behavior change. For example, an AMI patient a retired policeman who attended centered-based CR, stated his goal of regaining adequate energy level to enjoy life not for thorough rehabilitation: “I would follow your therapy planning and come here regularly but would not adhere to the intensity of therapy strictly. I hope I can feel happy when I attend the CR program.” On the other hand, younger AMI patients tended to search for more CR knowledge and think about the CR benefits. The competency of self-management and digital skills affect patients’ decisions to accept CR referral. Additionally, previous studies provided an insight regarding coping mechanisms with three core elements of illness perceptions, cognition and regulation processing, and adaptive coping strategies (34). These factors have also been observed among patients in the post-AMI period.
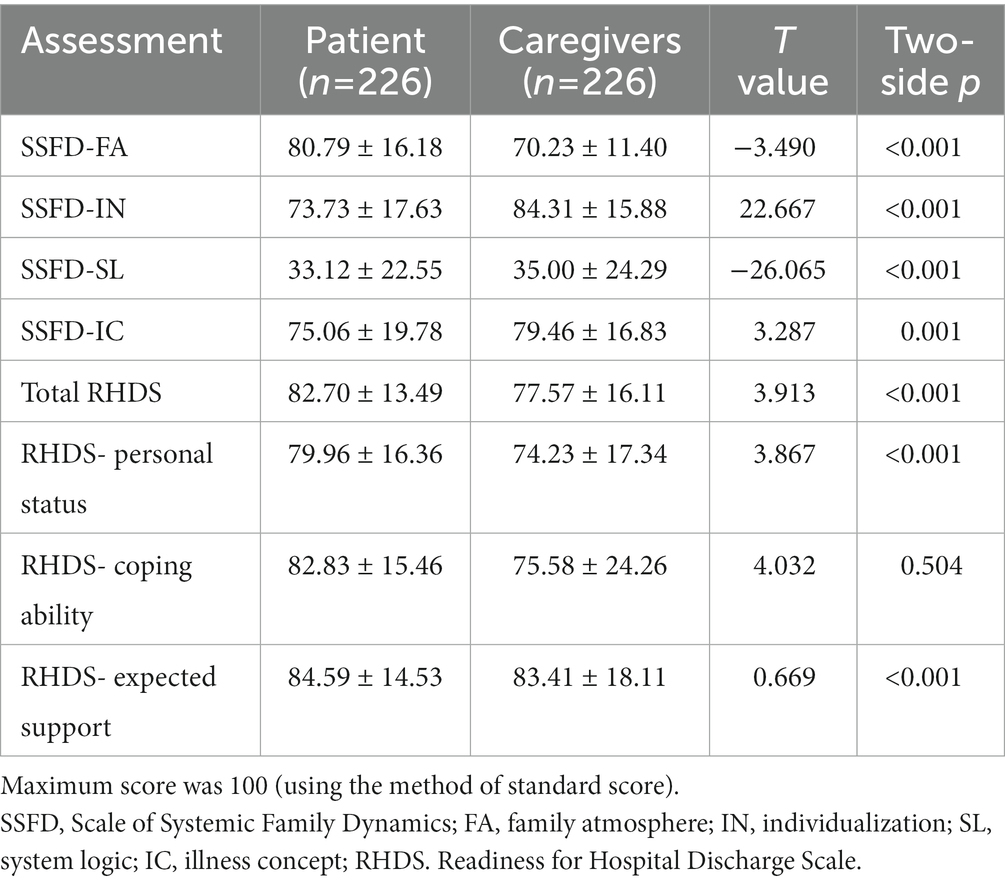
Table 1. Differences in AMI patients’ and caregivers’ perceived discharge readiness and family dynamic (n = 226).
Interpersonal factors. We tested the differences on patients’ and caregivers’ perceived discharge readiness and perceived family dynamic using the method of paired sample T-test. The result showed that all subscale of SSFD and RHDS (expect for the coping ability) had statistically significant differences between patients and caregivers (p < 0.001). Comparing with the caregivers, AMI patients perceived lower level of family function and better readiness for discharge (see Table 1). The perceptions of discharge readiness and family dynamic were further explained by qualitative interviews. All AMI patients thought highly about the functions of their family caregivers in the process of CR programs. Furthermore, six factors related to interpersonal relationships were proposed from the aspects of family members, friends, healthcare providers, work colleagues, other peers, and community.
The combined findings of needs assessment, culture-adapted guidelines, and clinical experiences of implementation planning group, implementation outcomes, and performance objectives were synthesized (see Figure 3). Chinese guidelines of CR and secondary preventions of cardiovascular diseases were reviewed, core components of CR program were extracted, including initiation of CR program in hospital, systematic individual patient assessment, personalized CR therapy (physical exercise, diet, weight control, lipid control, BP monitoring, smoking cessation, alcohol control, and stress management), and managerial strategies for CR programs. Moreover, the performance objectives in the health transition linking sub-sequential phase of CR program were explored based on the analysis of patients’ expectations and their self-initiated coping behaviors. For instance, a shipyard worker appeared to complain that “I read the doctor’s discharging summary, then I know I should start center-based CR in one month after hospital discharge……Now because I was required to return to work, I would like to know how to transfer to home rehabilitation. Sometimes, I would send messages to the therapist using my private relationship (he privately contacted his doctors).” Specifically, two streams of healthcare providers and patients were outlined, accordingly adaptive tasks and technical tasks as the determinants of implementation intervention were proposed (see Figure 3).
Using deductive analysis of the ACI theory, the theoretical methods for this CR program were tabulated with a combination of behavior change techniques. Figure 4 illustrates how implementation interventions work on CR attendance and completion through their impact on the determinants and behaviors of those responsible for CR program adoption under the umbrella of theory basis. Additionally, these provided information for general intervention tasks by control of stimuli (details as needs assessment at the institutional, interpersonal, and individual levels) and promotion of coping process in terms of physiological mode, self-concept mode, role function mode, and interdependence mode (details as performance objectives for adoption, implementation, and evaluation).
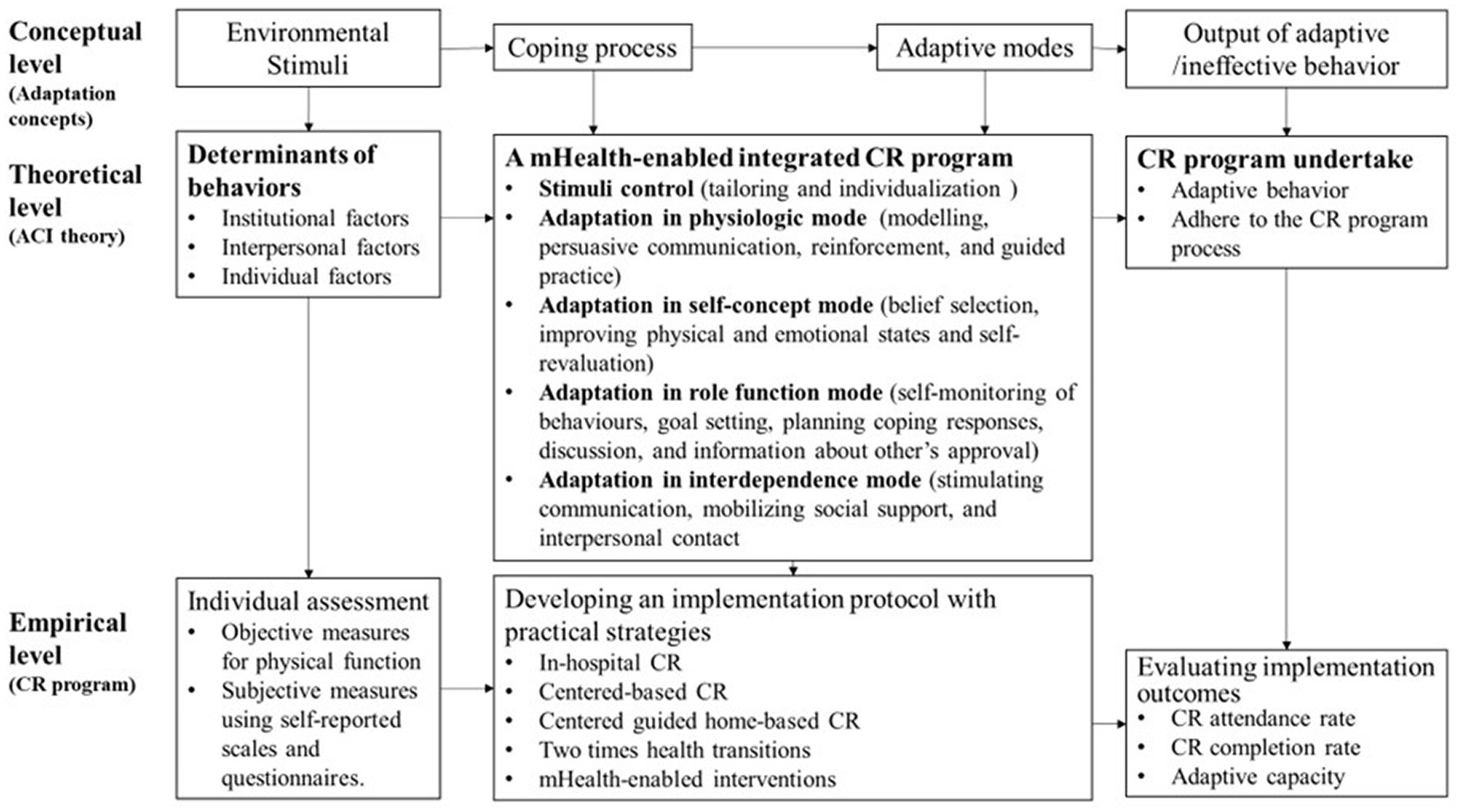
Figure 4. Conceptual-theoretical-empirical framework for this integrated CR program based on the ACI theory.
In this study, the CR program will be implemented in a qualified CRC equipped with a standard therapy pattern for three CR phases. Aligning with the ACI theory and evidence-based CR evaluation, the implementation outcomes for measuring adaptation level will target CR attendance rate, CR completion rate, and adaptive capacity (see Figure 4). Implementation interventions, consisting of three CR phases, general objectives, theoretical methods, practical applications, and delivery methods, were integrated based on previous studies and are presented in Table 2. Patients’ health needs and perspectives extracted from qualitative and quantitative data were analyzed to be facilitators and barriers of CR attendance as the determinants of CR behaviors. These findings from IM phase one guided the identification of performance objectives created in IM phase two. After reviewing the ACI theory, which unite all concepts throughout the whole project, the conceptual-theoretical-empirical framework for practice guide was developed and behavior change methods were selected and confirmed according to experts’ perspective and recommendations. The theoretical methods created in IM phase three, laid the foundation for implementation interventions. Additionally, patients’ comments on the practical interventions were embedded into the implementation protocol. For example, 3 AMI patients who were IT engineers expressed their expectations on how doctors and nurses could help them with self-monitoring. “I designed a digital and renewable chart to track my daily routine. It would be great if you can give me feedback every week.” Therefore, the format of discussion and care delivery modes were enriched and individualized to realize the goal-setting and planning coping response. Overall, Table 2 showed the mHealth-enabled integrated CR program which was combined with experts’ suggestions from the Delphi panel and patients’ comments.
This study provides an example of using the IM framework with a combination of ACI theory and evidence of cardiac rehabilitation to create complex interventions to support the improvement of CR attendance and completion. Following the IM framework, implementation planning group participated in each phase of study development which strengthened the practical applications for real-world interventions. Moreover, AMI patients with realistic experiences from different CR phases gave abundant sources of perspectives on intervention development and also on how they should be implemented. The findings demonstrated that facilitation of individual adaptation in the post-AMI period needs to consider as early as possible before hospital discharge. Patients’ and caregivers’ needs associated with long-term cardiac rehabilitation are the foundation of behavior change interventions. Our study provided an opportunity for health professionals to better integrate three CR phases based on contextual resources to make prosperous feasibility for patients CR undertake (41).
To improve compliance with CR program, CR knowledge and CR service should be recommended to AMI patients formally in the hospital stay. We found that the Chinese population had a good level of knowledge about minimizing physical activity in the immediate period after an illness. Therefore, there is a need to change this belief post AMI as the initiation of CR program is important. Persuasive communication and discussion aiming at introducing CR program could be regarded as educational strategies and be held by an interprofessional team. Meanwhile, methods of tailoring a CR program and individualizing it could be encouraged. This approach is in line with a previous study showed that participants in an educational program would be engaged actively if the intervention contents were tailored according to their needs (42). Thus, individuals’ needs assessment should include a better connection and transition to next CR phase in outpatient setting.
We found that physicians’ attitudes toward CR therapy and therapists’ involvement in bedside CR played an important role in center-based CR attendance. Findings of discharge readiness assessment showed that AMI patients and caregivers had high-level needs of health coaching on lifestyle modifications and long-term follow-up. Also, patients were strongly influenced by health professionals who recommended a CR program. The phenomenon may be attributable to an improvement of professional training for educators within the CR field. Similar to other CR programs (43), an individual evaluation of an individual patients socio-demographics, level of functionality, and medication treatment are required. Moreover, combining an adapted behavior change method and performance objectives for adaptation improvement has been observed in several studies (44, 45). Due to the essence of ACI theory explaining the coping process and combined with the empirical data from patients and caregiver, we used the approach of modeling and planning coping response to help with the development of patients’ adaptive behaviors. It is acknowledged that patients can actively learn and find a suitable way with a guidance of healthcare professionals, ultimately to adapt to changeable circumstances in a crisis. According to a mixed-method study on women’s adjustment to AMI (46), coping strategies, self-efficacy, social support, and quality of life were core elements and should be considered. Similarly, the factors mentioned above were embedded and addressed by combination use of behavior change methods. In future studies, participatory problem-solving and planning method can be taken into consideration in clinical practice for a better connection of center-based CR and center-guided home-based CR.
Regarding the inventions for center-guided home-based CR, we found that it takes time for patients to step back into a normal life. In this transition period, interventions on rebuilding habits of health behaviors and improving the adaptive capacity are needed. Aligning with the performance objectives, nine interventional methods were identified to perform CR at home, including guided practice, goal setting, planning coping responses, self-monitoring of behaviors, discussion, information about other’s approval, stimulating communication, mobilizing social support, and interpersonal contact. The findings are supported by previous studies where interventional strategies of peer support and reflection discussion were used in a community-informed virtual world-based CR program (47). A systematic review (48) showed that methods of social support and goal setting were frequently adopted in the home-based CR program. In this process, considering the convenience of intervention delivery, mobile technologies for enhancing the interactions of information, and communication appeared to offer appropriate options for bridging the gap over different phases of CR involvement. Telephone contact and instant message application provided opportunities for AMI patients to keep in touch with healthcare professionals. Remote coaching with indirect exercise supervision via digital device also is commonly used (13). However, more explorations on integrating mobile techniques and implementation inventions for use in the clinical contexts are needed in future studies.
With the guidance of the IM framework, we have identified the core components of implementation interventions for practical use to facilitate individuals’ adaptive behaviors to CR therapy. Additionally, digital strategies based on current mobile technologies are selected and attached to different CR phases. For better implementation in subsequent trials, we will review patients’ perspectives and feedback through a thematic analysis with all the results and make the intervention practices. Meanwhile, we will include software engineers as part of our research team and design a smartphone application. The features of planned application will be based on intervention contents developed in this study. Then, pilot studies and a randomized controlled trial will be conducted to evaluate the feasibility, effects, and acceptability of the CR program. Underpinning by the theory basis, this lends itself to guide the analysis of the interactions among different implementation interventions and makes it possible to determine how improvements in one component may influence the function of another.
This study adopted a robust framework to develop interventions for using in a mHealth-enabled integrated CR program underpinned by the adaptation theory to improve the CR attendance and CR completion of AMI patients. Empirical evidence shows the values of IM framework and ACI theory for use in real-world practice. Future studies can focus on testing the effectiveness of implementation interventions on increasing the CR undertake and whether is accepted by AMI patients and beneficial to their adaptation, ultimately to improve individual-level health outcomes.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics committee of the Renji Hospital (No. KY2021-098-B). The patients/participants provided their written informed consent to participate in this study.
XW conceptualized the study, carried out the study, and led the manuscript writing. LX carried out the study and was responsible for the clinical data collection. GL reviewed and revised the manuscript. AS and HC collected the data and helped sort out the research materials. JS, DC, and HZ were the members of research team and assisted with study development. All authors contributed to the article and approved the submitted version.
This study was supported by Shanghai Sailing Program (21YF1422400), Shanghai Jiao Tong University School of Medicine: Nursing Development Program, KC Wong Fellowship, and the Innovation research team of high-level local universities in Shanghai (SHSMU-ZDCX20212801). The findings and opinions expressed in this paper are those of the authors and do not reflect the official position of funders.
All authors would like to thank all participants and their caregivers for sharing the actual experiences and to acknowledge our research partner and its faculty staff in which Renji Hospital affiliated with Shanghai Jiao Tong University School of Medicine.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bellmann, B, Lin, T, Greissinger, K, Rottner, L, Rillig, A, and Zimmerling, S. The beneficial effects of cardiac rehabilitation. Cardiol Ther. (2020) 9:35–44. doi: 10.1007/s40119-020-00164-9
2. Kirolos, I, Yakoub, D, Pendola, F, Picado, O, Kirolos, A, Levine, YC, et al. Cardiac physiology in post myocardial infarction patients: the effect of cardiac rehabilitation programs-a systematic review and update meta-analysis. Ann Transl Med. (2019) 7:416. doi: 10.21037/atm.2019.08.64
3. Dunlay, SM, Pack, QR, Thomas, RJ, Killian, JM, and Roger, VL. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. (2014) 127:538–46. doi: 10.1016/j.amjmed.2014.02.008
4. Taylor, RS, Dalal, HM, and McDonagh, STJ. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol. (2022) 19:180–94. doi: 10.1038/s41569-021-00611-7
5. Ades, PA, Keteyian, SJ, Wright, JS, Hamm, LF, Lui, K, Newlin, K, et al. Increasing cardiac rehabilitation participation from 20 to 70%: a road map from the million hearts cardiac rehabilitation collaborative. Mayo Clin Proc. (2017) 92:234–42. doi: 10.1016/j.mayocp.2016.10.014
6. Ritchey, MD, Maresh, S, McNeely, J, Shaffer, T, Jackson, SL, Keteyian, SJ, et al. Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. (2020) 13:e005902. doi: 10.1161/CIRCOUTCOMES.119.005902
7. Xu, L, Yang, Y, Chen, H, Jiang, M, and Pu, J. Study on influencing factors and effect evaluation of patients with acute myocardial infarction in the cardiac rehabilitation center. J Shanghai Jiao Tong University (Med Sci). (2022) 42:646–52. doi: 10.3969/j.issn.1674-8115.2022.05.013
8. Kim, SH, Ro, JS, Kim, Y, Leigh, JH, and Kim, WS. Underutilization of hospital-based cardiac rehabilitation after acute myocardial infarction in Korea. J Korean Med Sci. (2020) 35:e262. doi: 10.3346/jkms.2020.35.e262
9. de Araújo, S, Pio, C, Chaves, GSS, Davies, P, Taylor, RS, and Grace, SL. Interventions to promote patient utilisation of cardiac rehabilitation. Cochrane Database Syst Rev. (2019) 2019:CD007131. doi: 10.1002/14651858.CD007131.pub4
10. Ogmundsdottir Michelsen, H, Sjolin, I, Schlyter, M, Hagstrom, E, Kiessling, A, Henriksson, P, et al. Cardiac rehabilitation after acute myocardial infarction in Sweden – evaluation of programme characteristics and adherence to European guidelines: the perfect cardiac rehabilitation (perfect-CR) study. Eur J Prev Cardiol. (2020) 27:18–27. doi: 10.1177/2047487319865729
11. Doherty, PJ, and Harrison, AS. The National Audit of Cardiac Rehabilitation: Annual Statistical Report (2017) 2017.
12. Zhang, Z, Pack, Q, Squires, RW, Lopez-Jimenez, F, Yu, L, and Thomas, RJ. Availability and characteristics of cardiac rehabilitation programmes in China. Heart Asia. (2016) 8:9–12. doi: 10.1136/heartasia-2016-010758
13. Thomas, RJ, Beatty, AL, Beckie, TM, Brewer, LC, Brown, TM, Forman, DE, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. (2019) 140:e69–89. doi: 10.1161/CIR.0000000000000663
14. Committee of Cardiac Rehabilitation and Prevention of Chinese Association of Rehabilitation Medicine; Committee of Cardiovascular Disease of China Association of Gerontology and Geriatrics . China expert consensus on center guided home-based cardiac rehabilitation. Zhonghua Nei Ke Za Zhi. (2021) 60:207–15. doi: 10.3760/cma.j.cn112138-20200629-00630
15. Gaalema, DE, Savage, PD, Leadholm, K, Rengo, J, Naud, S, Priest, JS, et al. Clinical and demographic trends in cardiac rehabilitation: 1996–2015. J Cardiopulm Rehabil Prev. (2019) 39:266–73. doi: 10.1097/HCR.0000000000000390
16. Besnier, F, Gayda, M, Nigam, A, Juneau, M, and Bherer, L. Cardiac rehabilitation during quarantine in COVID-19 pandemic: challenges for center-based programs. Arch Phys Med Rehabil. (2020) 101:1835–8. doi: 10.1016/j.apmr.2020.06.004
17. Feinberg, JL, Russell, D, Mola, A, Bowles, KH, and Lipman, TH. Developing an adapted cardiac rehabilitation training for home care clinicians: patient perspectives, clinician knowledge, and curriculum overview. J Cardiopulm Rehabil Prev. (2017) 37:404–11. doi: 10.1097/HCR.0000000000000228
18. Prabhakaran, D, Chandrasekaran, AM, Singh, K, Mohan, B, Chattopadhyay, K, Chadha, DS, et al. Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. (2020) 75:1551–61. doi: 10.1016/j.jacc.2020.01.050
19. Widmer, RJ, Allison, TG, Lennon, R, Lopez-Jimenez, F, Lerman, LO, and Lerman, A. Digital health intervention during cardiac rehabilitation: a randomized controlled trial. Am Heart J. (2017) 188:65–72. doi: 10.1016/j.ahj.2017.02.016
20. Kauw, D, Huisma, PR, Medlock, SK, Koole, MAC, Wierda, E, Abu-Hanna, A, et al. Mobile health in cardiac patients: an overview on experiences and challenges of stakeholders involved in daily use and development. BMJ Innovations. (2020) 6:184–91. doi: 10.1136/bmjinnov-2019-000418
21. Dorje, T, Zhao, G, Tso, K, Wang, J, Chen, Y, Tsokey, L, et al. Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): a parallel-group, single-blind, randomised controlled trial. The Lancet Digital Health. (2019) 1:e363–74. doi: 10.1016/S2589-7500(19)30151-7
22. Duan, Y, Li, X, Guo, L, Liang, W, Shang, B, and Lippke, S. A WeChat mini program-based intervention for physical activity, fruit and vegetable consumption among Chinese cardiovascular patients in home-based rehabilitation: a study protocol. Front Public Health. (2022) 10:739100. doi: 10.3389/fpubh.2022.739100
23. Rawstorn, JC, Ball, K, Oldenburg, B, Chow, CK, McNaughton, SA, Lamb, KE, et al. Smartphone cardiac rehabilitation, assisted self-management versus usual care: protocol for a multicenter randomized controlled trial to compare effects and costs among people with coronary heart disease. JMIR Res Protoc. (2020) 9:e15022. doi: 10.2196/15022
25. McAuliffe, H, Mc Sharry, J, Dunne, D, Byrne, M, and Meade, O. Identifying the active ingredients of cardiac rehabilitation: a behaviour change technique and qualitative analysis. Br J Health Psychol. (2021) 26:1194–218. doi: 10.1111/bjhp.12531
26. Wang, XY, and Ye, ZH. Development of a middle-range theory of adaptation to chronic illness based on the Roy’s model. Chin J Nurs. (2021) 56:1193–200. doi: 10.3761/j.issn.0254-1769.2021.08.012
27. French, SD, Green, SE, O’Connor, DA, McKenzie, JE, Francis, JJ, Michie, S, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the theoretical domains framework. Implement Sci. (2012) 7:38. doi: 10.1186/1748-5908-7-38
28. Fernandez, ME, Ruiter, RAC, Markham, CM, and Kok, G. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. (2019) 7:209. doi: 10.3389/fpubh.2019.00209
29. Birken, SA, Powell, BJ, Presseau, J, Kirk, MA, Lorencatto, F, Gould, NJ, et al. Combined use of the consolidated framework for implementation research (CFIR) and the theoretical domains framework (TDF): a systematic review. Implement Sci. (2017) 12:2. doi: 10.1186/s13012-016-0534-z
30. Wang, XY, Zhang, Q, Shao, J, and Ye, ZH. Conceptualisation and measurement of adaptation within the Roy adaptation model in chronic care: a scoping review protocol. BMJ Open. (2020) 10:e036546. doi: 10.1136/bmjopen-2019-036546
31. Chen, DD, Ye, ZH, Shao, J, Tang, LW, Zhang, H, Wang, XY, et al. Effect of electronic health interventions on metabolic syndrome: a systematic review and meta-analysis. BMJ Open. (2020) 10:e036927. doi: 10.1136/bmjopen-2020-036927
32. Qiu, RL, Schick-Makaroff, K, Tang, LW, Wang, XY, Zhang, Q, and Ye, ZH. Chinese hospitalized cardiovascular Patients’ attitudes towards self-management: a qualitative study. Patient Prefer Adherence. (2020) 14:287–300. doi: 10.2147/PPA.S236348
33. Qiu, RL, Schick-Makaroff, K, Tang, LW, Wang, XY, Zhang, Q, and Ye, ZH. ‘There is always a way to living with illness’-self-management strategies reported by Chinese hospitalized patients with cardiovascular disease: a descriptive qualitative study. Int J Health Plann Manag. (2021) 36:1260–75. doi: 10.1002/hpm.3172
34. Qiu, R, Tang, L, Wang, X, and Ye, Z. Life events and adaptive coping approaches to self-management from the perspectives of hospitalized cardiovascular patients: a qualitative study. Front Psych. (2021) 12:692485. doi: 10.3389/fpsyt.2021.692485
35. Yu, L, Zhao, X, Zeng, W, Yan, J, Yu, Y, Zeng, J, et al. Psychometric testing of the scale of systemic family dynamics among students in Guangdong. Chinese J Health Statistics. (2014) 31:979–81.
36. Weiss, ME, and Piacentine, LB. Psychometric properties of the readiness for hospital discharge scale. J Nurs Meas. (2006) 14:163–80. doi: 10.1891/jnm-v14i3a002
37. Candela, L, Piacentine, LB, Bobay, KL, and Weiss, ME. Teaching students to teach patients: a theory-guided approach. J Nurs Educ Pract. (2018) 8:92. doi: 10.5430/jnep.v8n11p92
38. Wang, XY, Tang, LW, Howell, D, Zhang, Q, Qiu, RL, Zhang, H, et al. Theory-guided interventions for Chinese patients to adapt to heart failure: a quasi-experimental study. Int J Nursing Sci. (2020) 7:391–400. doi: 10.1016/j.ijnss.2020.09.004
39. Kok, G, Gottlieb, NH, Peters, GJ, Mullen, PD, Parcel, GS, Ruiter, RA, et al. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol Rev. (2016) 10:297–312. doi: 10.1080/17437199.2015.1077155
40. Xu, L, Wang, X, Chen, H, Pu, J, and Yang, Y. Construction of sports and medical integration intervention program in phase II cardiac rehabilitation for patients with acute myocardial infarction. Chin J Prac Nurs. (2023) 39:15–22. doi: 10.3760/cma.j.cn211501-20220627-02014
41. Squires, JE, Aloisio, LD, Grimshaw, JM, Bashir, K, Dorrance, K, Coughlin, M, et al. Attributes of context relevant to healthcare professionals’ use of research evidence in clinical practice: a multi-study analysis. Implement Sci. (2019) 14:52. doi: 10.1186/s13012-019-0900-8
42. Page, M, Crampton, P, Viney, R, Rich, A, and Griffin, A. Teaching medical professionalism: a qualitative exploration of persuasive communication as an educational strategy. BMC Med Educ. (2020) 20:74. doi: 10.1186/s12909-020-1993-0
43. Stefanakis, M, Batalik, L, Papathanasiou, J, Dipla, L, Antoniou, V, and Pepera, G. Exercise-based cardiac rehabilitation programs in the era of COVID-19: a critical review. Rev Cardiovasc Med. (2021) 22:1143–55. doi: 10.31083/j.rcm2204123
44. Chen, DD, Zhang, H, Cui, NQ, Song, F, Tang, LW, Shao, J, et al. Development of a behavior change intervention to improve physical activity adherence in individuals with metabolic syndrome using the behavior change wheel. Public Health. (2022) 22:1740. doi: 10.1186/s12889-022-14129-1
45. Connell, LE, Carey, RN, de Bruin, M, Rothman, AJ, Johnston, M, Kelly, MP, et al. Links between behavior change techniques and mechanisms of action: an expert consensus study. Ann Behav Med. (2019) 53:708–20. doi: 10.1093/abm/kay082
46. Fuochi, G, and Foa, C. Quality of life, coping strategies, social support and self-efficacy in women after acute myocardial infarction: a mixed methods approach. Scand J Caring Sci. (2018) 32:98–107. doi: 10.1111/scs.12435
47. Brewer, LC, Abraham, H, Kaihoi, B, Leth, S, Egginton, J, Slusser, J, et al. A community-informed virtual world-based cardiac rehabilitation program as an extension of center-based cardiac rehabilitation: mixed-methods analysis of a multicenter pilot study. J Cardiopulm Rehabil Prev. (2022) 43:22–30. doi: 10.1097/HCR.0000000000000705
Keywords: cardiac rehabilitation, mHealth, acute myocardial infarction, adaptation, behavior change, intervention mapping
Citation: Wang X, Xu L, Lee G, Song A, Shao J, Chen D, Zhang H and Chen H (2023) Development of an integrated cardiac rehabilitation program to improve the adaptation level of patients after acute myocardial infarction. Front. Public Health. 11:1121563. doi: 10.3389/fpubh.2023.1121563
Received: 11 December 2022; Accepted: 24 March 2023;
Published: 17 April 2023.
Edited by:
Santi Martini, Airlangga University, IndonesiaReviewed by:
Arief Hargono, Airlangga University, IndonesiaCopyright © 2023 Wang, Xu, Lee, Song, Shao, Chen, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiyi Wang, d2FuZ3hpeWk0ODY5QHNoc211LmVkdS5jbg==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.