- 1Division of Environmental and Occupational Health Sciences, School of Public Health, University of Illinois Chicago, Chicago, IL, United States
- 2Division of Field Studies and Engineering, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Cincinnati, OH, United States
Objectives: To document local health department (LHD) COVID-19 prevention or mitigation activities at workplaces in the United States and identify facilitators for and barriers to these efforts.
Methods: We conducted a web-based, cross-sectional national probability survey of United States LHDs (n = 181 unweighted; n = 2,284 weighted) from January to March 2022, collecting information about worker complaints, surveillance, investigations, relationships and interactions with employers/businesses, and LHD capacity.
Results: Overall, 94% LHD respondents reported investigating workplace-linked COVID-19 cases; however, 47% reported insufficient capacity to effectively receive, investigate and respond to COVID-19-related workplace safety complaints. Prior relationships with jurisdiction employers and LHD personnel with formal occupational health and safety (OHS) training were predictors of proactive outreach to prevent COVID-19 spread in workplaces (p < 0.01 and p < 0.001). LHD size predicted OHS personnel and sufficient financial resources to support workplace investigation and mitigation activities (p < 0.001).
Conclusions: Differences in LHD capacity to effectively respond to communicable disease spread in workplaces may exacerbate health disparities, especially between rural and urban settings. Improving LHD OHS capacity, especially in smaller jurisdictions, could facilitate effective prevention and mitigation of workplace communicable disease spread.
1. Introduction
The COVID-19 pandemic caused unprecedented communicable disease exposure in workplaces, with prolonged workplace outbreaks emerging across the United States especially in certain “essential” industries (e.g., manufacturing and wholesale trade) that disproportionately employ low-wage workers of color (1, 2). Factors such as indoor, close-proximity work, coupled with the concentration of jobs with low wages, no healthcare benefits or paid sick leave in densely populated areas with higher rates of multi-generational, crowded housing increased the risks of exposure to SARS-CoV-2, the virus that causes COVID-19, among these workers (3). While human contact patterns outside of households changed drastically early in the pandemic, contact rates at many workplaces remained elevated, especially in “essential” industries (4). Studies that examined associations between household members of workers in at-risk occupations and household cases (5) or COVID-19-related hospital admissions (6) highlight the risks or workplace to home transmission of COVID-19.
Workplace outbreaks of COVID-19 presented a novel challenge to employers and public health departments, whereby personnel at most workplaces had little experience controlling airborne infectious disease exposures and health department personnel had limited prior interactions with non-healthcare or non-congregate workplaces to prevent and mitigate such exposures. Case studies from various industries highlight the challenges that workplaces encountered when attempting to reduce exposures, such as inadequate ventilation and inappropriate administrative controls in nursing homes (7) and lack of compliance with masking or available ventilation controls in schools, along with barriers to installation of systems to reduce SARS-CoV-2 transmission (8, 9). In order to identify persons with COVID-19 with exposures linked to workplaces and prioritize workplaces for investigation and supports, the United States Centers for Disease Control and Prevention (CDC) recommended that health departments employ a prioritization scheme for identifying persons with COVID-19 and their contacts at non-healthcare workplaces (10, 11). While at least one health department described the development and implementation of such an approach (12), there is an absence of literature documenting other health departments' approaches to identifying persons with COVID-19 linked to their workplaces or the activities that departments undertook to prevent and mitigate COVID-19 in workplaces in their jurisdictions.
Local health departments (LHDs) were tasked with investigating and intervening in outbreaks that they did identify while simultaneously maintaining their pre-pandemic duties, including monitoring community health status and providing essential services to solve wide-ranging health problems in their catchment areas, for which LHD capacity was already limited (13, 14). Reports from the first year of the COVID-19 pandemic highlighted the disruptions in the continuity of essential health services globally (15, 16), and the reduction of or disruption to preventive health services resulted in documented reductions in cancer screenings (17), decreases in and delays in appropriate care for individuals with chronic diseases (18), and excess mortality from non-COVID-19 diseases (19). Especially in rural communities, LHDs serve as key providers of, and in some cases the only providers of, clinical services (20).
There is little literature on public health engagement with workplaces to prevent and mitigate workplace outbreaks of communicable diseases in the modern era. Communicable disease outbreaks and clusters in workplaces described in the pre-COVID-19 literature were limited, and many were industry-specific, readily contained, and easily traced and mitigated by local public health authorities (21). The COVID-19 pandemic thus serves as an opportunity to understand LHD actions in response to widespread transmission of SARS-CoV-2 in workplace settings, as well as potential gaps in LHD readiness and capacity to engage in workplace-based mitigation or prevention efforts. To fill this gap, this study sought to (A) document LHD actions related to prevention or mitigation of COVID-19 cases and exposures at workplaces and (B) examine facilitators for and barriers to COVID-19 workplace outbreak investigation and mitigation efforts completed by LHDs.
2. Methods
We conducted a web-based, cross-sectional national probability survey of United States (U.S.) LHDs from January to March 2022. Survey development began mid-2021 and included two rounds of content-focused review and pre-testing with subject matter experts from the National Institute for Occupational Safety and Health (NIOSH) and from the Occupational Health Sub-committee of the Council of State and Territorial Epidemiologists. We employed a stratified sampling design to draw a random sample of 1,214 LHDs from the National Association of County and City Health Officials (NACCHO) Directory of LHDs, a comprehensive list of U.S. LHDs, with strata defined by U.S. Census geographical region (Northeast, South, Midwest, West) and by population size served (three categories based on 2019 U.S. Census population estimates: < 50,000, 50,000–499,999, ≥500,000) (22). We sampled LHDs with email contacts listed in the NACCHO Directory, and we sampled at the district or regional level in states with public health decision making directed partially or completely by state-level decision makers (e.g., centralized, shared, or mixed governance structures) (23). Given considerable COVID-19-related strain on LHDs, we anticipated a low response rate across strata and thus oversampled strata with fewer LHDs to maximize statistical power in the final sample.
The survey questionnaire included 44 items across the following domains: (i) COVID-19-related complaints in workplaces; (ii) surveillance of occupational exposures and known positive cases by industry and occupation; (iii) workplace-based investigations of outbreaks; (iv) LHD relationships and interactions with employers or business establishments; and (v) LHD capacity and organizational characteristics. Survey items were primarily closed-ended multiple-choice or multiple-selections, with a small number of open-ended items. The survey was administered via Qualtrics software (Version 2022, Provo, UT).
To better characterize LHD respondents in our analyses, we added a governance structure variable (i.e., decentralized vs. centralized, shared, or mixed). To produce nationally representative estimates, we generated sampling weights for each stratum, accounting for oversampling of and differential response rates by strata. We calculated descriptive statistics for LHD responses to capacity measures and measures of LHD engagement with workers and businesses in the aggregate, representing categorical LHD characteristics and survey responses as weighted proportions and 95% confidence intervals (CIs). The survey resulted in several capacity metrics (e.g., personnel, relationships with workplaces) and worker or business engagement activities. We constructed simple logistic regression models to assess: (1) which LHD characteristics were associated with select capacity metrics and (2) which capacity metrics were associated with the following activities: (a) collected industry or occupation information at testing or through contact tracing; (b) received requests to evaluate engineering controls, such as ventilation systems; (c) conducted in-person investigations of workplaces in response to worker complaints; and (d) enlisted the support of enforcement agencies, such as state or federal Occupational Safety and Health Administration (OSHA) offices. We selected these activities based on their likelihood to be most impactful in reducing risk of exposure to SARS-CoV-2 in the workplace (e.g., identifying and removing persons with COVID-19 from the workplace, employing engineering controls to remove viral particles from the air, enforcing COVID-19-related emergency temporary standards where applicable). We used SPSS Statistical Software version 26.0 (IBM, 2019) for all analyses. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy [see e.g., 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.].
3. Results
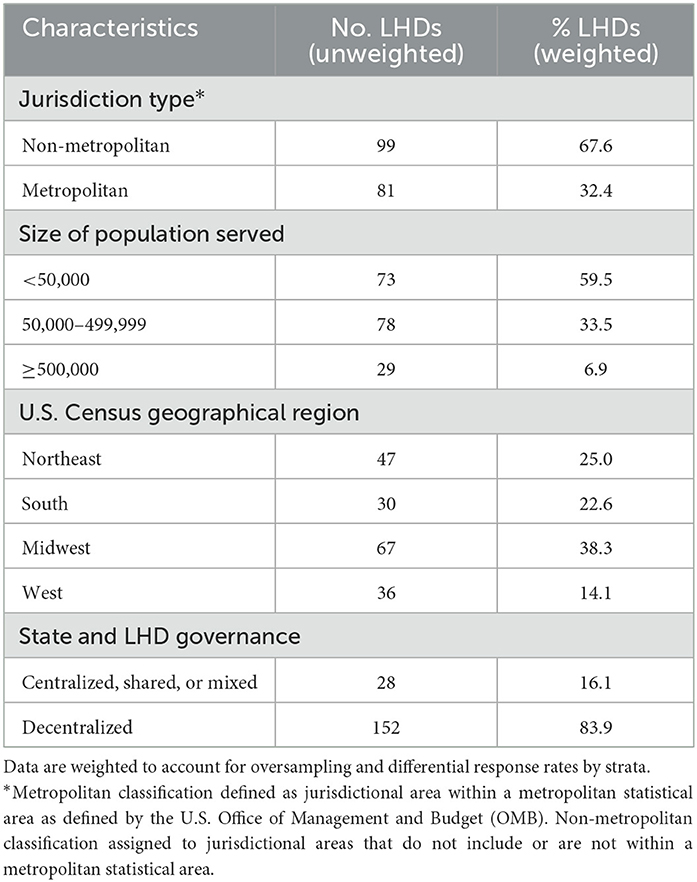
One-hundred eighty of 1,214 sampled LHDs (15%) responded to the survey. Response rate was highest among LHDs from the West region (11%), followed by Midwest and Northeast regions (8%, respectively), and lowest in the South region (6%). LHDs with more populous jurisdictions had the highest response rate (17% for populations ≥500,000), followed by medium-sized jurisdictions (10% for populations 50,000–499,999) and smaller jurisdictions (6% for populations < 50,000). Respondents most frequently represented non-metropolitan areas (n = 99), jurisdictions with 50,000–499,999 residents (n = 78), the Midwest region (n = 67), and decentralized governance structures (n = 152; see Table 1).
3.1. LHD capacity
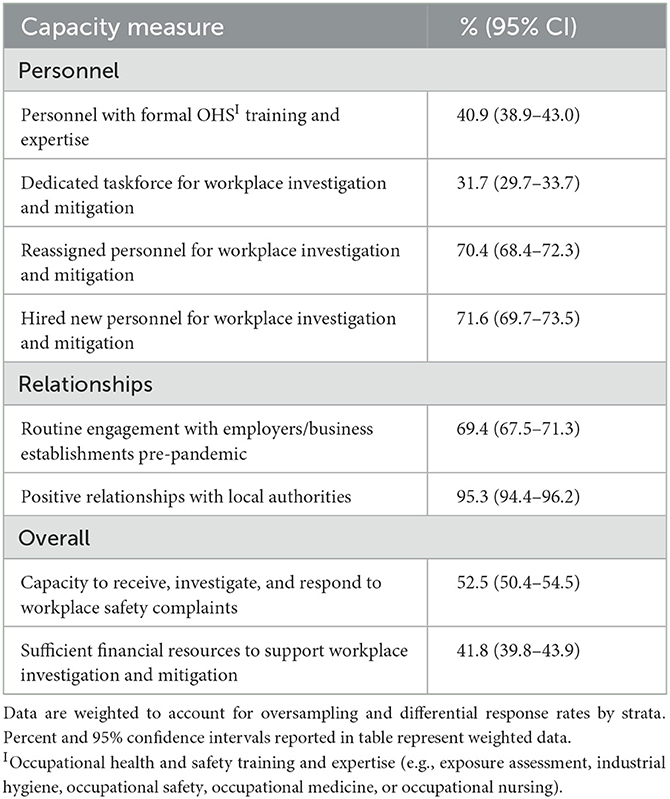
Approximately half of LHDs reported that they have the capacity to receive, investigate, and respond to workplace safety complaints (52.5%; 95% CI, 50.4%−54.5%), and fewer than half reported that they have the financial resources necessary to adequately support workplace investigation and mitigation activities (41.8%; 95% CI, 39.8%−43.9%; see Table 2). Fewer than half of all LHDs reported personnel on staff with formal occupational health and safety (OHS) training and expertise, such as training in exposure assessment, industrial hygiene, occupational safety, occupational medicine, or occupational nursing (40.9%; 95% CI, 38.9%−43.0%). The majority of LHDs reported reassigning personnel (70.4%; 95% CI, 68.4%−72.3%) or hiring new personnel (71.6%; 95% CI, 69.7%−73.5%) to assist with workplace investigation and mitigation activities during the COVID-19 pandemic (defined as the period beginning March 2020 and on-going at time of data collection); however, less than a third reported having a dedicated taskforce for workplace investigation and mitigation activities.
3.2. Engagement with workers, employers, and business establishments
Approximately half of all LHDs reported consistent collection of occupation or industry information from individuals through LHD-administered contact tracing programs (53.4%; 95% CI, 51.4%−55.5%), and about one third reported collection of occupation or industry information at LHD-administered testing sites (32.4%; 95% CI, 30.4%−34.3%; see Table 3). Fewer than half of all jurisdictions required employers to report known numbers of persons with COVID-19 to the LHD (46.6%; 95% CI, 44.6%−48.7%). While over 90% of LHDs reported investigating workplace-linked COVID-19 outbreaks, fewer than half of those LHDs reported that these investigations were conducted in-person at least some of the time (41.6%; 95% CI, 39.5%−43.7%). LHDs reported lack of or inconsistent enforcement of masking mandates and social distancing as the most frequent complaints from workers, while only 44.1% of LHDs (95% CI, 41.8%−46.5%) reported receiving complaints about appropriate engineering controls, such as venti lation, or about training specifically focused on COVID-19 prevention in the workplace. The majority of LHDs that received complaints from workers reported direct, remote engagement with employers to resolve complaints (86.0%; 95% CI, 84.3%−87.6%). Fewer than half of LHDs reported enlisting supports from outside agencies, such as enforcement agencies or non-enforcement public health agencies, to help resolve complaints (42.8%; 95% CI, 40.5%−45.2%). Nearly all LHDs also reported receiving requests for support from employers (96.1%; 95% CI, 95.2%−96.8%), with most requests focused on specific guidance for minimizing spread of COVID-19 in workplaces. In addition to requests for written information and signage, LHDs reported receiving requests to support on-site vaccination efforts (68.1%; 95% CI, 66.0%−70.1%), to connect workers with vaccinations off-site (73.7%; 95% CI, 71.8%−75.6%), and to support contact tracing (57.9%; 95% CI, 55.8%−60.1%) and testing efforts (52.4%; 95% CI, 50.2%−54.5%).
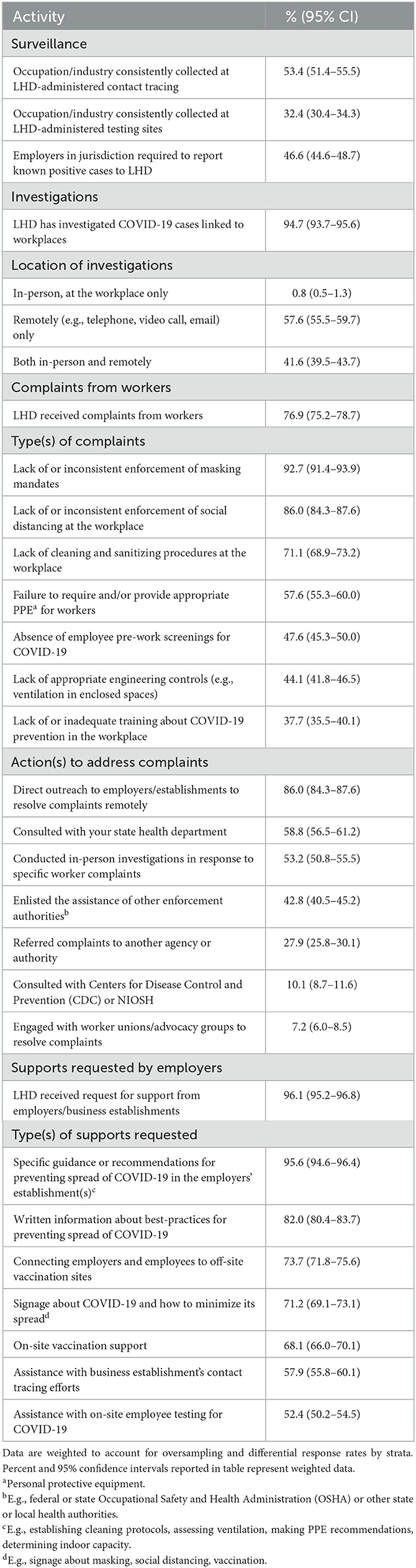
Table 3. Proportion of LHDs reporting engagement with workers and/or employment establishments (n = 180 unweighted; n = 2,284 weighted).
3.3. LHD characteristics as predictors of LHD capacity
There were several notable differences in reported LHD capacity by jurisdiction characteristic (see Table 4). Metropolitan-serving LHDs were more than twice as likely than those serving non-metropolitan jurisdictions to employ personnel with formal OHS training and expertise (OR = 2.7; 95% CI, 2.2–3.2). LHDs from increasingly populous jurisdictions were also significantly more likely to employ personnel with OHS training and expertise (population 50,000–499,999: OR = 1.9; 95% CI, 1.6–2.4; population ≥500,000: OR = 7.1; 95% CI, 5.0–10.0). The LHDs serving jurisdictions with at least 500,000 residents were twice as likely as those serving < 50,000 residents to have a dedicated taskforce for workplace investigation and mitigation activities; they were more than twice as likely to report having the capacity to receive, investigate, and respond to workplace safety complaints (OR = 2.4; 95% CI, 1.7–3.4); and they were twice as likely to report having sufficient financial resources to support workplace investigation and mitigation activities (OR = 2.1; 95% CI, 1.5–2.9). Jurisdictions in the South, Midwest, and West regions were all more likely to report having a dedicated taskforce for workplace investigation and mitigation activities (ORs = 6.2, 3.1, and 4.7) and having sufficient financial resources to support those activities (ORs = 2.9, 2.6, and 3.9) than jurisdictions in the Northeast. Jurisdictions in the Midwest and West were also more likely to report having the capacity to receive, investigate, and respond to workplace safety complaints than those in the Northeast (ORs = 2.0 and 1.9). Decentralized LHDs were less likely to report having a dedicated taskforce for workplace investigation and mitigation activities than those with other governance structures (OR = 0.7, 95% CI, 0.5–0.8) and were more likely to report having the capacity to handle complaints.
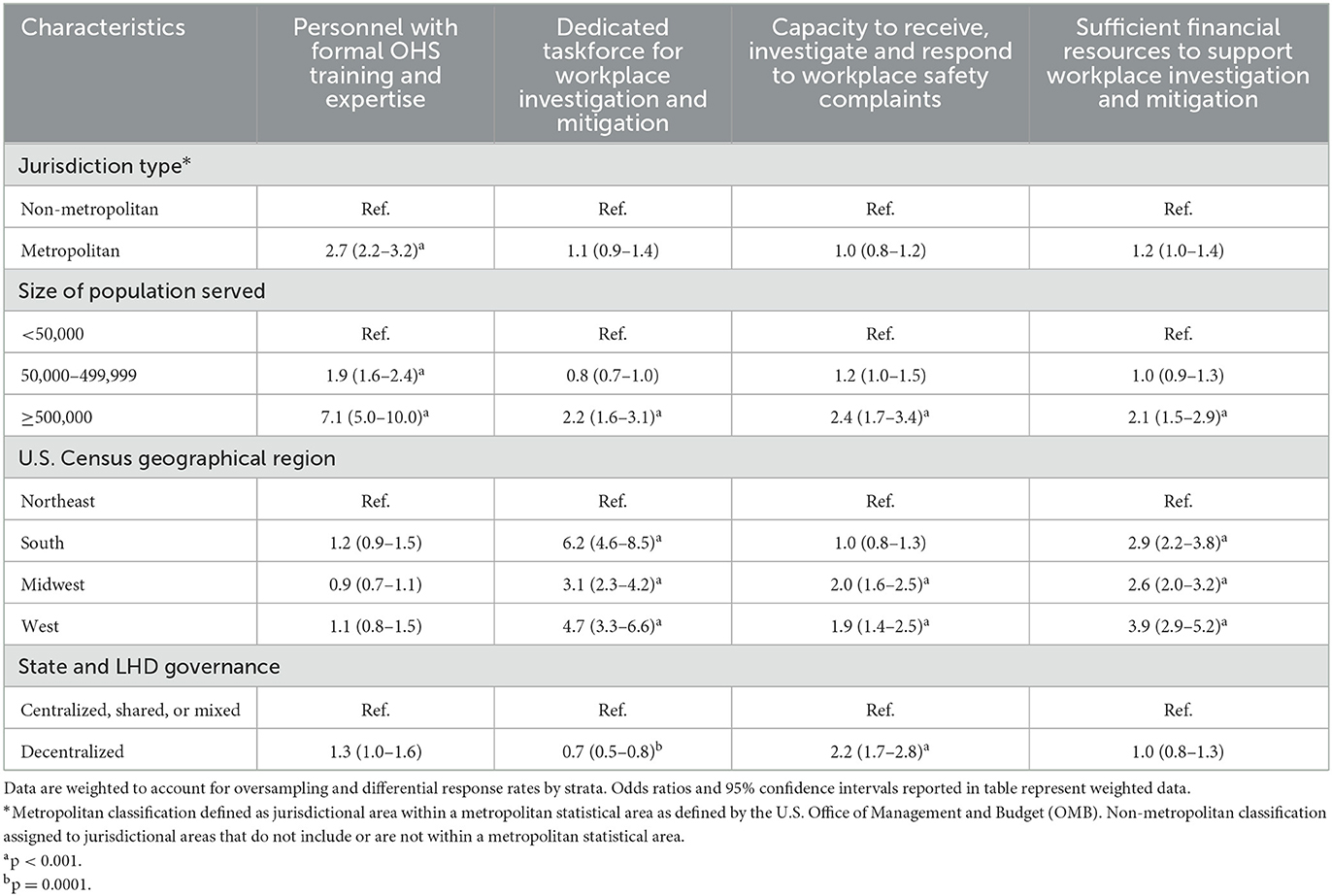
Table 4. Associations of LHD characteristics with select capacity measures (n = 180 unweighted; n = 2,284 weighted), OR (95% CI).
3.4. LHD capacity metrics as predictors of engagement with workers, employers, and business establishments
LHD capacity was significantly associated with several notable workplace-facing activities, shown in Table 5. LHDs that reported personnel with formal OHS training and expertise were significantly more likely to collect industry or occupation when contact tracing or conducting testing (OR = 1.8; 95% CI, 1.5–2.1), to report receiving requests to evaluate engineering controls (OR = 2.0; 95% CI, 1.6–2.4), and to conduct in-person investigations in response to complaints (OR = 2.4; 95% CI, 1.9–2.9) than those that did not. LHDs with a dedicated taskforce for workplace investigation and mitigation activities were also more likely to collect industry or occupation (OR = 1.6; 95% CI, 1.4–2.0) and to report requests to evaluate engineering controls (OR = 2.0; 95% CI, 1.7–2.5). LHDs that reassigned personnel for workplace investigation and mitigation activities were more likely to engage in all workplace-facing activities reported in Table 5 than LHDs that did not reassign personnel (ORs ranging from 1.3 to 1.9). LHDs that hired new personnel for these activities were more than twice as likely as those that did not to collect industry or occupation (OR = 2.3; 95% CI, 1.9–2.8) and to conduct in-person investigations of complaints (OR = 2.5; 95% CI, 2.0–3.1), and they were less likely to enlist support of enforcement agencies (OR = 0.7; 95% CI, 0.6–0.9). LHDs that reported routine engagement with employers prior to the pandemic were more likely to collect industry or occupation (OR = 2.1; 95% CI, 1.7–2.5) and were more likely to report requests to evaluate engineering controls (OR = 1.5; 95% CI, 1.2–1.9), as were LHDs that reported positive relationships with local authorities (ORs = 1.8; 95% CI, 1.1–2.7, and 3.2; 95% CI, 2.0–5.7). The latter group was also more likely to report conducting in-person investigations relative to LHDs that did not report positive relationships with local authorities (OR = 2.5; 95% CI, 1.6–3.9). LHDs that reported an overall capacity to receive, investigate, and respond to workplace safety complaints were nearly twice as likely to collect industry or occupation (OR = 1.9; 95% CI, 1.6–2.2) and to conduct in-person investigations at workplaces (OR = 1.9; 95% CI, 1.5–2.3). Those that reported having sufficient financial resources to support investigation and mitigation activities were also more likely to collect industry or occupation (OR = 2.5; 95% CI, 2.1–3.0) and were more likely to report requests for evaluation of engineering controls (OR = 1.6; 95% CI, 1.3–1.9).
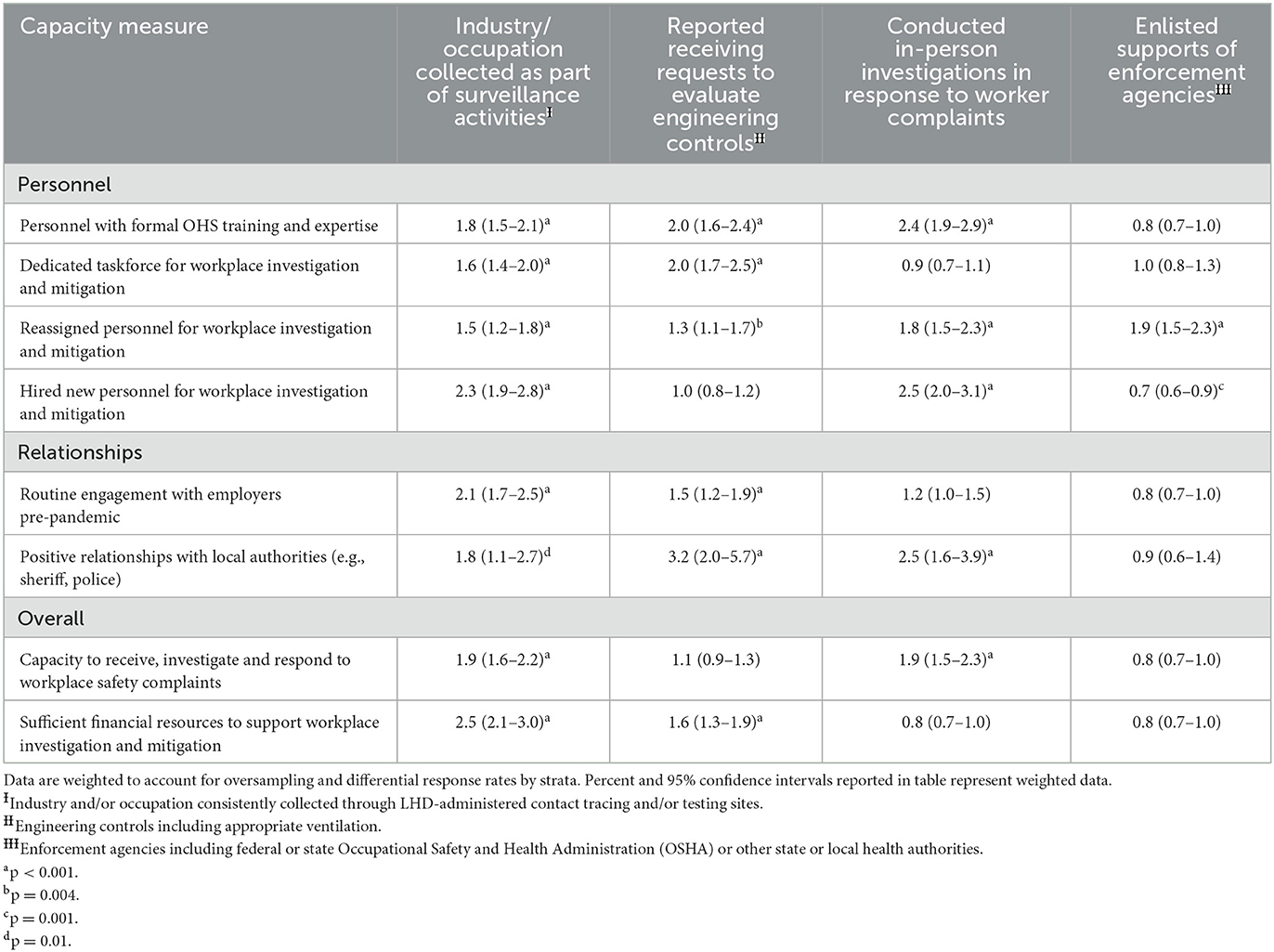
Table 5. Associations of LHD capacity with select workplace-facing activities (n = 180 unweighted; n = 2,284 weighted), OR (95% CI).
4. Discussion
Our study findings highlight the widespread engagement of LHDs with workplaces in the U.S. during the COVID-19 pandemic. While nearly all LHDs reported engagement with employers, business establishments, or workers in some capacity, we identified compelling differences in LHD capacity to surveil and intervene to prevent workplace spread of COVID-19 by jurisdiction type, size of population served, region, and LHD governance. We also found significant associations between these measures of capacity and select workplace-facing activities likely to be most effective in preventing or reducing exposure to SARS-CoV-2 (e.g., identifying known persons with COVID-19 and those exposed via testing and contact tracing; conducting thorough, in-person assessments of controls, especially engineering controls such as ventilation systems; enforcing health and safety regulations).
Despite ample evidence of occupation-based spread of COVID-19 early in the pandemic, nearly half of all LHDs did not report routine collection of industry or occupation for contact tracing purposes and less than a third reported collecting such information at LHD-administered testing sites. These statistics, coupled with the fact that employers were required to report known positive tests to fewer than half of all LHDs, highlight a notable missed opportunity to identify and potentially prevent workplace-based spread of COVID-19 across the U.S. by engaging with employers to reduce exposure risks in their establishments. When LHDs did identify COVID-19 cases linked to workplaces, the majority of LHDs reported conducting investigations of establishments remotely, potentially limiting their abilities to appropriately evaluate existing controls or to identify opportunities for more effective intervention to further reduce exposure risks in the physical workplace environment. In the future, collection of occupation and industry at testing and through contact tracing could help LHDs focus their investigative and mitigative efforts to ensure that workers at highest risk of infection are identified and better protected in their workplaces.
Compared with LHDs serving small (< 50,000) or medium (50,000–499,999) populations, LHDs serving large populations (≥500,000) reported an overall higher capacity to address the threat of COVID-19 in workplaces within their jurisdictions. LHDs in areas serving larger populations are likely to have a larger public health workforce (24), allowing them to more readily restructure and create a dedicated taskforce for workplace-facing activities. Larger LHDs may also be able to differentiate internal departments and attract more specialized personnel, such as individuals with formal OHS training. Employing personnel with OHS training and expertise was an important predictor of effective workplace-facing activities to prevent and reduce exposures, including collecting industry and occupation in surveillance activities, evaluating engineering controls, and conducting in-person investigations. Notably, LHDs that reported having OHS-trained personnel were less likely to report engagement with enforcement agencies, perhaps because these individuals are likely to be more familiar with regulatory standards and how to apply them in a workplace, or because these individuals may have the expertise required to operationalize CDC and state-level guidance. OHS training and expertise may be necessary to fulfill public health's core mission of preventing and controlling disease, specifically in a workplace context when airborne contaminants are of concern. Unlike the general public health workforce, those with OHS training and expertise are specifically trained to identify and evaluate hazards in the confines of a workplace and to select the most appropriate and effective available controls to address those hazards.
LHDs that reported routine engagement with employers prior to the pandemic and those that reported positive relationships with local authorities were also more likely to undertake high-impact workplace-facing activities, similar to our findings regarding employment of personnel with formal OHS training or expertise and having the agility to reconfigure their workforce. This finding aligns with strategies outlined in the Public Health 3.0 framework, specifically focused on the development and utilization of collaborative, strategic partnerships to effectively monitor and respond to drivers of population health (25). While robust relationships between these stakeholders was identified as a facilitator of LHD-workplace engagement, overall capacity to engage with workplaces and to fund such activities attenuate these findings. Only half of all LHDs reported overall capacity to receive, investigate, and respond to workplace safety complaints, and fewer than half reported sufficient financial resources to support efforts related to investigation and mitigation of COVID-19 in workplaces. Notably, workforce and funding needs of LHDs were not evenly distributed prior to the pandemic (26, 27), and this may have contributed to disparities in factors that facilitated workplace-focused prevention and mitigation efforts for COVID-19, such as having existing, collaborative relationships with business establishments from prior health assessment and planning activities.
LHDs in the Northeast were least likely to report sufficient financial resources, and LHDs in the Northeast and South were less likely to report overall capacity to receive, investigate, and respond to workplace safety complaints than LHDs in the Midwest and West. LHDs in states with decentralized governance structures were also more likely to report having an overall capacity to engage in these efforts. While perception of lack of capacity and resources is widespread, there may be regional-specific differences in demands (e.g., requests for support from employers, complaints from workers), LHD resources (e.g., funding, ability to attract and retain the public health workforce), or LHD decision latitude (e.g., enforcement authority, ability to enter workplaces). Centralized governance structures may reduce a LHD's ability to rapidly shift or reallocate resources to shore up capacity in these types of initiatives compared to LHDs where fiscal authority is at the local level.
While the threat of COVID-19 spread in workplaces galvanized the public health workforce to respond in a myriad of ways, it is evident that limitations in capacity constricted LHD's efforts. The chronic underfunding of the public health workforce and its impact on LHD readiness to respond to the COVID-19 pandemic is well-documented (28, 29), as are challenges related to prior cuts to and continuing decline of the public health workforce (14). More recently, researchers have highlighted the threat of further erosion of the public health workforce as burnout becomes more prevalent (30) and violence directed at public health officials, exacerbated by the continued politicization of the public health response to the COVID-19 pandemic, becomes increasingly common (31). It is thus important that we contextualize this study's findings in the realities facing public health, and that we recognize that the capacity limitations identified in this paper may not be easily remedied without increased financial resources for LHDs across the U.S. Further, and in the spirit of Public Health 3.0, there could be an examination of how the larger public health system, including enforcement and non-enforcement public health agencies and for-profit OHS firms that employ individuals with formal OHS training, might collaborate with LHDs to identify, evaluate, anticipate, and control biological hazards in workplaces.
This study is subject to several limitations. First, this study was designed to generate preliminary prevalence data about LHD interactions with workplaces during the pandemic and was not intended to provide an in-depth exploration nor evaluation of factors that facilitated or hindered LHD efforts related to the investigation and mitigation of COVID-19 spread in workplaces. Further, this study was not designed to examine LHD engagement with workplaces in specific communities or those with worker sociodemographic characteristics that were associated with higher rates of COVID-19 infection. The results presented here provide a foundation for more extensive, qualitative inquiry around these factors in follow-up studies. Additionally, the response rate in this study was fairly low (15%). The low response rate is not unexpected given the timing of survey deployment (recruitment began as the initial Omicron variant peaked in early 2022) and the resultant strain on LHDs across the country. Our methods of identifying and contacting the appropriate respondent for this survey were also imperfect and may have limited the survey response rate: contact information for LHD administrators was not always up to date and administrators may not have been the appropriate respondent at all LHDs, especially those serving larger jurisdictions. Despite these limitations, responses from LHDs provide initial insight into actions related to workplace prevention and mitigation of COVID-19 and highlight key facilitators of and barriers to these activities during the pandemic.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Illinois Chicago Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TB: conceptualization, methodology, formal analysis, investigation, and writing—original draft. MG: conceptualization and writing—review and editing. Both authors contributed to the article and approved the submitted version.
Funding
This product was developed with funding support through an intergovernmental personnel agreement with the National Institute for Occupational Safety and Health (NIOSH). The findings and conclusions in this document are those of the authors and do not necessarily represent the official position of NIOSH.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bui DP, McCaffrey K, Friedrichs M, LaCross N, Lewis NM, Sage K, et al. Racial and ethnic disparities among COVID-19 cases in workplace outbreaks by industry sector — Utah, March 6–June 5, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1133–8. doi: 10.15585/mmwr.mm6933e3
2. Rho HJ, Brown H, Fremstad S. A Basic Demographic Profile of Workers in Frontline Industries. Washington, DC: Center for Economic Policy Research (2020) 7:3–10. Available online at: https://cepr.net/wp-content/uploads/2020/04/2020-04-Frontline-Workers.pdf
3. Faghri PD, Dobson M, Landsbergis P, Schnall PL. COVID-19 pandemic: what has work got to do with it? J Occup Environ Med. (2021) 63:e245–9. doi: 10.1097/JOM.0000000000002154
4. Nelson KN, Siegler AJ, Sullivan PS, Bradley H, Hall E, Luisi N, et al. Nationally representative social contact patterns among US adults, August 2020-April 2021. Epidemics. (2022) 40:100605. doi: 10.1016/j.epidem.2022.100605
5. Murti M, Achonu C, Smith BT, Brown KA, Kim JH, Johnson J, et al. COVID-19 workplace outbreaks by industry sector and their associated household transmission, Ontario, Canada, January to June, 2020. J Occup Environ Med. (2021) 63:574. doi: 10.1097/JOM.0000000000002201
6. Bonde JPE, Begtrup LM, Coggon D, Jensen JH, Flachs EM, Jakobsson K, et al. COVID-19-related hospital admission in spouses of partners in at-risk occupations. Scand J Work Environ Health. (2023) 1–8. doi: 10.5271/sjweh.4080
7. de Man P, Paltansing S, Ong DSY, Vaessen N, van Nielen G, Koeleman JGM. Outbreak of coronavirus disease 2019 (COVID-19) in a nursing home associated with aerosol transmission as a result of inadequate ventilation. Clin Infect Dis. (2021) 73:170–1. doi: 10.1093/cid/ciaa1270
8. Gettings J, Czarnik M, Morris E, Haller E, Thompson-Paul AM, Rasberry C, et al. Mask use and ventilation improvements to reduce COVID-19 incidence in elementary schools—Georgia, November 16–December 11, 2020. Morb Mortal Wkly Rep. (2021) 70:779. doi: 10.15585/mmwr.mm7021e1
9. Peters TM, Rabidoux D, Stanier CO, Anthony TR. Assessment of university classroom ventilation during the COVID-19 pandemic. J Occup Environ Hyg. (2022) 19:295–301. doi: 10.1080/15459624.2022.2053142
10. Centers for Disease Control and Prevention. Prioritizing NON-HEALTHCARE WORKSITE ASSESSMENTS for Coronavirus Disease 2019 (COVID-19). Atlanta, GA (2020).
11. Centers for Disease Control and Prevention. Prioritizing Case Investigations and Contact Tracing for COVID-19 in High Burden Jurisdictions. Atlanta, GA (2020).
12. Bonwitt J, Deya RW, Currie DW, Lipton B, Huntington-Frazier M, Sanford SJ, et al. COVID-19 surveillance and investigations in workplaces—Seattle & King County, Washington, June 15–November 15, 2020. Morb Mortal Wkly Rep. (2021) 70:916. doi: 10.15585/mmwr.mm7025a3
13. Massoudi BL, Chester K, Shah GH. Public health staff development needs in informatics: findings from a national survey of local health departments. J Public Heal Manag Pract. (2016) 22:S58. doi: 10.1097/PHH.0000000000000450
14. Hall K, Brees K, McCall T, Cunningham M, Alford A. 2020 Forces of Change: The COVID-19 Edition Washington DC. (2022). Available online at: https://www.naccho.org/uploads/downloadable-resources/2020-Forces-of-Change-The-COVID-19-Edition.pdf (accessed November 5, 2022).
15. World Health Organization. Pulse Survey on Continuity of Essential Health Services During the COVID-19 Pandemic: Interim Report, 27 August 2020. Geneva: World Health Organization (2020).
16. World Health Organization. Second Round of the National Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic: January-March 2021: Interim Report, 22 April 2021. Geneva: World Health Organization (2021).
17. Marcondes FO, Cheng D, Warner ET, Kamran SC, Haas JS. The trajectory of racial/ethnic disparities in the use of cancer screening before and during the COVID-19 pandemic: a large US academic center analysis. Prev Med. (2021) 151:106640. doi: 10.1016/j.ypmed.2021.106640
18. Kendzerska T, Zhu DT, Gershon AS, Edwards JD, Peixoto C, Robillard R, et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthc Policy. (2021) 14:575–84. doi: 10.2147/RMHP.S293471
19. Zhu D, Ozaki A, Virani SS. Disease-specific excess mortality during the COVID-19 pandemic: an analysis of weekly US death data for 2020. Am J Public Health. (2021) 111:1518–22. doi: 10.2105/AJPH.2021.306315
20. Hale NL, Klaiman T, Beatty KE, Meit MB. Local health departments as clinical safety net in rural communities. Am J Prev Med. (2016) 51:706–13. doi: 10.1016/j.amepre.2016.05.012
21. Su CP, De Perio MA, Cummings KJ, McCague AB, Luckhaupt SE, Sweeney MH. Case investigations of infectious diseases occurring in workplaces, United States, 2006-2015. Emerg Infect Dis. (2019) 25:397. doi: 10.3201/eid2503.180708
22. United States Census Bureau. Population Housing Unit Estimates Tables. (2019). Available online at: https://www.census.gov/programs-surveys/popest/data/tables.2019.List_58029271.html#list-tab-List_58029271 (accessed November 5, 2022).
23. Centers for Disease Control Prevention (CDC). Health Department Sites and Governance. (2020). Available online at: https://www.cdc.gov/publichealthgateway/sitesgovernance/index.html (accessed November 5, 2022).
24. Pilkington W, Kumar D. Public Health Departments Face Formidable Issues During COVID-19 Pandemic. Homeland Security Affairs (2020). p. 16. Available online at: www.hsaj.org/articles/16340
25. DeSalvo KB, Wang YC, Harris A, Auerbach J, Koo D, O'Carroll P. Public health 3.0: a call to action for public health to meet the challenges of the 21st century. Prev Chronic Dis. (2017) 14:E78. doi: 10.5888/pcd14.170017
26. Sellers K, Leider JP, Gould E, Castrucci BC, Beck A, Bogaert K, et al. The state of the US governmental public health workforce, 2014–2017. Am J Public Health. (2019) 109:674–80. doi: 10.2105/AJPH.2019.305011
27. Brownson RC, Burke TA, Colditz GA, Samet JM. Reimagining public health in the aftermath of a pandemic. Am J Public Health. (2020) 110:1605–10. doi: 10.2105/AJPH.2020.305861
28. Alford AA, Feeser K, Kellie H, Biesiadecki L. Prioritization of public health emergency preparedness funding among local health departments preceding the COVID-19 pandemic: findings from NACCHO's 2019 national profile of local health departments. J Public Heal Manag Pract. (2021) 27:215. doi: 10.1097/PHH.0000000000001338
29. Maani N, Galea S. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. (2020) 98:250. doi: 10.1111/1468-0009.12463
30. Stone KW, Kintziger KW, Jagger MA, Horney JA. Public health workforce burnout in the COVID-19 response in the US. Int J Environ Res Public Health. (2021) 18:4369. doi: 10.3390/ijerph18084369
Keywords: COVID-19, occupational exposure, public health practice, prevention, workplace, SARS-CoV-2
Citation: Bonney T and Grant MP (2023) Local health department engagement with workplaces during the COVID-19 pandemic—Examining barriers of and facilitators to outbreak investigation and mitigation. Front. Public Health 11:1116872. doi: 10.3389/fpubh.2023.1116872
Received: 05 December 2022; Accepted: 28 February 2023;
Published: 17 March 2023.
Edited by:
Ozayr Mahomed, University of KwaZulu-Natal, South AfricaReviewed by:
Tran B. Huynh, Drexel University, United StatesAdam Hege, Appalachian State University, United States
Copyright © 2023 Bonney and Grant. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tessa Bonney, dGJvbm5lNUB1aWMuZWR1
 Tessa Bonney
Tessa Bonney Michael P. Grant2
Michael P. Grant2