- 1Xiangya School of Nursing, Central South University, Changsha, China
- 2School of Public Health, Yale University, New Haven, CT, United States
Introduction: Delayed antiretroviral therapy (ART) initiation is associated with poor HIV outcomes and a higher likelihood of HIV transmission.
Methods: This cross-sectional study assessed the proportion of delayed ART initiation which was defined as initiating ART after 30 days of HIV diagnosis, and evaluated the pathways influencing ART initiation among adult PLWH in Changsha, China who were diagnosed between 2014 and 2022.
Results: Of 518 participants, 37.8% delayed in initiating ART. Based on the theory of reasoned action (TRA), delayed initiation was indirectly associated with perceptions toward ART through the mediating pathway of patients’ treatment willingness, with treatment willingness significantly being the full mediator.
Discussion: The findings may guide the development of interventions to improve timely uptake of ART in people who are newly diagnosed with HIV.
1. Introduction
Acquired immunodeficiency syndrome (AIDS) continues to be a global health crisis. Over 38 million people are living with HIV and 10 million do not have access to antiretroviral therapy (ART). There is no preventive vaccine or complete cure for HIV yet. However, people living with HIV (PLWH) can lead long and healthy lives by taking medicines that keep the virus undetectable, and people who maintain an undetectable viral load for at least six months are highly unlikely to transmit HIV through sex (1, 2). Since 2013, the Chinese Center for Disease Control and Prevention (CDC) has started a pilot program for early initiation of ART (3) and then rolled it out across the country in the subsequent years. ART coverage rate among PLWH in China was only 59.0% in 2014, and increased to 83.4% by 2018 (4). About 70% of HIV infected men who have sex with men intended to receive ART but about 60% were on ART in 2016 (5, 6). These findings suggested that there are significant gaps in ART initiation among PLWH in China. Delayed ART initiation can affect both treatment outcomes and the patient’s quality of life (7). The late onset of ART is strongly associated with lower immunologic response, poor virologic suppression, and a higher likelihood of developing related complications (8), and ultimately leads to treatment failure and even AIDS-related death (9). Studies have confirmed that timely initiation of ART can improve care engagement, shorten the duration of virologic suppression (10), and improve the health and life expectancy of HIV patients (9). Meanwhile, early initiation of ART significantly reduces HIV transmission (11). However, up to 30% of PLWH might delay their treatment both in developed and developing countries (12, 13, 14). The attitude and knowledge of clinicians (15), the interface of services between facilities, and limited resources have been reported as external factors affecting ART initiation (16, 17). Patients’ personal factors may also contribute to delayed initiation, such as demographic factors including low income, low education, and lack of household decision-making power (18), HIV-related characteristics (14), mental health (19, 20), and perceptions toward ART (21). Patients’ willingness to start treatment also influences the decision of ART initiation (22). However, no study has explored the pathway relationships and mechanisms of action among these factors. Identifying the possible pathways of influence will help with developing targeted interventions to promote timely ART initiation. We conducted a cross-sectional study in Changsha, China for assessing the perceptions toward ART and factors associated with delayed ART initiation among PLWH.
2. Methods
2.1. Study design and participants
This cross-sectional study was conducted among patients in the HIV clinic of a tertiary referral hospital in Changsha City, China. Patients who were aged 18 years or older and were diagnosed with HIV between 2014 and 2022 were invited to participate in the study. The sample size was calculated based on the precision of estimating the proportion of self-reported delay in ART initiation among participants. With an assumed 30% delay rate, a sample size of 323 or more participants is needed to have a 5% margin error with a 95% confidence level.
Each participant provided informed consent. The study was approved by the research ethics review committee of Xiangya School of Nursing, Central South University (NO. E2021134).
2.2. Data collection
A structured questionnaire was used to collect data during face-to-face interviews from October 2021 to June 2022. The questionnaire consisted of three parts: (1) socio-demographics including sex, age, place of residence, occupation, and sexual orientation; (2) HIV diagnosis and status including the year of HIV diagnosis, time of ART initiation, recent CD4 count, comorbidity; (3) perceptions toward ART and willingness to use ART.
Two investigators who had experience in working with PLWH conducted data collection. When patients were waiting to see a doctor in the HIV clinic, the clinic nurse referred them to meet the investigators. The investigator introduced the study and obtained a written consent from the patients who were interested in participating in the study and met the inclusion criteria. The investigators conducted a one-to-one interview with each participant in a private room and completed the questionnaire. They also verified key questionnaire information through cross-checking their electronic medical records including the dates of HIV diagnosis and ART initiation. If there were discrepancies between patient’s reported information and electronic records, the electronic records were used.
Delayed ART initiation: Delay ART initiation was defined if a participant started ART after 30 days of HIV diagnosis (23–25). This was based on self-report and was verified by checking patients’ electronic medical records.
Perceptions toward ART: The Health Belief Model-related ART perceptions scale was used to measure patients’ perceptions toward ART (21). This scale contains 8 domains including subjective norms, perceived severity, perceived susceptibility, perceived benefits, perceived barriers, perceptions on balance, self-efficacy, and cues to action. This scale has 26 items with a total score of 122, including 24 using a 5-point scale (from 1 = “extremely disagree” to 5 = “extremely agree”) and 2 using a yes or no option (1 = “yes,” 0 = “no”). A higher score represents high ART perception. In this study, this measure showed good internal consistency (Cronbach’s α = 0.830).
Treatment willingness: Participants were asked to rate their willingness to use ART on a scale from 1 to 10, with 1 representing the lowest willingness and 10 representing the highest willingness. The 10 points scoring format is simple to use and easier to understand for PLWH (26).
2.3. Statistical analysis
Double data entry was performed using the software Epidata 3.1. Descriptive and univariate analyses were performed using SPSS24.0. T-tests for continuous variables and chi-square (χ2) tests for categorical variables were used to compare two groups of delayed and timely ART initiation. A chi-square trend test was performed for the proportions of timely ART initiation over calendar years of HIV diagnosis.
The theory of reasoned action (TRA) was used to guide the development of the research questions, hypotheses, and the path analysis model. TRA proposes that attitude and subjective norms indirectly influence the occurrence of behavior by acting on behavioral willingness within human action (27). We hypothesized that attitudes toward ART and subjective norms influence ART initiation among PLWH through the treatment willingness as a mediator (Figure 1). Path analysis was performed using Mplus8.3. We used six goodness of fit indices to assess the model, including χ2, the ratio of χ2 over the degree of freedom (χ2/df), comparative fit index (CFI), Tucker Lewis index (TLI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). χ2 value with p>0.05, χ2/df between 1 and 3, RMSEA<0.07 (28), CFI and TLI values >0.95, and SRMR<0.08 (29) were considered acceptable. For the categorical outcome variable (delayed initiation or not), we used a Weighted Least Squares Mean Variance adjusted (WLSMV) parameter estimation algorithm which works best for the ordinal data in the Mplus (30). We calculated 95% confidence intervals (CIs) with 5,000 bootstrap samples for total effect, indirect effect, and direct effect.
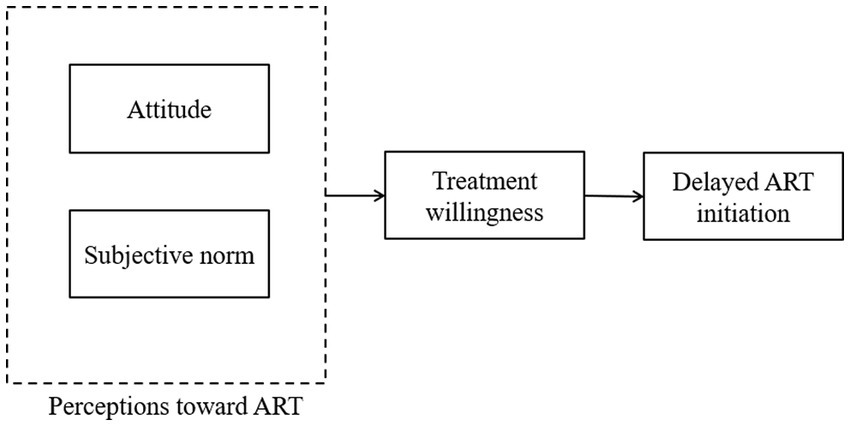
Figure 1. Hypothesized model for delayed initiation of ART based on the Theory of Reasoned Action. ART, antiretroviral therapy.
3. Results
Of 536 patients who participated in the study, 18 (3.4%) did not complete the study procedures and were excluded, and 518 were included in the analysis. Age ranged from 18 to 76 years (mean, 32.2; standard deviation (SD), 10.3). About 96% were male. The average duration of HIV diagnosis was 4.2 (SD, 2.3) years. The average time from diagnosis to ART initiation was 4.1 (SD, 11.2) months. The average score of willingness to initiate ART after diagnosis was 8.1 (SD, 2.9), and the average score of perceptions toward ART was 90.4 (SD, 13.3).
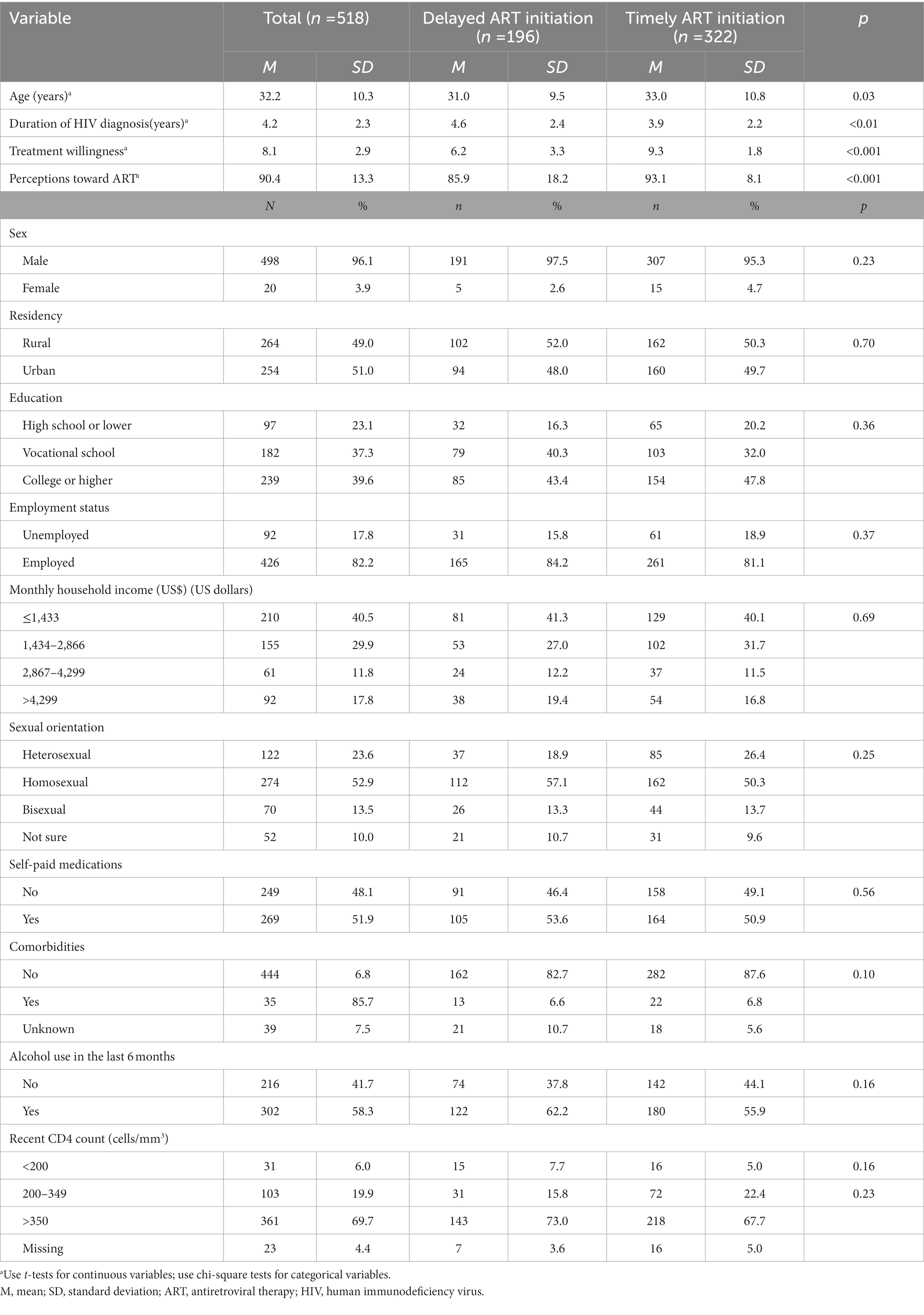
About one-third (37.8%) of patients delayed in initiating ART treatment. Table 1 shows the characteristics of participants who delayed initiation of ART and those who timely initiated ART. Patients who delayed initiation were younger than those who had timely initiation. Year of HIV diagnosis was significantly associated with delayed ART initiation (p<0.01), and there was an increasing trend of ART timely initiation since 2014 (trend χ2 = 10.514, p<0.01, Figure 2). In addition, treatment willingness (p<0.001) and perceptions toward ART (p<0.001) were also significantly associated with delayed ART initiation.
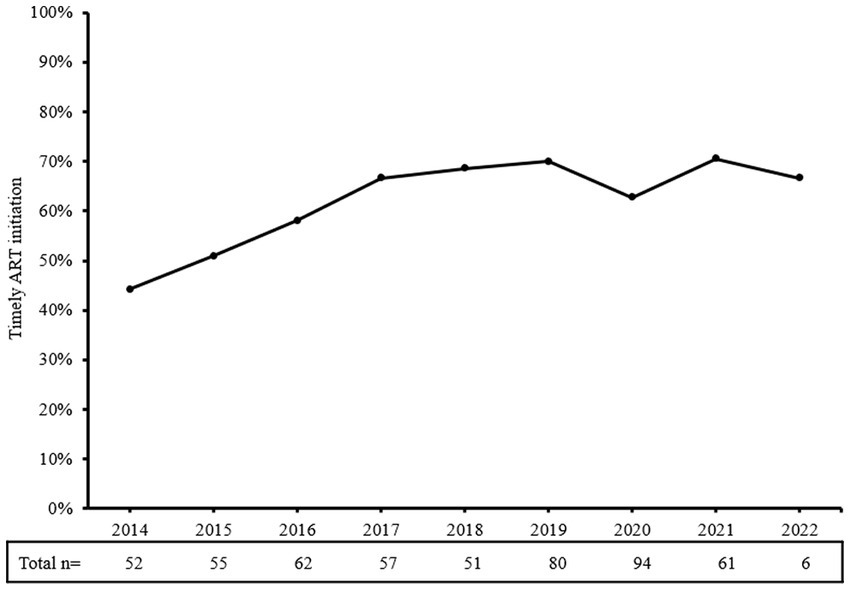
Figure 2. Proportions of timely initiation of ART among people who were newly diagnosed with HIV in the years 2014–2022. Timely initiation of ART has trended upward since 2014, although there was a small decline in 2020. ART, antiretroviral therapy.
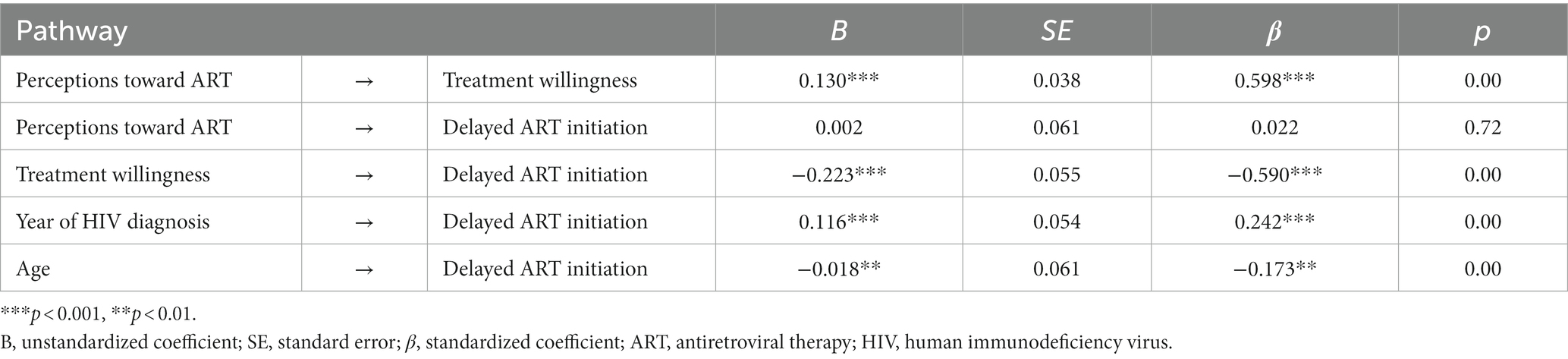
Age and year of HIV diagnosis were included in path analysis mode based on the univariate analysis and review (31). This model was tested and presented sufficient goodness of fit value, and the model fit indices included χ2 = 5.911 (p = 0.052), χ2/df = 2.955 (df = 2), CFI = 0.991, TLI =0.967, RMSEA = 0.061, and SRMR = 0.024. Table 2 shows that the standardized path coefficients (β) between delayed ART initiation and perceptions toward ART, treatment willingness, year of HIV diagnosis, and age are 0.022 (p = 0.72), −0.590 (p < 0.001), 0.242 (p < 0.001) and-0.173 (p < 0.01), respectively. Specifically, perceptions toward ART have a direct and positive association with treatment willingness (β = 0.598, p < 0.001).
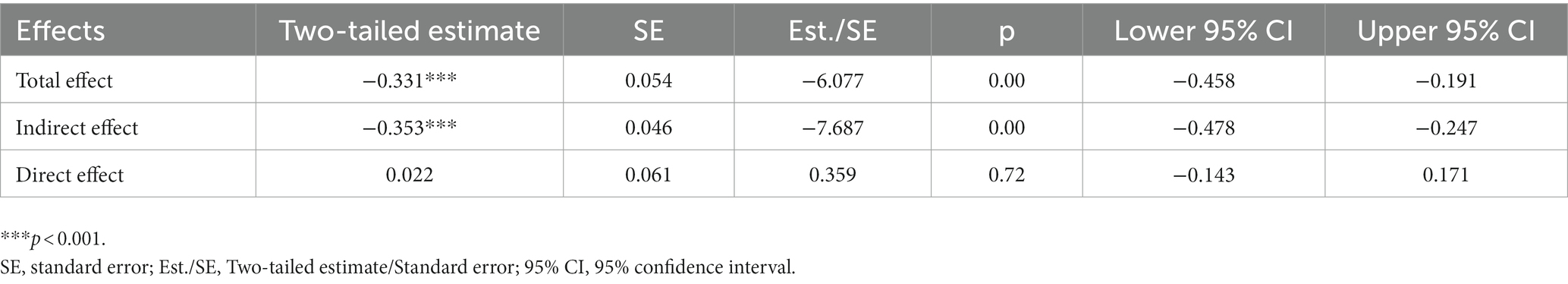
For the total mediated model (Figure 3 and Table 3), the total effect is-0.331 (p < 0.001, 95%CI: −0.458 to-0.191), the indirect effect is-0.353 (p < 0.001, 95%CI: −0.478 to-0.247), and the direct effect is 0.022 (p = 0.72, 95%CI: −0.143 to 0.171). The direct effect or the effect of perceptions toward ART on delayed ART initiation controlling for age and years of HIV diagnosis is non-statistically significant, therefore, treatment willingness plays a fully mediating role in the impact of perceptions toward ART on delayed ART initiation.
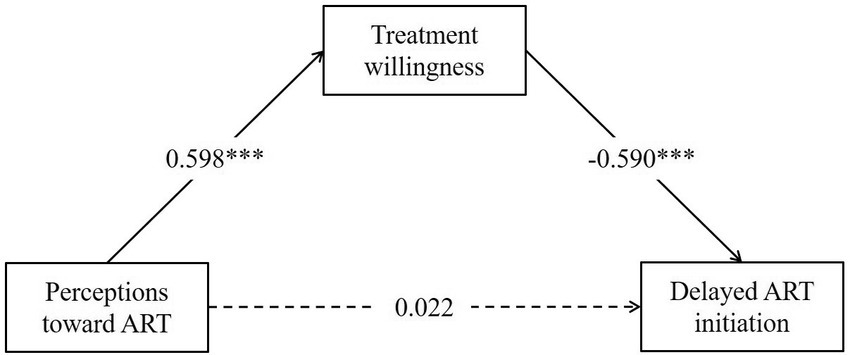
Figure 3. Model for perceptions toward ART and delayed ART initiation among people living with HIV in Changsha, China. The solid line indicates that the pathway is significant and the dashed line is insignificant. Treatment willingness plays a fully mediating role in the impact of perceptions toward ART on delayed ART initiation. ART, antiretroviral therapy. ***p < 0.001.
4. Discussion
This study showed a 37.8% proportion of delayed ART initiation among PLWH in Changsha, China during 2014–2022. It is significantly lower than the national average between the year 2011–2014 (76.6%) (25) and lower than the average rate during 2010–2015 in San Francisco, United States (62.0%) (32) and it is close to the rates reported in some studies in low-and middle-income countries, such as South Africa (33). Due to the changing definition of delayed ART initiation (8), caution should be taken when comparing the rates across regions and countries. While we used the definition in the current version of Chinese national ART guidelines, other studies may use different definitions, such as a specific CD4 count or a different duration from HIV diagnosis to ART initiation (24). This variation in definition may contribute to difference in the reported rates of delayed ART initiation so cautions should be taken when making direct comparison with other studies.
The overall trend of timely initiation rates increased over calendar years, and this is consistent with another study in China (34). It may be due to the continuous optimization of treatment policies and improvement of the HIV treatment environment (35). The decline in 2020 may be related to COVID-19 outbreak (36). ART interruption in 2022 has also been found in other regions such as South Africa (37). Measures taken to slow the transmission of COVID-19 and the additional strain placed on health systems have disrupted HIV treatment services (38). The greatest disruptions occurred in the first half of 2020 when many countries were in their first emergency embargo (37). Having access to timely ART was a concern in HIV care during the COVID-19 pandemic (39). In addition, morbidity and mortality associated with COVID-19, fear of transmission, and government response policies might lead to a reduction in ART initiation, especially for the vulnerable population among PLWH (37, 40).
This study demonstrated that the relationship between perceptions toward ART and delayed ART initiation was fully mediated by treatment willingness. It is consistent with findings from both qualitative and quantitative studies. A consolidation of qualitative evidence covering high-income countries, and low-and middle-income countries showed that perceptions toward ART were associated with delayed ART initiation (22, 41). Two cohort studies also demonstrated this association (42, 43). Poloko and colleagues found that individual treatment willingness also influenced ART initiation (44). However, unlike previous studies, our study found no direct impact of perceptions toward ART on delayed initiation, but rather through the mediation of treatment willingness. We need to be aware that there is a know-do gap between perceptions toward ART and initiation behavior (45). In practice, interventions that simply enhance ART perceptions may not directly help patients initiate ART as rapidly as possible; we still need to be mindful of patients’ treatment willingness and design targeted interventions to ensure that all patients are not left behind.
Our study pointed to a relationship between younger age and delayed ART initiation. Our findings were similar to a Swiss prospective cohort study, although delayed ART initiation of that study was defined by CD4 counts (46). A Canadian study that also used days to determine delayed initiation as we did was also consistent with our findings (14). However, unlike the study by Hassan et al. Age was not significantly associated with delayed initiation in their study. A historical cohort study contradicted us and concluded that older age was associated with delayed ART initiation (47). Such a difference may be due to the different regions and study periods of our study.
In addition, we found that economic-related components, including employment status, monthly household income, and self-paid medications were none significant. In general, researchers believe that patients with higher economic status are more likely to start ART early (14, 48). Yet, one study even found that monetary incentives continued to fail to facilitate ART initiation as soon as possible (49). These differences may be influenced by culture and policy in different study contexts. This also suggests that we can also try to explore new non-financial interventions to help patients initiate ART as soon as possible.
Our study validated the TRA model. First, our study further validated the theory by confirming the mediating role of treatment willingness. Second, we broadened the application of TRA in HIV care scenarios. In previous studies, TRA has been used mainly for medication adherence (50, 51), HIV self-testing (52), and condom use (53). To our knowledge, this is the first study of innovatively applying the TRA model for explaining ART initiation among PLWH, and study findings may serve as a scientific basis for developing interventions on ART treatment.
The study has limitations. First, this study does not provide causal inferences between perceptions toward ART and initiation of ART due to the nature of cross-sectional study design. Prospective cohort studies and intervention clinical trials are needed to assess the causal relationship. Second, data on perceptions and initiation of ART are based on self-report, and therefore, recall bias may exist. As patients were newly diagnosed with HIV between 2014 and 2022, most had been in treatment for a long time when they participated in this survey, and this may have influenced the findings on ART perceptions and reported dates on HIV diagnosis and ART initiation. We guided study participants through recalling their situation at the time of HIV diagnosis and incorporated prompts in the questionnaire to assist with memory recall. The information on the dates of HIV diagnosis and ART initiation was verified by checking patients’ electronic medical records to minimize the recall bias. However, recall bias is still possible. Third, although the number of participants exceeded the required sample size, only 3.9% of the participants were female. The low proportion of female participants may limit the generalizability of our study findings. Forth, delayed ART initiation was defined as initiating ART after 30 days of HIV diagnosis in this study regardless of patients’ disease status, but the recommendations for the time of initiating ART in both international and Chinese ART guidelines have been changing over time. This definition we used in this study may or may not cause bias in assessing the relationship between ART perception and initiation. Finally, this study was conducted in one city and the same participants could not represent all PLWH in China. Further research is warranted to replicate the study findings in other parts of China.
5. Conclusion
In conclusion, this study found a high proportion of delayed ART initiation among PLWH in Changsha, China and a fully mediating role of treatment willingness between perceptions toward ART and delayed ART initiation. The findings may guide the development of interventions for reducing delayed initiation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the research ethics review committee of Xiangya School of Nursing, Central South University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
YZ: design of methodology (lead), investigation (equal), data curation (lead), formal analysis (lead), visualization (lead), software (lead), original draft (lead), and review and editing (equal). YL: investigation (equal), data curation (supporting), and validity (lead). XX: conceptualization (equal) and design of methodology (supporting). H-ZQ: review and editing (equal). HW: supervision (lead), project administration (lead), funding acquisition (lead), conceptualization (equal), and review and editing (equal). All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the National Natural Science Foundation of China (No. 82273746) and the Provincial Natural Science Foundation of Hunan grant (No. 2022JJ30769). This research was also supported by the Hunan Provincial Innovation Foundation for Postgraduate (No. CX20220337) and the Fundamental Research Funds for the Central Universities of Central South University (No. 1053320213461).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cohen, MS, Chen, YQ, Mccauley, M, Gamble, T, Hosseinipour, MC, Kumarasamy, N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. (2011) 365:493–505. doi: 10.1056/NEJMoa1105243
2. Grinsztejn, B, Hosseinipour, MC, Ribaudo, HJ, Swindells, S, Eron, J, Chen, YQ, et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 Hptn 052 randomised controlled trial. Lancet Infect Dis. (2014) 14:281–90. doi: 10.1016/S1473-3099(13)70692-3
3. Xia, P, Okumura, J, Yan, P, Xie, M, Wu, S, Zhuang, M, et al. Steps towards preventive HIV treatment in Fujian, China: problems identified via an assessment of initial antiretroviral therapy provision. PLoS One. (2013) 8:E76483. doi: 10.1371/journal.pone.0076483
4. Zhao, Y, Han, M, Ma, Y, and Li, D. Progress towards the 90-90-90 targets for controlling HIV — China, 2018. China CDC Weekly. (2019) 1:4–7. doi: 10.46234/ccdcw2019.003
5. Yang, X, Wang, Z, Harrison, S, and Lau, JT. Coverage and adherence of antiretroviral therapy among Chinese HIV-positive men who have sex with men with high Cd4 counts in the era of ‘treat all’. Tropical Med Int Health. (2020) 25:308–18. doi: 10.1111/tmi.13353
6. Yang, X, Wang, Z, Wang, X, Ma, T, Xue, H, He, Y, et al. Behavioral intention to initiate antiretroviral therapy (art) among Chinese HIV-infected men who have sex with men having high Cd4 count in the era of “treatment for all”. Am J Mens Health. (2019) 13:1557988319828615. doi: 10.1177/1557988319828615
7. Nijhawan, AE, Kitchell, E, Etherton, SS, Duarte, P, Halm, EA, and Jain, MK. Half of 30-day hospital readmissions among HIV-infected patients are potentially preventable. AIDS Patient Care STDs. (2015) 29:465–73. doi: 10.1089/apc.2015.0096
8. Bai, R, Du, J, Lv, S, Hua, W, Dai, L, and Wu, H. Benefits and risks of rapid initiation of antiretroviral therapy: a systematic review and Meta-analysis. Front Pharmacol. (2022) 13:898449. doi: 10.3389/fphar.2022.898449
9. Xie, Y, Zhu, J, Lan, G, and Ruan, Y. Benefits of early art initiation on mortality among people with HIV. Lancet HIV. (2022) 9:E377. doi: 10.1016/S2352-3018(22)00098-4
10. O'shea, JG, Gallini, JW, Cui, X, Moanna, A, and Marconi, VC. Rapid antiretroviral therapy program: development and evaluation at a veterans affairs medical center in the southern United States. AIDS Patient Care STDs. (2022) 36:219–25. doi: 10.1089/apc.2022.0039
11. Cohen, MS, Chen, YQ, Mccauley, M, Gamble, T, Hosseinipour, MC, Kumarasamy, N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. (2016) 375:830–9. doi: 10.1056/NEJMoa1600693
12. Bantie, B, Kassaw Yirga, G, Abate, MW, Amare, AT, Nigat, AB, Tigabu, A, et al. Delayed art initiation in "test and treat era" and its associated factors among adults receiving antiretroviral therapy at public health institutions in Northwest Ethiopia: a multicenter cross-sectional study. PLoS One. (2022) 17:E0271127. doi: 10.1371/journal.pone.0271127
13. Fuge, TG, Tsourtos, G, and Miller, ER. Risk factors for late linkage to care and delayed antiretroviral therapy initiation amongst HIV infected adults in sub-Saharan Africa: a systematic review and Meta-analyses. Int J Infect Dis. (2022) 122:885–904. doi: 10.1016/j.ijid.2022.07.037
14. Mehraj, V, Cox, J, Lebouché, B, Costiniuk, C, Cao, W, Li, T, et al. Socio-economic status and time trends associated with early ART initiation following primary HIV infection in Montreal, Canada: 1996 to 2015. J Int AIDS Soc. (2018) 21:e25034. doi: 10.1002/jia2.25034
15. Barbosu, CM, Alcántara, L, Sharma, S, Marriott, J, Babiy, O, Deamer, R, et al. The implementation of a state-wide rapid initiation of antiretroviral therapy as a best practice in primary care practices using an academic detailing approach: lessons learned from New York state, United States. Int J Mch Aids. (2022) 11:E539. doi: 10.21106/ijma.539
16. Harkness, A, Wawrzyniak, AJ, Kolber, MA, Villamizar, K, Botero, V, Rodriguez, JE, et al. Multilevel determinants of rapid antiretroviral treatment implementation and demand in Miami-Dade County. J Acquir Immune Defic Syndr. (2022) 90:S177–89. doi: 10.1097/QAI.0000000000002978
17. Pettit, AC, Pichon, LC, Ahonkhai, AA, Robinson, C, Randolph, B, Gaur, A, et al. Comprehensive process mapping and qualitative interviews to inform implementation of rapid linkage to HIV care programs in a mid-sized urban setting in the southern United States. J Acquir Immune Defic Syndr. (2022) 90:S56–64. doi: 10.1097/QAI.0000000000002986
18. Parcesepe, AM, Lahuerta, M, Lamb, MR, Ahoua, L, Abacassamo, F, and Elul, B. Household decision-making and HIV care continuum outcomes among women living with HIV in Mozambique. AIDS Patient Care STDs. (2020) 34:173–83. doi: 10.1089/apc.2019.0268
19. Tao, J, Vermund, SH, Lu, H, Ruan, Y, Shepherd, BE, Kipp, AM, et al. Impact of depression and anxiety on initiation of antiretroviral therapy among men who have sex with men with newly diagnosed HIV infections in China. AIDS Patient Care STDs. (2017) 31:96–104. doi: 10.1089/apc.2016.0214
20. Xie, J, Wang, Z, Li, Q, He, Q, Xu, G, Li, Y, et al. Associations between antiretroviral therapy-related experiences and mental health status among people living with HIV in China: a prospective observational cohort study. AIDS Res Ther. (2021) 18:60. doi: 10.1186/s12981-021-00370-y
21. Du, X, He, Q, Yang, T, Wang, Y, Xu, H, Hao, C, et al. Intention to start art after the launch of expanded treatment strategy among people living with HIV in China: a behavioral theory-based cross-sectional study. AIDS Care. (2020) 32:1182–90. doi: 10.1080/09540121.2019.1686601
22. Ahmed, S, Autrey, J, Katz, IT, Fox, MP, Rosen, S, Onoya, D, et al. Why do people living with Hiv not initiate treatment? A systematic review of qualitative evidence from low-and middle-income countries. Soc Sci Med. (2018) 213:72–84. doi: 10.1016/j.socscimed.2018.05.048
23. Massanella, M, Bender Ignacio, RA, Lama, JR, Pagliuzza, A, Dasgupta, S, Alfaro, R, et al. Long-term effects of early antiretroviral initiation on HIV reservoir markers: a longitudinal analysis of the Merlin clinical study. Lancet Microbe. (2021) 2:E198–209. doi: 10.1016/S2666-5247(21)00010-0
24. Zhao, Y, Mcgoogan, JM, and Wu, Z. The benefits of immediate art. J Int Assoc Provid Aids Care. (2019) 18:2325958219831714. doi: 10.1177/2325958219831714
25. Zhao, Y, Wu, Z, Mcgoogan, JM, Sha, Y, Zhao, D, Ma, Y, et al. Nationwide cohort study of antiretroviral therapy timing: treatment dropout and Virological failure in China, 2011-2015. Clin Infect Dis. (2019) 68:43–50. doi: 10.1093/cid/ciy400
26. Dawes, J. Do data characteristics change according to the number of scale points used? An experiment using 5-point, 7-point and 10-point scales. Int J Mark Res. (2008) 50:61–104. doi: 10.1177/147078530805000106
27. Hill, RJ, Fishbein, M, and Ajzen, I. Belief, attitude, intention and behavior: an introduction to theory and research. Contemp Sociol. (1977) 6:244. doi: 10.2307/2065853
28. Steiger, JH. Understanding the limitations of global fit assessment in structural equation modeling. Personal Individ Differ. (2007) 42:893–8. doi: 10.1016/j.paid.2006.09.017
29. Hu, L-T, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
30. Flora, DB, and Curran, PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol Methods. (2004) 9:466–91. doi: 10.1037/1082-989X.9.4.466
31. Mccoy, K, Lipira, L, Kemp, CG, Nevin, PE, Huh, DJMT, Mugavero, MJ, et al. Exploring HIV-related stigma as a determinant of engagement in HIV care by African American women. J Assoc Nurses AIDS Care. (2020) 31:167–75. doi: 10.1097/JNC.0000000000000140
32. Truong, HM, Pipkin, S, Grant, RM, Liegler, T, Okeefe, KJ, and Scheer, S. Increased uptake of early initiation of antiretroviral therapy and baseline drug resistance testing in San Francisco between 2001 and 2015. PLoS One. (2019) 14:E0213167. doi: 10.1371/journal.pone.0213167
33. Onoya, D, Sineke, T, Hendrickson, C, Mokhele, I, Maskew, M, Long, LC, et al. Impact of the test and treat policy on delays in antiretroviral therapy initiation among adult HIV positive patients from six clinics in Johannesburg, South Africa: results from a prospective cohort study. BMJ Open. (2020) 10:E030228. doi: 10.1136/bmjopen-2019-030228
34. Wu, C, Zhang, B, Dai, Z, Zheng, Q, Duan, Z, He, Q, et al. Impact of immediate initiation of antiretroviral therapy among men who have sex with men infected with HIV in Chengdu, Southwest China: trends analysis, 2008-2018. BMC Public Health. (2021) 21:689. doi: 10.1186/s12889-021-10580-8
35. Liu, Z, Tang, X, Liu, Y, Zhang, L, Yang, Y, Zheng, Y, et al. HIV prevention and health poverty alleviation – Liangshan prefecture, Sichuan Province, China, 2017-2020. China Cdc Wkly. (2021) 3:1031–5. doi: 10.46234/ccdcw2021.250
36. Yang, X, Zeng, C, Tam, CC, Qiao, S, Li, X, Shen, Z, et al. HIV service interruptions during the Covid-19 pandemic in China: the role of Covid-19 challenges and institutional response from healthcare Professional's perspective. AIDS Behav. (2022) 26:1270–8. doi: 10.1007/s10461-021-03484-6
37. Benade, M, Long, L, Rosen, S, Meyer-Rath, G, Tucker, JM, and Miot, J. Reduction in initiations of HIV treatment in South Africa during the Covid pandemic. BMC Health Serv Res. (2022) 22:428. doi: 10.1186/s12913-022-07714-y
38. Wu, X, Wu, G, Ma, Y, Huang, X, Yang, Y, Cai, Y, et al. The impact of Covid-19 non-pharmaceutical interventions on HIV care continuum in China: an interrupted time series analysis. Lancet Reg Health West Pac. (2022) 29:100569. doi: 10.1016/j.lanwpc.2022.100569
39. Jiang, H, Zhou, Y, and Tang, W. Maintaining HIV care during the Covid-19 pandemic. Lancet HIV. (2020) 7:E308–9. doi: 10.1016/S2352-3018(20)30105-3
40. Vrazo, AC, Golin, R, Fernando, NB, Killam, WP, Sharifi, S, Phelps, BR, et al. Adapting HIV services for pregnant and breastfeeding women, infants, children, adolescents and families in resource-constrained settings during the Covid-19 pandemic. J Int AIDS Soc. (2020) 23:E25622. doi: 10.1002/jia2.25622
41. Hollingdrake, O, Lui, CW, Mutch, A, Dean, J, Howard, C, and Fitzgerald, L. Factors affecting the decision to initiate antiretroviral therapy in the era of treatment-as-prevention: synthesis of evidence from qualitative research in high-income settings. AIDS Care. (2019) 31:397–402. doi: 10.1080/09540121.2018.1533235
42. Gebru, T, Lentiro, K, and Jemal, A. Perceived Behavioural predictors of late initiation to HIV/Aids care in Gurage zone public health facilities: a cohort study using health belief model. BMC Res Notes. (2018) 11:336. doi: 10.1186/s13104-018-3408-4
43. Yang, T, Yang, X, Li, L, Xu, H, Fan, L, Li, Q, et al. HIV diagnosis period influences art initiation: findings from a prospective cohort study in China. AIDS Res Ther. (2021) 18:59. doi: 10.1186/s12981-021-00379-3
44. Kebaabetswe, P, Manyake, K, Kadima, E, Auletta-Young, C, Chakalisa, U, Sekoto, T, et al. Barriers and facilitators to linkage to care and art initiation in the setting of high art coverage in Botswana. AIDS Care. (2020) 32:722–8. doi: 10.1080/09540121.2019.1640843
45. Grimsrud, A, Wilkinson, L, Eshun-Wilson, I, Holmes, C, Sikazwe, I, and Katz, IT. Understanding engagement in HIV Programmes: how health services can adapt to ensure no one is left behind. Curr HIV/AIDS Rep. (2020) 17:458–66. doi: 10.1007/s11904-020-00522-1
46. Wolbers, M, Bucher, HC, Furrer, H, Rickenbach, M, Cavassini, M, Weber, R, et al. Delayed diagnosis of HIV infection and late initiation of antiretroviral therapy in the Swiss HIV cohort study. HIV Med. (2008) 9:397–405. doi: 10.1111/j.1468-1293.2008.00566.x
47. Afrashteh, S, Fararouei, M, Ghaem, H, and Gheibi, Z. Factors associated with late antiretroviral therapy initiation among people living with Hiv in southern Iran: a historical cohort study. Front Public Health. (2022) 10:881069. doi: 10.3389/fpubh.2022.881069
48. Tefera, E, and Mavhandu-Mudzusi, AH. Experiences of antiretroviral therapy initiation among HIV-positive adults in Ethiopia: a descriptive phenomenological design. HIV Aids (Auckl). (2022) 14:243–54. doi: 10.2147/HIV.S361913
49. Maughan-Brown, B, Smith, P, Kuo, C, Harrison, A, Lurie, MN, Bekker, LG, et al. A conditional economic incentive fails to improve linkage to care and antiretroviral therapy initiation among HIV-positive adults in Cape Town, South Africa. AIDS Patient Care STDs. (2018) 32:70–8. doi: 10.1089/apc.2017.0238
50. Gill, MM, Umutoni, A, Hoffman, HJ, Ndatimana, D, Ndayisaba, GF, Kibitenga, S, et al. Understanding antiretroviral treatment adherence among HIV-positive women at four postpartum time intervals: qualitative results from the Kabeho study in Rwanda. AIDS Patient Care STDs. (2017) 31:153–66. doi: 10.1089/apc.2016.0234
51. Momplaisir, FM, Fortune, K, Nkwihoreze, H, Groves, AK, Aaron, E, and Jemmott, JB 3rd. Outcome expectancies toward adherence to antiretroviral therapy for pregnant and postpartum women with HIV. Womens Health (Lond). (2021) 17:174550652110610. doi: 10.1177/17455065211061094
52. Schnall, R, John, RM, and Carballo-Dieguez, A. Do high-risk Young adults use the HIV self-test appropriately? Observations from a think-aloud study. AIDS Behav. (2016) 20:939–48. doi: 10.1007/s10461-015-1240-6
Keywords: human immunodeficiency virus, antiretroviral therapy (ART), delayed initiation, treatment willingness, perception
Citation: Zhou Y, Li Y, Xiao X, Qian H-Z and Wang H (2023) Perceptions toward antiretroviral therapy and delayed ART initiation among people living with HIV in Changsha, China: mediating effects of treatment willingness. Front. Public Health. 11:1105208. doi: 10.3389/fpubh.2023.1105208
Edited by:
Devasena Gnanashanmugam, Cepheid, United StatesReviewed by:
Zixin Wang, The Chinese University of Hong Kong, ChinaSheila Araujo Teles, Universidade Federal de Goiás, Brazil
Copyright © 2023 Zhou, Li, Xiao, Qian and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Honghong Wang, aG9uZ2hvbmdfd2FuZ0Bob3RtYWlsLmNvbQ==
 Yaqin Zhou
Yaqin Zhou Yixuan Li
Yixuan Li Xueling Xiao
Xueling Xiao Han-Zhu Qian2
Han-Zhu Qian2 Honghong Wang
Honghong Wang