- 1Department of Public Health, Asian University for Women, Chittagong, Bangladesh
- 2Department of Gender Studies, Asian University for Women, Chittagong, Bangladesh
Objectives: Bangladesh has one of the highest adolescent childbearing rates in South Asia, which prevent women from realizing their full potential in life. This study aimed to compare the prevalence and determinants of adolescent childbearing in Bangladesh using data from the 2014 and 2017–18 Bangladesh Demographic and Health Survey (BDHS).
Methods: Nationally representative surveys of respondents were selected using a two-stage sampling process. The study recruited 2,023 and 1,951 ever-married women aged 15–19 from 2014 and 2017–18 BDHS surveys, respectively, from rural and urban settings from all eight geographic divisions of Bangladesh. Univariate and multivariate logistic regression models were fit to determine the factors associated with adolescent childbearing.
Result: The adolescent childbearing prevalence rate was 30.8% in 2014 BDHS and 27.6% in 2017–18 BDHS. Marriage at age 13 years or less also reduced significantly in 2017–18 compared to 2014 (12.7% vs. 17.4%, respectively). Significantly higher odds of adolescent childbearing were found in 2014 among women in the Sylhet Division (adjusted odds ratio (AOR) = 3.0; 95% confidence interval (CI): 1.6–6.1) and the Chittagong Division (AOR = 1.8; 95% CI: 1.8–2.7) compared to the Barisal Region; however, in 2017, there were no significant differences was found across the geographic Divisions. Compared to women in the lowest wealth quintile, women in all other quintiles had lower odds of adolescent childbearing, with the lowest odds found among women in the wealthiest quintile (AOR = 0.3; 95% CI: 0.2–0.6). Women who married at age 14–17 had 60% lower odds of adolescent childbearing compared to the women who married at age 10–13.
Conclusion: Nearly one-third of married adolescents in Bangladesh were pregnant or had at least one child in 2014, and it was reduced only marginally in 2017–18. Marriage at an early age and income inequalities among families were significant predictors of adolescent childbearing in Bangladesh. This study highlighted change in the magnitude and determinants of adolescent childbearing in Bangladesh taken data from two nationally representative surveys conducted 4 years apart.
Introduction
Remarkable progress has been made globally in reducing early marriage, adolescent childbearing, and maternal mortality over the past few decades, although adolescent childbearing remains a social and public health concern (1–3). The fact that every year approximately 12 million girls age 15–19 give birth in low and middle-income countries is evidence of this grave concern (4, 5). Adolescent pregnancy and childbearing have deleterious consequences at the individual, societal and global levels (6, 7). Adolescent motherhood negatively affects a girl’s health, wellbeing, and educational progress, and prevents her from realizing her full potential (8–12).
Adolescent childbearing is the consequence of complex relationships with multiple factors. High pregnancy rates among adolescent girls are associated with lack of education, less decision-making power in household and family planning, less reproductive knowledge, poverty, and the experience of early marriage (6, 8, 13, 14). The age difference between spouses is also an influential factor in determining early pregnancy (15, 16). Adolescent childbearing rates often are higher in countries where early marriage is prevalent (17, 18). Girls who marry at young ages are more likely to experience multiple pregnancies, recurrent miscarriage, termination of pregnancy, and delivery complications (19, 20). One-third of married teenage girls in Bangladesh become mothers or are pregnant by their 18th birthday (18).
Bangladesh has one of the highest rates of adolescent fertility in South Asia, where 1 girl in 10 has a child before the age of 15 whereas 1 in 3 adolescent becomes mother or pregnant by the age of 19., Adolescent fertility has been one of the widely discussed issues where scientific literature highlighting the social, economic, and reproductive health consequences, particularly connected to a growing risk of intrauterine growth restriction, child undernutrition, preterm birth, and infant mortality (20–23). However, only limited progress has been made thus far mainly because of insufficient attention from policymakers and lack of coordinated efforts by government, non-government, and community-based organizations (24–26). The Government of Bangladesh ratified strict laws against early marriage, however, its success will be grounded on holistic approaches that promote social mobilization and other structural interventions including poverty alleviation, gender equity, and girl’s education that prevent early marriage and reduce the high rate of adolescent pregnancy in Bangladesh (20, 27).
Achieving further improvement in lowering adolescent pregnancy rates is a priority for Bangladesh in achieving the Sustainable Development Goals (SDG) targets such as Goal 3 on good health and wellbeing, and Goal 5 on gender equality of girls and women (28). This study compared the prevalence of adolescent childbearing and the factors associated with adolescent pregnancy by using data collected by the nationally representative Bangladesh Demographic Health Survey (BDHS) conducted in 2014 and 2017–18. Independent variables influence the intermediate variables involved with adolescent childbearing in a society. The conceptual framework aids in understanding the role of modifiable and non-modifiable variables on adolescent childbearing (Figure 1).
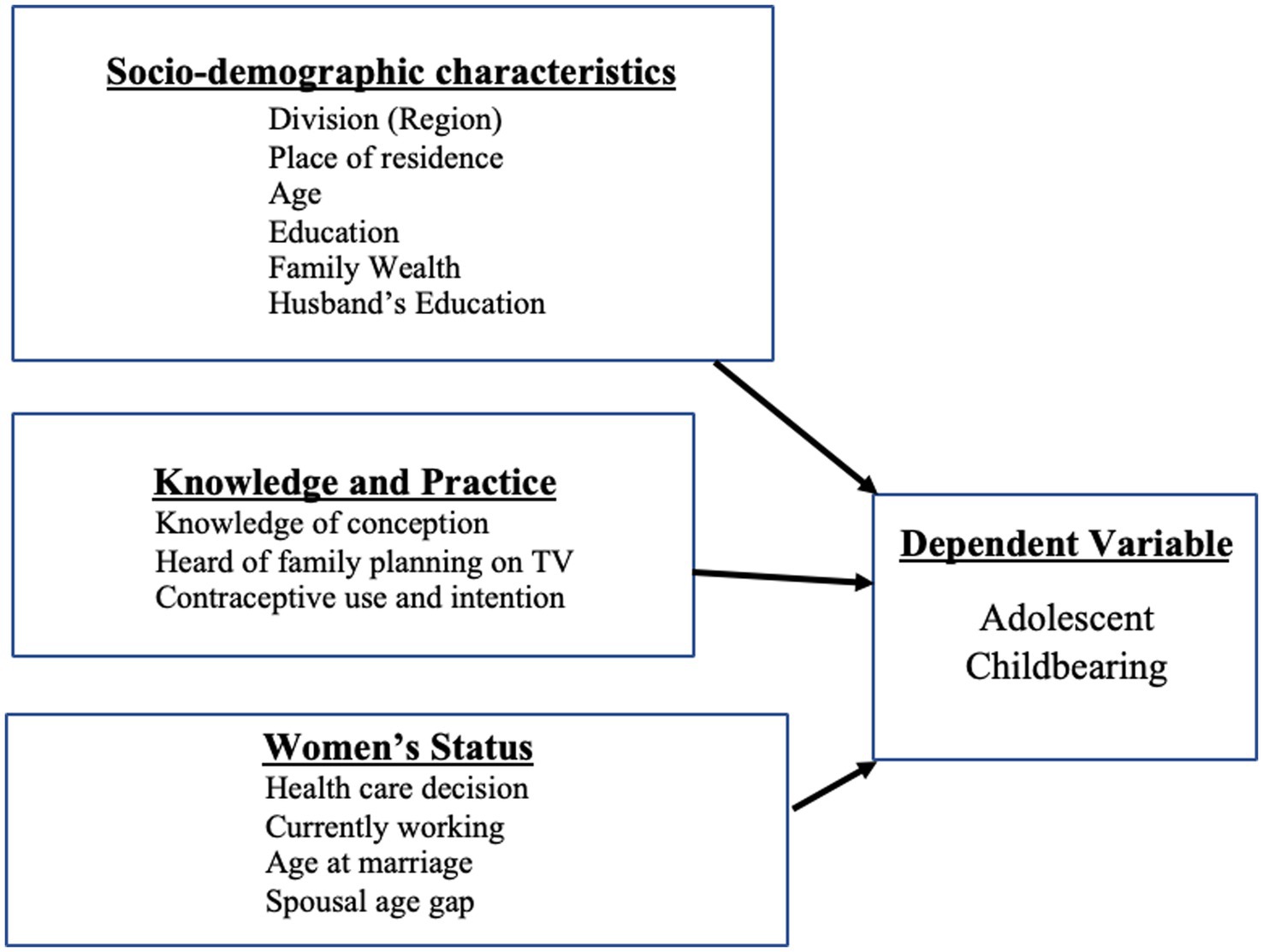
Figure 1. Conceptual framework depicting the linkages among the independent, intermediate, and dependent variables.
The study findings will provide evidence of change that has been observed in the prevalence and determinants of adolescent childbearing in Bangladesh between 2014 and 2018. This information will be useful to guide the intervention and policy reform needed to increase the age at first birth and reduce adolescent childbearing in Bangladesh.
Materials and methods
Data
This study uses data from the 2014 and 2017–18 Bangladesh Demographic Health Survey, which were the seventh and eighth DHS surveys conducted in Bangladesh. In general, DHS surveys provide information on childbearing, contraception and family planning methods, maternal and child health, and community-level data on the accessibility and availability of health services. All ever-married women age 15–49 in the selected households were eligible to be interviewed. The surveys were designed to produce representative results for the country, urban and rural areas, and for each of the eight administrative divisions. Details about the survey methodology are available in the DHS final report (29). The 2014 BDHS interviewed 17,863 women of age 15–49 and the 2017–18 BDHS survey recruited 20,127 women. Our study samples included 2,023 and 1,951 ever-married women of age 15–19 recruited respectably in 2014 and 2017–18 surveys. BDHS surveys were approved by ICF Institutional Review Board (IRB) and additionally by Bangladesh Medical Research Council (BMRC).
Variables
The dependent variable was adolescent childbearing, defined as women age 15–19 who were pregnant or had at least one child at the time of interview. Independent variables were: (a) sociodemographic characteristics of the woman and husband; (b) knowledge and practice; and (c) women’s status. Sociodemographic characteristics included division (region), place of residence (urban/rural), family wealth quintile, and woman’s and husband’s education level (no education, incomplete primary, complete primary, incomplete secondary, complete secondary, and higher). Knowledge and practice variables included knowledge of conception, heard about family planning on television in the past few months, and contraceptive use and intention (uses modern method, traditional method, non-user but intends to use, and does not intend to use). Knowledge of conception was recoded as correct knowledge if the respondent answered that the fertile period is in the middle of the women’s cycle and incorrect knowledge for any other answer. Variables that described the women’s status included health care decisions on women’s health care (woman alone, woman and her husband jointly, the husband alone, someone else, and other), working status (currently working or not), age at marriage, and spousal age gap. Age at Marriage was recoded as 10–13, 14–17, and 18–19 years; Knowledge of conception was recoded as no/wrong knowledge, and correct knowledge; spousal age gap was recoded as 2 years or less, 3–5 years, 6–10 years and more than 10 years.
Statistical analysis
Descriptive analysis was used to assess the sociodemographic characteristics of the study population for the ever-married sample in the surveys. The prevalence of adolescent childbearing was estimated for all ever-married women of age 19 or below by using all women factors. Univariate and multivariate logistic regression models were fit to determine the factors associated with adolescent childbearing. The dependent variable was adolescent childbearing, categorized as a binary variable defined as women age 15–19 who were pregnant or had at least one child at the time of interview. The multivariate logistic models were fit with adjustment of all the independent variables except for the husband’s education, which was found to be highly correlated with the women’s education. -values and 95% confidence intervals are reported to indicate the statistical significance of the odds ratios (OR). Statistical significance was set at p value <0.05.
The analysis considered the multi-stage sampling design of the survey and sampling weights. The “all-women factor” was used to adjust the sample weights in this ever-married women sample to make the estimates representative for all women for all analyses except Table 1, which describes the variables among ever-married women. All-women factors are used for adjustments of sampling weight for each woman, multiplying the weight variable for the woman by her appropriate all-women factor to inflate the number of cases from the number of ever-married women to the number of all women.
Results
Among ever-married women age 15–19 years, the majority lived in rural areas in 2014 (74%) and also in 2017 (76%). About half of the study subjects had incomplete secondary educations in 2014 (50%) and 2017 (55%), while 5% of the women had no formal education in 2014 reduced to 2% in 2017. Only 16% of the adolescent women were working at the time of interview in 2014 increased to 24% in 2017. Around three-quarters of the adolescent women (81% in 2014 and 75% in 2017) had no or incorrect knowledge of conception. Close to half of the respondents (46% in 2014 and 43% in 2017) reported using modern contraception methods to avoid pregnancy. Health care decisions were made jointly by 40% with husband in 2014 increased to 52% in 2017. Approximately 17% of adolescent women married at age 10–13 in 2014 and reduced to 13% in 2017, while most of them got married at age 14–17 found in both the surveys (Table 1).
In 2014 BDHS, prevalence of adolescent childbearing was found to be 30.8% among women; 29.6% in urban areas, and 31.2% in rural areas. Whereas, in 2017–18, the adolescent childbearing was found to be 27.6%; 27.7% in urban areas, and 27.5% in rural areas. Although it has decreased in 2017–18 compared to 2014, adolescent childbearing remained consistently higher in Rajshahi and Rangpur divisions (37% in 2014 and 33% in 2017–18) compared with other divisions (Table 2).
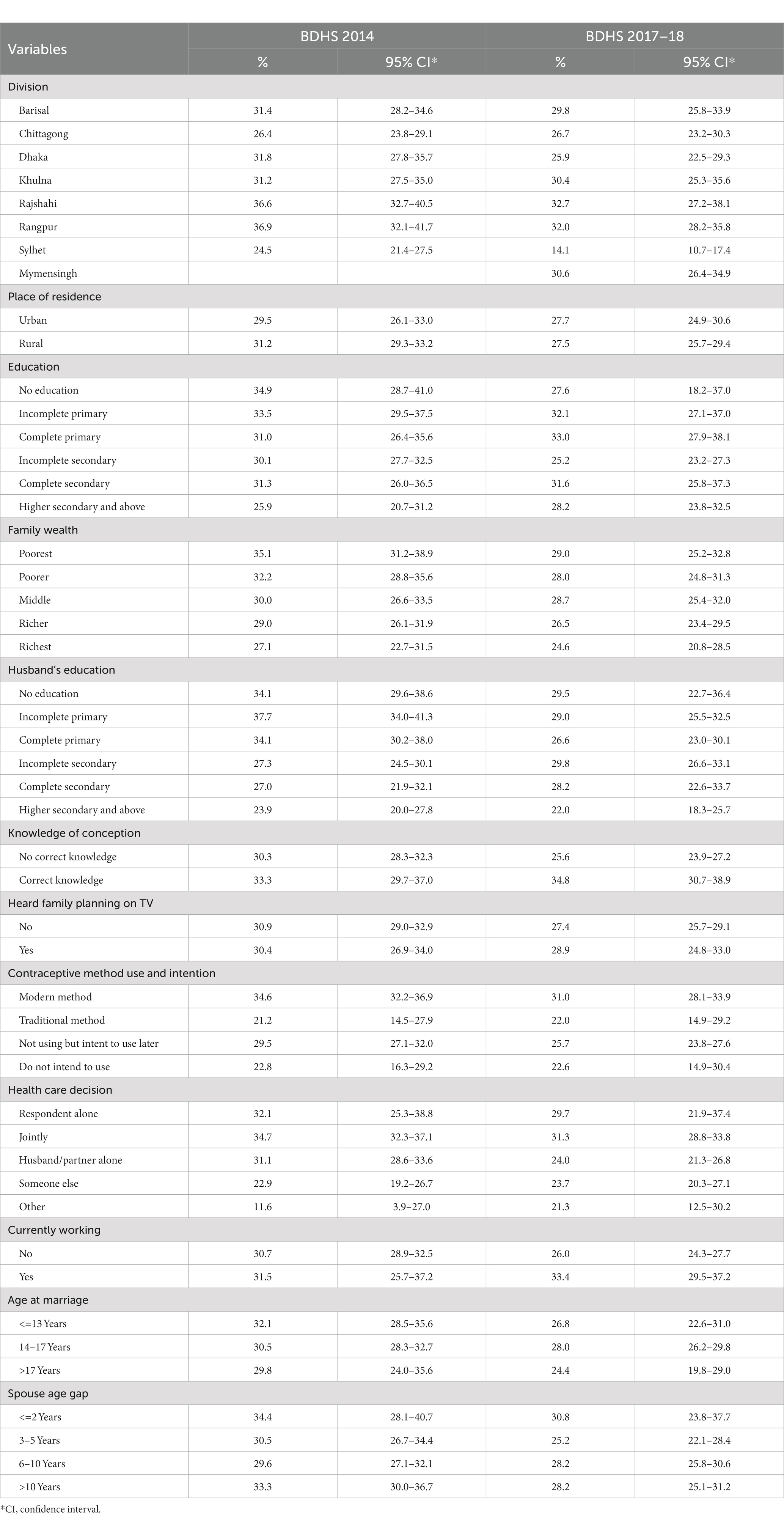
Table 2. Estimates of adolescent childbearing with 95% confidence interval from BDHS 2014 and BDHS 1017–18.
Adolescent childbearing decreased consistently with increasing family wealth as found in both survey years. In the 2014 survey, the adolescent childbearing ratio was found to be highest among women with no education (35%) but in 2017–18 it was found highest among women who completed primary education (33%). Similarly, the lowest adolescent childbearing was observed both in 2014 and 2017–18 surveys (26 and 28% respectively) among women whose husbands had higher secondary and above education. Interestingly, adolescent childbearing was found to be lowest among women who reported using traditional methods of contraception in both of the survey years (21 and 22%, respectively). The childbearing was found to be consistently lowest in both survey years when women got married at 18 years and later (30 and 24% respectively). Interestingly, working women had a higher childbearing reported both in 2014 and 2017–18 surveys (32 and 33% respectively) compared to women who did not work.
In the adjusted logistic models from data in the 2014 survey, the highest odds of adolescent childbearing were found in the Sylhet Division (AOR = 3.0; 95% CI: 1.6–6.1) and the Chittagong Division (AOR = 1.8; 95% CI: 1.8–2.7) when compared to the Barisal Division (Table 3). However, in 2017–18 BDHS geographic divisions were not found to be a significant determinant of adolescent childbearing, even though the Chittagong division had the highest adjusted odds (AOR = 1.5; 95% CI: 0.9–2.4). Compared to women in the lowest quintile, women in all other quintiles had significantly lower odds of adolescent childbearing, with the lowest odds found among women in highest quintiles (AOR = 0.3; 95% CI: 0.2–0.6) in 2014 BDHS and (AOR = 0.7; 95% CI: 0.4–1.3) in 2017–18 BDHS, respectively. Women who married at age 14–17 had 60% lower odds of adolescent childbearing and those who married at age 17–19 had 80% lower odds of adolescent childbearing compared to women who married at age 10–13 as found in both 2014 and 2017–18 BDHS. These findings were statistically significant. Women who used traditional contraceptives had 70% lower odds of adolescent childbearing as found in both of the surveys. Women who had 10 plus years of age gap with husband had 1.3 times higher odds having childbearing in 2014 BDHS and 1.5 times higher odds of childbearing in 2017–18 BDHS. However, these findings were not statistically significant.
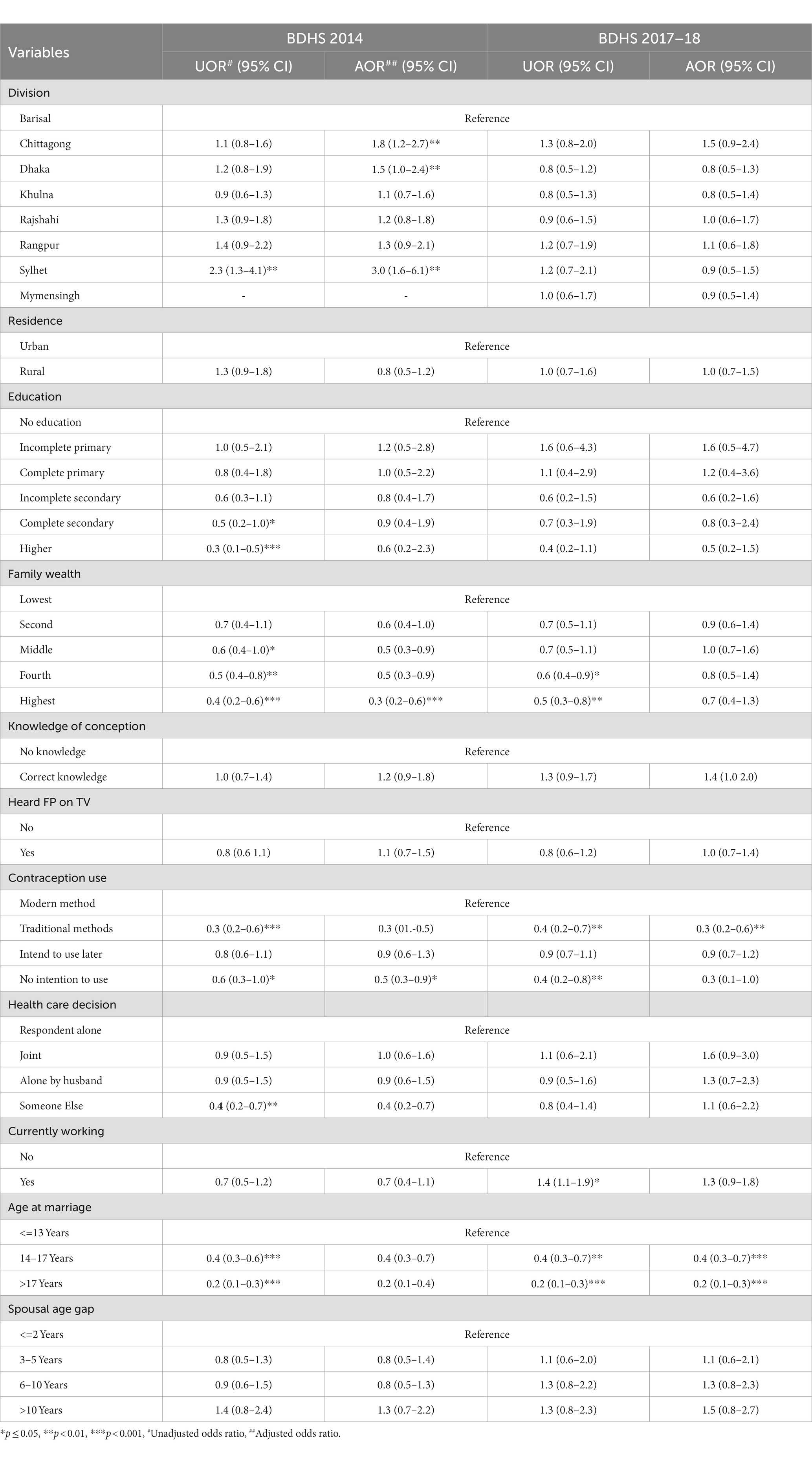
Table 3. Logistic regression of adolescent childbearing of ever-married women age 15–19 years, BDHS 2014 and BDHS 17–18 survey data.
Discussion
Based on the data of 2014 and 2017–18 BDHS, nearly one-third of married adolescents were either pregnant or already had at least one child before their twentieth birthday, which is substantially higher than in other South Asian countries (7, 9, 22). Considerable progress has been observed in the reduction of adolescent childbearing comparing data from BDHS 2014 and 2017–18, which shows further decline of adolescent childbearing from a study reported BDHS data from 1993 to 2014 (11). Bangladesh remains as one of the leading countries in the world with high rates of teenage childbearing. The high prevalence of adolescent childbearing could be a hindrance for women’s status in Bangladesh because of the negative consequences in health, as well as social and economic wellbeing. Four plausible explanations for high childbearing among adolescents include early age at marriage, early first birth, low contraceptive use among teenagers, and short birth interval (23).
Age at marriage was found to be a significant predictor of adolescent childbearing in this study. Adolescent women who married at age 14–19 had significantly lower odds of adolescent childbearing compared to the women who married at age 10–13. The proportion of adolescent women who got married at age < =13 years reduced substantially comparing data from BDHS 2014 and 2017–18, yet Bangladesh has some of the highest rates of child marriage worldwide, with more than half of all girls being married before the legal age of 18. Girls are often under pressure from both families to give birth to a child early in the marriage (12). Bangladesh enacted Child Marriage Restraint Act in 2017 against early marriage, however, progress has been steady slow over the years because it requires strong complementary social mobilization and other structural interventions that include poverty alleviation, gender equity, and an education program for girls (30). Adolescent women have a lower contraceptive prevalence rate than other women and a higher unmet need for family planning. The prevalence rates of modern contraceptive use rate among adolescent girls age 15–19 was 45.7% in 2014 and 42.6% in 2017–18, compared to 67.7% among women age 25–29 (24, 31). This is important to notice that there has been a little decline of modern methods use among adolescent women between 2014 and 2018.
This study findings suggest that adolescent girls who belong to the highest wealth quintile were significantly less likely to experience adolescent childbearing. Income inequality is a growing source of concern globally contributing negatively to health and developmental outcomes both within and across the countries. The disparity between rich and poor families has influenced overall adolescent health and adolescent childbearing (32). Women from richer households are more likely to have better control over the decision to use contraception and are more aware of the consequences of early childbearing on their own and their children’s health (14, 27). Household wealth could also reflect greater access to media as a tool for better knowledge and awareness including the decision to use contraceptives and reduce adolescent childbearing (13, 33, 34).
There were considerable variations in adolescent childbearing rates across geographic divisions in Bangladesh in 2014 BDHS. After adjusting for the effect of confounding variables, significantly higher odds of adolescent childbearing were found in the Sylhet and Chittagong divisions compared to Barisal Region. These two divisions were reported as low performing regions in Bangladesh for contraceptive use and other maternal and reproductive health indicators (35, 36). The significant variations in adolescent childbearing in these two divisions may be due to differences in religious, cultural, and program coverage (34, 37). However, in 2017–18 BDHS, observed inequality in adolescent childbearing by geographic divisions were not statistically significant. This finding overlays a reflection of an ongoing effort from the government and other stakeholders in reducing regional disparities in adolescent childbearing by introducing regional family planning programs that target the low performing areas in Bangladesh. Adolescents using traditional contraceptive methods have lower fertility than those using modern methods; while working women have higher fertility than those who did not work. These findings are apparently contrary to our understanding; however, sensitivity analyses revealed age of the adolescent was the determining factor in that adolescents who reported using traditional methods were younger in age and thus less likely to experience child bearing and access to modern methods. While currently working adolescents were mostly older and more likely to have a child or being pregnant.
This study has some limitations, both 2014 BDHS and 2017–18 data collected through cross-sectional surveys. So, the causality cannot be ascertained from the predictors as we have discussed in our study findings. However, the DHS data had a large sample size and nationally representative sampling methodology, which increase the generalizability of our study findings. Besides, some unmeasured characteristics including parental socioeconomic status and cultural influences on childbearing after marriage might have a systemic influence on adolescent childbearing in Bangladesh.
Conclusion
This study has offered a comparison of the magnitude and determinants of adolescent childbearing in Bangladesh in terms of economic, social, and reproductive factors taken data from two nationally representative surveys conducted 4 years apart. This study highlighted that the adolescent girls from the highest wealth quintile had lower odds of childbearing during their adolescent period. Age at marriage was found to be a significant determinant of adolescent childbearing. To address the issues of family wealth inequality, and child marriage, it is paramount to strengthen structural interventions that target individual and societal level change and raise awareness, poverty alleviation, girls education, and employment (38). Bangladesh is one of the few developing countries that has achieved most of the Millennium Development Goals that include reducing poverty, increasing female education, and reducing gender inequality (2, 18, 28). The study findings highlighted that Bangladesh is making progress in reducing adolescent childbearing among married adolescent women. The study findings could be useful in formulating policies and interventions that address modifiable factors to further reduce adolescent childbearing and achieve improved health and psychosocial wellbeing for women in Bangladesh.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: https://dhsprogram.com/.
Ethics statement
Bangladesh Demographic Health Surveys were reviewed and approved by Bangladesh Medical Research Council Ref: BMRC/NREC/2016-2019/324. Written informed consent to participate in this study was provided by the participants themselves or participants’ legal guardian/next to kin.
Author contributions
NA, MM, and SN conceptualized the study and interpreted the data and prepared the final manuscript. MM and NA analyzed the data. All authors contributed to the article and approved the submitted version.
Funding
No funding was needed for this study, which used secondary data from Bangladesh Demographic Health Survey (BDHS). The DHS Program (#AID-OAA-C-13-00095) was implemented with support from the United States Agency for International Development (USAID).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1088465/full#supplementary-material
References
1. Austrian, K, Soler-Hampejsek, E, Behrman, JR, Digitale, J, Jackson Hachonda, N, Bweupe, M, et al. The impact of the Adolescent Girls Empowerment Program (AGEP) on short and long term social, economic, education and outcomes: a cluster randomized controlled trial in Zambia. BMC Public Health. (2020) 20:1–15. doi: 10.1186/s12889-020-08468-0
2. Secretariat, U. The millennium development goals report 2015. New York, NY: United Nations (2015).
3. Wang, Y, and Qiao, J. Trends and social determinants of adolescent marriage and childbearing in China. Lancet Glob Health. (2020) 8:e873–4. doi: 10.1016/S2214-109X(20)30207-2
4. Darroch, JE, Woog, V, Bankole, A, Ashford, LS, and Points, K. Costs and benefits of meeting the contraceptive needs of adolescents. New York: Guttmacher Institute (2016).
5. Santelli, JS, Song, X, Garbers, S, Sharma, V, and Viner, RM. Global trends in adolescent fertility, 1990–2012, in relation to National Wealth, income inequalities, and educational expenditures. J Adolesc Health. (2017) 60:161–8. doi: 10.1016/j.jadohealth.2016.08.026
6. Alemayehu, T, Haidar, J, and Habte, D. Adolescents’ undernutrition and its determinants among in-school communities of Ambo town, West Oromia. Ethiopia East Afr J Public Health. (2010) 7:263–7. doi: 10.4314/eajph.v7i3.64738
7. Birchall, J. Early marriage, pregnancy and girl child school dropout. K4D Helpdesk Report. Brighton, UK: Institute of Development Studies (2018).
8. Chen, XK, Wen, SW, Fleming, N, Demissie, K, Rhoads, GG, and Walker, M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol. (2007) 36:368–73. doi: 10.1093/ije/dyl284
9. Ganchimeg, T, Ota, E, Morisaki, N, Laopaiboon, M, Lumbiganon, P, Zhang, J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG Int J Obstet Gynaecol. (2014) 121:40–8. doi: 10.1111/1471-0528.12630
10. Hossain, B, Gafur, T, Islam, M, and Hasan, S. Trends, patterns and determinants of marriage in Bangladesh, population monograph. Dhaka: Bangladesh Bureau of Statistics (2015).
11. Islam, MM, and Gagnon, AJ. Child marriage-related policies and reproductive health in Bangladesh: a cross-sectional analysis. Lancet. (2014) 384:S8. doi: 10.1016/S0140-6736(14)61871-7
12. Jaén-Sánchez, N, González-Azpeitia, G, Saavedra-Santana, P, Saavedra-Sanjuán, E, Manguiza, A-A, Manwere, N, et al. Adolescent motherhood in Mozambique. Consequences for pregnant women and newborns. PLoS One. (2020) 15:e0233985. doi: 10.1371/journal.pone.0233985
13. Angeles, G, Guilkey, DK, and Mroz, TA. The effects of education and family planning programs on in Indonesia. Econ Dev Cult Chang. (2005) 54:165–201. doi: 10.1086/431261
14. Barbieri, M, Hertrich, V, and Grieve, M. Age difference between spouses and contraceptive practice in sub-Saharan Africa. Population. (2005) 60:617–54. doi: 10.3917/pope.505.0617
15. MacQuarrie, K. Marriage and dynamics: The influence of marriage age on the timing of first birth and birth spacing. Rockville, Maryland, USA: ICF International (2016).
16. Cherry, AL, Byers, L, and Dillon, M. A global perspective on teen pregnancy. Maternal Child Health. (2009):375–97. doi: 10.1007/b106524_21
17. Fund UNCs. The State of the World’s Children. Executive summary. A Fair Chance for Every Child. New York: UNICEF (2016). 2016 p.
18. King, JC. The risk of maternal nutritional depletion and poor outcomes increases in early or closely spaced pregnancies. J Nutr. (2003) 133:1732S–6S. doi: 10.1093/jn/133.5.1732S
19. Masuda, K, and Yamauchi, C. How does female education reduce adolescent pregnancy and improve child health? Evidence from Uganda’s universal primary education for fully treated cohorts. J Dev Stud. (2020) 56:63–86. doi: 10.1080/00220388.2018.1546844
20. Ferdousi, N. Child marriage in Bangladesh: socio-legal analysis. Int J Sociol Anthropol. (2014) 6:1–7. doi: 10.5897/IJSA11.024
22. Nahar, Q, and Min, H. Trends and determinants of adolescent childbearing in. Bangladesh: Macro International Incorporated (2008).
23. Islam, MM, Islam, MK, Hasan, MS, and Hossain, MB. Adolescent motherhood in Bangladesh: trends and determinants. PLoS One. (2017) 12:e0188294. doi: 10.1371/journal.pone.0188294
25. Research NIOP, Training, Mitra, Associates, Macro International. Bangladesh Demographic and Health Survey 2007. Dhaka: NIPORT (2009). Available at: https://dhsprogram.com/publications/publication-fr207-dhs-final-reports.cfm.
26. Marchetta, F, and Sahn, DE. The role of education and family background in marriage, childbearing, and labor market participation in Senegal. Econ Dev Cult Chang. (2016) 64:369–403. doi: 10.1086/683982
27. Datta, SK, and Rabbany, H. Sustainable development goals and Bangladesh: the role of parliament. Int J Develop Res. (2016) 6:8599–606.
28. Demographic, B. Health Survey 2014. National Institute of Population Research and Training-NIPORT/Bangladesh, Mitra and Associates, and ICF International. Dhaka, Bangladesh: NIPORT, Mitra and Associates, and ICF International (2016).
29. Shukrana, U. Ramifications and solutions for existing child marriage law in Bangladesh. J Hum Rights Peace Stud. (2020) 6:89–106.
30. Hossain, MB, Khan, MHR, Ababneh, F, and Shaw, JEH. Identifying factors influencing contraceptive use in Bangladesh: evidence from BDHS 2014 data. BMC Public Health. (2018) 18:192. doi: 10.1186/s12889-018-5098-1
31. Viner, RM, Hargreaves, DS, Ward, J, Bonell, C, Mokdad, AH, and Patton, G. The health benefits of secondary education in adolescents and young adults: an international analysis in 186 low-, middle-and high-income countries from 1990 to 2013. SSM Populat Health. (2017) 3:162–71. doi: 10.1016/j.ssmph.2016.12.004
32. Islam, MM, and Hasan, AS. Mass media exposure and its impact on family planning in Bangladesh. J Biosoc Sci. (2000) 32:513–26. doi: 10.1017/S0021932000005137
33. Rabbi, AF. Mass media exposure and its impact on: current scenario of Bangladesh. J Sci Res. (2012) 4:383. doi: 10.3329/jsr.v4i2.8917
34. Hajizadeh, M, Alam, N, and Nandi, A. Social inequalities in the utilization of maternal care in Bangladesh: have they widened or narrowed in recent years? Int J Equity Health. (2014) 13:120. doi: 10.1186/s12939-014-0120-4
35. Islam, MK, Haque, MR, and Hema, PS. Regional variations of contraceptive use in Bangladesh: a disaggregate analysis by place of residence. PLoS One. (2020) 15:e0230143. doi: 10.1371/journal.pone.0230143
36. Mollborn, S. Predictors and consequences of adolescents’ norms against teenage pregnancy. Sociol Q. (2010) 51:303–28. doi: 10.1111/j.1533-8525.2010.01173.x
37. World Health Organization. Strengthening intersectoral collaboration for adolescent health. Geneva: World Health Organization (2016).
Keywords: adolescent childbearing, geographic inequality, determinants, Demographic Health Survey, Bangladesh
Citation: Alam N, Mollah MMH and Naomi SS (2023) Prevalence and determinants of adolescent childbearing: comparative analysis of 2017–18 and 2014 Bangladesh Demographic Health Survey. Front. Public Health. 11:1088465. doi: 10.3389/fpubh.2023.1088465
Edited by:
Zhiqiang Feng, University of Edinburgh, United KingdomReviewed by:
Isaac Fwemba, University of Ghana, GhanaAmbrose Akinlo, Obafemi Awolowo University, Nigeria
Copyright © 2023 Alam, Mollah and Naomi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nazmul Alam, bmF6bXVsLmFsYW1AYXV3LmVkdS5iZA==
 Nazmul Alam
Nazmul Alam Mohammad Manir Hossain Mollah1
Mohammad Manir Hossain Mollah1