- Department of Immunization and Prevention, Hangzhou Center for Disease Control and Prevention, Hangzhou, China
Objective: During the COVID-19 epidemic, vaccination staff had three main aspects of work: routine vaccination for children and adults, COVID-19 vaccination and COVID-19 prevention and control. All these works significantly increased the workload of vaccination staff. This study aimed to investigate the prevalence and influencing factors of burnout among vaccination staff in Hangzhou, China.
Methods: A total of 501 vaccination staff from 201 community/township healthcare centers in Hangzhou were recruited using a cross-sectional survey through WeChat social platform. The Maslach Burnout Inventory-General Scale (MBI-GS) was used to assess the level of burnout. Descriptive statistics were made on the characteristics of participants. Univariate analysis using the chi-square test and multivariable analysis using binary logistic regression were conducted to determine the relative predictors of burnout. Univariate analysis and multiple linear regression were used to determine the relative predictors of exhaustive emotion, cynicism, and personal accomplishment.
Results: During the COVID-19 pandemic, 20.8% of the vaccination staff experienced burnout. Educational level above undergraduate education level, medium professional title, and more working time in COVID-19 vaccination work reported a higher degree of job burnout. The vaccination staff was experiencing a high degree of exhaustive emotion, cynicism, and low personal accomplishment. Professional title, working place, and working time for COVID-19 vaccination were associated with exhaustive emotion and cynicism. Professional title and participation time for COVID-19 prevention and control were associated with personal accomplishment.
Conclusions: Our findings suggest that the prevalence rate of burnout is high among vaccination staff during the COVID-19 pandemic, especially with a low level of personal accomplishment. Psychological intervention for vaccination staff is urgently needed.
1. Introduction
An unprecedented outbreak of pneumonia of unknown etiology in Wuhan, Hubei Province, China, emerged in December 2019 (1, 2). It was named coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus type 2 (SARS-CoV-2) (3). On March 11, 2020, the World Health Organization (WHO) officially classified the global COVID-19 outbreak as a pandemic (4). Although countries worldwide have taken active and effective measures to control the epidemic, the current global epidemic is still severe (5). As of September 22, 2022, 610 million confirmed cases and 6.5 million deaths had been reported globally (6).
Since the outbreak, China, one of the countries with the most severe COVID-19 epidemic in the world, has implemented several strict but effective measures, such as lockdown cities, controlling traffic (7), mass isolation of individuals with cases (8), construction of Fangcang shelter hospitals (9), and public education campaigns encouraging the use of masks and hand washing (10). One of the most effective measures to prevent COVID-19 was COVID-19 vaccination. The COVID-19 vaccine is remarkably effective in preventing severe COVID-19 symptoms and death, and the COVID-19 booster vaccination can further improve the protective effect. Studies found that the risk of developing severe COVID-19 disease for those aged 18 to 59 who had received a booster COVID-19 vaccination was 94% lower than those who did not receive the vaccine. For people 60 and older, the figure is 95% (11). Since July 2020, China has officially launched emergency vaccination for high-risk exposed groups, including frontline medical workers, border and port staff, et al. In December 2020, the vaccination of key population groups, including cold chain logistics staff, medical staff, public transport workers, et al., was launched. Since then, China has gradually expanded the age range for COVID-19 vaccination from 18 years old and above to 3 years old and above. Currently, the inactivated COVID-19 vaccine in China is administered in three doses (12–14).
Vaccination staff at community/township health service centers are the leading force in COVID-19 vaccination in Hangzhou, China. Vaccination staff refers to all the personnel working in the vaccination clinic, including health prechecker, registration personnel, inoculator, logistics manager, etc. According to “Technical specifications for vaccination work” issued by the National Health Commission (15), each town (subdistrict) has a vaccination clinic set up in the community/township health service center. Before the COVID-19 epidemic, the vaccination staff was primarily responsible for childhood vaccination, including Expanded Program on Immunization (EPI) and Non-Expanded Program on Immunization (non-EPI) vaccination, as well as adult vaccination, such as flu vaccine, HPV vaccine, 23-valent pneumonia vaccine, and herpes zoster vaccine, et al. Their work included vaccination, cold chain management, adverse events following immunization (AEFI) reporting, report form filling, vaccine education, and other works. During the COVID-19 pandemic, the job of COVID-19 vaccination had fallen to them. Vaccine recipients are expanded from children and a few adults to the entire population over the age of three. In addition, vaccination staff, as primary care workers, also work on COVID-19 prevention and control, including nucleic acid sampling, elimination, hospital transmission, et al. (16). All these works significantly increased the working hours and workload of the vaccination staff.
According to previous studies, the epidemic of COVID-19 had placed a severe strain on healthcare workers (17–20) and significantly increased psychological problems of job burnout (20). As first described by Freudenberger (21), and subsequently developed by Maslach and Leiter (22) and Maslach et al. (23), chronic stress associated with emotionally intense work demands for which resources are inadequate can result in burnout. The three critical dimensions of this response are overwhelming exhaustion, feminism and detachment from the job, and a sense of ineffectiveness and lack of accomplishment (24). The exhaustion dimension is also described as wearing out, losing enerlosingletion, debilitation, and fatigue. The cynicism dimension was originally called depersonalization (given the nature of human services occupations), but is also described as negative or inappropriate attitudes toward clients, irritability, loss of idealism, and withdrawal. The inefficacy dimension was originally called reduced personal accomplishment and is also described as reduced productivity or capability, low morale, and an inability to cope (24). The first burnout measure based on a comprehensive program of psychometric research was the Maslach Burnout Inventory (MBI). It has been considered the standard tool for research in this field and has been translated and validated in many languages.
Prior studies showed that job burnout was high among medical staff during COVID-19. A survey has reported that 34.7% of physicians suffer from job burnout in Canada (25). In Huo et al. (11) study, about 34.5% of medical staff experienced burnout. For nurses, a study showed that about half of the nurses reported moderate and high work burnout in China (26). It is worth noting that job burnout could have many negative consequences. In terms of work, burnout is frequently associated with various forms of negative reactions and job withdrawal, including job dissatisfaction, low organizational commitment, absenteeism, turnover, lower productivity, and impaired quality of work (27–30). In addition, burnout can be “contagious” (31, 32). It could have a negative impact on colleagues, both by causing more significant personal conflict and by disrupting job tasks. In terms of personal health, burnout could contribute to poor health, which in turn contributes to burnout (33).
Vaccination staff plays an essential role in preventing and controlling the COVID-19 epidemic. They are responsible for routine and COVID-19 vaccination and, meanwhile, like other primary health care workers, for COVID-19 prevention and control. Currently, the COVID-19 pandemic continues to be a global threat, and SARS-CoV-2 is still developing (34). In the future, vaccination with a booster shot of the COVID-19 vaccine is still an important measure to prevent COVID-19 (35). Mass vaccination of the whole population will likely become routine work. Therefore, it is crucial to determine the influencing factors of job burnout of vaccination staff and reduce their job burnout.
There were many studies on job burnout in different medical specialties, such as nurses, doctors, physicians. No studies on burnout among vaccination staff have been found. This paper filled this gap in the literature by providing an in-depth exploration of the mental health of vaccination staff during the COVID-19 pandemic. This study attempted to gain a deeper understand of this reality and to contribute as much as possible to this important group of vaccination staffs in pandemic. The findings not only offered a scientific foundation for group intervention research involving vaccination staff, but also provided scientific basis for further strengthening the vaccination campaign during the COVID-19 pandemic, and could be a reference for job burnout of vaccination staff in other regions of China.
2. Materials and methods
2.1. Study design and participants
We conducted a cross-sectional survey to assess the job burnout of vaccination staff in Hangzhou, China, during the COVID-19 epidemic from June 10 to 17. Hangzhou, the capital city of Zhejiang Province, is a well-developed city in eastern China. Under the jurisdiction of the City of Hangzhou are 10 urban districts, one county-level city, two counties, and a total of 191 towns (subdistricts). By the end of 2021, Hangzhou's permanent residents population totals 12.204 million (36). Hangzhou had few cases of COVID-19 before 2022, and all were imported cases. Since the beginning of 2022, locally transmitted confirmed cases of COVID-19 emerged in Hangzhou, and several cluster infections occurred. Hangzhou doubled down on efforts to prevention and control the epidemics. According to the above reasons, the information collection in this survey starts in January 2022. To calculate the sample size for this survey, we referred to previous literature (19) and hypothesized that 30% of vaccination staff would have a level of burnout at a margin of error ± 6%, and we assumed a 95% confidence interval, a power of 80%. Using a sample size calculator and considering 14 factors to be entered in the multivariable analysis, the target sample size was 457. Then we added a 10% non-respondent rate, giving a final sample size of 500. To avoid face-to-face interaction, we edited the questionnaire on the Wen Juan Xing online platform, formed a link to the questionnaire, and sent it to each survey respondent via WeChat, one of mainland China's most essential and widely used social tools. The respondents answered the self-administered questionnaire by visiting the Uniform Resource Location (URL) on their phones. All 201 vaccination clinics in Hangzhou participated in the survey, and at least two vaccination staff were randomly selected from each clinic to participate in the survey. Finally, a total of 501 vaccination staff were recruited. All the participants were given consent to participate and assured de-identification and confidentiality in handling their data before they answered the questionnaires.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Hangzhou municipal center for disease control and prevention. The participants provided their written informed consent to participate in this study.
2.2. Assessments tools
2.2.1. Assessment of socio-demographic and work-related factors
A self-administered questionnaire was designed to collect socio-demographic information. The following socio-demographic factors were assessed: gender (male/female), age, marital status (currently married, currently not married), education level (less than undergraduate, undergraduate and above), family income (< 5,000 CYN, 5,000–9,999 CYN, 10,000–19,999 CYN, 20,000–29,999 CYN, ≧30,000 CYN), working years, professional title (junior, medium, senior), working place (urban, suburb, rural).
We divided the work of vaccination staff during the epidemic of COVID-19 into three main categories: routine vaccination work, COVID-19 vaccination work, and COVID-19 control, and prevention work. Variables of routine vaccination work included the daily number of vaccinations in each vaccination clinic (< 100 persons, 100–199 persons, 200–299 persons, ≧300 persons), weekly vaccination working days for each vaccination clinic (0.5 days, 1 day, 1.5–2 days, 2.5–3 days, ≧3 days). Variables of COVID-19 vaccination work included the doses of COVID-19 vaccination in each vaccination clinic in 2022 (0–9,999 doses, 10,000–19,999 doses, 20,000–39,999 doses, 40,000–59,999 doses, ≧60,000 doses), the extent to which COVID-19 vaccination work takes up time off work or rest days (not participating, during working time, a few of works take up time off work or rest days, most of work takes up time off work or rest days, all the work takes up time off work or rest days). Variables of COVID-19 prevention and control work included the extent to which COVID-19 prevention and control work takes up time off work or rest days (not participating, during working time, a few of works take up time off work or rest days, most of work takes up time off work or rest days, all the work takes up time off work or rest days), and duration of participation in COVID-19 prevention and control work (not participating, < 1 week, 1 week-1month, 1-2 months, ≧2 months).
2.2.2. Assessments for burnout
The Chinese version of the Maslach Burnout Inventory General Survey (MBI-GS) (37) was used to assess job burnout in this survey, which has been widely used among healthcare workers in China. MBI-GS consists of three dimensions of job burnout: Emotional Exhaustion (EE): (5 items), which means feelings of being emotionally overextended and depleted of one's emotional resources; Cynicism (CY) (4 items), which means a negative, callous, or excessively detached response to other people; Personal Accomplishment (PA): (6 items), which means a decline in one's feelings of competence and achievement in one's work. Each item consists of a 7-point Likert scale: 0 = never, 1 = barely, 2 = occasionally, 3 = often, 4 = frequently, 5 = very frequently, and 6 = every day, ranging from 0 (“never”) to 6 (“every day”). Higher scores on the dimensions of EE and CY indicate burnout, and so as the lower scores on the dimension of PA. The MBI-GS has shown good reliability and validity in previous studies in China (38, 39). In this study, the result of reliability analysis showed that the scale was in a high level of internal consistency in all three dimensions in the current sample. The Cronbach's alpha for all 15 items was 0.900, and for EE, CY and PA was 0.963, 0.942, and 0.936, respectively.
Based on several previous studies in China (19, 40), subscales scores are considered as low, moderate, or high level of burnout syndrome according to these cut-points: low EE < 9, moderate EE 9–13, high EE>13; low CY < 3, moderate CY 3–9, high CY>9; low PA < 18, moderate PA 30–18, high PA>30. High EE and high CY or low PA are conditions for burnout (“exhaustion+1”), which is considered to be the most effective categorization to distinguish between individuals with high and low burnout (41).
2.3. Statistical analysis
Frequencies and percentages were summarized for the categorical variables. Mean and standard deviation (SD) were calculated for continuous numerical data. Comparisons of sociodemographic and work-related variables of participants between the burnout group and the non-burnout group were analyzed by chi-square test. A multivariable analysis using binary logistic regression was conducted to determine the relative predictors of burnout when controlled for potential confounding among the various predictor variables. Correlates with a P < 0.1 in the univariate analysis were included in the multivariable analysis using the “Forward: LR” method. Then, to further identify the independent factors associated with MBI-GS scores, variables with P < 0.1 in the univariate analysis were entered into the multiple linear regression, with the MBI-GS subscores as dependent variables. All statistical analyses were conducted using SPSS (version 24.0).
3. Results
3.1. Demographic characteristics and work-related situations of participants
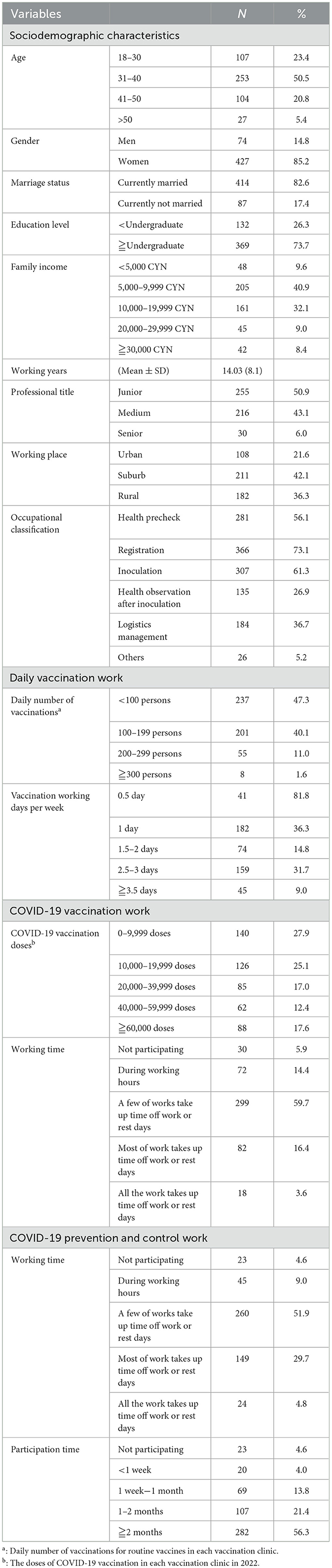
In total, 501 individuals were included in the analysis. Among all the participants, 85.2% were female, and 14.8% were male. Almost half of the participants were in the age range of 31–40 (50.5%). 50.9% had a junior professional title. The majority of participants were married (82.6%), undergraduate and above (73.7%), and had household incomes between 5,000–9,999 CNY (40.9%) and 10,000–19,999 CNY (32.1%). The average working years was 14.03 ± 8.1 years. 36.3% of the participants worked in urban areas, 42.1% in suburbs, and 36.3% in rural areas. Most participants held two or more jobs at the same time. Majority of participants were responsible for registration (73.1%), followed by inoculation (61.3%) and health pre-check (56.1%). Other jobs (5.2%) included report filling, administration, etc.
Regarding routine vaccination work, 47.3% of the participants worked in vaccination clinics with a daily number of vaccinations < 100 people. 36.3 and 31.7% of participants worked in the vaccination clinic with 1 day per week and 2.5–3 days per week vaccination working time, respectively.
In terms of COVID-19 vaccination work, 27.9% of the participants worked in vaccination clinics that had administered 0–9,999 doses of COVID-19 vaccine, and the proportion administering 10,000–19,999 doses, 20,000–39,999 doses, 40,000–59,999 doses, and ≧60,000 doses were 25.1, 17.0, 12.4, and 17.6%, respectively. For COVID-19 vaccination working time, more than half of the participants (59.7%) reported that few works took up time off work or rest days.
In terms of COVID-19 prevention and control work, more than half of participants (51.9%) indicated that few works took up time off work or rest days. 56.3% of participants had been involved in this work for over 2 months.
More detailed information about participants' demographic and job-related characteristics is shown in Table 1.
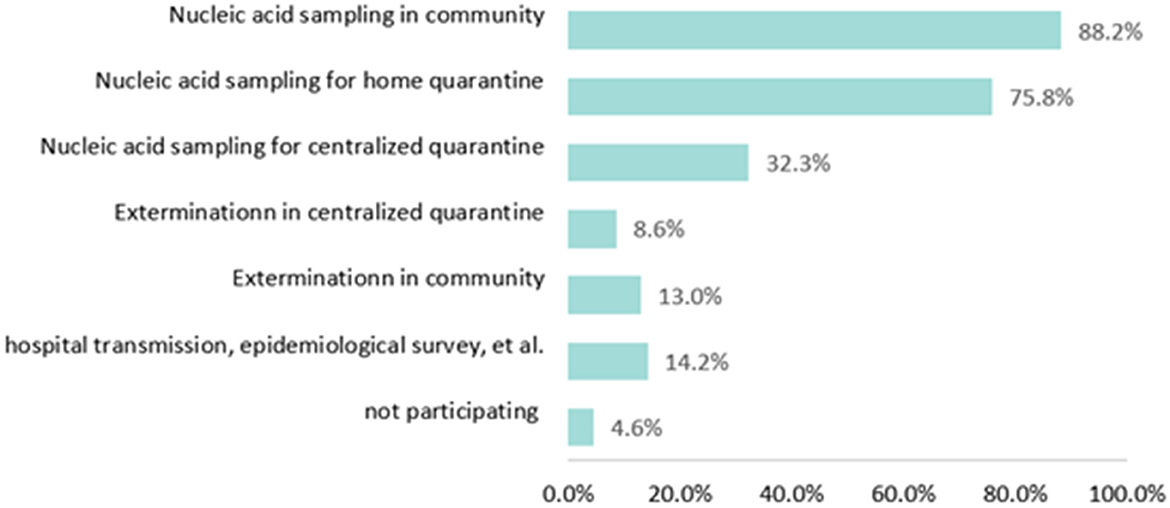
As shown in Figure 1, the majority of the vaccination staff participated in nucleic acid sampling work in the community (88.2%) and nucleic acid sampling work for home quarantine (75.7%). About one-third of vaccination staff (32.3%) participated in nucleic acid sampling for centralized quarantine. 14.2% of vaccination staff participated in other prevention and control work for COVID-19, including nucleic acid sampling at highway chokepoints, epidemiological investigation of close contacts, hospital transmission, et al. (Figure 1).
3.2. Prevalence of burnout in vaccination staff
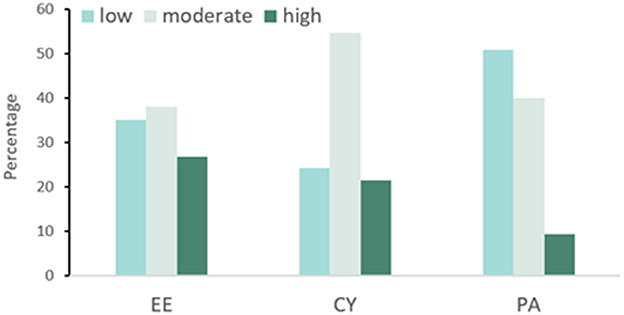
The prevalence of burnout in vaccination staff was 20.8% (104/501). For EE, 26.7% (134/501), 38.1% (191/501), and 35.1% (176/501) vaccination staff were at a high, moderate, and low level, respectively. For CY, high, moderate, and low levels accounted for 21.4% (107/501), 54.5% (273/501), and 24.2% (121/501), respectively. For PA, almost half of the vaccination staff were at a low level (50.7%, 254/501), 39.9% (200/501), and 9.4% (47/501) were at a moderate and a high level (Figure 2).
3.3. Factors associated with burnout
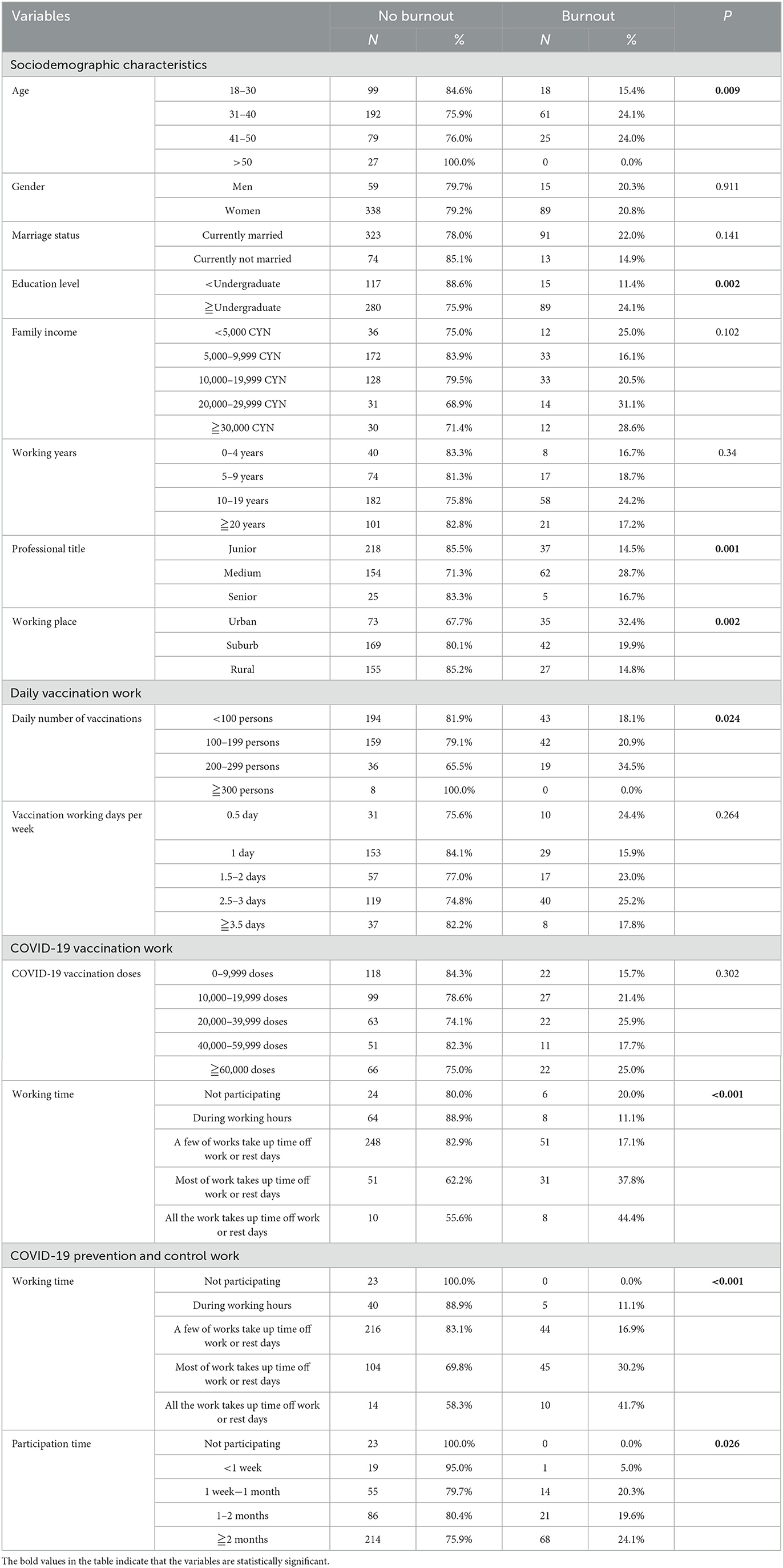
Chi-squared tests revealed that there were significant differences between burnout and non-burnout groups in terms of age, education level, professional title, working place, the daily number of vaccinations, COVID-19 vaccination doses, working time of COVID-19 vaccination, working time and participation time of COVID-19 prevention and control (all P < 0.1). The burnout rates of each type of variable are shown in Table 2.
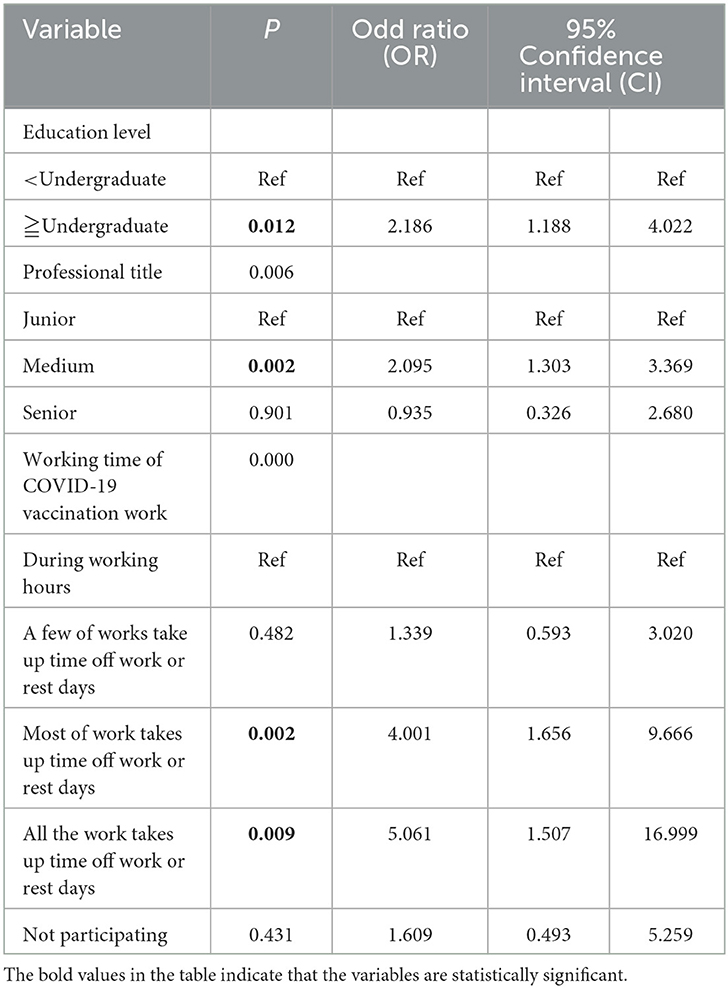
Further, the binary logistic regression model revealed that the possibility of having burnout symptoms was significantly higher in participants who had high education level (OR = 2.186, 95% CI:1.188–4.022, p = 0.012), medium professional title (OR = 2.095, 95% CI:1.303–3.369, p = 0.002), most (OR = 4.001, 95% CI:1.656–9.666, p = 0.002) and all (OR = 5.061, 95% CI:1.507–16.999, p = 0.009) of COVID-19 vaccination work takes up time off work or rest days (Table 3).
3.4. Factors associated with MBI-GS three components in vaccination staff
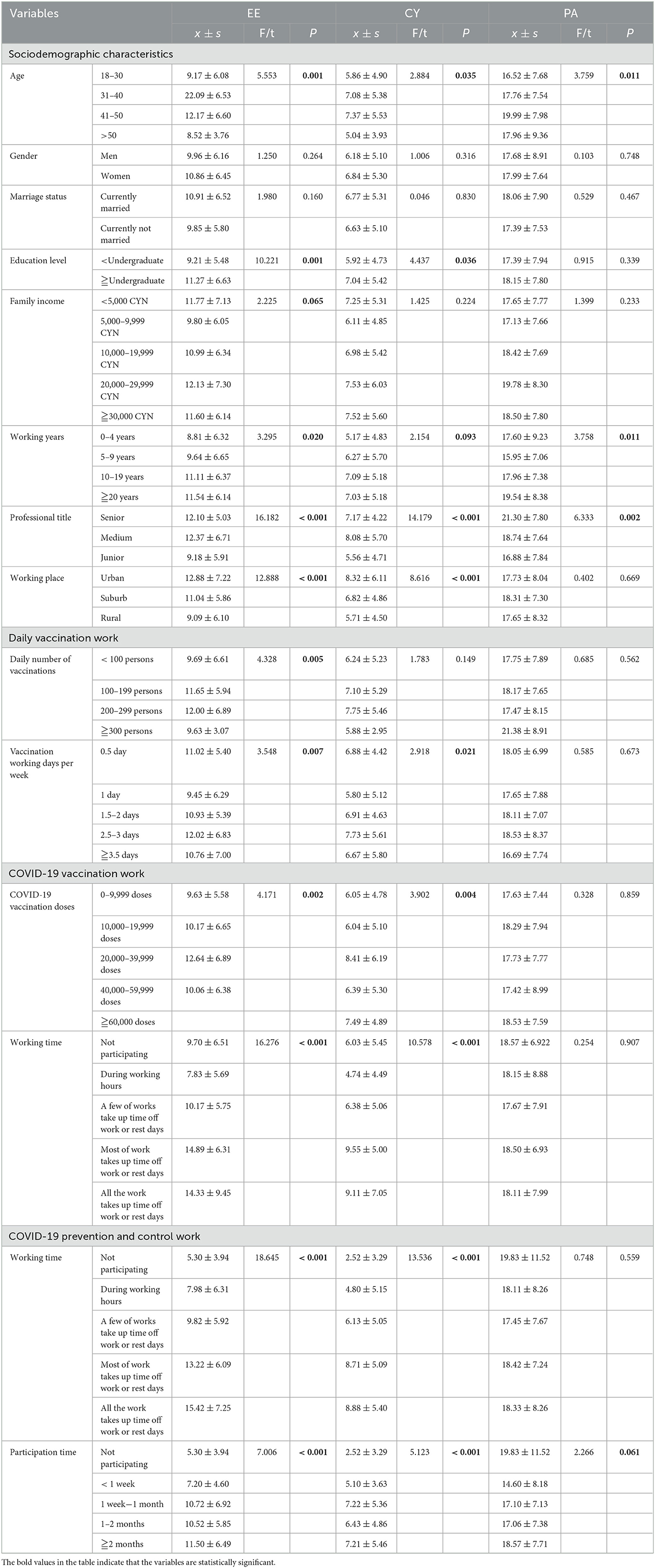
The average burnout score was 10.73 ± 6.41 on the EE subscale, 6.74 ± 5.27 on the CY subscale, and 17.95 ± 7.83 on the PA subscale. MBI-GS subscale scores after grouping according to demographics and work-related variables were present in Table 4. Univariable analysis showed that all variables for COVID-19 vaccination work and COVID-19 prevention and control work were statistically associated with EE and CY. Based on this, variables associated with CY added age, education level, working years, professional title, working place, and vaccination working days per week. Compared with CY, EE added the statistically significant variables of family income and the daily number of vaccinations. Regarding PA, only age, working years, professional title, and participation time for COVID-19 prevention and control were statistically significant (P < 0.1) (Table 4).
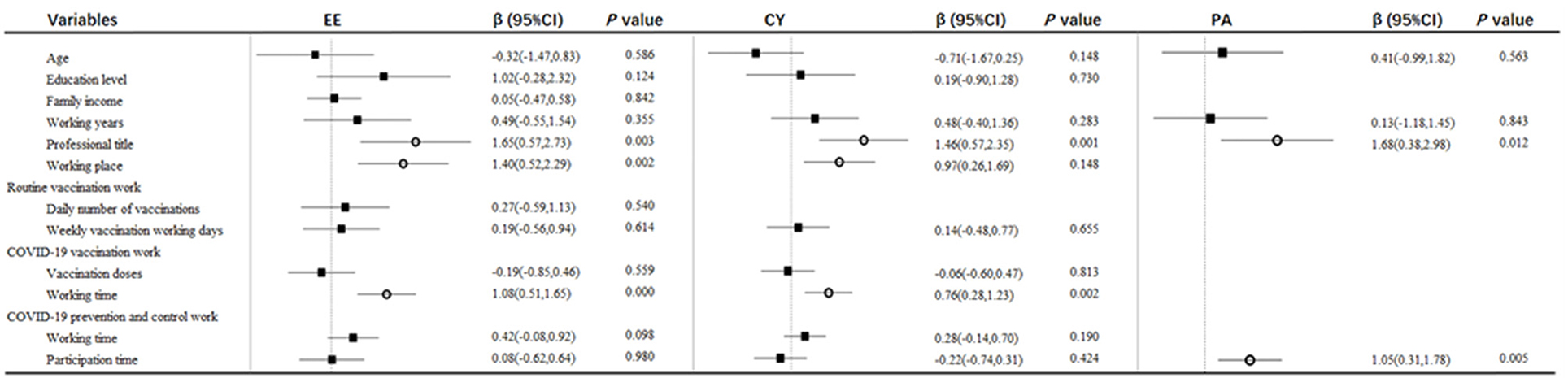
Then multiple linear regressions were performed to identify independent related factors to each MBI-GS subscale. EE was independently correlated with professional title (β = 1.647, t = 2.998, p = 0.003), working place (β = 1.403, t = 3.108, p = 0.002), working time for COVID-19 vaccination (β = 1.079, t = 3.717, p < 0.001). CY was independently correlated with professional title (β = 1.460, t = 3.216, p = 0.001), working place (β = 0.971, t = 2.671, p = 0.008), working time for COVID-19 vaccination (β = 0.755, t = 3.119, p = 0.002). PA was independently correlated with professional title (β = 1.677, t = 2.534, p = 0.012) and participation time for COVID-19 prevention and control work (β = 1.047, t = 2.804, p = 0.005) (Figure 3).
4. Discussion
During the COVID-19 pandemic, the work of COVID-19 vaccination and epidemic control has greatly increased the workload of vaccination staff, therefor it is necessary to investigate the burnout situation of vaccination staff. The main findings of this study were: (1) The overall prevalence of burnout syndrome among vaccination staff was 20.8% in Hangzhou, China. (2) The predictors associated with job burnout were educational level, professional title, and COVID-19 vaccination working time. (3) The vaccination staff was experiencing a high degree of exhaustive emotion, cynicism, and especially low personal accomplishment.
As far as we know, there has not been much consensus on the “diagnosing” of burnout. First, different criteria were used to distinguish the high and low levels of the three dimensions. For example, studies used 9 and 13 as the cutoff to distinguish the different levels of EE (19). However, other studies used 11 and 15 (42, 43) or 11 and 14 (44). Second, the criteria for determining burnout are inconsistent. Studies used the three components' weighted score as criteria (44–46), and other studies used any of the components to classify the level of burnout (43, 47). In this study, referring to Huo et al. (19) and Li et al.'s (48) studies, we used the “exhaustion+1” criterion to define burnout symptoms and distinguish different levels of burnout. Brenninkmeijer et al. indicated that a categorization in which both high exhaustion and high distance or low competence were conditions for burnout (“exhaustion+1”), resulted in a relatively small chance of an inaccurate qualification of burnout and seemed to be an effective categorization for mapping differences in burnout (42).
The results of this study showed that vaccination staff had a high level of burnout (20.8%), and the prevalence of EE, CY, and PA at high in this study was 26.7, 21.4, and 50.7%, respectively. Compared to previous studies using the same criterion, the level of burnout in vaccination staff was lower than that in medical staff (36.5%) (19). The high level of EE and CY in vaccination staff was also lower than that in medical staff (EE: 40.9%, CY: 63.7%) and frontline health professionals (EE: 34.2%, CY: 50.8%), respectively (19, 48). Based on this, it could be assumed that the situation of job burnout, EE and CY for vaccination staff was better than that for other medical staff during the COVID-19 epidemic in China. Exhaustion emotion is the central quality of burnout and is associated with workload, including working hours (49, 50), work shifts (51), and work pressure (52). Compared with vaccination staff, other medical workers, especially the frontline health professionals (48), had a heavy workload to save and care for COVID-19 patients, and they were under tremendous pressure, such as the high risk of contracting the virus and bringing to their families (52). All of this could cause them to have higher levels of EE. Cynicism emerged from the presence of work overload and social conflict. It prompted medical staff to take action to distance themselves emotionally and cognitively from their work. Previous studies have indicated that deteriorating doctor-patient relationships could lead to a high level of CY in medical staff (53, 54). In China, the doctor-patient relationship has always been a big problem (55, 56). According to previous studies, difficulty in seeing a doctor, poor communication, high medical expenses, and high expectations for doctors were all the influencing factors for bad doctor-patient relationships (18). These conditions were more common in medical staff in hospitals than in vaccination clinics. Therefore, we hypothesized that these factors lead to higher levels of EE and CY in medical workers than in vaccination staff. However, on the contrary, regarding the low level of PA, the situation is much worse in the vaccination staff than in other medical staff. From Guo and Li's study, the level of PA at low in medical staff was 35.2 and 46%, respectively (19, 48), which was lower than that in vaccination staff (50.7%) in this study. The component of PA represents the self-evaluation dimension of burnout and refers to feelings of incompetence and a lack of achievement and productivity in work (57). First, vaccination staff is public health providers working in primary care institutions. In China, the social status of primary medical institutions is generally lower than that of hospitals. People are more willing to bypass primary medical institutions to seek care at hospitals (58). Similarly, public health providers have a lower social status than clinicians. People trust clinicians more than public health providers. All these factors contributed to the low PA of vaccination staff (59). Second, for the work of vaccination staff, on the one hand, the main work was to vaccinate the population. Their sense of job accomplishment was not as apparent as doctors treating patients and saving lives. On the other hand, vaccine hesitancy is widespread in the population (60–62). Vaccination staff who regularly interact with vaccine-hesitant people was prone to question their competence and had a higher level of burnout and lower level of job satisfaction (63), which could lead them to doubt the value of their work. In addition, during the COVID-19 period, like clinicians, vaccination staff made an outstanding contribution to the fight against the COVID-19 epidemic. However, compared with clinicians and other medical workers, vaccination staff had low income, low returns, low social status, and low social support (64). All these reasons contributed to the low level of PA in vaccination staff (26). In the future, more studies are needed to study the interventions to reduce the PA in vaccination staff.
In this study, the score of the three components of EE, CY, and PA were 10.73 ± 6.41, 6.74 ± 5.27, and 17.95 ± 7.83, respectively. According to previous studies, during the COVID-19 epidemic in China, vaccination staff had lower scores of EE and CY but higher scores of PA than other health professionals (19, 48, 65, 66). The results were consistent with the distribution of high levels of EE, CY, and low levels of PA in vaccination staff and medical staff discussed above. However, it was worth mentioning that although the EE and CY scores of vaccination staff were lower than those of medical workers, it did not mean that the EE and CY levels of vaccination staff were not high. To Lu's study, the scores of EE and CY in biosafety laboratory staff were 10.00 ± 5.99 and 4.64 ± 4.59, which were lower than that in vaccination staff during the COVID-19 epidemic (52). With the arrival of COVID-19, the workload of vaccination staff has dramatically increased. In addition to routine work of vaccinations for children and some adults, they also needed to vaccinate people over the age of three. This study found that nearly 80% of participants reported that the COVID-19 vaccination work took up time off work and rest days. Furthermore, the vaccination staff was involved in the COVID-19 prevention and control work. They need to concrete implementation of COVID-19 prevention and control. Figure 1 shows that 88.2% of participants worked for nucleic acid sampling in the community, 75.8% worked for nucleic acid sampling for home quarantine, and 86.4% of participants in this study reported that the COVID-19 prevention and control work took up time off work and rest days. As a result, the workload and working hours for vaccination staff had increased significantly, which caused the high level of EE. After that, vaccination staff became indifferent and repulsive to their service objects and to their own profession, thus causing a high level of CY (23). On the other hand, as we know, there may be an tiny chance of adverse events following vaccination. The amount of COVID-19 vaccine inoculated is enormous. Therefore, the number of people with adverse events becomes obvious in public view. Some people attributed the adverse events to vaccination staff and even attached violence to them. This would worsen the working environment of vaccination staff and cause high CY. To better understand the level of EE, CY, and PA among vaccination staff and to compare them with other health care workers, further work is required to establish a norm for medical workers and to monitor the job burnout level of vaccination staff in a long-term manner.
Among the related factors of job burnout, we found that vaccination staff with higher education level had more job burnout than those with lower education level. This was consistent with previous findings studied in medical staff (67–69). A possible explanation for this might be that highly educated vaccination staff usually had more responsibility and expectations (67). They would have a more important role played in work, which pushed them to suffer from a greater risk of job burnout (52).
Another finding was that vaccination staff with the medium professional title had a higher level of burnout, EE, and CY. Previous studies also reported this finding in primary healthcare workers and nurses in China (45, 70). There were several possible explanations for this result. First, according to China's medical system and the professional title system of health professionals (71), vaccination staff with medium titles were always in middle age and the central workforce in vaccination clinics, during which the heavy workload might result in a high level of EE (72). Second, vaccination staff with medium professional titles were in the promotion period of careers. However, in China, the work resource for health care workers is very scarce (45, 64). Only a tiny percentage of vaccination staff with medium professional titles could upgrade to senior professional titles (73), which inevitably leading to competition among colleagues. The lack of critical resources and the poor quality of colleague relationships would reduce job satisfaction and increase CY in vaccination staff (24). In terms of PA, a possible explanation might be that with the rise of professional title, the workability and work sense of accomplishment of vaccination staff were also gradually increased, and they were more able to appreciate their personal and work value.
The result of this study showed that working place was associated with EE and CY. The EE and CY scores of vaccination staff were highest in urban areas and lowest in rural areas. Related conclusions from previous studies were mixed. A general practitioner study showed no difference in EE, CY, and PA between urban and rural areas (74). Another study showed that compared with rural areas, public health service providers in urban areas had higher EE and CY but no statistical difference in PA (59). Within the context of our study setting, there were several possible explanations for the finding in this study. First, in Hangzhou, vaccination-related work has been done better in urban areas than in suburban or rural areas. Vaccination staff in urban areas have higher requirements for their work, such as a higher vaccination rate, better service attitude, and a more convenient service experience. These might lead to an increase in workload, and increase their working pressure. Previous literature had reported an association between working pressure and burnout (20). Secondly, the massive influx of migrants in urban areas has brought considerable challenges to the COVID-19 prevention and control efforts, making COVID-19 epidemic prevention and control more difficult (75). Thirdly, compared with urban areas, rural or suburban areas had relatively better health care environments and better doctor-patient relationships (76). All these factors might cause result in high EE and CY in the urban area.
Regarding the job-related factors, we found that vaccination staff who reported that the work of COVID-19 vaccination took up more time off work or rest days was more likely to be burnout and have a high level of EE and CY. The more work that takes up time off work or rest days, the longer work hours will be. Moreover, the relationship between prolonged working hours and burnout, EE, and CY has been well demonstrated (49, 54, 67, 77). Considering that COVID-19 vaccination is currently a positive and effective way to prevent COVID-19 (78), and booster shots of COVID-19 vaccine might be needed in the future (35), it is essential to improve the efficiency of COVID-19 vaccination and arrange working hours reasonably to reduce the job burnout among vaccination staff.
The current study found that the longer time vaccination staff participated in COVID-19 prevention and control, the more personal accomplishment they felt. Since 2022, there have been multiple COVID-19 outbreaks in Hangzhou. The vaccination staff was involved in the COVID-19 prevention and control work, including nucleic acid sampling, extermination, and hospital transmission, et al. (Table 1). Through the joint efforts of vaccination staff and the whole society, the epidemic in Hangzhou has been controlled at a stable level (79), which might give vaccination staff a great sense of accomplishment and work value. Furthermore, vaccination staff who participated in COVID-19 prevention and control work might get more honors, more bonuses, and higher social support from superior and organization, which could improve their PA.
This study has strengths and limitations. To our knowledge, this is the first study to investigate burnout among vaccination staff in China. The three main aspects of work for vaccination staff during COVID-19, including routine vaccination work, the COVID-19 vaccination work, and the COVID-19 prevention and control work, were all considered in this study. However, this study has some limitations. First, there is no consensus on the diagnosis of job burnout. We only selected one of the diagnosis methods, so it was difficult to directly compare the prevalence of job burnout with other studies. Second, the indicators of workload in this paper were not very precise. We could not determine the amount of vaccination for each vaccination staff, so the vaccination dose for each vaccination staff's clinic was used. In addition, regarding working hours, we used the subjective judgment method of vaccination staff' self-assessment, which may be biased compared to the specific assessment time. It was better to use concrete numbers, i.e., 40 h per week, to measure burnout. Third, because this survey was conducted by online questionnaire, compared with a face-to-face questionnaire survey, it was inevitable that there would be some problems with survey quality, such as unclear questionnaire questions and filling errors.
5. Conclusion
The present study found that vaccination staff in Hangzhou, China, had high levels of job burnout, EE and CY, and these conditions were better than than other medical staff The level of PA among vaccination staff was much worse than other medical staff. The factors influencing burnout included level of education, professional title, and working time for COVID-19 vaccination work. The professional title, working place, and the working time for COVID-19 vaccination were associated with the degree of EE and CY. For PA, the associated factors were professional title and participation time for COVID-19 prevention and control. Interventions should be taken to reduce the level of job burnout and alleviate psychological pressure in vaccination staff, especially to enhance their personal achievement. Further research should conduct to reach consensus on the “diagnosing” of burnout, and the research on the norm of burnout among medical staff is warranted.
Data availability statement
The datasets presented in this article are not readily available because the data that support the findings of this study are available from the corresponding author upon reasonable request. Requests to access the datasets should be directed to YL, c21pbGVmb3JldmVyODFAMTI2LmNvbQ==.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Hangzhou Center for Disease Control and Prevention. The patients/participants provided their written informed consent to participate in this study.
Author contributions
WG and YL planned and designed the study. ZL, YX, XuZ, and JC were responsible for data management. JuW, XC, and JiW for data analysis. WG drafted the manuscript. JD and XiZ for supervision. All authors contributed to interpretation of study results, critical revision of the paper and approval of final version, and agree to be accountable for all aspects of this article.
Funding
This research was funded by Medical Science and Technology Project of Zhejiang Province (Grant No. 2020KY780) and Hangzhou Medical and Health Science and Technology Project (Grant No. A20210434).
Acknowledgments
Thanks to all the vaccination staff who participated in this study, and all the colleagues who have given me generous support and helpful advice during the period of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
2. Chen L, Liu W, Zhang Q, Xu K, Ye G, Wu W, et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect. (2020) 9:313–9. doi: 10.1080/22221751.2020.1725399
3. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. (2020) 5:536–44. doi: 10.1038/s41564-020-0695-z
4. The World Health Organization. Coronavirus Disease 2019 (COVID-19). Situation Report – 51. 2020. Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=ba62e57_10 (accessed September 21, 2020).
5. The World Health Organization. Weekly Epidemiological Update on COVID-19 - 14 September 2022. 109 ed. Geneva, Switzerland (2022).
6. The World Health Organization. WHO Coronavirus (COVID-19) Dashboard. (2022). Available online at: https://covid19.who.int/ (accessed September 22, 2022).
7. Bangura MS, Gonzalez MJ, Ali NM, Ren R, Qiao Y. A collaborative effort of China in combating COVID-19. Glob Health Res Policy. (2020) 5:47. doi: 10.1186/s41256-020-00174-z
8. Cheng S, Zhao Y, Kaminga AC, Zhang X, Xu H. China's fight against COVID-19: what we have done and what we should do next? Front Public Health. (2022) 10:548056. doi: 10.3389/fpubh.2022.548056
9. Chen S, Zhang Z, Yang J, Wang J, Zhai X, Bärnighausen T, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. (2020) 395:1305–14. doi: 10.1016/S0140-6736(20)30744-3
10. Lau H, Khosrawipour V, Kocbach P, Mikolajczyk A, Schubert J, Bania J, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. (2020) 26:taaa037. doi: 10.1093/jtm/taaa037
11. Joint Prevention Control Mechanism of the State Council. What is the Actual Effect of COVID-19 Vaccine in China? Can the Elderly with Chronic Diseases be Vaccinated? The Latest Response! Available online at: http://www.gov.cn/fuwu/2022-07/23/content_5702510.htm (accessed February 2, 2022).
12. Joint Prevention Control Mechanism of the State Council. Who Can Get Vaccinated? Where Should I Get Vaccinated? 11 Definitive Questions and Answers About the COVID-19 Vaccine! Available online at: http://www.gov.cn/fuwu/2020-12/19/content_5571152.htm (accessed September 26, 2020).
13. Joint Prevention Control Mechanism of the State Council. Ministry of Education: Vaccinate Students Aged 12 to 17 in a Safe and Secure Manner. (2021). Available online at: http://www.gov.cn/xinwen/2021-08/05/content_5629673.htm (accessed September 26, 2021).
14. Joint Prevention Control Mechanism of the State Council. The Current Epidemic is Still Developing Rapidly, and Many Places Have Initiated COVID-19 Vaccination for People Aged 3-11 Years. Authoritative release!. (2021). Available online at: http://www.gov.cn/fuwu/2021-10/31/content_5647958.htm (accessed May 1, 1985).
15. National Health Commission. The General Office of the National Health and Family Planning Commission Issued a Notice on the Standardization of Vaccination Work (2016 edition). Available online at: http://www.nhc.gov.cn/jkj/s3581/201701/8033406a995d460f894cb4c0331cb400.shtml (accessed September 28, 2016).
16. Yan YY, Fan TY, Zheng YL, Yang HQ Li TS, Wang HT, et al. Prevention and control of COVID-19 by primary health care facilities in China: a field-survey-based qualitative study in three typical cities. BMC Health Serv Res. (2022) 22:399. doi: 10.1186/s12913-022-07770-4
17. Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med. (2020) 173:120–36. doi: 10.7326/M20-1632
18. Xu B. The impact of COVID-19 on the doctor-patient relationship in China. Front Public Health. (2022) 10:907009. doi: 10.3389/fpubh.2022.907009
19. Huo L, Zhou Y, Li S, Ning Y, Zeng L, Liu Z, et al. Burnout and its relationship with depressive symptoms in medical staff during the COVID-19 epidemic in China. Front Psychol. (2021) 12:616369. doi: 10.3389/fpsyg.2021.616369
20. Sirois FM, Owens J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: a rapid systematic review of the evidence. Front Psychiatry. (2020) 11:589545. doi: 10.3389/fpsyt.2020.589545
21. Freudenberger HJ. Staff burnout. J Soc Issues. (1974) 30:6. doi: 10.1111/j.1540-4560.1974.tb00706.x
23. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. (2001) 52:25. doi: 10.1146/annurev.psych.52.1.397
24. Maslach C, Leiter M. Understanding the burnout experience; recent research and its implications for psychiatry. World Psychiatry. (2016) 15:8. doi: 10.1002/wps.20311
25. Gajjar J, Pullen N, Li Y, Weir S, Wright JG. Impact of the COVID-19 pandemic upon self-reported physician burnout in Ontario, Canada: evidence from a repeated cross-sectional survey. BMJ Open. (2022) 12:e060138. doi: 10.1136/bmjopen-2021-060138
26. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. (2020) 24:100424. doi: 10.1016/j.eclinm.2020.100424
27. Schaufeli W, Enzmann D. The Burnout Companion to Study and Practice: A Critical Analysis. London: Taylor and Francis (1998).
28. Liu X, Liu J, Liu K, Baggs JG, Wang J, Zheng J, et al. Association of changes in nursing work environment, non-professional tasks, and nursing care left undone with nurse job outcomes and quality of care: a panel study. Int J Nurs Stud. (2021) 115:103860. doi: 10.1016/j.ijnurstu.2020.103860
29. Zhang Y, Wu X, Wan X, Hayter M, Wu J, Li S, et al. Relationship between burnout and intention to leave amongst clinical nurses: the role of spiritual climate. J Nurs Manag. (2019) 27:1285–93. doi: 10.1111/jonm.12810
30. Al Sabei SD, Labrague LJ, Miner Ross A, Karkada S, Albashayreh A, Al Masroori F, et al. Nursing work environment, turnover intention, job burnout, and quality of care: the moderating role of job satisfaction. J Nurs Scholarsh. (2020) 52:95–104. doi: 10.1111/jnu.12528
31. Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs. (2005) 51:11. doi: 10.1111/j.1365-2648.2005.03494.x
32. Gonzalez-Morales MG, Peiro JM, Rodriguez I, Bliese PD. Perceived collective burnout: a multilevel explanation of burnout. Anxiety Stress Coping. (2012) 25:43–61. doi: 10.1080/10615806.2010.542808
33. Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. (2015) 12:652–66. doi: 10.3390/ijerph120100652
34. Sharma A, Balda S, Apreja M, Kataria K, Capalash N, Sharma P. COVID-19 diagnosis: current and future techniques. Int J Biol Macromol. (2021) 193:1835–44. doi: 10.1016/j.ijbiomac.2021.11.016
35. Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. (2021) 398:2126–8. doi: 10.1016/S0140-6736(21)02758-6
36. Hangzhou Municipal Government Hangzhou Hangzhou Bureau of Statistics. Hangzhou Overview. Available online at: http://tjj.hangzhou.gov.cn/art/2022/6/30/art_1655071_34573337.html (accessed October 4, 2022).
37. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behav. (1980) 2:15. doi: 10.1002/job.4030020205
38. Fang P, Liu X, Huang L, Zhang X, Fang Z. Factors that influence the turnover intention of Chinese village doctors based on the investigation results of Xiangyang City in Hubei Province. Int J Equity Health. (2014) 13:9. doi: 10.1186/s12939-014-0084-4
39. Wu S, Zhu W, Wang Z, Wang M, Lan Y. Relationship between burnout and occupational stress among nurses in China. J Adv Nurs. (2007) 59:233–9. doi: 10.1111/j.1365-2648.2007.04301.x
40. Wu H, Liu L, Sun W, Zhao X, Wang J, Wang L. Factors related to burnout among Chinese female hospital nurses: cross-sectional survey in Liaoning Province of China. J Nurs Manag. (2014) 22:621–9. doi: 10.1111/jonm.12015
41. Brenninkmeijer V, VanY, Peren N. How to conduct research on burnout; advantages and disadvantages of a unidimensional approach in burnout research. Occup Environ Med. (2003) 60 (Suppl. I):5. doi: 10.1136/oem.60.suppl_1.i16
42. Qiao Z, Chen L, Chen M, Guan X, Wang L, Jiao Y, et al. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: a cross-sectional study. BMC Public Health. (2016) 16:335. doi: 10.1186/s12889-016-2890-7
43. Li S, Li Y, Lv H, Jiang R, Zhao P, Zheng X, et al. The prevalence and correlates of burnout among Chinese preschool teachers. BMC Public Health. (2020) 20:160. doi: 10.1186/s12889-020-8287-7
44. Pei P, Lin G, Li G, Zhu Y, Xi X. The association between doctors' presenteeism and job burnout: a cross-sectional survey study in China. BMC Health Serv Res. (2020) 20:715. doi: 10.1186/s12913-020-05593-9
45. Xu W, Pan Z, Li Z, Lu S, Zhang L. Job burnout among primary healthcare workers in rural China: a multilevel analysis. Int J Environ Res Public Health. (2020) 17:727. doi: 10.3390/ijerph17030727
46. Hou J, Xu B, Zhang J, Luo L, Pen X, Chen S, et al. Psychological status and job burnout of nurses working in the frontline of the novel coronavirus in China during the delta variant outbreak: a cross-sectional survey. Psychol Res Behav Manag. (2022) 15:533–46. doi: 10.2147/PRBM.S343749
47. Shi C, Luo JM, Xiao Y. The association of sleep quality and burnout among Chinese medical residents under standardized residency training in a tertiary hospital. Sleep Breath. (2022) 1–8. doi: 10.1007/s11325-022-02621-2
48. Li D, Wang Y, Yu H, Duan Z, Peng K, Wang N, et al. Occupational burnout among frontline health professionals in a high-risk area during the COVID-19 outbreak: a structural equation model. Front Psychiatry. (2021) 12:575005. doi: 10.3389/fpsyt.2021.575005
49. Wen J, Cheng Y, Hu X, Yuan P, Hao T, Shi Y. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci Trends. (2016) 10:27–33. doi: 10.5582/bst.2015.01175
50. Balch CM, Shanafelt TD, Dyrbye L, Sloan JA, Russell TR, Bechamps GJ, et al. Surgeon distress as calibrated by hours worked and nights on call. J Am Coll Surg. (2010) 211:609–19. doi: 10.1016/j.jamcollsurg.2010.06.393
51. Dall'Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses' job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. (2015) 5:e008331. doi: 10.1136/bmjopen-2015-008331
52. Lu Y, Liu Q, Yan H, Gao S, Liu T. Job burnout and its impact on work ability in biosafety laboratory staff during the COVID-19 epidemic in Xinjiang. BMC Psychiatry. (2021) 21:543. doi: 10.1186/s12888-021-03555-x
53. Chen X, Jing L, Wang H, Yang J. How medical staff alleviates job burnout through sports involvement: the mediating roles of health anxiety and self-efficacy. Int J Environ Res Public Health. (2022) 19:11181. doi: 10.3390/ijerph191811181
54. Zhao X, Liu S, Chen Y, Zhang Q, Wang Y. Influential factors of burnout among village doctors in China: a cross-sectional study. Int J Environ Res Public Health. (2021) 18:2013. doi: 10.3390/ijerph18042013
55. Yang Q, Zhang H, Yu M, Hu X, Gu Y, Sun X, et al. Chinese minority perceives the doctor-patient relationship differently: a cultural and economic interpretation. Front Public Health. (2019) 7:330. doi: 10.3389/fpubh.2019.00330
56. Si Y. When to end the continuing violence against physicians in China. J Public Health. (2021) 43:e129–30. doi: 10.1093/pubmed/fdaa116
57. Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. (2008) 93:498–512. doi: 10.1037/0021-9010.93.3.498
58. Li H, Yuan B, Meng Q, Kawachi I. Contextual factors associated with burnout among Chinese primary care providers: a multilevel analysis. Int J Environ Res Public Health. (2019) 16 3555. doi: 10.3390/ijerph16193555
59. Lu S, Zhang L, Klazinga N, Kringos D. More public health service providers are experiencing job burnout than clinical care providers in primary care facilities in China. Hum Resour Health. (2020) 18:95. doi: 10.1186/s12960-020-00538-z
60. Larson HJ, Gakidou E, Murray CJL. The vaccine-hesitant moment. N Engl J Med. (2022) 387:58–65. doi: 10.1056/NEJMra2106441
61. McNeil A, Purdon C. Anxiety disorders, COVID-19 fear, and vaccine hesitancy. J Anxiety Disord. (2022) 90:102598. doi: 10.1016/j.janxdis.2022.102598
62. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. (2020) 14:e0008961. doi: 10.1371/journal.pntd.0008961
63. McClure CC, Cataldi JR, O'Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. (2017) 39:1550–62. doi: 10.1016/j.clinthera.2017.07.003
64. Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
65. Luo A, Kong W, He H, Li Y, Xie W. Status and influencing factors of social media addiction in Chinese medical care professionals: a cross-sectional survey. Front Psychol. (2022) 13:888714. doi: 10.3389/fpsyg.2022.888714
66. Zhang X, Jiang X, Ni P, Li H, Li C, Zhou Q, et al. Association between resilience and burnout of front-line nurses at the peak of the COVID-19 pandemic: positive and negative affect as mediators in Wuhan. Int J Ment Health Nurs. (2021) 30:939–54. doi: 10.1111/inm.12847
67. Wang Z, Xie Z, Dai J, Zhang L, Huang Y, Chen B. Physician burnout and its associated factors a cross-sectional study in Shanghai. J Occup Health. (2014) 56:10. doi: 10.1539/joh.13-0108-OA
68. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. (2011) 306:8. doi: 10.1001/jama.2011.1247
69. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. (2012) 172:1377–85. doi: 10.1001/archinternmed.2012.3199
70. Wan Z, Lian M, Ma H, Cai Z, Xianyu Y. Factors associated with burnout among Chinese nurses during COVID-19 epidemic: a cross-sectional study. BMC Nurs. (2022) 21:51. doi: 10.1186/s12912-022-00831-3
71. Ministry Ministry of Human Resources Social Security RPC,. Guidelines on Deepening the Reform of the Professional Title System for Health Professionals. Available online at: http://www.gov.cn/zhengce/zhengceku/2021-08/05/content_5629566.htm (accessed September 30, 2021).
72. Yates SW. Physician stress and burnout. Am J Med. (2020) 133:160–4. doi: 10.1016/j.amjmed.2019.08.034
73. Zhang A, Nikoloski Z, Albala SA, Yip W, Xu J, Mossialos E. Patient choice of health care providers in china: primary care facilities vs. hospitals. Health Syst Reform. (2020) 6:e1846844. doi: 10.1080/23288604.2020.1846844
74. Gan Y, Jiang H, Li L, Yang Y, Wang C, Liu J, et al. Prevalence of burnout and associated factors among general practitioners in Hubei, China: a cross-sectional study. BMC Public Health. (2019) 19:1607. doi: 10.1186/s12889-019-7755-4
75. Fan C, Cai T, Gai Z, Wu Y. The Relationship between the migrant population's migration network and the risk of COVID-19 transmission in China-empirical analysis and prediction in prefecture-level cities. Int J Environ Res Public Health. (2020) 17:2630. doi: 10.3390/ijerph17082630
76. Du L, Wu R, Chen X, Xu J, Ji H, Zhou L. Role of treatment adherence, doctor-patient trust, and communication in predicting treatment effects among tuberculosis patients: difference between urban and rural areas. Patient Prefer Adherence. (2020) 14:2327–36. doi: 10.2147/PPA.S277650
77. Gopal R, Glasheen JJ, Miyoshi TJ, Prochazka AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. (2005) 165:5. doi: 10.1001/archinte.165.22.2595
78. Chenchula S, Karunakaran P, Sharma S, Chavan M. Current evidence on efficacy of COVID-19 booster dose vaccination against the Omicron variant: a systematic review. J Med Virol. (2022) 94:2969–76. doi: 10.1002/jmv.27697
79. Hangzhou, Municipal Government,. What Epidemic Prevention and Control Measures Have Been Taken in Shangcheng District and Yuhang District? How do Ordinary Citizens Protect Themselves? Here Comes the Definitive Answer. Available online at: http://www.hangzhou.gov.cn/art/2022/7/9/art_1228998467_59061113.html (accessed September 30, 2022).
Keywords: prevalence, vaccination staff, COVID-19, burnout, China
Citation: Gu W, Liu Y, Lu Z, Wang J, Che X, Xu Y, Zhang X, Wang J, Du J, Zhang X and Chen J (2023) Associated factors of burnout among Chinese vaccination staff during COVID-19 epidemic: A cross-sectional study. Front. Public Health 11:1086889. doi: 10.3389/fpubh.2023.1086889
Received: 01 November 2022; Accepted: 20 February 2023;
Published: 08 March 2023.
Edited by:
Sima Rafiei, Qazvin University of Medical Sciences, IranReviewed by:
Adriano Friganovic, University of Rijeka, CroatiaChuanxi Fu, Zhejiang Chinese Medical University, China
Haimei Jia, Fuzhou Center for Disease Control and Prevention, China
Copyright © 2023 Gu, Liu, Lu, Wang, Che, Xu, Zhang, Wang, Du, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Liu, c21pbGVmb3JldmVyODFAMTI2LmNvbQ==
 Wenwen Gu
Wenwen Gu Yan Liu
Yan Liu Yuyang Xu
Yuyang Xu Xuechao Zhang
Xuechao Zhang