
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 15 February 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1078009
This article is part of the Research Topic Reviews in Infectious Diseases – Surveillance, Prevention and Treatment View all 5 articles
Background: Vaccination is the most effective method to prevent the spread of infectious diseases. Nevertheless, vaccine hesitancy has been an issue. Parental hesitancy toward vaccines is a major part of the problem. COVID-19 vaccine acceptance is no different, it poses another challenge in facing the pandemic. In Low- and Middle-Income Countries (L&MICs) several studies measured parents' acceptance to vaccinate their children against COVID-19 and resulted in different acceptance proportions.
Aims: The paper aims at obtaining a precise estimate of the overall proportion of L&MICs' parents accepting to vaccinate their children against COVID-19 and identifying the main determinant of their decisions.
Methods: This meta-analysis follows the PRISMA 2020 statement on updated guidelines and the checklist for reporting systematic reviews. Studies published between December till February 2022 were assessed for inclusion. The final effect size (i.e., the proportion of parents in L&MICs accepting to vaccinate their children against COVID-19) was measured using the Arcsine proportions method. Analysis was done using R program.
Results: The proportion of parents in L&MICs accepting to vaccinate their children against COVID-19 is 49%. The major reason for their acceptance is their belief that COVID-19 vaccine is fundamental to the fight against the pandemic while the most common factor for parents' hesitancy to vaccinate their children against COVID-19 is their concerns about vaccine efficacy, safety, and possible side effects.
Conclusion: The proportion of parents in L&MICs accepting to vaccinate their children against COVID-19 is lower than the global level. To increase parental acceptance, responsible authorities should concentrate on increasing their population's trust in the government and in vaccine manufacturers. As well as concentrating on increasing acceptance of the vaccine idea in general.
Vaccination is one of the most important achievements in medical and public health history. It has proved to be the most effective method to prevent the spread of infectious diseases (1). Nevertheless, vaccine hesitancy has been an issue for a while now. Some people are reluctant to be vaccinated, which increases their risk for diseases and increases the risk of public threat through diminishing the ability to achieve and sustain “herd immunity” (2). Vaccine hesitancy is defined as the “delay in acceptance or refusal of vaccination despite availability of vaccination services” (3). People's acceptance of a vaccine is known to be influenced by several factors related to the people themselves (e.g., education level, complacency, convenience), to the vaccine (e.g., safety and efficacy) and to external factors (e.g., policies, media, confidence) (4, 5).
People opposing vaccines are called “anti-vaxxers.” Studies have found that anti-vaxxers are mostly mothers who are older in age with higher education and socioeconomic status (6). Since children are normally the largest vaccine recipient group, parental hesitancy toward vaccines is a major part of the problem of stopping the spread of infectious diseases.
COVID-19 is no different case from other infectious diseases when it comes to vaccines. Although COVID-19 has resulted in millions of deaths and the count is still going on. COVID-19 vaccine acceptance proves to pose another challenge in facing the pandemic (7). COVID-19 vaccine acceptance is a worldwide issue (8). However, L&MICs seem to have a special context where certain L&MICs have a higher acceptance rate than some High-Income Countries (HICs) (9). A number of studies address COVID-19 vaccines acceptance in L&MICs (9–11). These studies concluded different acceptance proportions and different factors influencing vaccine acceptance decisions. As for the parents' population, many studies were performed to study parents' acceptance of COVID-19 vaccines and the determinants of their behavior. However, many of these studies were conducted in HICs (12–14).
Given the difference in the COVID-19 vaccine acceptance rate between L&MICs countries and HICs and the fact that fewer studies are addressing parental vaccination hesitancy and the factors underlying the parents' decisions, and the urgency of research in L&MICs countries, we set our research questions as follows. “What proportion of the parents' population is willing to give the COVID-19 vaccine to their children in L&MICs?” And “what are the factors influencing their decision?”. Thereafter, this meta-analysis study aims at assessing the published literature on parents' acceptance in L&MICs in order to provide a more credible estimate of the proportion of parents accepting to vaccinate their children against COVID-19 as well as to identify determinants of COVID-19 vaccine parents' acceptance to vaccinate their children in L&MICs.
This meta-analysis followed the PIO framework (Population, Intervention, and Outcome)used in the Evidence Based Medicine EBM (15) and the PRISMA 2020 statement on updated guidelines and the checklist for reporting systematic reviews (16). The target population (P) was the L&MICs population, of parents, caregivers, and guardians; intervention (I) was COVID-19 vaccination intention, and outcome (O) was COVID-19 vaccine hesitancy or acceptance among the target population.
Studies included in this meta-analysis needed to confirm with the following criteria: published between December 2021 (first vaccine approval) till February 2022, use either quantitative or mixed methodology, express COVID-19 acceptance or hesitancy using proportions or absolute numbers, target L&MICs' population (parents, caregivers, and guardians) with accessibility to the COVID-19 vaccine, and finally, original peer-reviewed studies published in English.
On the other hand, exclusion criteria were: studies targeting populations other than parents, caregivers, or guardians; written in languages other than English; targeting HICs countries; using a qualitative approach.
The search for the peer-reviewed studies was performed in three main databases: PubMed, Web of Science, and Cochrane Library. The following keywords–COVID-19, vaccine, hesitancy, and acceptance–were searched in the three databases using Boolean operators, truncation, and wildcard, where appropriate. The search term differed according to each database recommended search mechanism. Accordingly, the exact used search terms were:
(“COVID-19”[MeSH Terms] OR “COVID-19 Vaccines”[MeSH Terms]) AND (“vaccine*”[Text Word] OR “Vaccines”[MeSH Terms]) AND (“vaccine acceptance”[Text Word] OR “Vaccination Hesitancy”[MeSH Terms]) AND (english[Filter]).
#1 MeSH descriptor: [Vaccination Hesitancy] explode all trees.
#2 (vaccin* NEXT(hisitanc* or acceptanc*)):ti,ab,kw (Word variations have been searched).
#3 #1 Or #2.
#4 MeSH descriptor: [COVID-19 Vaccines] explode all trees.
#5 (COVID* NEXT (Vaccin*)):ti,ab,kw (Word variations have been searched).
#6 #4 OR #5.
#7 #3 AND #6.
(((AB=(vaccin* acceptance)) OR AB=(vaccin* hesitancy)) AND AB=(COVID-19)) AND ((LA==(“ENGLISH”) NOT CU==(“USA” OR “ENGLAND” OR “ITALY” OR “CANADA” OR “FRANCE” OR “DENMARK” OR “KUWAIT” OR “PEOPLES R CHINA” OR “GERMANY” OR “AUSTRALIA” OR “SAUDI ARABIA” OR “CROATIA” OR “VENEZUELA” OR “U ARAB EMIRATES” OR “NEW ZEALAND” OR “ROMANIA” OR “CYPRUS” OR “HUNGARY” OR “LUXEMBOURG” OR “URUGUAY” OR “TRINIDAD TOBAGO” OR “SWITZERLAND” OR “SWEDEN” OR “SOUTH KOREA” OR “SINGAPORE” OR “QATAR” OR “PORTUGAL” OR “POLAND” OR “PANAMA” OR “OMAN” OR “NORWAY” OR “NETHERLANDS” OR “MALTA” OR “LITHUANIA” OR “JAPAN” OR “ISRAEL” OR “IRELAND” OR “GREECE” OR “FINLAND” OR “CZECH REPUBLIC” OR “CHILE” OR “BELGIUM” OR “BARBADOS” OR “BAHRAIN” OR “AUSTRIA”)) NOT (SE==(“LECTURE NOTES IN COMPUTER SCIENCE” OR “LECTURE NOTES IN OPERATIONS RESEARCH SPRINGER”) OR CF==(“16TH INTERNATIONAL CONFERENCE ON AVAILABILITY RELIABILITY AND SECURITY ARES” OR “EASTERN ALLERGY CONFERENCE”))).
The databases' search was done in the title and abstract.
Two authors (W.A.E.K.-M. and B.M.S.) independently identified and extracted the studies from the databases. The identified studies were imported into Zotero, a citation managing software that can locate duplicates and eliminate them. After removing the duplicates, the remaining studies were screened independently by both reviewers for eligibility. The screening was done in two steps. The first screening included title and abstract screening. Studies that passed the first screening went into the second step of screening where a full text article assessment was performed to confirm eligibility.
Studies which passed the two steps of screening were imported to an excel sheet table. The following information was extracted and entered to the excel sheet for each study: title, author, year of publication, sample size, proportions of the population that accepted/hesitated/refused the vaccine, and factors underlying parents' decisions.
The chosen studies were evaluated by two independent reviewers. The studies were evaluated based on the five Cochrane criteria: bias resulting from deviations from intended interventions, bias resulting from missing outcome data, bias in measuring the outcome, bias resulting from the randomization process, and bias resulting from the selection of reported results. The studies met four of the criteria for validation. The randomization criterion was not used since the studies are not randomized control studies. The two reviewers discussed their findings and came to an agreement on the included ones.
Data analysis was done in two steps. First, a descriptive analysis of the studies was performed including distribution of the studies among countries and among country classification, sample size, type of study, and data collected in each study. Second, a meta-analysis using R program. Meta-analysis was first done using the observed proportion method. This method assumes that parents' acceptance proportions follow a normal or binomial distribution (bell-shaped, centered around 0.5) with minimal variance which is seldom the case. Then second, using the Arcsine proportion model. The Arcsin proportion model is one of the statistical models used to transform proportions (i.e., the data used in this study) so that their distribution be more approximate to a normal distribution which is an assumption required by meta-analysis models (17). The Arcsin model acknowledges that proportional data derived from real studies are mostly not normally distributed (skewed) and that there is variance among different studies measures (e.g., proportion). Thus, accounting for skewness and stabilizing the variance among studies making it more constant. Both the observed proportions analysis and the Arcsine proportion analysis were done using: first, fixed effect model which assumes homogeneity of studies, and second, a random effect model. The random effect model is used due to the fact that the include studies are heterogeneous as proved in the fixed effect model. Finally, a brief analysis of the major factors underlying parents' COVID-19 vaccine acceptance was done.
The primary database search resulted in 806 studies. The number of studies was reduced to 742 after the first stage of screening and elimination of duplicates. Checking the title and abstract against the eligibility criteria, 712 studies were eliminated for one of the following reasons: being a qualitative study, not done in L&MICs, and the population used in the study is not parents. The remaining 30 studies passed through a full-text screening.
From the remaining 30 studies, seventeen studies were eliminated for combining both HICs and L&MICs in the same study calculations or for not collecting the same data as required by the methodology (Figure 1).
Thirteen studies were finally included in the meta-analysis. The studies included were cross-sectional type of studies. Only 10 out of 13 studies clearly stated the type of study in the text (Table 1). Two studies declared using a validated data collection tool (18, 19), while three provided the sources upon which their questionnaires were based (20, 21, 29). Certain variations were noticed among the studies: first, the study population. Seven out of thirteen studies did not have any specifications on the parents nor the children population in their sample, while two studies specified the age of participants as a criterion to choose participants (18, 23), one study specified that the participants were mothers (24), and two studies defined the parents' population to have children with specific medical conditions (25, 29). Second, the sample size, which ranged between 201 participants and 3079 participants among the studies. Third, the measurement term used within the study. Three main terms were used (acceptance, hesitancy, and refusal). Three out of thirteen studies used and provided data for all three terms (18, 25–27), while five studies used hesitancy only (20, 22, 23, 28, 29), and four used acceptances only (19, 21, 24, 30).
As for the country where studies were performed, one can notice that 69% of the studies took place in Upper Middle-Income Countries UMICs (six in Turkey, two in China, and one in Brazil), while three studies were done in Lower Middle-Income Countries LMICs (two in Bangladesh and one in Vietnam) and one study in Nigeria, which is a Low-Income Country LIC (Table 1).
Looking at the required statistic (acceptance proportion) -which is either directly provided by the study or calculated through using other terms (e.g., hesitancy and refusal)- and the sample size, one can observe that it ranges between 4.9 and 91%, indicating huge variation among included studies (Table 1).
Although the 13 included studies have a wide range of sample sizes and resulted in different COVID-19 vaccine acceptance among parents, they are all significant. None of the studies crosses the vertical null effect line (Figure 2).
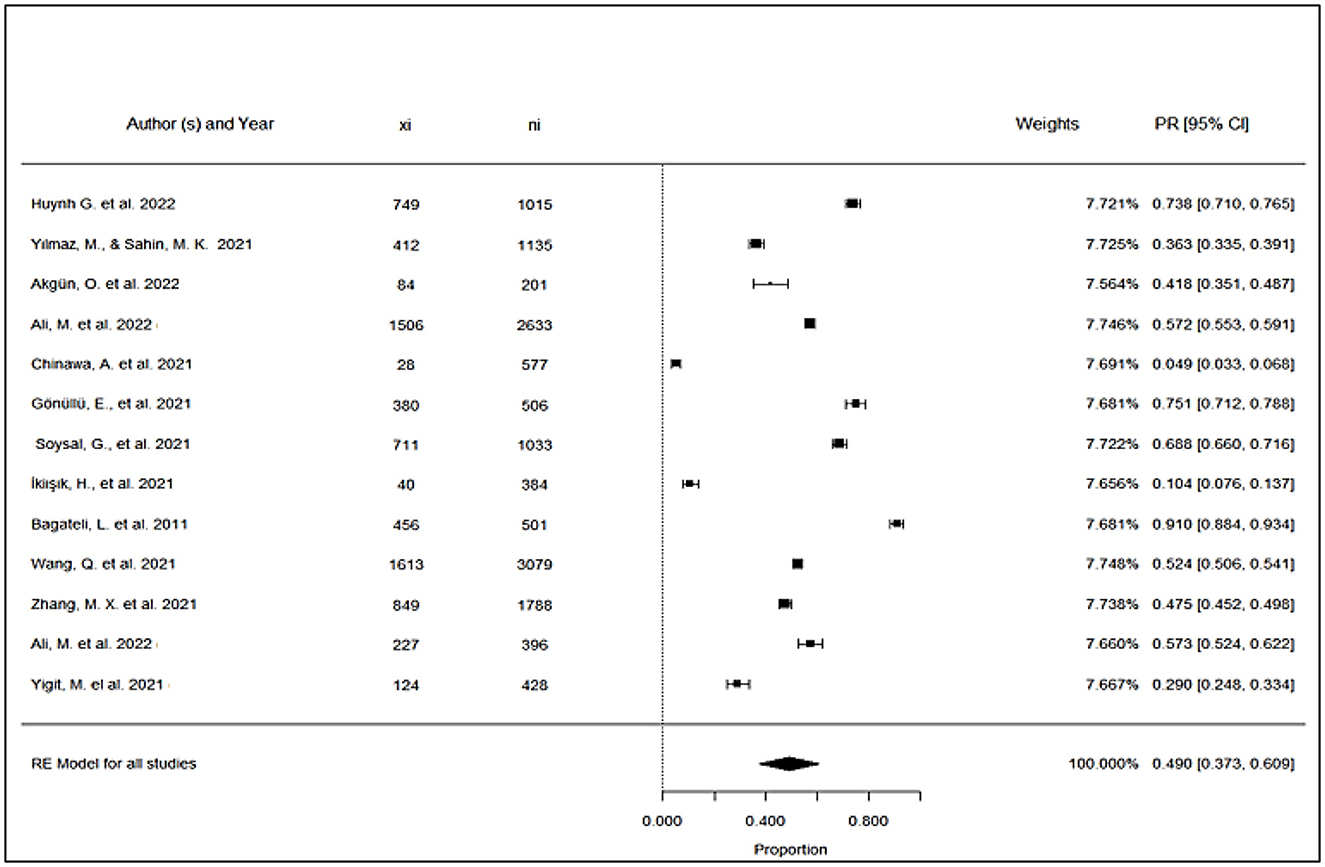
Figure 2. Forest plot: proportion of parents accepting to vaccinate their children against COVID-19 in L&MICs.
However, knowing that using the observed proportions method entails assuming that the proportions identified across the collection of studies follow a normal or binomial distribution with minimal variance, the Arcsine proportions method - which acknowledges that proportional data derived from real studies is mostly skewed and that there is variance among different studies measures- was used. The meta-analysis (Table 2) using the arcsine proportion models shows high heterogeneity among studies and the random effect model indicates the model is effective (p < 0.0001).

Table 2. Arcsine proportions of parents accepting to vaccinate their children against COVID-19 in L&MICs and effect sizes.
When the results of arcsine proportions are transferred to normal proportions, the final effect size for these studies becomes 49.0% which happens to be significant with confidence limits of 37.3% and 60.9% within a confidence interval of 95% (Figure 2). Moreover, the studies have narrow confidence limits resulting in minimal differences in weights assigned to the different studies (Figure 2).
Concerning the factors affecting parents' decisions regarding the COVID-19 vaccination of their children, they are numerous and vary among studies (Annex 1). The most common factor for parents' hesitancy to vaccinate their children against COVID-19 is their concerns about vaccine efficacy, safety, and possible side effects. This factor was mentioned in 11 studies out of 13. On the other hand, the most common factor for parents' acceptance to vaccinate their children is their conviction that the vaccine is needed to control COVID-19 and end the pandemic. Lastly, parents refused to vaccinate their children due to distrust of vaccine manufacturing companies and vaccine safety and efficacy.
Given the COVID-19 gravity, assessing vaccine hesitancy has become very crucial for governments and policymakers. Persuading people to be vaccinated is essential to protect themselves and others by limiting the global spread. An important category regarding vaccine hesitancy is the parents or caregivers who influence the vaccination process of their children. The number of studies included in this meta-analysis, and their distribution indicates the weak attention given to parents' behavior against COVID-19 vaccine in L&MICs especially in LICs (24). Taking into account the higher fertility rate and higher proportion of children in L&MICs, concentrating on parents' behavior might be a key factor in fighting against the COVID-19 pandemic.
It is worth noting that the most common announced factor for parents' acceptance to vaccinate their children is that the vaccine is needed to control COVID-19 and end the pandemic which indicates a certain level of these parents' awareness regarding COVID-19 and the vaccine (23, 25, 26, 30). Other acceptance factors mentioned in the studies are equally important (Annex 1). Parents accepting to vaccinate their children are found to be the parents who accept the notion of vaccines in general, they believe that the benefit of vaccination outweighs its harm. These are parents who are vaccinated yearly against influenza and who follow vaccination regimes for their children (18, 30). This signifies that parents' acceptance to vaccinate their children against COVID-19 is more related to the fact that they believe in the benefit of vaccine rather than the fear of COVID-19 itself.
As for factors related to COVID-19 vaccine hesitancy and refusal, the most commonly identified factor is the uncertainty about COVID-19 vaccine efficacy, safety and possible side effects (18, 22, 26, 27, 29). This factor highlights the lack of trust that the parents have in their governments as well as vaccine manufacturers (27, 29). This factor can be related to the final proportion of parents accepting to vaccinate their children against COVID-19, which is around 49% (Figure 2).
The above proportion is lower than the worldwide estimated proportion. According to a similar meta-analysis done on a global level (i.e., HICS, MICs and LICs are included), parents' willingness to vaccinate their children ranges between 25.6 and 92.2% worldwide; and the overall proportion of parents intending to vaccinate their children against COVID-19 is 60.1% (31). This may be related to various reasons. In African countries, the demand for vaccine decreased due to public concerns about the possibility of COVID-19 exposure when receiving vaccination. This concern has equally affected parental health-seeking behavior resulting in lower parental acceptance (32). Other reasons for the lower parental acceptance in L&MICs might be related to factors such as trust in authorities and subsequently trust in the type of vaccine provided by the country. Also, some L&MICs might concentrate less on health promotion strategies and the availability of data on COVID-19 vaccines' safety and efficacy compared to HICs. Finally, the economic status and the educational background may play a role in the reduced parental acceptance. People in some of these countries are extremely poor with low education hence might be ignorant of the benefits of the vaccine. Others might trust traditional medical practice over conventional medicine resulting in lower acceptance rate.
Given that educational background, economic status, and available health promotion strategies all influence individual perceptions of vaccines, addressing the fears of anti-vaxxers is of great importance, especially in the presence of inconsistent information regarding vaccine safety and efficacy that may be present on different live or online networks. Healthcare providers can help parents overcome their fears about vaccinating themselves and their children. Healthcare providers need to have the proper knowledge and the essential skills to address these fears correctly.
The fact that there are different terms used to address parents' behavior concerning vaccinating their children against COVID-19 indicates that researchers ought to consider adding a clear definition of the terms they use in their studies to avoid confusions, especially that the terms acceptance and refusal are present in the definition of vaccine hesitancy. Moreover, not all studies use a validated data collection tool, resulting in variation in the data collected, especially the factors underlying parents' decisions, which in turn renders comparing between the studies and stating unified factors for the L&MICs parents' decisions more difficult.
This study has its limitations such as language bias. Only English studies were eligible to be included, which means that many non-English studies are missing. Also, the timeframe for the study. Although it is necessary to set a timeframe for the study as the pandemic is still ongoing and more studies will come out, setting a timeframe here limits the number of studies included. These limitations call for further research that can include other languages published studies over a longer period of time.
This meta-analysis concludes that the proportion of parents in L&MICs accepting to vaccinate their children against COVID-19 is 49%, and the major reason for their acceptance is that they believe that COVID-19 vaccine is fundamental to the fight against the pandemic. To increase parental acceptance, responsible authorities should concentrate on increasing their population trust in the government as well as in the vaccine manufacturers. In addition, authorities ought to concentrate on increasing acceptance of the vaccine idea in general through highlighting the need for the vaccine to end the pandemic and assuring the efficacy and safety of the vaccine. Further research on parental behavior concerning vaccinating of their children is needed in L&MICs especially in LICs.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
WA participating in conceptualization, methodology framing, validation, formal analysis, investigation, writing the original draft, reviewing, and editing of the manuscript. BS participated in methodology framing, validation, investigation, writing, reviewing, and editing of the manuscript. HE-F participated in validation, reviewing, and editing of the manuscript. SC participating in conceptualization, methodology framing, validation, formal analysis, investigation, reviewing, and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1078009/full#supplementary-material
1. Frieden TR, Khabbaz RF, Redd SC, Bell BP, Fenton K, Schuchat A, Cock KD. A CDC framework for preventing infectious diseases-Sustaining the essentials and innovating for the future. Centers for Disease Control and Prevention. Atlanta. (2011).
2. Jacobson RM. St Sauver JL, Finney Rutten LJ. Vaccine hesitancy. Mayo Clin Proc. (2015) 90:1562–8. doi: 10.1016/j.mayocp.2015.09.006
3. Report of the Sage Working Group on Vaccine Hesitancy | The Compass for SBC. (2014). Available online at: https://www.thecompassforsbc.org/sbcc-tools/report-sage-working-group-vaccine-hesitancy (accessed February 07, 2022).
4. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
5. Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccines Immunother. (2013) 9:1755–62. doi: 10.4161/hv.25085
6. Hussain A, Ali S, Ahmed M, Hussain S. The anti-vaccination movement: a regression in modern medicine. Cureus. (2018) 10:e2919. doi: 10.7759/cureus.2919
7. Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. (2020) 35:775–9. doi: 10.1007/s10654-020-00671-y
8. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. (2021) 9:160. doi: 10.3390/vaccines9020160
9. Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat Med. (2021) 27:1385–94. doi: 10.1038/s41591-021-01454-y
10. Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, Hasan MT, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low-and middle-income countries. Vaccines. (2021) 9:515. doi: 10.3390/vaccines9050515
11. Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient Prefer Adherence. (2021) 15:1795. doi: 10.2147/PPA.S324564
12. Cella P, Voglino G, Barberis I, Alagna E, Alessandroni C, Cuda A, et al. Resources for assessing parents' vaccine hesitancy: a systematic review of the literature. J Prev Med Hyg. (2020) 61:E340–73.
13. Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. (2020) 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027
14. Goldman RD, Bone JN, Gelernter R, Krupik D, Ali S, Mater A, et al. National COVID-19 vaccine program progress and parents' willingness to vaccinate their children. Hum Vaccines Immunother. (2021) 17:4889–95. doi: 10.1080/21645515.2021.1999144
15. Mezaoui H, Gontcharov A, Gunasekara I. Enhancing PIO element detection in medical text using contextualized embedding. ArXiv190611085. (2019) 217–22. doi: 10.48550/arXiv.1906.11085
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
17. Lin L, Xu C. Arcsine-based transformations for meta-analysis of proportions: Pros, cons, and alternatives. Health Sci Rep. (2020) 3:e178. doi: 10.1002/hsr2.178
18. Soysal G, Durukan E, Akdur R. The evaluation of vaccine hesitancy and refusal for childhood vaccines and the COVID-19 vaccine in individuals aged between 18 and 25 years. Turk J Immunol. (2021) 9:120–7. doi: 10.4274/tji.galenos.2021.35229
19. Wang Q, Xiu S, Zhao S, Wang J, Han Y, Dong S, et al. Vaccine hesitancy: COVID-19 and influenza vaccine willingness among parents in wuxi, China—a cross-sectional study. Vaccines. (2021) 9:342. doi: 10.3390/vaccines9040342
20. Huynh G, Nguyen H, Tran K, An P, Tran T. Determinants of COVID-19 vaccine hesitancy among parents in Ho Chi Minh City, Vietnam. Postgrad Med. (2022) 134:1–6. doi: 10.1080/00325481.2022.2044142
21. Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani GP. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines. (2021) 9:1115. doi: 10.3390/vaccines9101115
22. Ali M, Proma TS, Tasnim Z, Islam MdA, Urmi TA, Ahmed S, et al. Parental COVID-19 vaccine hesitancy for children with neurodevelopmental disorders: a cross-sectional survey. Trop Med Health. (2022) 50:24. doi: 10.1186/s41182-022-00415-6
23. Ikiışık H, Akif Sezerol M, Taşçi Y, Maral I. COVID-19 vaccine hesitancy: a community-based research in Turkey. Int J Clin Pract. (2021) 75:e14336. doi: 10.1111/ijcp.14336
24. Chinawa AT, Chinawa JM, Ossai EN, Obinna N, Onukwuli V, Aronu AE, et al. Maternal level of awareness and predictors of willingness to vaccinate children against COVID 19; A multi-center study. Hum Vac Immunother. (2021) 17:3982–8. doi: 10.1080/21645515.2021.1963172
25. Akgün Ö, Kayaalp GK, Demirkan FG, Çakmak F, Tanatar A, Guliyeva V, et al. Exploring the attitudes, concerns, and knowledge regarding COVID-19 vaccine by the parents of children with rheumatic disease: cross-sectional online survey. Vaccine. (2022) 40:1829–36. doi: 10.1016/j.vaccine.2022.01.061
26. Yilmaz M, Sahin M. Parents' willingness and attitudes concerning the COVID-19 vaccine: a cross-sectional study. Int J Clin Pract. (2021) 75. doi: 10.1111/ijcp.14364
27. Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. (2021) 40:e134–6. doi: 10.1097/INF.0000000000003042
28. Zhang MX, Lin XQ, Chen Y, Tung TH, Zhu JS. Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev Vaccines. (2021) 20:1339–49. doi: 10.1080/14760584.2021.1967147
29. Ali M, Ahmed S, Bonna AS, Sarkar AS, Islam MA, Urmi TA, et al. Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study. F1000Research. (2022) 11:90. doi: 10.12688/f1000research.76181.2
30. Gönüllü E, Soysal A, Atici S, Engin M, Yeşilbaş O, Kasap T, et al. Pediatricians' COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: a cross-sectional survey in Turkey. Hum Vaccines Immunother. (2021) 17:2389–96. doi: 10.1080/21645515.2021.1896319
31. Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. (2022) 157:106994. doi: 10.1016/j.ypmed.2022.106994
Keywords: vaccine hesitancy, COVID-19, Low-Income Countries, Middle-Income Countries, parental
Citation: Abu El Kheir-Mataria W, Saleh BM, El-Fawal H and Chun S (2023) COVID-19 vaccine hesitancy among parents in Low- and Middle-Income Countries: A meta-analysis. Front. Public Health 11:1078009. doi: 10.3389/fpubh.2023.1078009
Received: 23 October 2022; Accepted: 30 January 2023;
Published: 15 February 2023.
Edited by:
Sunil Dhiman, Defence Research and Development Establishment (DRDE), IndiaReviewed by:
Khadijeh Ezoji, Babol University of Medical Sciences, IranCopyright © 2023 Abu El Kheir-Mataria, Saleh, El-Fawal and Chun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sungsoo Chun, c3VuZ3Nvby5jaHVuQGF1Y2VneXB0LmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.