
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 02 June 2023
Sec. Public Health Education and Promotion
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1077068
This article is part of the Research TopicProtecting, Promoting and Supporting BreastfeedingView all 12 articles
 Nieves Amat Camacho1,2*
Nieves Amat Camacho1,2* Abdullahi Chara3
Abdullahi Chara3 Emily Briskin4
Emily Briskin4 Umberto Pellecchia4
Umberto Pellecchia4 Htet Aung Kyi3
Htet Aung Kyi3 Maria Livia de Rubeis4
Maria Livia de Rubeis4 Faisal Hussain3
Faisal Hussain3 Tasneem Ahmed5
Tasneem Ahmed5 Oluwakemi F. Ogundipe5
Oluwakemi F. Ogundipe5 Chiara Burzio5
Chiara Burzio5 Uba Kamis6
Uba Kamis6 Lawan M. Bukar7
Lawan M. Bukar7 Johan Von Schreeb1
Johan Von Schreeb1 Ourania Kolokotroni8
Ourania Kolokotroni8 Francesco Della Corte2
Francesco Della Corte2 Temmy Sunyoto4
Temmy Sunyoto4Background: Breastfeeding (BF) should be protected, promoted, and supported for all infants in humanitarian settings. The re-establishment of exclusive BF is also a central part of the management of acutely malnourished infants under 6 months (<6 m). Médecins Sans Frontières (MSF) runs a nutrition project in Maiduguri, a protracted emergency setting in North-East Nigeria. This study aimed to explore caregivers' (CGs) and health workers' (HWs) perceptions of BF practice, promotion, and support among CGs with infants <6 m in this setting.
Methods: We conducted a qualitative study using in-depth interviews and focus group discussions combined with non-participant observations. Participants included CGs of young infants enrolled in MSF nutritional programs or who attended health promotion activities in a displacement camp. MSF HWs were involved at different levels in BF promotion and support. Data were collected involving a local translator and analyzed using reflexive thematic analysis directly from audio recordings.
Results: Participants described how feeding practices are shaped by family, community, and traditional beliefs. The perception of breastmilk insufficiency was common and led to early supplementary feeding with inexpensive but unsuitable products. Participants often linked insufficient breastmilk production with poor maternal nutrition and stress, in a context shaped by conflict and food insecurity. BF promotion was generally well received but could be improved if tailored to address specific barriers to exclusive BF. Interviewed CGs positively valued BF support received as part of the comprehensive treatment for infant malnutrition. One of the main challenges identified was the length of stay at the facility. Some participants perceived that improvements in BF were at risk of being lost after discharge if CGs lacked an enabling environment for BF.
Conclusion: This study corroborates the strong influence of household and contextual factors on the practice, promotion, and support of BF. Despite identified challenges, the provision of BF support contributes to improvements in BF practice and was positively perceived by CGs in the studied setting. Greater attention should be directed toward providing support and follow-up for infants <6 m and their CGs in the community.
Infants aged <6 months of age (<6 m), with unique food and fluid requirements and an immature immune system, are increasingly vulnerable during humanitarian emergencies (1, 2). Non-breastfed and partially breastfed infants are at higher risk of morbidity and mortality, especially where access to safe breastmilk substitutes, potable water, hygiene, and healthcare services is limited (3–5).
The Operational Guidance for Infant and Young Child Feeding in Emergencies recommends the early initiation of breastfeeding (BF) in all newborns, the transition from mixed to exclusive BF, and the continuation of exclusive BF until 6 months of age. For non-breastfed infants, the guidelines advise considering alternative options such as relactation, wet nursing, or the use of donor human milk. In cases where mothers cannot breastfeed temporarily or definitively, the decision to provide infant formula should be individually assessed and include a package of support for artificial feeding (6).
The re-establishment of exclusive BF is also considered a central part of the management of malnourished infants <6 m, although current recommendations are based on limited and low-quality evidence (7). Increased knowledge of prevention and treatment options is needed, including effective ways to support the re-establishment of BF (8–11).
Considerable barriers can hinder the uptake of BF during humanitarian emergencies. They include the deterioration of maternal wellbeing (due to displacement, stress, and gender-based violence), a lack of privacy or access to lactation support, and the inappropriate distribution of infant formula (8, 12–14). In addition, supporting BF can be challenging for health professionals regardless of their specialization, as they face a demand that requires knowledge, practical skills, and cultural sensitivity, for which they may not feel properly prepared (15).
Unfortunately, scarce literature informs the feasibility, acceptability, and effectiveness of different strategies to promote and support BF during humanitarian emergencies (13, 16, 17). The impact of BF counseling on stressed, traumatized, or malnourished mothers and infants also remains unstudied (18).
For more than a decade, the population in North-East Nigeria has been affected by an ongoing humanitarian emergency driven by a conflict involving Nigerian government forces and armed opposition groups. Nearly 2.2 million people were internally displaced there in mid-2021, a region also exposed to drought, flooding, and disease outbreaks. The loss of livelihoods and food security was further exacerbated by the COVID-19 pandemic (19). Between January and December 2022, over 1.3 million children under 5 years were expected to suffer from acute malnutrition in North-East Nigeria (including over 300,000 cases of severe malnutrition) and more than 152,000 pregnant and lactating women could be acutely malnourished and needing nutrition support (20). The international medical humanitarian organization, Médecins Sans Frontières (MSF), runs a project in Maiduguri, North-East Nigeria, providing nutrition and health support to displaced and host populations in the area.
This study aimed to explore caregivers' (CGs) and health workers' (HWs) experiences and perceptions of BF practice, promotion, and support among infants <6 m in North-East Nigeria. The results can contribute to a strategy for BF promotion and support among CGs with healthy and malnourished infants <6 m in this context.
This qualitative study followed the approach of reflexive thematic analysis proposed by Braun and Clarke, situated within an interpretive qualitative paradigm. This method, increasingly used for applied qualitative health research, respects and expresses the subjectivity of participants' accounts, while acknowledging the reflexive influence of researchers' interpretations (21–23). We adopted a critical orientation to examine how the wider social context may have shaped people's constructed meanings (24). This article adheres to the consolidated criteria for reporting qualitative research (COREQ) checklist (25).
Borno is one of the states in North-East Nigeria, predominantly inhabited by Kanuri, Hausa, Fulani, Babur, Shuwa, and Marghi ethnic groups. Most of the population are Muslim, with smaller Christian and traditionalist minorities. Households are commonly headed by men, and polygyny is estimated to be present in approximately 23% of households (26).
This study took place in an MSF project run in Maiduguri, the capital of Borno State. The project focuses on nutrition and health support for internally displaced people (IDP), mainly providing the following services:
- Ambulatory therapeutic feeding center (ATFC): the center has the capacity for 150 consultations/day, managing severely malnourished children without medical complications and following up with malnourished infants <6 m after discharge.
- Inpatient therapeutic feeding center (ITFC): the center has a 120-bed capacity, including a dedicated ward for infants <6 m (approximately 15 beds).
- Outreach activities covered 10 informal IDP camps providing ATFC, outpatient consultations, sexual and reproductive health, water and sanitation, health promotion, mental healthcare, disease surveillance, and a referral system.
BF promotion targets CGs of both malnourished and non-malnourished infants. It takes place in the community (during outreach health promotion activities) and at the hospital (in waiting areas and hospitalization wards), as part of the general health promotion strategy including other topics. Community health educators and health promotors undertake BF promotion through individual or group talks using pre-determined messaging, flipcharts, or educational videos. During admission to the ITFC ward for malnourished infants <6 m, comprehensive BF support is provided to mothers or wet nurses aiming to re-establish exclusive BF. Discharge from the ITFC depends, in part, on achieving and maintaining weight gain on exclusive BF. Specific support includes frequent encouragement of BF, assistance on BF technique (correct positioning and latching), and breastmilk stimulation through supplementary suckling technique while ensuring appropriate maternal nutrition and rest. Mental health support and psycho-stimulation are provided by mental health counselors in the ward as well as in private dedicated spaces when needed. A team of three health workers is dedicated to this ward in each shift, normally comprising one nurse, one midwife, and one nutritional assistant. Doctors perform daily ward rounds and follow up with infants when necessary.
We purposively selected CGs of infants <6 m (mothers, wet nurses, and close family members) attending the MSF hospital for ATFC follow-up visits or admitted at the ITFC, and during health promotion activities at Mashidimami II, an informal IDP camp. We also selected HWs employed at the MSF project, directly involved in BF promotion or support for CGs with infants <6 m or supervising those activities. Study participants were selected aiming to include different socio-demographic characteristics and job profiles and according to logistical feasibility (availability to participate in the study during the data collection period).
Eligible participants were approached in person by the first author (NAC), and a translator when needed, to explain the study purpose and data collection process and to ask if they would like to participate voluntarily. All invited participants agreed to take part in the study (Figure 1). The recruitment of participants continued until the saturation of salient concepts was observed (27).
Data were collected in March 2022 by NAC with the support of a local translator and a young female community health educator. She was trained for the study and was involved in the preparation of in-depth interviews (IDIs) and revision of audio recordings, to check the consistency of translation and discuss methodological reflexivity within the process (28). A sample of her translations was also assessed by another research team member to ensure translation accuracy.
To favor a confidential environment for more in-depth answers, we choose to conduct IDIs with CGs. Before starting IDIs, basic socio-demographic information was collected from participants and documented on a written form. We used an interview guide with questions and probes (Supplementary material 1), which was tested on two participants; some questions were added as a result. The guide contained questions about infant feeding practices, barriers and enablers to BF, experiences receiving BF promotion and support, and preferences/suggestions for feeding support. The IDIs lasted from 20 to 45 min, were conducted in either Hausa or Kanuri languages, and took place at a private area within the MSF hospital and the informal IDP camp.
Four focus group discussions (FGDs) were organized to explore HWs' experiences and perspectives. Discussions were in English, led by NAC at the MSF hospital, and took from 45 to 80 min. The FGDs were guided by a script containing five key questions with probes comprising: perceptions about common feeding practices; perceived barriers to BF; experiences promoting and supporting BF; barriers to BF promotion and support; perceptions on how BF promotion and support could be improved (Supplementary material 1). An IDI was conducted with one clinical manager to get more in-depth information. The data collection process is summarized in Figure 1. All IDIs and FGDs were audio-recorded with prior authorization from interviewees.
During the data collection period, NAC was immersed in project activities, especially in the ITFC ward dedicated to infants <6 m. She recorded her observations of contextual and personal dynamics in field notes according to recommendations by Phillippi and Lauderdale (29). Notes of non-verbal information and impressions during IDIs and FGDs were not taken during the interviews but were written afterward. At the end of each day, NAC listened to audio-recording samples and revised and expanded the field notes with more thoughtful perceptions (reflective journaling). Most prominent answers were discussed with other field workers involved in the study to gather their views and adjust the data collection process if needed (adding new probes to the IDI guide or FGD script).
We performed direct analysis from the audio recordings, which included original data in English and the recorded translations from Hausa/Kanuri to English. Direct coding from audio files can provide a high level of detail and the ability to capture intonations while reducing coding time (30, 31). Rapid qualitative techniques have been found suitable for complex humanitarian settings to enable the timely acquisition of data during operations (32, 33).
As shown in Table 1, reflexive thematic analysis followed the recommended steps (21, 34). Data were open-coded by NAC, mostly inductively, to best represent its meaning as communicated by the participants. A deductive approach ensured that themes were relevant to answer research questions and objectives (21). Semantic (more explicit) and latent (underlying) meanings were considered, and sometimes extracts were coded twice. Microsoft OneNote was used to code the data from audio files and combine it with field notes (35).
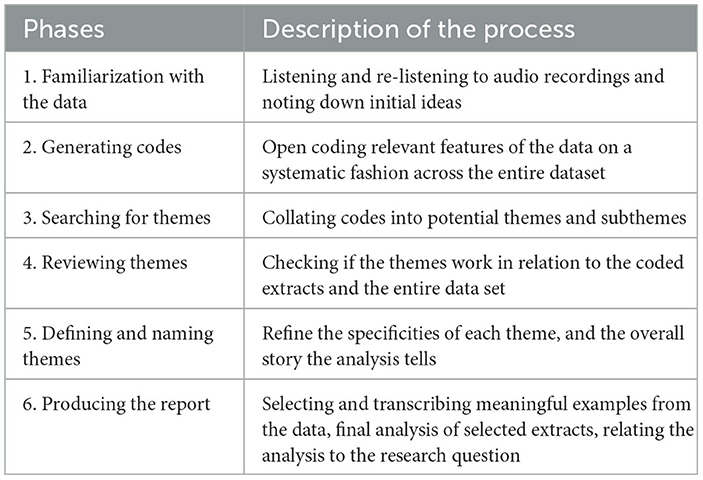
Table 1. Phases of reflexive thematic analysis [adapted from Braun and Clarke (34)].
Audio files, field notes, and the coding matrix were shared among a subgroup of researchers, who helped to refine the themes and subthemes. The results were discussed in a consultative meeting that included the study team members and MSF staff at different levels.
We strived for the trustworthiness of findings by following several steps throughout all phases of reflexive thematic analysis (thick descriptions, prolonged data engagement, reflective journaling, and peer debriefing) as suggested by Nowell et al. (36).
NAC is a female nurse and PhD student from Europe, with some previous experience in qualitative research and humanitarian fieldwork. She is also a mother. Both NAC and the translator were female, which favored trust building with female participants during data collection. The study was conditioned by being conducted within the frame of a project run by an international NGO providing free healthcare. Socio-cultural differences between the principal investigator and the study participants were noteworthy but partly balanced by the presence and inputs of the translator and the inclusion of local colleagues within the research team who could better grasp contextual nuances.
Ethics approval was granted by the MSF Ethics Review Board (ID 2207) and the Borno State Health Research Ethics Committee, Nigeria (Approval No. 113/2022). All study participants granted their written, informed consent before data collection. For illiterate participants, we read the consent form in Hausa or Kanuri languages, and consent was recorded using a thumbprint, witnessed by the translator. We offered in-kind compensation for CGs after they participated in the study. The audio recordings and the signed informed consent forms are stored in a password-protected folder on an MSF server, where they will be kept for 10 years before being deleted.
The characteristics of CGs participating in the study are summarized in Table 2. Most mothers were grand multipara, with a median age of 30 years (IQR = 26–39) and seven children (IQR = 4–7). Only four mothers declared to be exclusively BF at the time of the interview, but two of them reported BF difficulties. Regarding HWs, half of the participants were female, aged between 20 and 40 years, and most had worked on the project for more than 2 years.
The results were grouped into five overarching themes with subthemes (Figure 2) and are described below with illustrative quotes from study participants. To ensure the confidentiality and anonymity of the HWs, quotes were identified as coming from health promotors (referring to health promotors, community health educators, or mental health counselors) or clinical staff (referring to doctors, nurses, midwives, or nutritional assistants).
Overall, there was a positive perception of BF; it was seen as a natural part of motherhood and women felt as if it was a duty. Mothers expressed their wish to breastfeed their babies even if they encountered difficulties. On the other hand, HWs identified a small percentage of mothers who preferred not to breastfeed for different reasons, such as the impact of BF on body image or the assumed superiority of other animal milk (cow or goat), infant formula, or therapeutic milk.
“I feel happy whenever I breastfeed the baby, and breastfeeding is very good… I don't see the reason why I would give birth and I cannot breastfeed the baby.” Mother3
“Some women do not want to breastfeed because [they say]: we feel that when we breastfeed our breasts fall down, so it's no more attractive to the husband.” Clinical staff
In contrast to the mothers' wishes, HWs perceived infant feeding practices, and health-seeking behaviors were frequently determined by the elder members of the family or by the husband. When a mother's and family's preferences contradicted each other, the preferences of the family were usually followed. In some cases, the family enabled and encouraged exclusive BF. The main support for BF expected from husbands was the provision of extra food for mothers while lactating. From the HW's perspective, marital dynamics such as polygyny, early marriage, or domestic violence also shaped mothers' ability and desire to breastfeed.
“The tradition here is that you have to go with what the husband wants or what the mother-in-law wants. So even if you as a mother want to do exclusive breastfeeding, if the husband say no or his mother say no, you cannot do it.” Health promotor [sic]
Infant feeding practices seemed to be greatly influenced by specific traditions and beliefs, which differed among different communities and ethnic groups. Several traditional practices contributed to the delayed start of BF. Traditional medicine and traditional healers were well-rooted inside communities, and they were the first choice for most participants with health concerns including BF. If there was no improvement following traditional healers' advice or the health issues were perceived to be more serious, people sought care in hospitals or formal healthcare facilities. Sometimes traditional healers discouraged exclusive BF or advised them to stop BF.
“In our tradition, if a baby is born, she will not be breastfed till after 3 days. On the fourth day, they will start breastfeeding the baby. (…) we give cow milk, fresh milk, and water during these 3 days.” Grandmother 1
“I had enough breastmilk but when I went to traditional healers, they told me that I had enough breast, but the breast is not that nutritious that can be sufficient for the baby.” Mother 3
Two grandmothers explained how they tried to breastfeed a grandchild for the first days of life, while the baby's mother was sick post-partum. In both cases, the mother died, and grandmothers became the main CGs and wet nurses who could partially breastfeed. However, wet nursing appears to be accepted only when a mother has died and when the wet nurse is the grandmother or some other close relative (a sister or a sister-in-law). In other cases, wet nursing was rarely considered.
“In my culture is not accepted, for me to give the baby to nursing mother to breastfeed.” Mother 9 (mother with twins on formula feeding) [sic]
“They will not agree [a family member to wet-nurse her baby]. My sisters have their own children so I don't think they will agree to breastfeed my baby.” Mother5
Even when mothers initially wished to breastfeed, they commonly felt they could not produce enough breastmilk to feed their children appropriately. This perception of breastmilk insufficiency was driven by cues like babies frequently crying, not falling asleep after BF, or not gaining weight as expected. As a solution, mothers' families provided unsuitable products for infant feeding that were available and affordable to them. Most families could not afford infant formula, so they often used sachets of powdered milk (“Cowbell” commercial name), or a porridge called “pap”.
“The breastmilk is not enough for the baby, because he is crying all the time, day and night, and I do not have money to buy infant formula, so I decided to buy Cowbell milk, which is the one that adults use.” Mother4
There was also a belief that breastmilk was not sufficient for the baby and that other supplements must be added, especially water, due to the extreme weather conditions (very hot and dry). In this setting of food insecurity, all CGs and HWs strongly believed that maternal nutrition critically influenced breastmilk production and its quality. This was the most commonly described issue among CGs and HWs and shaped BF beliefs, experiences, and support.
“When I gave birth, I didn't have enough breastmilk and the father didn't have money to supply food that can make the breast enough the children.” Mother 8 [sic]
“Sometimes you will go to an IDP camp, and you come across a mother and her children, eating some leaves, just only those leaves (…) You cannot say this mother is able to provide enough breastmilk for a baby.” Health promotor
CGs sensed that emotional stress affected breastmilk production and hampered BF, and HWs perceived that stress negatively affected mothers' ability to breastfeed. Participants often verbalized how stress affected them as a result of conflict, displacement, and loss of livelihoods in the context of increasing poverty.
“I think what makes my breastmilk not flowing is emotional stress because I think a lot… I am thinking how can I breastfeed this baby till 6 months, how can I get food for the rest of the family.” Mother 2
“This Boko Haram crisis caused a lot of poverty and displacement of people from their homes. So, people that initially, maybe they are not rich, but they used to farm and provide to eat. Now, because of the displacement they live no longer in their villages, they don't have anything.” Clinical staff
From HWs' observations, breastmilk insufficiency was sometimes caused by inadequate BF practices in terms of positioning, latching, or frequency, even among multipara mothers. Mothers recognized their lack of knowledge of appropriate practices but did not identify this as a factor leading to breastmilk insufficiency.
“Some do have breastmilk, but the method and the way they position, or the way they latch the baby or the times they take to breastfeed are normally the issues.” Clinical staff
Another issue affecting BF was maternal medical conditions, including those affecting the breasts or the nipples. In some cases, mothers were discouraged from BF, for instance, when known to be HIV positive or presenting mastitis. When mothers had experienced previous neonatal or infant mortality, the death of the child is usually attributed to “poisonous” breastmilk, and normally mothers refused or were pushed to give up BF for further children. Most of the mothers interviewed were grand multipara. Some mothers felt their ability to BF changed over time, decreasing with older age and higher parity, since they were able to breastfeed their first children but experienced difficulties with later ones.
“They believe if they give their child the breastmilk, the child may end up dying. Because already they are told that the breastmilk is bad. We use to face this challenge. And it is very difficult to convince the mother that the milk has no problem.” Health promotor
There was a shared perception that infant feeding practices were slowly improving over time. This change was due to the exposure of mothers to encouragement about exclusive BF through the radio, during antenatal care, promotion by NGOs, or after hospital delivery. It was perceived that communities were generally open to BF promotion messaging, and some families were willing to follow recommended practices.
“Here in our community before we did not get the knowledge of breastfeeding babies only with breastmilk, so we breastfeed, we give water and also “pap” after 2 or 3 months. But now we have the knowledge of exclusive breastfeeding.” Grandfather
“They really understand and like the messages. Because there are some mothers that when they gave birth, I advised them about exclusive breastfeeding. And those mothers followed what I educate them, and they successfully breastfed their children until 6 months without giving water. And later they are appreciating… they never fed a child like this” Health promotor
HWs identified several mechanisms contributing to the uptake of recommended feeding practices. One was the inclusion of key community members and traditional healers, as well as an open invitation to health promotion talks, including elderly family members. Another was the identification of cases that serve as an example of the positive result of promoted practices, following the idea that, “seeing is believing”.
“Our people, they mostly believe in their traditional things. So that's why we used to include traditional healers and traditional birth attendants in our programs, so that we get more trust from the community.” Health promotor.
“I have a granddaughter who is living with me now, she has been fed only with breastmilk for the first 6 months. And from my observations, her health is different [better] from the other children who are fed with water, “pap” and breastmilk.” Grandfather (encouraging exclusive BF within his community)
The fear of infants getting infectious diseases or developing malnutrition also guided the change in feeding practice, as BF promotion messages emphasized the risks of infants who were not breastfed.
“They [at health facilities] are showing us pictures of malnourished babies as a result of giving formula and water for babies less than six… this led them to malnutrition and some other diseases (…) Everybody is afraid of disease, so that's why we decide to follow exclusive breastfeeding.” Mother 11
Although mothers may have accepted the recommended practices, they often lacked the practical skills, self-confidence, or support to adhere to them. In those situations, the perceptions of breastmilk insufficiency prevailed over general BF promotion messages.
“Giving the breastmilk only is the best way but most of the women are not able to produce enough breastmilk for the baby, so that's why we decided to introduce formula.” Mother 3 [sic]
“The best way to feed an under 6 months old baby is exclusive breastfeeding, but if the breast is not enough for the baby, I will introduce other milk for the baby, because the baby will be malnourished if the breastmilk is not enough.” Mother 10
The general strategy for health promotion within this MSF project included messaging on BF but it was not the main focus. HWs believed that general health messages did not always target the specific issues and multifactorial causes of lactation failure. HWs proposed several solutions to integrate BF support during health promotion activities more effectively. Proposed solutions included increasing the emphasis on BF physiology and practical skills, tailored messaging, and additional training for health promotors to enable them to provide this type of information and support.
“If we send general messages, I don't think we will be able to make the connection with the women. (…) I am not convinced that they receive the messages that they need to know how to increase the milk production. Because I am not sure how much is focused on the timelines, how often they should feed…” Clinical staff [sic]
CGs with infants <6 m normally came to the MSF nutrition project to seek care for malnourished or sick infants. On admission, most reported suboptimal feeding practices and complained of insufficient breast milk. However, their expectation was not to re-establish exclusive BF but to receive medical treatment for the infant, obtain free infant formula, or get a short medical treatment that could improve their breastmilk production.
“They don't get the full picture that there is no medical intervention. It's just to eat well, drink a lot of fluids, then keep breastfeeding, and then child will improve slowly (…) The point is to help them produce milk, so that we can discharge on breastmilk only. But maybe they don't understand the whole idea of double suckling to increase stimulation and all that.” Clinical staff [sic]
Before being admitted, CGs received explanations about the treatment, and they were also informed about a possible long length of stay. While feeling a bit overwhelmed by this change from initial expectations, staff clarifications, and reassurance helped them to adhere to treatment. Although CGs generally expressed their wish to stay admitted as long as needed to re-establish exclusive BF, they also raised concerns associated with a long stay. HWs pointed out that the duration of stay was a major problem in the care of infants <6 m. The willingness to stay decreased over time; as the health status of the infant improved, the CGs saw no reason to stay.
“The issue is I left my children with my neighbor and my husband has travelled (…). I would like my baby to feel better early so I am discharged and go home to take care of my own children.” Mother 1
“Once the child is still on medication, they are normally ok, there is a treatment going, so they are ok. But once the medication finishes, and then they are still staying, the child is not sick, he is not having anything, they feel like. ‘why are we still here?”'. Clinical staff [sic]
The mothers interviewed for this study were supported by their families, who encouraged them to stay and comply with the treatment at the ITFC. While many of their husbands were absent, they agreed for them to stay. However, HWs reported that this was not always the case. CGs sometimes felt distressed or powerless when admitted since they had left their family back home. Moreover, many CGs were emotionally unstable on arrival to the facility, given the vulnerability of the post-partum period, and the worries associated with infant feeding difficulties, sickness, or malnutrition.
“To think about home is something we can't stop it, but they [MSF staff] always advise us to reduce it, because if it becomes much, it will affect us and the baby.” Mother 7 [sic]
HWs perceived a certain reluctance from women to accept direct BF support from male staff, due to a lack of trust in talking about “female issues”. CGs did accept care from male staff, although it reflected the differences and barriers between men and women in this culture.
“The male and the female are different, so women feel more comfortable with the female staff than the male, and the male also sometimes doesn't feel comfortable because caregiver is a female, that's why there are feeling shy to come very close.” Mother 7 [sic]
“They won't say they disagree, but then you know, facial expression matters a lot. Some don't relax, they don't tend to feel comfortable when is a male trying to assist them. While others don't care whoever it is.” Clinical staff (male)
Acknowledging the numerous ethnic groups in the area, cultural differences between CGs and HWs—including the language barrier—also shaped the provision of BF support. When facing communication difficulties, HWs normally identified staff at the facility who could translate. Sometimes HWs felt frustrated and found it difficult to understand CGs' behaviors, practices, and decisions; this was a barrier to effectively engage with them.
“She would tell you that she is so worried, but yet she doesn't want to breastfeed. If you are too concerned about your child's illness, or his condition, at least breastfeed him, but she won't.” Clinical staff
While admitted, CGs demonstrated incorrect BF practices that sometimes the staff were not able to recognize (signs of ineffective suckling or BF only from one breast) or did not address for some time. From their viewpoint, this was due to a lack of time and knowledge. HWs reflected on possible solutions to improve staff capacities and practical BF support. They included the provision of practical, bedside training on different techniques. There was little engagement of nutritional assistants in direct BF support, so this could be addressed by training them for this purpose. Tools to assess BF practice and records of the progress could be better used to ensure a more systematic approach to BF support.
Despite initial expectations that were not met and the challenges in inpatient BF support, CGs gradually adapted to the routine at the facility and most accepted and complied with the recommendations to increase breastmilk production. The uptake of supplementary suckling technique was good overall and CGs and infants slowly demonstrated improved BF practice while hospitalized.
“It's strange for me to give the breast together with the tube for the baby, but I am not finding difficulties to do it.” Grandmother 1
“I think it really helped my baby because if I would use a cup for my baby, I think half of the milk will pour down. But by using the tube, the baby will take almost all the milk.” Mother 7
Different enablers contributed to this acceptance. The role of mental health counselors seemed crucial for BF support in this context. Their support was constantly required by other clinical staff, as they—as well as some health promotors—were the ones who were able to effectively encourage GCs to follow advice. They followed a culturally sensitive approach and supported women emotionally by listening to them, talking to them calmly, and encouraging them with positive examples.
“Maybe sometimes the doctor wants to do some important, but because of the refusal they have to stop (…) But if there's maybe a HP or counsellor to help them, they are very comfortable… What can you do? You cannot deny culture” Clinical staff
CGs also supported each other and encouraged other CGs to follow recommendations, after seeing the improvements with their infants.
“Caregivers also encourage themselves. Even when they are depressed and one says 'I don't have breastmilk', they use themselves as examples, to tell them 'When I came in, I didn't have milk, but due to the counseling, and the treatment doctors, nutrition assistants, the nurses, everybody… the support, and then the milk comes out.” Clinical staff
At the same time, BF support was included in the overall comprehensive treatment provided—rest, appropriate nutrition, and care for the infants—and mothers felt well treated and comfortable at the facility; this is an enabling environment to breastfeed. Above all, CGs saw improvements in infants' health and nutritional status, and also for themselves. All interviewed mothers felt grateful for the services provided and were willing to recommend the uptake of BF to other CGs.
“The women feel comfortable being at the ward and we use to sit down and have a chat, breastfeed our children… sometimes we are even with the staff” Mother 7
“When I was admitted I received a lot of support and guide from the staff. I feel comfortable with them and… there are meals, there are food, everything in the facility is ok. When I went back home my family were happy to see how I have changed.” Grandmother 3 [sic]
On admission, CGs are told that accepting BF support is part of the treatment process during hospitalization and that infant formula is not provided upon the mother's desire. HWs highlighted a lack of a straightforward solution for mothers not wishing to breastfeed. Yet, they thought that a more flexible approach to formula provision will cause an increase in formula feeding demand and consumption—and a subsequent increase in risks of artificial feeding. Infant formula in this context is an expensive product and HWs reported how some CGs obtained it for free then sold it to get money; this also happens with other therapeutic supplements given at the facility. HWs described a few scenarios that frequently lead to formula supply after BF support, such as wet nursing or multiple births. They perceived that there was a lack of unified criteria for formula provision in some cases, for example, when mothers were not achieving exclusive BF after a period of BF support.
“We know all the advantages of breastfeeding… we know that it's free, we know that it's hygienic. So I would rather improve our services [BF support] than to make infant formula a convenient option (…) I think there should be a clearly defined criteria when to switch to formula” Clinical staff [sic]
When discharged, infants were followed up weekly at ATFC until they recovered. Some CGs and HWs feared that BF practices would decrease or stop after discharge since CGs lacked access to appropriate food, staff encouragement, and support at home. Both CGs and HWs strongly believed that maternal nutrition was crucial for an adequate supply of breastmilk, something that was not often possible at home.
“For the purpose of their care in the facility, they will breastfeed, because we encourage them, and we do psycho-education… so they do it. But when they are being discharged home, and when they come up for follow-up, we find that the child has already stopped.” Clinical staff [sic]
“When I was in admission in the facility, they gave us food (…) so it helped the breast to start producing breastmilk. But immediately when I went back home because I can't afford to buy this kind of food and eat, the supply of the milk is going down.” Grandmother 3 (attending for follow-up at ATFC) [sic]
It was perceived that ATFC services, traditionally targeting only older children, were not including BF promotion or support during follow-up visits but were focused on following up on weight changes or general health status. HWs suggested that BF promotion and support should be included in a stronger community-based approach to ensure sustainability after the hospital interventions.
“When they come, we treat and then they go back, but there is still a gap, so it should be community-based (…) This is where we should start these cultural beliefs… If we don't do it, no matter what you do, they'll come back.” Clinical staff [sic]
The experiences and perspectives shared by participants portray a setting in which BF is practiced by most mothers, but the uptake of exclusive BF seems low. In a survey exploring infant feeding practices in Borno State, only 33% of caregivers reported having fed their children only with breastmilk for the first 6 months of life (37). Available reports suggest an increase in exclusive BF rates over time, as perceived by participants in this study (38–40).
This study exposes enabling and disabling factors for BF practice and support perceived by CGs and HWs in the studied context, which are summarized in Table 3. Yet, many of these perceived factors have also been identified in other humanitarian and low-middle-income settings and among mothers and infants globally (18, 41). While medical humanitarian organizations may not directly tackle structural barriers—such as household dynamics, traditional beliefs, displacement, and food insecurity—these factors should be recognized and addressed when developing strategies to promote and support BF. At the program level, BF promotion messages and support activities should be adapted to the common barriers to BF reported in this specific context. There is a need to strengthen HWs' capacities for lactation support while providing them with knowledge and skills to effectively counsel women so they can gain confidence in their ability to breastfeed despite being stressed or having poor nutrition. Staff training should also be enlarged to a wider range of healthcare roles, such as nutritional assistants or health promotors. Specific areas for improvement are mentioned throughout this discussion.
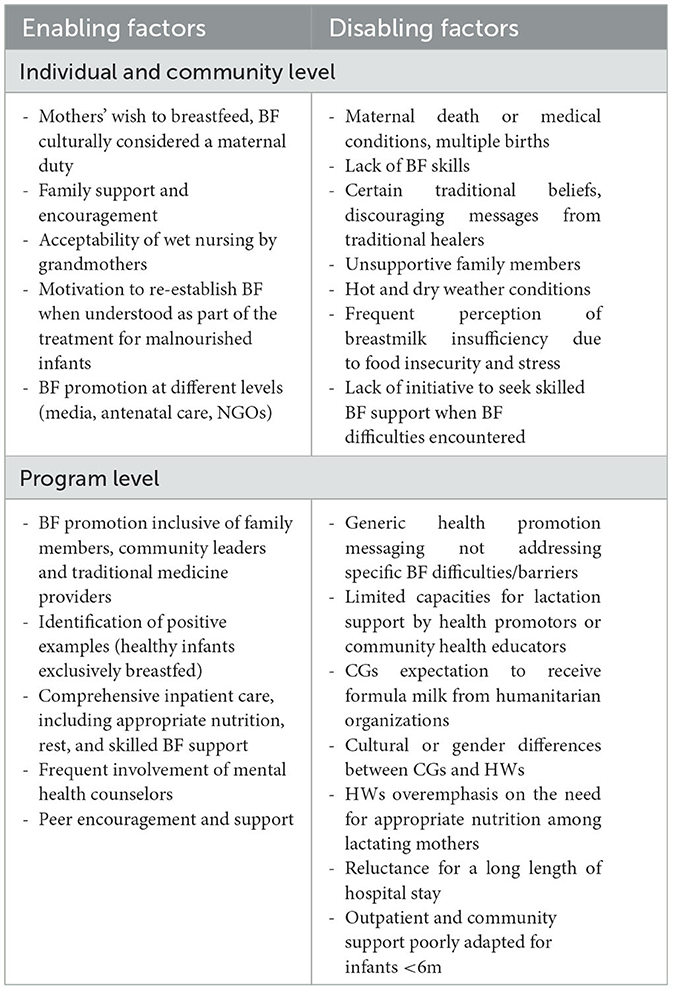
Table 3. Summary of perceived enabling and disabling factors for BF practice, promotion, and support.
Interviewed mothers were generally disempowered by infant feeding decisions or healthcare-seeking behaviors. This has been already shown in other studies looking at social norms in Borno state (42) or focusing on African cultures (43). This limitation of mothers' autonomy should be considered when providing BF messages and support, by involving key family members, when possible. In this setting, we found grandmothers who were willing to wet nurse accepted to be hospitalized with their grandchildren to receive inpatient BF support as part of the treatment for infant malnutrition. However, there was a perception that wet nurses seldom achieved exclusive BF despite support. Future studies should assess the outcomes of BF support among wet nurses, including infant nutritional recovery. Similarly, there is a need to increase staff capacities and explore strategies to provide enhanced support for wet nurses, acknowledging the high maternal mortality ratio observed in Nigeria and other humanitarian settings (44).
The conflict and displacement in Maiduguri have augmented the risk of acute malnutrition among infants and reduced dietary availability for mothers (2). Food insecurity can impact BF practice through various pathways. It can compromise maternal nutrition, not only affecting mothers' wellbeing but also leading to the perception of insufficient breastmilk and resulting in mixed feeding or premature cessation of BF. Additionally, food insecurity can induce stress or depression, often triggered by the inability to provide enough food for the family (45–49). Stress does not directly affect breast milk production. However, it can temporarily delay breastmilk release through reduced oxytocin secretion and reduced maternal self-confidence, as well as impact mother–infant behaviors (e.g., maternal anxious behavior subsequently increasing infants' irritability during feeds) (50–52). These mechanisms potentially affecting BF practice could be overcome when providing holistic support and reassurance. Offering mental and psychosocial support for lactating mothers is particularly relevant to promoting maternal wellbeing and protecting and enabling BF in humanitarian settings, where stressors likely increase (20, 53).
Generally, CGs thought reduced breastmilk production and flow were irreversible and felt powerless to change that situation. To reverse this perception, sensitive counseling can provide information and support to reinforce maternal self-efficacy and lead to improvements in BF (18). Messages should focus on the mechanisms of breastmilk production and how it can be increased (49). CGs and HWs should improve their understanding and management of certain infant behaviors, such as fussiness or crying, that often led to direct feeding supplementation and discontinuation of BF (54).
In this context, HWs strongly emphasize the importance to increase the intake of fluids and nutritious food for lactating mothers. It has been previously documented how these messages can undermine BF practice in contexts where mothers cannot reach the recommended intake (53). Up to now, there is not enough evidence suggesting the need to increase fluid intake beyond what lactating women require to meet their physiological needs (55). Breastmilk production and macronutrient composition seem to be little affected by maternal intake although maternal micronutrient deficiencies appear more reflected in breastmilk. In the case of severely malnourished mothers, BF can be extra challenged by energy depletion and the mother feeling unwell. While mothers can maintain lactation even when having a poor diet and nutritional status, more research is needed to investigate the extent of the influence of these factors on infant growth (56–59). Nonetheless, in resource-limited settings, exclusive BF likely remains the most complete and safe option for infants <6 m and should be strongly promoted and supported (60). The messages encouraging a healthy diet among lactating mothers should be delivered sensitively, in coherence with mothers' access to food, and coupled with maternal nutritional support when possible. At the same time, maternal nutritional status should be assessed and considered to better support mothers and infants.
The Operational Guidance for Infant Feeding in Emergencies outlines the limited circumstances when infant formula should be provided in emergencies (6). These recommendations arise with the purpose to protect mothers and infants from a wide distribution of formula, which may discourage mothers from re-establishing BF and undermine overall BF practice in the community (61, 62). However, as previously documented, the guidance is sometimes not understood or difficult to follow by those translating recommendations into practice. For instance, HWs may feel they are dismissing maternal autonomy or may hesitate to decide when BF support is considered ineffective and infant formula should be provided in those cases (8, 14). Staff training sessions should encourage discussions around the practical application of guidelines in a specific context, acknowledging HWs' dilemmas and experiences. Further research should also focus on identifying the best ways to support non-breastfed infants in emergencies.
Within this project, inpatient BF support worked effectively to help achieve partial and exclusive BF. CGs generally accepted the use of supplementary suckling techniques and the advice to stimulate BF (e.g., frequent suckling and bedding-in). The acceptability and outcomes of relactation support can vary widely among contexts (46, 63). The success in the studied setting was likely linked to peer support and the constant encouragement by HWs in a clinical setting where the use of supplementary suckling was well established. One of the main issues challenging BF support in the facility was the prolonged length of stay in some cases. This was also mentioned by CGs receiving relactation support in Kenya (46). As proposed by HWs, the feasibility and outcomes of outpatient support or intermittent admission—allowing mothers to go home for a few days and return to continue BF support—could be considered in this context. This study highlighted several reasons to consider a community-based approach for the management of malnourished infants <6 m. The Community Management of At-risk Mothers and Infants under 6 months of age (C-MAMI) care pathway, already supports and guides this approach, although its practical applicability and impact are being evaluated (64).
Several study limitations should be considered. Participant CGs had already accepted treatment at the facility. Hence, CGs who refused MSF treatment, who may have had different views, were not included in the sample. We recruited participants reachable at the facility or IDP camp during the limited data collection period, which did not allow interviewing other GCs (e.g., father and adolescent mother). A degree of social desirability bias must be considered in the answers recorded. HWs may have had a sense of performance evaluation that might have changed their opinions. CGs were receiving free care from MSF and were also offered an incentive for their participation in the study. This bias was mitigated by triangulating information from different sources, researchers' observations, and discussions among the research team in the field (65). Finally, the results of this study captured findings in a particular setting and time, so that they may not be generalizable to other contexts or more acute emergencies.
Since this operational research study aimed to create evidence-based practice, the authors disseminated the results among MSF field staff and managers in the Maiduguri project. It was hoped that this information would contribute to improving infant feeding support in this specific context (Supplementary material 2). These operational recommendations could be applied in other similar humanitarian contexts.
This study re-emphasizes that the practice of BF does not only depends on mothers' wishes, knowledge, and skills but it is strongly influenced by household and contextual factors. The perception of breastmilk insufficiency linked to poor maternal nutrition is one of the most common barriers to BF in this setting and should be particularly addressed during BF promotion and support. Within the studied project, BF support seems to contribute to improvements in BF practice, and it is positively valued by CGs, despite challenges and areas for improvement in HWs' capacities. A key factor enabling the acceptance of BF support was its integration as part of the comprehensive care provided to CGs and malnourished infants during admission. A greater focus should be placed on providing targeted support and follow-up for infants <6 m and their CGs in the community.
Data could be available upon reasonable request and with permission from Medecins Sans Frontiers. Requests to access the datasets should be directed to bmlldmVzLmFtYXQuY2FtYWNob0BraS5zZQ==.
The studies involving human participants were reviewed and approved by MSF Ethics Review Board (ID 2207) and the Borno State Health Research Ethics Committee, Nigeria (Approval No. 113/2022). The patients/participants provided their written informed consent to participate in this study.
NAC, EB, AC, TS, JVS, OK, and UP contributed to study design. HK, FH, AC, and CB supported data collection process. NAC collected and analyzed the data with contributions from AC, EB, UP, and TS. NAC drafted the first version of the article. All authors contributed to the discussion of results and read and approved the manuscript.
This study was funded by Medecins Sans Frontiers Brussels and Karolinska Institutet. The work of NA was sponsored by a scholarship granted by the University of Piemonte Orientale (UPO) as part of the International Doctoral Program in Global Health, Humanitarian Aid and Disaster Medicine.
The authors would like to acknowledge the contributions of Zara Bukar Dalama, Jean Claude Nzala, Hanne Beernaerts, and Alain Assumani, as well as other MSF colleagues who supported data collection in Maiduguri, and Tony Reid for language editing. The authors also thank all study participants, who generously contributed to the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1077068/full#supplementary-material
1. Gasseer NA, Dresden E, Keeney GB, Warren N. Status of women and infants in complex humanitarian emergencies. J Midwifery Women S Heal. (2004) 49:7–13. doi: 10.1016/j.jmwh.2004.05.001
2. Iacoella F, Tirivayi N. Child nutrition during conflict and displacement: evidence from areas affected by the Boko Haram insurgency in Nigeria. Public Health. (2020) 183:132–7. doi: 10.1016/j.puhe.2020.03.012
3. Lamberti LM, Walker CLF, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. (2011) 11:S15. doi: 10.1186/1471-2458-11-S3-S15
4. Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, et al. Optimal breastfeeding practices and infant and child mortality: A systematic review and meta-analysis. Acta Paediatrica Int J Paediatrics. (2015) 104:3–13. doi: 10.1111/apa.13147
5. Black RE, Allen LH, Bhutta ZA, Caulfield LE, Onis M de, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
6. IFE Core Group. Operational Guidance on Infant Feeding in Emergencies (OG-IFE) version 3.0. Emergency Nutrition Network; ENN Online. (2017). Available online at: https://www.ennonline.net/operationalguidance-v3-2017
7. World Health Organization. Updates on the Management of Severe Acute Malnutrition in Infants and Children. World Health Organization (2013).
8. Haidar MK, Farhat JB, Saim M, Morton N, Defourny I. Severe malnutrition in infants displaced from Mosul, Iraq. Lancet Global Heal. (2017) 5:e1188. doi: 10.1016/S2214-109X(17)30417-5
9. Dureab F, Al-Falahi E, Ismail O, Al-Marhali L, Jawaldeh AA, Nuri NN, et al. An overview on acute malnutrition and food insecurity among children during the conflict in Yemen. Children. (2019) 6:77. doi: 10.3390/children6060077
10. Grijalva-Eternod CS, Kerac M, McGrath M, Wilkinson C, Hirsch JC, Delchevalerie P, et al. Admission profile and discharge outcomes for infants aged less than 6 months admitted to inpatient therapeutic care in 10 countries. A secondary data analysis. Maternal Child Nutr. (2017) 13:3. doi: 10.1111/mcn.12345
11. Kerac M, James PT, McGrath MG, Brennan E, Opondo C, Frison S. Infant malnutrition in low- and middle-income countries: assessment and prevalence of small and nutritionally at-risk infants aged under 6 months in 54 Demographic & Health Survey datasets. Medrxiv. (2021) 12.23.21268306. doi: 10.1101/2021.12.23.21268306
12. Hwang CH, Iellamo A, Ververs M. Barriers and challenges of infant feeding in disasters in middle- and high-income countries. Int Breastfeed J. (2021) 16:62. doi: 10.1186/s13006-021-00398-w
13. Hirani SAA, Richter S, Salami BO, Vallianatos H. Breastfeeding in disaster relief camps. Adv Nurs Sci. (2019) 42:E1–12. doi: 10.1097/ANS.0000000000000231
14. Gribble KD, Palmquist AEL. ‘We make a mistake with shoes [that's no problem] but… not with baby milk': facilitators of good and poor practice in distribution of infant formula in the 2014–2016 refugee crisis in Europe. Maternal Child Nutr. (2021) 18:e13282. doi: 10.1111/mcn.13282
15. Almeida JM de, Luz S de AB, Ued F da V. Support of breastfeeding by health professionals: integrative review of the literature. Revista Paulista De Pediatria Engl Ed. (2015) 33:355–62. doi: 10.1016/j.rppede.2015.06.016
16. Rabbani A, Padhani ZA, Siddiqui FA, Das JK, Bhutta Z. Systematic review of infant and young child feeding practices in conflict areas: what the evidence advocates. BMJ Open. (2020) 10:e036757. doi: 10.1136/bmjopen-2020-036757
17. Dall'Oglio I, Marchetti F, Mascolo R, Amadio P, Gawronski O, Clemente M, et al. Breastfeeding protection, promotion, and support in humanitarian emergencies: a systematic review of literature. J Hum Lact. (2020) 36:687–98. doi: 10.1177/0890334419900151
18. Group IC, ENN, Aid, I. Operational Guidance: Breastfeeding Counselling in Emergencies. (2021). Available online at: https://www.ennonline.net/breastfeedingcounsellinginemergencies (accessed May 2, 2023).
19. Committee IR. Emergency Watchlist. (2022). Available online at: https://www.rescue.org/report/2022-emergency-watchlist?gclid=Cj0KCQjwhsmaBhCvARIsAIbEbH763Qbn4F6N1r7As3YF8NLFCxB_7alRzX_lZJgue9mMxhGWu1mfpNsaAlsLEALw_wcB (accessed May 2, 2023).
20. Unit IGS. Ipc Acute Malnutrition Analysis January – December 2022 [Internet]. (2022). Available online at: https://reliefweb.int/report/nigeria/nigeria-ipc-acute-food-insecurity-and-acute-malnutrition-analysis-january-december-2022-published-june-23-2022
21. Byrne D. A worked example of Braun and Clarke's approach to reflexive thematic analysis. Qual Quant. (2021) 2021:1–22. doi: 10.1007/s11135-021-01182-y
22. Campbell K, Orr E, Durepos P, Nguyen L, Li L, Whitmore C, et al. Reflexive thematic analysis for applied qualitative health research. Qual Rep. (2021) 26:6. doi: 10.46743/2160-3715/2021.5010
23. Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Heal. (2014) 9:26152. doi: 10.3402/qhw.v9.26152
24. Braun V, Clarke V. Thematic analysis. In:Association AP, , editor. APA Handbook of Research Methods in Psychology, Research Designs. Washington: American Psychological Association. (2012) p. 57–71. doi: 10.1037/13620-004
25. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
26. Amare M, Arndt C, Mahrt K, Mavrotas G. Polygynous family structure and child undernutrition in Nigeria. J Dev Stud. (2021) 57:1–22. doi: 10.1080/00220388.2021.1898591
27. Weller SC, Vickers B, Bernard HR, Blackburn AM, Borgatti S, Gravlee CC, et al. Open-ended interview questions and saturation. PLoS ONE. (2018) 13:e0198606. doi: 10.1371/journal.pone.0198606
28. Caretta MA. Situated knowledge in cross-cultural, cross-language research: a collaborative reflexive analysis of researcher, assistant and participant subjectivities. Qual Res. (2015) 15:489–505. doi: 10.1177/1468794114543404
29. Phillippi J, Lauderdale J, A. Guide to field notes for qualitative research: context and conversation. Qual Health Res. (2018) 28:381–8. doi: 10.1177/1049732317697102
30. Halcomb EJ, Davidson PM. Is verbatim transcription of interview data always necessary? Applied Nurs Res. (2006) 19:38–42. doi: 10.1016/j.apnr.2005.06.001
31. Neal JW, Neal ZP, VanDyke E, Kornbluh M. Expediting the analysis of qualitative data in evaluation: a procedure for the rapid identification of themes from audio recordings (RITA). Am J Evaluation. (2015) 36:118–32. doi: 10.1177/1098214014536601
32. Johnson GA, Vindrola-Padros C. Rapid qualitative research methods during complex health emergencies: a systematic review of the literature. Soc Sci Med. (2017) 189:63–75. doi: 10.1016/j.socscimed.2017.07.029
33. Vindrola-Padros C, Johnson GA. Rapid techniques in qualitative research: a critical review of the literature. Qual Health Res. (2020) 30:1596–604. doi: 10.1177/1049732320921835
34. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
35. Tessier S. From field notes, to transcripts, to tape recordings: evolution or combination? Int J Qual Meth. (2012) 11:446–60. doi: 10.1177/160940691201100410
36. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Meth. (2017) 16:1609406917733847. doi: 10.1177/1609406917733847
37. FHI. Borno State Health, WASH & Nutrition KAP Survey Report. Integrated Humanitarian Assistance to North-East Nigeria Project. Family Health International (2018). Available online at: https://reliefweb.int/report/nigeria/borno-state-health-wash-nutrition-kap-survey-report-integrated-humanitarian (accessed May 2, 2023).
38. Save The Children. Maternal and Young Child Feeding, WASH and Child Protection KAP Survey Report: Jere, Konduga, Mafa, and MMC. Save the Children (2020). Available online at: https://www.humanitarianresponse.info/fr/operations/nigeria/assessment/maternal-and-young-child-feeding-wash-and-child-protection-kap-survey (accessed May 2, 2023).
39. Benova L, Siddiqi M, Abejirinde IOO, Badejo O. Time trends and determinants of breastfeeding practices among adolescents and young women in Nigeria, 2003–2018. BMJ Global Heal. (2020) 5:e002516. doi: 10.1136/bmjgh-2020-002516
40. Onubogu CU, Onyeka IN, Esangbedo DO, Ndiokwelu C, Okolo SN, Ngwu EK, et al. Changes in breastfeeding and nutritional status of Nigerian children between 1990 and 2008, and variations by region, area of residence and maternal education and occupation. Paediatr Int Child H. (2016) 36:248–59. doi: 10.1179/2046905515Y.0000000048
41. Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. (2016) 387:491–504. doi: 10.1016/S0140-6736(15)01044-2
42. Nigeria Learning Collaborative. Borno State Snapshot: Social Norms Women's Economic Empowerment in Nigeria. (2021). Available online at: https://www.alignplatform.org/resources/borno-state-snapshot-social-norms-and-womens-economic-empowerment-nigeria (accessed May 2, 2023).
43. Oyelana O, Kamanzi J, Richter S, A. critical look at exclusive breastfeeding in Africa: through the lens of diffusion of innovation theory. Int J Afr Nurs Sci. (2020) 14:100267. doi: 10.1016/j.ijans.2020.100267
44. UNFPA. Maternal Mortality In Humanitarian Crises And In Fragile Settings. (2015). Available online at https://www.unfpa.org/sites/default/files/resource-pdf/MMR_in_humanitarian_settings-final4_0.pdf (accessed May 2, 2023).
45. Webb-Girard A, Cherobon A, Mbugua S, Kamau-Mbuthia E, Amin A, Sellen DW. Food insecurity is associated with attitudes towards exclusive breastfeeding among women in urban Kenya. Maternal Child Nutr. (2012) 8:199–214. doi: 10.1111/j.1740-8709.2010.00272.x
46. Kahindi J, Jones C, Berkley JA, Mwangome M. Establishing exclusive breastfeeding among in-patient malnourished infants in a rural Kenyan hospital: mothers' experiences of a peer supporter intervention. Int Breastfeed J. (2020) 15:40. doi: 10.1186/s13006-020-00278-9
47. Gatti L. Maternal perceptions of insufficient milk supplyin breastfeeding. J Nurs Scholarship. (2008) 4:40. doi: 10.1111/j.1547-5069.2008.00234.x
48. Huang Y, Liu Y, Yu X, Zeng T. The rates and factors of perceived insufficient milk supply: a systematic review. Maternal Child Nutr. (2021) 18:e13255. doi: 10.1111/mcn.13255
49. Piccolo O, Kinshella MLW, Salimu S, Vidler M, Banda M, Dube Q, et al. Healthcare worker perspectives on mother's insufficient milk supply in Malawi. Int Breastfeed J. (2022) 17:14. doi: 10.1186/s13006-022-00460-1
50. UvnäsMoberg K, Ekström-Bergström A, Buckley S, Massarotti C, Pajalic Z, Luegmair K, et al. Maternal plasma levels of oxytocin during breastfeeding—a systematic review. PLoS One. (2020) 15:e0235806. doi: 10.1371/journal.pone.0235806
51. Walter MH, Abele H, Plappert CF. The role of oxytocin and the effect of stress during childbirth: neurobiological basics and implications for mother and child. Front Endocrinol. (2021) 12:742236. doi: 10.3389/fendo.2021.742236
52. Nagel EM, Howland MA, Pando C, Stang J, Mason SM, Fields DA, et al. Maternal psychological distress and lactation and breastfeeding outcomes: a narrative review. Clin Ther. (2022) 44:215–27. doi: 10.1016/j.clinthera.2021.11.007
54. Segura-Pérez S, Richter L, Rhodes EC, Hromi-Fiedler A, Vilar-Compte M, Adnew M, et al. Risk factors for self-reported insufficient milk during the first 6 months of life: A systematic review. Maternal Child Nutr. (2022) 2022:e13353. doi: 10.1111/mcn.13353
55. Ndikom CM, Fawole B, Ilesanmi RE. Extra fluids for breastfeeding mothers for increasing milk production. Cochrane Db Syst Rev. (2014) (6):CD008758. doi: 10.1002/14651858.CD008758.pub2
56. Daniel AI, Shama S, Ismail S, Bourdon C, Kiss A, Mwangome M, et al. Maternal BMI is positively associated with human milk fat: a systematic review and meta-regression analysis. Am J Clin Nutrition. (2021) 113:1009–22. doi: 10.1093/ajcn/nqaa410
57. Bravi F, Wiens F, Decarli A, Pont AD, Agostoni C, Ferraroni M. Impact of maternal nutrition on breast-milk composition: a systematic review. Am J Clin Nutrition. (2016) 104:646–62. doi: 10.3945/ajcn.115.120881
58. Samuel TM, Zhou Q, Giuffrida F, Munblit D, Verhasselt V, Thakkar SK. Nutritional and non-nutritional composition of human milk is modulated by maternal, infant, and methodological factors. Frontiers Nutrition. (2020) 7:576133. doi: 10.3389/fnut.2020.576133
59. Dror DK, Allen LH. Overview of nutrients in human milk. Adv Nutr. (2018) 9:278S-294S. doi: 10.1093/advances/nmy022
60. World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organization (2009).
61. Gribble K, Fernandes C. Considerations regarding the use of infant formula products in infant and young child feeding in emergencies (IYCF-E) programs. World Nutr. (2018) 9:261–83. doi: 10.26596/wn.201893261-283
62. Gribble KD, McGrath M, MacLaine A, Lhotska L. Supporting breastfeeding in emergencies: protecting women's reproductive rights and maternal and infant health. Disasters. (2011) 35:720–38. doi: 10.1111/j.1467-7717.2011.01239.x
63. Camacho NA, Schreeb J, Corte FD, Kolokotroni O. Interventions to support the re-establishment of breastfeeding and their application in humanitarian settings: a systematic review. Maternal Child Nutrition. (2023) 19:e13440. doi: 10.1111/mcn.13440
64. Network EN. MAMI Care Pathway Package, Version 3. (2021). Available online at: https://www.ennonline.net/mamicarepathway
Keywords: breastfeeding support, infant malnutrition, humanitarian settings, breastfeeding, North-East Nigeria
Citation: Amat Camacho N, Chara A, Briskin E, Pellecchia U, Kyi HA, de Rubeis ML, Hussain F, Ahmed T, Ogundipe OF, Burzio C, Kamis U, Bukar LM, Von Schreeb J, Kolokotroni O, Della Corte F and Sunyoto T (2023) Promoting and supporting breastfeeding in a protracted emergency setting—Caregivers' and health workers' perceptions from North-East Nigeria. Front. Public Health 11:1077068. doi: 10.3389/fpubh.2023.1077068
Received: 28 October 2022; Accepted: 09 May 2023;
Published: 02 June 2023.
Edited by:
Mary A. Uyoga, North-West University, South AfricaReviewed by:
Solina Richter, University of Saskatchewan, CanadaCopyright © 2023 Amat Camacho, Chara, Briskin, Pellecchia, Kyi, de Rubeis, Hussain, Ahmed, Ogundipe, Burzio, Kamis, Bukar, Von Schreeb, Kolokotroni, Della Corte and Sunyoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nieves Amat Camacho, bmlldmVzLmFtYXQuY2FtYWNob0BraS5zZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.