- 1College of Medicine, University of Arkansas for Medical Sciences Northwest, Springdale, AR, United States
- 2Office of Community Health and Research, University of Arkansas for Medical Sciences Northwest, Springdale, AR, United States
- 3Iakwe Home Health LLC, Honolulu, HI, United States
Introduction: Striking health disparities exist in the Republic of the Marshall Islands (RMI). The RMI has one of the highest age-adjusted type 2 diabetes mellitus (T2DM) rates in the world (23.0%) compared to global (9.3%) and United States (US; 13.3%) rates. We conducted health screenings including clinical indicators of T2DM and hypertension among Marshallese in the RMI.
Methods: Screenings were conducted at 20 churches on Majuro Atoll. Participants completed questionnaires and biometric data collection assessing glycated hemoglobin (HbA1c), blood pressure, and body mass index.
Results: Screenings included 528 participants and showed a high prevalence of T2DM, obesity, and hypertension. One-third of participants were referred to the non-communicable disease clinic. The percent of adults in this study with T2DM-indicative HbA1c (48.5%) is higher than observed at the national level (23.0%).
Discussion: Results highlight the need for non-communicable disease-related programs in the RMI.
Introduction
The Republic of the Marshall Islands (RMI) is part of the United States (US) Affiliated Pacific Islands (USAPI) through a Compact of Free Association (COFA) (1). The RMI is made up of 29 atolls and five isolated islands in the North Pacific Ocean, about halfway between Hawaii and Australia, with a population of ~80,000 (2). Although research in the RMI is limited, the available data demonstrates striking health disparities including a high rate of type 2 diabetes mellitus (T2DM) (3–6). The International Diabetes Foundation has ranked the RMI with one of the highest age-adjusted T2DM rates in the world (23.0%) (7) compared to lower rates in the US (13.3%) and globally (9.3%) (7, 8).
Health disparities in the RMI are linked to historical trauma experienced by Marshallese, resulting from testing of nuclear weapons on the atolls by the US (9, 10). Between 1946 and 1958, the US military tested numerous nuclear weapons, resulting in the exposure of Marshallese to significant levels of radiation (9, 10). Due to the contamination of the RMI from nuclear testing, the Marshallese transitioned from a diet sourced through local farming and fishing to a diet reliant on highly processed commodity foods imported from the continental US and a more sedentary lifestyle (9–13). Further, American scientists conducted research on the Marshallese people in an attempt to understand the effects of nuclear fallout; however, this research was conducted without consideration of language differences or informed consent, creating distrust in outside researchers (9, 10).
The long-term objective of the study team is to understand and address the epidemic of T2DM in the RMI in collaboration with the Ministry of Health and non-governmental organizations in the RMI. The purpose of this study was to conduct health screenings as part of a needs assessment that included clinical health indicators of T2DM and hypertension among Marshallese living in the RMI, as well as diabetes self-management knowledge and behaviors for Marshallese previously diagnosed with T2DM. The main aims of the health screenings were to: (1) conduct a needs assessment to understand the current prevalence and severity of T2DM in faith-based organizations in the RMI; and (2) identify the barriers to T2DM treatment and self-management in the RMI. The findings from the health screenings will be utilized to inform future T2DM and other non-communicable disease related programs in the RMI. Health counseling was provided to all participants, and referrals to health care providers were arranged for those participants with screening results out of the normal/healthy range.
Study design
Community-based participatory research
This study utilized a community-based participatory research (CBPR) approach, which promotes equitable and ethical research (14–17). The use of a CBPR approach is important given the historical trauma experienced by the Marshallese people, including the nuclear weapons testing conducted in the RMI by the US military and the resulting unethical research on Marshallese exposed to nuclear fallout (9). CBPR engages community partners, honors their unique contributions at all stages of research, and ensures Marshallese cultural knowledge informs the process (18).
Community partners
A community advisory board that included seven members from our community partners in the RMI led the assessment. Community partners included the RMI Ministry of Health and Human Services (MOHHS), the Marshallese Educational Initiative (MEI), and Kora In Jiban Lolorjake Ejmour (KIJLE; approximately translated to “Women for Health”). The MOHHS has been designated by the RMI's Constitution as the state health agency and is vital to researchers appropriately implementing research activities in the RMI (19). The study team has built a strong working relationship with MOHHS and has full time staff with a dedicated office space in MOHHS. MOHHS worked closely with the study team to develop the study protocol and received weekly updates on study activities and progress. The study team collaborated with the MOHHS non-communicable disease (NCD) team to provide counseling at each screening event for all participants. Participants who needed further care were referred to the NCD clinic with scheduled appointments provided by NCD providers at screening events.
MEI is a non-profit organization that promotes cultural, intellectual, and historical awareness of the Marshallese people; MEI is headquartered in Springdale, Arkansas with outreach in the RMI. KIJLE is a non-profit women's group, which collaborates with the MOHHS to engage the community in public health initiatives. KIJLE is important to maintaining cultural congruence during implementation as they represent the matriarchal leadership of the RMI.
Study setting
The study was conducted in 20 churches located on Majuro Atoll. Churches play an important role in Marshallese culture; prior needs assessments in Arkansas have shown that 96.5% of Marshallese adults report regular church attendance (20). Most of the health screenings were done inside the church buildings; however, due to limited room at some locations, a few set up the health screenings at an outside location. In all cases, the study team arranged the counseling tables away from the general screening area for privacy. The study team worked with the churches to ensure rooms were available for glycated hemoglobin (HbA1c) testing to ensure the testing kits could remain temperature controlled.
Study team
The study team was comprised of the principal investigator and several co-investigators who have prior experience conducting research studies with Marshallese participants in the US and the RMI. The study manager has 15 years of community health and research experience and is a native of the RMI. The study manager previously relocated to the RMI and was responsible for the management of all local community health workers (CHWs) who served as research staff during this study. Local CHWs and research staff completed Collaborative Institutional Training Initiative Human Subjects research training, training on Health Insurance Portability and Accountability Act of 1996 privacy requirements, blood borne pathogen safety training, trainings in biometric data collection, and study-specific trainings. At least six data collectors and one MOHHS NCD provider were present at every data collection event.
Church and participant recruitment
CHWs and community advisory board members assisted with recruiting churches to participate in the health screenings. Additional recruitment efforts included announcements on the local radio station, through text messaging, and through invitations extended to non-participating churches who inquired about participation after hearing of the health screenings taking place elsewhere. When a church was identified as being interested in participating, the study team would meet with the pastors face-to-face to present information about the needs assessment and its recruitment goals. Once a church agreed to participate, town hall style question and answer sessions were used to inform and recruit individual participants. Additionally, the health screenings were advertised via postings on local websites, social media, and study flyers. Potential participants were advised of the time commitment involved in the health screening and were invited to participate in other scheduled screenings if they were unable to stay for the full screening event.
Eligibility determination
The study team captured biometric and survey data on individuals who met the inclusion criteria and consented to participate in the study. Participant inclusion criteria included: (1) self-identified as Marshallese and (2) over 18 years of age.
Consent
Previous research with the Marshallese community has highlighted Marshallese participants' desire for a simplified consent process and the preference for verbal discussion of study requirements (21). Therefore, as the health screenings were considered a minimal risk study, a waiver of consent documentation was requested and granted by the University of Arkansas for Medical Sciences Institutional Review Board (IRB #262557). The study information sheet was provided to participants in Marshallese, and plain language was used to increase understanding. Participants were allowed time to read or have a CHW read the information sheet to them. Participants were encouraged to ask any questions they may have had. All participants received a paper version of the study information sheet in Marshallese for their records. Participants verbally acknowledged consent prior to data collection.
Remuneration
Remuneration was provided to all participants who consented to take part in the study. Participants were given $10 as compensation for their participation. Individuals who wanted to receive a health screening but declined the opportunity to participate in the study were provided a screening free of charge but did not receive compensation.
Methods and analysis
Data collection
All data collection staff had previous experience collecting biometric and survey data in the RMI. REDCap was utilized to store and manage data (22). To prevent/minimize missing data, REDCap includes a missing data report in the Quality Assurance tool which allowed for convenient quality assurance validation and monitoring, as well as prompt collection of missing data. All of the instruments used in the study were chosen collaboratively with Marshallese stakeholders and have been translated into Marshallese and validated with Marshallese participants. The research team has used these same questions with more than 1,000 Marshallese participants in multiple studies (23, 24).
Biometric data
The biometric data collection was completed by qualified, trained research staff and was carried out using standard infection, prevention, and control practices. Waste was disposed of in a safe manner in accordance with MOHHS instructions. Biometric measures collected included HbA1c, weight, height, and blood pressure. HbA1c was collected via finger prick using aseptic techniques and analyzed using PTS Diagnostic's A1CNOW+ point-of-care HbA1c tests. Participants' weight (without shoes) was measured to the nearest 0.5 pound using a calibrated digital scale. Height (without shoes) was measured to the nearest 0.25 inch using a stadiometer. Body mass index (BMI) was calculated using collected height and weight [(weight in pounds*703)/(height in inches2)]. Systolic and diastolic blood pressure was measured using a digital blood pressure device with the participant seated, arm elevated, and cuff placed at approximately heart height. Categorical blood pressure (normal, pre-hypertension, stage 1 hypertension, and stage 2 hypertension) were informed by the American Heart Association standards (25). Pulse pressure was calculated by subtracting the diastolic from the systolic blood pressure value (26). All individuals who participated in the health screening received a paper copy of their biometric results.
Survey data
After consent was provided, participants took a short 10-min survey before or after the health screening. The survey instrument included questions adapted from the Behavioral Risk Factor Surveillance System (BRFSS) survey (27). All survey documents were translated into Marshallese and were self-administered or interviewer-administered, depending on the preference and/or literacy level of the participant. Due to past findings from research with Marshallese communities in the RMI and Arkansas, the length of the survey was reduced from prior studies to ensure accurate responses and to reduce participant burden.
Analysis
Descriptive statistics, including means and standard deviations for continuous variables and frequency and percentages for categorical variables, are used to report the results of the health screenings. Descriptive statistics are provided for demographic and biometric data. The analysis was completed using STATA 17 (28).
Results
Sample
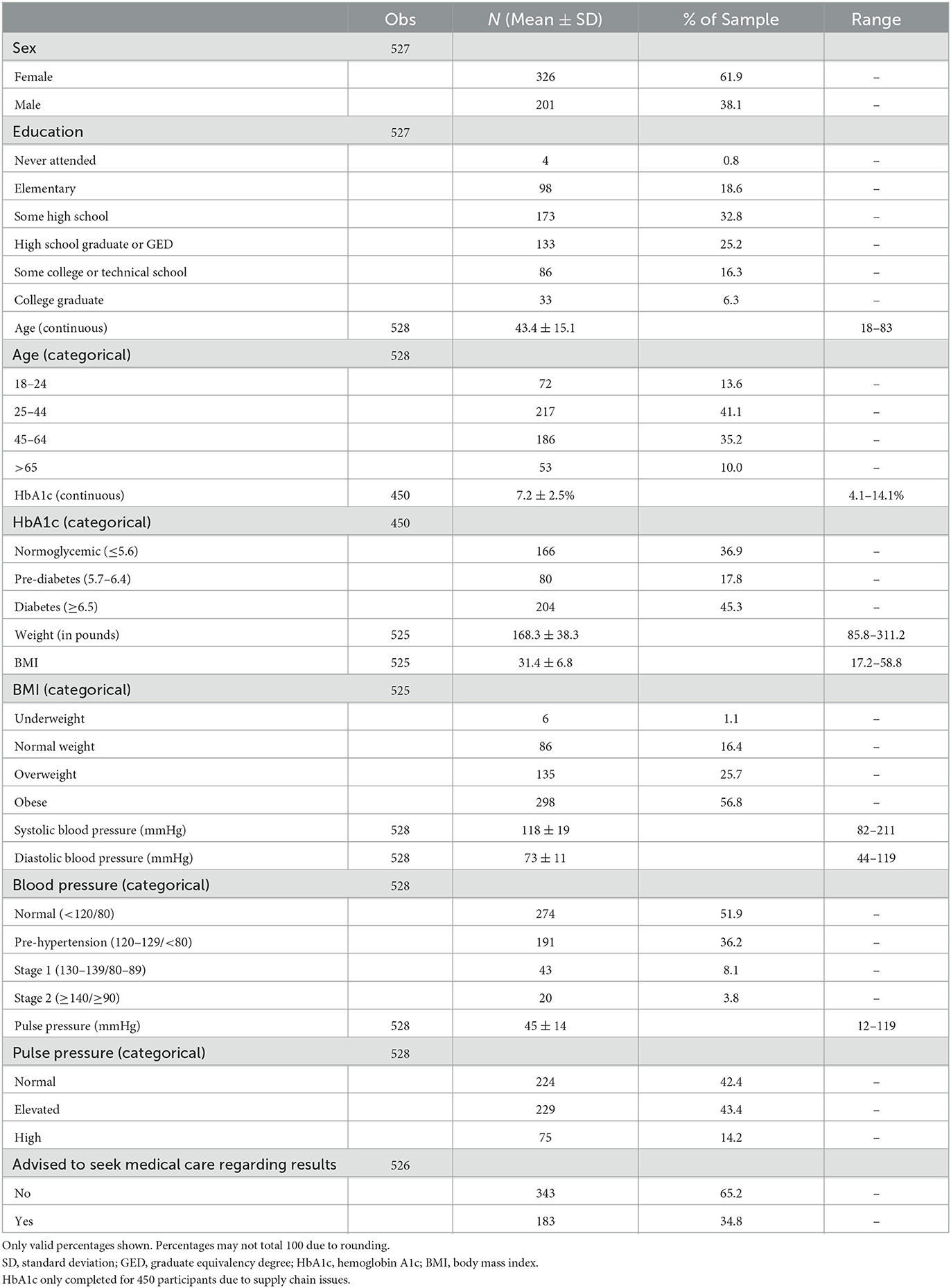
Five hundred and twenty eight (528) Marshallese adults participated in the health screenings. Due to issues and delays with the supply chain (in some cases, supplies took more than a month to arrive from the US with unreliable tracking data), only 450 participants were able to have their HbA1c tested during the screenings. Table 1 presents the demographics of the sample and the results of the health screenings.
Demographics
The sample was predominately female (61.9%) with a mean age of 43.4 years (± 15.1 years). Just over one-third (35.2%) of the participants were between the ages of 45 and 64. The majority of participants either had some high school education (32.8%) or were a high school graduate (25.2%).
Biometrics
HbA1c
The mean HbA1c of the sample was 7.2% (± 2.5%). The majority of the sample had an HbA1c indicative of glucose dysregulation; 17.8% had an HbA1c indicating prediabetes (5.7–6.4%) and 45.3% had an HbA1c indicating diabetes (≥6.5%).
Weight and BMI
The mean weight of the sample was 168.3 lbs. (± 38.3 lbs.), and the mean BMI was 31.4 ± 6.8. The majority of participants were either overweight (25.7%) or obese (56.8%).
Blood pressure and pulse pressure
The sample had a mean systolic blood pressure of 118 mmHg (± 19 mmHg) and a mean diastolic blood pressure of 73 mmHg (± 11 mmHg). Just over a third (36.2%) had blood pressure indicative of prehypertension, 8.1% had blood pressure indicative of stage 1 hypertension, and 3.8% had blood pressure indicative of stage 2 hypertension.
The mean pulse pressure of the sample was 45 mmHg (± 14 mmHg). Forty-three (43.4%) percent had an elevated pulse pressure (40–49 mmHg), and 14.2% had a high pulse pressure (≥50 mmHg).
Referrals to medical care
Over a third (34.8%) of participants were referred to the NCD clinic with scheduled appointments with a health care provider.
Dissemination plan
Throughout previous work with the Marshallese community, the study team has found that individual in-person meetings, as well as church meetings, town hall meetings, using infographics, and using plain language summaries, are the culturally preferred methods for dissemination of study results (29). Individual participant results were shared with participants during the diabetes health screening events.
Study staff will provide a summary of the results back to the Marshallese community utilizing existing community partnerships. Culturally and linguistically appropriate infographics and summaries will be created and used as flyers and posters to be distributed or displayed at community events. Flyers and/or posters will also be available in a digital format for posting on Facebook or other social media platforms.
To ensure participant confidentiality is maintained, aggregated de-identified results will be shared with the congregations at participating churches. Aggregated de-identified results may also be shared in town hall style events hosted by community partners; town hall meetings will be announced through social media, newspaper, and radio. A summary of the results will be provided in a formal report and presentation to the RMI MOHHS. Additionally, results of this study will be used for academic presentations, posters, or publications.
Discussion
In this study, Marshallese adults from 20 churches on Majuro Atoll in the RMI were invited to participate in diabetes health screenings. This report describes the recruitment strategies and study protocol and provides the results of the biometric data. The data from our study will inform our future research addressing health disparities in the RMI, especially those related to cardiometabolic diseases including diabetes and hypertension.
The results of the screenings show a high prevalence of diabetes, obesity, and hypertension among the participants in the study. The percent of screened adults with an HbA1c indicative of diabetes in this study (45.3%) is even higher than the diabetes prevalence observed at the national level (23.0%) (7). This is also higher than the proportion found in similar health screenings for Marshallese adults conducted in northwest Arkansas (38.4%) (24). These results provide evidence of the health disparities faced by the Marshallese living in the RMI and highlight the need for further diabetes and other non-communicable disease-related programs in the RMI. Although the rate of non-communicable disease among the participants in the health screening study was high, we were able to assist over 180 people in setting up appointments with non-communicable disease providers.
Historical trauma experienced by Marshallese, resulting from testing of nuclear weapons on the atolls by the US, has long been linked to the health disparities the small island nation faces today (9, 10). Between 1946 and 1958, the US military tested numerous nuclear weapons, resulting in the exposure of Marshallese to significant levels of radiation (9, 10). Following these tests, American scientists conducted research on the Marshallese population in an attempt to understand the effects of nuclear fallout without any consideration of language differences or informed consent, creating distrust in outside researchers (9, 10). Given the long history between the US and the RMI, it is important for our research team to develop a trusting relationship with the Marshallese community.
In 2011, members of the research team became increasingly aware of the significant health disparities of the Marshallese community in northwest Arkansas and began meeting with Marshallese community members, Marshallese community organizations, and Marshallese churches with the goal of setting a community-driven research agenda using a CBPR approach (30). The research team conducted field work to gain a better understanding of Marshallese history and culture, and community members were invited to share their history, stories, and perspectives on health and research (30). Members of the Marshallese community were asked to join with the research team to review secondary data from the Census, Behavioral Risk Factor Surveillance System (BRFSS), Arkansas Department of Health Vital Records, and needs assessments conducted in 2004 and 2010 by the local hometown health coalition and community foundation (30). Through this work, Marshallese community members asked the research team to focus their efforts on addressing the high rates of T2DM in the community.
As part of developing the work on T2DM in Arkansas (later adapted for the RMI setting), the lead investigator brought together a diverse interprofessional research team and engaged 31 Marshallese community stakeholders, including patients, family members, and health care providers to select and adapt an appropriate intervention to address the high rates of T2DM with community support. The Marshallese stakeholders included patients with T2DM, family members of people with T2DM, and community health care providers. Representatives from Marshallese community-based organizations, the Marshallese Consulate, and Marshallese churches were included and represented patients, caregivers, and their organizations. Discussions were conducted both in English and in Marshallese and a bilingual translator provided interpretation. The use of the Marshallese language increased comfort and shifted the power of gaining knowledge and sharing information to the Marshallese stakeholders. Using the native language was important both to the research team and to the Marshallese stakeholders given the historical trauma experienced by Marshallese people and the distrust in American scientists it created. Further, as part of our efforts to build trust with the Marshallese community in Arkansas, we included a native Marshallese physician, Marshallese nurses, and additional Marshallese staff as part of the research team. At the urging of the Arkansas-based Marshallese stakeholders, we have worked diligently to bring our efforts to address T2DM to the RMI. Overall, because of the long-standing relationship with, and support from, the Marshallese community in Arkansas, Marshallese community organizations, and the RMI MOHHS, we have been able to successfully adapt our studies and health screenings to benefit Marshallese living in the RMI; without the support and involvement of Marshallese people, these efforts would not be possible. These relationships have been, and will continue to be, a vital part of our work with the Marshallese community in the US and the RMI; this study is one of several our research team has conducted in partnership with Marshallese communities in the US and the RMI dating back to the original conversations in 2011 (24, 30–37).
The health screening study was instrumental in highlighting the barriers to study administration in the RMI. Biometric data collection was not without its difficulties. Due to issues and delays with the supply chain (in some cases, supplies took more than a month to arrive with unreliable tracking data), only 450 participants were able to have their glycated HbA1c tested during the screenings. Maintaining the correct temperature for the A1CNOW+ test kits was difficult in churches without air conditioning, and special care was needed to ensure ice packs and coolers were available as needed to maintain the test equipment. Electricity was not always reliable, which limits the potential screening equipment that can be utilized during studies. Further, although churches play an important role in Marshallese life, there are limitations given the sheer number of events and activities that utilize these spaces. The study team did encounter some difficulties with utilizing churches for data collection. On occasion, the start time of the health screenings were delayed or ultimately rescheduled due to needing to have the buildings unlocked or due to another event taking place at the church.
There are limitations to consider when interpreting the findings. The convenience sample limits the ability to generalize the results, and due to a lack of community-level data, no direct comparisons of the study sample can be made to the general population of Marshallese living in the RMI or abroad. The sampling method also limits comparisons to other studies. Moreover, some participants in the screenings may have been aware of potential health conditions and, therefore, may have been more likely to agree to participate in the study. Finally, we recognize BMI is a problematic measure. Marshallese participants are often uncomfortable with having research staff measure their waist and/or hip circumference, which limits the options of determining weight-related risk factors.
Despite these limitations, we were able to provide health screenings to over 500 Marshallese adults. The aims of this study were 2-fold: (1) to conduct a needs assessment to understand the current prevalence and severity of diabetes within faith-based settings in the RMI and (2) to identify the barriers to T2DM treatment and self-management among members of faith-based organizations in the RMI. The data we have collected will help us to meet these aims and will position the research team and our community partners well to address the needs of Marshallese adults in the RMI.
Data availability statement
The deidentified data underlying the results presented in this study may be made available upon reasonable request from the corresponding author, PM, at cGFtY2VsZmlzaEB1YW1zLmVkdQ==.
Ethics statement
This study involving human participants was reviewed and approved by the University of Arkansas for Medical Sciences Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
JA, BR, and PM: study conception and design. JA, BR, GO'C, WB, and PM: data collection. JA, BR, PM, and PM-K: analysis and interpretation of results. JA, BR, GO'C, WB, SR, PM, and PM-K: draft manuscript preparation. All authors reviewed the results and approved the final version of the manuscript.
Funding
Community engagement efforts were supported by University of Arkansas for Medical Sciences Translational Research Institute funding awarded through the National Center for Advancing Translational Sciences of the National Institutes of Health [Grant Number: 1U54TR001629-01A1]. The health screening study was supported by an award from the Sturgis Foundation. JA was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number: KL2TR003108.
Acknowledgments
This study was made possible by a community-based participatory research partnership with local Marshallese faith-based leaders, the RMI Ministry of Health and Human Services, Kora In Jiban Lolorjake Ejmour (KIJLE), and the Marshallese Consulate General in Springdale, Arkansas.
Conflict of interest
PM-K was employed by Iakwe Home Health LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
BMI, body mass index; BRFSS, Behavioral Risk Factor Surveillance System; CBPR, community-based participatory research; CHW, community health worker; COFA, Compact of Free Association; HbA1c, glycated hemoglobin; IRB, Institutional Review Board; KIJLE, Kora In Jiban Lolorjake Ejmour; MEI, Marshallese Educational Initiative; MOHHS, RMI Ministry of Health and Human Services; NCD, non-communicable disease; RMI, Republic of the Marshall Islands; T2DM, type 2 diabetes mellitus; US, United States; USAPI, United States Affiliated Pacific Islands.
References
1. United, States Congress. Compact of Free Association Amendments Act of 2003. Washington, DC: U.S. Government Printing Office. Available online at: http://www.gpo.gov/fdsys/pkg/PLAW-108publ188/html/PLAW-108publ188.htm (accessed December 17, 2003).
2. Central, Intelligence Agency. The World Factbook: Australia-Oceania: Marshall Islands. Washington, DC: Office of Public Affairs. Available online at: https://www.cia.gov/library/publications/the-world-factbook/geos/rm.html (accessed June 2, 2020).
3. Ichiho H, Anson R, Keller E, Lippwe K, Aitaoto N. An assessment of non-communicable diseases, diabetes, and related risk factors in the Federated States of Micronesia, State of Pohnpei: A systems perspective. Hawaii J Med Public Health. (2013) 72:49–56.
4. Minegishi M, Fujimori K, Nakajima N, Watanabe M, Doi H, Otomo H, et al. Diabetes Mellitus and obesity among participants receiving screening for cancer in the Republic of the Marshall Islands. J Int Health. (2007) 22:133–41. doi: 10.11197/jaih.22.133
5. World Health Organization. Diabetes Fact Sheet. (2017). Available online at: http://www.who.int/news-room/fact-sheets/detail/diabetes (accessed August 09, 2018).
6. Hawley N, McGarvey S. Obesity and diabetes in Pacific Islanders: The current burden and the need for urgent action. Curr Diab Rep. (2015) 15:29. doi: 10.1007/s11892-015-0594-5
8. Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: U.S. Dept of Health and Human Services (2020).
9. Barker H. Bravo for the Marshallese: Regaining Control in a Post-Nuclear, Post-Colonial World. Belmont, CA: Cengage Learning (2012).
10. Guyer RL. Radioactivity and rights: Clashes at Bikini Atoll. Am J Public Health. (2001) 91:1371–6. doi: 10.2105/AJPH.91.9.1371
11. Pollock N. Health transitions, fast and nasty: Exposure to nuclear radiation. Pac Health Dialog. (2002) 9:275–82.
12. Ahlgren I, Yamada S, Wong A. Rising Oceans, Climate Change, Food Aid, and Human Rights in the Marshall Islands. Health and Human Rights. (2014) 16:69–80.
13. Gittelsohn J, Haberle H, Vastine A, Dyckman W, Palafox N. Macro- and microlevel processes affect food choice and nutritional status in the Republic of the Marshall Islands. J Nutr. (2003) 133:310S–3S. doi: 10.1093/jn/133.1.310S
14. Schensul JJ. Community, culture and sustainability in multilevel dynamic systems intervention science. Am J Community Psychol. (2009) 43:241–56. doi: 10.1007/s10464-009-9228-x
15. Schensul JJ, Trickett E. Introduction to multi-level community based culturally situated interventions. Am J Community Psychol. (2009) 43:232–40. doi: 10.1007/s10464-009-9238-8
16. Gorin SS, Badr H, Krebs P, Prabhu Das I. Multilevel interventions and racial/ethnic health disparities. J Natl Cancer Inst Monogr. (2012) 2012:100–11. doi: 10.1093/jncimonographs/lgs015
17. Trickett EJ. Multilevel community-based culturally situated interventions and community impact: An ecological perspective. Am J Community Psychol. (2009) 43:257–66. doi: 10.1007/s10464-009-9227-y
18. Minkler M, Wallerstein N. Community-Based Participartory Research for Health: From Process to Outcomes. San Francisco, CA: Jossey-Bass Publishers (2008).
19. Republic of the Marshall Islands Ministry of Health. 3 Year Rolling Strategic Plan October 2017- September 2019. Majuro, MH: Republic of Marshall Islands Ministry of Health (2017).
20. McElfish PA, Moore R, Laelan M, Ayers BL. Using CBPR to address health disparities with the Marshallese community in Arkansas. Ann Hum Biol. (2018) 45:264–71. doi: 10.1080/03014460.2018.1461927
21. Purvis R, Eisenberg L, Trudeau C, Long C, McElfish P. Facilitators, barriers, and recommendations related to the informed consent of Marshallese in a randomized control trial. Clin Ethics. (2020) 15:75–83. doi: 10.1177/1477750920903458
22. Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Infrom. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
23. McElfish PA, Andersen JA, Felix HC, Purvis RS, Rowland B, Scott AJ, et al. Relationship between sleep duration and quality and glycated hemoglobin, body mass index, and self-reported health in Marshallese adults. Sleep Health. (2021) 7:332–8. doi: 10.1016/j.sleh.2021.01.007
24. McElfish P, Rowland B, Long C, Hudson J, Piel M, Buron B, et al. Diabetes and hypertension in Marshallese adults: Results from faith-based health screenings. J Racial Ethn Health Disparities. (2017) 4:1042–50. doi: 10.1007/s40615-016-0308-y
25. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. (2018) 71:e13–115. doi: 10.1161/HYP.0000000000000065
26. Homan TD, Bordes S, Cichowski E. Physiology, Pulse Pressure. Treasure Island, FL: StatPearls Publishing. (2018).
27. Centers for Disease Control Prevention. 2019 BRFSS Questionnaire. (2019). Available online at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2019-BRFSS-Questionnaire-508.pdf (accessed May 05, 2021).
29. Purvis R, Long C, James L, Kimminau K, Riklon S, Carlton A, et al. Dissemination protocol for community-based participatory research partnerships with Marshallese Pacific Islanders in Arkansas. Progr Commun Health Partnersh. (2020) 2021:39. doi: 10.1353/cpr.2021.0039
30. McElfish P, Kohler P, Smith C, Warmack S, Buron B, Hudson J, et al. Community-driven research agenda to reduce health disparities. Clin Transl Sci. (2015) 8:690–5. doi: 10.1111/cts.12350
31. Andersen JA, Felix HC, Eswaran H, Payakachat N, Willis DE, Bogulski C, et al. Factors associated with first-time telehealth utilization for Marshallese living in the United States. Telemed Rep. (2021) 2:217–23. doi: 10.1089/tmr.2021.0023
32. Andersen JA, Felix H, Selig J, Rowland B, Bing W, Hudson J, et al. Feasibility and efficacy of a pilot family model of diabetes self-management intervention in the Republic of the Marshall Islands. Contemp Clin Trials Commun. (2021) 23:100824. doi: 10.1016/j.conctc.2021.100824
33. Andersen JA, Willis DE, Malhis JR, Long CR, McElfish PA. The association between education and basic needs insecurity for Marshallese during the COVID-19 pandemic. J Racial Ethnic Health Disparit. (2022) 9:1882–7. doi: 10.1007/s40615-021-01125-1
34. Felix H, Xiaocong L, Rowland B, Long C, Yeary K, McElfish P. Physical activity and diabetes-related health beliefs of Marshallese adults. Am J Health Behav. (2017) 41:553–60. doi: 10.5993/AJHB.41.5.4
35. Felix H, Rowland B, Long CR, Narcisse MR, Piel M, Goulden PA, et al. Diabetes self-care behaviors among Marshallese adults living in the United States. J Immigr Minor Health. (2018) 20:1500–7. doi: 10.1007/s10903-017-0683-4
36. Felix HC, Narcisse MR, Long CR, English E, Haggard-Duff L, Purvis RS, et al. The effect of family diabetes self-management education on self-care behaviors of Marshallese adults with type 2 diabetes. Am J Health Behav. (2019) 43:490–7. doi: 10.5993/AJHB.43.3.4
Keywords: Republic of the Marshall Islands, Native Hawaiian and Pacific Islanders, type 2 diabetes, hypertension, community-based participatory research, faith-based organizations
Citation: Andersen JA, Rowland B, O'Connor G, Bing WI, Riklon S, Mendoza-Kabua P and McElfish PA (2023) Faith-based health screenings for Marshallese adults living in the Republic of the Marshall Islands: Study design and results. Front. Public Health 11:1075763. doi: 10.3389/fpubh.2023.1075763
Received: 20 October 2022; Accepted: 06 March 2023;
Published: 28 March 2023.
Edited by:
Milton Eder, University of Minnesota Twin Cities, United StatesReviewed by:
Shanna N. McClain, National Aeronautics and Space Administration (NASA), United StatesRawiri Keenan, University of Waikato, New Zealand
Copyright © 2023 Andersen, Rowland, O'Connor, Bing, Riklon, Mendoza-Kabua and McElfish. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pearl A. McElfish, cGFtY2VsZmlzaEB1YW1zLmVkdQ==
 Jennifer A. Andersen1
Jennifer A. Andersen1 Pearl A. McElfish
Pearl A. McElfish