- 1Department of Physical Education, College of Education, Chonnam National University, Gwangju, Republic of Korea
- 2Department of Medical Education and Humanities, School of Medicine, Kyung Hee University, Seoul, Republic of Korea
- 3Preventive Medicine (AgeTech-Service Convergence Major), College of Medicine, Kyung Hee University, Seoul, Republic of Korea
Introduction: During the coronavirus disease 2019 (COVID-19) pandemic, many populations have experienced reduced physical activity (PA) levels, weight gain, and increased anxiety and depression. However, according to a previous study, engaging in PA has a positive effect on damages caused by COVID-19. Therefore, this study aimed to investigate the association between PA and COVID-19 using the National Health Insurance Sharing Service Database in South Korea.
Methods: Logistic regression analysis was used to analyze the association of PA with COVID-19 and mortality. The analysis was adjusted for body mass index, sex, age, insurance type, comorbidity, and region of residence at baseline. Disability and lifestyle (weight, smoking, and drinking status) were adjusted consecutively.
Results: The results indicated that engaging in insufficient PA as per the WHO guidelines predicts a higher risk of COVID-19 when controlling for personal characteristics, comorbidity, lifestyle, disability, and mortality.
Discussion: This study revealed the need to engage in PA and manage weight to reduce the risk of infection and mortality associated with COVID-19. Because engaging in PA is an important component of weight management and can help restore physical and mental health after the COVID-19 pandemic, it should be emphasized as a pillar of recovery after COVID-19.
1. Introduction
The novel coronavirus disease 2019 (COVID-19) has been a prominent global issue since its emergence in 2019. It is an infectious respiratory disease with mild-to-severe symptoms, which may include fever, cough, loss of taste or smell, and diarrhea (1, 2). However, in severe cases, chest pain, loss of speech, loss of mobility, and confusion may occur. COVID-19 is rapidly spread by respiratory droplets released during coughing, sneezing, speaking, singing, or breathing by the infected individual (3). Thus, the rapid spread of COVID-19 has caused an unprecedented number of cases and deaths. As of August 2022, there were over 593,236,266 confirmed cases and about 6,448,504 deaths worldwide (4). In South Korea, particularly, the fatality rate of older adults over 80 years old was 2.35% (5).
Recent studies show that COVID-19 has impacted mental health. There is evidence of increased severity of depression compared to those before pandemic (6, 7). It seems that quarantine throughout the COVID-19 pandemic negatively impacted the mental health of previously unaffected individuals; for example, the anxiety and depression of people whose family, colleagues, classmates, or neighbors were affected by quarantine were increased (8). In addition, the risks of anxiety, depression, stress, and sleep disorders in COVID-19 patients were increased (9). Post-traumatic stress symptoms were occasionally experienced after infection, but results concerning physical health were limited (10). However, it is unclear how factors relating to lifestyles are linked to the prognosis of COVID-19.
Engaging in physical activity (PA) has played an important role in improving psychological and physical health. It was found that engaging in regular moderate-to-vigorous PA (MVPA) is associated with reducing anxiety and negative self-perceptions, as well as improving physical health (11). In addition, engaging in MVPA is associated with losing and managing body weight that may predispose individuals to several types of chronic diseases, such as obesity and high blood pressure (12). However, a recent study shows that people spend more time engaging in sedentary behavior and less time engaging in PA than before the pandemic (13). Individuals engaging in PA is found to be more associated with lower risk of COVID-19 and mortality than those who do not meet the recommended PA level (150 min of MVPA at least once a week) (14, 15), although these results did not consider other factors of health such as personal characteristics, comorbidity, and disability level.
Thus, we aimed to examine the associations of MVPA with COVID-19 and mortality. To produce more robust study results, we tried to include controlling variables beyond MVPA, using nationally representative data.
2. Methods
2.1. Database
The National Health Insurance Service (NHIS) of South Korea is a social insurance system for the entire nation, and registration is compulsory; approximately 97% of the Korean population is currently registered (16). The NHIS assists people with scheduling medical checkups every 2 years and records their results automatically. These data include various information such as demographic information, payment specification, consultation statement, diagnosis statements, and prescriptions. With these records they developed the National Health Insurance Sharing Service for researcher to support various studies providing sample cohort DB, customized cohort DB, health screening cohort, etc.
This study used NHIS-COVID19 DB that included 4,363 adult COVID-19 patients in South Korea between January 1, 2020, and July 14, 2020, who had medical records between 2015 and 2018, the most recent data before the pandemic. We selected 67,125 adults for the control group in NHIS DB who also had medical checkup data. We used the most recent records in our study; the final data included COVID-19 status, demographic information, comorbidity, disability status, and lifestyle, including PA and body mass index (BMI). This study conformed to the Guidelines on De-identification of Personal Data of Korea and was approved by the Kyung Hee University's Institutional Review Board (IRB No. KHSIRB20-301[EA]) as a review exemption study. Thus, the requirement for informed consent was waived.
2.2. Variables
2.2.1. PA
PA was measured using a self-report questionnaire from NHIS. Moderate PA (MPA) was measured with the following question: “During the last week, how many times a week and for how many hours a day did you engage in physical activity at a moderate level for more than 10 min (e.g., fast walking, doubles tennis, riding bicycle, cleaning)?” Vigorous PA (VPA) was assessed with the following question: “During the last week, how many days a week and for how many hours a day did you engage in physical activity at a vigorous level for more than 10 min (e.g., running, aerobic, fast riding a bicycle)?” PA was categorized into two groups according to PA guidelines: 150 min of MVPA at least once a week (1 min of VPA = 2 min of MPA). The items have been widely used in the literature (17).
2.2.2. BMI
BMI is a simple obesity indicator calculated as weight/square of height (kg/m2). In this study, BMI was categorized into four groups according to the World Health Organization (WHO) BMI classification (underweight = BMI <18.5, normal range = 18.5 ≤ BMI <25, overweight = 25 ≤ BMI <30, obese = 30 ≤ BMI).
2.2.3. Covariates
We adjusted for sex, age, region of residence, economic status, the number of comorbidities, disability, smoking status, drinking status, and weight, which are reportedly associated with COVID-19 (18, 19). Residence was categorized into the five regions (Seoul, Daegu, Gyeonggi, Gyeong-buk, and other) of South Korea (from January 1, 2020 to August 14, 2020) with the most confirmed COVID-19 cases.
Economic status was measured using health insurance premiums. Health insurance premiums are categorized into five quintiles. In South Korea, every person must pay part of their income as an insurance premium. Thus, a higher quintile indicates a higher economic status. Basic livelihood security recipients were included in the medical aid.
Comorbidity refers to an underlying condition (e.g., diabetes, hypertension) that may cause and affect other diseases. In this study, the number of comorbidities was investigated with the question: “Among the following diseases, which diseases have you been diagnosed with, or have you been treated for?” with the examples of comorbidity, stroke, heart disease (e.g., myocardial infarction, angina pectoris), hypertension, diabetes, dyslipidemia, pulmonary tuberculosis, and other diseases including cancer.
Disability status included the presence, severity, and type of disability, including non-disabled, physical disability, encephalopathy, visual impairment, hearing impairment, and others. Disabled persons were registered with the Ministry of Health and Welfare of South Korea; hence, the NHIS data included their disability status. Severity and type of disability were measured according to the Act on Welfare of Persons with Disability.
Smoking was measured with the question: “In your life, have you ever smoked over five packs of cigarettes (100 pieces)?” Drinking was measured using the question, “How many times do you drink a week?”
2.3. Statistical analysis
The effects of PA and BMI on infection and mortality associated with COVID-19 were analyzed using logistic regression analysis, which was adjusted for sex, age, insurance type, comorbidities, and region of residence at baseline. Disability and lifestyle (e.g., need for weight management, smoking, and drinking status) were adjusted conjointly. Cases with missing data were excluded from the analysis. The 95% confidence interval (CI) was estimated using the SAS PROC PHREG. Statistical significance was set at p < 0.05. Statistical analyses were conducted using the SAS software (SAS Institute Inc., Cary, NC, USA).
3. Results
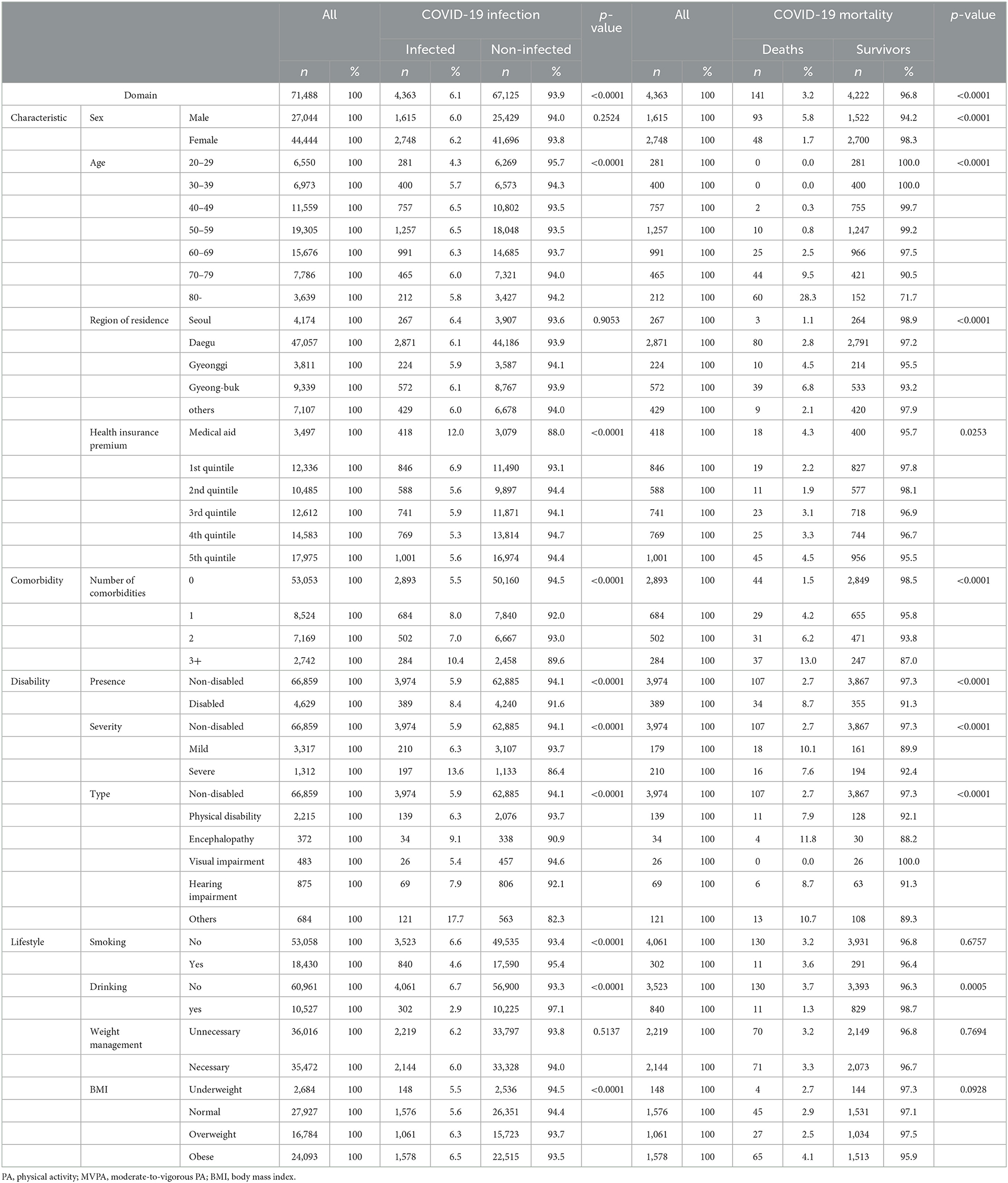
The analysis included 71,488 participants (62% women) over 20 years of age who had received medical checkups from 2015 to 2018. There were 4,363 COVID-19 confirmed cases (6.1%), including 141 deaths (3.3%; 48 women) (Table 1). Among the participants, 418 people with medical aid were developed COVID-19 (12%), with the highest ratio compared to the other quintiles. According to disability status, severe disability was associated with a higher infection rate (13.6%) than mild disability (6.3%) and non-disability (5.9%). People with comorbidities had a higher infection rate (number of comorbidities: 1 = 8%, 2 = 7%, 3 = 10.4%) than those without comorbidities (5.5%).
Of the confirmed cases, 73.75% of the deaths were of participants aged more than 70 years, while 1.41% were of those under 50 years old. Most deaths occurred in people who lived in Daegu (80 people, fatality rate of 2.8%) and Gyeong-Buk (39 people, fatality rate of 6.8%), whereas only 22 people died in other regions. Regarding comorbidities, 44 patients (1.5%) who had no underlying diseases died, while 97 patients (fatality rate, 1 = 4.2%, 2 = 6.2%, over 3 = 13%) died of COVID-19.
3.1. Associations between PA and COVID-19
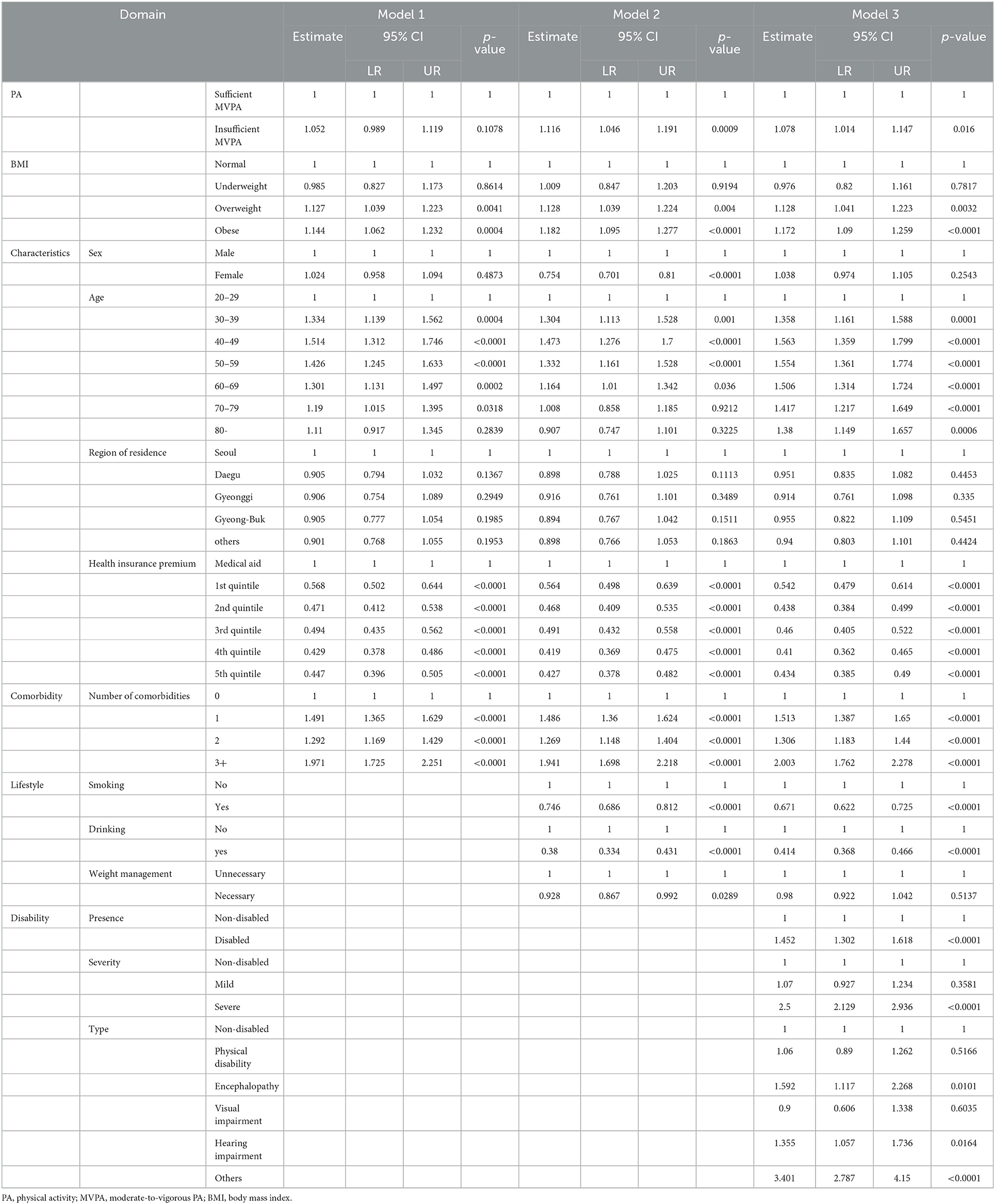
According to logistic regression Model 1 of COVID-19 (Table 2), which was adjusted for characteristics and comorbidity, not engaging in sufficient MVPA (95% CI: 0.989–1.119, p = 0.108) did not affect the risk COVID-19. According to logistic regression Model 2 of COVID-19, which was additionally adjusted for the need for weight management, smoking, and drinking status, not engaging in sufficient MVPA (OR: 1.116, 95% CI: 1.046–1.191, p < 0.01) predicted a higher risk of COVID-19 than engaging in sufficient MVPA. According to logistic regression Model 3 of COVID-19, which was additionally adjusted for disability status, not engaging in sufficient MVPA (OR: 1.078, 95% CI: 1.014–1.147, p < 0.05) still predicted a higher risk of COVID-19 than sufficient MVPA.
3.2. Associations between PA and COVID-19-associated mortality
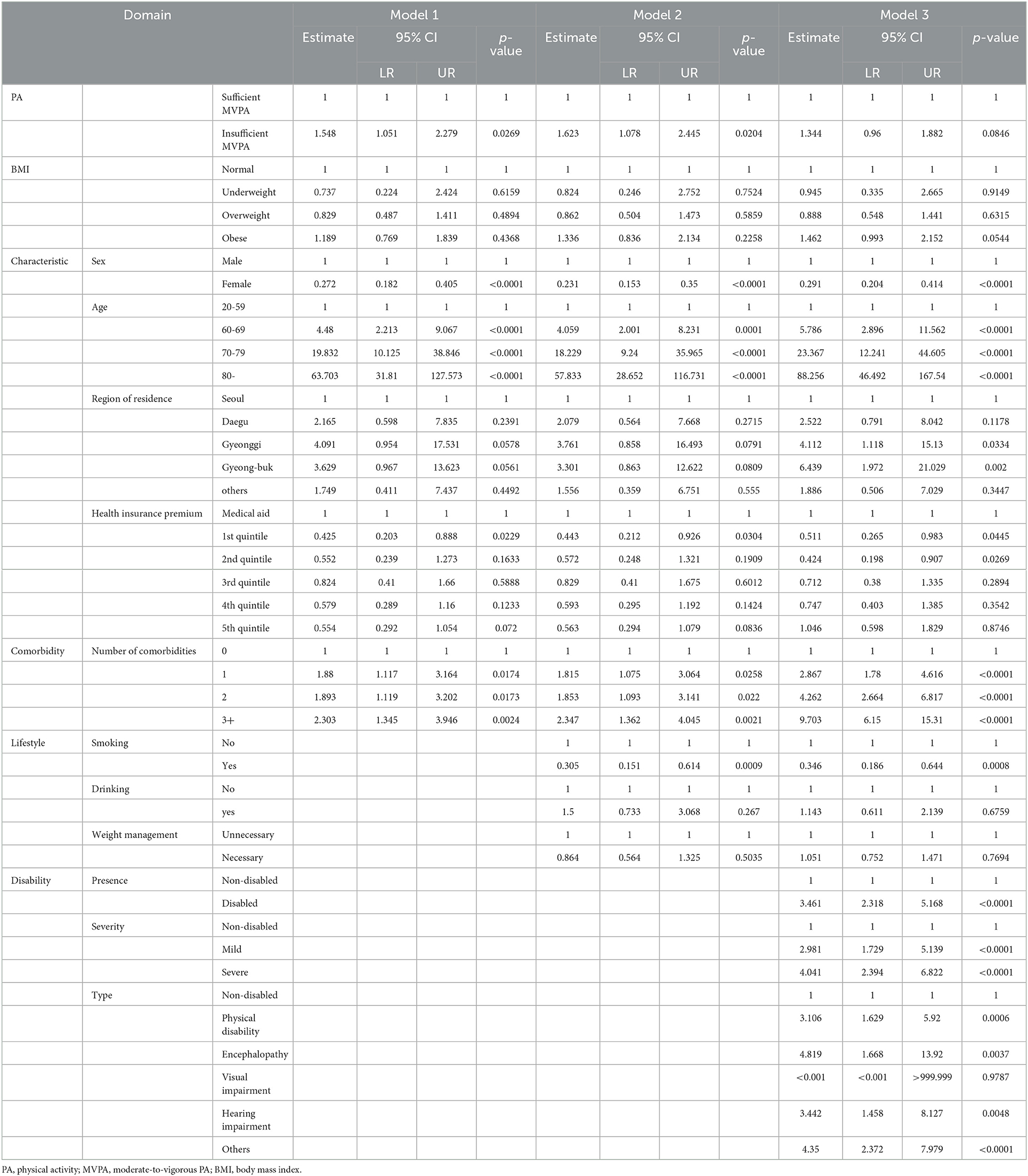
According to logistic regression Model 1 of COVID-19-associated mortality (Table 3), which was adjusted for characteristics and comorbidity, not engaging in sufficient PA (OR: 1.548, 95% CI: 1.051–2.279, p < 0.05) predicted a higher risk of COVID-19-associated mortality than engaging in sufficient PA. According to logistic regression Model 2 of COVID-19-associated mortality, which was additionally adjusted for the need for weight management, smoking, and drinking status, not engaging in sufficient MVPA (OR: 1.623, 95% CI: 1.078–2.445, p < 0.05) still predicted a higher risk of COVID-19-associated mortality than engaging in sufficient MVPA. According to logistic regression Model 3 of COVID-19-associated mortality, which was additionally adjusted for disability status, engaging in sufficient MVPA (95% CI: 0.96–1.882, p = 0.085) did not predict COVID-19-associated mortality. However, the presence of disability and the levels of severity of disability predicted COVID-19-associated mortality.
4. Discussion
This study aimed to determine the effect of MVPA on COVID-19 and the association between BMI and COVID-19, considering disability status. Investigating NHIS data on COVID-19 revealed several associations. Engaging in insufficient MVPA was associated with higher risk of infection and mortality associated with COVID-19, depending on confounding variables.
The importance of engaging in an active lifestyle was found to be influential on the risk of COVID-19 over the pandemic period. The result of this study aligns with those of a recent study, which reported the decrement of PA engagement over the period of COVID-19 (20) and the lower likelihood of developing COVID-19 (14). However, the current study has taken a step forward by utilizing the most recent data available before the pandemic. It is widely known that engaging in adequate MVPA is associated with positive health outcomes. However, the current study adds another piece of information on the role of engaging in MVPA. For example, a special focus should be paid to individuals with disabilities regardless of the type of disabilities. During the pandemic, disadvantaged populations may experience issues with accessing health information and PA programs in local communities. For example, statistics show a 4% decrement in PA participation by individuals with disabilities in 2021, compared to the participation rate in 2020 (21). Thus, it might be important to dedicate effort toward improving their participation. A recent review emphasized the role of supportive environments to stimulate one's autonomy, competence, and relatedness (i.e., social supports from close people) in PA settings (22). Given that older individuals are more susceptible to infection, these efforts must be focused on them. For example, local communities may provide newly developed programs to educate PA leaders, who may motivate older adults in their communities.
Engaging in insufficient MVPA could play an important role in reducing mortality associated with COVID-19. Previously, insufficient MVPA was reported as a negative predictor of all-cause mortality (23). However, the relation has not been confirmed in the patients with COVID-19. Interestingly, the estimates from the mortality results are higher than from the infection results, which suggests the importance of regular MVPA participation. Since the infection is an on-going phenomenon, engaging in MVPA should be recommended in South Korea. Particular attention should be paid to people, who are aged or physically disabled. It is noted that individuals with disability show much higher risks of mortality than those without disability. Thus, barriers to PA should be eliminated, particularly perceived barriers, such as feeling uncomfortable, a lack of time, and other priorities (24). A technique to overcome these barriers could be providing clear intervention based on the stage of intention of individuals with disability. It is important for researchers and regional practitioners to consider levels of motivation and volition (i.e., psychological willingness to participate in PA) (25) to provide proper PA guidelines.
This study has some limitations. First, this study's sampling period (8 months) was relatively short to determine the tendency of COVID-19, as the situation continues to evolve. At the beginning of this study, in August 2020, there were 4,222 confirmed cases and only 141 people had died of COVID-19 in South Korea. However, there are now more confirmed cases and deaths in South Korea. Second, it is difficult to generalize the results of South Korea and apply them to the rest of the world. Furthermore, the fatality rate in South Korea was deferred from the rate of the world. Thus, the results of this study may not be generalized. Finally, COVID-19 variants continue to evolve and affect individuals differently (26). As a result, the results from this study could not be applied to different variants. Thus, further studies must include various cases and variants to strengthen the associative findings between PA and COVID-19. Lastly, the current study did not examine the roles of light PA and sedentary behavior due to the limited data from the secondary source. Future research may include those variables to clarify the results of the current study.
In conclusion, this study examined the role of sufficient MVPA on both COVID-19 and associated mortality and found that engaging in sufficient MVPA may play a role in reducing the risk of COVID-19 and associated mortality. The main implication of the results is that an active lifestyle should be promoted in the community. In addition, urgent implementation is needed for people who are older or physically disabled.
Data availability statement
Data can be accessed with the permission of NHIS. Datasets of NHIS can be found here: https://nhiss.nhis.or.kr/bd/ay/bdaya001iv.do.
Author contributions
Conceptualization and analysis: I-HO and S-YP. Writing: SP and HK. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2022S1A5A8050449). This study was supported by the Translational R&D Program on Smart Rehabilitation Exercises (TRSRE-PS04), National Rehabilitation Center, Ministry of Health and Welfare, Korea.
Acknowledgments
We would like to acknowledge the contributions of specific colleagues, institutions, or agencies that aided the efforts of the authors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Klopfenstein T, Zahra H, Kadiane-Oussou N, Lepiller Q, Royer PY, Toko L, et al. New loss of smell and taste: uncommon symptoms in COVID-19 patients on Nord Franche-Comte cluster, France. Int J Infect Dis. (2020) 100:117–22. doi: 10.1016/j.ijid.2020.08.012
2. Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. BioRxiv. (2020) 3:7806. doi: 10.1101/2020.01.30.927806
3. World Health Organization. Coronavirus disease (COVID-19). Available online at: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed March 22, 2022).
4. World Health Organization. COVID-19 Weekly Epidemiological Update. Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-−24-august-2022 (accessed August 25, 2022).
5. Korea Disease Control and Prevention Agency. Cases in Korea. (2022). Available online at: http://ncov.kdca.go.kr/en/bdBoardList.do?brdId=16&brdGubun=161&dataGubun=&ncvContSeq=&contSeq=&board_id= (accessed August 18, 2022).
6. Twenge JM, Joiner TE, US. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. (2020) 37:954–56. doi: 10.1002/da.23077
7. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, physical activity, and relationship status on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. (2020) 136:110186. doi: 10.1016/j.jpsychores.2020.110186
8. Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. (2020) 26:1–12. doi: 10.12659/MSM.924609
9. Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with COVID-19: cohort study. BMJ. (2022) 376:e068993. doi: 10.1136/bmj-2021-068993
10. Bo HX Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2021) 51:1052–3. doi: 10.1017/S0033291720000999
11. Fox KR. The influence of physical activity on mental wellbeing. Public Health Nutr. (1999) 2:411–8. doi: 10.1017/S1368980099000567
12. Chin SH, Kahathuduwa CN, Binks M. Physical activity and obesity: what we know and what we need to know. Obes Rev. (2016) 17:1226–44. doi: 10.1111/obr.12460
13. Luciano F, Cenacchi V, Vegro V, Pavei G. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur J Sport Sci. (2021) 21:1459–68. doi: 10.1080/17461391.2020.1842910
14. Cho DH, Lee SJ, Jae SY, Kim WJ, Ha SJ, Gwon JG, et al. Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study. J Clin Med. (2021) 10:1539. doi: 10.3390/jcm10071539
15. Ezzatvar Y, Ramírez-Vélez R, Izquierdo M, Garcia-Hermoso A. Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose–response meta-analysis of data from 1 853 610 adults. Br J Sports Med. (2022) 56:1188–93. doi: 10.1136/bjsports-2022-105733
16. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. (2017) 46:e15. doi: 10.1093/ije/dyv319
17. Park S, Park SY, Cheong HK, Oh IH. Moderate-to-vigorous physical activity and risk of all-cause mortality in people with anxiety disorders in South Korea. Int J Sport Exerc Psychol. (2022) 3:1–13. doi: 10.1080/1612197X.2022.2066708
18. Meister T, Pisarev H, Kolde R, Kalda R, Suija K, Milani L, et al. Clinical characteristics and risk factors for COVID-19 infection and disease severity: a nationwide observational study in Estonia. PLoS ONE. (2022) 17:e0270192. doi: 10.1371/journal.pone.0270192
19. Han E, Tan J, Turk E, Sridhar D, Leung M, Shibuya K, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. (2020) 396:1525–34. doi: 10.1016/S0140-6736(20)32007-9
20. Yang HJ, Park S, Yoon TY, Ryoo JH, Park SK, Jung JY, et al. Nationwide changes in physical activity, nutrient intake, and obesity in South Korea during the COVID-19 pandemic era. Front Endocrinol. (2022) 13:965842. doi: 10.3389/fendo.2022.965842
21. Ministry Ministry of Culture Sports Tourism. [Internet]. Sejong; Sports for the Disabled Division. Press release, the participation rate of people with disabilities in sports for the disabled in 21 years decreased by 20.2% due to the influence of COVID-19. Available online at: https://www.mcst.go.kr/kor/s_notice/press/pressView.jsp?pSeq=19356 (accessed January 27, 2022).
22. Quested E, Kritz M, Hancox JE, Ntoumanis N, Thøgersen-Ntoumani C. Promoting self-determined motivation for physical activity: From theory to intervention work. In Essentials of exercise and sport psychology; An open access textbook, Zenko Z, Jones L, Eds.; Society for Transparency, Openness, and Replication in Kinesiology. (2021): 37-61. Available online at: https://selfdeterminationtheory.org/wp-content/uploads/2021/08/2021_QuestedKritzEtAl_PromotingSelfDetermined.pdf (accessed October 1, 2022).
23. Clarke AE, Janssen I. A compositional analysis of time spent in sleep, sedentary behavior and physical activity with all-cause mortality risk. Int J Behav Nutr Phys Act. (2021) 18:1–12. doi: 10.1186/s12966-021-01092-0
24. Buffart LM, Westendorp T, Van Den Berg-Emons RJ, Stam H, Roebroeck ME. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J Rehabil Med. (2009) 41:881–5. doi: 10.2340/16501977-0420
25. Jaarsma EA, Smith B. Promoting physical activity for disabled people who are ready to become physically active: a systematic review. Psychol Sport Exerc. (2018) 37:205–23. doi: 10.1016/j.psychsport.2017.08.010
26. World Health Organization. Tracking SARS-CoV-2 Variants. (2022). Available online at: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed March 22, 2022).
Keywords: physical activity, COVID-19, quarantine, lifestyle, COVID-19-associated mortality
Citation: Park S, Kim H, Park S-Y and Oh I-H (2023) Pre-pandemic physical activity as a predictor of infection and mortality associated with COVID-19: Evidence from the National Health Insurance Service. Front. Public Health 11:1072198. doi: 10.3389/fpubh.2023.1072198
Received: 17 October 2022; Accepted: 17 January 2023;
Published: 14 February 2023.
Edited by:
Yanan Zhao, Nanjing Normal University, ChinaReviewed by:
Jennifer Hale-Gallardo, United States Department of Veterans Affairs, United StatesWenSheng Zhou, Nanjing Xiaozhuang University, China
Copyright © 2023 Park, Kim, Park and Oh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: In-Hwan Oh,  cGFyZW5jaHltZUBnbWFpbC5jb20=
cGFyZW5jaHltZUBnbWFpbC5jb20=
 Saengryeol Park
Saengryeol Park Hyeseong Kim
Hyeseong Kim So-Youn Park
So-Youn Park In-Hwan Oh
In-Hwan Oh