
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 25 January 2023
Sec. Public Health Education and Promotion
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1072085
This article is part of the Research Topic Influence of Lifestyle Factors in the Management of Diabetes Mellitus View all 15 articles
Introduction: Low awareness of the necessity of taking medication is common among patients with diabetes mellitus (DM) due to their lack of understanding of the disease. Therefore, it is essential to determine the underlying risks influencing low awareness to design effective intervention strategies. This study aims to evaluate the association of sociodemographic and behavioural factors with low awareness to take medication among patients with DM in Indonesia.
Method: Retrospective data were obtained from the Indonesian Family Life Survey (IFLS-5), a national cross-sectional population-based survey among respondents with DM aged ≥15 years. DM status was confirmed by HbA1c testing, while sociodemographic and other health-related information was obtained from self-reported data. Gender, age, educational level, marital status, economic status, comorbidity, religiosity, residence and health insurance status were considered sociodemographic, whereas blood glucose monitoring status, sleeping problems, depression status, having a general medical check-up, satisfaction with healthcare needs and happiness status were considered behavioural risk factors. Awareness of DM medication was determined by self-reported responses to the question asked by the surveyor. Logistic regression analysis was used to evaluate the association between sociodemographic and behavioural factors and low awareness of DM medication. Odds ratios (ORs) with 95% confidence intervals (CIs) were reported.
Result: Most of the 706 respondents were female (58.8%) and aged 55–65 years (28.8%). Most of them showed low awareness of diabetes medication (87.7%). Irregular blood glucose monitoring (OR: 23.61, 95% CI 11.46–48.65; p < 0.001), without any comorbidity (OR: 2.03, 95% CI 1.05–3.90; p = 0.034), never had any general medical check-up (OR: 2.52, 95% CI 1.12–5.36; p = 0.016), 26–35 years of age (OR: 4.96, 95% CI 1.06–23.19; p = 0.042), 36–45 years of age (OR: 5.04, 95% CI 1.17–21.69; p = 0.030) and having no health insurance coverage (OR: 2.08, 95% CI 1.12–3.87; p = 0.021) were significantly associated with low awareness of diabetes medication.
Conclusion: Healthcare professionals should regularly evaluate blood glucose level, perform routine medical check-ups, prioritise patient satisfaction by providing appropriate care, involve patients in decision-making by determining their needs and then tailor an intervention to meet the need for, and improve their awareness of, DM medication.
Diabetes mellitus (DM) has increased drastically in the past three decades; around 422 million people worldwide have diabetes, with deaths totalling 1.5 million (1). The number of patients with DM in Southeast Asia is predicted to increase by 113 million by 2030 (2). DM ranks second among the most common non-communicable diseases in Indonesia, with a prevalence of 10.9% (3). In addition, more than half of the individuals with DM in Indonesia (73.7%) were unaware of their condition (4). Therefore, if DM is left unmanaged and untreated, it could lead to either microvascular (retinopathy, nephropathy and neuropathy) or macrovascular (stroke, cardiovascular disease and peripheral artery disease) complications (5). Unfortunately, no complete cure for diabetes has been found; thus, long-term treatment to prevent or delay complications and maintain the patient's quality of life is needed (6).
Healthcare professionals have a crucial role in developing strategies to facilitate medication adherence so that patients can optimise diabetes treatment and limit the progression of diabetes (6). This emphasises the significance of patient education and awareness of DM medication after having acquired awareness of DM (7). Thus, the first approach for healthcare practitioners could be to increase DM medication awareness. Awareness of medication was defined as a patient's common knowledge or understanding about his/her medication without direct instruction or as a sort of medication self-consciousness (8). Awareness is one of the five primary types of related concerns with the potential to improve therapy since they are obstacles to medication adherence from the patient's perspective (9). It is somewhat distinct from medication adherence, defined as the process whereby patients take their medication as prescribed (10). Inadequate medication adherence among DM patients remains a major problem leading to disease progression (11). At least 45% of treatment failures among DM patients are caused by low adherence to anti-diabetic medical treatments (12). This could lead to increases in health expenses yearly at both patient and societal levels (13).
Patients with good comprehension and high awareness of diabetic medication exhibited an improvement in their glucose control (14) and medication adherence (15). Therefore, identifying factors associated with medication awareness is an important first step to improving medication adherence. Although studies about medication awareness in patients with diabetes are limited, some studies have explored a positive correlation between the frequency of healthcare professional counselling and the patient's level of awareness to take their medication (16, 17). The Indonesian Family Life Survey (IFLS) is a longitudinal socioeconomic and health survey in Indonesia, which covers ~83% of the Indonesian population (18). Previous studies that employed IFLS-4 or IFLS-5 mostly examined the prevalence of DM and its sociodemographic risk factors (19–22). Other research evaluated the association between socioeconomic characteristics and the incidence of diabetes (23, 24). Until now, no study has investigated psychosocial and sociodemographic factors associated with medication awareness among DM patients using IFLS. It is still unclear as to which components or focal points are necessary to increase DM medication awareness in Indonesia. Therefore, addressing its fundamental causes is vital for developing effective intervention strategies. This study aims to identify sociodemographic and behavioural factors associated with low awareness of DM medication in Indonesia.
The cross-sectional study design utilised in this study is based on secondary data, IFLS-5. The IFLS is a longitudinal study that used a multistage stratified sample design to represent 83% of the Indonesian population (18). The IFLS sampling strategy stratified on provinces and urban/rural locations and then sampled randomly within these strata. Provinces were chosen to optimise population representation, represent Indonesia's cultural and socioeconomic variety and be cost-effective to survey, given the country's size and geography. Therefore, 13 of the 27 provinces that existed at the time were included. The IFLS randomly selected 321 enumeration areas (EA) within each of the 13 provinces, oversampling urban EAs and EAs in smaller provinces to facilitate urban–rural and Javanese–non-Javanese comparisons. Twenty households from each urban EA and 30 households from each rural EA were selected (18). The IFLS gathered sociodemographic, economic, and health status characteristics, including self-reported health status, symptoms and pain assessments, as well as biomarker assessments. Preliminary testing of the IFLS questionnaire ensured its reliability and validity before the full-scale survey was conducted (18). The ethical review boards of the RAND's Human Subjects Protection Committee (s0064-06-01-CR01) approved IFLS research. Before data collection, every respondent provided written consent (18). Approval was sought from the research ethics committee of Universitas Padjadjaran, Indonesia, which waived the requirement because this study uses anonymous data from the IFLS.
Data were collected from IFLS-5 from individuals aged at least 15 years after the survey. Individuals with available data on HbA1c and medication for chronic diseases were included.
Patients with DM were defined as having an HbA1c value of ≥6.5% (25). The blood samples examined were obtained from dried blood spots (DBSs) and taken through the capillaries at the fingertips (18). These blood samples are easier to obtain than those taken through intravenous vessels and are more durable in terms of storage (26). However, the results of the HbA1c examination from DBS will first be converted to whole blood HbA1c, the gold standard of HbA1c examination, so that it can be used in the diagnosis of DM (18).
Awareness of DM medication was determined by the responses to the following question posed by the surveyor: Are you currently taking prescription medication weekly to manage your DM? Those who responded with a “yes” were considered to have a good awareness of DM medication, whereas those who responded with a “no” were thought to have low awareness. This questionnaire has been validated and involved extensive pretests and analysis of the pretest data (18).
Sociodemographic and behavioural risk factors were analysed as potential contributors to low awareness of DM medication. Age, gender, educational level, marital status, residency, economic status, health insurance coverage, religiosity and comorbidity status were categorised into sociodemographic and behavioural factors. At the same time, behavioural factors included blood glucose monitoring status, general medical check-ups, health care satisfaction, happiness status, insomnia and depressive symptom status.
Sociodemographic factors were age after the survey, gender (male/female), level of education (no education, elementary school, junior high school, senior high school and university), marital status (currently married and currently unmarried), residency (urban and rural) and health insurance coverage (yes and no). To assess the economic status, we divided the annual household income in rupiah by family size during the previous 12 months (per capita income). Capita income was categorised per quintile. The quintile is categorised by sorting the per capita income from lowest to highest and then dividing them into five equal groups (the first quintile = an income ≤ $77.01; the second quintile = $77.01–$256.70; the third quintile = $256.70–$483.55; the fourth quintile = $483.55–$924.7; the fifth quintile ≥ $924.7). To evaluate religiosity, we asked the question How religious are you? The individuals who said they were extremely religious or religious were classified as religious, whereas those who said they were somewhat religious or not religious were classified as non-religious (27).
Depressive symptoms were assessed using a self-reported Centre for Epidemiologic Studies Depression (CES-D) scale (18). The CES-D consists of 10 items highly linked to the presence of depressive symptoms (28). Eight of the questions examine the negative symptoms of depression (e.g., I felt fearful and lonely), whereas the other two examined the positive symptoms (e.g., I felt hopeful about the future). The respondents stated how frequently each item applied to them in the previous week using a four-point Likert-type scale (0 = rarely or never, 1 = some or little, 2 = moderately or much of the time, and 3 = frequently or almost always). After reversing the positive mood items, the total score is obtained by summing all elements. An individual with a total score of ≥10 is deemed to have depressive symptoms (29). The CES-D questionnaire was translated into Indonesian (forward translation) and then re-translated separately into English by two translators (back translation) (18).
Ten Patient-Recorded Outcomes Measurement Information System (PROMIS) questions were used to assess the severity of insomnia (18). Each measure of sleep quality and sleep impairment during the previous week was determined using a set of five items (30). Each item was rated using a five-point Likert-type scale (0 = never/not at all; 1 = a little bit; 2 = somewhat; 3 = quite a bit; 4= always/very much). Insomnia was defined as a total score of ≥21–40 (31). The PROMIS questionnaire was translated into Indonesian (forward translation) and then re-translated separately into English by two translators (back translation) (18).
The question Has a doctor/paramedic/nurse/midwife ever told you that you have the following chronic ailments or diseases? was used to evaluate whether the individuals had comorbid disease status, with the following potential responses: hypertension; DM; TB; asthma and other chronic lung diseases; cardiac disease (heart attack/coronary heart disease/angina or other heart diseases); liver disease; stroke; cancer or other malignancies; gout/uric acid; depression and vision and hearing abnormalities (27). Individuals who responded only with DM were classified as having no comorbidity. Individuals who responded with DM and one to three additional chronic diseases were classified as having 1–3 comorbidities, whereas individuals with four or more comorbidities were classified as having >4 comorbidities.
Individuals' response to the question How regularly do you have your blood glucose checked? determined the classification of blood glucose monitoring status as either regular or irregular. Individuals' response to Have you had a general check-up in the recent 5 years? as either yes or no determined one's status as having/not having had a general medical check-up. Happiness level was determined by asking Overall, how would you describe the current state of these days? Would you say you are very happy, happy, unhappy or very unhappy? (27). Those who responded with very happy or happy were categorised as happy, whereas those who responded with unhappy or very unhappy were categorised as unhappy. Satisfaction with healthcare was measured with the question In relation to your healthcare, which of the following is true: it is less than adequate for my needs; it is just adequate for my needs or it is more than adequate for my needs? (27). Low healthcare satisfaction corresponds to the response “it is just less than adequate for my needs,” and high healthcare satisfaction corresponds to “it is just adequate for my needs” or “it is more than adequate for my needs.”
Descriptive statistics were used to summarise the characteristics of the individuals. Awareness of DM medication was estimated for each age group and gender. The Little test was performed to assess whether the incomplete data type was classified as Missing Completely At Random (MCAR). The Little test assumes that the missing-ness of the data is independent of both observed and unobserved data, thus, a p > 0.05 is considered MCAR because it is asymptotically distributed under the null hypothesis that there are no differences between the observed and unobserved data (32). Since the missing data were MCAR (p > 0.005), complete case analyses could be carried out (32). A Chi-square test was conducted to evaluate the bivariate relationship between the individuals' characteristics and outcomes. The potential factors related to the outcome in the bivariate analysis at a significance threshold of p < 0.25 were included in the initial multivariate model. To determine the odds ratio (OR) with a 95% confidence interval (95% CI), multivariate logistic regression with manual backward elimination was used. The p-values for the factors included in the final model were all fixed to p < 0.05. The Hosmer–Lemeshow test was used to assess the goodness-of-fit statistic; R-squared is a number ranging from 0 to 1, indicating how much the combination of independent factors influences the value of the dependent variable at the same time (33). All statistical analyses were performed using Stata software version 14.0 for Windows.
A total sample of 706 individuals without missing data on awareness of DM medication was included in this study. The majority of the respondents were female (58.8%) and aged 55–65 years (28.8%; Table 1). A high proportion of individuals had irregular blood glucose monitoring (90.1%), with most of them (88.4%) not having undergone a general medical check-up. Approximately half of the individuals were not covered by health insurance (50.4%) and had no comorbidities (50.1%). Out of the total respondents, 22.1% experienced depression, whereas 85.9% had insomnia.
The prevalence of low awareness of DM medication was 87.9% in females and 86.0% in males. Gender, educational level, marital status, economic status, religiosity, happiness status, insomnia and depressive symptoms were not statistically significant differences between the low-awareness DM medication group and the high-awareness DM medication group (Table 1). Age, residency, health insurance coverage, blood glucose monitoring status, comorbidities and general medical check-up were selected as potential factors associated with low awareness of DM medication on the basis of bivariate analyses. In the multivariate model, irregular blood glucose monitoring (OR: 23.61, 95% CI 11.46–48.65; p < 0.001), having no comorbidity (OR 2.03, 95% CI 1.05–3.90; p = 0.034), not having undergone any general medical check-up (OR 2.52, 95% CI 1.12–5.36; p = 0.016), 26–35 years of age (OR 4.96, 95% CI 1.06–23.19; p = 0.042), 36–45 years of age (OR 5.04, 95% CI 1.17–21.69; p = 0.030) and having no health insurance coverage (OR 2.08, 95% CI 1.12–3.87; p = 0.021) were significantly associated with low awareness of diabetes medication (Table 2). The goodness-of-fit p-value of the model was 0.552, with an R-squared value of 34.71%.
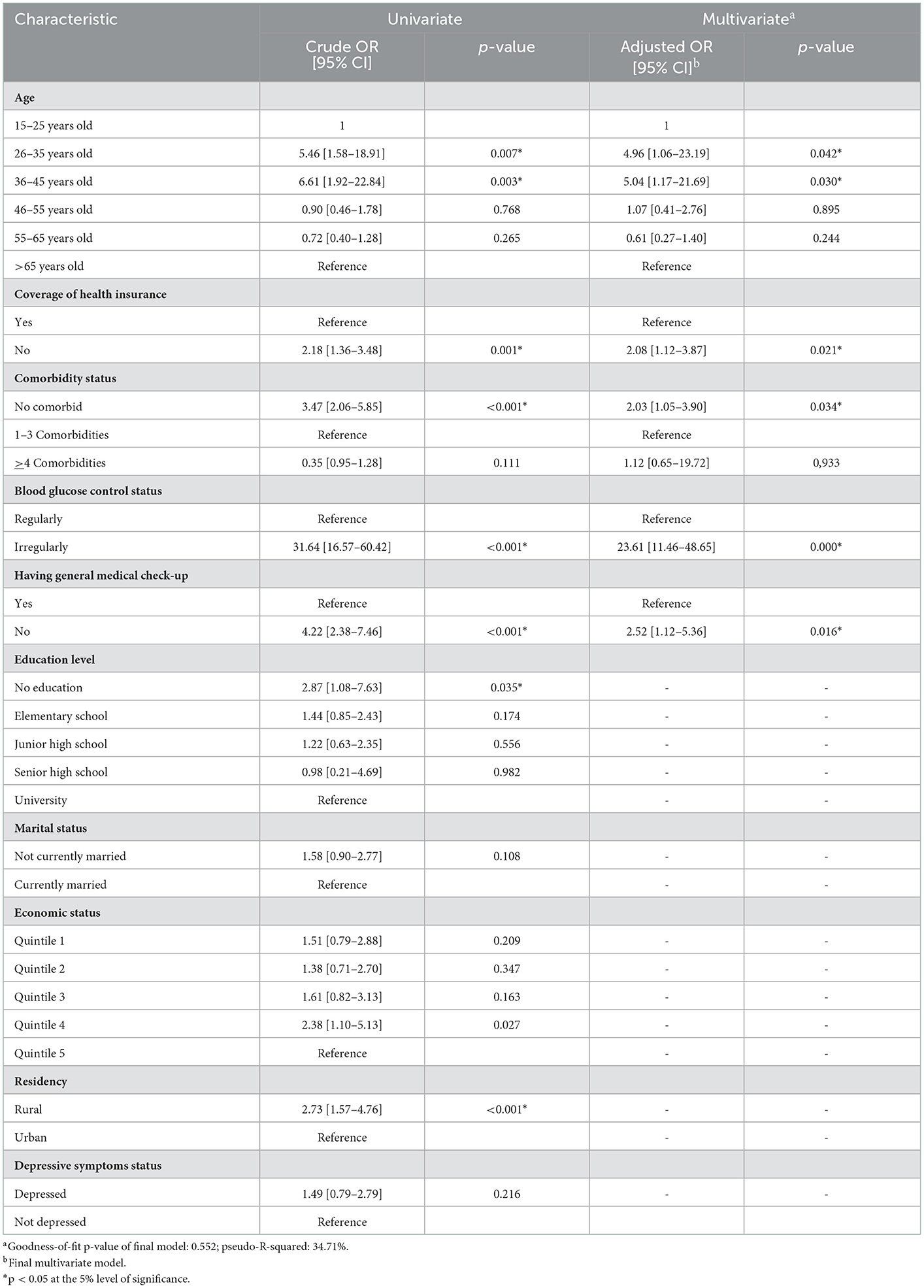
Table 2. Association between sociodemographic and behavioural factors and low awareness of diabetes mellitus medication.
This study revealed that more than three-quarters of DM patients had low awareness of their medication therapy. This implies that only one out of four patients had high awareness of their medication therapy. Age and healthcare insurance coverage are sociodemographic factors associated with awareness of DM medication, whereas blood glucose monitoring status, comorbidity status, and having a routine medical check-up are behavioural factors associated with awareness of DM medication.
We observed that the young (26–35 years old) and middle (36–45 years old) adulthood were associated with low awareness of DM medication, similar to what a Malaysian study revealed (34). This might be due to the old misconception that DM is a disease that primarily only affects the elderly (35). However, the prevalence of type 2 diabetes in adolescents and adults is dramatically increasing due to unhealthy lifestyles and obesity, which has a more aggressive disease profile, leading to premature complications that affect the quality of life and long-term outcomes (36).
In this study, coverage of health insurance and awareness of DM medication were observed to be in significant association. Individuals with no health insurance were twice as likely to have low awareness of their medication therapy when compared with those who have health insurance. This might be because self-paying DM patients may have high substantial medical expenses or financial issues. In turn, this may lead them to forego diabetic care as well as DM medication that would otherwise help them survive their conditions (37). Another possible explanation for this is that patients without medical insurance more likely skip regular medical care (38) and do not acquire better education, which may lead to low awareness of DM medication therapy.
We further observed that the number of comorbidities had a significant association with awareness of DM medication. This study revealed that individuals with no comorbidities were twice as likely to have low awareness of their DM medication when compared with those with 1–3 comorbidities. This finding is in line with the results of a study conducted in Malaysia reporting that patients with comorbidities had a high level of awareness; however, their level of self-care practise for diabetes remained low (39). Other recent qualitative research showed that patients with no comorbidities felt they may have prevented disease progression had they been given a more detailed explanation of their situation earlier as they were unaware of the risk factors, complications, and comorbidities (40).
DM individuals with irregular blood glucose monitoring likely had low awareness of their medication therapy when compared with individuals with regular blood glucose monitoring. The possible reason is perhaps that patients with regular blood glucose monitoring were more conscious of the consequences of not taking the drugs appropriately (41). DM patients who never had general medical check-ups were twice as likely to have low awareness of DM medication when compared with those who had had a general medical check-up. This might be because general medical check-ups provide health-related information, help identify issues early, assist in planning treatments as well as improve the awareness of medication (42).
A majority of the sociodemographic factors were not associated with low awareness of DM medication. Sociodemographic factors, such as marital status, may be overly generic when predicting an individual's DM medication awareness. A study revealed no correlation between gender and low awareness of DM medication (43). However, males were reported to be less aware of DM than females were (44, 45). Furthermore, in our study, educational level is not related to medication awareness as health literacy may be more essential than educational level (46). By contrast, another study found individuals with higher educational levels to have more awareness (47). The current study also found residency not to be associated with low awareness of DM medication, contradicting the results of a previous study, which reported a correlation between urban residence and high awareness of DM medication as urban residents seek therapy more often and have easier access to care (48). Moreover, religiosity was not associated with DM medication awareness in this study. This finding is contrary to the results of previous studies suggesting that, in terms of providing assistance and coping with a disease condition, religiosity played a significant role (49, 50). We further observed that depressive symptoms, happiness, insomnia and satisfaction with healthcare are not associated with low awareness of DM medication therapy. Previous studies have reported that depressive symptoms (51), insomnia (52), and happiness (53) were not associated with awareness of DM medication, which is in line with the present results. By contrast, in previous studies, the individuals more satisfied with their healthcare were possibly more aware of their DM medication (54, 55).
The awareness of DM patients about their medication is crucial for ensuring that they take their DM medication as prescribed to avoid any complications or associated morbidities and mortality (56). These findings may help us understand the significance of the issue of awareness of DM medication as well as offer potential solutions. During the early stages of the disease, it may be necessary for patients to be better informed to increase their awareness of DM medication, particularly among those at high risk of developing comorbidities and complications (57). To raise patients' awareness of DM medication, healthcare professionals are essential information resources and play a leading role in the awareness-raising effort (58). Patient education can be improved by first determining the individual's learning needs and then providing them with individualised educational interventions tailored to meet their requirements (59). This study, thus, advocates for better management of DM by inquiring about medication adherence during clinical consultations and improving the quality of DM care. Furthermore, patient education, counselling and behavioural support are critical for achieving successful DM medication therapy. These tailored interventions could be effective in clarifying misconceptions and help clear up any misunderstandings to increase their level of awareness (60). In addition, healthcare professionals should monitor blood glucose, perform general medical check-ups regularly, prioritise patient satisfaction by ensuring that they receive appropriate care and establish a respectful and caring relationship with patients by involving them in decision-making (61). The current findings may be useful as a point of reference for healthcare professionals, addressing factors related to low awareness of DM medication (Figure 1).
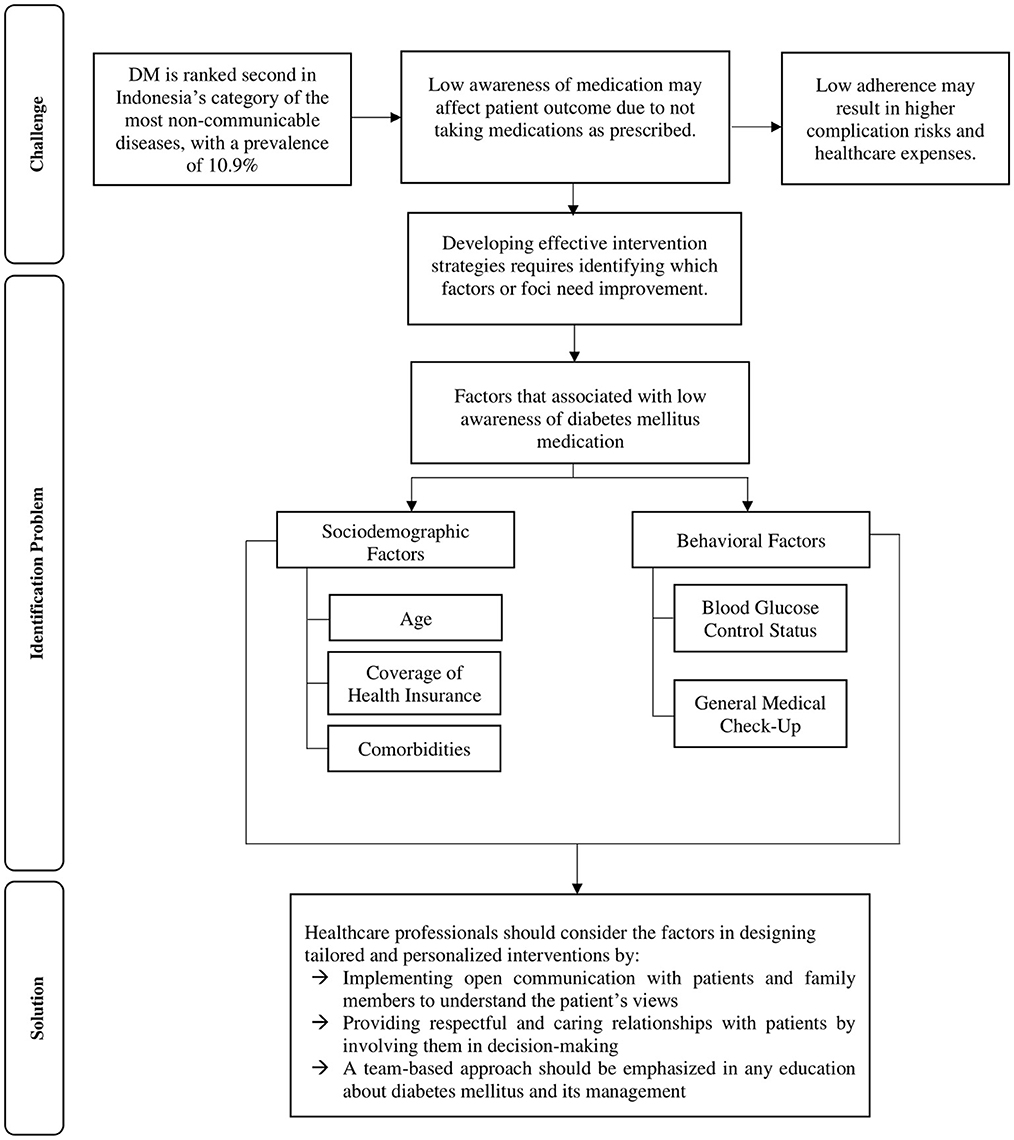
Figure 1. Problems, challenges and solutions to increase the level of awareness of diabetes mellitus medication in Indonesia.
Until now, the present study appears to be the first to assess the awareness of DM medication and its associated factors in Indonesia. The study's strength is that we used the IFLS data, which represents 83% of the Indonesian population with an attrition rate of only 6%. The IFLS provides numerous benefits, including large samples, which are relatively heterogenous, less expensive than collecting new data and representative of the Indonesia setting. Besides, in this analysis, individuals were included on the basis of an objective measurement of HbA1c >6.5%, providing a more objective individual selection and avoiding selection bias. Despite its strengths, the study certainly has certain limitations related to methodological issues. First, notably, the cross-sectional design of the study precludes any causal inferences regarding the relationship between sociodemographic and behavioural factors and low awareness of DM medication. Second, since we performed a complete case analysis, it may have reduced the statistical power, probably increasing the possibility of bias in our estimation, which might be an overestimation or underestimation of conclusions. Third, we have a wide CI value, indicating a greater likelihood of uncertainty regarding whether we have precisely estimated the strength of the association. Fourth, this study was at risk to recall bias due to disparities in accuracy in recalling past events based on self-reported answers from several variable independents. Fifth, this study was unable to distinguish between DM types 1 and 2. Sixth, as we relied on a secondary database that provides binary outcomes for the awareness, it might not be adequate to explain the multidimensional aspects of behavioural science (62). Further studies are needed to consider these aspects when assessing awareness of medication. Seventh, our model's overall association was low, indicating the possibility of other unmeasured factors influencing the low awareness of DM medication, such as another comorbid disease such as kidney disease (63), healthy lifestyle (64), education about DM (65), the number of medicines in the therapy (66), duration of DM (67), ethnic background (68) or medication beliefs (69).
Healthcare professionals should monitor blood glucose, perform general medical check-ups regularly, prioritise patient satisfaction by ensuring that they receive appropriate care and establish a respectful and caring relationship with patients by involving them in the decision-making process. Patient education can be improved by first determining the individual's learning needs and then providing them with individualised educational interventions tailored to meet their requirements in order to improve their awareness of DM medication. Therefore, our findings reveal the need to develop intervention strategies targeting those who irregularly monitor their blood glucose level; who irregularly undergo general medical check-ups, with multiple comorbidities; who have no health insurance coverage and who are young.
Publicly available datasets were analysed in this study. This data can be found here: https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html.
The Ethical Review Boards of the RAND's Human Subjects Protection Committee (s0064-06-01-CR01) approved IFLS research. Research Ethics Committee of Universitas Padjadjaran, Indonesia, waived the requirement because this study uses anonymous data from the IFLS.
QK wrote the first draft of this manuscript. SA and RA participated in the design of the study. QK and SA participated in data analysis and interpretation. QK, SA, and RA revised the manuscript. All authors approved the final manuscript.
This study was supported by a grant-in-aid from Universitas Padjadjaran. QK was supported by a postgraduate scholarship (PMDSU Scholarship) from the Indonesian Ministry of Education, Culture, Research, and Technology.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. Fact Sheets: Diabetes. World Heal Organ. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/diabetes#::text=In2019%2Cdiabetes%20was%20the%20direct%20cause%20of%201.5%20million,age%20of%2070%20from%20diabetes (accessed February 21, 2022).
3. Kemenkes RI. Hasil Riset Kesehatan Dasar Tahun 2018. Jakarta: Kementrian Kesehatan Republik Indonesia (2018).
4. IDF. IDF Diabetes Atlas: Indoensia Diabetes Report 2000 – 2045. (2021). Available online at: https://www.diabetesatlas.org/data/en/country/94/id.html (accessed October 29, 2022).
5. Shi Y, Vanhoutte PM. Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes. (2017) 9:434–49. doi: 10.1111/1753-0407.12521
6. ADA. Standards of Medical Care in Diabetes-2020 Abridged for Primary Care Providers. United States. American Diabetes Association (2020).
7. AlShayban DM, Naqvi AA, Alhumaid O, AlQahtani AS, Islam MA, Ghori SA, et al. Association of disease knowledge and medication adherence among out-patients with type 2 diabetes mellitus in Khobar, Saudi Arabia. Front Pharmacol. (2020) 11:1–9. doi: 10.3389/fphar.2020.00060
8. Gafoor AK. Considerations in measurement of awareness. Natl Semin Emerg Trends Educ. (2012) 1–6. Available online at: https://files.eric.ed.gov/fulltext/ED545374.pdf (accessed November 11, 2022).
9. Gordon K, Smith F, Dhillon S. Effective chronic disease management: patients' perspectives on medication-related problems. Patient Educ Couns. (2007) 65:407–15. doi: 10.1016/j.pec.2006.09.012
10. Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. (2012) 73:691–705. doi: 10.1111/j.1365-2125.2012.04167.x
11. Araya EM, Gebrezgabiher HA, Tekulu GH, Alema NM, Getnet D, Gebru HT, et al. Medication non-adherence and associated factors among diabetic patients visiting general hospitals in the eastern zone of Tigrai, Northern Ethiopia. Patient Prefer Adherence. (2020) 14:2071–83. doi: 10.2147/PPA.S278148
12. Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. (2016) 10:1299–306. doi: 10.2147/PPA.S106821
13. Feldhaus I, Nagpal S, Verguet S. Alleviating the burden of diabetes with health equity funds: economic evaluation of the health and financial risk protection benefits in Cambodia. PLoS ONE. (2021) 16:e0259628. doi: 10.1371/journal.pone.0259628
14. McPherson ML, Smith SW, Powers A, Zuckerman IH. Association between diabetes patients' knowledge about medications and their blood glucose control. Res Soc Adm Pharm. (2008) 4:37–45. doi: 10.1016/j.sapharm.2007.01.002
15. Okuyan B, Sancar M, Izzettin FV. Assessment of medication knowledge and adherence among patients under oral chronic medication treatment in community pharmacy settings. Pharmacoepidemiol Drug Saf. (2012) 22:209–14. doi: 10.1002/pds.3275
16. Alkatheri AM, Albekairy AM. Does the patients' educational level and previous counseling affect their medication knowledge? Ann Thorac Med. (2013) 8:105–8. doi: 10.4103/1817-1737.109823
17. Abdu-Aguye SN, Labaran KS, Danjuma NM, Mohammed S. An exploratory study of outpatient medication knowledge and satisfaction with medication counselling at selected hospital pharmacies in Northwestern Nigeria. PLoS ONE. (2022) 17:1–14. doi: 10.1371/journal.pone.0266723
18. Strauss J, Witoelar F, Sikoki B. The fifth wave of the Indonesia family life survey: overview and field report: volume 1. RAND Corporation (2016) 94p.
19. Kamilah FZ, Habibie F, Rahma GR, Sofyan MNF, Isnaini NS, Nadhilah ND, et al. Analysis of the determinants of diabetes mellitus in Indonesia: a case study of the 2014 indonesian family life survey. Dis Prev Public Heal J. (2021) 15:88. doi: 10.12928/dpphj.v15i2.3079
20. Safitri AZ, Fajariyah RN, Astutik E. Risk factors of diabetes mellitus in urban communities in Indonesia (IFLS 5). J Berk Epidemiol. (2021) 9:184. doi: 10.20473/jbe.V9I22021.184-191
21. Tanoey J, Becher H. Diabetes prevalence and risk factors of early-onset adult diabetes: results from the Indonesian family life survey. Glob Health Action. (2021) 14:2001144. doi: 10.1080/16549716.2021.2001144
22. Asrullah M, L'Hoir M, Feskens EJM, Melse-Boonstra A. Trend in age at menarche and its association with body weight, body mass index and non-communicable disease prevalence in Indonesia: evidence from the Indonesian Family Life Survey (IFLS). BMC Public Health. (2022) 22:1–10. doi: 10.1186/s12889-022-12995-3
23. Indrahadi D, Wardana A, Pierewan AC. The prevalence of diabetes mellitus and relationship with socioeconomic status in the Indonesian population. J Gizi Klin Indones. (2021) 17:103. doi: 10.22146/ijcn.55003
24. Finkelstein EA, Chay J, Bajpai S. The economic burden of self-reported and undiagnosed cardiovascular diseases and diabetes on Indonesian households. PLoS ONE. (2014) 9:e99572. doi: 10.1371/journal.pone.0099572
25. ADA. Classification and diagnosis of diabetes : standards of medical care in diabetes — 2022. Diabetes Care. (2022) 45:17–38. doi: 10.2337/dc22-S002
26. Mastronardi CA, Whittle B, Tunningley R, Neeman T, Paz-Filho G. The use of dried blood spot sampling for the measurement of HbA1c: a cross-sectional study. BMC Clin Pathol. (2015) 15:1–7. doi: 10.1186/s12907-015-0013-5
28. Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for depression in the general population with the center for epidemiologic studies depression (ces-d): a systematic review with meta-analysis. PLoS ONE. (2016) 11:1–17. doi: 10.1371/journal.pone.0155431
29. Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. (2013) 20:429–36. doi: 10.1177/1073191113481998
30. Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, et al. Development of short forms from the PROMIS sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. (2011) 10:6–24. doi: 10.1080/15402002.2012.636266
31. Peltzer K, Pengpid S. Prevalence, social and health correlates of insomnia among persons 15 years and older in Indonesia. Psychol Heal Med. (2019) 24:757–68. doi: 10.1080/13548506.2019.1566621
32. Li C. Little's test of missing completely at random. Stata J. (2013) 13:795–809. doi: 10.1177/1536867X1301300407
33. Dodge Y. Chi-square Goodness of Fit Test. In: The Concise Encyclopedia of Statistics. New York, NY: Springer New York, 72–6.
34. Ho BK, Jasvindar K, Gurpreet K, Ambigga D, Suthahar A, Cheong SM, et al. Prevalence, awareness, treatment and control of diabetes mellitus among the elderly: the 2011 National Health and Morbidity Survey, Malaysia. Malaysian Fam Physician. (2014) 9:12–9.
35. Song SH. Emerging type 2 diabetes in young adults. Adv Exp Med Biol. (2012) 771:51–61. doi: 10.1007/978-1-4614-5441-0_7
36. Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. (2018) 6:69–80. doi: 10.1016/S2213-8587(17)30186-9
37. Al-Sanaani EA, Ismail A, Manaf MRA, Suddin LS, Mustafa N, Sukor N, et al. Health insurance status and its determinants among patients with type 2 diabetes mellitus in a tertiary teaching hospital in Malaysia. PLoS ONE. (2022) 17:1–17. doi: 10.1371/journal.pone.0267897
38. Tipirneni R, Politi MC, Kullgren JT, Kieffer EC, Goold SD, Scherer AM. Association between health insurance literacy and avoidance of health care services owing to cost. JAMA Netw open. (2018) 1:e184796. doi: 10.1001/jamanetworkopen.2018.4796
39. Abdulghani HM, AlRajeh AS, AlSalman BH, AlTurki LS, AlNajashi NS, Irshad M, et al. Prevalence of diabetic comorbidities and knowledge and practices of foot care among diabetic patients: a cross-sectional study. Diabetes, Metab Syndr Obes Targets Ther. (2018) 11:417–25. doi: 10.2147/DMSO.S171526
40. Lopez-Vargas PA, Tong A, Howell M, Phoon RKS, Chadban SJ, Shen Y, et al. Patient awareness and beliefs about the risk factors and comorbidities associated with chronic kidney disease : a mixed-methods study. Nephrology. (2017) 22:374–81. doi: 10.1111/nep.12829
41. Pascal IGU, Ofoedu JN, Uchenna NP, Nkwa AA, Uchamma GUE. Blood glucose control and medication adherence among adult type 2 diabetic Nigerians attending a primary care clinic in under-resourced environment of eastern Nigeria. N Am J Med Sci. (2012) 4:310–5. doi: 10.4103/1947-2714.98590
42. Ngo TT, Hoang PN, Pham HV, Nguyen DN, Bui HTT, Nguyen AT, et al. Routine medical check-up and self-treatment practices among community-dwelling living in a mountainous area of Northern Vietnam. Biomed Res Int. (2021) 2021:8734615. doi: 10.1155/2021/8734615
43. Shahzad A, Ahmad MM, Anwer I, Ijaz N, Shahzad M, Usman M. Gender-specific knowledge of diabetes and its management among patients visiting outpatient clinics in Faisalabad, Pakistan. Cureus. (2018) 10:2–10. doi: 10.7759/cureus.3119
44. Siddiqui M, Khan M, Carline T. Gender differences in living with diabetes mellitus. Mater Socio Medica. (2013) 25:140. doi: 10.5455/msm.2013.25.140-142
45. Obirikorang Y, Obirikorang C, Anto EO, Acheampong E, Batu EN, Stella AD, et al. Knowledge of complications of diabetes mellitus among patients visiting the diabetes clinic at Sampa Government Hospital, Ghana: a descriptive study. BMC Public Health. (2016) 16:1–8. doi: 10.1186/s12889-016-3311-7
46. Zowgar AM, Siddiqui MI, Alattas KM. Level of diabetes knowledge among adult patients with diabetes using diabetes knowledge test. Saudi Med J. (2018) 39:161–8. doi: 10.15537/smj.2017.2.21343
47. Al-Rasheedi AAS. The role of educational level in glycemic control among patients with type II diabetes mellitus. Int J Health Sci. (2014) 8:177–87. doi: 10.12816/0006084
48. Deepa M, Bhansali A, Anjana R, Pradeepa R, Joshi S, Joshi P, et al. Knowledge and awareness of diabetes in urban and rural India: the Indian council of medical research india diabetes study (phase i): Indian council of medical research india diabetes 4. Indian J Endocrinol Metab. (2014) 18:379–85. doi: 10.4103/2230-8210.131191
49. Watkins YJ, Quinn LT, Ruggiero L, Quinn MT, Choi Y-K. Spiritual and religious beliefs and practices, and social support's relationship to diabetes self-care activities in African Americans. Diabetes Educ. (2013) 39:231–9. doi: 10.1177/0145721713475843
50. Duke N. Type 2 diabetes self-management: spirituality, coping and responsibility. J Res Nurs. (2021) 26:743–60. doi: 10.1177/17449871211026958
51. Egede LE, Ellis C. The effects of depression on diabetes knowledge, diabetes self-management, and perceived control in indigent patients with type 2 diabetes. Diabetes Technol Ther. (2008) 10:213–9. doi: 10.1089/dia.2007.0278
52. Schipper SBJ, Van Veen MM, Elders PJM, van Straten A, Van Der Werf YD, Knutson KL, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia. (2021) 64:2367–77. doi: 10.1007/s00125-021-05541-0
53. Liu SY, Huang J, Dong QL, Li B, Zhao X, Xu R, Yin HF. Diabetes distress, happiness, and its associated factors among type 2 diabetes mellitus patients with different therapies. Medicine. (2020) 99:e18831. doi: 10.1097/MD.0000000000018831
54. White RO Eden S, Wallston KA, Kripalani S, Barto S, Shintani A, Rothman RL. Health communication, self-care, and treatment satisfaction among low-income diabetes patients in a public health setting. Patient Educ Couns. (2015) 98:144–9. doi: 10.1016/j.pec.2014.10.019
55. Boels AM, Vos RC, Hermans TGT, Zuithoff NPA, Müller N, Khunti K, et al. What determines treatment satisfaction of patients with type 2 diabetes on insulin therapy? An observational study in eight European countries. BMJ Open. (2017) 7:e016180. doi: 10.1136/bmjopen-2017-016180
56. Al-Qazaz HK, Sulaiman SA, Hassali MA, Shafie AA, Sundram S, Al-Nuri R, et al. Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int J Clin Pharm. (2011) 33:1028–35. doi: 10.1007/s11096-011-9582-2
57. Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. (2018) 6:130–42. doi: 10.1016/S2213-8587(17)30239-5
58. Tan E, Khoo J, Gani LU, Malakar RD, Tay TL, Tirukonda PS, et al. Effect of multidisciplinary intensive targeted care in improving diabetes mellitus outcomes: a randomized controlled pilot study - the integrated diabetes education, awareness and lifestyle modification in Singapore (IDEALS) Program. Trials. (2019) 20:1–10. doi: 10.1186/s13063-019-3601-3
59. Adam L, O'Connor C, Garcia AC. Evaluating the impact of diabetes self-management education methods on knowledge, attitudes and behaviours of adult patients with type 2 diabetes mellitus. Can J Diabetes. (2018) 42:470–7.e2. doi: 10.1016/j.jcjd.2017.11.003
60. Cruz-Cobo C, Santi-Cano MJ. Efficacy of diabetes education in adults with diabetes mellitus type 2 in primary care: a systematic review. J Nurs Scholarsh. (2020) 52:155–63. doi: 10.1111/jnu.12539
61. Tamhane S, Rodriguez-Gutierrez R, Hargraves I, Montori VM. Shared decision-making in diabetes care. Curr Diab Rep. (2015) 15:1–10. doi: 10.1007/s11892-015-0688-0
62. Trevethan R. Deconstructing and assessing knowledge and awareness in public health research. Front Public Heal. (2017) 5:16–9. doi: 10.3389/fpubh.2017.00194
63. Nordheim E, Jenssen TG. Chronic kidney disease in patients with diabetes mellitus. Endocr Connect. (2021) 10:R151–9. doi: 10.1530/EC-21-0097
64. Ang BW, Tan MY, Goh CM, Rahardja S, Lim BY, Chiew W, et al. Impact of knowledge and attitudes on lifestyle practices in preventing type 2 diabetes mellitus. Ann Acad Med Singapore. (2019) 48:247–63. doi: 10.47102/annals-acadmedsg.V48N8p247
65. Foma MA, Saidu Y, Omoleke SA, Jafali J. Awareness of diabetes mellitus among diabetic patients in the Gambia: a strong case for health education and promotion. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-1124
66. Shams N, Amjad S, Kumar N, Ahmed W, Saleem F. Drug non-adherence in type 2 diabetes mellitus; predictors and associations. J Ayub Med Coll Abbottabad. (2016) 28:302–7.
67. Ghouse J, Isaksen JL, Skov MW, Lind B, Svendsen JH, Kanters JK, et al. Effect of diabetes duration on the relationship between glycaemic control and risk of death in older adults with type 2 diabetes. Diabetes, Obes Metab. (2020) 22:231–42. doi: 10.1111/dom.13891
68. Taylor YJ, Davis ME, Monahan S, Robertson S, Robinson MD. Awareness of racial disparities in diabetes among primary care residents and preparedness to discuss disparities with patients. J Racial Ethn Heal Disparities. (2019) 6:237–44. doi: 10.1007/s40615-018-0518-6
69. Alfian SD, Annisa N, Fajriansyah F, Perwitasari DA, Abdulah R, Hak E, et al. Modifiable factors associated with non-adherence to antihypertensive or antihyperlipidemic drugs are dissimilar: a multicenter study among patients with diabetes in Indonesia. J Gen Intern Med. (2020) 35:2897–906. doi: 10.1007/s11606-020-05809-y
Keywords: awareness medication, diabetes mellitus, determinants, IFLS, Indonesia
Citation: Khoiry QA, Alfian SD and Abdulah R (2023) Sociodemographic and behavioural risk factors associated with low awareness of diabetes mellitus medication in Indonesia: Findings from the Indonesian Family Life Survey (IFLS-5). Front. Public Health 11:1072085. doi: 10.3389/fpubh.2023.1072085
Received: 17 October 2022; Accepted: 05 January 2023;
Published: 25 January 2023.
Edited by:
Celestino Sardu, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Edward Zimbudzi, Monash University, AustraliaCopyright © 2023 Khoiry, Alfian and Abdulah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sofa D. Alfian,  c29mYS5hbGZpYW5AdW5wYWQuYWMuaWQ=
c29mYS5hbGZpYW5AdW5wYWQuYWMuaWQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.