
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 01 June 2023
Sec. Health Economics
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1069131
This article is part of the Research Topic Translating Health Economics Research into Public Health Action: Towards an Economy of Wellbeing View all 15 articles
Background: In 2020, the Chinese government developed and implemented an innovative case-based payment method under the regional global budget called the diagnosis-intervention packet (DIP) payment to pay for inpatient care. This study aims to assess the changes to inpatient care provision in hospitals after the DIP payment reform was implemented.
Methods: This study used inpatient medical costs per case, the proportion of the out-of-pocket (OOP) expenditure in inpatient medical costs, and the average length of stay (LOS) of inpatient care as outcome variables, and conducted an interrupted time series analysis to evaluate changes after the DIP payment reform. January 2021 was taken as the intervention point when a national pilot city of the DIP payment reform in the Shandong province began using the DIP payment to pay for inpatient care of secondary and tertiary hospitals. The data used in this study were obtained from the aggregated monthly claim data of inpatient care of secondary and tertiary hospitals.
Results: Compared to the pre-intervention trend, the inpatient medical costs per case, the proportion of the OOP expenditure in inpatient medical costs both in tertiary and secondary hospitals significantly decreased after the intervention. After the intervention, the reduction in the inpatient medical costs per case, the proportion of the OOP expenditure in inpatient medical costs in tertiary hospital were both higher than those in secondary hospital (p < 0.001). The average LOS of inpatient care in secondary hospital significantly increased after the intervention, and it immediately increase 0.44 day after intervention (p = 0.211). Moreover, the change of average LOS of inpatient care in secondary hospital after intervention was opposite to that in tertiary hospital, it had no statistical difference (p = 0.269).
Conclusion: In the short term, the DIP payment reform could not only effectively regulate provider behavior of inpatient care in hospitals, but also improves the rational allocation of the regional healthcare resources. However, the long-term effects of the DIP payment reform need to be investigated in the future.
The growth of health expenditure has become a critical issue for healthcare policymakers and governments in many countries. To remedy this, countries have sought to improve the efficiency of healthcare delivery and reduce the growth rate of health expenditure by implementing healthcare provider payment reforms (1). Among the global empirical evidence of provider payment methods reforms, case-based payment approaches, such as the diagnosis-related group (DRG) system, have been widely adopted to pay for inpatient care (2, 3). Moreover, previous research has highlighted that case-based payment methods not only promoted the transparency and quality of healthcare services, but also enabled policymakers to not accurately compare the healthcare service performance of different hospitals (4).
Over past decades, total health expenditure (THE) in China has rapidly increased (5). This is thought to be a result of the prolonged use of fee-for-service (FFS) payments for inpatient care (6, 7), which has been associated with over-treatment and induced demand (8, 9). In an effort to curb the increase of the health expenditure, many cities throughout China have tried to design and implement various case-based payment methods (10, 11). The design frameworks of these case-based payments were based on the characteristics of local healthcare service markets, and as a result, it is difficult to generate generalizable findings from their implementation. Consequently, the Chinese government initiated DRG payment system reform in 2019 to control the growth of health expenditure (12). When developing the reforms, it was noted that a number of studies showed that the DRG payment system cannot cover all forms of healthcare services, and it also leads to unintended provider behaviors, such as up-coding, cream skimming, or induced demand behavior (13, 14). In addition, it was recognized that the operation of the DRG payment system requires a high administrative cost and advanced information system (15). Accordingly, the Chinese government decided to develop an innovative case-based payment system with a uniform design framework, which was intended to avoid some of the problems associated with existing DRG payment systems (16). Eventually, in 2020, the Chinese government launched an innovative case-based payment method under the regional global budget called the diagnosis-intervention packet (DIP) payment.
However, as the DIP payment is a recent initiative. There are few studies about the effect evaluation of the DIP payment, which leads that the current studies have not been able to adequately demonstrate its impact on changes to inpatient care provision until now. Among the few related studies, Lai et al. (17) discovered that the inpatient medical costs per case and the medication costs of inpatient care were significantly decreased after the DIP payment was implemented in Guangzhou. However, Qian et al. (18) outlined that the implementation of DIP yet increases the inpatient medical costs per case. Accordingly, this study selects the pilot city of the DIP payment in Shandong province as case city and aims to explore the changes to inpatient care provision in secondary and tertiary hospitals after the DIP payment reform was implemented, which can comprehensively demonstrate the impacts of diagnosis-intervention packet payment on the providers’ behavior of inpatient care.
As with the DRG payment system, the DIP payment includes a series of classifications of DIP disease groups. Based on the same major diagnosis principles and similar treatment procedures, the National Healthcare Security Administration firstly enacted the uniform score catalogue and classification standards of the DIP disease groups, containing 11,553 core disease groups and 2,499 comprehensive disease groups. Subsequently, according to the uniform classification standards of the DIP disease groups, the 71 pilot cities of the DIP payment reform throughout China were required to enact the catalog of core disease groups and comprehensive disease groups. Meanwhile, the pilot cities needed to formulate the average score of each local DIP disease group by using the average medical cost of all inpatient care cases in the last 3 years.
Although the DIP payment has several differences with the DRG payment (Table 1), however the most significant feature of the new system is the design of payment standards of DIP disease groups (Figure 1). Unlike predetermined DRG payment systems, the payment standards of DIP payments are not fixed. Although the scores that reflect the consumption of healthcare resources of DIP disease groups are certain, the monetary value, or unit cost, of each score is not predefined. The value of the DIP payment depends on the regional global budget of insurance funding and the regional sum score of all inpatient care in the pilot cities (19). More specifically, the annual unit price of each score equals the annual regional global budget divided by the annual sum score of all inpatient care under this region, together with a further risk-adjustment (Equation 1). As such, if the healthcare service volumes increase, then the unit price of each score will be devalued, which will affect the revenue of the hospitals. The aforementioned risk-adjustment includes the Case Mix Index (CMI), the status of the hospital and the type of health insurance, are brought into the calculation of the reimbursements of hospitals.
Reimbursements to hospitals are further adjusted based on several indicators of performance. These include, quality of medical records, readmission rate, length of stay (LOS) and mortality. These adjustments are made in the form of organization level ‘fines’ (Equation 2).
Through this design, the policymakers hope that the DIP payment can effectively incentivize individual hospitals to improve the efficiency and quality of their services, while promoting the allocative efficiency of regional healthcare resources.
As one of the 71 pilot cities in China, City A is the only pilot and typical city of the DIP payment reform in the Shandong province. It has three urban areas and two country areas. In 2021, the number of the resident population is 2.20 million residents, and the Gross Domestic Product per capita is 156.90 CNY which is the highest in Shandong province (20). Moreover, City A has seven tertiary hospitals and thirty-nine secondary hospitals that used the single case-based payment system under the regional global budget to pay for inpatient care before the DIP payment was introduced. The single case-based payment system in City A had many similarities to the DIP system that replaced it, however, important differences can be seen in relation to the number of disease groups, risk adjustment and payment ceilings for individual hospitals (Table 2).
In 2020, City A introduced the DIP payment system to categorize inpatient care without changing the reimbursement policies of inpatient care. From January 2021, City A started to use the DIP payment to pay for all inpatient care of local secondary and tertiary hospitals.
As such, the implementation of the DIP payment reform in City A was conceptualized as a quasi-experiment, with January 2021 serving as the intervention point in this study. An interrupted time series (ITS) design was used to assess whether the DIP payment reform produced significant changes to inpatient care provision in secondary and tertiary hospitals.
Fortunately, City A is the only one in Shandong province that did not have a COVID-19 pandemic before May 2022. All the residents’ healthcare consumption always can be satisfied in local hospitals. Therefore, we collected and aggregated the monthly medical claim data of inpatient care for secondary and tertiary hospitals in City A during January 2019 to April 2022, which was obtained from the Healthcare Security Administration in City A.
To accurately quantify the change to inpatient care provision in hospitals, several variables were selected for measurement during the study observation, including inpatient medical costs per case, proportion of the out-of-pocket (OOP) expenditure in inpatient medical costs, and average LOS of inpatient care. All data in the study was adjusted using the related consumer price index, with 2019 serving as the base year (20). A log transformation was performed for the skewed data distribution in this study. Additionally, the ordinary least squares (OLS) regressions incorporated seasonal adjustments for the variables that displayed conspicuous seasonal effects (21).
The ITS analysis was used to assess the changes to inpatient care provision. In the ITS analysis, a segmented OLS regression model with a Newey-West test was used to assess the impacts of the DIP payment reform on the change to inpatient care provision in hospitals (22). The segmented regression model we adopted is shown below:
Yt is the dependent variable we measured at every monthly point t, Tt is the time series variable representing the time in months since the start of observation until to the time t, Xt is a dummy variable representing the intervention point (pre-intervention period is 0 and the post-intervention period is 1), Tt Xt is an interaction term of the time and intervention, and εt is the residual term representing the unknown variation component of the regression model. β0 represents the baseline level; β1 represents the baseline trend prior to intervention; β2 represents the immediate level of change after the intervention compared to the pre-intervention; β3 represents the trend change after the intervention compared to the pre-intervention; and β1+ β3 represents the trend after the intervention (23). The actest command was conducted to assess autocorrelation and the autocorrelation results were both present at lag1 (24). STATA 16.0 was used to perform all statistical analysis. Two-sided hypothesis tests of no effect, with p < 0.05 were considered statistically significant.
Figure 2 demonstrates that the inpatient medical costs per case in tertiary hospitals perceptibly decreased after the intervention. The inpatient medical costs per case in tertiary hospital decreased by 150 CNY per month compared to the pre-intervention trend (p < 0.001) (Table 3). Moreover, compared to the pre-intervention trend, the inpatient medical costs per case in secondary hospital decreased only slightly after the intervention, having no statistically significant difference (p = 0.307). However, the inpatient medical costs per case in tertiary hospitals keep decreasing by 0.07 CNY per month, which is opposite to that in secondary hospitals (p < 0.05) (Table 3).
After the intervention, the proportion of the OOP expenditure in inpatient medical costs in secondary and tertiary hospitals both decreased slightly (p < 0.001) (Figure 3). The proportion of the OOP expenditure in inpatient medical costs in secondary decreasing by 0.09 percentage points per month compared to the pre-intervention trend (p < 0.01). Furthermore, the reduction in the proportion of the OOP expenditure in inpatient medical costs in tertiary hospital was more pronounced than that in secondary hospital (Table 3), decreasing by 0.17 percentage points per month compared to the pre-intervention trend (p < 0.001) (Table 3).
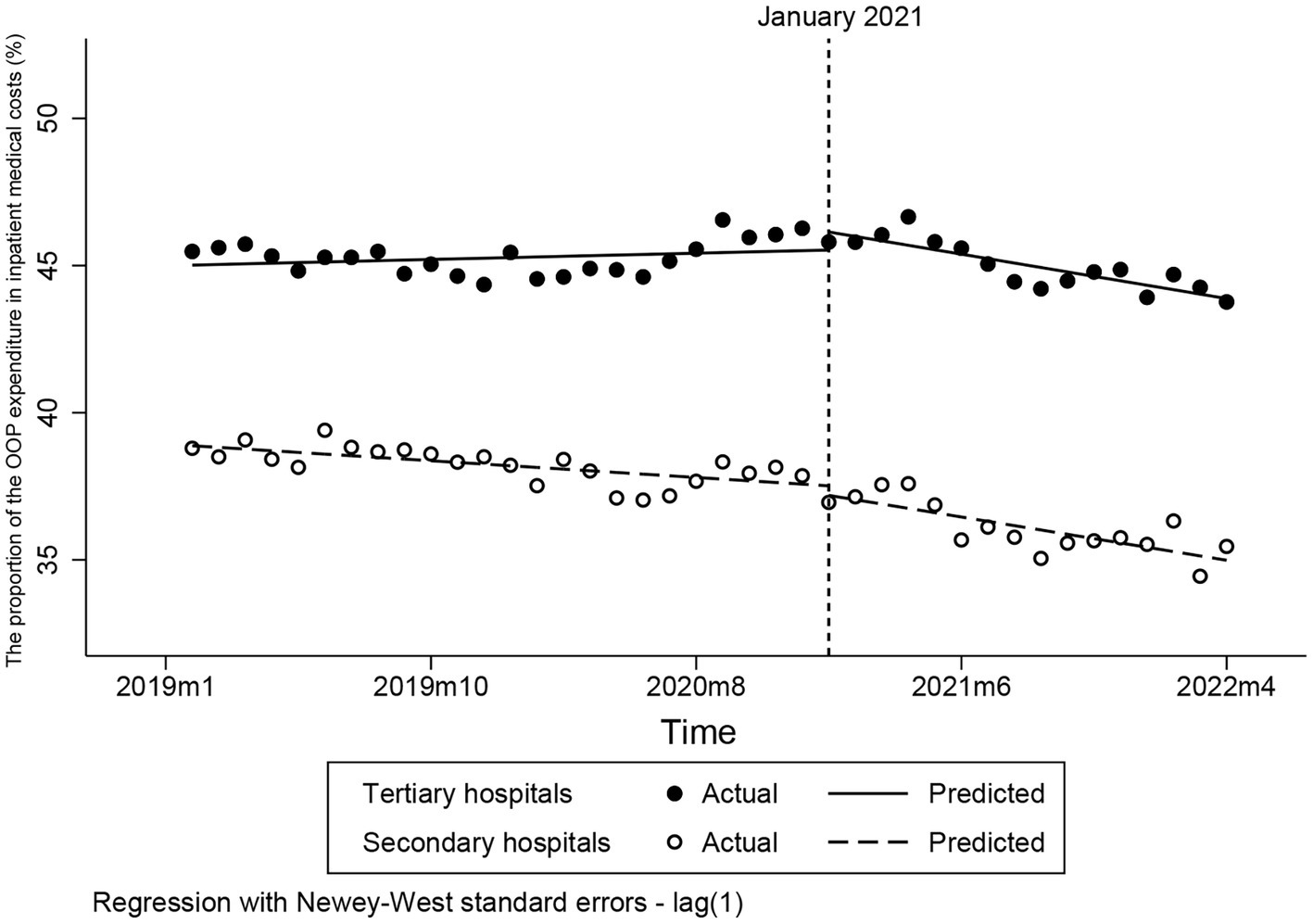
Figure 3. Changes to the proportion of the OOP expenditure in inpatient medical costs. OOP, out-of-pocket.
Prior to intervention, the baseline trend of the average LOS of inpatient care in secondary and tertiary hospitals had no obvious difference (Figure 4). After the intervention, the average LOS of inpatient care in secondary immediately increase 0.44 day in February 2021 which is significantly obvious than that in tertiary hospitals (p = 0.211). However, the change in average LOS of inpatient care in secondary and tertiary hospitals were opposite. Compared to the pre-intervention trend, the average LOS of inpatient care in tertiary hospital decreased by 0.05 day (p < 0.001), and the average LOS of inpatient care in secondary hospital increased 0.04 day (p < 0.001) (Table 3).
The rapid growth of the inpatient health expenditure poses a serious challenge for the Chinese government (25). Faced with this predicament, the Chinese government has implemented a series of healthcare provider payment reform policies including the DIP payment reform, especially since the National Healthcare Security Administration was established in 2018 (26).
In this study, we found that the inpatient medical costs per case decreased after the implementation of the DIP payment reform, which was aligned to the related studies (17). Consequently, this result is believed to illustrate the advantage of the DIP payment reform design in controlling the inpatient medical costs, especially for tertiary hospitals. Based on the design of the DIP payment, in the situation where the unit price of each score in the DIP payment was unknown before the end of a year, hospitals under the DIP payment had to improve the efficiency of their inpatient care in order to prevent the potential money devaluation of scores of DIP disease groups. Furthermore, although the detailed classifications of DIP disease groups make the provider payment more rational and scientific, however it also brings higher requirement to capacity of cost containment and management of different hospitals. In this case, the hospitals especially tertiary hospitals under the DIP payment will have more initiatives to control the medical costs to ensure the normal revenue of hospitals.
Previous studies highlight that the single healthcare provider payment reforms occasionally result in the increase in the proportion of the OOP expenditure or other medical costs of healthcare services (27, 28). In China, the healthcare service purchasers, such as the Healthcare Security Administration, preferred to use the single healthcare provider payments, such as the global budget or quota payments to pay for hospitals through “premium packages” (7, 29). Additionally, the payment standards of single healthcare provider payments used in China commonly lack the detailed risk-adjustment mechanisms that generate payment standards, which cannot satisfy the practical demand of different hospitals (30). Therefore, hospitals have had to decrease the provision of healthcare services reimbursed by medical insurance to prevent overspending of the medical insurance budget. In China, due to the service volume in tertiary hospitals is much larger than that in secondary hospitals, therefore that phenomenon is more obvious in tertiary hospitals (31). Surprisingly, for both secondary and tertiary hospitals, the proportion of the OOP expenditure in inpatient medical costs was found to significantly decrease after the intervention, fully illustrating that the implementation of the DIP payment reform could effectively promote hospitals to increase the provision of healthcare services covered by medical insurance and regulate the provider behavior in hospitals. It is concluded that the average score of the disease groups, along with the risk-adjustment mechanism of payment standards, are the key factors contributing to this effect. The establishment of the risk-adjustment mechanism aligns the payment standards more closely with the practical demand of secondary and tertiary hospitals, thereby alleviating the pressure of cost containment while providing more rational treatments and services to patients. In addition, this result convincingly proves that the risk-adjustment factors mechanism can promote payment standards more reasonable, which can better satisfy the actual operation costs of hospitals with different statuses.
It is worth noting that the average LOS in secondary hospital experienced an obvious increase after the DIP payment reform was implemented, which was opposite to that in tertiary hospital. We consider that this opposite result is a positive reaction to the implementation of the DIP payment. In order to better reflect the service capacity of hospitals, the reimbursements of hospitals in the DIP payment are relevant to the severity degree of inpatient cases and the status of hospitals. It not only promoted hospitals have more initiatives to treatment the sicker cases, but also achieved that the hospitals under the DIP payment have no necessary to strictly control the LOS of inpatient care due to the cost containment. Accordingly, the reasons we conclude behind the change of the average LOS in this study was that the implementation of the DIP payment enhanced the enthusiasm of inpatient care provision in secondary hospitals, which made some patients who can be treated in secondary hospitals accept more treatments. Additionally, the number of secondary hospitals is more than that of tertiary hospitals, and the copayment ratio of inpatient care in City A is increased with the status of hospitals increases. In this case, the patients got more inpatient care in secondary hospitals also led to the LOS in tertiary hospitals decreasing. Furthermore, the reduction of the proportion of the OOP expenditure in inpatient medical costs in tertiary hospitals compared to the pre-intervention trend is more obvious than that in secondary hospitals after the DIP payment reform was implemented, which further illustrates that the DIP payment reform can effectively alleviate the cost-control pressure of inpatient care in tertiary hospitals. Therefore, combined with the change in the proportion of OOP expenditure in inpatient medical costs and average LOS in secondary and tertiary hospitals, we believe that the DIP payment reform not only alleviated the provision pressure of inpatient care in tertiary hospitals but also improved the rational allocation of the regional healthcare resources. However, Vuagnat et al. outlined that case-based payments, such as the DRG payment, could indirectly lead hospitals to increase the average LOS and readmission rates of inpatient care for the sake of getting more premium (32). Furthermore, related study highlighted that the implementation of the DIP payment could potentially increase the frequency of up-coding behavior in hospitals (17). According to the change in average LOS in this study, we cannot rule out the possibility that the implementation of the DIP payment reform might also generate unintended consequences for inpatient care in secondary hospitals.
This study has several limitations that needed to be addressed: First, this study did not introduce a control group which means that we cannot rule out the possibility that the estimated changes are due to the impact of other phenomena, that changed patient and hospital behavior. Second, due to its recent introduction, we were only able to assess the short-term effects of the DIP payment reform, yet it is possible that there may be a lag in realizing the full effect of policy changes as patients and providers adapt to the new incentives. Third, this study did not involve patient outcomes, such as patient satisfaction or readmission rate, which could indicate a potential impact of the DIP payment on quality of inpatient care.
The DIP payment could effectively regulate provider behavior of inpatient care in hospitals in the short term, both of which are clearly reflected in the decrease of inpatient medical costs per case and the proportion of the OOP expenditure in inpatient medical costs in secondary and tertiary hospitals. Meanwhile, the implementation of the DIP payment could improve the rational allocation of the regional healthcare resources, which is reflected in the significant increase of the average LOS of inpatient care in secondary hospital and the decrease of average LOS of inpatient care in tertiary hospital. However, the long-term effects of the DIP payment reform still need to be evaluated in the future. In summary, we suggest the countries that are using the case-based payment or ongoing provider payment reform of inpatient care refer to the design elements of the DIP payment to further improve the design of case-based payments.
The data analyzed in this study is subject to the following licenses/restrictions: the data that support the findings of this study are available from the Healthcare Security Administrations but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Requests to access these datasets should be directed to YD, MjAxOTIwNzI0QG1haWwuc2R1LmVkdS5jbg==.
YD, CZ, and QS: conceptualization. JY, SD, and QS: project administration and supervision. YD and CZ: data curation, methodology, and software. YD: writing—original draft. YD, SD, and QS: writing—review and editing. All authors contributed to the article and approved the submitted version.
This work was undertaken as part of the UK China Health and Economy Partnership, a higher education programme funded by the GlaxoSmithKline (GSK) and supported by the British Council through an unrestricted grant. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
DIP, diagnosis-intervention packet; OOP, out-of-pocket; DRG, diagnosis-related group; ITS, interrupted time series analysis; OLS, ordinary least squares; LOS, length of stay.
1. Caryn, B, Sarah, B, and Kristiina, K. Transition to diagnosis related group (DRG) payments for health: lessons from case studies. World Bank Group (2020). doi: 10.1596/978-1-4648-1521-8
2. Kim, S, Jung, C, Yon, J, Park, H, Yang, H, Kang, H, et al. A review of the complexity adjustment in the Korean diagnosis-related group (KDRG). Health Inf Manag J. (2020) 49:62–8. doi: 10.1177/1833358318795804
3. Kone, I, Maria, ZB, Nordstrom, K, Simone, EB, and Wangmo, T. A scoping review of empirical evidence on the impacts of the DRG introduction in Germany and Switzerland. Int J Health Plan Manag. (2019) 34:56–70. doi: 10.1002/hpm.2669
4. Peter Leslie, A, and Dale, H. Case-based payment systems for hospital funding in Asia: an investigation of current status and future directions Geneva, World Health Organization (2015). doi: 10.1787/9789264173446-en
5. Wang, L, and Chen, Y. Determinants of China's health expenditure growth: based on Baumol's cost disease theory. Int J Equity Health. (2021) 20:213. doi: 10.1186/s12939-021-01550-y
6. Zhou, W, Jian, W, Wang, Z, Pan, J, Hu, M, and Yip, W. Impact of global budget combined with pay-for-performance on the quality of care in county hospitals: a difference-in-differences study design with a propensity-score-matched control group using data from Guizhou province, China. BMC Health Serv Res. (2021) 21:1296. doi: 10.1186/s12913-021-07338-8
7. Guan, X, Zhang, C, Hu, H, and Shi, L. The impact of global budget on expenditure, service volume, and quality of care among patients with pneumonia in a secondary hospital in China: a retrospective study. BMC Public Health. (2020) 20:522. doi: 10.1186/s12889-020-08619-3
8. Gao, C, Xu, F, and Liu, GG. Payment reform and changes in health care in China. Soc Sci Med. (2014) 111:10–6. doi: 10.1016/j.socscimed.2014.03.035
9. Yu, J, Qiu, Y, and He, Z. Is universal and uniform health insurance better for China? Evidence from the perspective of supply-induced demand. Health Econ Policy Law. (2020) 15:56–71. doi: 10.1017/S1744133118000385
10. Shi, M, Wang, J, Zhang, L, Yan, Y, Miao, YD, and Zhang, X. Effects of integrated case payment on medical expenditure and readmission of inpatients with chronic obstructive pulmonary disease: a nonrandomized, comparative study in Xi County, China. Curr Med Sci. (2018) 38:558–66. doi: 10.1007/s11596-018-1914-1
11. Liu, S, Wang, J, Zhang, L, and Zhang, X. Caesarean section rate and cost control effectiveness of case payment reform in the new cooperative medical scheme for delivery: evidence from Xi County, China. Bmc Pregnancy Childbirth. (2018) 18:66. doi: 10.1186/s12884-018-1698-0
12. National Healthcare Security Administration. Notification about publishing the technical specification and catalogue scheme of the diagnosis-related groups payment (DRG) (in Chinese). (2019). Available at: (http://www.nhsa.gov.cn/art/2019/10/24/art_104_6464.html).
13. Yu, L, and Lang, J. Diagnosis-related groups (DRG) pricing and payment policy in China: where are we? Hepatobil Surg Nutr. (2020) 9:771–3. doi: 10.21037/hbsn-2020-8
14. Zhao, C, Wang, C, Shen, C, and Wang, Q. Diagnosis-related group (DRG)-based case-mix funding system, a promising alternative for fee for service payment in China. Biosci Trends. (2018) 12:109–15. doi: 10.5582/bst.2017.01289
15. Inke, M, and Friedrich, W. DRG-based payment systems in low- and middle-income countries: implementation experiences and challenges. World Health Organization (2012)
16. National Healthcare Security Administration. Notification about publishing the pilot implementation scheme of the regional points of global budget and the case-based payment methods (in Chinese). (2020). Available: (http://www.nhsa.gov.cn/art/2020/10/19/art_37_3752.html).
17. Lai, Y, Fu, H, Li, L, and Yip, W. Hospital response to a case-based payment scheme under regional global budget: the case of Guangzhou in China. Soc Sci Med. (2022) 292:114601. doi: 10.1016/j.socscimed.2021.114601
18. Qian, M, Zhang, X, Chen, Y, Xu, S, and Ying, X. The pilot of a new patient classification-based payment system in China: the impact on costs, length of stay and quality. Soc Sci Med. (2021) 289:114415. doi: 10.1016/j.socscimed.2021.114415
19. National Healthcare Security Administration. Notification about publishing the technical specification and catalogue of diseases of the diagnosis-intervention packet (DIP) payment for National Healthcare Security (in Chinese). (2020). Available at: (http://www.nhsa.gov.cn/art/2020/11/20/art_37_3987.html).
20. Shandong Provincial Bureau of Statistics. Shandong statistical yearbook 2021 (in Chinese) Jinan: China Statistics Press (2021).
21. Kim, H, Lee, JT, Fong, KC, and Bell, ML. Alternative adjustment for seasonality and long-term time-trend in time-series analysis for long-term environmental exposures and disease counts. BMC Med Res Methodol. (2021) 21:2. doi: 10.1186/s12874-020-01199-1
22. Jandoc, R, Burden, AM, Mamdani, M, Levesque, LE, and Cadarette, SM. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol. (2015) 68:950–6. doi: 10.1016/j.jclinepi.2014.12.018
23. Fuller, D, Sahlqvist, S, Cummins, S, and Ogilvie, D. The impact of public transportation strikes on use of a bicycle share program in London: interrupted time series design. Prev Med. (2012) 54:74–6. doi: 10.1016/j.ypmed.2011.09.021
24. Lopez Bernal, J, Cummins, S, and Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2016) 46:dyw098. doi: 10.1093/ije/dyw098
25. Zhai, T, Goss, J, Dmytraczenko, T, Zhang, Y, Li, J, and Chai, P. China's health expenditure projections to 2035: future trajectory and the estimated impact of reforms. Health Affair. (2019) 38:835–43. doi: 10.1377/hlthaff.2018.05324
26. National Healthcare Security Administration. Notification about enacting the implementation scheme of three years for reform of DRG/DIP payment methods (in Chinese). (2021). Available at: (http://www.nhsa.gov.cn/art/2021/11/26/art_37_7406.html).
27. Yan, J, Lin, HH, Zhao, D, Hu, Y, and Shao, R. China's new policy for healthcare cost-control based on global budget: a survey of 110 clinicians in hospitals. BMC Health Serv Res. (2019) 19:84. doi: 10.1186/s12913-019-3921-8
28. Dong, Y, Chen, J, Jing, X, Shi, X, Chen, Y, Deng, X, et al. Impact of capitation on outpatient expenses among patients with diabetes mellitus in Tianjin, China: a natural experiment. BMJ Open. (2019) 9:e24807. doi: 10.1136/bmjopen-2018-024807
29. Li, HM, Chen, YC, Gao, HX, Zhang, Y, Su, D, Chang, JJ, et al. Changes in inpatients' distribution and benefits under institution level-based quota payment for specific diseases in rural China: an interrupted time-series analysis. Int J Health Plan Manag. (2019) 34:e436–46. doi: 10.1002/hpm.2660
30. Feng, C, Meiyan, J, and Jianyun, Z. Payment mode of foreign medical insurance and its enlightenment (in Chinese). Chin J Pharmaceuticals. (2017) 48:936–42.
31. He, R, Miao, Y, Zhang, L, Yang, J, Li, Z, and Li, B. Effects of expanding outpatient benefit package on the rationality of medical service utilization of patients with hypertension: a quasi-experimental trial in rural China. BMJ Open. (2019) 9:e25254. doi: 10.1136/bmjopen-2018-025254
Keywords: case-based payment method, diagnosis-intervention packet (DIP) payment, inpatient care provision, interrupted time series analysis, China
Citation: Ding Y, Yin J, Zheng C, Dixon S and Sun Q (2023) The impacts of diagnosis-intervention packet payment on the providers’ behavior of inpatient care—evidence from a national pilot city in China. Front. Public Health. 11:1069131. doi: 10.3389/fpubh.2023.1069131
Received: 13 October 2022; Accepted: 12 May 2023;
Published: 01 June 2023.
Edited by:
Timotej Jagric, University of Maribor, SloveniaReviewed by:
Kazumitsu Nawata, Hitotsubashi University, JapanCopyright © 2023 Ding, Yin, Zheng, Dixon and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang Sun, cWlhbmdzQHNkdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.