- 1Public Health and Community Medicine Department, Faculty of Medicine, Cairo University, Manial, Cairo, Egypt
- 2Pediatric Department, Faculty of Medicine, Cairo University, Manial, Cairo, Egypt
- 3Pediatric Clinical Nutrition Department, National Nutrition Institute, Cairo, Egypt
- 4Public Health and Community Medicine Department, Faculty of Medicine, Port Said University, Port Said, Egypt
Introduction: Several studies in developing countries found that more need-based training is required for health care providers (HCPs) in child malnutrition management.
Methods: An exploratory cross-sectional study was conducted to explore barriers to providing adequate nutrition care as perceived by the healthcare providers (HCPs) in the child malnutrition clinic at a Children's University Hospital in Egypt. Participants were selected using the purposive sampling technique. Five out of seven HCPs in the clinic were included (two male physicians, one female physician, and two female nurses). Qualitative data were collected through in-depth interviews. The interview guide consisted of semi-structured open-ended questions. Quantitative data were the resulting scores from the scoring system used to assess the understandability and actionability of the patient education materials (PEMs) that are available in the clinic. The Patient Education Materials Assessment Tool for Printable Materials (PEMAT-P) for the scoring. Statistical analysis: The thematic content analysis technique was employed for qualitative data. The percent score was generated for the PEM actionability and understandability for quantitative data.
Results: Most common child malnutrition conditions encountered by HCPs were nutritional deficiencies. Barriers to the delivery of adequate nutrition care to children were physician-centered: limited nutrition education in the medical school, health system-centered: an insufficient number of HCPs, lack of nutritional supplements, lack of patient education materials (PEMs) that suit the characteristics of the served community, lack of updated standard of practice (SOP) and guidelines, inadequate nutrition training of HCPs, and insufficient time for each patient, and caregivers-centered: the low socioeconomic status and false cultural, nutritional beliefs.
Conclusion: There are different barriers to adequate nutrition care for child malnutrition in low-resource healthcare settings. Mainly nutritional deficiencies. Most of the barriers were health system-related in the form of insufficient resources (shortage of workforce; concerning the high caseload, nutritional supplements, and PEMs) and inadequate management of resources (lack of skill-based training, lack of updated SOP and guidelines, and lack of properly designed PEMs that facilitate communication with the target caregivers).
Introduction
Malnutrition during infancy and childhood may lead to impaired growth, delayed and improper social and cognitive development, low academic achievement, and later in life, reduced productivity (1).
Globally, malnutrition is still a significant cause of death and disease among children, especially those under 5 years (U5Y) of age. Undernutrition type of malnutrition is associated with 45% of child deaths.1 Most of those deaths take place in low- and middle-income countries that also have rising rates of childhood obesity (see text footnote 1).2 In 2020, 38.9 million children U5Y of age were overweight worldwide, 45.4 million were wasted, and 149.2 million were stunted (see text footnote 2). Stunting, which is defined by the World Health Organization (WHO) as a height that is more than two standard deviations below the median child's growth standards, is largely irreversible3 and associated with extremely high health and economic costs4 (2). Stunting is the impact of chronic malnutrition afflicting the child during the first 1,000 days of life. The number of stunted children is declining in all world regions except Africa (see text footnote 4).
Children's nutritional status is a powerful and sensitive indicator for assessing child health, food security, and the need to improve economic, environmental, and health policies (see text footnote 1). Although Egypt has achieved remarkable progress in child health in the past two decades, the country's U5Y child mortality rate in 2013 was below the Millennium Development Goal (MDG) 44 (see text footnote 4), (2) and far below Sustainable Development Goal (SDG) 2 (3)5. The prevalence of child malnutrition in Egypt is predominantly high, with 11% of infants born with a low birth weightweight (see text footnote 2), and 9.5% of children U5Y of age are underweight, which is higher than the average for Africa (6.0%), and 22% are stunted, which is the largest prevalence of stunting in the Middle East (see text footnote 4), (2, 3). Furthermore, stunted growth is a public health problem that has persisted in Egypt for a long time, as reported in EDHS 2014 (percent of stunted U5Y children was reported as 23, 23, 29, and 22% in the years 2000, 2005, 2008, and 2014, respectively) (3).
Educating the caregivers of children has been proven in many studies to not only increase their knowledge but also improve the health outcomes of these children (4–6). A systematic review to explore factors associated with successful nutrition education interventions for children showed that engaging parents through face-to-face education and identification of specific child's or parent's behaviors that needed to be modified were fundamental factors (7). Thus, the role of health care providers (HCPs) in educating caregivers is crucial to overcoming child malnutrition (8). Several studies in developing countries found that there is a need for more in-service, need-based, and skill-based training of HCPs involved in child malnutrition management.
The main objective of the present study was to explore barriers to providing adequate nutrition care services in the child malnutrition clinic to inform future service delivery strategies for managing child malnutrition, particularly in low-resource healthcare settings.
Materials and methods
Design and context of the study
The current study is a clinic-based exploratory cross-sectional study that used a qualitative approach. The study was conducted in the Center of Social and Preventive Medicine (CSPM) Malnutrition Clinic, Faculty of Medicine, Cairo University, Egypt, among HCPs (physicians and nurses) of the clinic.
The study was performed in accordance with the Consolidated Criteria for Reporting Qualitative Research CORE-Q (9).
Sampling technique and sample size
Participants were selected via a purposive sampling technique (10). The interviews were continued until they reached data saturation, where no new themes, subthemes, or explanations emerged from the interviews (11). Eligibility criteria were any HCPs (physicians and nurses) working in the CSPM malnutrition clinic during the study duration who were willing to participate. Out of seven HCPs, participants were five HCPs (two male physicians, one female physician, and two female nurses) because no new data were added starting from the third interview and saturation was achieved at the fifth interview. The interviewed physicians graduated between 1995 and 2001, and the interviewed nurses graduated in 1985 and 1990. One physician was a general practitioner; the other two were continuing their postgraduate studies in family medicine and pediatrics, respectively. The median number of working years mentioned by the HCPs was 6 years, ranging from 8 to 20 years.
Data types and collection tools
Qualitative data were collected through in-depth, audiotaped face-to-face interviews (each lasting up to 45 min) conducted by one of the researchers, who has experience conducting interviews and has worked on many qualitative studies. The interview guide (Appendix 1), which was pilot-tested beforehand, consisted of semi-structured, open-ended questions. The interview guide was developed following systematic literature reviews (3, 4, 6, 8, 12). A trained note-taker assisted the investigator in recording the sessions using a voice recorder and written notes. Quantitative data were the scoring system results used to assess the understandability and actionability of the educational leaflets distributed to caregivers by HCPs. For scoring, researchers used the Patient Education Materials Assessment Tool for Printable Materials (PEMAT-P) (13). The tool provides two scores for each material: a score for understandability and a separate score for actionability. The researchers scored the education material on each item of the material content, excluding the non-applicable (NA) items. Each item was given either 1 point (agree) or 0 points (disagree) (Tables 1A, B). First, the total points for the material items were summed up to calculate the score. Then, the sum was divided by the total possible points: the number of items on which the material was rated, excluding the items classified as NA. After that, the result was divided by 100 to get a percentage (%). This percentage score is the understandability score or the actionability score of the material on the PEMAT; the more understandable or actionable the material, the higher the score (13).

Table 1A. Assessment of printed patient education materials provided to caregivers in CSPM (using PEMAT-P): understandability.
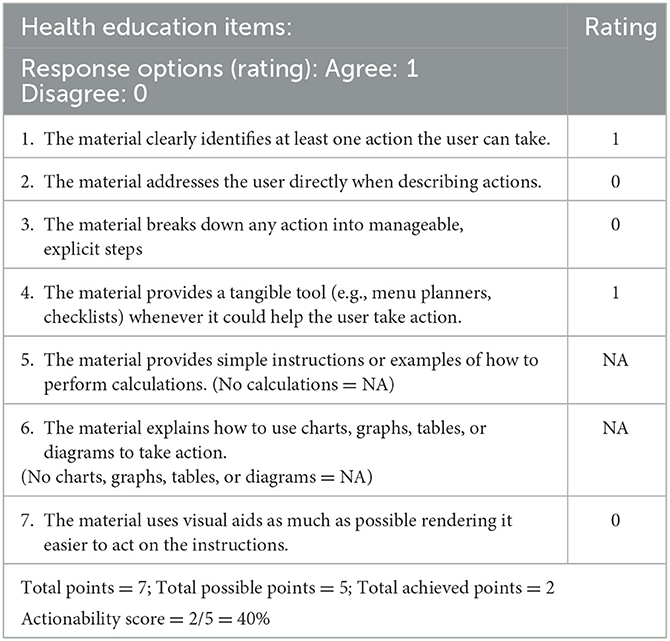
Table 1B. Assessment of printed patient education materials provided to caregivers in CSPM (using PEMAT-P): actionability.
Statistical analysis
For qualitative data
Data processing was based on the thematic content analysis technique (14, 15), which aims to get descriptions of the message content using a systematic and objective procedure. The thematic analysis is a three-stage analysis. The first stage involves understanding the idea through comprehensive and repeated readings of the data transcripts. The second stage is material exploration, which involves selecting the participants' statements and organizing them into categories (themes). The third stage deals with the processing and interpretation of results. The participants' quotations were used to clarify the meaning of the themes and summaries. Two investigators carried out the analysis. They read the transcript multiple times, made meaningful statements, and created themes and sub-themes.
For quantitative data
The PEMAT-P tool provides two scores for each material: a score for understandability and a separate score for actionability. The researchers scored the education material on each item of the material content, excluding the non-applicable (NA) items. Each item was given either 1 point (agree) or 0 points (disagree) (Tables 1A, B). First, the total points for the material items were summed up to calculate the score. Then, the sum was divided by the total possible points: the number of items on which the material was rated, excluding the items classified as NA. After that, the result was divided by 100 to get a percentage (%). This percentage score is the understandability score or the actionability score of the material on the PEMAT; the more understandable or actionable the material, the higher the score (13).
Ethical considerations
The study protocol was revised and approved by the Medical Research Committee in the Public Health and Community Medicine Department. All the study participants were treated according to the Helsinki Declaration of biomedical ethics (16). Written informed consent from each participant was obtained after proper orientation regarding the study objectives. Data confidentiality and informant privacy were upheld throughout the whole study. For each participant, we used “I” (interviewee) followed by a number per the chronological order of the interviews (I01, I02, I03..., etc.). The necessary municipal and federal authorities approved the study to be carried out. Using the voice recorder was authorized, and transcriptions of the recordings were performed.
Results
Qualitative data analysis results
By analyzing the qualitative data derived from the interviews, the researchers came up with the following themes:
• Views of HCPs toward malnutrition problems
HCPs mentioned that “the most frequent malnutrition problems that come to seeking medical advice were rickets, parasitism, underweight, kwashiorkor, and failure to thrive.”
Physicians mentioned that “laboratory investigation was the best method to assess the nutritional status.”
To improve the child's nutritional status, all HCPs confirmed the importance of “nutrition education, counseling, and provision of supplements such as iron and vitamin D” during infancy.
• Barriers to providing nutrition care to children
HCPs affirmed that there are three types of barriers that restrict providing quality medical nutrition care.
Physician-centered barriers
• Limited opportunities for applied/clinical nutrition education in medical schools
Physicians mentioned that “limited nutrition education in medical school and even in postgraduate studies (namely master's degree)” is the major challenge for gaining an adequate medical knowledge. Physicians said that “they learned the biochemistry of nutrition but not the basic nutrition knowledge needed to share with the patients.” They expressed dissatisfaction with their medical school education “We believe that we are ill-qualified to provide nutrition advice in the clinical setting.”
Furthermore, physicians explained that the nutrition course they received was not applicable to patients. As a result, they were not prepared to counsel caregivers. Some HCPs felt their clinical rotations did not prepare them for the prevention or management of childhood malnutrition from the nutritional aspect due to the limited experience of tutors in clinical nutrition.
Health system-centered barriers
These include barriers related to the resources and process components of the health system.
• Inadequate capacity building of HCPs in the workplace
Physicians expressed their views of inadequate nutrition training programs for physicians: “Training prepared us inadequately for work in low-resource settings.” One physician delineated his participation in training programs at the Faculty of Medicine, Cairo University. He said the first hospital training course started in June 2009 and included six sessions taught over 1 week. The training approach included theoretical educational sessions, practical training, demonstration exercises, group-based exercises, and case studies about breastfeeding. Another HCP received a nutrition course at the Ministry of Health in 2004, including four sessions taught over 2 days about growth monitoring. However, all respondents affirmed that they do not have access to regular refresher courses to reinforce their learning, provide practice demonstrations, and keep them up to date. In addition, they identified specific areas that are not satisfactorily covered in their nutrition education: nutrition counseling, infant and young children feeding, breastfeeding, and nutritional treatment of micronutrient deficiencies.
HCPs mentioned that training is significantly infrequent; that they hadn't received any nutrition care training in the past year. The most recent source of information they had about the contemporary infant feeding issues was the patients' handouts from the National Nutrition Institute. The only topic in which HCPs received training was exclusive breast feeding (EBF) where physicians and nurses have had similar exposure to training. Nurses attended more training than physicians. However, there is a rapid turnover of physicians and nurses, which makes such training needed continuously.
• Insufficient time to provide quality nutrition care
Physicians ascertained that they could not provide quality nutrition counseling in the CSPM malnutrition clinic due to the high caseload for the small number of physicians and nurses. Thus, they do not have enough time for growth monitoring or caregiver education on EBF, infant nutrition, sick children's nutrition, and pregnant women's nutrition. In addition, they added that there are too many patients per day, patient contact time is roughly 20–25 min long, and there are around 40 patients every day, except on Saturdays, on which there are even more patients.
Three HCPs said local women are always interested in hearing them talk and demonstrate rather than watching or reading visual materials independently. HCPs explained that with so little time spent with patients in the clinic, nutrition counseling is quite challenging. One physician said, “In my opinion, there are relatively few things that doctors can do to help set up the malnutrition clinic because malnutrition is a complex problem that necessitates behavioral intervention. However, there is not enough time for that,” and “Physicians focus on immediate medical concerns instead of the more long-term concern of childhood nutrition.”
• Shortage in the workforce and lack of motivation
HCPs cited a shortage in staffing as a barrier to meeting their clients health and nutrition needs. They all mentioned, “There has been no new recruitment of residents and nurses, no incentives or support in recognition of our hard work.” On the other hand, the low salary (1200 LE per month), insufficient opportunities for financial growth, and the lack of professional advancement increased the turnover rate of the already-appointed residents. Temporary contracts were used to hire all new doctors. The consensus among HCPs was that “There is a need for more service providers.”
• Shortage in logistics and supplies
HCPs demarcated the scarcity of visual PEM, resources for demonstrations for nurses regarding infant feeding, especially breastfeeding charts, posters (particularly those showing local foods in food groups and demonstrating proper hygienic practices), information leaflets, booklets, and picture information cards. In general, the availability of PEM for caregivers was suboptimal for all areas of child health except for child feeding starting at 6 months up to 9 years of age.
Weighing scales (for babies and pregnant women), stature measuring boards (for length and height), oral rehydration solution (ORS), and infant formula milk for infants in particular categories (6–24 months) were available. However, nutritional supplements such as iron, zinc, folic acid, and vitamin A were suboptimal and coupled with a marked shortage of PEM addressing micronutrient deficiencies.
There were no CSPM-specific guidelines or national protocols for the nutritional management of malnourished children. Only educational and instructional leaflets from the National Nutrition Institute for complementary feeding are available.
Caregivers-centered barriers
• Low socioeconomic status (SES)
HCPs recognize that “childhood malnutrition is a complicated problem influenced by numerous factors.” This concept makes HCPs understand that there are barriers facing caregivers face in trying to comply with nutritional advice. The most obvious barrier is the low SES status with subsequent limited access to healthy food and inability to recall the detailed medical advice provided.
Physicians mentioned that caregivers usually have limited nutrition knowledge, preventing them from selecting and preparing healthy complementary food. One HCP said, “Many parents who are unaware of what is and is not healthy for their children.”
• Culture and context:
Recognizing that people had prior specific cultural or traditionally-rooted beliefs is critical. This included the belief that breastfeeding after getting pregnant could cause kwashiorkor in the breastfed child. The potential conflict between health workers' counseling and cultural beliefs and perceptions is more general, extending beyond nutrition issues, and has been well known.
Suggestions of HCPs to improve performance in the malnutrition clinic
• Updating knowledge by continuing medical education (CME)
HCPs demanded more nutrition education, saying it could be provided through periodic rotations and seminars. One physician said, “We are provided periodic lectures on asthma; why we do not have lectures on nutritional therapy for malnutrition? Not only to teach us about malnutrition epidemiology, but to show us some of the techniques and resources we could need in the future, as well as to instruct us on how to deal with patients in the real world.”
One physician said, “To help parents improve their infants' nutrition, doctors must be aware of the specific advice they can give the caregivers regarding their infants' feeding—what, when, and how to feed.” HCPs expressed a need for specific hints on preparing healthy food that could be shared with patients. HCPs stated that they required evidence-based nutrition expertise in addition to patient-friendly information. They valued recommendations based on scientific literature.
HCPs mentioned the most needed topics to emphasize in education: “breastfeeding, complementary feeding for 6- to 24-month-old children, counseling skills, and communication skills.”
They recommended getting continuous support and training through nutrition seminars and the introduction of software programs on nutrition counseling to facilitate and ensure proper quality performance of HCPs in malnutrition management, such as history taking, diagnosis, and nutrition education and counseling, including standardization of the nutrition counseling process. In addition, the curriculum of undergraduate training for medical and nursing students should include applied nutrition.
• Counseling skills
HCPs affirmed the need for “more capacity-building in nutrition counseling” as practical training on counseling caregivers is crucial for learning by doing.
Four out of five interviewees believed that physicians and nurses have the greatest need to understand nutrition education, communication, and counseling because they are in direct contact with the target groups for nutrition care (mothers and children). In Egypt, the public and patients usually seek nutritional advice and counseling from physicians, who often lack nutrition knowledge.
Regarding service delivery, there was a consensus that CSPM clinics needed to be strengthened by providing them with the required staffing for nutrition care services, nutrition training facilities (e.g., a working nutrition kitchen), and PEM to support both preventive and curative nutrition care. HCPs expressed a willingness to provide quality services if the necessary resources were made available and the issue of a large caseload was addressed. They also suggested increasing the availability of dieticians in childcare clinics, including malnutrition clinics.
Counseling was a challenging demand as counselors, on the one hand, try to simplify messages to make them easily understandable, and simultaneously provide mothers with sufficient information to make informed choices.
• Guidelines for efficient and effective nutrition care service
Guidelines must be developed on values that match the SES and culture of the clients. Disregarding those aspects have numerous and severe drawbacks, including infeasibility/inapplicability of the medical recommendations, confusion among both mothers and HCPs, and harmful feeding practices with diets that are inadequate for meeting the nutritional needs of the children.
Quantitative data analysis results
The PEM provided to the caregivers at the malnutrition clinic was assessed using the PEMAT-P scoring tool regarding the understandability and actionability of the material.
The PEM had an understandability score of 54% and an actionability score of 40%, respectively (Tables 1A, B).
Discussion
The current study explores the barriers to providing adequate nutrition care to children as perceived by the workforce (HCPs) at the CSPM malnutrition clinic which exists in a law-resource setting (i.e., has minimal budget allocations and serves a low-SES community). Although this clinic is logistically, financially, and legally affiliated with the MOH, it is located at the Children's Hospital of the Faculty of Medicine, Cairo University. It is considered a reference center to which cases diagnosed as malnutrition are referred from the hospital clinics. The CSPM malnutrition clinic is considered a model center for managing children's malnutrition using nutritional supplements and nutrition education to caregivers. Therefore, the conduction of the current study was crucial to help in decision-making for improving performance in the CSPM malnutrition clinic.
The study delineated that the most frequent malnutrition problems encountered in the studied clinic were nutritional deficiencies, namely rickets, underweight, kwashiorkor, and failure to thrive. This finding is consistent with the existing evidence in Egypt as per the Egypt Demographic and Health Survey (EDHS) and other local studies (12). The evidence also demonstrates that the significant factors, namely poverty, low maternal education level, and lack of health and nutrition awareness among parents, contributing to the high prevalence of such nutritional problems are related to the low SES of children caregivers (3, 17).
The study revealed the barriers to providing adequate nutrition care in three broad themes: physician-centered, health system-centered, and caregiver-centered.
The physician-centered barriers included limited education in clinical nutrition, mainly applied practical tactics, in medical school during both the undergraduate and postgraduate programs. HCPs perceived this barrier as the primary barrier. Many studies assessing the situation of nutrition education in medical schools have reported both undergraduate and postgraduate nutrition curricula as insufficient with a limited capacity of learners to identify cases of malnutrition or provide nutrition education for patients (18–20). However, other studies suggested that there is no need for more nutrition education in medical schools. The only requirement is to train future medical professionals to understand the role of nutrition in health and to encourage them to refer patients for nutrition counseling with a registered nutritionist or registered dietitian who is more qualified to provide dietary advice due to their greater education, training, and experience (21). Nevertheless, physicians who lack the necessary nutrition training could postpone making the initial diagnosis of malnutrition cases with the subsequent delay in the referral of cases to nutritionists or dieticians (7, 22).
The WHO defined the health system as all organizations, people, and actions whose primary purpose is to promote, restore, and maintain health (23). Therefore, as with any system, health system components are resources (workforce, finances, technology, and information, including updated standard of practice (SOP) and guidelines, process (the way of resource management), and output (range of provided services, e.g., how many of the clients are covered with services).6 In our study, health system-centered barriers are related to the resources and process components of the health system.
There was a workforce shortage due to insufficient HCPs regarding the high caseload. Hence, it was not only the lack of or inadequate skills of HCPs that hindered the provision of adequate nutrition counseling but also the insufficient time available for each patient. Individual needs should be considered when developing and communicating nutrition advice (24). Accordingly, a full assessment and understanding of the patient's psychosocial needs require roughly 15 min longer than simply comprehending the patient's initial complaint (22, 25). With the limited time concerning the high caseload, it is impossible to set aside that time for a needs analysis or dietary counseling.
Our findings also revealed the failure of the CSPM administration to recruit more HCPs, retain the competent HCPs, or upgrade the nutrition-related knowledge and service delivery skills of the existing HCPs, e.g., through providing updated SOP or guidelines and conducting periodic skill-based training. This situation led HCPs to try gaining updated information, infrequently and irregularly, from another healthcare institute, such as the National Nutrition Institute (NNI) at Cairo University.
In addition, HCPs complained of a lack of motivation due to the absence of appropriate incentives. Although some studies found that financial incentives did not cause long term behavior changes among physicians (26), yet, several other studies affirmed that the financial and otherwise incentives influence the behavior of HCPs in various ways, including adjustments to their output volume and effectiveness, as well as the type and standard of services they provide to clients (27, 28).
Nutritional supplementation with adequate nutrition education is an evidence-based essential package of nutrition interventions, particularly in low SES communities. To be effective, this package should be delivered during key life stages, such as during pregnancy and throughout childhood (29, 30). Hence, the lack of health technology and supplies such as nutritional supplements and PEM was viewed by the HCPs as a significant barrier to delivering adequate nutrition care. Moreover, the quality of the existing PEM was described by the HCPs as inadequate. This was also confirmed by the low PEM understandability and actionability scores (50 and 40%, respectively) which were far below the lowest recommended level (70%) necessary for patients to understand or act on the information they receive from the material (13). This is expected because the communication section of the MOH, which produces these PEMs, does not pre-test most of the health education materials or update the channels of conveying them. For instance, short educational videos that convey important health messages in a simple and practical form are not available at all at the CSPM.
Similar health system-centered barriers were stated by physicians in several studies, such as the pivotal study conducted by Kushner in 1995 and another study conducted 15 years later (31, 32). Those studies found that the most significant barriers to providing quality nutrition service were the lack of incentives and time followed by the lack of updated knowledge. However, in our study, HCPs first stated the lack of updated knowledge and refreshing training. This may be because Egypt's health sector workforce policy permits HCPs to work in both the public and private health sectors, allowing HCPs to operate their private clinics and increase their income.
Unfortunately, the insufficient resource component of the health system is a commonly encountered barrier in many countries (8, 31, 32) because healthcare funds are skewed mainly toward treatment, with little funds directed toward nutrition education programs or malnutrition prevention in general (33, 34). However, the insufficient resources barrier in child nutrition care is more encountered in low-and-middle-income countries and usually negatively impacts children under five the most. This is unlike in higher-income countries where children who are negatively impacted in nutrition care are those older than 5 years of age, usually hospitalized, with the barriers related mainly to the process component of the health system (35). Economic growth has been widely considered an effective tool for mitigating poverty and improving public health (4, 33, 36). In Egypt, even though the total health expenditure- as an absolute number- is increasing, the total health expenditure as a percentage of the gross domestic product is declining. Also, the Egyptian healthcare market is mainly based on out-of-pocket payments (the expenses for healthcare that are not reimbursed by insurance) (5, 8, 37). Thus, considering the progressively declining SES of the Egyptian population, the Egyptian healthcare system, specifically the preventive sector, whose budget is the primary source of funds allocated for child nutritional care in the public sector, is facing extreme financial challenges (5, 38). Cost-effectiveness (determining the expected gains and cost per gain) is central to the health system's success. Therefore, health system resources should be directed to health services after making cost-effective analyses to decide on proper resource allocation, e.g., allocating resources for nutrition care technology, such as nutritional supplements, and specific community groups (39, 40).
Implications
The study focused on a significant public health problem in Egypt and most developing and underdeveloped countries, childhood malnutrition. This study tackled a crucial issue related to the crucial role of pediatric clinical nutrition services in overcoming such a problem. As well, the study provided valuable insight into barriers to providing adequate nutrition care to children. The identified barriers are essential when considering quality improvement of nutrition care practices for malnourished children.
Strengths
First; the study was conducted in a model malnutrition clinic in a Children's Hospital, presenting a prototypical solution to overcome children's malnutrition problems and their impact on growth and development. Second; the study was of a qualitative research nature and thus provided an in-depth understanding of barriers hindering the provision of adequate clinical nutrition services and counseling. Third; using a specific approach for testing the PEM added another dimension to the study, as it raised the importance of capacity building in designing and testing the PEM. And fourthly; the clinical nutrition concept was raised in the study for specific pediatric clinics. The same concept could be applied to other medical clinics.
Limitations
From our view, limitations of the study include that the study was conducted in one center, the only reference center for managing malnourished children. Additionally, as with any exploratory operations research, information derived from the study could not be generalized. However, the methodology used in the study could be generalized to be used in different medical settings. Furthermore, the views of the clients (caregivers) were not examined as it was beyond the scope of this study. Those views may have led to more understating of nutrition services' quality and barriers to adequate service. However, surprisingly, previous studies, such as one conducted in Bangladesh, showed that caregivers' satisfaction was above average despite the low quality of child nutritional services (27). The low expectations of the caregivers in the low SES communities could explain this. Similarly, a relatively high level of satisfaction could have been shown in this study for the same reason and because there are not many pediatric nutrition care clinics serving this district, making this clinic a unique one-of-a-kind center.
Recommendations
To overcome barriers to providing adequate care in malnutrition clinics, there are multifaceted approaches directed to upgrading the resources and process components of the health system as follows: Medical schools are encouraged to integrate clinical nutrition in the pediatrics curriculum of undergraduate and postgraduate medical students and nursing students. Also, the specialty of clinical nutrition should be introduced into the masters and doctorate degrees and clinical nutrition training agenda should be included in the continuous medical education program to improve nutrition-related knowledge, counseling skills, and capacity building in designing and testing health education materials. Furthermore, marketing for the unique health and nutrition services provided to children in the nutrition clinics motivates HCPs to work in such clinics and encourages decision-makers to improve resources, especially regarding nutritional supplements, to such clinics. Regarding MOH, we recommend the establishment of pediatric clinical nutrition fellowship programs, introducing clinical nutrition clinics in the primary health care facilities and hospitals, increasing the production and availability of nutritional supplements, particularly for children's most common nutritional deficiency problems, and producing adequately designed and tested PEMs that suit the sociodemographic characteristics of the served communities.
Conclusion
There are different barriers to adequate nutrition care for child malnutrition in low-resource healthcare settings. Mainly nutritional deficiencies. Most of the barriers were health system-related in the form of insufficient resources (shortage of workforce; concerning the high caseload, nutritional supplements, and PEMs) and inadequate management of resources (lack of skill-based training, lack of updated SOP and guidelines, and lack of properly designed PEMs that facilitate communication with the target caregivers).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Faculty of Medicine, Cairo University (N-139-2022). The patients/participants provided their written informed consent to participate in this study.
Author contributions
GE has made substantial contributions to the conception and design, analysis and interpretation of data, and writing the manuscript. MS has made substantial contributions to the acquisition of data and writing the manuscript. AT, SH, EA, and SI were involved in drafting the manuscript (Sections Methods and Results) and revising it carefully for important intellectual content and statistical analysis. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1064837/full#supplementary-material
Footnotes
1. ^Available online at: https://www.who.int/news-room/fact.sheets/detail/malnutrition (accessed June 2, 2021).
2. ^Available online at: https://www.who.int/publications/i/item/9789240025257 (accessed September 12, 2021).
3. ^Available online at: https://www.who.int/publications/i/item/WHO-NMH-NHD-14.3 (accessed December 20, 2021).
4. ^UNICEF Report. (2021). Available online at: https://www.who.int/publications/i/item/9789240025257 (accessed December 20, 2021).
5. ^Available online at: https://egypt.un.org/en/sdgs/2 (accessed May 21, 2022).
6. ^Available online at: https://healthmanager.ie/2011/03/the-differences-between-outputs-and-outcomes/ (accessed September 20, 2021).
References
1. Rashad AS, Sharaf MF. Economic growth and child malnutrition in Egypt: new evidence from national demographic and health survey. Soc Indic Res. (2018) 135:769–95. doi: 10.1007/s11205-016-1515-y
2. World Food Program (WFP) Report. Egypt Annual Country Report. (2021). Available online at: https://docs.wfp.org/api/documents/WFP-0000137873/download/ (accessed January 20, 2021).
3. Metwally AM, El-Sonbaty M, El Etreby LA, El-Din EMS, Hamid NA, Hussien HA, et al. Stunting and its determinants among governmental primary school children in Egypt: a school-based cross-sectional study. Open Access Maced J Med Sci. (2020) 8:650–7. doi: 10.3889/oamjms.2020.4757
4. Vollmer S, Harttgen K, Subramanyam MA, Finlay J, Klasen S, Subramanian S V. Association between economic growth and early childhood undernutrition: evidence from 121 demographic and health surveys from 36 low-income and middle-income countries. Lancet Glob Heal. (2014) 2:e225–34. doi: 10.1016/S2214-109X(14)70025-7
5. Fasseeh A, ElEzbawy B, Adly W, ElShahawy R, George M, Abaza S, et al. Healthcare financing in Egypt: a systematic literature review. J Egypt Public Health Assoc. (2022) 97:1–11. doi: 10.1186/s42506-021-00089-8
6. Salem M, Yousof H, Abdelmoneim O. Improvement of healthy diet related knowledge among a sample of Egyptian women in three upper Egypt governorates using a community-based intervention. Open Access Maced J Med Sci. (2019) 7:2947. doi: 10.3889/oamjms.2019.748
7. Mogre V, Stevens FCJ, Aryee PA, Amalba A, Scherpbier AJJA. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students' perspectives on barriers and strategies. BMC Med Educ. (2018) 18:1–11. doi: 10.1186/s12909-018-1130-5
8. Huntington D, Zaky HHM, Shawky S, Fattah FA, El-Hadary E. Impact of a service provider incentive payment scheme on quality of reproductive and child-health services in Egypt. J Health Popul Nutr. (2010) 28:273. doi: 10.3329/jhpn.v28i3.5556
9. Booth A, Hannes K, Harden A, Noyes J, Harris J. COREQ Guidelines for Reporting Health Research: A User's Manual. Oxford: John Wiley & Sons Ltd. (2014). p. 214–26.
10. Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Quality Quantity. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
11. Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. (2015) 20:1408–16. doi: 10.46743/2160-3715/2015.2281
12. Farahat Taghreed M, Ragab Seham, Salama Aml A, Abdel El Halim Hend N. Prevalence of stunted growth in children less than 5-year old in Qualyoubia governorate. Menoufia Med J. (2017) 30:1089–92. doi: 10.4103/mmj.mmj_158_17
13. Shoemaker SJ, Wolf MS, Brach C. Development of the Patient Education Materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns. (2014) 96:395–403. doi: 10.1016/j.pec.2014.05.027
14. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
15. Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. (2020) 48:592–8. doi: 10.1016/j.ajic.2020.03.018
16. Carlson VR, Boyd KM, Webb DJ. The revision of the Declaration of Helsinki: past, present and future. Br J Clin Pharmacol. (2004) 57:695–713. doi: 10.1111/j.1365-2125.2004.02103.x
17. Sharaf MF, Mansour EI, Rashad AS. Child nutritional status in Egypt: a comprehensive analysis of socioeconomic determinants using a quantile regression approach. J Biosoc Sci. (2019) 51:1–17. doi: 10.1017/S0021932017000633
18. Devries S, Willett W, Bonow RO. Nutrition education in medical school, residency training, and practice. JAMA. (2019) 321:1351–2. doi: 10.1001/jama.2019.1581
19. Mihalynuk T V, Coombs JB, Rosenfeld ME, Scott CS, Knopp RH. Survey correlations: proficiency and adequacy of nutrition training of medical students. J Am Coll Nutr. (2008) 27:59–64. doi: 10.1080/07315724.2008.10719675
20. Adams KM, Lindell KC, Kohlmeier M, Zeisel SH. Status of nutrition education in medical schools. Am J Clin Nutr. (2006) 83:941S−4S. doi: 10.1093/ajcn/83.4.941S
21. Jones G, Macaninch E, Mellor DD, Spiro A, Martyn K, Butler T, et al. Putting nutrition education on the table: development of a curriculum to meet future doctors' needs. Br J Nutr. (2022) 1–9. doi: 10.1017/S0007114522001635
22. Adamski M, Gibson S, Leech M, Truby H. Are Doctors Nutritionists? What Is the Role of Doctors in Providing Nutrition Advice? Wiley Online Library (2018). doi: 10.1111/nbu.12320
23. Arteaga O. Health Systems. In:Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer (2014).
24. Bauer KD, Liou D. Nutrition Counseling Education Skill Development. Cengage Learning (2020). Available online at: https://books.google.com.eg/books?hl=en&lr=&id=DozKDwAAQBAJ&oi=fnd&pg=PP1&dq=24.+Bauer+KD,+Liou+D.+Nutrition+Counseling+and+Education+Skill+Development.+Cengage+Learning+(2020).&ots=2JTlbLxnX3&sig=nIWza46fGIP76oWP4TVdiRlTwLE&redir_esc=y#v=onepage&q=24.%20Bauer%20KD%2C%20Liou%20D.%20Nutrition%20Counseling%20and%20Education%20Skill%20Development.%20Cengage%20Learning%20(2020).&f=false
25. Michie S, Stralen MV, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:1–2. doi: 10.1186/1748-5908-6-42
26. Chauhan BF, Jeyaraman M, Mann AS, Lys J, Skidmore B, Sibley KM, et al. Behavior change interventions and policies influencing primary healthcare professionals' practice—an overview of reviews. Implement Sci. (2017) 12:1–6. doi: 10.1186/s13012-016-0538-8
27. Billah SM, Saha KK, Khan AN, Chowdhury AH, Garnett SP, Arifeen SE, et al. Quality of nutrition services in primary health care facilities: implications for integrating nutrition into the health system in Bangladesh. PLoS ONE. (2017) 12:e0178121. doi: 10.1371/journal.pone.0178121
28. Lazear EP. Compensation and incentives in the workplace. J Econ Perspect. (2018) 32:195–214. doi: 10.1257/jep.32.3.195
29. Vaivada T, Gaffey MF, Das JK, Bhutta ZA. Evidence-based interventions for improvement of maternal and child nutrition in low-income settings: what's new? Curr Opin Clin Nutr Metab Care. (2017) 20:204–10. doi: 10.1097/MCO.0000000000000365
30. Stephenson J, Heslehurst N, Hall J, Schoenaker DA, Hutchinson J, Cade JE, et al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet. (2018) 391:1830–41. doi: 10.1016/S0140-6736(18)30311-8
31. Kolasa KM, Rickett K. Barriers to providing nutrition counseling cited by physicians: a survey of primary care practitioners. Nutr Clin Pract. (2010) 25:502–9. doi: 10.1177/0884533610380057
32. Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prevent Med. (1995) 24:546–52. doi: 10.1006/pmed.1995.1087
33. Wang F. The roles of preventive and curative health care in economic development. PLoS ONE. (2018) 13:e0206808. doi: 10.1371/journal.pone.0206808
34. Segal J,. Why Don't We Fund More Prevention. Social Finance (2019). Available online at: https://socialfinance.org/blog/why-dont-we-fund-more-prevention/
35. Paulsen MM, Varsi C, Paur I, Tangvik RJ, Andersen LF. Barriers and facilitators for implementing a decision support system to prevent and treat disease-related malnutrition in a hospital setting: qualitative study. JMIR Format Res. (2019) 3:e11890. doi: 10.2196/11890
36. Dfid GB. Growth: Building Jobs and Prosperity in Developing Countries. London: Department for International Development (2008).
37. Pande A, El Shalakani A, Hamed A. How can we measure progress on social justice in health care? The case of Egypt. Health Syst Reform. (2017) 3:14–2 doi: 10.1080/23288604.2016.1272981
38. World Bank Group. Understanding Poverty and Inequality in Egypt: Background Papers (2019). Available online at: https://policycommons.net/artifacts/1280775/understanding-poverty-and-inequality-in-egypt/1872761/
39. Floreskul V, Juma FZ, Daniel AB, Zamir I, Rawdin A, Stevenson M, et al. Cost-effectiveness of Vitamin D supplementation in pregnant woman and Young children in preventing rickets: a modeling study. Front Public Health. (2020) 8:439. doi: 10.3389/fpubh.2020.00439
40. Cylus J, Papanicolas I, Smith PC, World Health Organization. Health System Efficiency: How to Make Measurement Matter for Policy and Management. World Health Organization. Regional Office for Europe (2016). Available online at: https://apps.who.int/iris/handle/10665/326305
Keywords: malnutrition, low-resource healthcare settings, skill-based training, updated standard of practice, guidelines, nutritional supplements, patient education materials
Citation: Elhady GW, Ibrahim Sk, Abbas ES, Tawfik AM, Hussein SE and Salem MR (2023) Barriers to adequate nutrition care for child malnutrition in a low-resource setting: Perspectives of health care providers. Front. Public Health 11:1064837. doi: 10.3389/fpubh.2023.1064837
Received: 08 October 2022; Accepted: 14 February 2023;
Published: 09 March 2023.
Edited by:
Terry Huang, City University of New York, United StatesReviewed by:
Kumar Gaurav Chhabra, NIMS University, IndiaFarooq Ahmed, Quaid-i-Azam University, Pakistan
Copyright © 2023 Elhady, Ibrahim, Abbas, Tawfik, Hussein and Salem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ghada Wahby Elhady, Z3dlbGhhZHlAa2FzcmFsYWlueS5lZHUuZWc=
 Ghada Wahby Elhady
Ghada Wahby Elhady Sally kamal Ibrahim2
Sally kamal Ibrahim2 Enas S. Abbas
Enas S. Abbas Marwa Rashad Salem
Marwa Rashad Salem