- 1Department of Nutrition and Dietetics, School of Allied Health Sciences, University of Health and Allied Sciences, Ho, Ghana
- 2Department of Dentistry and Surgery, School of Medicine, Nantong University, Nantong, China
- 3Department of Clinical Medicine, School of Medicine, Fujian Medical University, Fuzhou, China
- 4Department of Pharmaceutics, School of Pharmacy, Nantong University, Nantong, China
- 5Department of Midwifery, School of Nursing and Midwifery, University of Health and Allied Sciences, Ho, Ghana
- 6Department of Community Health Nursing, Nurses Training College, Ho, Ghana
- 7Department of Public Administration and Health Services Management, School of Business, University of Ghana, Accra, Ghana
- 8Global Health and Infectious Diseases Group, Kumasi Centre for Collaborative Research in Tropical Medicine, Kumasi, Ghana
Background: Neonates are at a greater risk of infection, but data on the maternal knowledge and practice of infection prevention in neonates (IPNs) are scarce. This study aimed to assess sociodemographic characteristics and reproductive health factors associated with maternal knowledge and practice of IPNs in North Dayi District, Ghana.
Methods: This was a multicenter cross-sectional study conducted among 612 mothers. A structured questionnaire was used for data collection adapted from previous studies and the IPN guidelines of the World Health Organization (WHO). Bivariable analyses were performed to determine the association between maternal knowledge and practice of IPNs and sociodemographic characteristics and reproductive health factors.
Results: Analysis showed that less than one-fifth of the mothers (12.9%) had poor knowledge of IPNs, while 21.6% incorrectly practiced it. Mothers who had poor knowledge of IPNs [adjusted odds ratio (AOR) = 13.33 (95% CI: 7.69–23.26), p < 0.001] were more likely to have a poor practice of IPNs.
Conclusion: About one-fifth of the mothers in this study had poor knowledge or poor practice of IPNs according to the WHO’s guidelines. The Health Directorate of North Dayi District should explore the risk factors associated with poor IPNs and increase successful guideline adherence with intensified educational outreach and campaigns.
Introduction
Globally, the WHO report of 2020 showed that an estimated 2.4 million neonatal deaths occurred in the first month of newborn life (1). Of these, 43% occurred in developing countries, mostly in Sub-Saharan Africa (SSA), followed by 36% in central and southern Asia (1). Neonatal infection (35.8%) is the major cause, followed by prematurity (27.5%) and other birth complications (22.9%) during the neonatal period (2, 3). Neonatal infection refers to sepsis involving the bloodstream in newborns less than 28 days old (1, 4). Without a substantial reduction in infection-related neonatal deaths in developing countries, it is questionable that the Sustainable Development Goal (SDG), which targets the reduction of neonatal mortality to at least 12 per 1,000 live births by 2030, will be met (5).
The WHO recommends the following measures to prevent neonatal death: ANC visits (a minimum of eight), skilled delivery, and PNC visits (a minimum of three) (1, 2, 4). Other recommendations of the WHO include immunization against tetanus, education on neonatal danger signs and skilled care such as thermal care, cord care, breastfeeding, and bathing of neonates (1, 2, 4). Additionally, the WHO endorses that babies who are delivered at home should be visited by healthcare professionals on the day of birth (1, 2). Studies have shown that home deliveries may pose serious complications for babies because of the traditional care they receive from relatives and traditional birth attendants (6–8).
Despite this, the high incidence of neonatal death can be prevented by proper infection prevention in neonates (IPNs) (1). IPNs refer to a comprehensive approach intended to improve the health of neonates from pregnancy through childbirth and the postnatal phase (4). Studies have found an association between the knowledge of mothers (2, 4–6, 9–13) and the practice of mothers (2, 7–9, 14–17) and IPNs. Other studies have shown sociodemographic characteristics (mother age (14, 18), marital status (8) educational status (6–8, 11, 16, 19), income level (6, 9, 15, 16), employment status (2, 5, 8, 10), type of residence (4, 8, 20) and access to media (19, 20)) and reproductive health factors [parity (9, 10, 12, 15, 16, 20), number of ANC visits (2, 4, 9–11, 15, 19), place of delivery (2, 9, 15), number of PNC visits (2, 4, 6, 9, 19), and walking distance (9)] to be associated with IPNs.
In Ghana, despite the extra effort and measures adopted to improve IPNs, the status among mothers is still a major concern (5, 14). Studies performed in Ghana have found poor knowledge (5), poor practice (14), home delivery (2), and less than minimum attendance of ANC and PNC according to WHO recommendations (2) as major concerns of IPNs. In the North Dayi District, the levels and factors associated with IPNs had not been studied, and no studies were found for comparison, despite the steady rise of neonatal deaths attributed to infection in the district. It is necessary to conduct a study in which the findings will add to the literature and serve as useful information for educating mothers on IPNs to reduce the rates of neonatal mortality in North Dayi District and beyond. Hence, this study aimed to assess the sociodemographic characteristics and reproductive health factors associated with maternal knowledge and practice of IPNs in North Dayi District, Ghana.
Materials and methods
Study design and setting
A multicenter cross-sectional study was conducted between June 2020 and August 2020 in North Dayi District, Ghana. The North Dayi District is one of the 261 Metropolitan, Municipal and District Assemblies (MMDAs) in Ghana and forms part of the 18 municipalities and districts in the Volta Region. The North Dayi District was established by the Legislative Instrument (LI) 2076 of 2012. Its capital is Anfoega. It borders Kpando municipality to the north, South Dayi District to the south, and Afazato South District to the east (21). The total population is 39,913, representing 46.7% males and 53.3% females. The villages include Anfoega, Vakpo, Wusuta, Tsrukpe, Botoku, Tsoxor, Awate, Aveme, and Tsyome Sabadu. The study design provides an accurate report of IPNs among mothers through the analysis and interpretation of the questionnaire-based survey. Additionally, it is suitable, reduces cost and saves time for conducting the study (Figure 1).

Figure 1. Map showing the North Dayi district where the study was conducted in the Volta Region, Ghana.
Eligibility criteria
Included were mothers who visited the various facilities with babies aged less than a year and consented to participate in the study. The reason for the inclusion of mothers having babies aged less than a year was based on the 2020 WHO report that babies who die within the first 28 days of birth suffer from conditions associated with a lack of quality care (1). Excluded were mothers who visited the various facilities with babies aged at least a year or above, those unable to communicate properly and those who disagreed to take part in the study.
Study population and sample size
Mothers who visited the various facilities had babies who were less than a year old. On average, these are the numbers of mothers who visited the various facilities during the study period. Aveme Danyigba Health Centre (n = 187), Tsyome Sabadu Health Centre (n = 190), Awate Health Centre (n = 205), Tsrukpe Health Centre (n = 194), Botoku Health Centre (n = 180), Vakpo Health Centre (n = 210) and Wusuta Health Centre (n = 185). In 1 month, the total monthly attendance was 1,351. Yamane’s formula n = N/1 + N(e2) (22) was used to calculate the sample size, where n = sample size, N = population size, e = margin of error (5%), plus 10% nonresponse, and an estimated sample size of 339 was obtained. This sample size was distributed proportionally across the various facilities to avoid bias during the data collection.
Sampling technique and procedure
Data collection was performed systematically to reduce the effects of bias. Thus, the study population was divided by the estimated sample size, r = N/n = 1351/339 = 3.985, to obtain a fraction that was approximated to four. In every facility, the first mother and, sequentially, every fifth mother thereafter were sampled to participate in the study. The data collection commenced with the first through to the fifth mother at the various facilities. It continued until the last mother in attendance was served. A total of 659 questionnaires were administered face-to-face, with 612 (92.9%) fully answered and used for the analysis.
Data collection tool
A structured questionnaire was designed and divided into three sections. It was adapted from previous studies (2, 4, 6, 7, 9–11, 18). The questions on the knowledge and practice of IPNs were also adapted from previous studies (2, 4, 6, 7, 9–11, 18) and standardized according to the IPN guidelines of the WHO (23, 24). Section 1: sociodemographic characteristics (mother’s age, marital status, educational status and income level), reproductive health factors (parity, number of ANC visits, gestational age, place of last delivery, baby’s condition after birth and number of PNC visits). Section 2: Knowledge of IPNs. Section 3: Practice of IPNs.
Assessment of knowledge and practice of infection prevention In neonates
These sections of the questionnaire comprised 20 closed-ended questions. Ten questions for each on knowledge of IPNs with three responses (“True,” False,” and “Do not know”) and on the practice of IPNs with three answers (“Yes,” “No,” and “Not sure”). The correct answer on knowledge or practice of IPNs was given 1 point, and the incorrect answer was awarded 0 points (including “Do not know” or “Not sure”). The “do not know” and “not sure” responses were included to avoid biases in answering the questions (25). A cumulative percentage method of assessment was used to score the answers and rounded up to 100%. Cumulative scores of <70% of the correct answers were considered “poor,” and cumulative scores of ≥70% were considered “good” (2, 6).
Operational definitions
Good knowledge of IPNs: Mothers who scored at least 70% out of 10 questions on knowledge adapted from IPN guidelines of the WHO. Poor knowledge of IPNs: Mothers who scored less than 70% out of 10 questions on knowledge adapted from IPN guidelines of the WHO. Good practice of IPNs: Mothers who scored at least 70% out of 10 questions on practice adapted from IPN guidelines of the WHO. Poor practice of IPNs: Mothers who scored less than 70% out of 10 questions on practice adapted from IPN guidelines of the WHO.
Validity and reliability
To ensure validity, the questionnaire was designed in consultation with experts in the field to adequately address all aspects of the issues being studied. To ensure reliability, the questionnaire was pretested on 5% of the sample size at Ve Dafor Health Center. The questions were then revised after the pretest to ensure correct wording, clarity, transparency, simplicity and proper rephrasing to ensure the collection of consistent and reliable data.
Data quality assurance
After validating and pretesting the questionnaire, the data were collected by trained research assistants through face-to-face interviews. The questionnaire was initially designed in English but translated into the local languages (Ewe and Twi) of the mothers when necessary during the process of data collection. The data collected were cross-checked for consistency and completeness and kept with the principal researcher.
Data analysis
Data collected were double-checked for completeness and entered into the Excel spreadsheet 2013. It was imported into Statistical Package for Social Sciences (version 25.00) for analysis. Descriptive data are presented as frequencies and percentages. Bivariable analyses were performed to determine the association between the knowledge and practice of IPNs and the mother’s sociodemographic characteristics and reproductive health factors. We considered it appropriate to set statistical significance as p < 0.01 instead of p < 0.05. With a p-value of <0.05, there is a 1 in 20 chance that a variable will appear to be significant when it is not and purely by chance because we are testing for many explanatory variables. Significant variables (p < 0.01) in the bivariable analyses were included in multivariable logistic regression. In the multivariable logistic regression, a p < 0.01 was considered significant.
Ethical considerations
Approval was sought from the North Dayi District, Ghana Health Service with the identification number (NDDHD/GR/002/20) on 11/06/2020 and the management of the health facilities. The introduction was made by research assistants, and consent was sought from each mother by their thumbprint. The aims of the study were explained to the mothers, and approval was granted for the data collection. Privacy and confidentiality were ensured by filling out the questionnaire individually without asking for private information.
Results
Sociodemographic characteristics and reproductive health factors
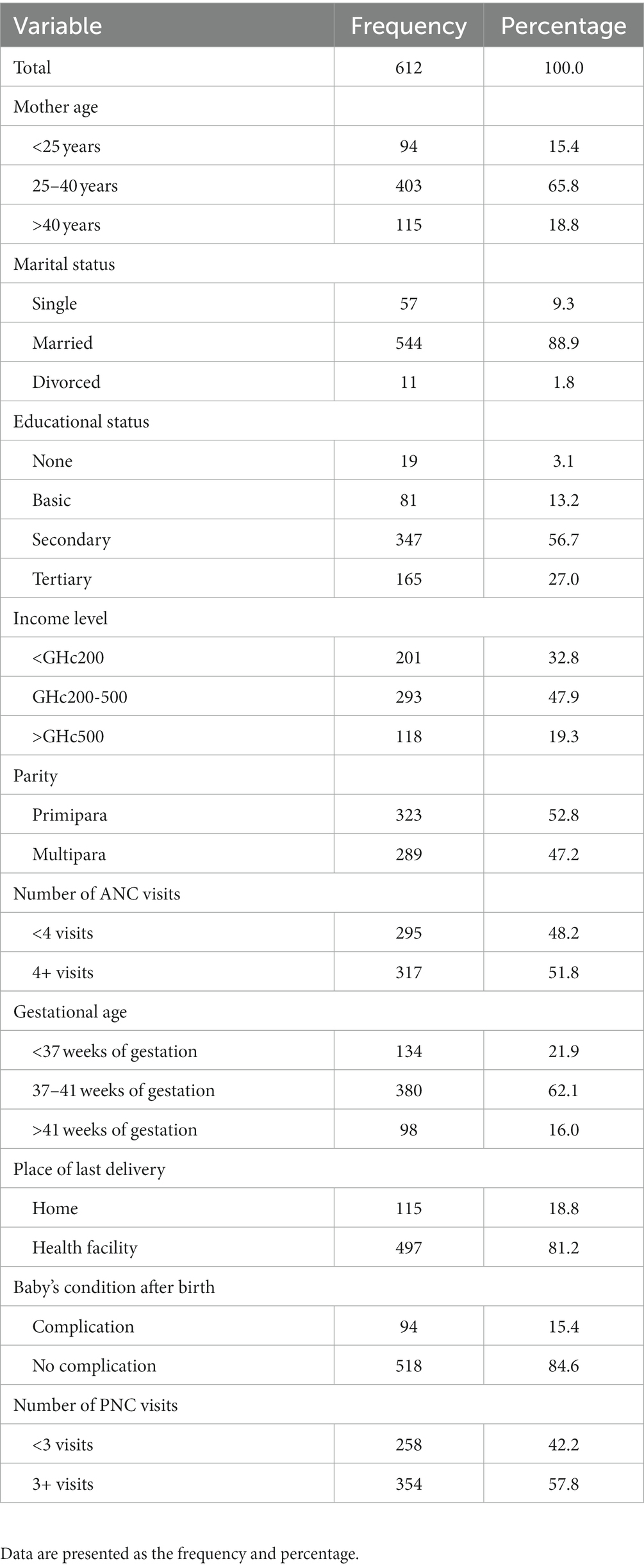
A total of 612 mothers were included as respondents in the study. The majority (65.8%) were between the ages of 25 and 40 years. About 88.9% were married. Over half (n = 347) had attained secondary education. Forty-eight percent earned an income between GHc200 and 500 GHc. More than half (52.8%) were primiparous mothers. About 51.8% had visited ANC four times or more. The majority (62.1%) had delivered between 37 and 41 weeks of gestation. Over three-quarters (n = 497) had delivered at the health facilities. Approximately 85 % had babies without complications after birth. Fifty-eight percent (n = 354) had attended PNC three times or more (Table 1).
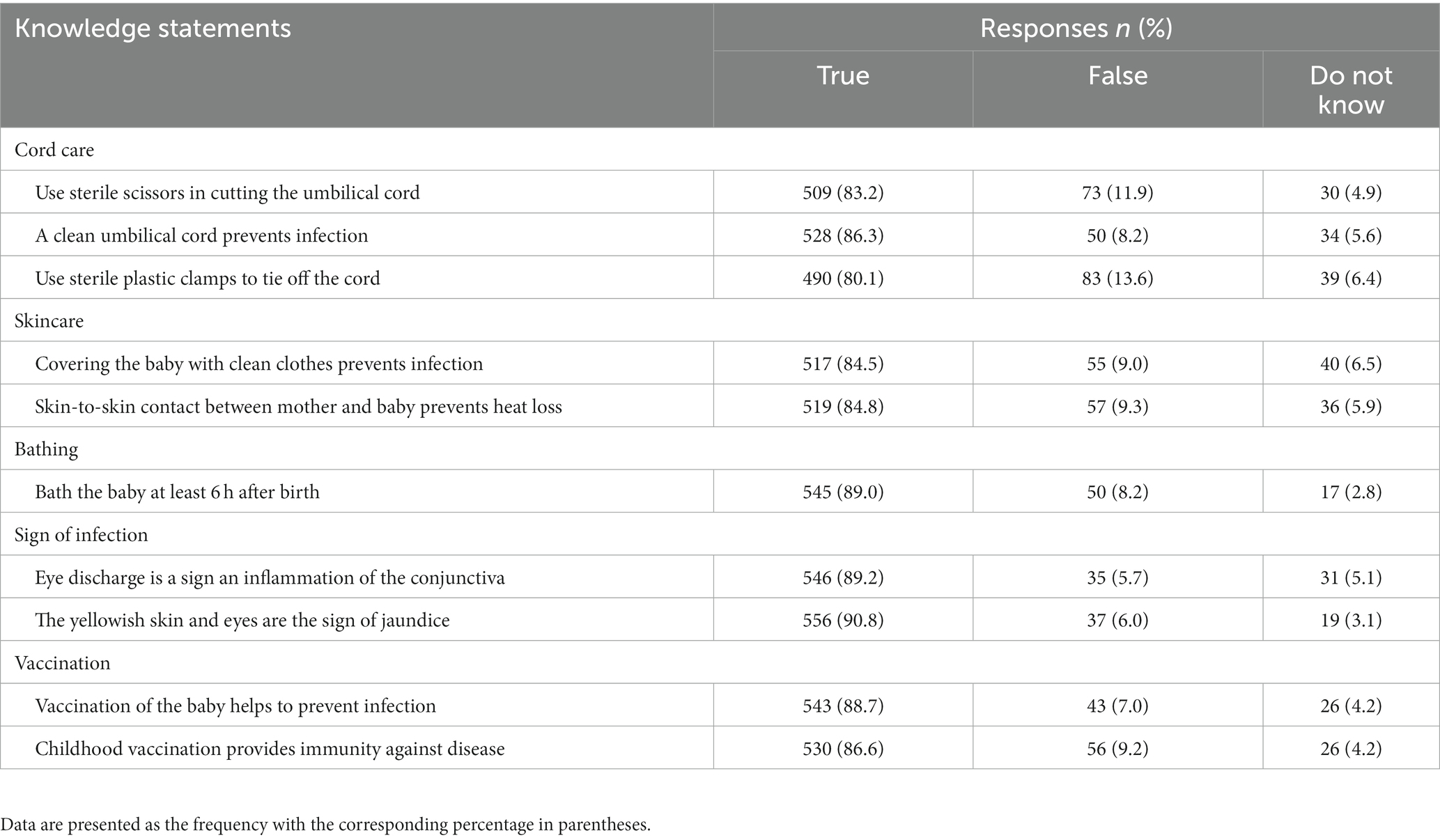
Knowledge of infection prevention in neonates
Over three-quarters (83.2%) knew that sterile scissors should be used in cutting the umbilical cord. The majority (86.3%) knew that a clean umbilical cord prevents infection. Approximately 80 % were aware that sterile plastic clamps should be used to tie off the cord. The majority (n = 517) knew that babies covered with clean clothes prevented infection. Over half (84.8%) knew that skin-to-skin contact between the mother and baby prevents heat loss. Eighty-nine percent knew that babies could be bathed at least 6 h after birth. About 89.2% were aware that eye discharge is a sign of inflammation of the conjunctiva. More than half (n = 556) knew that yellowish skin and eyes were signs of jaundice. More than three-quarters (88.7%) knew that vaccination of the baby helps to prevent infection. The majority (86.6%) knew that childhood vaccination provides immunity against disease (Table 2).
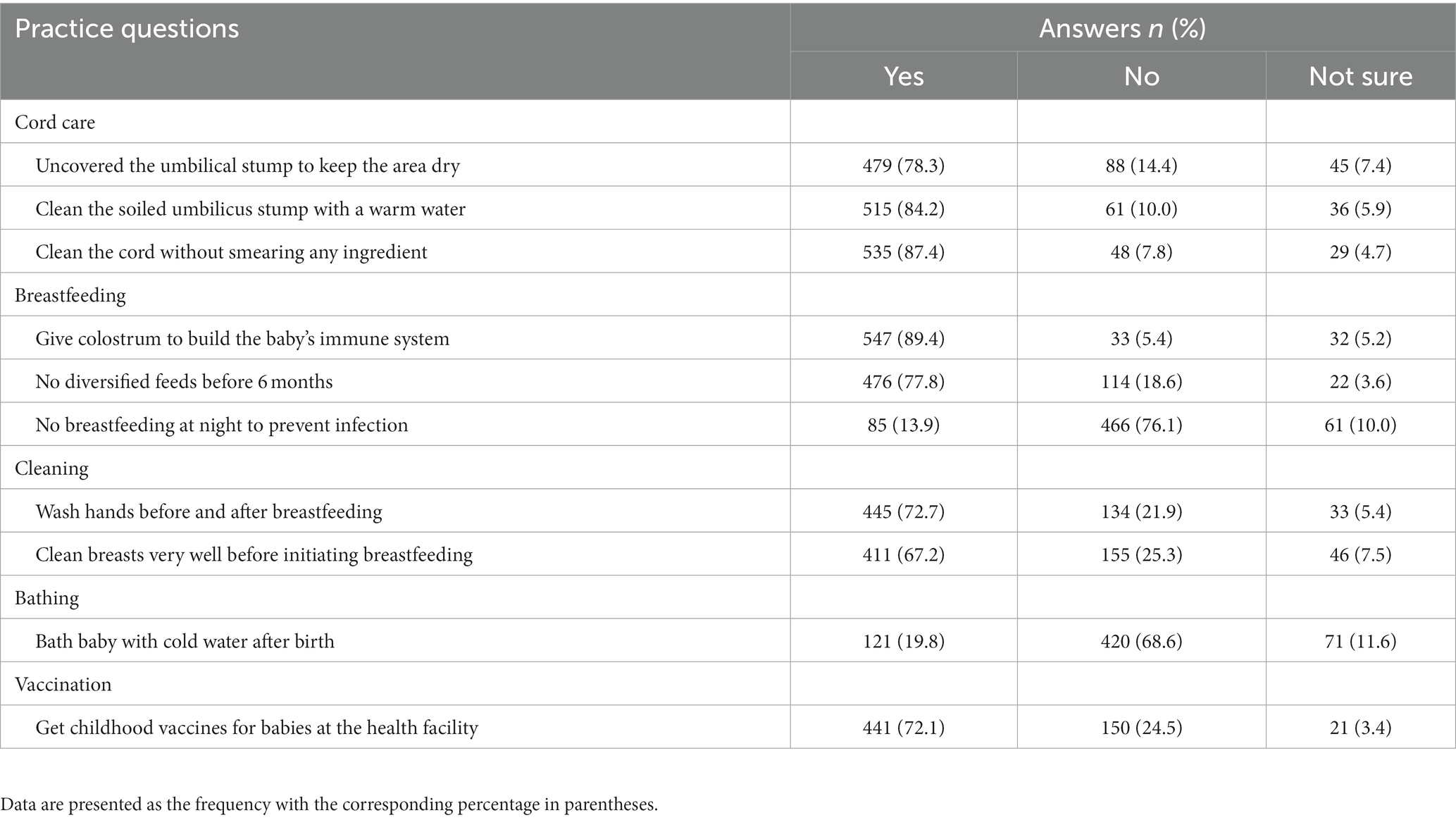
Practices of infection prevention in neonates
The majority (78.3%) uncovered the umbilical stump to keep the area dry. Over three-fourths (n = 515) cleaned the soiled umbilical stump with warm water. More than three-quarters (n = 535) cleaned the cord without smearing any ingredient. The majority (89.4%) gave colostrum to build the baby’s immune system. Over half (77.8%) practiced no diversified feeding before 6 months. About 76.1% breastfed at night to prevent infection. Approximately 73% washed their hands before and after breastfeeding. Over two-thirds (n = 411) cleaned their breasts very well before initiating breastfeeding. More than half (n = 420) bathed their babies with cold water after birth. The majority (72.1%) received childhood vaccines for babies at the health facility (Table 3).
Levels of maternal knowledge and practices of infection prevention in neonates
Less than one-fifth (12.9%) and (21.6%) of the mothers had poor knowledge and poor practices of IPNs, respectively.
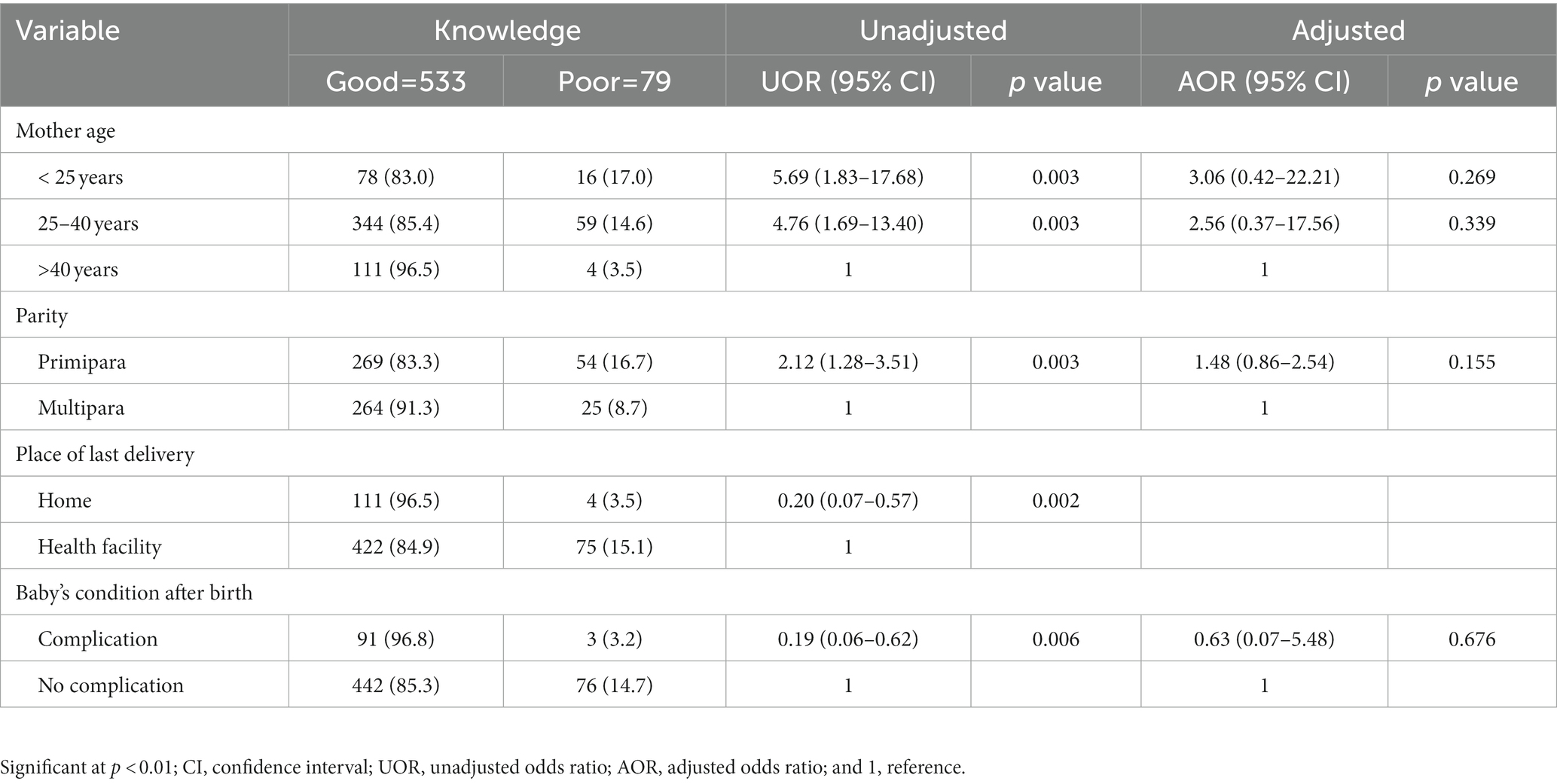
Factors associated with knowledge of infection prevention in neonates
The study found significant differences in the levels of knowledge of IPNs with age, parity, place of current delivery and baby’s condition after birth (p < 0.01; Table 4). In the multivariable analyses, none of these variables was statistically significant (p < 0.01; Table 5).
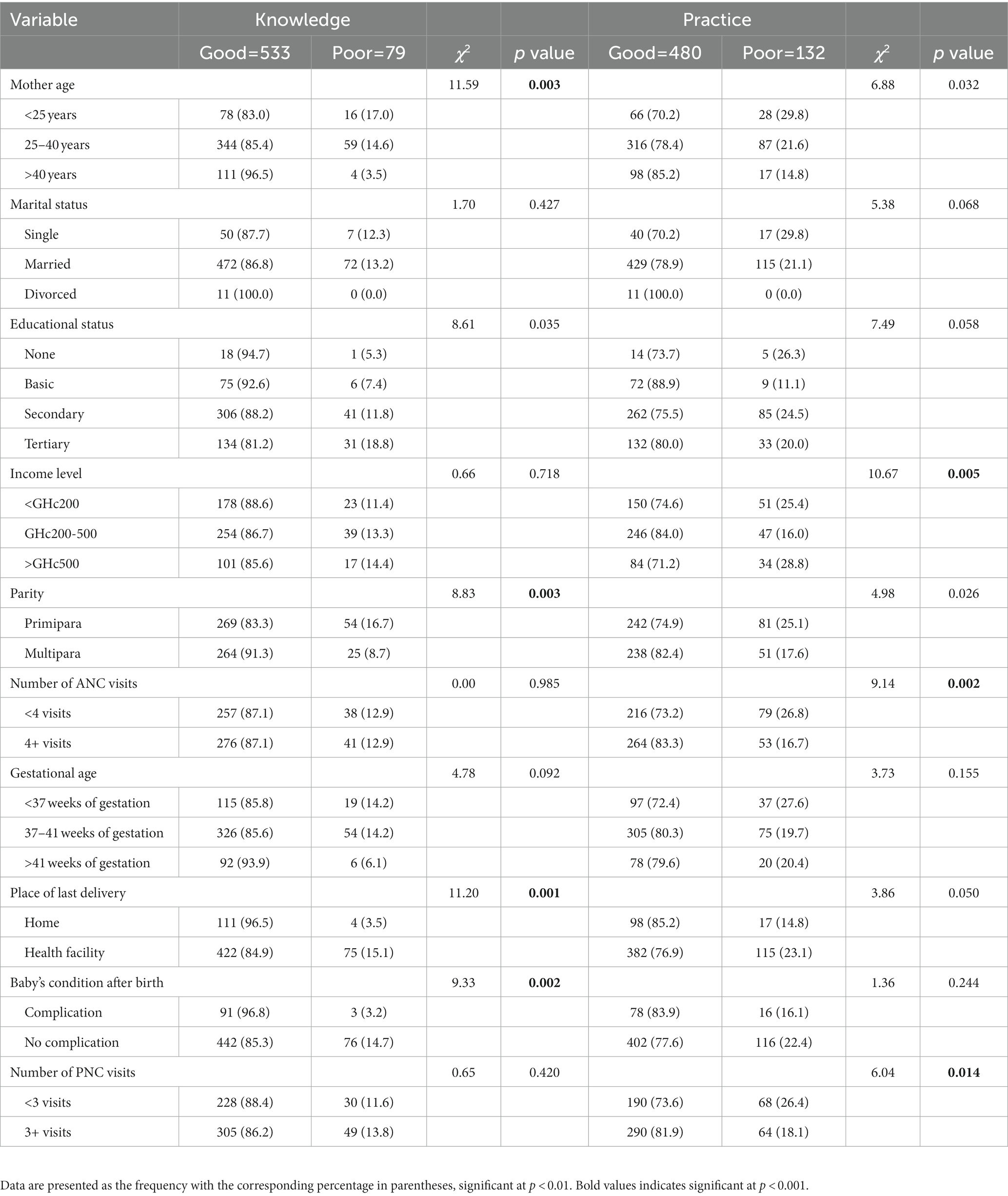
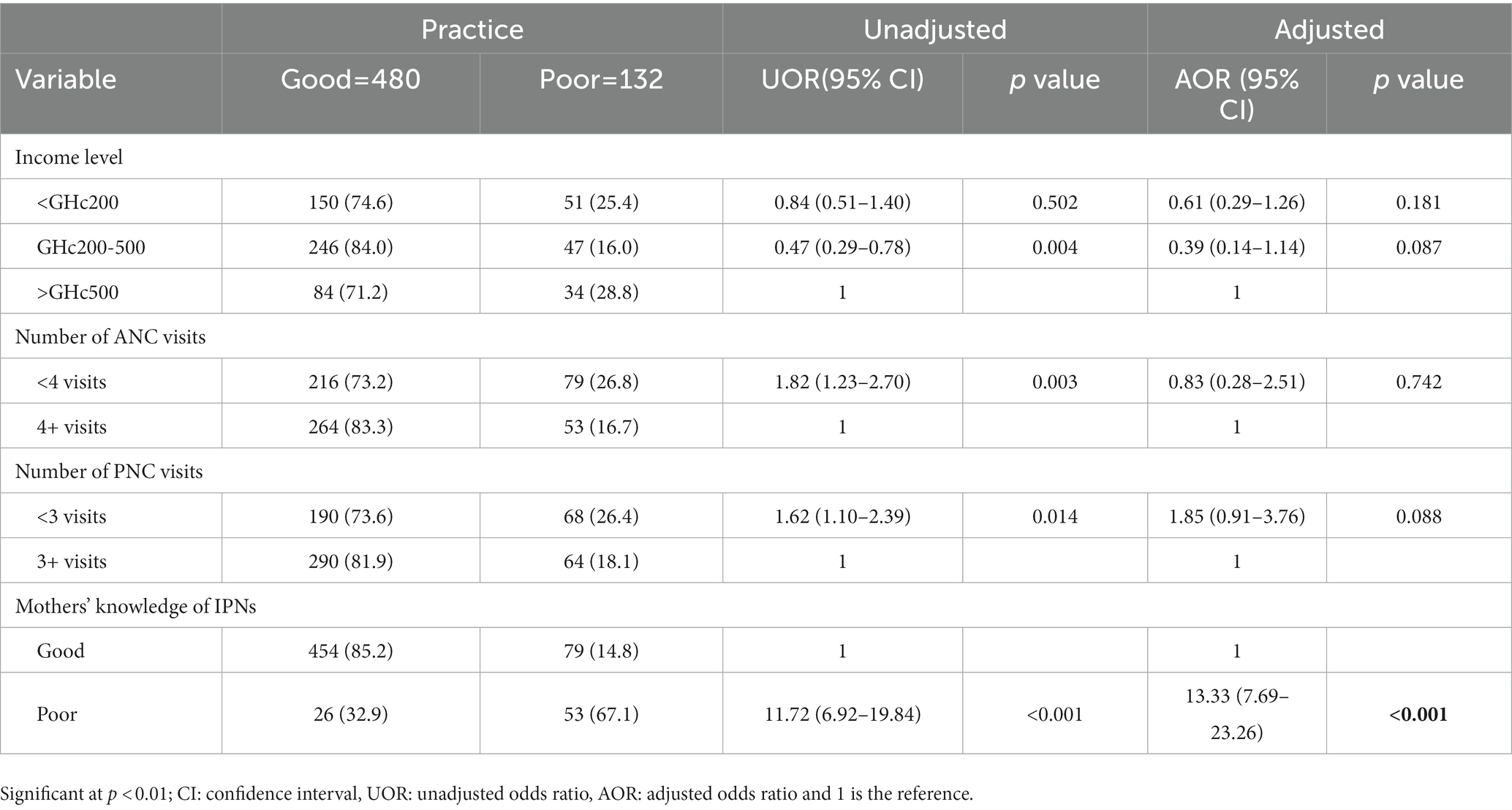
Table 4. Association between knowledge and practice of infection prevention in neonates and mothers’ sociodemographic characteristics and reproductive health factors.
Factors associated with practices of infection prevention in neonates
The study found significant associations in the levels of practice of IPNs with income level, number of ANC visits, number of PNC visits and mothers’ knowledge of IPNs (p < 0.01; Table 4). In the multivariable analyses, only mothers’ knowledge of IPNs was statistically significant (p < 0.01). Mothers who had poor knowledge of IPNs [AOR = 13.33 (95% CI: 7.69–23.26), p < 0.001] were 13.33 more likely to have a poor practice of IPNs compared to those who had good knowledge of IPNs (Table 6).
Discussion
In Ghana, neonatal deaths occur every 15 min, and the mortality rate of 29 per 1,000 in 2014 shows that Ghana’s neonatal mortality rate (NMR) is greater than Africa’s average of 27 per 1,000, which is the maximum NMR in West Africa (26). This implies that without intensive efforts, Ghana is unable to attain Sustainable Development Goal (SDG) 3 of reducing under five and NMRs to 25 and 12 per 1,000 live births, respectively (26). Per the Ghana Demographic and Health Survey, from 1993 to 2014, the NMR in Ghana declined by 44%, while the northern region reported a 67% reduction, 25% in the Volta Region and 10% in the Upper West Region (27). Presently, data are scarce on neonatal mortality due to infection in Ghana and particularly in the Volta region, and reducing NMR to acceptable levels is difficult without good maternal knowledge and practice regarding infection prevention. This study aimed to assess sociodemographic characteristics and reproductive health factors associated with maternal knowledge and practice of IPNs in North Dayi District, Ghana.
The findings of this study showed that less than one-fifth of the mothers had poor knowledge of IPNs according to the WHO’s guidelines. Similar findings were shown in studies conducted in Ghana, South Sudan, Nepal and Kenya (2, 9–11), which found that less than half of the mothers had poor knowledge of IPNs. In the present study, over three-quarters of the mothers had a formal background of education, and the types of education provided to mothers by the knowledgeable healthcare professionals and their prioritization of ANC and PNC could contribute to their good knowledge of IPNs. In contrast, another study performed in Ghana (5), Ethiopia (6, 12) and Saudi Arabia (13) found that over half of the mothers had poor knowledge of IPNs. The disparities across these studies compared with the present study could be the cut-off point used for knowledge scores.
In our study, the percentage of mothers who incorrectly practiced IPNs was less than half, which corresponds to studies performed in Ghana, Ethiopia and Nepal (2, 8, 9) that found the poor practice of IPNs in less than half of the mothers. The reason is that the majority of the mothers in the present study were compliant with the acquired knowledge of IPNs, which is shown in their practice. The opposite was found in studies performed in Ghana (14), Uganda (15), Ethiopia (7, 16) and Nigeria (17), which reported that over half of the mothers poorly practiced IPNs. The disparities could be due to the study population, cut-off point used for categorization of the practice of IPNs, noncompliance of mothers with knowledge of IPNs and cultural differences in regards to practices of IPNs.
This study revealed that mothers who had poor knowledge of IPNs were more likely to have poor IPN practices than those who had good IPN knowledge. This finding concurs with studies performed in Ethiopia (7, 8) and Nepal (9), which found that mothers who had good knowledge of IPNs were more likely to have good practices of IPNs. This means that the good knowledge of IPNs among the majority of the mothers in the present study increases their practices of IPNs. The findings would be useful for the Health Directorate of North Dayi District to develop appropriate strategies for mothers with inadequate knowledge of IPNs, which can be reflected in their practice of IPNs.
Strengths and limitations
The study provides information on maternal knowledge and practice of IPNs in North Dayi District, which has not been thoroughly presented by previous studies in Ghana, to aid in strategy and policy development to prevent and reduce neonatal infection. Regardless of the strengths, the study has some limitations. First, the results regarding the maternal knowledge and practice of IPNs are likely to be based on mothers’ recall, which could result in social desirability bias. Second, the sample size excluded mothers who did not attend the various health facilities during the study period, those unable to communicate properly and those who attended but disagreed to take part in the study. Excluding mothers who did not attend the clinic for various reasons, could undermine the reported rates in this study. Thirdly, we did not study IPN with neonatal deaths secondary to infection. To date, we could not find any reports on the percentage of neonatal deaths due to infection in Ghana, particularly in North Dayi District, whether low or high and perhaps more focus needs to be given to further studies.
Conclusion
Less than one-fifth of the mothers had poor knowledge and poor practice of IPNs according to the WHO’s guidelines. Mothers who had poor knowledge of IPNs were more likely to have a poor practice of IPNs. The Ghana Health Service should continue to enforce home visits by nurse assistants to identify and educate mothers who are unable to attend ANC and PNC. The Health Directorate of North Dayi District should encourage the use of IPN guidelines by the WHO for outreach and campaigns. Finally, the limitations identified in our study highlight the need for similar studies in communities to develop strategies to prevent and reduce neonatal infection.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Approval was sought from the North Dayi District Health Directorate, Ghana Health Service with identity (NDDHD/GR/002/20) on 11/06/2020. Permission was granted by the management of the health centers. The research assistants introduced themselves, and consent was granted from each neonatal mother before the data collection. The aims of the study were clarified by the language of the neonatal mothers. Informed approval was granted by the neonatal mother by a thumbprint. No place was allowed for personal documentation for confidentiality purposes. The questionnaires were answered individually to certify privacy. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
LT, BA, ED, DO, and JG conceptualized and designed the study. LT, JT, NA, KS, KM, SS, and KC coordinated and participated in the data collection. LT drafted the manuscript. All authors were involved in reviewing it for intellectual content. All authors contributed to the article and approved the submitted version.
Acknowledgments
We acknowledge the management of the various health facilities for their contributions to the data collection. Additionally, we appreciate the mothers who took part in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1062268/full#supplementary-material
Abbreviations
WHO, World Health Organization, SSA, Sub-Saharan Africa, ANC, Antenatal Clinic, PNC, Postnatal Clinic, SDG, Sustainable Development Goal, AOR, adjusted odds ratio, UOR, Unadjusted Odds Ratio, Cl, confidence interval, NMR, Neonatal mortality rate,
References
1. World Health Organization WHO. WHO key facts on newborn mortality. (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021 (Accessed April 21, 2022).
2. Ayete-Nyampong, J, and Udofia, EA. Assessment of knowledge and quality of essential newborn care practices in La Dade Kotopon Municipality, Ghana. PLoS One. (2020) 15:1–15. doi: 10.1371/journal.pone.0237820
3. Belachew, A, and Tewabe, T. Neonatal sepsis and its association with birth weight and gestational age among admitted neonates in Ethiopia: systematic review and meta-analysis. BMC Pediatr. (2020) 20:55–7. doi: 10.1186/s12887-020-1949-x
4. Bekele, K, Bekele, F, Mekonnen, M, Jemal, K, and Fekadu, G. Neonatal care practice and associated factors among mothers of infants 0–6 months old in North Shewa zone, Oromia region, Ethiopia. Sci Rep. (2022) 12:1–8. doi: 10.1038/s41598-022-14895-3
5. Salia, SM, Afaya, A, Wuni, A, Ayanore, MA, Salia, E, Kporvi, DD, et al. Knowledge, attitudes and practices regarding neonatal jaundice among caregivers in a tertiary health facility in Ghana. PLoS One. (2021) 16:1–20. doi: 10.1371/journal.pone.0251846
6. Berhea, TA, Belachew, AB, and Abreha, GF. Knowledge and practice of essential newborn care among postnatal mothers in Mekelle City, North Ethiopia: a population-based survey. PLoS One. (2018) 13:e0202542–12. doi: 10.1371/journal.pone.0202542
7. Sakelo, AN, Assefa, N, Oljira, L, and Assefa, ZM. Newborn care practice and associated factors among mothers of one-month-old infants in Southwest Ethiopia. Int J Pediatr. (2020) 2020:1–7. doi: 10.1155/2020/3897427
8. Misgna, HG, Gebru, HB, and Birhanu, MM. Knowledge, practice and associated factors of essential newborn care at home among mothers in Gulomekada District, eastern Tigray, Ethiopia, 2014. BMC Pregnancy Childbirth. (2016) 16:144–52. doi: 10.1186/s12884-016-0931-y
9. Singh, DR, Harvey, CM, Bohara, P, Nath, D, Singh, S, Szabo, S, et al. Factors associated with newborn care knowledge and practices in the upper Himalayas. PLoS One. (2019) 14:1–18. doi: 10.1371/journal.pone.0222582
10. Mesekaa, LA, Mungai, LW, and Musoke, R. Mothers’ knowledge on essential newborn care at Juba Teaching Hospital, South Sudan. South Sudan Med J. (2017) 10:56–9.
11. Amolo, L, Irimu, G, and Njai, D. Knowledge of postnatal mothers on essential newborn care practices at the Kenyatta National Hospital: a cross sectional study. Pan Afr Med J. (2017) 28:159–66. doi: 10.11604/pamj.2017.28.97.13785
12. Berhan, D, and Gulema, H. Level of knowledge and associated factors of postnatal mothers’ towards essential newborn care practices at governmental health centers in Addis Ababa, Ethiopia. Adv Public Heal. (2018) 2018:1–10. doi: 10.1155/2018/8921818
13. Abu-Shaheen, A, AlFayyad, I, Riaz, M, Nofal, A, AlMatary, A, Khan, A, et al. Mothers’ and caregivers’ knowledge and experience of neonatal danger signs: a cross-sectional survey in Saudi Arabia. Biomed Res Int. (2019) 2019:1–7. doi: 10.1155/2019/1750240
14. Saaka, M, and Iddrisu, M. Patterns and determinants of essential newborn care practices in rural areas of northern Ghana. Int J Popul Res. (2014) 2014:1–10. doi: 10.1155/2014/404387
15. Owor, MO, Matovu, JKB, Murokora, D, Wanyenze, RK, and Waiswa, P. Factors associated with adoption of beneficial newborn care practices in rural eastern Uganda: a cross-sectional study. BMC Pregnancy Childbirth. (2016) 16:1–11. doi: 10.1186/s12884-016-0874-3
16. Berhe, M, Medhaniye, AA, Kahsay, G, Birhane, E, and Abay, M. Essential neonatal care utilization and associated factors among mothers in public health facilities of Aksum town, North Ethiopia, 2016. PLoS One. (2017) 12:1–11. doi: 10.1371/journal.pone.0175902
17. Oluwatosin, OA. Comparative study and determinants of infection control practices of mothers of under-five children in selected health care institutions in Ibadan. Int J Infect Control. (2014) 10:1–9. doi: 10.3396/ijic.v10i4.029.14
18. Memon, J, Holakouie-Naieni, K, Majdzadeh, R, Yekaninejad, MS, Garmaroudi, G, Raza, O, et al. Knowledge, attitude, and practice among mothers about newborn care in Sindh, Pakistan. BMC Pregnancy Childbirth. (2019) 19:1–9. doi: 10.1186/s12884-019-2479-0
19. Nigatu, SG, Worku, AG, and Dadi, AF. Level of mother’s knowledge about neonatal danger signs and associated factors in north West of Ethiopia: a community based study. BMC Res Notes. (2015) 8:309–15. doi: 10.1186/s13104-015-1278-6
20. Mersha, A, Assefa, N, Teji, K, Bante, A, and Shibiru, S. Mother’s level of knowledge on neonatal danger signs and its predictors in Chencha district, Southern Ethiopia. Am J Nurs Sci. (2017) 6:426–32. doi: 10.11648/j.ajns.20170605.17
21. Tuglo, LS. Prevalence and determinants of lower extremity amputations among type I and type II diabetic patients: a multicenter-based study. Int Wound J. (2022) 19:1–7. doi: 10.1111/iwj.13935
22. Tuglo, LS. Comparison of adiposity anthropometric indices and their associations with visceral fat levels determined by bioelectrical impedance analysis among diabetic patients. Sci Rep. (2022) 12:1–9. doi: 10.1038/s41598-022-22848-z
23. World Health Organization WHO. WHO recommendations on maternal and newborn care for a positive postnatal experience. (2022). Available at: https://www.who.int/publications/i/item/9789240045989 (Accessed July 10, 2022).
24. Maternal and Child Survival Program MCSP. Postnatal Care for Mothers and Newborns Highlights from the World Health Organization 2013 guidelines. (2015). Available at: http://www.mcsprogram.org.2015 (Accessed December 11, 2021).
25. Tuglo, LS, Agbadja, C, Bruku, CS, Kumordzi, V, Tuglo, JD, Asaaba, LA, et al. The association between pregnancy-related factors and health status before and after childbirth with satisfaction with skilled delivery in multiple dimensions among postpartum mothers in the Akatsi South District, Ghana. Front Public Health. (2022) 9:1–12. doi: 10.3389/fpubh.2021.779404
26. Adjei, G, Darteh, EKM, Nettey, OEA, and Doku, DT. Neonatal mortality in the central districts of Ghana: analysis of community and composition factors. BMC Public Health. (2021) 21:1–14. doi: 10.1186/s12889-021-10156-6
Keywords: sociodemographic characteristics, reproductive health factors, knowledge, practice, infection prevention in neonates, mothers, Ghana
Citation: Tuglo LS, Agyekum BA, Darku ED, Alida NM, Seelo KP, Magaga K, Chiambiro KV, Tuglo JD, Sakre SM, Otoo DD and Gmanyami JM (2023) Sociodemographic characteristics and reproductive health factors associated with maternal knowledge and practice of infection prevention in neonates in North Dayi District, Ghana. Front. Public Health. 11:1062268. doi: 10.3389/fpubh.2023.1062268
Edited by:
Fook-Choe Cheah, Universiti Kebangsaan Malaysia Medical Center (UKMMC), MalaysiaReviewed by:
Victor Samuel Rajadurai, KK Women's and Children's Hospital, SingaporeSusan Coffin, University of Pennsylvania, United States
Socorro De Leon-Mendoza, Kangaroo Mother Care Foundation Philippines, Philippines
Merlin Willcox, University of Southampton, United Kingdom
Copyright © 2023 Tuglo, Agyekum, Darku, Alida, Seelo, Magaga, Chiambiro, Tuglo, Sakre, Otoo and Gmanyami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lawrence Sena Tuglo, bHN0dWdsbzIwMTJAdWhhcy5lZHUuZ2g=
†ORCID: Lawrence Sena Tuglo, https://orcid.org/0000-0001-8695-2384
 Lawrence Sena Tuglo
Lawrence Sena Tuglo Benjamin Adu Agyekum2
Benjamin Adu Agyekum2 Khauhelo Magaga
Khauhelo Magaga Kudzai Victor Chiambiro
Kudzai Victor Chiambiro