
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 21 March 2023
Sec. Family Medicine and Primary Care
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1043347
This article is part of the Research TopicProgress in Understanding and Treating Distress, Sleep, and Personality in Heart and Lung DiseaseView all 9 articles
 Qiao Wang1,2†
Qiao Wang1,2† Shimin Hu1,2,3,4†
Shimin Hu1,2,3,4† Na Clara Pan1,2,3,4
Na Clara Pan1,2,3,4 Tingting Zhang1,2,3,4
Tingting Zhang1,2,3,4 Liankun Ren1,2*
Liankun Ren1,2* Yuping Wang1,2,3,4*
Yuping Wang1,2,3,4*Introduction: Compared with sleep disorders, no consensus has been reached on whether a subjective complaint of having trouble sleeping is associated with increased all-cause and heart disease mortality risk. Previous studies displayed considerable heterogeneity in population disease characteristics and duration of follow-up. Therefore, the aims of this study were to examine the relationship between sleep complaints and all-cause and heart disease mortality and whether the associations were influenced by follow-up time and population disease characteristics. In addition, we aimed to figure out the influence of the joint effects of sleep duration and sleep complaints on mortality risk.
Methods: The present study utilized data from five cycles of the National Health and Nutrition Examination Survey (NHANES) (2005~2014) linked with the most updated 2019 National Death Index (NDI). Sleep complaints were determined by answers to “Have you ever told a doctor or other health professional that you have trouble sleeping?” and “Have you ever been told by a doctor or other health professional that you have a sleep disorder?”. Those who answered ‘Yes' to either of the aforementioned two questions were considered as having sleep complaints.
Results: A total of 27,952 adult participants were included. During a median follow-up of 9.25 years (interquartile range, 6.75–11.75 years), 3,948 deaths occurred and 984 were attributable to heart disease. A multivariable-adjusted Cox model revealed that sleep complaints were significantly associated with all-cause mortality risk (HR, 1.17; 95% CI, 1.07–1.28). Subgroup analysis revealed that sleep complaints were associated with all-cause (HR, 1.17; 95% CI, 1.05–1.32) and heart disease (HR, 1.24; 95% CI, 1.01–1.53) mortality among the subgroup with cardiovascular disease (CVD) or cancer. In addition, sleep complaints were more strongly associated with short-term mortality than long-term mortality. The joint analysis of sleep duration and sleep complaints showed that sleep complaints mainly increased the mortality risk in those with short (<6 h/day, sleep complaints HR, 1.40; 95% CI, 1.15–1.69) or recommended (6–8 h/day, sleep complaints HR, 1.15; 95% CI, 1.01–1.31) sleep duration group.
Discussion: In conclusion, sleep complaints were associated with increased mortality risk, indicating a potential public benefit of monitoring and managing sleep complaints in addition to sleep disorders. Of note, persons with a history of CVD or cancer may represent a potentially high-risk group that should be targeted with a more aggressive intervention of sleep problems to prevent premature all-cause and heart disease death.
Sleep is essential for the maintenance of human life (1). Sleep disorders typically cause disturbances in the quality and duration of sleep, resulting in impaired daytime functioning and distress. Sleep disorders can be divided into seven major categories according to the International Classification of Sleep Disorders, third edition (ICSD-3) (2), which include insomnia disorders, sleep-related breathing disorders, central disorders of hypersomnolence, circadian rhythm sleep–wake disorders, sleep-related movement disorders, parasomnias, and other sleep disorders. Insomnia and obstructive sleep apnea are the two most common sleep disorders, with approximately 6–23% (3, 4) and 6–17% (5) of the general population fulfilling the diagnostic criteria of insomnia and moderate to severe obstructive sleep apnea, respectively. Sleep disorders negatively affect immune function (6, 7), endocrine homeostasis (8), nutrient metabolism (9, 10), and cognitive function (11, 12), and therefore contribute to a considerable burden of physical and mental health problems (13–15), including cardiovascular disease (CVD) (16, 17).
Growing epidemiological evidence supports that sleep disorders are associated with increased mortality in the general population (18–20). However, the high missed diagnosis rate of insomnia has been revealed in a recent study (4), which reported an insomnia disorder estimate of 25.2% among Australian adults using the widely accepted contemporary ICSD-3 criteria, of which only 5.5% have been ever diagnosed with insomnia. Moreover, a large number of people suffer from self-perceived sleep problems but do not meet the diagnostic criteria for sleep disorders. A multi-center survey of 22,330 adults from 13 countries (21, 22) reported that more than 35% of participants experienced insomnia symptoms, with ~17% meeting insomnia disorder criteria during the first months of the 2019 Coronavirus pandemic. Although considered an imprecise measure, subjective sleep complaints remain an important indicator of sleep health, as they may reflect the presence of sleep impairment that is difficult to identify and assess (1).
A number of studies have previously focused on the relationship between mortality and sleep problems; however, variation existed in the definition of sleep problems in the literature, with two main categories: sleep complaints (single or multiple sleep symptoms) and sleep disorders (clinical diagnosis). Compared with sleep disorders, it is unclear whether the subjective complaint of having trouble sleeping is associated with increased all-cause and heart disease mortality risk in the general population. Although progress has been made in evaluating the relationship between mortality and sleep complaints, such as insomnia symptoms, the conclusions were inconsistent (23–31). Those studies displayed considerable heterogeneity in population inclusion criteria (e.g., age, gender, or specific diseases) and duration of follow-up (ranging from years to decades). Furthermore, the joint effects of sleep duration and sleep complaints on mortality risk may also significantly affect the results. We assumed that the inconsistency in the conclusions of these articles may be partially due to the heterogeneities mentioned earlier.
Therefore, the aims of this study were to examine the relationship between sleep complaints and all-cause and heart disease mortality and whether the associations were influenced by follow-up time and disease status utilizing data from five cycles of the National Health and Nutrition Examination Survey (NHANES) (2005~2014) linked with the most updated 2019 National Death Index (NDI). In addition, we aimed to figure out the influence of the joint effects of sleep duration and sleep complaints on mortality risk.
All participants were selected from five cycles of “continuous NHANES” (2005~2014). Details of the NHANES have been described online (https://www.cdc.gov/nchs/index.htm). Briefly, NHANES used a complex multistage probability sampling method to collect nationally representative health-related data of the US population. Data were obtained by in-person interview and mobile physical examination. In the present study, 50,965 participants from the continuous NHANES (2005–2014) datasets were first enrolled. Then, we excluded participants who were aged < 18 years (n = 20,670) or with no data on mortality (n = 57), sleep behaviors (n = 110), history of CVD or cancer disease (n = 1,973), and other covariates (n = 203). Therefore, a total of 27,952 participants were included in the final analysis (Supplementary Figure S1). The NHANES has been approved by the National Center for Health Statistics Ethics Review Board. All participants gave written informed consent. The present investigation relied on deidentified publicly available data and the project was approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University [approval number (2022) 127]. The study method and results were reported following the Strengthening the Reporting of Observational Studies in Epidemiology Statement for cross-sectional studies (32).
Sleep complaints were determined through two questions at the baseline visit. Question 1 was “Have you ever told a doctor or other health professional that you have trouble sleeping?”, with responses “Yes”, “No”, “Refused”, or “Don't know”, and question 2 was “Have you ever been told by a doctor or other health professional that you have a sleep disorder?”, with responses “Yes”, “No”, “Refused”, or “Don't know”. Those who answered ‘Yes' to question 1 and/or question 2 were considered as having sleep complaints, those who answered ‘Yes' to question 2 were considered as having a sleep disorder, and those who answered ‘Yes' to question 1 but ‘No' to question 2 were considered as having sleep complaints only. Sleep duration was determined using the following question: “How much sleep do you get (hours)?”, and then was categorized into four groups (< 6 h, 6–8 h, 8–10 h, and ≥ 10 h/day). Baseline weight and height were measured during a mobile physical examination. For those who did not participate in the physical examination, we used the current self-reported weight and height recorded in the baseline questionnaire as an alternative. The baseline body mass index (BMI) was calculated as weight (kg) divided by the square of height (m2). Information on covariates was available through baseline questionnaires, including age, sex, education level (high school or below vs. college or above), smoking status (never smoker vs. former/current smoker), leisure time moderate-to-vigorous physical activity (MVPA) [meeting (≥10 MET-h/week) vs. not meeting the guideline (< 10 MET-h/week)], and history of diabetes, hypertension, CVD (including congestive heart failure, coronary heart disease, and stroke), and cancer (history of or currently suffering from any kind of cancer or malignancy). Depression was measured using the Patient Health Questionnaire-9 (PHQ-9), a nine-item self-report instrument used as a screening and diagnostic tool (33). Each instrument was given a point ranging from 0 to 3 according to the frequency of symptoms of depression over the past 2 weeks and the total PHQ-9 score ranged from 0 to 27. As recommended by a previous study (34), a PHQ-9 total score of ≥ 5 was regarded as clinically relevant depression in this study.
The outcome was the final mortality status as well as the leading cause of death until 31 December 2019 ascertained by the mortality data from the NDI. The NDI is a highly reliable resource for death identification and the method could be found from the National Center for Health Statistics (https://www.cdc.gov/nchs/data-linkage/mortality-public.htm#). The causes of death were classified according to the codes of the International Statistical Classification of Diseases, 10th Revision (ICD-10). Deaths from heart diseases were identified according to ICD-10 codes I00-I09, I11, I13, and I20-I51. Persons who survived were administratively censored on December 31, 2019. Follow-up time for each person was months between the NHANES interview date and death or the last known date alive or censored from the mortality file.
We accounted for complex survey design factors according to the public guidelines for using NHANES data (https://www.cdc.gov/nchs/nhanes/about_nhanes.htm), including the sample weights, stratification, and clustering. Baseline characteristics across with or without sleep complaints were presented as weighted mean (SE) for continuous variables and number (weighted percentage) for categorical variables and were compared using the Rao-Scott χ2 test for categorical variables and the t-test for continuous variables.
Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of all-cause and heart disease mortality associated with sleep complaints. We tested the proportional hazards assumption for complex survey data by creating time-dependent covariates. We first examined the relationship between sleep complaints and all-cause and heart disease mortality in all included participants. We then conducted these analyses among subgroups with or without a history of CVD or cancer, separately. We further investigated the relationship between sleep complaints and short- and long-term outcomes among the total population and the subgroup with CVD or cancer at baseline using the survival status at 2 years of follow-up or excluding individuals who died within 2 years of follow-up, respectively. A crude model and two multivariable models were constructed. Model 1 showed unadjusted results. In model 2, we adjusted for the baseline age (years, continuous), and gender. In model 3, we additionally adjusted for education level, smoking status, leisure time MVPA level, BMI, history of diabetes, and hypertension. Plots were constructed to visualize the fully adjusted (model 3) cumulative incidence of all-cause and heart disease death for participants with and without sleep complaints. Given the symptoms of depression commonly co-occur with insomnia and were associated with mortality (26), we also repeated the main analyses after adding depression (categorical variable, PHQ-9 total score ≥ 5 vs. PHQ-9 total score < 5) as a confounder in the cox models.
The combined effects of sleep duration (< 6 h, 6–8 h, 8–10 h, and ≥ 10 h/day) and sleep complaints were estimated in the multivariate Cox models. In addition, we examined the non-linear relationship between sleep duration and risk of all-cause and heart disease death with restricted cubic splines.
All statistical analyses were performed using R (version 4.1.2) and SAS (version 9.4) with survey-specific commands and a two-tailed P-value of < 0.05 was considered to be statistically significant.
A total of 27,952 participants (mean age, 46.9 years; men, 48.5%) were included in the statistical analysis. The weighted prevalence of sleep complaints was 27.2% (95% CI, 25.3–29.0%), which was much higher than that of sleep disorders (8.3% [95% CI, 7.7–8.9%]). Table 1 shows the baseline characteristics of the participants with and without sleep complaints. In general, compared with participants without sleep complaints, those who suffered from it were more likely to be older, women, former or current smokers, physically inactive, and had a shorter sleep duration, higher BMI, and higher prevalence of hypertension, diabetes mellitus, CVD, cancer, and depression.
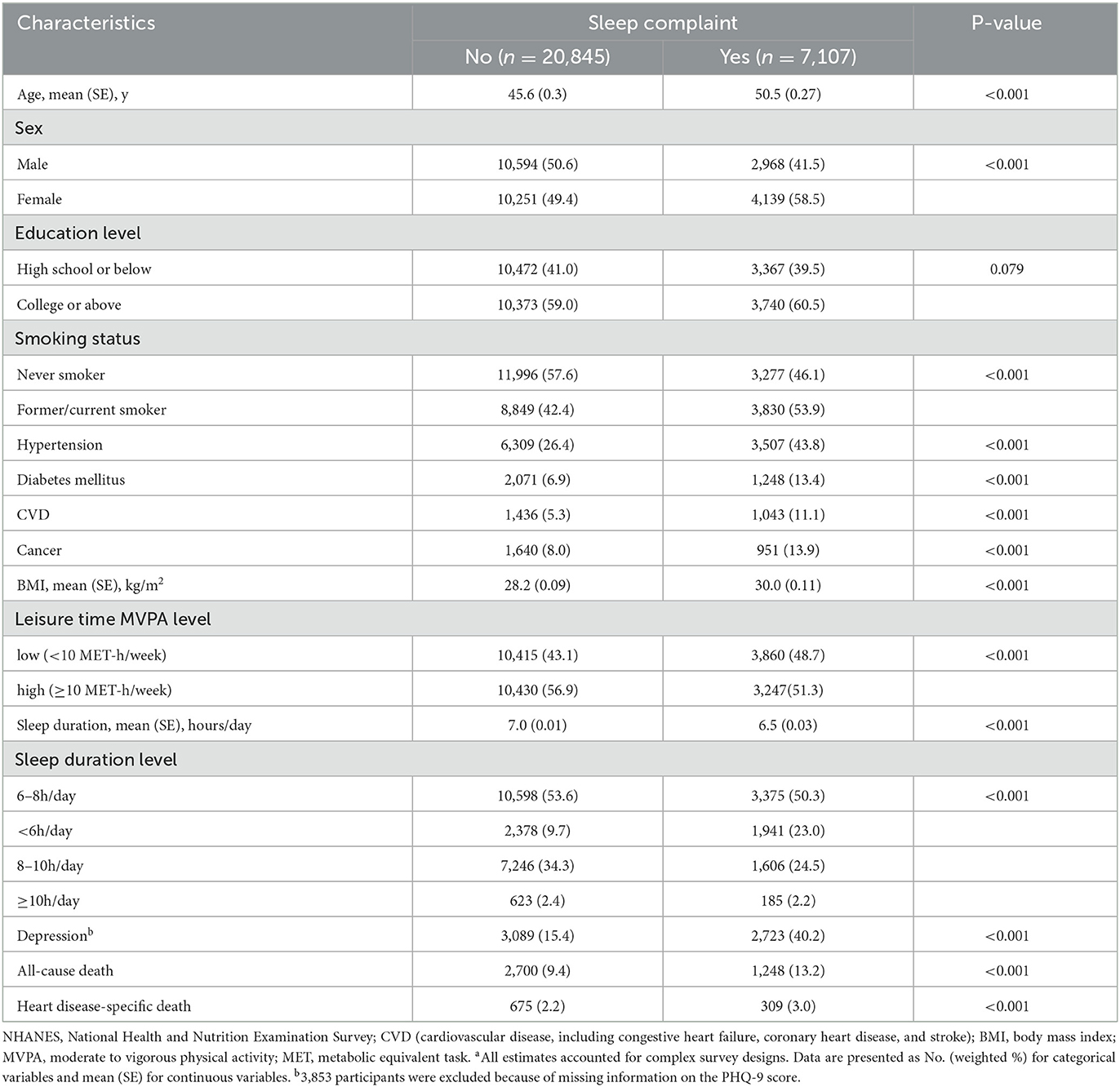
Table 1. Baseline characteristics of all included participants by sleep complaints from NHANES 2005 through 2014a.
During a median follow-up of 9.25 years (interquartile range, 6.75–11.75 years), 3,948 deaths occurred, including 984 deaths from heart disease. Sleep complaints were associated with all-cause and heart disease mortality in crude models (Table 2). After adjustment for age, sex, education level, smoking status, leisure time MVPA level, BMI, and history of diabetes and hypertension, the multivariable-adjusted HR of sleep complaints on all-cause mortality risk decreased but remained statistically significant (HR, 1.17; 95% CI, 1.07–1.28) (Table 2). However, the multivariable-adjusted HR of sleep complaints on heart disease mortality was no longer statistically significant (Table 2). Figures 1A, B shows the adjusted cumulative incidence curves of all-cause and heart disease mortality for sleep complaints among all included participants.
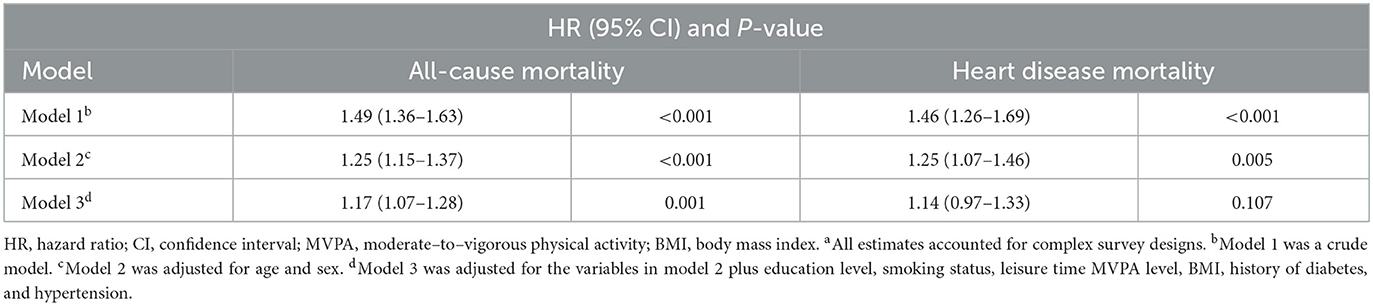
Table 2. Association of sleep complaints with all-cause and heart disease mortality among all participantsa.
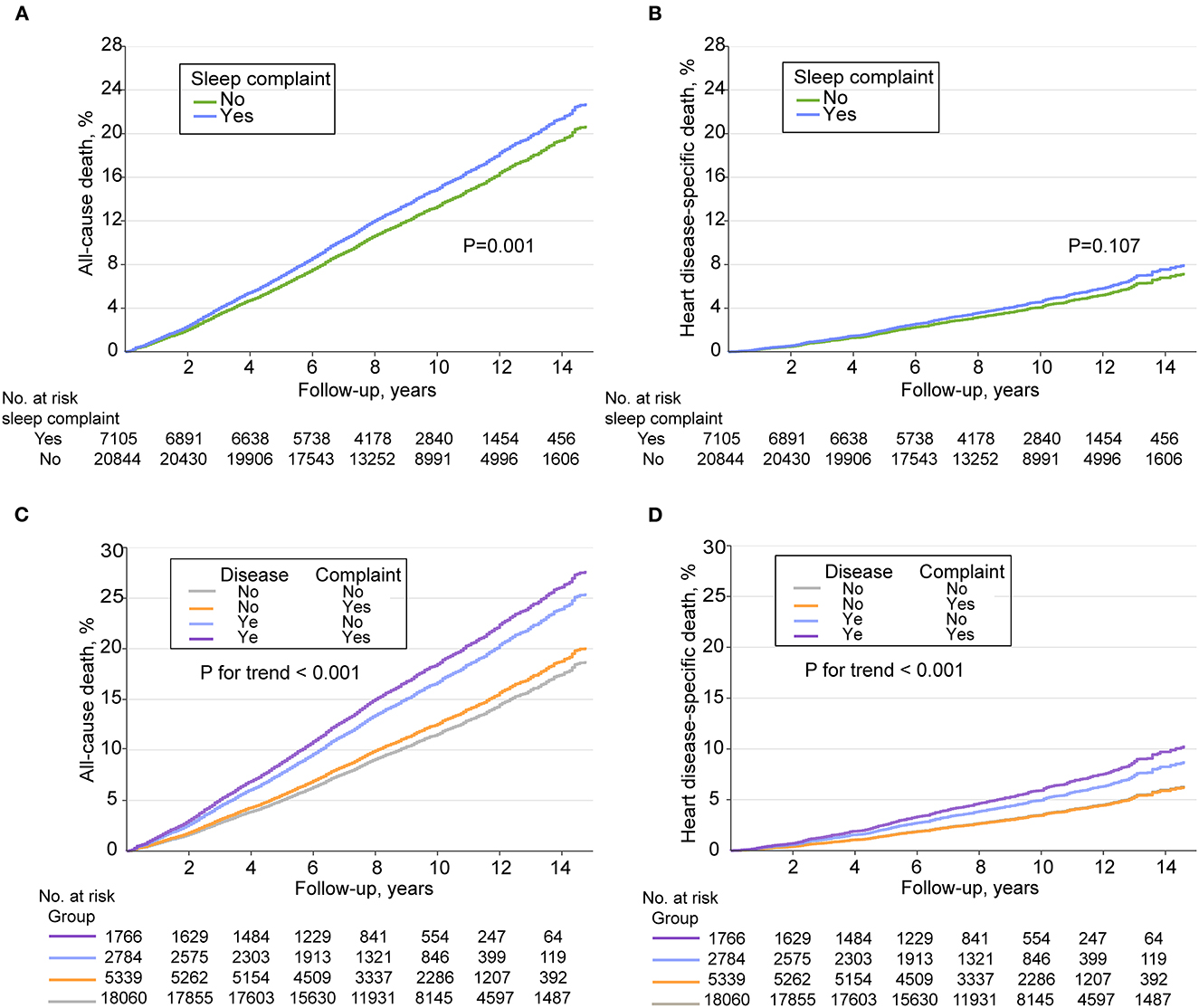
Figure 1. Adjusted cumulative incidence curves of all-cause and heart disease mortality among adults in the National Health and Nutrition Examination Survey 2005 through 2014. (A) Adjusted cumulative incidence curves of all-cause mortality stratified by sleep complaints. (B) Adjusted cumulative incidence curves of heart disease mortality stratified by sleep complaints. (C) Adjusted cumulative incidence curves of all-cause mortality stratified by cross groups of sleep complaints and disease (cardiovascular disease or cancer). (D) Adjusted cumulative incidence curves of heart disease mortality stratified by cross groups of sleep complaints and disease (cardiovascular disease or cancer).
Figures 1C, D shows the adjusted cumulative incidence curves of all-cause and heart disease mortality for cross groups of sleep complaints and CVD or cancer at baseline [no sleep complaint and no CVD or cancer (group 1); isolated sleep complaints (group 2); isolated CVD or cancer (group 3); with sleep complaints and CVD or cancer (group 4)] among all included participants, using group 1 as the reference. An increasing trend of risk of all-cause and heart disease mortality from group 1 to group 4 was observed (P < 0.001 for trend; detailed statistical results are shown in Supplementary Table S1). When participants were stratified according to the presence or absence of CVD or cancer at baseline, sleep complaints were found to be associated with all-cause (multivariable-adjusted HR,1.17; 95% CI, 1.05–1.32) and heart disease (multivariable-adjusted HR, 1.24; 95% CI, 1.01–1.53) mortality among the group with CVD or cancer only (Table 3).
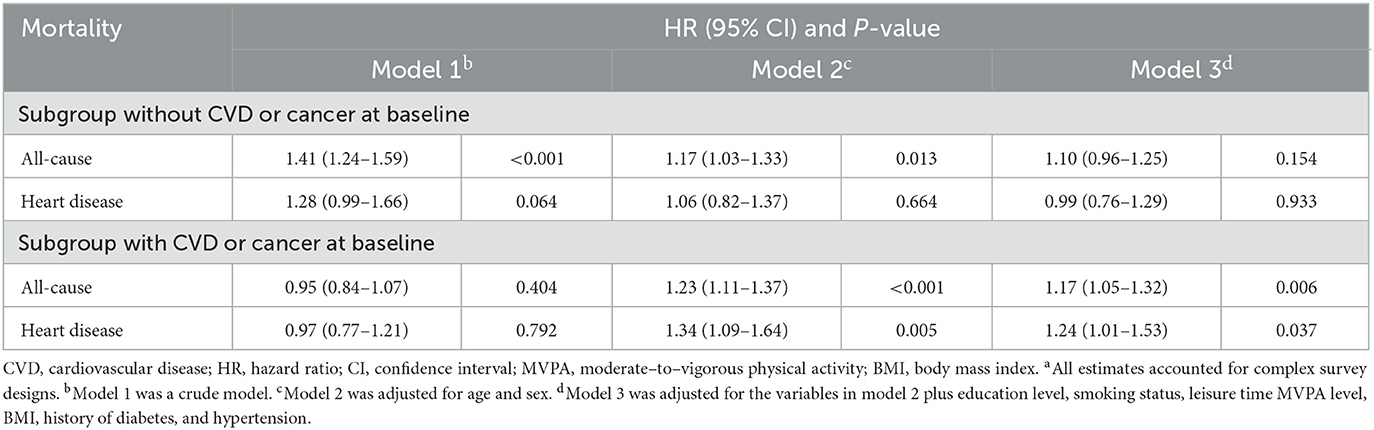
Table 3. Associations of sleep complaints with all-cause and heart disease mortality in subgroups with or without CVD or cancera.
Among all participants, sleep complaints were associated with a 1.41-fold (95% CI, 1.13–1.76) and 1.13-fold (95% CI, 1.02–1.25) increased risk of short- and long-term all-cause death, respectively, and among those with CVD or cancer at baseline, the hazard ratios were 1.37 (95% CI, 1.08–1.75) and 1.14 (95% CI, 1.00–1.29). The association between sleep complaints and short-term heart disease mortality was only evident for participants with CVD or cancer at baseline, with a multivariable-adjusted HR of 1.96 (95% CI, 1.20–3.21) (Table 4).
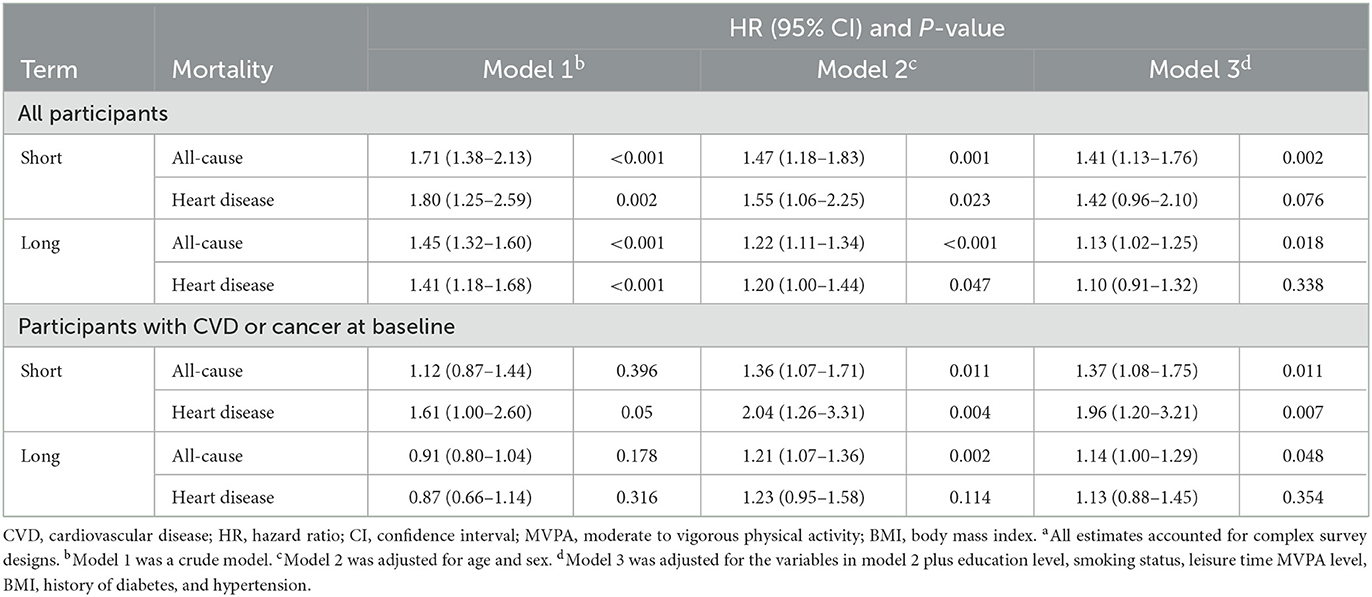
Table 4. Associations of sleep complaints with short- or long-term all-cause and heart disease mortality among all participants and subgroups with CVD or cancera.
The restricted cubic splines indicated a U-shaped relationship between sleep duration and all-cause or heart disease mortality among all participants, and the lowest risk was observed at the sleep duration of about 7 h/day (Figure 2A). Participants with sleep complaints had shorter sleep than those without (Figure 2B and Supplementary Table S2). In the joint analysis of sleep duration (< 6 h, 6–8 h, 8–10 h, and ≥10 h/day), as well as sleep complaints and the risk of mortality, participants sleeping ≥10 h per day with sleep complaints had the highest risk for all-cause mortality (HR, 2.44; 95% CI, 1.95–3.06), and those sleeping 6–8h per day free from sleep complaints (the reference group, HR = 1.00) had the lowest risk (Figure 2C). Of the eight combined subgroups, five subgroups had fewer than 100 deaths from heart disease during the follow-up; the joint analysis results for heart disease mortality need to be interpreted with caution due to the small statistical power (Supplementary Tables S3–S5). When participants were stratified by sleep duration, sleep complaints were associated with a higher risk of all-cause mortality only among the short (< 6 h/day; HR, 1.40; 95% CI, 1.15–1.69) or recommended (6–8 h/day; HR, 1.15; 95% CI, 1.01–1.31) sleep duration group. When participants were stratified by sleep complaints, the U-shaped association between sleep duration and all-cause mortality was consistent (Figure 2D and Supplementary Tables S3–S5). The effects of sleep complaints and sleep duration on all-cause mortality can be cumulated; however, their interaction was not statistically significant (p = 0.190). We repeated the main analyses of the associations between sleep complaints and all-cause and heart disease mortality after appending sleep duration (categorical variable) as a confounder in the Cox models, and there were no substantial alterations in the results (Supplementary Table S6).
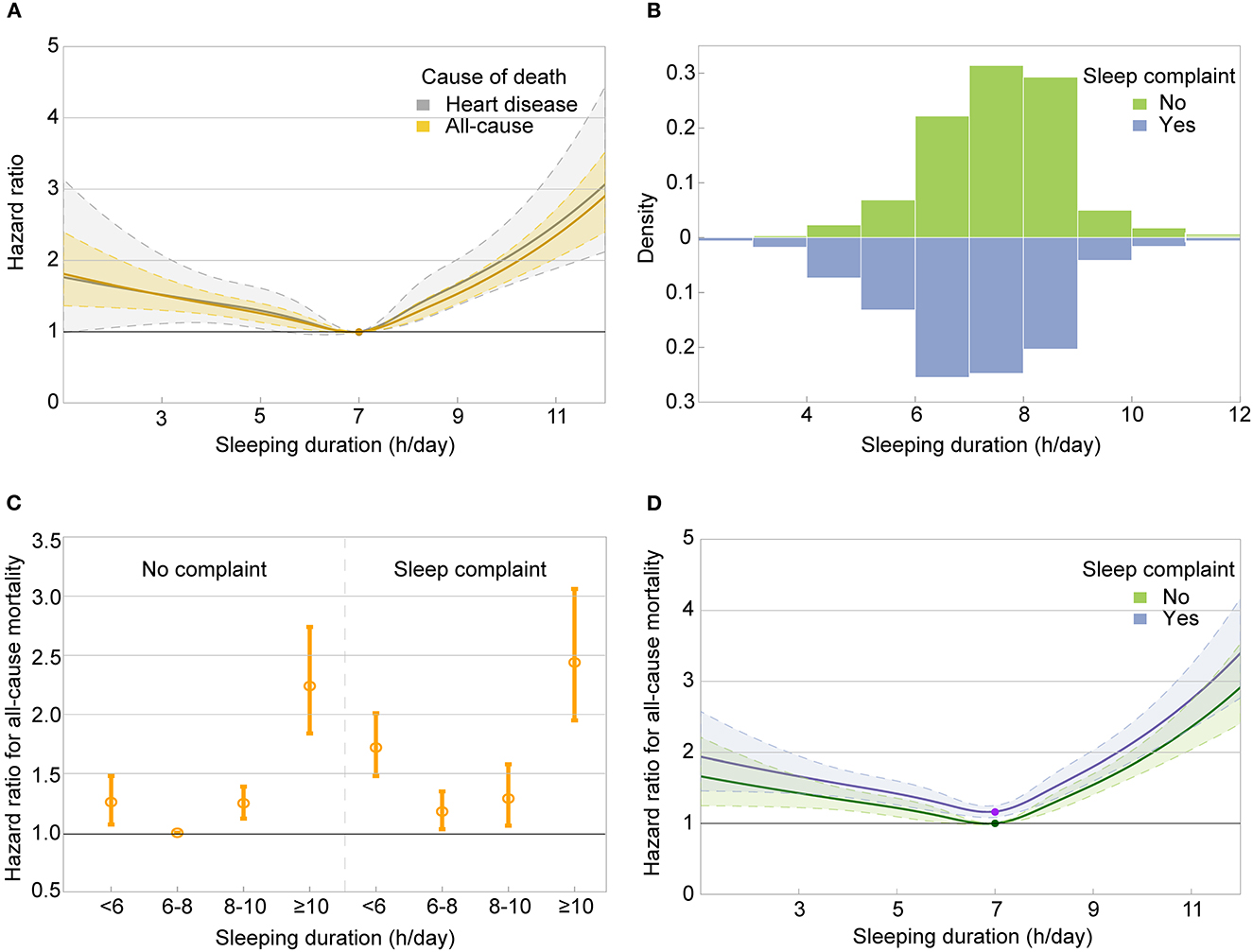
Figure 2. Relationship between sleep duration, sleep complaints, and mortality. (A) Dose–response association between sleep duration and risk of all-cause and heart disease mortality. (B) The distribution of sleep duration by sleep complaints. (C) The hazard ratios of all-cause mortality among eight combined groups of sleep duration and sleep complaints in the joint analysis. (D) Dose–response association between sleep duration and risk of all-cause mortality by sleep complaints. Associations in panels (A, D) were examined by multivariable Cox regression models based on restricted cubic splines. The solid line represents estimates of hazard ratios and the dashed line represents 95% CIs. P-values for non-linear association were <0.001 in both panels. Risk estimates in panels (A, C, D) were adjusted for baseline age, sex, education level, smoking status, leisure time moderate-to-vigorous physical activity level, body mass index, history of diabetes, and hypertension.
We further compared the relationship of mortality with sleep complaints, isolated sleep complaints, and sleep disorders, as these three groups may reflect the severity of sleep problems to some extent. The relationship of mortality with isolated sleep complaints or sleep disorders was similar to that with sleep complaints, with the highest effect size associated with sleep disorders, the intermediate with sleep complaints, and the lowest with isolated sleep complaints in the multivariable-adjusted models (Supplementary Table S7). There were no substantial alterations when further adding sleep duration as a confounder (Supplementary Table S6).
We also conducted the main analyses after adding depression (categorical variable, PHQ-9 total score ≥ 5 vs. PHQ-9 total score < 5) as a confounder in the Cox models given the potentially complex relationships among sleep complaints, depression, and mortality (18, 20, 26). When further adjusting for depression, sleep complaints remained associated with short-term all-cause and heart disease mortality in those with CVD or cancer at baseline (Supplementary Table S8). We also explored the association of mortality with isolated sleep complaints and sleep disorders after adding depression as a confounder in the Cox models; the results were consistent with that of the main analysis, with the highest effect size associated with sleep disorders, the intermediate with sleep complaints, and the lowest with isolated sleep complaints (Supplementary Table S8).
First, we found a significant difference in the HR of all-cause mortality for individuals with sleep complaints when compared with those without. In addition, in the stratified analyses, a 17% higher all-cause mortality risk and a 24% higher heart disease mortality risk of sleep complaints were observed among those with a history of CVD or cancer at baseline, while, by contrast, no association was statistically significant among those without. In addition, the strength of the association between sleep complaints and short-term mortality (within 2 years from baseline) was considerably stronger than that of the association between sleep complaints and long-term mortality. Therefore, our findings supported that the controversial findings in previous studies can be partially explained by significant diverseness across studies on demographic features of the study populations (e.g., the proportion of patients with CVD or cancer), and methodological issues (e.g., follow-up duration).
The causes and mechanisms underlying the discrepant associations between sleep complaints and short- or long-term mortality were not entirely clear. The relationship between sleep complaints and elevated short-term mortality risk might be partly attributable to the participant's medical conditions. That is, sleep problems might simply be a concomitant symptom of a health condition rather than act as a risk factor. Therefore, the association between sleep problems and long-term mortality risk might be more convincing for inferring a causal association between sleep problems and mortality risk. The results of this study supported an association between sleep complaints and long-term all-cause mortality risk, but the association might be underestimated due to the misclassification bias caused by the decreasing representativeness of baseline characteristics for the entire follow-up period as the follow-up period increases. The association between sleep complaints and long-term mortality risk needs to be further investigated in longitudinal studies using more finely grained repeated recordings of sleep profiles and other covariates. Although the short-term association between sleep complaints and mortality risk may be less robust for causal inference, the association found in this study between sleep complaints and short-term all-cause and heart disease mortality risk in people with CVD or cancer at baseline suggested, at a minimum, that the presence of sleep complaints in people with CVD or cancer may act as a “label”, indicating that individuals with sleep complaints in this particular group are at greater risk of short-term death and require additional attention and management.
In contrast to the inconsistent results of sleep complaints, the U-shaped association between sleep duration and mortality has been recognized by strong evidence from prospective studies (35–41) and the consensus statement from the American Academy of Sleep Medicine and Sleep Research Society (42). However, few studies have focused on the pattern of joint effects of sleep duration and sleep complaints on mortality risk, having fully considered the U-shaped association between sleep duration and mortality risk. Hedström et al. (28) reported that the U-shaped association between sleep duration and increased mortality risk appeared restricted to those with insomnia symptoms (28), which was partially inconsistent with the study by Chien et al. (43) as they did not observe a significant U-shaped association between sleep duration and mortality in either the infrequent insomnia group or the frequent insomnia group (43). In this study, the U-shaped association between sleep duration and all-cause mortality risk was observed both in participants with and without sleep complaints. In addition, the two studies mentioned above concluded that the association between insomnia and mortality is only evident among long sleepers (≥9 h/day), while we found that sleep complaints were associated with a higher risk of all-cause mortality only among the short (< 6 h/day) or recommended (6–8 h/day) sleep duration groups in the present study. Although the sample size of the Swedish National March Cohort (SNMC) (28) and this study were both larger than 20,000 people, obvious variation in baseline characteristics also existed between the two populations. In particular, the SNMC had a higher prevalence of sleep complaints than that of this study (75.3 vs. 27.2%), and the proportions of the short (< 6 h/day) and recommended (6–8 h/day) sleep duration groups in the SNMC cohort were 8.2% and 89.5%, while in this cohort, they were 15.5% and 50.0%, respectively. An international multi-center harmonized survey published the findings that of the 22,330 general adults from 13 countries and four continents, 36.7% had clinical insomnia symptoms (22). The sleep characteristics of this study were closer to the aforementioned multi-center study. Of note, in this study, the short sleep duration group (< 6 h/day, 47.0%) had the highest prevalence of sleep complaints, followed by the recommended group (6–8 h/day, 25.9%), which is consistent with the study by Hedström et al. (28). These findings increase the need to focus on the subgroup with sleep complaints even though they may have the optimal sleep duration.
The relationships between depression, sleep problems, and mortality risk are complex (18, 20, 26). In the study by Leggett et al., (26) the authors concluded that both insomnia symptoms and depressive symptoms are associated with a greater risk of death; however, depressive symptoms accounted for the insomnia association when both were considered in the model (26). The purpose of the present study was to determine the relationship between mortality and sleep complaints, and we observed that the independent associations were statistically significant, even when further adjusted for depression (PHQ-9 ≥5). In the current study, the weighted mean (SE) of the PHQ-9 score in subjects with sleep disorders or complaints was 5.5 (0.17) and 5.0 (0.10), respectively. The PHQ-9 score of the sleep complaints group was lower than that of the sleep disorder group. The findings of this study suggest that the relationship between sleep complaints and a higher risk of short-term all-cause and heart disease mortality in a population with mild depressive symptoms cannot be fully explained by depression, which was supported by the finding from a recent study concluding that clinical insomnia was independently associated with an increased risk of recurrent major adverse cardiovascular events in patients with coronary heart disease, even after adjustment for depression (44).
The present study had several limitations. First, owing to the cross-sectional nature of the NHANES study, the survival analyses were based on baseline sleep behaviors assessment, which may not accurately reflect the long-term status. Second, covariates collected at baseline may also change over time. There might be a complex interplay between covariates that can change over time and sleep complaints. Third, residual or unknown confounders cannot be entirely excluded, although a multitude of potential confounding factors both associated with sleep and mortality have been taken into consideration. Fourth, the identification of sleep complaints and disorders was dependent on the answers to questions in a sleep questionnaire completed in the home using the Computer-assisted Personal Interview (CAPI) system. The CAPI was programmed with built-in consistency checks to reduce data entry errors. The CAPI also uses online help screens to assist interviewers define key terms used in the questionnaire. Therefore, the answers were reliable but still lacked validation from objective examinations and information about the specific diagnosis (e.g., obstructive sleep apnea), quantitative statistics of sleep disorders, as well as whether sleep problems are primary or secondary. Finally, we did not adjust the use of sleep medication in the multivariate Cox models. However, assuming that having sleep complaints is a risk factor for death, the protective effects of sleep drugs will bias the effect to negative results. Even so, we still found that sleep complaints were associated with a higher risk of all-cause mortality and heart disease mortality, indicating that the positive results in this study were reliable, but the effect size might be underestimated.
Overall, sleep complaints at baseline were positively associated with a higher risk of all-cause mortality and heart disease mortality, particularly for those with a history of CVD or cancer at baseline, and the association persisted after further adjustment for sleep duration and depression. Even among people who sleep within the recommended duration, sleep complaints remained associated with all-cause mortality. These findings emphasize the importance of managing sleep complaints, particularly in those with CVD and cancer.
The original datasets used in this study are publicly available, and they can be found at: https://www.cdc.gov/nchs/index.htm.
The studies involving human participants were reviewed and approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University. The NHANES has been approved by the National Center for Health Statistics Ethics Review Board. All participants gave written informed consent.
YW and LR contributed to the study design and manuscript edits. QW and SH contributed to the data analysis and data interpretation and drafted the manuscript. NP and TZ contributed to the data interpretation and manuscript edits. All authors contributed to the article and approved the submitted version.
YW was supported by grant 2021YFC2501400 from the National Key Research and Development Program of China. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
We thank all the National Health and Nutrition Examination Survey (NHANES) study participants, data managers, and staff for contributing to this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1043347/full#supplementary-material
ICSD-3, the International Classification of Sleep Disorders, third edition; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Survey; NDI, National Death Index; BMI, body mass index; MVPA, moderate-to-vigorous physical activity; PHQ-9, Patient Health Questionnaire-9; ICD-10, International Statistical Classification of Diseases, 10th revision; HR, hazard ratios; CI, confidence intervals; SNMC, the Swedish National March Cohort.
1. Grandner MA, Fernandez FX. The translational neuroscience of sleep: a contextual framework. Science. (2021) 374:568–73. doi: 10.1126/science.abj8188
2. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
3. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
4. Appleton SL, Reynolds AC, Gill TK, Melaku YA, Adams RJ. Insomnia prevalence varies with symptom criteria used with implications for epidemiological studies: role of anthropometrics, sleep habit, and comorbidities. Nat Sci Sleep. (2022) 14:775–90. doi: 10.2147/NSS.S359437
5. Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. (2017) 34:70–81. doi: 10.1016/j.smrv.2016.07.002
6. Besedovsky L, Lange T, Haack M. The sleep-immune crosstalk in health and disease. Physiol Rev. (2019) 99:1325–80. doi: 10.1152/physrev.00010.2018
7. Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. (2016) 80:40–52. doi: 10.1016/j.biopsych.2015.05.014
8. Gamble KL, Berry R, Frank SJ, Young ME. Circadian Clock control of endocrine factors. Nat Rev Endocrinol. (2014) 10:466–75. doi: 10.1038/nrendo.2014.78
9. Allada R, Bass J. Circadian mechanisms in medicine. N Engl J Med. (2021) 384:550–61. doi: 10.1056/NEJMra1802337
10. Koren D, Taveras EM. Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metabolism. (2018) 84:67–75. doi: 10.1016/j.metabol.2018.04.001
11. Rasch B, Born J. About sleep's role in memory. Physiol Rev. (2013) 93:681–766. doi: 10.1152/physrev.00032.2012
12. Lal C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. (2012) 141:1601–10. doi: 10.1378/chest.11-2214
13. Morin CM, Drake CL, Harvey AG, Krystal AD, Manber R, Riemann D, et al. Insomnia disorder. Nat Rev Dis Primers. (2015) 1:15026. doi: 10.1038/nrdp.2015.26
14. Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: is it a bad thing to be awake when reason sleeps? Sleep Med Rev. (2016) 29:101–7. doi: 10.1016/j.smrv.2015.10.003
15. Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. (2014) 10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716
16. Zheng B, Yu C, Lv J, Guo Y, Bian Z, Zhou M. et al. Insomnia symptoms and risk of cardiovascular diseases among 5 million adults: a 10-year cohort. Neurology. (2019) 93:e2110–e20. doi: 10.1212/WNL.0000000000008581
17. Jarrin DC, Alvaro PK, Bouchard MA, Jarrin SD, Drake CL, Morin CM. Insomnia and hypertension: a systematic review. Sleep Med Rev. (2018) 41:3–38. doi: 10.1016/j.smrv.2018.02.003
18. Li W, Chen D, Ruan W, Peng Y, Lu Z, Wang D. Associations of depression, sleep disorder with total and cause-specific mortality: a prospective cohort study. J Affect Disord. (2022) 298:134–41. doi: 10.1016/j.jad.2021.10.131
19. Huyett P, Siegel N, Bhattacharyya N. Prevalence of sleep disorders and association with mortality: results from the nhanes 2009-2010. Laryngoscope. (2021) 131:686–9. doi: 10.1002/lary.28900
20. Bach L, Kalder M, Kostev K. Depression and sleep disorders are associated with early mortality in women with breast cancer in the United Kingdom. J Psychiatr Res. (2021) 143:481–4. doi: 10.1016/j.jpsychires.2020.11.036
21. West LC, Kushida CA. Important advances in sleep research in 2021. Lancet Neurol. (2022) 21:15–7. doi: 10.1016/S1474-4422(21)00426-9
22. Morin CM, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. (2021) 87:38–45. doi: 10.1016/j.sleep.2021.07.035
23. Mahmood A, Ray M, Ward KD, Dobalian A, Ahn SN. Longitudinal associations between insomnia symptoms and all-cause mortality among middle-aged and older adults: a population-based cohort study. Sleep. (2022) 45: zsac019. doi: 10.21203/rs.3.rs-690063/v1
24. Tao F, Cao Z, Jiang Y, Fan N, Xu F, Yang H, et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: a prospective cohort study of 407,500 UK biobank participants. Sleep Med. (2021) 81:401–9. doi: 10.1016/j.sleep.2021.03.015
25. Garfield V, Joshi R, Garcia-Hernandez J, Tillin T, Chaturvedi N. The relationship between sleep quality and all-cause, CVD and cancer mortality: the southall and brent revisited study (Sabre). Sleep Med. (2019) 60:230–5. doi: 10.1016/j.sleep.2019.03.012
26. Leggett AN, Sonnega AJ, Lohman MC. The association of insomnia and depressive symptoms with all-cause mortality among middle-aged and old adults. Int J Geriatr Psychiatry. (2018) 33:1265–70. doi: 10.1002/gps.4923
27. Li LJ, Yang Y, Guan BY, Chen Q, Wang AX, Wang YJ, et al. Insomnia is associated with increased mortality in patients with first-ever stroke: a 6-year follow-up in a chinese cohort study. Stroke Vasc Neurol. (2018) 3:197–202. doi: 10.1136/svn-2017-000136
28. Hedström AK, Bellocco R, Ye W, Trolle Lagerros Y, Åkerstedt T. Association between insomnia and mortality is only evident among long sleepers. Nat Sci Sleep. (2019) 11:333–42. doi: 10.2147/NSS.S222049
29. Ge L, Guyatt G, Tian J, Pan B, Chang Y, Chen Y, et al. Insomnia and risk of mortality from all-cause, cardiovascular disease, and cancer: systematic review and meta-analysis of prospective cohort studies. Sleep Med Rev. (2019) 48:101215. doi: 10.1016/j.smrv.2019.101215
30. Kwok CS, Kontopantelis E, Kuligowski G, Gray M, Muhyaldeen A, Gale CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. (2018) 7:e008552. doi: 10.1161/JAHA.118.008552
31. Li Y, Zhang X, Winkelman JW, Redline S, Hu FB, Stampfer M. et al. Association between insomnia symptoms and mortality: a prospective study of US Men. Circulation. (2014) 129:737–46. doi: 10.1161/CIRCULATIONAHA.113.004500
32. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
33. Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (Phq-9). J Affect Disord. (2004) 81:61–6. doi: 10.1016/S0165-0327(03)00198-8
34. Kroenke K. Phq-9: global uptake of a depression scale. WPA. (2021) 20:135–6. doi: 10.1002/wps.20821
35. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. (2011) 32:1484–92. doi: 10.1093/eurheartj/ehr007
36. Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev. (2018) 39:25–36. doi: 10.1016/j.smrv.2017.06.011
37. Short MA, Weber N. Sleep duration and risk-taking in adolescents: a systematic review and meta-analysis. Sleep Med Rev. (2018) 41:185–96. doi: 10.1016/j.smrv.2018.03.006
38. Liu TZ, Xu C, Rota M, Cai H, Zhang C, Shi MJ, et al. Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. (2017) 32:28–36. doi: 10.1016/j.smrv.2016.02.005
39. Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. (2010) 33:585–92. doi: 10.1093/sleep/33.5.585
40. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc. (2017) 6:e005947. doi: 10.1161/JAHA.117.005947
41. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large us sample. Sleep. (2008) 31:1087–96. doi: 10.5665/sleep/31.8.1087
42. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Joint consensus statement of the american academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. (2015) 38:1161–83. doi: 10.5665/sleep.4886
43. Chien KL, Chen PC, Hsu HC, Su TC, Sung FC, Chen MF, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. (2010) 33:177–84. doi: 10.1093/sleep/33.2.177
Keywords: sleep complaint, sleep duration, sleep disorder, all-cause mortality, heart disease mortality
Citation: Wang Q, Hu S, Pan NC, Zhang T, Ren L and Wang Y (2023) Association of sleep complaints with all-cause and heart disease mortality among US adults. Front. Public Health 11:1043347. doi: 10.3389/fpubh.2023.1043347
Received: 14 September 2022; Accepted: 20 February 2023;
Published: 21 March 2023.
Edited by:
Costas Papageorgiou, Priory Hospital Altrincham, United KingdomReviewed by:
John Munkhaugen, Drammen Hospital, Vestre Viken Hospital Trust, NorwayCopyright © 2023 Wang, Hu, Pan, Zhang, Ren and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuping Wang, ZG9jdG9yd2FuZ3l1cGluZ0AxNjMuY29t; Liankun Ren, cmxrYnJhaW4yMDAwQHlhaG9vLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.