- 1Department of Actuarial Science, School of Insurance, Guangdong University of Finance, Guangzhou, China
- 2Department of Medical Statistics, School of Public Health, Sun Yat-sen University, Guangzhou, China
- 3Center for Migrant Health Policy, Sun Yat-sen University, Guangzhou, China
Universal health coverage is vital to the World Health Organization’s (WHO’s) efforts to ensure access to health as a human right. However, it has been reported that migrants, including both international immigrants and internal migrants, underuse health services. Establishing a conceptual framework to facilitate research on the health service behaviors (HSB) of migrants is particularly important. Many theoretical frameworks explaining the general population’s HSB have been published; however, most theoretical frameworks on migrants’ HSB only focus on international immigrants without the inclusion of internal migrants. Of note, internal migrants are much more abundant than immigrants, and this group faces similar barriers to HSB as immigrants do. Based on theoretical frameworks of immigrants’ HSB and Anderson’s behavior model, the author proposes a new conceptual framework of migrants’ HSB that includes both immigrants and internal migrants. The new conceptual framework divides the determinants into macro-structural or contextual factors, health delivery system characteristics, and characteristics of the population at risk and describes subgroup-specific factors. The author added some variables and reclassified variables in some dimensions, including characteristics of health delivery systems and access to healthcare. The characteristics of health delivery systems comprise the volume, organization, quality, and cost of the health delivery system, while the characteristics of access to healthcare include time accessibility, geographic accessibility, and information accessibility. The outcomes of HSB have been expanded, and relationships between them have been reported. The mediating effects of some variables have also been described. This conceptual framework can facilitate a deep and comprehensive understanding of the HSB determination process for migrants, including internal migrants.
1. Introduction
“Giving everyone, everywhere an equal chance at a safe and healthy life” is the fundamental object of the World Health Organization (WHO). Therefore, universal health coverage is vital to the WHO’s efforts to ensure the achievement of this fundamental object. The United Nation’s (UN’s) Sustainable Development Goal (SDG) 3.8 also aims to “Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.” (1) However, migrants, defined as “individuals who has changed their usual place of residence, either by crossing an international border (named as international migrants or international immigrants) or moving within their country of origin to another region, district or municipality (named as internal migrants (IMs))” (2), are often excluded from the local health systems and tend to underuse the available health services (3, 4). Exploring the health service behaviors (HSB) of migrants could promote universal health coverage and contribute to the achievement of the SDG. Establishing a conceptual framework to facilitate research about migrants’ HSB is particularly important.
Many theoretical frameworks for explaining the general populations’ HSB have been published. However, theoretical frameworks for migrants were insufficient. Few theoretical frameworks accounted for the IMs. The 2022 World Migration Report reported 281 million international immigrants, while the most recent estimate of IMs globally was 740 million in 2009, which is over three times the number of international immigrants at the time (2, 5). Much larger numbers migrate within their own countries (5). Similar to international immigrants, the IMs always suffer from poor living (6) and working conditions (7, 8) and unequal access to various social welfare programs (9), including health services (10–12), than the local residents. Consequently, IMs had various barriers to accessing health services similar to immigrants. Previous studies on IMs’ HSB always reported the results based on immigrants. To some extent, the theoretical framework for explaining immigrants’ HSB would also be appropriate for IMs.
However, migrating within their home countries, IMs would suffer fewer language and/or communication barriers, cultural differences, and information barriers that would be encountered in a new health system. Some characteristics of migration, such as the reason for migration and migration range (divided into migration across provinces, cities, or counties/districts in China), were more prominent as the determinants of IMs’ HSB (13–15). According to the Seventh National Population Census, there were 261 million IMs in China in 2020, making up the majority of IMs worldwide. Although the majority of them in China enrolled in social medical insurance, they might encounter difficulties in using them in local places due to the bad flexibility caused by conflicts between cross-regional health service utilization (HSU) and localized and fragmented management of medical insurance (16, 17). Suffering from different challenges, the IMs and immigrants would have different principal reasons for opposing HSB. In other words, some determinants might be the main barriers to immigrants’ HSB, but they hardly affect IMs’ choices in terms of HSB. Considering these differences, it is important to clarify the determinants of HSB between immigrants and IMs in the theoretical framework of migrants’ HSB.
In addition, IMs can choose either the host cities for health services or their hometowns where their medical insurance always belongs (18, 19). Medical services in different locations have various expenses and thus could affect the expenditures for medical care in migrants’ hometowns (20), especially when the medical expenses are paid by the hometown’s medical insurance. Unpredictably high expenses outside the regions could result in large insurance payments. In terms of immigrants, medical expenses and financial burdens for health services also differ across countries (21). Consequently, medical location is an important characteristic of HSB. Moreover, the medical location was found to be associated with other characteristics of HSB, such as the site of medical service (22, 23).
This study aimed to explain the HSB of migrants comprehensively by establishing a conceptual framework based on the theoretical framework of the general population and immigrants. Establishing the conceptual framework of migrants’ HSB would yield information concerning several aspects of migrant-related HSB: (1) to help further distinguish the determinants of immigrants’ and IMs’ HSB; (2) to gain new knowledge on the determinants of immigrants’ and IMs’ HSB; (3) to explain the relationships between different characteristics of HSB and differences of their determinants; and (4) to help manage medical insurance funds.
2. Existing theoretical models of health service behaviors
Many theoretical models of HSB are described in the literature. As concluded by Yang and Hwang (24), the models proposed before the 1990s explain people’s HSB through illness and stages of illness behavior or medical care (named sociological models), psychological factors or processes (named socio-psychological models), the structure of the healthcare system (named institutional models), and health belief models. All of these models focus on individuals or different aspects of the healthcare institution but neglect other factors related to the health service delivery system and macro-structural or contextual factors.
2.1. Anderson’s health behavior model
The most famous model explaining people’s HSB and used in most studies in the literature is Anderson’s health behavior model (hereinafter referred to as Anderson’s model). Anderson’s model was first proposed in 1968 and revised three times afterward (25). The initial model explained people’s HSU based on three sets of factors: (1) predisposing characteristics (demographic, social structure, and health beliefs); (2) enabling resources (personal/family and community); and (3) need (perceived and evaluated). The mediating relationships occurred systematically in sequence. The phase two model added factors of the healthcare system that included policy, resources, and organization. In addition, the model in this phase specified the type, site, purpose, and time interval of HSB. The mediating relationship occurred between the population characteristics and the healthcare system. In phase three, a new category of the determinant of health behaviors was added, namely the external environment. The outcome was also expanded to HSU and personal health practices. The phase four model had the most complex form. The determinants of health behaviors consisted of the healthcare system, external environment, and population characteristics mentioned in the initial model; the former two categories of factors had mediating effects on the population characteristics. The outcome had a feedback effect on population characteristics (25).
To predict HSB, the models proposed before phase four might be more effective, namely the initial model with the addition of the healthcare system, environmental factors, and specified dimensions of the HSB. However, Anderson’s model was proposed to explain general populations’ HSB. Migrants differ from the general populations in social welfare, living, and working conditions as mentioned earlier, thus the migrant-specific factors need to be distinguished. The original model also needs to be revised as new determinants are discovered.
2.2. Immigrants’ health behavior model
Based on Anderson’s models and literature on immigrant’ HSB, several theoretical frameworks on immigrant-related health service utilization were proposed in previous studies. Helena Legido-Quigley and colleagues (26) examined the barriers that immigrants suffered in accessing healthcare and categorized these factors into leadership/governance, healthcare financing, service delivery, health workforce, information and research, medical products and technologies, and migrants’ healthcare-seeking behavior. Helena Legido-Quigley and colleagues highlighted environmental factors, factors of the healthcare system, and population characteristics without indicating mediating relationships that might have occurred among them.
Yang and Hwang’s (24) immigrant health behavior model comprehensively describes the determination factors of immigrants’ HSU. They divided the determinations into macro-structural or contextual factors and characteristics of the population at risk (consisting of predisposing factors, enabling resources, and needs), which is consistent with Anderson’s model. Referring to the determinants, Yang and Hwang considered the influence of non-health policies and divided resources into three types: (1) financial resources; (2) social resources; and (3) access to healthcare. They further categorized immigrant-specific factors: (1) immigrant-specific health needs or conditions; (2) homeland-based financial and social resources and transnational access to healthcare; (3) immigrant-specific predisposing factors; and (4) context of emigration, reception, and HSU in the homeland. They refuted the overall mediating relationships occurring and considered the mediating effects of some specific determinants and addressed those specific influences.
Yang and Hwang’s immigrant health behavior model was proposed based on Anderson’s model and followed the classification of determinants in this model. However, Yang and Hwang ignore the influence of the healthcare delivery system, which was another important component of HSB, whereas Helena Legido-Quigley and colleagues highlight the influence of the healthcare delivery system. These specific factors of the health delivery systems in the latter model would help to improve Yang and Hwang’s immigrant health behavior models.
All these models excluded IMs, a much larger group. IMs suffer from bad socioeconomic status and less social welfare and thus have more barriers to health services. IMs also differed from immigrants in many aspects as mentioned earlier. Therefore, it is necessary to revise the existing models and distinguish the determinants of HSB between the two subgroups.
3. Conceptual framework of this study
Based on Anderson’s (25) and Yang and Hwang’s immigrant health behavior models (24), we constructed the fundamental framework of this study. We searched literature published between January 2010 and January 2022 in the following electronic databases: Science Direct, Web of Science, PubMed, Wiley Online Library, and Google Scholar. We also conducted an additional search using the snowballing method. Search terms associated with “migration” or “immigrant” and “health service,” “health facilities” or “medical location” were applied. Combining determinants mentioned by Helena Legido-Quigley and colleagues (26) and reviewing the literature on migrants’ health service utilization, choice of health facilities, and medical locations, the authors supplemented and revised the existing framework of Yang and Hwang’s immigrant health behavior models (24) and proposed the conceptual framework of this study (Figure 1) based on the grounded theory. Specifically, according to the previous studies, we supplemented the dimension of health delivery system characteristics, expanded the health service behaviors, health delivery system characteristics, and access to healthcare, and distinguished determinants of immigrants’ and IMs’ HSB. However, we did not emphasize the immigrant-specific factors mentioned in Yang and Hwang’s immigrant health behavior models except for the immigrant-specific predisposing factors because this study focused on distinguishing subgroup-specific factors between immigrants and IMs. The other immigrant-specific factors on macro-structural/contextual factors, enabling resources, and needs were integrated into the general factors if they worked similarly in the two subgroups.
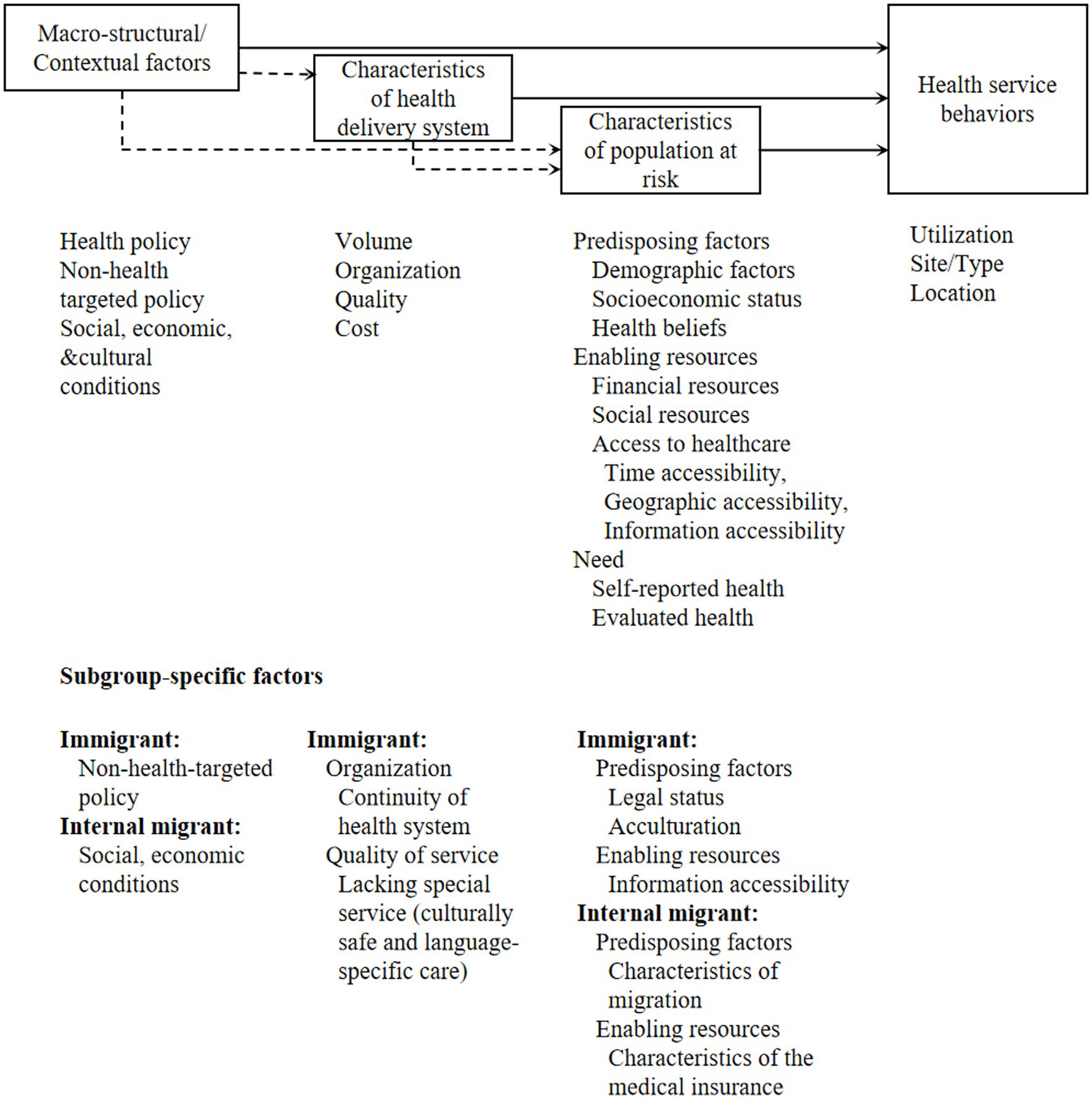
Figure 1. An analytical framework for migrants' health service behaviors. A solid line denotes a direct effect; a broken line indicates that some of the factors within this category have an indirect effect on the outcomes of migrants' health service behaviors.
3.1. Health service behavior
3.1.1. Definitions and measurements
Since the dimensions of HSB reflect different aspects of health service-seeking behavior and the determining factors and their mechanism are not the same as each other, it is necessary to specify these dimensions. According to the definition in Anderson’s HSB model (27), we updated the characteristics of HSB and included utilization, type, and site. The utilization of HSB was divided into use or no use.
The updated type refers to the kind of service received and the provider (27) by merging the type and purpose in Anderson’s model: (1) preventive service; (2) outpatient service; (3) inpatient service; (4) emergency services; (5) dental service; (6) pharmacist service; (7) traditional health services; and (8) others. These types of illness-related services (except preventive services) can be substituted for each other up to a point.
Another characteristic of HSB is the site, which differed from the site mentioned by Anderson; it refers to the place (types of health institution) at which the care was received: (1) clinic; (2) hospital; or (3) other. Clinics and hospitals include private and public institutions. The classification of the site can vary among different countries according to the structure of their healthcare system. For instance, in some countries (such as China), the health delivery system has different levels of healthcare institutions (28–32). All healthcare institutions provide similar illness-related services. A higher level of healthcare institution incorporates more experienced experts and advanced equipment. Patients are permitted to choose the health facility (28–31) and tend to prefer doctors at higher-level healthcare institutions (33). The site of HSB in these countries may be further divided into primary, secondary, and tertiary health institutions.
3.1.2. Migrant-specific characteristics of HSB
Migrants who migrate from their hometown to another destination can use health services in both places; hence, their HSU can also be characteristic of a specific location. The location of HSB refers to the location at which the care was received, namely hometown or home country, host city or the destination, or other places.
3.1.3. Interaction effect between characteristics of HSB
Characteristics of the healthcare site were found to be associated with location (22). Migrants may return to use health services of higher healthcare facilities, which are generally regarded as higher quality (23). Some literature also found that migrants may return for services in lower-level health facilities as required by the health policy, such as the hierarchical medical system in China (22). Migrants also tended to seek healthcare services in high-level hospitals with higher perceived quality in locations other than their hometowns or destinations (22), which was consistent with the purpose of transnational medical tourism.
Characteristics of type and site are closely associated with each other. The type was more frequently mentioned in literature on HSB of immigrants, while the site was more important to IMs, especially those living in countries with multi-level health providers but less restriction in terms of choosing them. Both types and sites were associated with healthcare accessibility and indicated the quality of service that migrants receive.
3.2. Health service utilization of migrants
In general, immigrants (3, 34–36) and IMs (12, 37, 38) have poor HSU levels when compared with the local residents. Factors associated with migrants’ HSU could be divided into three dimensions: (1) macro-structural or contextual factors; (2) characteristics of the health delivery system; and (3) characteristics of the population at risk (24, 27).
3.2.1. Macro-structural/contextual factors and HSU
According to Yang and Hwang (24), macro-structural or contextual factors refer to those that were at the societal or community level and beyond individual control. Macro-structural and contextual factors could be divided into healthcare policy, non-health-targeted policy, and specific regional context factors related to larger social, economic, and cultural conditions (24).
3.2.1.1. General factors
Healthcare policy was found to be an important determinant of both immigrants’ and IMs’ HSU because legislation is always not migrant-inclusive in the healthcare policies. Legal status is always considered one of the most important determinants of immigrants’ health service access. One such example is South Africa; although the South African Constitution and the National Health Act mandate universal health coverage, the Immigration Act and the 2019 NHI Bill demands that people with a legal immigrant status be able to access healthcare (39). Immigrants in host countries generally suffer from complicated bureaucratic policies (40, 41) and specific legal barriers (42, 43). Specifically, the registration procedure regulations (44), inability to verify their identities (45), legal barriers in accessing healthcare (3), and/or lack of confidence in the legal system (46) consequently limit immigrants’ HSU. Similarly, cumbersome administrative procedures and a lack of specific strategies for IMs’ health access also exclude IMs from certain medical services (47). IMs in China also have limited access to health services in their local residence if they do not register with the local government or have stable work in the host city. Residence permits aimed to eliminate inequity rights between IMs and local residents have limited effect on facilitating IMs’ health service access in megacities in China (4). The on-the-spot medical bill settlement system in China aimed to achieve portability of medical insurance and thus was expected to have a positive effect on IMs’ HSU; however, the policy’s effect has yet to be studied.
3.2.1.2. Subgroup-specific factors
Internal migrants’ HSU was only influenced by healthcare policies, while immigrants’ HSU can also be affected by non-healthcare policies. Juárez et al. found that non-health-targeted policies, such as restricted eligibility for welfare support, would decrease HSU without reducing public health insurance coverage (48). The threat of deportation also presents a barrier to health service access (43, 49).
Specific regional context factors related to greater social, economic, and cultural conditions also make sense. Referring to IMs, the specific regional context would include geographical location (50), urban/rural areas (51–53), economic development level of the region (54), city service quality index (55, 56), community health index (55), and/or the proportion of ethnic minorities (56), in addition to cultural factors (47, 57, 58). These aspects are usually associated with the health service resources, quality and accessibility of the service, financial resources, and cultural comfort during HSU. Studies concerning immigrants mainly cite cultural aspects, such as supportive communities (49) and/or immigrant-friendly environments (49), sociocultural structure and deep stigma about a certain illness (such as Chagas Disease (59)), racialized medical perceptions (42), and gender-based cultural norms, including information barriers and stigma (42). In a word, factors of regional context appeared to be more complex among IMs, while the literature on immigrants mainly focused on the cultural aspect because cultural difference between countries was more significant, and health beliefs and habits would differ across countries.
3.2.2. Characteristics of health delivery system and HSU
Characteristics of health delivery systems could be categorized into the volume, organization, quality, and cost of the healthcare delivery system.
3.2.2.1. General factors
First, the volume of the healthcare delivery system was associated with migrants’ HSU because the capacity of the healthcare delivery system is reflected through its volume. A specific healthcare delivery system would first meet the healthcare needs of local residents. Limited healthcare resources (60) and an overburdened public health system (61) were found to be barriers to immigrants’ HSU. IMs’ HSU was also limited by the volume of medical institutions (47, 56) and hospital beds (56).
Second, according to the law of supply and demand, the cost is another characteristic related to migrants’ HSU. Healthcare costs, which are always prohibitive (43), were felt to be one of the main barriers to healthcare access by both immigrants (44, 60, 62–65) and IMs (66–68). Although at times the treatment costs were not considered as barriers, co-payment by patients (69) and the unpredictable nature of out-of-pocket expenses (70) would also limit immigrants’ and IMs’ HSU. In addition to the high cost of healthcare services, difficulty meeting the costs of transport to appointments (65) was also reported.
Third, the healthcare system’s organization influences migrants’ HSU because the organization determines the access, progress, results, and efficiency of the healthcare service. Accessibility of the healthcare system was frequently mentioned in the literature in terms of both immigrants (44, 65, 71) and IMs (58, 72, 73) and measured in different ways. For example, immigrants in host countries always have difficulty navigating a new healthcare system (44, 71). The healthcare system of India restricts some treatment to Indian nationals (45). The limited availability of female-only safe spaces has led to a reduction in refugees’ (61) and IMs’ (58) utilization of maternity care. Furthermore, the efficiency of the healthcare system has also been reported in many literature studies. Long waiting times were considered the main barrier for the immigrants (64, 69, 74) and IMs (68), while the time consumed by medical treatment (67) would also affect the HSU of IMs.
Fourth, quality of the service (75) was reported to be one of the main factors associated with immigrants’ HSU, but reports concerning this aspect in terms of IMs are seldom found in the literature. The reason for this might be a lack of information. Subjective quality of service was important because better subjective satisfaction would increase the desire to seek healthcare when needed. The perceived poor quality of care (43), low standard of care in private clinics (60), or fear of harmful/poor treatment (44) were cited as barriers to immigrants’ and IMs’ (73) HSU. Some literature also refers to the objective quality of service, such as premature hospital discharge (74). Moreover, experiences or relationships with health personnel (71, 76) and trust in health providers (46, 77), factors that are related to the quality of service, were also cited as influencing factors of immigrants’ and IMs’ (58, 73, 78) HSU.
3.2.2.2. Subgroup-specific factors
First, the organization of the healthcare system was described in different aspects between immigrants and IMs, and the continuity of the healthcare system was mentioned only in the literature concerning immigrants. Fragmentation of the healthcare system (60), lack of continuity of care (46, 79, 80), and not having a general practitioner (81) were frequent complaints expressed by immigrants with unmet healthcare service needs. This difference might be because the structure of the healthcare delivery system and standard for healthcare services in different regions of a certain country are similar to each other.
Second, some factors of quality of the service were immigrant-specific factors, namely discrimination (39, 82, 83) and difficulty in communication (80) due to cultural differences (61, 84) and language barriers (74) during healthcare service. These factors were also important determinants that limited immigrants’ HSU because they determine the affective comfort during the service. Consequently, lacking special services, such as culturally safe and language-specific care (71), was also found to be associated with immigrants’ HSU.
3.2.2.3. Mediating effects on the relationship between macro-structural/contextual factors and HSU
Healthcare delivery systems in terms of volume, organization, quality, and cost in most countries are mainly run and funded by the governments or at least managed by the government (28, 29, 32, 85) and thus are influenced by government policy (86). Policies issued by the government can determine resource distribution, organization, financing, and pricing of the healthcare delivery system. Health providers’ attitudes toward immigrants were also found to be associated with the social context of an immigrant-friendly environment.
3.2.3. Characteristics of the population at risk and HSU
Characteristics of populations at risk associated with migrants’ HSU are related to the predisposing factors, enabling resources, and needs (27).
3.2.3.1. General factors
3.2.3.1.1. Predisposing factors
Predisposing factors associated with HSU are constituted by demographic characteristics, socioeconomic status, and health beliefs (27).
Referring to demographic characteristics, general factors, including gender, age, marital status, and education level, were found to be associated with health knowledge and attitude and thus affected migrants’ HSU. Gender was found to be associated with both immigrants’ (64, 71, 87–91) and IMs’ (12, 13, 17, 50, 55, 92–94) HSU; however, the association was mixed. Age also had a mixed effect on immigrants’ (64, 90) and IMs’ (12–14, 38, 92, 95, 96) HSU. Marital status was more frequently regarded as a protective factor for immigrants’ (81, 89, 97) and IMs’ (13, 14, 17, 50, 55) HSU, while some articles reported that marital status had no influence on HSU by IMs (12, 38). Higher education level was also shown to play a protective role in both immigrants’ (98) and IMs’ (99–104) HSU but did not have any influence on HSU in a few articles about IMs (38). Furthermore, IMs’ HSU is associated with the type of hukou (100, 105). The hukou system is a household registration system in China, categorizing people as either rural or urban residents (106). People with different hukou had different living environments, habits, and health beliefs and thus migrants from urban or rural areas had different HSU.
Migrant-specific demographic factors, including generation, race or ethnicity, and duration at a specific destination, were associated with immigrants’ and IMs’ HSU. First-generation immigrants (64, 107–109) and old-generation IMs (50) had worse HSU than the others because the early generation had more barriers to becoming integrated into society. The home country of the immigrants, including Asia or developing countries (88–91, 110, 111), and nationality (112) of IMs were found to be associated with HSU. Immigrants from some countries and some minority IMs possess special health beliefs and habits that can affect their HSU. A longer duration of residency would improve migrants’ social integration and familiarity with the healthcare system and decrease barriers to local medical insurance. Duration of residency in the destinations was found to be positively associated with HSU of immigrants (35, 89, 113, 114) and IMs (14, 15, 101, 115), while a few studies showed mixed results (87, 110).
Another factor associated with immigrants’ (64) and IMs’ (58, 103, 116) HSU is socioeconomic status. However, another article on IMs showed that this factor was not relevant (12). Socioeconomic status included different contexts that are related to living and working conditions. Some of these factors determine the most pressing problems that migrants suffer, which might include prior health problems. Referring to living conditions, studies on immigrants found that different types of accommodation (46, 113) and precarious living conditions (117) are associated with HSU. Working conditions associated with migrants’ HSU include work status and type of industry (for IMs), working conditions, employer-related factors, and job security. Employment status (100, 118, 119) and type of industry (11, 12, 55) were found to be associated with IMs’ HSU. Harsh working conditions are associated with immigrants’ HSU (43, 74). Unsupportive employers (82, 120), such as reluctance of employers to organize treatment for work-related accidents (45), would prevent immigrants from HSU. Barriers to immigrants’ HSU also included a lack of job security, such as fear of losing a job (63), a lack of discharge care (74), such as isolation, a lack of housing, food, and medical follow-up (74), and a loss of regular work wages (64, 74) or underpayment of medical leave wages (74). Some issues exist in both populations but are only described in one of these two populations. This difference might occur because of limited information.
In addition, literature on immigrants’ HSU showed that health belief identification (89) and health literacy (75, 98, 121) are associated with migrants’ HSU, and so are the IMs (58, 103). Quality of life (98) was also found to be a facilitator of immigrants’ HSU.
3.2.3.1.2. Enabling resources
Enabling resources associated with HSU are constituted by social and financial resources and access to healthcare (24, 27). Incorporation of these necessary resources would directly facilitate the HSU.
Referring to social resources, social isolation or support was found to be associated with immigrants’ (71, 84, 98) and IMs’ (15, 47, 58, 122) HSU. Specifically, not having someone to trust and confide (89) and lacking a person to accompany the immigrants to the healthcare facilities (97) were found to be associated with a decrease in HSU by immigrants, while immigrants with more negative family relationships had more HSU (123) because of the poor health status. The number of friends (14, 55, 95) is positively associated with IMs’ HSU, while the number of family members yielded mixed results (17, 38).
Financial resources are another aspect of enabling resources associated with migrants’ HSU. First, financial constraints (120) are often measured by wage or income and reflect the purchasing capacity for commodities, including health services, thus affecting the HSU of both immigrants (76, 82, 89, 97, 124, 125) and IMs (14, 17, 50, 55, 70, 72, 94, 99, 126–128). Satisfaction with income (92) appears to be related to HSU. Some researchers indicated that the competing priorities of daily living were barriers to immigrants’ (121) and IMs’ (11) HSU. However, minimal research on IMs found financial constraints (12), and major financial sources (38) are irrelevant because they do not directly determine the purchasing capacity for healthcare services. Second, since participation in any medical insurance program could effectively reduce the medical burden, medical insurance (13, 95, 129) is another important aspect of financial resources associated with migrants’ HSU and whether insurance is associated with immigrants’ (77, 82, 88, 130–132) and IMs’ (11, 12, 50, 57, 72, 78, 92, 100, 127, 128, 133) HSU. Immigrants’ HSU is associated with paying the medical insurance premium regularly (114), which was associated with the availability of medical insurance.
The authors divided the access to healthcare (128) into time accessibility, geographic accessibility, and information accessibility. The former two factors would affect both immigrants’ and IMs’ (78) HSU. First, time pressures (79), including lack of leave for illness (63), scheduling conflicts (59, 69, 90), and time flexibility (97), are associated with immigrants’ HSU. Long working hours are associated with immigrants’ (45) and IMs’ (72) HSU. The number of rest days is also associated with immigrants’ HSU (125). Second, distance to the health facilities was also found to be associated with immigrants’ and IMs’ (58) HSU (40, 60, 64). Some indices are only described in immigrants because of limited information.
3.2.3.1.3. Needs
Needs are another important individual-level factor that can be associated with migrants’ HSU (38, 64). Needs are measured by self-rated health and evaluated health assessments. A self-rated health assessment includes self-rated health and feeling different degrees of symptoms. In several studies, self-rated health was associated with immigrants’ (98, 114) and IMs’ (13, 17, 55) HSU. Feeling different degrees of symptoms was also found to be related to both immigrants’ (125) and IMs’ (50, 112, 126) HSU. Evaluated health can be measured by the disease status and the evaluated degree of symptoms. Disease status was associated with both immigrants’ (113, 131) and IMs’ (14, 17, 134) HSU. The evaluated degree of symptoms was related to IMs’ HSU in another study (135). Research on immigrants’ HSU found that reasons for hospitalization were not relevant (110), while the type of disease would determine IMs’ HSU (119).
3.2.3.2. Subgroup-specific factors
Differences exist in terms of some specific variables of predisposing factors and enabling resources.
3.2.3.2.1. Immigrant-specific factors
Referring to predisposing factors, some indices of demographic factors, including legal status and acculturation (language competence or communication barriers, discrimination or xenophobia, cultural difference, and self-identified), have only been associated with immigrants’ HSU. Legal status was an immigrant-specific factor, while reasons for migration have only been highlighted in studies concerning IMs. Specifically, immigrants with undocumented status (98, 136) had a lower level of utilization for various healthcare services (137) because their legal status was always a precondition for health system access. Acculturation is mentioned as a protective factor in the overwhelming majority of studies on immigrants’ HSU (138). These studies explain acculturation by language competence (40, 41, 43, 44, 46, 60, 62, 64, 65, 69, 76, 77, 79, 97, 114, 120, 124, 139, 140) or communication barriers (3, 117, 121), discrimination or xenophobia (3, 42, 43, 60, 65, 71, 120), cultural differences (62, 75, 76, 79, 89, 117, 121, 124), and self-identified (89). All factors induce poor affective comfort during the HSU process. Poor language competence and communication barriers also impede effective communication, which is very important to the health outcome and thus affects their HSU. Cultural differences would also affect communication (141).
Referring to enabling resources, information accessibility is a factor only frequently mentioned in immigrants’ HSU. Information accessibility or information barriers (42, 71, 117, 121) can be defined as a lack of awareness of laws and their rights regarding healthcare (62, 142, 143) and unfamiliarity with a new health system (41, 65, 77) (e.g., locations (82) and doctors (69)).
3.2.3.2.2. IMs-specific factors
Migration range, reasons for migration, and acculturation (language) are associated with IMs’ HSU. Migration range (13, 14) was associated with IMs’ HSU because the cultural difference including health attitudes always increased but social resources decreased along with the migration distance. The reason for migration (14, 15) was found to be associated with IMs’ HSU because the need for health maintenance and economic status differed between IMs for different migration-related reasons. Language was also reported to be associated with IMs’ HSU (115) by acting as a measurement of social integration, except for some Indian IMs (144). Although language is associated with both immigrants’ and IMs’ HSU, the influencing mechanism of language is different. Immigrants’ language competence would determine their ability to accurately communicate with doctors, while the dialect competence of IMs would only affect their discrimination or xenophobia from local doctors.
Referring to enabling resources, characteristics of medical insurance are associated with the availability of the insurance at the selected destinations and thus are related to IMs’ HSU. For example, medical insurance type (14, 100, 145) and place of insurance enrollment (14, 17, 50, 56, 105) were found to be associated with IMs’ HSU. These features would determine the level of insurance compensation and flexibility for IMs to transfer their medical insurance between hometowns and destinations (16, 17). This is because some types of medical insurance are not available in the local health system, and these local characteristics would determine the availability of medical insurance.
3.2.3.3. Mediating effects on the relationship between other determinants and HSU
Macro-structural/contextual factors and characteristics of healthcare delivery would affect the characteristics of the population at risk. First, non-health target policies could affect the characteristics of the population at risk. Limited by the policy, undocumented immigrants can seldom obtain work permits, which results in poverty and harsh living and working conditions (43). These precarious living conditions can also be associated with poor work-related housing (117). Second, healthcare policies affect the characteristics of the population at risk. For example, eligibility in enrollment of health insurance schemes, availability of cross-border health or social insurance schemes (26), and portability of health insurance in the hometown determine enrollment in available health insurance (134). Third, social, economic, and cultural environments can also influence migrants’ socioeconomic status, financial resources, social resources, and acculturation.
Characteristics of the healthcare delivery system can also affect the characteristics of the population at risk. The volume and organization can determine the access to healthcare of a country’s population, including migrants. Quality of service can affect the health outcome of migrants and their health service needs. The high costs of healthcare services have led to financial barriers to healthcare.
Finally, factors of the different dimensions of these characteristics of populations at risk are connected. On the one hand, factors affect the relationship between other factors and HSU. English language proficiency often mediates the relationship between gender and HSU (88). Social support has mediating effects on the relationships between HSU and independent variables, such as migrating duration and reason for migration (15), which also play a role in HSU. The unpredictable nature of out-of-pocket expenses can prevent migrants from seeking formal health services, thus ignoring their insurance enrollment (70). On the other hand, such factors can affect each other. Insurance enrollment was found to be associated with socioeconomic factors (116), including employment (11, 139), demographic characteristics (128), duration of migration (132), and financial constraints (70, 128). Language skills are often associated with the duration of migration (132). Time accessibility (70) and needs (133) can also be associated with financial constraints.
3.3. Choice of types/sites
Depending on the progression of the disease, the populations at risk can use different types of services, including preventive services (primary care), outpatient services/emergency services (secondary care), and inpatient services in sequence. The latter two are provided for patients, while the first was mainly provided for all of the populations. Emergency services are open almost all year round and can provide immediate help by specialists in the hospital (146), thus providing better access to healthcare services. Moreover, immigrant patients also use traditional services (147). Depending on the site of service providers, the patients can use services from pharmacies, clinics, and hospital services (including emergency services). The providers can be private or communal/public. Health providers in some countries can be divided into different levels with different levels of services (32), and patients can choose them freely (28–31).
The immigrants had a higher utilization rate of emergency services during off-peak hours (3, 90, 148, 149) and underuse of primary healthcare services (3, 147) and preventive services (147). As a result, immigrants had a higher risk of avoidable hospitalization (150). Referring to the site of healthcare, immigrants were found to be more likely to use healthcare services from public health facilities, while the general population also used private healthcare (151). However, IMs in some countries are more likely to visit private providers (33, 37), traditional healers (37), and pharmacies (72) because of the lower costs associated with these healthcare service formats. In countries with different levels of hospitals, IMs were found to be less likely to choose high-level hospitals than residents (33). The determinations could also be divided into three dimensions: (1) macro-structural/contextual factors; (2) characteristics of the health delivery system; and (3) characteristics of the population at risk. However, the influence mechanisms differed from those of HSU. Some determinants were also different from those of HSU.
3.3.1. Macro-structural/contextual factors
Choice of types/sites was found to be associated with macro-structural/contextual factors, namely health policy, non-health targeted policies, and social, economic, and cultural conditions. The influence mechanisms were different from HSU choices. The healthcare policy regulates the rules of searching for healthcare, including the choice of sites. In some countries, patients, including migrants, can choose healthcare facilities freely (28–31), while in others, they can only utilize healthcare services in a certain order to obtain relatively cheap services (32, 152). The effects of non-health-targeted policies are also reflected in immigrants as obtaining the relevant documentation necessary to register their child’s birth is an important factor considered by immigrant women during their care-seeking decision-making (153), including the choice of sites.
Social conditions were also found to be associated with patients’ choices of sites. Insufficient research on migrants at present exists. IMs’ choice of sites for healthcare was found to be associated with the region (154) and province (22) in which they were living. In the general population, physical environment (155) is associated with patients’ choice of sites for health services, but the choice of cities was not relevant to their choices (156). Minority patients appear to be more likely to use services from hospitals with more minority patients (157).
3.3.2. Characteristics of the health delivery system
Characteristics of a healthcare delivery system, namely volume, organization, quality of service, and cost, are also associated with the choice of healthcare type or site. These characteristics have different influence mechanisms on the HSU. Extensive research on the association between characteristics of the health delivery system and the general population’s choice of healthcare type or site has been done, while there was minimal research concerning immigrants and no research concerning IMs.
First, induced demand is a common problem in the health service market; thus, volume was found to be one important factor associated with the general population’s choice of healthcare site, but a lack of research on migrants exists. A higher density of hospitals was found to be associated with lower use of primary care facilities (158) among the general population. Higher physician densities are associated with a greater probability of visiting such health facilities (158, 159). However, insufficient research concerning migrants and the association between the volume and choice of sites is available. Second, previous studies had proved that organization (visit time or waiting time (146, 160, 161)) was an important factor associated with the choice of healthcare site with little research showing negative results (156) in the general population. In terms of immigrants, visit time and 24-h medical consultations (162) were found to be important factors associated with the choice of healthcare site because these factors reflect the efficiency of the health facilities and are associated with the time accessibility of immigrants. Third, motivated by quality preference, the quality of service (160, 163, 164) was also found to be an important factor associated with the general population’s choice of healthcare type and site. In this study, the quality of service was measured by different indices, such as facility size (160), reputation/word of mouth (155, 165), equipment (160, 166), providers’ medical skills (155, 160)/school of graduation (167) and/or the presence of a specialist (146, 166), perceived quality of care (164), providers’ interpersonal behavior (155), positive experience with the facility (146, 165, 166), specific quality information provided by performance reports (165), average health gain (168), and complication rates (169). In terms of immigrants, the quality of service (153) including providers’ medical skills (162, 170) was also reported to be associated with the choice of healthcare site. Fourth, in the perception of cost performance, cost (155), especially out-of-pocket cost (161) or affordability of a facility, was considered another factor associated with the choice of sites in the general population. Cost (153) was also found to be an important consideration for immigrants.
3.3.3. Characteristics of the population at risk
The characteristics of the population at risk associated with the choice of sites also could be divided into predisposing factors, enabling resources, and needs. The internal mechanisms of these factors were also different from the HSU. Some issues exist in both populations but are only described in one of these two populations.
Predisposing factors were divided into demographic factors and socioeconomic status. Migrants with different demographic and socioeconomic characteristics reported different preferences as to the site or type of HSU. First, demographic factors were found to be associated with the choice of sites for IMs (22) and immigrants. Specifically, age (90, 162, 171), gender (90), and education (171–173) were reported to be associated with immigrants’ choice of sites and types (162, 171). IMs’ choice of healthcare site was also associated with education level (100). Furthermore, legal status, generation, race or ethnicity, migration characteristics, and acculturation were also found to be associated with the choice of healthcare site or type. Rural or urban registration (33) and the generation (50) were associated with the choice of healthcare site and type among IMs, and this finding might be associated with differences in their HSU habits. Similarly, nationality was also associated with the choice of healthcare type or site among immigrants (90, 173). Immigration background was not relevant in the choice of sites (174) in the general population in addition to IMs after considering the other confounding factors (175). Some variables are IM-specific factors. Migration characteristics (22), including migration range (176), were found to be associated with the choice of sites among IMs. Some variables are immigrant-specific factors. Not maintaining their identity was a major reason for the reluctance to seek treatment at a public hospital (172) among immigrants. Duration of migration (172) and language (153, 172) were also associated with the utilization of public hospitals among immigrants. Second, socioeconomic status was associated with IMs’ and immigrants’ choices of sites (22, 154). The type of industry was associated with obtaining medications from a drug store (172) among immigrants.
Enabling resources consisted of financial resources and access to healthcare. Better enabling resources for a healthcare facility was associated with higher utilization of this facility. First, financial resources included financial constraints and medical insurance. Financial constraints are often measured by wage or income and were associated with the choice of healthcare site or type (171) among IMs (127) and immigrants (171, 172). Medical insurance was another important aspect of financial resources associated with immigrants’ (172, 173) and IMs’ (127) choices of healthcare sites with some negative results (22, 154) among IMs. The average reimbursement rate of medical insurance (159) and/or out-of-pocket costs (161) were also found to be important considerations in the choice of healthcare site in the general population, but no study has been performed on migrants’ views of this aspect. Second, access to healthcare (170, 173), especially geographic accessibility (153), was associated with immigrants’ choice of healthcare site, but no study could be found concerning IMs. We did not find any research on the association between social resources and migrants’ choice of sites or types.
Needs were measured by self-reported health and evaluated health assessments. Self-rated health (173) was associated with immigrants’ choice of healthcare type. Feeling different degrees of symptoms was another factor considered by immigrants (74) and IMs (50) when choosing healthcare sites. Disease type was also associated with immigrants’ (173) and IMs’ (22) choice of healthcare site. They tended to choose higher-level health facilities, which are supposed to be of higher quality, for severe symptoms and diseases.
3.4. Medical locations
The choice of the location of healthcare services (named medical location) by the migrants could be divided into three categories: (1) hometown/home country, also named medical return; (2) host city/destination; and (3) other places, also named cross-border medical or medical tourism (20). The cost of healthcare might range across different regions within certain countries or different countries (21, 32) consistent with the level of economic development. The use of medical services in developed regions by populations from developing regions would help to meet their health need, attain the health system goals of developing countries (177), and stimulate improvements in the quality of local health services (178). Migrants’ preference for medical locations also depended on macro-structural/contextual factors, characteristics of the health delivery system, and characteristics of the population at risk. Some of the influence mechanisms were similar to the HSU and choice of types or sites; however, differences in the constituent and importance of determinants were found.
3.4.1. Macro-structural/contextual factors
Macro-structural/contextual factors associated with medical locations consist of healthcare policy and social, economic, and cultural conditions. The influence mechanism differed from those of choice of types or sites. Limited by the healthcare policy, IMs in China could only get higher reimbursement from their medical insurance by returning for medical services before the promotion of the on-the-spot medical bill settlement system. Medical travel from Cambodia was driven and shaped by the interaction of the healthcare system and socio-economic or cultural factors at different levels, including regional trade liberalization and the pressure of relatives and other advisers in local communities (178). The medical diaspora organizations could facilitate health service utilization of immigrants in that particular destination (177), thus reducing their medical return. The locations in which the patients lived were also found to be associated with their medical travel (20).
3.4.2. Characteristics of the health delivery system
The characteristics of the healthcare delivery system, including quality of service (178) and cost, were associated with patients’ medical locations. The influencing mechanism was similar to that of the choice of types or sites. However, the constituent of determinants was different. First, the pursuit of quality healthcare (179), perceived quality of healthcare (21, 180), and dissatisfaction with the current system (21, 181) would lead to an increase in transnational medical utilization of the immigrants. Perception of low quality of health services also was a motive for the medical return of immigrants (182–186). Second, cost (186, 187) or value for money (21) was found to be another factor associated with the medical location of immigrants. Some researchers indicated that affordability did not emerge as an independent motive but influenced the other factors (182). Moreover, seeking second opinions (21, 181, 182, 188) also emerged as a motivation for transnational medical utilization. No evidence of the relationship between medical locations and the volume or organization of the health delivery system was found.
3.4.3. Characteristics of the population at risk
The characteristics of the population at risk included predisposing factors, enabling resources, and needs. Their influence mechanisms were similar to the HSU than the choice of types and sites. Some issues exist in both populations but are only described in one of these two populations.
Predisposing factors were divided into demographic factors and socioeconomic status. First, demographic factors, including gender, age, nationality, acculturation, duration in the destinations, and characteristics of migration, were associated with migrants’ medical locations. Acculturation was found to play a more important role in the choice of medical locations than the choice of types or sites. Gender (189), age (189, 190), and education level (174, 190) were associated with IMs’ medical locations. Nationality (181) was enumerated in immigrants’ medical returns. Social integration was associated with immigrants’ (188) and IMs’ (e.g., permanent settlement intention (18, 191)) medical locations. The immigrant population had a mixed result (192) in terms of social integration. Duration at the destinations was another factor associated with the healthcare locations of IMs (190). Some variables are IM-specific factors. The characteristics of migration, including the reason for migration (190) and migration accompanied by someone (191), were associated with IMs’ medical return. Some variables are immigrant-specific factors. Acculturation measured by language and communication (21, 180), discrimination experiences (188), and cultural differences (183, 193) was associated with immigrants’ medical locations for which the latter yielded mixed results (192). In addition, medical culture was previously mentioned in studies on immigrants (21, 181, 182, 187). Second, socioeconomic status, such as working status (118) and owning a house (190), was also associated with IMs’ medical return.
Enabling resources included financial and social resources and access to healthcare. These determinants and their influence mechanisms were found to be similar to the HSU. First, financial resources consisted of financial constriction and medical insurance. The financial resources had a mixed association with the healthcare locations (174, 194) in the general population. Although we did not find any literature on the association between migrants’ medical locations and financial constriction, financial status was a precondition for medical travel (183). Enrollment status in the accessible medical insurance was another factor associated with the medical locations of immigrants (21, 180, 184) and IMs (190, 191, 195), especially the local medical insurance (184, 191). The characteristics of medical insurance, such as the location/type (18, 195) and compensation rules (193) of a specific form of medical insurance, were also described in the literature concerning migrants. Second, social resources as measured by relatives living in their home country by immigrants (196) and family members living together by IMs (190) were found to be another factor associated with medical locations. Three, access to healthcare at the selected destination was also associated with migrants’ medical locations. Established healthcare records in the current residency (190) were found to be negatively associated with IMs’ medical return but having a usual source of care (180) was not a significant factor associated with immigrants’ medical return. The perception of availability (182, 185), including convenience (186) and time availability (21), was reported to be associated with immigrants’ medical returns. Furthermore, immigrants who had a high level of digital information technology use were more likely to undertake medical tourism than others with less technology use (192).
Needs measured by self-reported health and evaluated health were associated with immigrants’ (181) and IMs’ medical locations, but only research concerning immigrants was found. Self-reported health assessments were found to be associated with the medical return of immigrants (181, 184) with few negative results (180). Perceived severity of disease was also associated with immigrants’ medical return (77). Some disease types, such as major non-work-related injuries and chronic diseases (74), neoplasms, and diseases of the circulatory system (189), were associated with immigrants’ medical return (74) and populations’ medical travel (189).
4. Conclusion
Our study established a conceptual framework for migrant HSB. This conceptual framework included and delineated the determinants of immigrants’ and IMs’ HSB, provided new knowledge concerning the determinants of immigrants and IMs’ HSB, reclassified some dimensions of the determinants, explained the relationships between different characteristics of HSB, and indicated the differences in terms of their determinants. The results of this study may help facilitate a better understanding of the HSB of migrants and the management of medical insurance funds.
Following the previous models describing general populations and immigrants’ HSB, we divided the determinants of migrants’ HSB into three dimensions: (1) macro-structural/contextual factors; (2) characteristics of healthcare delivery system; and (3) characteristics of populations at risk. The classifications of determinants were consistent with Anderson’s model. The macro-structural/contextual factors consisted of healthcare policies, non-health-targeted policies, and specific regional context factors related to larger social, economic, and cultural conditions. Characteristics of the population at risk were categorized as predisposing factors, enabling resources, and needs. Characteristics of HSB were divided into different aspects, including site, type, location, and utilization. We also specified the mediating effects of some variables and the path of their influence on HSB.
We modified previous models. First, we distinguished the determinants of immigrants’ and IMs’ HSB. Some determinants, such as non-healthcare policies, the continuity of the healthcare system, legal status, acculturation, and information accessibility, were associated with immigrants’ HSB but seldom affected IMs’ HSB. Other factors associated with IMs’ HSB but ignored in the literature on immigrants included reasons for migration, migration range, and characteristics of the medical insurance. Determinants related to regional context were more complex among IMs, while only cultural aspects made sense for immigrants. Second, we reclassified some dimensions of the determinants. This new conceptual framework divides the characteristics of the health delivery system into volume, organization, quality, and cost. Access to healthcare was divided into time accessibility, geographic accessibility, and information accessibility. Information accessibility acted as an important barrier to immigrants’ HSU. Third, we divided the characteristics of HSB into site/type, locations, and utilization. We merged the type and site because they were found to be closely associated with each other and reflect healthcare accessibility and the quality of services the patients receive. Fourth, we highlighted the interaction of the site and location of HSB. By enumerating the determinants of site and location, respectively, we showed the difference in determinants between different aspects of HSB. However, this conceptual framework might need to be adjusted when studying the HSB of special populations, such as displaced persons. Moreover, the characteristic of time interval on HSB was not included in this conceptual framework. Revisions would be necessary if new determinants and relationships are found in future studies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
BP developed the concept of the manuscript, conducted the literature search, developed the conceptual framework, and drafted the manuscript. LL conceptualized this study and manuscript. All authors provided critical feedback, revised the manuscript for intellectual content, and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 71904211).
Acknowledgments
We thank all members of the research team for their hard work in the process of research design and manuscript writing. We thank the Charlesworth Group for their assistance in language editing. We also would like to thank the family members of the first author for their support during the period of manuscript writing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HSB, health service behaviors; HSU, health service utilization; SDG, Sustainable Development Goal; IMs, internal migrants.
References
1. UN. Sustainable development goal 3 (2016). Available at: https://www.globalgoals.org/goals/3-good-health-and-well-being/
2. Klugman, J. Human development report 2009. Overcoming barriers: human mobility and development. UNDP-HDRO Human Development Reports 2009 (2009).
3. Lebano, A, Hamed, S, Bradby, H, Gil-Salmerón, A, Durá-Ferrandis, E, Garcés-Ferrer, J, et al. Migrants' and refugees' health status and healthcare in Europe: a scoping literature review. BMC Public Health. (2020) 20:1039. doi: 10.1186/s12889-020-08749-8
4. Xu, H, Yang, H, Wang, H, and Li, X. The association of residence permits on utilization of health care services by migrant workers in China. Int J Environ Res Public Health. (2021) 18:9623. doi: 10.3390/ijerph18189623
5. McAuliffe, M. AT, editors. World migration report 2022. Geneva: International Organization for Migration (IOM) (2021).
6. Sznajder, KK, Winchester, MS, Biney, AAE, Dodoo, ND, Letsa, D, and Dodoo, FN. The migration experience and differential risks to sexual and reproductive health in Ghana. Health Educat Behav. (2020) 47:718–27. doi: 10.1177/1090198120939492
7. Jahn, HJ, Ling, L, Han, L, Xia, Y, and Krämer, A. Migration and health in megacities: a Chinese example from Guangzhou, China In: A Krämer, MH Khan, and F Kraas, editors. Health in megacities and urban areas. Heidelberg: Physica-Verlag HD (2011). 189–208. doi: 10.1007/978-3-7908-2733-0_12
8. do, HN, Vu, M, Nguyen, AT, Nguyen, HQT, Bui, TP, Nguyen, QV, et al. Do inequalities exist in housing and working conditions among local and migrant industrial workers in Vietnam? Results from a multi-site survey. Saf Sci. (2021) 143:105400. doi: 10.1016/j.ssci.2021.105400
9. Jayaram, N, and Varma, D. Examining the ‘Labour’ in labour migration: migrant workers' informal work arrangements and access to labour rights in urban sectors. Indian J Labour Econom. (2020) 63:999–1019. doi: 10.1007/s41027-020-00288-5
10. Zhang, J, Lin, S, Liang, D, Qian, Y, Zhang, D, and Hou, Z. Public health services utilization and its determinants among internal migrants in China: evidence from a nationally representative survey. Int J Environ Res Public Health. (2017) 14:1002. doi: 10.3390/ijerph14091002
11. Lattof, S, Coast, E, and Leone, T. Priorities and challenges accessing health care among female migrants. Health Serv Insights. (2018) 11:1178632918804825. doi: 10.1177/1178632918804825
12. Le, A, Vu, L, and Schelling, E. Utilization of health care services among internal migrants in Hanoi and its correlation with health insurance: a cross-sectional study. Tap chi y te cong cong. (2015) 3:44–56.
13. Niu, L, Liu, Y, and Wang, X. Using nomogram to predict the hospitalization forgone among internal migrants in China: A nationally representative cross-sectional secondary data analysis. Risk Manag Healthcare Pol. (2021) 14:3945–54. doi: 10.2147/RMHP.S301234
14. Zhang, X, Yu, B, He, T, and Wang, P. Status and determinants of health services utilization among elderly migrants in China. Global Health Res Policy. (2018) 3:8. doi: 10.1186/s41256-018-0064-0
15. Long, C, Wang, R, Feng, D, Ji, L, Feng, Z, and Tang, S. Social support and health services use in people aged over 65 years migrating within China: A cross-sectional study. Int J Environ Res Public Health. (2020) 17:4651. doi: 10.3390/ijerph17134651
16. Fang, H, Jin, Y, Zhao, M, Zhang, H, Rizzo, JA, Zhang, D, et al. Does migration limit the effect of health insurance on hypertension management in China? Int J Environ Res Public Health. (2017) 14:1256. doi: 10.3390/ijerph14101256
17. Zhao, X, Ming, D, and Ma, W. Utilization and cost of outpatient care and their influencing factors among middle and aged peasant-workers in China. Beijing da xue xue bao Yi xue ban. (2015) 47:464–8. doi: 10.3969/j.issn.1671-167X.2015.03.018
18. Peng, BL, and Ling, L. Association between rural-to-urban migrants' social medical insurance, social integration and their medical return in China: a nationally representative cross-sectional data analysis. BMC Public Health. (2019) 19:86. doi: 10.1186/s12889-019-6416-y
19. Müller, A. Hukou and health insurance coverage for migrant workers. J Curr Chin Aff. (2016) 45:53–82. doi: 10.1177/186810261604500203
20. De Curtis, M, Bortolan, F, Diliberto, D, and Villani, L. Pediatric interregional healthcare mobility in Italy. Ital J Pediatr. (2021) 47:139. doi: 10.1186/s13052-021-01091-8
21. Mathijsen, A, and Mathijsen, FP. Diasporic medical tourism: a scoping review of quantitative and qualitative evidence. Glob Health. (2020) 16:27. doi: 10.1186/s12992-020-00550-x
22. Haiqin, W, Yongyi, W, and Zhiyuan, H. Does health insurance impact on the hospital seeking behavior among floating population? Evidence from the 2014 National Floating Population Dynamic Monitoring Survey. Chin J Health Pol. (2016) 9:61–6. doi: 10.3969/j.issn.1674-2982.2016.05.011
23. Horton, SB. Medical returns as class transformation: situating migrants' medical returns within a framework of transnationalism. Med Anthropol. (2013) 32:417–32. doi: 10.1080/01459740.2012.749875
24. Yang, PQ, and Hwang, SH. Explaining immigrant health service utilization: A theoretical framework. SAGE Open. (2016) 6:2158244016648137. doi: 10.1177/2158244016648137
25. Andersen, RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
26. Legido-Quigley, H, Pocock, N, Tan, ST, Pajin, L, Suphanchaimat, R, Wickramage, K, et al. Healthcare is not universal if undocumented migrants are excluded. BMJ. (2019) 366:l4160. doi: 10.1136/bmj.l4160
27. Aday, LA, and Andersen, R. A framework for the study of access to medical care. Health Serv Res. (1974) 9:208–20.
29. Blümel, M, Spranger, A, Achstetter, K, Maresso, A, and Busse, R. Germany: health system review. Health Syst Transit. (2020) 22:1–272.
30. Younger, DS. Health Care in India. Neurol Clin. (2016) 34:1103–14. doi: 10.1016/j.ncl.2016.06.005
31. Yang, N, Shen, L, Shu, T, Liao, S, Peng, Y, and Wang, J. An integrative method for analyzing spatial accessibility in the hierarchical diagnosis and treatment system in China. Soc Sci Med. (2021) 270:113656. doi: 10.1016/j.socscimed.2020.113656
32. González Block, M, Reyes Morales, H, Hurtado, LC, Balandrán, A, and Méndez, E. Mexico: health system review. Health Syst Transit. (2020) 22:1–222.
33. Wei, X, Pearson, S, Zhang, Z, Qin, J, Gerein, N, and Walley, J. Comparing knowledge and use of health services of migrants from rural and urban areas in Kunming City. China J Biosoc Sci. (2010) 42:743–56. doi: 10.1017/S0021932010000313
34. Xu, J, Chen, X, Liu, K, Guo, G, and Li, Y. Health service utilization of international immigrants in Yiwu, China: implication for health policy. J Immigr Minor Health. (2021) 23:207–14. doi: 10.1007/s10903-020-01066-7
35. Saunders, CL, Steventon, A, Janta, B, Stafford, M, Sinnott, C, Allen, L, et al. Healthcare utilization among migrants to the UK: cross-sectional analysis of two national surveys. J Health Serv Res Policy. (2021) 26:54–61. doi: 10.1177/1355819620911392
36. Pega, F, Govindaraj, S, and Tran, NT. Health service use and health outcomes among international migrant workers compared with non-migrant workers: A systematic review and meta-analysis. PLoS One. (2021) 16:e0252651. doi: 10.1371/journal.pone.0252651
37. Ginsburg, C, Collinson, MA, Gómez-Olivé, FX, Gross, M, Harawa, S, Lurie, MN, et al. Internal migration and health in South Africa: determinants of healthcare utilisation in a young adult cohort. BMC Public Health. (2021) 21:554. doi: 10.1186/s12889-021-10590-6
38. Ma, S, Zhou, X, Jiang, M, Li, Q, Gao, C, Cao, W, et al. Comparison of access to health services among urban-to-urban and rural-to-urban older migrants, and urban and rural older permanent residents in Zhejiang Province, China: a cross-sectional survey. BMC Geriat. (2018) 18:174. doi: 10.1186/s12877-018-0866-4
39. White, J, and Rispel, L. Policy exclusion or confusion? Perspectives on universal health coverage for migrants and refugees in South Africa. Health Policy Plan. (2021) 36:1292–306. doi: 10.1093/heapol/czab038
40. Leppälä, S, Lamminpää, R, Gissler, M, and Vehviläinen-Julkunen, K. Hindrances and facilitators in humanitarian migrants' maternity care in Finland: qualitative study applying the three delays model framework. Scand J Caring Sci. (2020) 34:148–56. doi: 10.1111/scs.12716
41. Hahn, K, Steinhäuser, J, and Goetz, K. Equity in health care: A qualitative study with refugees, health care professionals, and administrators in one region in Germany. Biomed Res Int. (2020) 2020:4647389. doi: 10.1155/2020/4647389
42. Germain, S, and Yong, A. COVID-19 highlighting inequalities in access to healthcare in England: A case study of ethnic minority and migrant women. Fem Leg Stud. (2020) 28:301–10. doi: 10.1007/s10691-020-09437-z
43. Fleischman, Y, Willen, SS, Davidovitch, N, and Mor, Z. Migration as a social determinant of health for irregular migrants: Israel as case study. Soc Sci Med. (2015) 147:89–97. doi: 10.1016/j.socscimed.2015.10.046
44. Alawa, J, Zarei, P, and Khoshnood, K. Evaluating the provision of health services and barriers to treatment for chronic diseases among Syrian refugees in Turkey: A review of literature and stakeholder interviews. Int J Environ Res Public Health. (2019) 16:2660. doi: 10.3390/ijerph16152660
45. Regmi, P, van Teijlingen, E, Mahato, P, Aryal, N, Jadhav, N, Simkhada, P, et al. The health of Nepali migrants in India: A qualitative study of lifestyles and risks. Int J Environ Res Public Health. (2019) 16:3655. doi: 10.3390/ijerph16193655
46. Rodella Sapia, M, Wangmo, T, Dagron, S, and Elger, B. Understanding access to professional healthcare among asylum seekers facing gender-based violence: a qualitative study from a stakeholder perspective. BMC Int Health Hum Rights. (2020) 20:25. doi: 10.1186/s12914-020-00244-w
47. Gawde, NC, Sivakami, M, and Babu, BV. Utilization of maternal health services among internal migrants in Mumbai, India. J Biosoc Sci. (2016) 48:767–96. doi: 10.1017/S0021932016000195
48. Juárez, S, Honkaniemi, H, Dunlavy, A, Aldridge, R, Barreto, M, Katikireddi, S, et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. Lancet Glob Health. (2019) 7:e420–35. doi: 10.1016/S2214-109X(18)30560-6
49. Wang, R, Rojo, M, Crosby, S, and Rajabiun, S. Examining the impact of restrictive federal immigration policies on healthcare access: perspectives from immigrant patients across an urban safety-net hospital. J Immigr Minor Health. (2022) 24:178–87. doi: 10.1007/s10903-021-01177-9
50. Guan, Y, Zhang, M, Zhang, X, Zhao, Z, Huang, Z, Li, C, et al. Medical treatment seeking behaviors and its influencing factors in employed floating population in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:301–8. doi: 10.3760/cma.j.issn.0254-6450.2019.03.009
51. Thapa, NR, Adhikari, S, and Budhathoki, PK. Influence of internal migration on the use of reproductive and maternal health services in Nepal: an analysis of the Nepal Demographic and Health Survey 2016. PLoS One. (2019) 14:e0216587. doi: 10.1371/journal.pone.0216587
52. Şantaş, G, Erigüç, G, and Eryurt, MA. The impact of internal migration on the maternal and child health services utilization in Turkey. Soc Work Public Health. (2019) 34:519–28. doi: 10.1080/19371918.2019.1635941
53. Cotton, C. Migration and young women's access to maternal healthcare in sub-Saharan Africa. Health Place. (2019) 55:136–44. doi: 10.1016/j.healthplace.2018.12.006
54. Xie, Y, Guo, Q, and Meng, Y. The health service use of aged rural-to-urban migrant workers in different types of cities in China. BMC Health Serv Res. (2021) 21:606. doi: 10.1186/s12913-021-06638-3
55. Li, D, Zhai, S, Zhang, J, Yang, J, and Wang, X. Assessing income-related inequality on health service utilization among Chinese rural migrant workers with new co-operative medical scheme: A multilevel approach. Int J Environ Res Public Health. (2021) 18:10851. doi: 10.3390/ijerph182010851
56. Li, D, Zhu, L, Zhang, J, and Yang, J. Decomposing differences of health service utilization among Chinese rural migrant workers with new cooperative medical scheme: A comparative study. Int J Environ Res Public Health. (2021) 18:9291. doi: 10.3390/ijerph18179291
57. Le, AT-K. Health and access to health services of rural-to-urban migrant populations in Viet Nam. Basel: University of Basel (2013).
58. Mohamed, AA, Bocher, T, Magan, MA, Omar, A, Mutai, O, Mohamoud, SA, et al. Experiences from the field: A qualitative study exploring barriers to maternal and child health service utilization in IDP settings Somalia. Int J Women's Health. (2021) 13:1147–60. doi: 10.2147/IJWH.S330069
59. Castaldo, M, Cavani, A, Segneri, MC, Costanzo, G, and Marrone, R. Anthropological study on Chagas Disease: sociocultural construction of illness and embodiment of health barriers in Bolivian migrants in Rome, Italy. PLoS One. (2020) 15:e0240831. doi: 10.1371/journal.pone.0240831
60. Gebreyesus, T, Gottlieb, N, Sultan, Z, Ghebrezghiabher, H, Tol, W, Winch, P, et al. Barriers to contraceptive careseeking: the experience of Eritrean asylum-seeking women in Israel. Ethn Health. (2020) 25:255–72. doi: 10.1080/13557858.2017.1418299
61. Scott, H, and Wallis, N. Maternity care for refugees living in Greek refugee camps: what are the challenges to provision? Birth. (2021) 48:114–21. doi: 10.1111/birt.12522
62. Ang, J, Koh, C, Chua, B, Narayanaswamy, S, Wijaya, L, Chan, L, et al. Are migrant workers in Singapore receiving adequate healthcare? A survey of doctors working in public tertiary healthcare institutions. Singap Med J. (2020) 61:540–7. doi: 10.11622/smedj.2019101
63. Joshi, S, Simkhada, P, and Prescott, G. Health problems of Nepalese migrants working in three gulf countries. BMC Int Health Hum Rights. (2011) 11:3. doi: 10.1186/1472-698X-11-3
64. Klein, J, and von dem Knesebeck, O. Inequalities in health care utilization among migrants and non-migrants in Germany: a systematic review. Int J Equity Health. (2018) 17:160. doi: 10.1186/s12939-018-0876-z
65. Kang, C, Tomkow, L, and Farrington, R. Access to primary health care for asylum seekers and refugees: a qualitative study of service user experiences in the UK. Br J Gen Pract. (2019) 69:e537–45. doi: 10.3399/bjgp19X701309
66. Hesketh, T, Ye, X, Li, L, and Wang, H. Health status and access to health care of migrant workers in China. Public Health Reports. (2008) 123:189–97. doi: 10.1177/003335490812300211
67. Liang, Y, and Guo, M. Utilization of health services and health-related quality of life research of rural-to-urban migrants in China: A cross-sectional analysis. Soc Indic Res. (2015) 120:277–95. doi: 10.1007/s11205-014-0585-y
68. Su, S, Zhang, F, Liu, Q, Wang, Y, Wen, J, Tang, X, et al. Factors associated with utilization of reproductive healthcare services among migrant women workers in Chong Qing, China. Int J Gynecol Obstet. (2014) 127:66–8. doi: 10.1016/j.ijgo.2014.04.005
69. Kohlenberger, J, Buber-Ennser, I, Rengs, B, Leitner, S, and Landesmann, M. Barriers to health care access and service utilization of refugees in Austria: evidence from a cross-sectional survey. Health Policy. (2019) 123:833–9. doi: 10.1016/j.healthpol.2019.01.014
70. Lattof, S. Health insurance and care-seeking behaviours of female migrants in Accra. Ghana Health Policy Plann. (2018) 33:505–15. doi: 10.1093/heapol/czy012
71. Machado, S, Wiedmeyer, M, Watt, S, Servin, A, and Goldenberg, S. Determinants and inequities in sexual and reproductive health (SRH) care access among Im/migrant women in Canada: findings of a comprehensive review (2008–2018). J Immigr Minor Health. (2022) 24:256–99. doi: 10.1007/s10903-021-01184-w
72. Peng, Y, Chang, W, Zhou, H, Hu, H, and Liang, W. Factors associated with health-seeking behavior among migrant workers in Beijing. China BMC Health Services Research. (2010) 10:69. doi: 10.1186/1472-6963-10-69
73. Mirkuzie, AH. Exploring inequities in skilled care at birth among migrant population in a metropolitan city Addis Ababa, Ethiopia; a qualitative study. Int J Equity Health. (2014) 13:110. doi: 10.1186/s12939-014-0110-6
74. Tam, WJ, Goh, WL, and Chua, J. 健康是本钱 – Health is my capital: a qualitative study of access to healthcare by Chinese migrants in Singapore. Int J Equity Health. (2017) 16:102. doi: 10.1186/s12939-017-0567-1
75. Raymundo, G, Smith-Merry, J, and McNab, J. Experiences of health service literacy and access amongst Australian young adults from migrant backgrounds. Health Promot J Austr. (2021) 32:69–79. doi: 10.1002/hpja.408
76. Salami, B, Mason, A, Salma, J, Yohani, S, Amin, M, Okeke-Ihejirika, P, et al. Access to healthcare for immigrant children in Canada. Int J Environ Res Public Health. (2020) 17:3320. doi: 10.3390/ijerph17093320
77. Qiu, J, Song, D, Nie, J, Su, M, Hao, C, Gu, J, et al. Utilization of healthcare services among Chinese migrants in Kenya: a qualitative study. BMC Health Serv Res. (2019) 19:995. doi: 10.1186/s12913-019-4846-y
78. Siddaiah, A, Kant, S, Haldar, P, Rai, SK, and Misra, P. Maternal health care access among migrant women labourers in the selected brick kilns of district Faridabad, Haryana: mixed method study on equity and access. Int J Equity Health. (2018) 17:171. doi: 10.1186/s12939-018-0886-x
79. van Loenen, T, van den Muijsenbergh, M, Hofmeester, M, Dowrick, C, van Ginneken, N, Mechili, E, et al. Primary care for refugees and newly arrived migrants in Europe: a qualitative study on health needs, barriers and wishes. Eur J Pub Health. (2018) 28:82–7. doi: 10.1093/eurpub/ckx210
80. Brandenberger, J, Tylleskär, T, Sontag, K, Peterhans, B, and Ritz, N. A systematic literature review of reported challenges in health care delivery to migrants and refugees in high-income countries – the 3C model. BMC Public Health. (2019) 19:755. doi: 10.1186/s12889-019-7049-x
81. Linhas, R, Oliveira, O, Meireles, P, Oliveira, P, de Melo, MB, Lourenço, J, et al. Immigrants' access to health care: problems identified in a high-risk tuberculosis population. Pulmonology. (2019) 25:32–9. doi: 10.1016/j.pulmoe.2018.04.002
82. Adhikary, P, Aryal, N, Dhungana, R, KC, RK, Regmi, P, Wickramage, K, et al. Accessing health services in India: experiences of seasonal migrants returning to Nepal. BMC Health Serv Res. (2020) 20:992. doi: 10.1186/s12913-020-05846-7
83. White, J, Blaauw, D, and Rispel, L. Social exclusion and the perspectives of health care providers on migrants in Gauteng public health facilities, South Africa. PLoS One. (2020) 15:e0244080. doi: 10.1371/journal.pone.0244080
84. Žagar, M, Rotar Pavlič, D, Švab, I, Maksuti, A, Ilić, B, Smrekar, M, et al. Through health workers' eyes: a qualitative study of health service provision for migrants at Schengen border. Int J Equity Health. (2019) 18:117. doi: 10.1186/s12939-019-1022-2
85. Cylus, J, Richardson, E, Findley, L, Longley, M, O'Neill, C, and Steel, D. United Kingdom: health system review. Health Syst Transit. (2015) 17:1–126.
86. Tao, W, Zeng, Z, Dang, H, Lu, B, Chuong, L, Yue, D, et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. BMJ Glob Health. (2020) 5:e002086. doi: 10.1136/bmjgh-2019-002087
87. Wetzke, M, Happle, C, Vakilzadeh, A, Ernst, D, Sogkas, G, Schmidt, RE, et al. Healthcare utilization in a large cohort of asylum seekers entering Western Europe in 2015. Int J Environ Res Public Health. (2018) 15:2163. doi: 10.3390/ijerph15102163
88. Read, JG, and Smith, PB. Gender and national origin differences in healthcare utilization among U.S. Immigrants from Mexico, China, and India. Ethn Health. (2018) 23:867–83. doi: 10.1080/13557858.2017.1297776
89. Lai, D, and Chau, S. Predictors of health service barriers for older Chinese immigrants in Canada. Health Soc Work. (2007) 32:57–65. doi: 10.1093/hsw/32.1.57
90. Shachaf, S, Davidovitch, N, Halpern, P, and Mor, Z. Utilization profile of emergency department by irregular migrants and hospitalization rates: lessons from a large urban medical center in Tel Aviv, Israel. Int J Equity Health. (2020) 19:56. doi: 10.1186/s12939-020-1152-6
91. Dalla Zuanna, T, Cacciani, L, Barbieri, G, Ferracin, E, Zengarini, N, di Girolamo, C, et al. Avoidable hospitalisation for diabetes mellitus among immigrants and natives: results from the Italian network for longitudinal metropolitan studies. Nutr Metabol Cardiovasc Dis. (2020) 30:1535–43. doi: 10.1016/j.numecd.2020.05.006
92. Zheng, L, Hu, R, Dong, Z, and Hao, Y. Comparing the needs and utilization of health services between urban residents and rural-to-urban migrants in China from 2012 to 2016. BMC Health Serv Res. (2018) 18:717. doi: 10.1186/s12913-018-3522-y
93. Ismayilova, L, Lee, HN, Shaw, S, el-Bassel, N, Gilbert, L, Terlikbayeva, A, et al. Mental health and migration: depression, alcohol abuse, and access to health care among migrants in Central Asia. J Immigr Minor Health. (2014) 16:1138–48. doi: 10.1007/s10903-013-9942-1
94. Fan, JX, Wen, M, Jin, L, and Wang, G. Disparities in healthcare utilization in China: do gender and migration status matter? J Fam Econ Iss. (2013) 34:52–63. doi: 10.1007/s10834-012-9296-1
95. Lin, Y, Chu, C, Chen, Q, Xiao, J, and Wan, C. Factors influencing utilization of primary health care by elderly internal migrants in China: the role of social contacts. BMC Public Health. (2020) 20:1054. doi: 10.1186/s12889-020-09178-3
96. Wen, X, Zheng, H, Feng, Z, Tucker, W, Lu, Y, and Yuan, Z. Hospitalization services utilization between permanent and migrant females in underdeveloped rural regions and contributing factors-A five-time data collection and analysis. Int J Environ Res Public Health. (2019) 16:3419. doi: 10.3390/ijerph16183419
97. Weng, S, Malik, A, Wongsin, U, Lohmeyer, F, Lin, L, Atique, S, et al. Health service access among Indonesian migrant domestic workers in Taiwan. Int J Environ Res Public Health. (2021) 18:3759. doi: 10.3390/ijerph18073759
98. Haj-Younes, J, Strømme, E, Igland, J, Abildsnes, E, Kumar, B, Hasha, W, et al. Use of health care services among Syrian refugees migrating to Norway: a prospective longitudinal study. BMC Health Serv Res. (2021) 21:572. doi: 10.1186/s12913-021-06571-5
99. Wang, Y, Jing, Z, Ding, L, Tang, X, Feng, Y, Li, J, et al. Socioeconomic inequity in inpatient service utilization based on need among internal migrants: evidence from 2014 national cross-sectional survey in China. BMC Health Serv Res. (2020) 20:984. doi: 10.1186/s12913-020-05843-w
100. Cai, X, Yang, F, and Bian, Y. Gap analysis on hospitalized health service utilization in floating population covered by different medical insurances – Case study from Jiangsu Province, China. Int J Equity Health. (2019) 18:84. doi: 10.1186/s12939-019-0992-4
101. Razzaque, A, Clair, K, Chin, B, Islam, M, Mia, M, Chowdhury, R, et al. Association of time since migration from rural to urban slums and maternal and child outcomes: Dhaka (north and south) and Gazipur City corporations. J Urban Health. (2020) 97:158–70. doi: 10.1007/s11524-019-00395-9
102. Kusuma, YS, Kumari, R, and Kaushal, S. Migration and access to maternal healthcare: determinants of adequate antenatal care and institutional delivery among socio-economically disadvantaged migrants in Delhi, India. Trop Med Int Health. (2013) 18:1202–10. doi: 10.1111/tmi.12166
103. Akhter, S, Mahmood, N, and Rutherford, S. A systematic review of the health of internal migrants in Bangladesh. Int J Health Plann Manag. (2022) 37:673–90. doi: 10.1002/hpm.3380
104. Geddam, JB, Ponna, SN, Kommu, PR, Kokku, SB, Mamidi, RS, and Bontha, VB. Utilization of maternal health services by the migrant population living in the non-notified slums of Hyderabad city, India. J Community Health. (2017) 29:29–38. doi: 10.47203/IJCH.2017.v29i01.006
105. Yao, Q, Liu, C, and Sun, J. Inequality in health services for internal migrants in China: A national cross-sectional study on the role of fund location of social health insurance. Int J Environ Res Public Health. (2020) 17:6327. doi: 10.3390/ijerph17176327
106. Qiu, P, Yang, Y, Zhang, J, and Ma, X. Rural-to-urban migration and its implication for new cooperative medical scheme coverage and utilization in China. BMC Public Health. (2011) 11:520. doi: 10.1186/1471-2458-11-520
107. Führer, A, Tiller, D, Brzoska, P, Korn, M, Gröger, C, and Wienke, A. Health-related disparities among migrant children at school entry in Germany. How does the definition of migration status matter? Int J Environ Res Public Health. (2019) 17:212. doi: 10.3390/ijerph17010212
108. Schröder, CC, Dyck, M, Breckenkamp, J, Hasselhorn, HM, and du Prel, JB. Utilisation of rehabilitation services for non-migrant and migrant groups of higher working age in Germany – results of the lidA cohort study. BMC Health Serv Res. (2020) 20:31. doi: 10.1186/s12913-019-4845-z
109. Sauzet, O, David, M, Naghavi, B, Borde, T, Sehouli, J, and Razum, O. Adequate utilization of emergency services in Germany: is there a differential by migration background? Front Public Health. (2020) 8:613250. doi: 10.3389/fpubh.2020.613250
110. Del Puente, F, Riccardi, N, Taramasso, L, Sarteschi, G, Pincino, R, and Di Biagio, A. Migrants and imported disease: trends of admission in an Italian infectious disease ward during the migration crisis of 2015–2017. BMC Public Health. (2020) 20:738. doi: 10.1186/s12889-020-08886-0
111. Seo, JY, Chao, YY, and Strauss, SM. Work-related symptoms, safety concerns, and health service utilization among Korean and Chinese nail salon workers in the Greater New York City Area. Asia Pac J Public Health. (2019) 31:199–209. doi: 10.1177/1010539519840255
112. Shao, S, Wang, M, Jin, G, Zhao, Y, Lu, X, and Du, J. Analysis of health service utilization of migrants in Beijing using Anderson health service utilization model. BMC Health Serv Res. (2018) 18:462. doi: 10.1186/s12913-018-3271-y
113. Xiong, M, Zhao, P, Zou, X, Hall, B, Cao, H, and Wang, C. Health service utilisation among African migrants in China: a nationwide cross-sectional study. BMJ Open. (2021) 11:e046746. doi: 10.1136/bmjopen-2020-046746
114. Shakya, P, Tanaka, M, Shibanuma, A, and Jimba, M. Nepalese migrants in Japan: what is holding them back in getting access to healthcare? PLoS One. (2018) 13:e0203645. doi: 10.1371/journal.pone.0203645
115. Liu, S, Hu, CX, and Mak, S. Comparison of health status and health care services utilization between migrants and natives of the same ethnic origin--the case of Hong Kong. Int J Environ Res Public Health. (2013) 10:606–22. doi: 10.3390/ijerph10020606
116. Guan, M. Should the poor have no medicines to cure? A study on the association between social class and social security among the rural migrant workers in urban China. Int J Equity Health. (2017) 16:193. doi: 10.1186/s12939-017-0692-x
117. Chowdhury, N, Naeem, I, Ferdous, M, Chowdhury, M, Goopy, S, Rumana, N, et al. Unmet healthcare needs among migrant populations in Canada: exploring the research landscape through a systematic integrative review. J Immigr Minor Health. (2021) 23:353–72. doi: 10.1007/s10903-020-01086-3
118. Song, X, Zou, G, Chen, W, Han, S, Zou, X, and Ling, L. Health service utilisation of rural-to-urban migrants in Guangzhou, China: does employment status matter? Trop Med Int Health. (2017) 22:82–91. doi: 10.1111/tmi.12801
119. Fayehun, O, Ajisola, M, Uthman, O, Oyebode, O, Oladejo, A, Owoaje, E, et al. A contextual exploration of healthcare service use in urban slums in Nigeria. PLoS One. (2022) 17:e0264725. doi: 10.1371/journal.pone.0264725
120. Loganathan, T, Rui, D, Ng, C, and Pocock, N. Breaking down the barriers: understanding migrant workers' access to healthcare in Malaysia. PLoS One. (2019) 14:e0218669. doi: 10.1371/journal.pone.0218669
121. Maneze, D, DiGiacomo, M, Salamonson, Y, Descallar, J, and Davidson, PM. Facilitators and barriers to health-seeking behaviours among Filipino migrants: inductive analysis to inform health promotion. Biomed Res Int. (2015) 2015:506269. doi: 10.1155/2015/506269
122. Kaur, M, Singh, S, Gupta, M, Bahuguna, P, and Rani, S. Inequity in access to health services between migrants and natives of Chandigarh, India. Int J Migrat Health Soc Care. (2015) 11:147–55. doi: 10.1108/IJMHSC-03-2014-0010
123. Guo, M, Sabbagh Steinberg, N, Dong, X, and Tiwari, A. Is family relations related to health service utilisation among older immigrants: evidence from Chinese elderly in the United States. Health Soc Care Community. (2019) 27:215–25. doi: 10.1111/hsc.12642
124. Kugel, C, and Seda, C. Migrant and seasonal farmworkers: cancer risks, barriers to care, and ways to overcome them. Clin J Oncol Nurs. (2021) 25:219–22. doi: 10.1188/21.CJON.219-222
125. Lee, W, Neo, A, Tan, S, Cook, AR, Wong, ML, Tan, J, et al. Health-seeking behaviour of male foreign migrant workers living in a dormitory in Singapore. BMC Health Serv Res. (2014) 14:300. doi: 10.1186/1472-6963-14-300
126. Zou, G, Zeng, Z, Chen, W, and Ling, L. Self-reported illnesses and service utilisation among migrants working in small-to medium sized enterprises in Guangdong. China Public Health. (2015) 129:970–8. doi: 10.1016/j.puhe.2015.04.015
127. Li, Z, Wang, D, Xu, H, and Xue, Y. Demand for outpatient services and its determinants in migrant population in Fujian province, 2017. Chin J Public Health. (2019) 35:838–41. doi: 10.11847/zgggws1122279
128. Mou, J, Cheng, J, Zhang, D, Jiang, H, Lin, L, and Griffiths, S. Health care utilisation amongst Shenzhen migrant workers: does being insured make a difference? BMC Health Serv Res. (2009) 9:214. doi: 10.1186/1472-6963-9-214
129. Xi, S, Song, Y, Li, X, Li, M, Lu, Z, Yang, Y, et al. Local-migrant gaps in healthcare utilization between older migrants and local residents in China. J Am Geriatr Soc. (2020) 68:1560–7. doi: 10.1111/jgs.16421
130. Liu, L, Gjebrea, O, Ali, F, and Atun, R. Determinants of healthcare utilisation by migrant workers in the State of Qatar. Health Policy. (2020) 124:873–80. doi: 10.1016/j.healthpol.2020.04.011
131. Phaiyarom, M, Pudpong, N, Suphanchaimat, R, Kunpeuk, W, Julchoo, S, and Sinam, P. Outcomes of the health insurance card scheme on migrants' use of health services in Ranong Province, Thailand. Int J Environ Res Public Health. (2020) 17:4431. doi: 10.3390/ijerph17124431
132. Müllerschön, J, Koschollek, C, Santos-Hövener, C, Kuehne, A, Müller-Nordhorn, J, and Bremer, V. Impact of health insurance status among migrants from sub-Saharan Africa on access to health care and HIV testing in Germany: a participatory cross-sectional survey. BMC Int Health Hum Rights. (2019) 19:10. doi: 10.1186/s12914-019-0189-3
133. Zhang, F, Shi, X, and Zhou, Y. The impact of health insurance on healthcare utilization by migrant workers in China. Int J Environ Res Public Health. (2020) 17:1852. doi: 10.3390/ijerph17061852
134. Lam, K, and Johnston, J. Health insurance and healthcare utilisation for Shenzhen residents: a tale of registrants and migrants? BMC Public Health. (2012) 12:868. doi: 10.1186/1471-2458-12-868
135. Lu, CH, Wang, PX, Lei, YX, and Luo, ZC. Influence of health-related quality of life on health service utilization in Chinese rural-to-urban female migrant workers. Health Qual Life Outcomes. (2014) 12:121. doi: 10.1186/s12955-014-0121-4
136. Torres, JM, and Waldinger, R. Civic stratification and the exclusion of undocumented immigrants from cross-border health care. J Health Soc Behav. (2015) 56:438–59. doi: 10.1177/0022146515610617
137. Gimeno-Feliu, LA, Pastor-Sanz, M, Poblador-Plou, B, Calderón-Larrañaga, A, Díaz, E, and Prados-Torres, A. Overuse or underuse? Use of healthcare services among irregular migrants in a north-eastern Spanish region. Int J Equity Health. (2021) 20:41. doi: 10.1186/s12939-020-01373-3
138. Waldman, K, Koyanagi, A, Wang, JS, Ko, J, DeVylder, J, and Oh, H. Acculturative stress, disability, and health treatment utilization among Asian and Latin American immigrants in the United States. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:1275–84. doi: 10.1007/s00127-019-01691-0
139. Kumar, R. Refugee articulations of health: a culture-centered exploration of Burmese Refugees' resettlement in the United States. Health Commun. (2021) 36:682–92. doi: 10.1080/10410236.2020.1712035
140. Al-Sharifi, F, Winther Frederiksen, H, Knold Rossau, H, Norredam, M, and Zwisler, AD. Access to cardiac rehabilitation and the role of language barriers in the provision of cardiac rehabilitation to migrants. BMC Health Serv Res. (2019) 19:223. doi: 10.1186/s12913-019-4041-1
141. Gaya-Sancho, B, Vanceulebroeck, V, Kömürcü, N, Kalkan, I, Casa-Nova, A, Tambo-Lizalde, E, et al. Perception and experience of transcultural care of stakeholders and health service users with a migrant background: A qualitative study. Int J Environ Res Public Health. (2021) 18:10503. doi: 10.3390/ijerph181910503
142. Norredam, M, and Agyemang, C. Tackling the health challenges of international migrant workers. Lancet Glob Health. (2019) 7:e813–4. doi: 10.1016/S2214-109X(19)30224-4
143. Tomkow, L, Kang, C, Farrington, R, Wiggans, R, Wilson, R, Pushkar, P, et al. Healthcare access for asylum seekers and refugees in England: a mixed methods study exploring service users' and health care professionals' awareness. Eur J Pub Health. (2020) 30:527–32. doi: 10.1093/eurpub/ckz193
144. Narayan, L. Addressing language barriers to healthcare in India. Natl Med J India. (2013) 26:236–8.
145. Ma, C, Huo, S, and Chen, H. Does integrated medical insurance system alleviate the difficulty of using cross-region health care for the Migrant Parents in China-- evidence from the China migrants dynamic survey. BMC Health Serv Res. (2021) 21:1053. doi: 10.1186/s12913-021-07069-w
146. Pförringer, D, Pflüger, P, Waehlert, L, Beivers, A, Seidl, F, Duscher, D, et al. Emergency room as primary point of access in the German healthcare system: objective evaluation and interview of motivation for ER entrance of 235 ER patients in a German hospital. Eur J Trauma Emerg Surg. (2021) 47:453–60. doi: 10.1007/s00068-019-01173-7
147. Mölsä, M, Tiilikainen, M, and Punamäki, RL. Usage of healthcare services and preference for mental healthcare among older Somali immigrants in Finland. Ethn Health. (2019) 24:607–22. doi: 10.1080/13557858.2017.1346182
148. Credé, SH, Such, E, and Mason, S. International migrants' use of emergency departments in Europe compared with non-migrants' use: a systematic review. Eur J Pub Health. (2018) 28:61–73. doi: 10.1093/eurpub/ckx057
149. Kietzmann, D, Knuth, D, and Schmidt, S. (non-)utilization of pre-hospital emergency care by migrants and non-migrants in Germany. Int J Public Health. (2017) 62:95–102. doi: 10.1007/s00038-016-0904-y
150. Bardin, A, Dalla Zuanna, T, Favarato, S, Simonato, L, Zanier, L, Comoretto, RI, et al. The role of maternal citizenship on pediatric avoidable hospitalization: A birth cohort study in north-East Italy. Indian J Pediatr. (2019) 86:3–9. doi: 10.1007/s12098-018-2826-6
151. Çilenti, K, Rask, S, Elovainio, M, Lilja, E, Kuusio, H, Koskinen, S, et al. Use of health services and unmet need among adults of Russian, Somali, and Kurdish Origin in Finland. Int J Environ Res Public Health. (2021) 18:2229. doi: 10.3390/ijerph18052229
152. Tambor, M, Pavlova, M, Woch, P, and Groot, W. Diversity and dynamics of patient cost-sharing for physicians' and hospital services in the 27 European Union countries. Eur J Pub Health. (2011) 21:585–90. doi: 10.1093/eurpub/ckq139
153. Tschirhart, N, Jiraporncharoen, W, Angkurawaranon, C, Hashmi, A, Nosten, S, McGready, R, et al. Choosing where to give birth: factors influencing migrant women's decision making in two regions of Thailand. PLoS One. (2020) 15:e0230407. doi: 10.1371/journal.pone.0230407
154. Wang, H, Zhang, D, Hou, Z, Yan, F, and Hou, Z. Association between social health insurance and choice of hospitals among internal migrants in China: a national cross-sectional study. BMJ Open. (2018) 8:e018440. doi: 10.1136/bmjopen-2017-018440
155. Mosadeghrad, AM. Patient choice of a hospital: implications for health policy and management. Int J Health Care Qual Assur. (2014) 27:152–64. doi: 10.1108/IJHCQA-11-2012-0119
156. Smith, H, Currie, C, Chaiwuttisak, P, and Kyprianou, A. Patient choice modelling: how do patients choose their hospitals? Health Care Manag Sci. (2018) 21:259–68. doi: 10.1007/s10729-017-9399-1
157. Keating, NL, Kouri, EM, He, Y, Freedman, RA, Volya, R, and Zaslavsky, AM. Location isn't everything: proximity, hospital characteristics, choice of hospital, and disparities for breast cancer surgery patients. Health Serv Res. (2016) 51:1561–83. doi: 10.1111/1475-6773.12443
158. Zhang, A, Nikoloski, Z, Albala, SA, Yip, W, Xu, J, and Mossialos, E. Patient choice of health care providers in China: primary care facilities versus hospitals. Health Syst Reform. (2020) 6:e1846844. doi: 10.1080/23288604.2020.1846844
159. Jin, Y, Yuan, B, Zhu, W, Zhang, Y, Xu, L, and Meng, Q. The interaction effect of health insurance reimbursement and health workforce on health care-seeking behaviour in China. Int J Health Plann Manag. (2019) 34:900–11. doi: 10.1002/hpm.2860
160. Liu, Y, Kong, Q, Wang, S, Zhong, L, and van de Klundert, J. The impact of hospital attributes on patient choice for first visit: evidence from a discrete choice experiment in Shanghai. China Health Policy Plan. (2020) 35:267–78. doi: 10.1093/heapol/czz159
161. Liu, Y, Kong, Q, and de Bekker-Grob, EW. Public preferences for health care facilities in rural China: A discrete choice experiment. Soc Sci Med. (1982) 237:112396. doi: 10.1016/j.socscimed.2019.112396
162. Kim, HY, Kim, JY, Park, HY, Jun, JH, Koo, HY, Cho, IY, et al. Health service utilization, unmet healthcare needs, and the potential of telemedicine services among Korean expatriates. Glob Health. (2018) 14:120. doi: 10.1186/s12992-018-0433-y
163. Sun, X, Meng, H, Ye, Z, Conner, KO, Duan, Z, and Liu, D. Factors associated with the choice of primary care facilities for initial treatment among rural and urban residents in southwestern China. PLoS One. (2019) 14:e0211984. doi: 10.1371/journal.pone.0211984
164. Ojifinni, O, Ige, O, and Asuzu, MC. Determinants of choice of health facility for reproductive morbidity by female traders in a Nigerian city. Ann Ib Postgrad Med. (2018) 16:37–43.
165. de Cruppé, W, and Geraedts, M. Hospital choice in Germany from the patient's perspective: a cross-sectional study. BMC Health Serv Res. (2017) 17:720. doi: 10.1186/s12913-017-2712-3
166. Dündar, C. Health-seeking behavior and medical facility choice in Samsun. Turkey Health Policy. (2017) 121:1015–9. doi: 10.1016/j.healthpol.2017.07.002
167. Kim, K, Ahn, S, Lee, B, Lee, K, Yoo, S, Lee, K, et al. Factors associated with patients' choice of physician in the Korean population: database analyses of a tertiary hospital. PLoS One. (2018) 13:e0190472. doi: 10.1371/journal.pone.0190472
168. Gutacker, N, Siciliani, L, Moscelli, G, and Gravelle, H. Choice of hospital: which type of quality matters? J Health Econ. (2016) 50:230–46. doi: 10.1016/j.jhealeco.2016.08.001
169. Schuldt, J, Doktor, A, Lichters, M, Vogt, B, and Robra, BP. Insurees' preferences in hospital choice-A population-based study. Health Policy. (2017) 121:1040–6. doi: 10.1016/j.healthpol.2017.08.004
170. Yendaw, E, and Tampah-Naah, AM. Health-seeking behaviour and practices among immigrant retail traders in an urban setting in North-Western Ghana. Int J Migrat Health Soc Care. (2021) 17:286–302. doi: 10.1108/IJMHSC-04-2020-0040
171. Shewamene, Z, Dune, T, and Smith, CA. Use of traditional and complementary medicine for maternal health and wellbeing by African migrant women in Australia: a mixed method study. BMC Complement Med Therap. (2020) 20:60. doi: 10.1186/s12906-020-2852-6
172. Kyaw, PP, and Geater, AF. Healthcare seeking preferences of Myanmar migrant seafarers in the deep south of Thailand. Int Marit Health. (2021) 72:1–9. doi: 10.5603/IMH.2021.0001
173. Seo, JY, Chao, YY, Yeung, KM, and Strauss, SM. Factors influencing health service utilization among Asian immigrant nail salon Workers in the Greater New York City Area. J Community Health. (2019) 44:1–11. doi: 10.1007/s10900-018-0544-7
174. Zhao, Y, Mao, L, Lu, J, Zhang, Q, Chen, G, Sun, M, et al. Status and factors associated with healthcare choices among older adults and children in an Urbanized County: A cross-sectional study in Kunshan, China. Int J Environ Res Public Health. (2020) 17:8697. doi: 10.3390/ijerph17228697
175. Peng, B, Zhang, H, Shi, L, and Ling, L. Migration status and healthcare seeking behaviours among the Chinese labor-force: a nationally representative study. BMJ Open. (2019) 9:e031798. doi: 10.1136/bmjopen-2019-031798
176. Zhang, L, Li, X, Yang, H, Mao, R, and Zhao, Q. Health status and health-seeking behaviour between interprovincial and intraprovincial rural-to-urban young migrants in Nanjing. China Asia-Pacific Population Journal. (2013) 26:39–54. doi: 10.18356/c2601935-en
177. Frehywot, S, Park, C, and Infanzon, A. Medical diaspora: an underused entity in low- and middle-income countries' health system development. Hum Resour Health. (2019) 17:56. doi: 10.1186/s12960-019-0393-1
178. Liverani, M, Ir, P, Jacobs, B, Asante, A, Jan, S, Leang, S, et al. Cross-border medical travels from Cambodia: pathways to care, associated costs and equity implications. Health Policy Plan. (2020) 35:1011–20. doi: 10.1093/heapol/czaa061
179. Şekercan, A, Woudstra, AJ, Peters, RJG, Lamkaddem, M, Akgün, S, and Essink-Bot, ML. Dutch citizens of Turkish origin who utilize healthcare services in Turkey: a qualitative study on motives and contextual factors. BMC Health Serv Res. (2018) 18:289. doi: 10.1186/s12913-018-3026-9
180. De Jesus, M, and Xiao, C. Cross-border health care utilization among the Hispanic population in the United States: implications for closing the health care access gap. Ethn Health. (2013) 18:297–314. doi: 10.1080/13557858.2012.730610
181. Şekercan, A, Lamkaddem, M, Snijder, MB, Peters, RJ, and Essink-Bot, ML. Healthcare consumption by ethnic minority people in their country of origin. Eur J Pub Health. (2015) 25:384–90. doi: 10.1093/eurpub/cku205
182. Lokdam, N, Kristiansen, M, Handlos, LN, and Norredam, M. Use of healthcare services in the region of origin among patients with an immigrant background in Denmark: a qualitative study of the motives. BMC Health Serv Res. (2016) 16:99. doi: 10.1186/s12913-016-1346-1
183. Lee, JY, Kearns, RA, and Friesen, W. Seeking affective health care: Korean immigrants' use of homeland medical services. Health Place. (2010) 16:108–15. doi: 10.1016/j.healthplace.2009.09.003
184. Su, D, Richardson, C, Wen, M, and Pagán, JA. Cross-border utilization of health care: evidence from a population-based study in South Texas. Health Serv Res. (2011) 46:859–76. doi: 10.1111/j.1475-6773.2010.01220.x
185. Bergmark, R, Barr, D, and Garcia, R. Mexican immigrants in the US living far from the border may return to Mexico for health services. J Immigr Minor Health. (2010) 12:610–4. doi: 10.1007/s10903-008-9213-8
186. Brijnath, B, Antoniades, J, and Adams, J. Investigating patient perspectives on medical returns and buying medicines online in two communities in Melbourne, Australia: results from a qualitative study. Patient. (2015) 8:229–38. doi: 10.1007/s40271-014-0082-z
187. Horton, S, and Cole, S. Medical returns: seeking health care in Mexico. Soc Sci Med. (1982) 72:1846–52. doi: 10.1016/j.socscimed.2011.03.035
188. Kemppainen, L, Kemppainen, T, Skogberg, N, Kuusio, H, and Koponen, P. Immigrants' use of health care in their country of origin: the role of social integration, discrimination and the parallel use of health care systems. Scand J Caring Sci. (2018) 32:698–706. doi: 10.1111/scs.12499
189. Tarkowski, K, Bojar, I, Kister, A, and Raczkiewicz, D. Changes in interregional migration of patients hospitalized in Poland - 2013-2017. Ann Agric Environ Med. (2019) 26:469–503. doi: 10.26444/aaem/105389
190. Ding, L, Li, X, Tang, X, Feng, Y, Wang, Y, Cheng, J, et al. Effect of social integration on childbirth return among internal migrant pregnant women: a nationally representative study in China. BMC Health Serv Res. (2020) 20:918. doi: 10.1186/s12913-020-05783-5
191. Zhao, J, Kong, F, and Li, S. Association between social integration and medical returns among the migrant elderly following children to Jinan City China. BMC Public Health. (2021) 21:1822. doi: 10.1186/s12889-021-11901-7
192. Shin, YK, Koskinen, V, Kouvonen, A, Kemppainen, T, Olakivi, A, Wrede, S, et al. Digital information technology use and transnational healthcare: A population-based study on older Russian-speaking migrants in Finland. J Immigr Minor Health. (2022) 24:125–35. doi: 10.1007/s10903-021-01301-9
193. Şekercan, A, Harting, J, Peters, RJG, and Stronks, K. Understanding transnational healthcare use in immigrant communities from a cultural systems perspective: a qualitative study of Dutch residents with a Turkish background. BMJ Open. (2021) 11:e051903. doi: 10.1136/bmjopen-2021-051903
194. Hu, B, Peng, D, Zhang, Y, and Yu, J. Rural population aging and the hospital utilization in cities: the rise of medical tourism in China. Int J Environ Res Public Health. (2020) 17:4790. doi: 10.3390/ijerph17134790
195. Hou, Z, and Zhang, D. Health insurance coverage and inpatient services choice among rural-to-urban migrants from a nationwide cross-sectional survey in China: does location matter? Lancet. (2017) 390:S27. doi: 10.1016/S0140-6736(17)33165-3
Keywords: health service behaviors, migrant, health delivery system characteristics, subgroup-specific factors, conceptual framework
Citation: Peng B and Ling L (2023) Health service behaviors of migrants: A conceptual framework. Front. Public Health. 11:1043135. doi: 10.3389/fpubh.2023.1043135
Edited by:
Stefania Salmaso, Independent Researcher, Rome, ItalyReviewed by:
Karen Lau, St George's, University of London, United KingdomCathy Zimmerman,University of London,United KingdomCopyright © 2023 Peng and Ling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Ling, lingli@mail.sysu.edu.cn
 Boli Peng
Boli Peng Li Ling
Li Ling