
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 30 January 2023
Sec. Family Medicine and Primary Care
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1035759
This article is part of the Research Topic Saving Mothers and Babies for the New World View all 17 articles
 Dagmawi Chilot1,2*
Dagmawi Chilot1,2* Daniel Gashaneh Belay3,4
Daniel Gashaneh Belay3,4 Tigist Andargie Ferede4
Tigist Andargie Ferede4 Kegnie Shitu5
Kegnie Shitu5 Melaku Hunie Asratie6
Melaku Hunie Asratie6 Sintayehu Ambachew7
Sintayehu Ambachew7 Yadelew Yimer Shibabaw8
Yadelew Yimer Shibabaw8 Demiss Mulatu Geberu9
Demiss Mulatu Geberu9 Melkamu Deresse10
Melkamu Deresse10 Adugnaw Zeleke Alem4
Adugnaw Zeleke Alem4Background: Complications during pregnancy and childbirth are the leading causes of maternal and child deaths and disabilities, particularly in low- and middle-income countries. Timely and frequent antenatal care prevents these burdens by promoting existing disease treatments, vaccination, iron supplementation, and HIV counseling and testing during pregnancy. Many factors could contribute to optimal ANC utilization remaining below targets in countries with high maternal mortality. This study aimed to assess the prevalence and determinants of optimal ANC utilization by using nationally representative surveys of countries with high maternal mortality.
Methods: Secondary data analysis was done using recent Demographic and Health Surveys (DHS) data of 27 countries with high maternal mortality. The multilevel binary logistic regression model was fitted to identify significantly associated factors. Variables were extracted from the individual record (IR) files of from each of the 27 countries. Adjusted odds ratios (AOR) with a 95% confidence interval (CI) and p-value of ≤0.05 in the multivariable model were used to declare significant factors associated with optimal ANC utilization.
Result: The pooled prevalence of optimal ANC utilization in countries with high maternal mortality was 55.66% (95% CI: 47.48–63.85). Several determinants at the individual and community level were significantly associated with optimal ANC utilization. Mothers aged 25–34 years, mothers aged 35–49 years, mothers who had formal education, working mothers, women who are married, had media access, households of middle-wealth quintile, richest household, history of pregnancy termination, female household head, and high community education were positively associated with optimal ANC visits in countries with high maternal mortality, whereas being rural residents, unwanted pregnancy, having birth order 2–5, and birth order >5 were negatively associated.
Conclusion and recommendations: Optimal ANC utilization in countries with high maternal mortality was relatively low. Both individual-level factors and community-level factors were significantly associated with ANC utilization. Policymakers, stakeholders, and health professionals should give special attention and intervene by targeting rural residents, uneducated mothers, economically poor women, and other significant factors this study revealed.
Maternal and child mortality remains a substantial public health concern worldwide. However, the risk of these problems is even higher in low- and middle-income countries (1, 2). The United Nations (UN) came up with the Millennium Development Goals (MDGs) to reduce maternal and child mortality in the world community to be achieved by 2015 (3). Despite the country's significant progress in achieving the MDG-5, it has been limited and uneven (4, 5). How the goals were designed, the lack of stakeholder commitment and interest, scarce resources, and lack of accountability were some of the factors for the slow and unequal progress (6, 7).
Complications during pregnancy and childbirth are the leading causes of maternal and child deaths and disabilities (8). The World Health Organization (WHO) recommended antenatal care (ANC) visits as a key strategy to endorse pregnant women's health (9, 10). The organization previously recommended a minimum of four ANC visits throughout the pregnancy; however, it revised its recommended minimum number of ANC visits from four to eight contacts in 2016 to have a safe pregnancy and healthy baby (11). Timely and frequent ANC promotes existing disease treatments, vaccination, malaria prophylaxis, iron supplementation, nutrition counseling, HIV counseling and testing, and urinary tract infection treatment (12–14).
The lowest levels of antenatal care are witnessed in sub-Saharan Africa and South Asia. Individual-level and community-level factors were consistently reported as the most important influences for ANC utilization. In recent studies conducted in low- and middle-income countries, women's education, residence, wealth index, husband's education, mass media, marital status, women's autonomy, husband support, and healthcare accessibility were the commonly reported determinants (15–20). In addition, it is been criticized that the MDG targets were not designed based on enough evidence of feasibility in low-income countries (21, 22). Moreover, limitations in the MDG development process, structure, content, implementation, and enforcement were one of the key obstacles (4, 23–25).
Numerous studies focusing on determinants of antenatal care use in low- and middle-income countries have been conducted and identified important factors. However, a minimum of four ANC visits (ANC4+) utilization in countries with high maternal mortality was not addressed, and getting reliable data on the implementation of MDG and interpretation of progress reports were frequently reported challenges. Identifying gaps in ANC4+ use specifically in these countries is important for stakeholders including policy planners and program managers to increase the utilization of services that decreases maternal–child mortality. In addition, giving a panoramic view of the problem and detecting possible determinates in high maternal mortality countries could help to implement SDG3. Therefore, the objective of our study was to assess the prevalence of ANC4+ visits among women aged 15–49 years and the potential factors associated with it in countries with high maternal mortality. Our study will provide evidence-based recommendations to improve ANC utilization in those reproductive-age women on a large scale.
The Demography and Health Surveys employed a cross-sectional study design to collect the data. In this study, we only included countries with high maternal mortality and have publically available DHS data (26).
This study is a secondary data analysis using the DHS data conducted in 27 countries. The DHS is a nationally representative survey that is conducted in low- and middle-income countries globally. We used individual record (IR) files to extract the study participants of this study. We weighted the sample using the individual weight of women (v005) to produce the proper representation. Hence, sample weights were generated by dividing (v005) by 1,000,000, and the total weighted sample size from the pooled data was 209,538 (Table 1).
Women aged 15–49 years with a birth in the last 5 years receiving antenatal care from a skilled provider for the most recent birth were the study population. Sample weight was used to correct for over- and under-sampling and generalizability of the findings.
Antenatal care visit was the outcome variable for this study. We dichotomized the ANC visits as inadequate and adequate according to the WHO classification (11). Inadequate ANC is <4 visits, whereas optimal if women had four and more visits.
Potential explanatory variables associated with completing optimal ANC visits were considered on two levels. Variables such as mother's age, maternal educational status, parity, marital status, sex of the household head, birth order, and wealth index were used at the individual level, whereas residence, community-level education, community-level poverty, and community-level media exposure were used as community-level variables.
Community-level media usage is the proportion of women in the community who use radio, TV, and newsletter, and it was categorized as low community-level media usage and high community-level media usage. “Low” refers to communities in which <50% of respondents had media access, while “high” indicates communities in which ≥50% of respondents had media access.
Community-level women's education refers to the proportion of women in the community who have formal education. It was categorized as low if communities in which < 50% of respondents had formal education and high if ≥50% of respondents had attended formal education.
Community-level poverty refers to the proportion of women in the community who had low-wealth quintiles. It was categorized as low if the proportion of low-wealth quintile households was < 50% and high if the proportion was ≥50%.
STATA version 14.2 was used to clean, recode, and analyze the data. A multilevel binary logistic regression model was fitted to identify significantly associated factors. Both community- and individual-level variables with a p-value of ≤0.2 in the bi-variable analysis were included in the multivariable model. Adjusted OR (AOR) with 95% CI and p < 0.05 were applied to determine significantly associated factors.
Four models were applied, comprising the null model (model 0) containing no variables, which is used to check the variability of ANC visits in the community and provide evidence to assess random effect using the interclass correlation coefficient (ICC). Model I was adjusted for individual-level variables, Model II with community-level factors, and Model III with variables from both individual- and community-level variables were fitted with the outcome variable.
The fixed effect is a measure of association that estimates the association between independent variables and ANC and is stated as AOR with a 95% confidence interval. The Intra-class Correlation Coefficient (ICC), Median Odds Ratio (MOR), and proportional change in variance (PCV) were computed to assess the clustering effect/variability.
In this study, 209,538 women in 27 countries with high maternal mortality were included. Of the total, about 45.97% were aged 25–34 years and 40.77% had no formal education. The majority of study participants (86.89%) were married; however, more than a quarter (27.28%) of pregnancies were unwanted. More than half (64.20%) of the participants had media exposure and 15.11% of women had terminated their pregnancies. In our study, around 42.06% of mothers were poor and most of them (69.82%) resides in rural areas (Table 2).
The pooled prevalence of adequate ANC visits in countries with high maternal mortality was found at 55.66% (95% CI: 47.48–63.85). Ghana (86.05%) had the highest ANC4+ visit and Liberia (85.07%) was in second place. Afghanistan was the country with the least ANC4+ visits, which was 16.19% (Figure 1).
In the multilevel analysis, mothers aged 25–34 years, mothers aged 35–49 years, maternal primary, and secondary education and above, working mothers, married, had media access, middle and rich, wanted pregnancy, had terminated pregnancy, female household head, and high community education were significantly associated variables with increased ANC visits while being rural residents and birth orders 2–5 and >5 were associated with low ANC visits (Table 3).
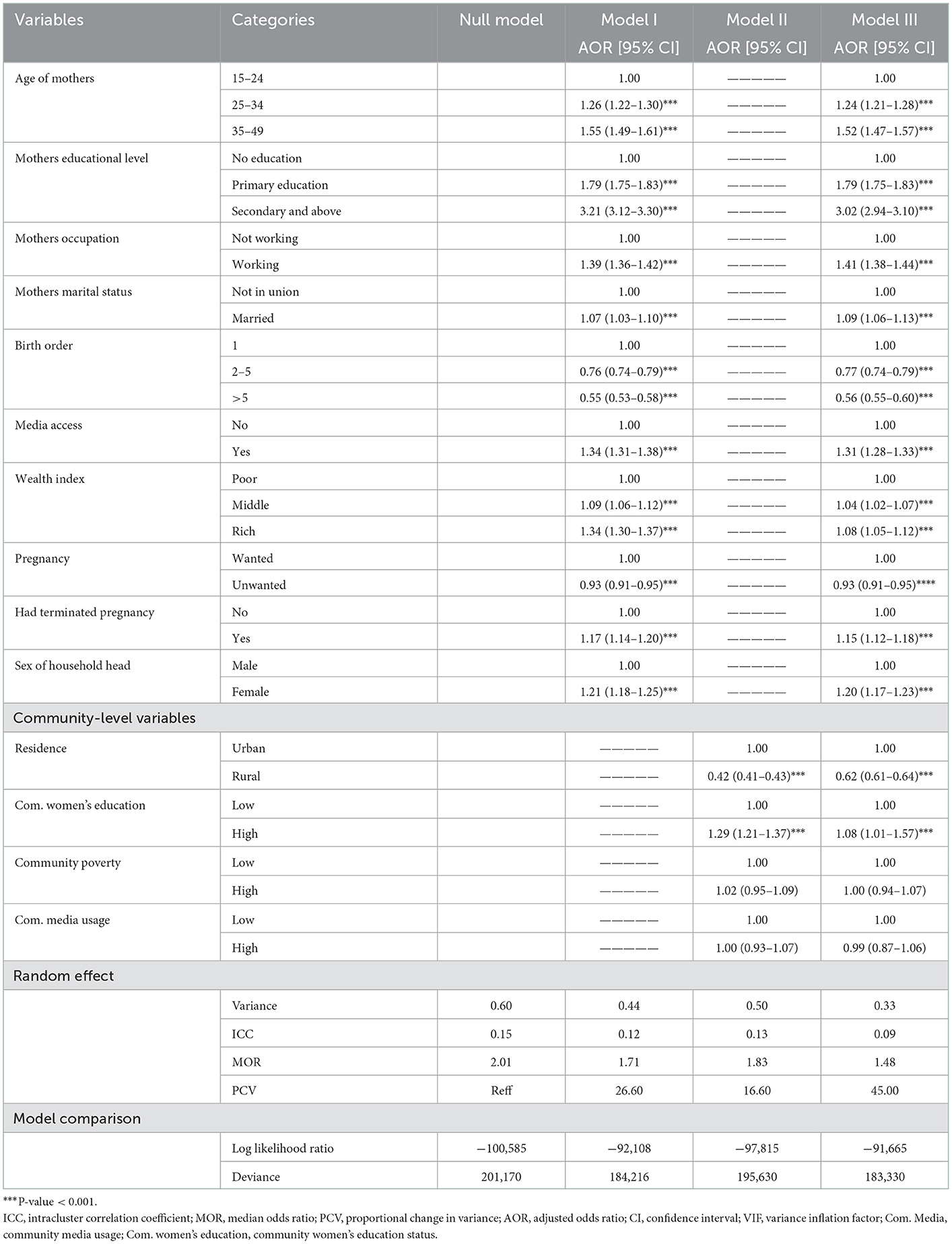
Table 3. Multivariable multilevel logistic regression analysis results of both individual-level and community-level factors associated with ANC visits in high maternal mortality countries.
Maternal mortality is a major public health problem, particularly in low- and middle-income countries. Early detection and intervention of complications that could happen during pregnancy have a paramount advantage and ANC visit is among those early opportunities. Optimal antenatal care is a key strategy to reduce maternal and child mortality as stated by the WHO and it could be influenced by many factors. Our study revealed a parallel relationship between women's age and ANC4+ contacts, as women's age increases, the odds of ANC4+ visits also increased. Those mothers aged 25–34 years and mothers aged 35–49 years were more likely to have adequate ANC visits compared to mothers aged 15–24 years. This finding is in agreement with previous studies conducted elsewhere (27–29). This could be because older women had more experience and better knowledge because of previous exposure to healthcare providers (30, 31).
In countries with high maternal mortality, the educational status of mothers had a similar directional relationship with ANC4+ visits. Generally, education enables women to obtain a better knowledge of the risk of pregnancy to themselves and their children. Therefore, educated mothers could have increased healthcare-seeking behavior to mitigate this risk and lead to adequate ANC usage (32–35). It has also been reported that education increased women's media penetration of the importance of ANC visits and increased the knowledge of optimal ANC usage importance (36, 37).
Occupation has been linked with ANC4+ visits (38). In our study, working mothers were more likely to have ANC4+ visits compared to their counterparts (39–41). This could be because working mother had their income and might alleviate transportation cost problems. In addition, women who generate an income might be less dependent on their husbands/partners and have better autonomy to utilize ANC frequently. However, husband/partner cooperation could increase self-esteem, reduce anxiety, and encourage the women to utilize optimal ANC visits (42–44). Husband involvement in ANC follow-up has a crucial role in pregnancy outcomes and is highly recommended by the WHO (45).
Media have been the easiest and quickest to disseminate information related to maternal health which could influence the utilization of ANC frequently. We found that women who had media exposure experienced ANC4+ compared to their counterparts (46, 47). In addition, the wealth index found a significant determinant for women to utilize adequate ANC. In our findings, the household of middle-income and the richest household were more likely to have ANC4+ visits compared to the poorest. Several previous studies were in agreement with this finding (48, 49). Although ANC services are provided for free in low- and middle-income countries, pregnant women who had financial problems may find it difficult to cover laboratory expenses and reach healthcare facilities. This could lead to delaying and inadequate ANC visit, and the impact could be high for those who live far from health institutions as the transportation cost is high.
Pregnancy wantedness has been an important determinant to utilize adequate ANC (50–52). Unwanted pregnancy could be associated with inadequate ANC usage because women might have denial and become careless about the child and their health. On the contrary, women who were pregnant because they want could have better psychosocial support from a partner, family member, relative, or friend who could lend support to the woman if any problem would arise. The introduction of life-saving modern obstetrics is difficult if the psychosocial needs of the women in these poor countries are not being taken care of. This study also revealed that women who had a history of terminated pregnancy were more likely to attend optimal ANC visits. This could be because that mothers who already experienced pregnancy termination for different reasons would be more alert to avoid such problems again and could have optimal ANC. It has been reported that women who assume that pregnancy is a risky event were more likely to attend ANC4+ visits (53).
Birth orders were found significantly associated with ANC4+ utilization. Women who had birth orders 2–5 and >5 were associated with low ANC visits compared with single birth orders. Our finding is also supported by previous studies in Ethiopia (34, 35). This might be due to increased confidence from a previous pregnancy and childbirth experience, and constraints of time and resources among women who had multiple birth orders (54). This study also revealed that place of residence was a significant factor for ANC4+ utilization. The odds of ANC4+ utilization were low among women of rural residents as compared to urban residents. This finding is in line with previous studies conducted in Nigeria (55, 56) and Ethiopia (34, 57, 58). The potential justifications for this discrepancy could be because of inequalities in healthcare service accessibility, infrastructure, and quality in service delivery in the rural and urban setups.
The strength of this study is that it used a large sample size and had adequate power to detect the true effect of the independent variables. It was based on an appropriate statistical method (multilevel analysis) to address the data's hierarchical nature. As a limitation, since the study used cross-sectional data, a causal relationship cannot be established. In addition, because it was based on the information contained in the dataset, potential variables including healthcare access, insurance, and quality healthcare are missed in the analysis.
With high disparity among countries, ANC4+ utilization in countries with high mortality was low. Both individual-level factors and community-level factors were significantly associated with ANC4+ utilization. Therefore, this study revealed that policymakers, stakeholders, and health professionals should give special attention and intervene by targeting rural residents, uneducated mothers, economically poor women, and other significant factors. However, these recommendations should be considered for country-specific contextual factors, considering the different cultural orientations and varied health systems.
Permission to access the data in this study was obtained from the measure DHS program via online request. The website and the data used were publicly available with no personal identifier.
The studies involving human participants were reviewed and approved by UOG IRB. The patients/participants provided their written informed consent to participate in this study.
DC: conceptualization. DC, DGB, and AZA: study design. DC, DGB, TAF, KS, MHA, SA, YYS, DMG, MD, and AZA: execution, acquisition of the data, analysis, interpretation, writing, reviewing, and editing. All authors contributed to the article and approved the submitted version.
The authors acknowledge the MEASURE DHS for providing us with the dataset.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; ANC, antenatal care; DHS, Demographic and Health Surveys; ICC, intracluster correlation coefficient; IR, individual record; MDG, Millennium Development goal; MOR, median odds ratio; PCV, a proportional change in variance; UN, United Nations; WHO, World Health Organization.
1. Organization WH. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO (2019).
2. Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet. (2015) 385:430–40. doi: 10.1016/S0140-6736(14)61698-6
3. Waage J, Banerji R, Campbell O, Chirwa E, Collender G, Dieltiens V, et al. The millennium development goals: A cross-sectoral analysis and principles for goal setting after 2015: Lancet and London International Development Centre Commission. Lancet. (2010) 376:991–1023. doi: 10.1016/S0140-6736(10)61196-8
4. Fehling M, Nelson BD, Venkatapuram S. Limitations of the millennium development goals: A literature review. Glob Public Health. (2013) 8:1109–22. doi: 10.1080/17441692.2013.845676
5. Banke-Thomas OE, Banke-Thomas AO, Ameh CA. Factors influencing utilisation of maternal health services by adolescent mothers in low-and middle-income countries: A systematic review. BMC Pregn Childb. (2017) 17:1–14. doi: 10.1186/s12884-017-1246-3
6. Secretary-General U. Keeping the Promise: A Forward-Looking Review to Promote an Agreed Action Agenda to Achieve the Millennium Development Goals by 2015: Report of the Secretary-General. New York, NY (2010).
7. Clemens MA, Kenny CJ, Moss TJ. The trouble with the MDGs: Confronting expectations of aid and development success. World Dev. (2007) 35:735–51. doi: 10.1016/j.worlddev.2006.08.003
8. Organization WH. The Department of Making Pregnancy Safer: Regional Highlights 2009. Geneva: World Health Organization (2010).
9. Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: A systematic review and meta-analysis. PLoS ONE. (2019) 14:e0222566. doi: 10.1371/journal.pone.0222566
10. Geltore TE, Anore DL. The Impact of Antenatal Care in Maternal and Perinatal Health. Empowering Midwives and Obstetric Nurses. London, UK: IntechOpen (2021). p. 107.
11. Organization WH. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization (2016).
12. Konje ET, Magoma MTN, Hatfield J, Kuhn S, Sauve RS, Dewey DM. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC Pregn Childb. (2018) 18:1–13. doi: 10.1186/s12884-018-2014-8
13. Agha S, Tappis H. The timing of antenatal care initiation and the content of care in Sindh, Pakistan. BMC Pregnancy Childbirth. (2016) 16:190. doi: 10.1186/s12884-016-0979-8
14. Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Opportunities for Africa's newborns: Practical data, policy and programmatic support for newborn care in Africa. Antenatal Care. (2006) 2006:55–62.
15. Sahito A, Rabbani U, Zahidie A, Fatmi Z. Determinants of antenatal care utilization in Pakistan: Pakistan demographic health survey 2012-2013. J Pioneer Med Sci. (2016) 6.
16. Kondale M, Tumebo T, Gultie T, Megersa T, Yirga H. Timing of first antenatal care visit and associated factors among pregnant women attending anatal clinics in Halaba Kulito governmental health institutions, 2015. J Women's Health Care. (2016) 5:2167–0420. doi: 10.4172/2167-0420.1000308
17. Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv Res. (2013) 13:1–10. doi: 10.1186/1472-6963-13-256
18. Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregn Childb. (2014) 14:1–13. doi: 10.1186/1471-2393-14-161
19. Boamah SA, Amoyaw J, Luginaah I. Explaining the gap in antenatal care service utilization between younger and older mothers in Ghana. J Biosoc Sci. (2016) 48:342–57. doi: 10.1017/S0021932015000218
20. Montalvo-Liendo N. Cross-cultural factors in disclosure of intimate partner violence: An integrated review. J Adv Nurs. (2009) 65:20–34. doi: 10.1111/j.1365-2648.2008.04850.x
21. Attaran A. An immeasurable crisis? A criticism of the millennium development goals and why they cannot be measured. PLoS Med. (2005) 2:e318. doi: 10.1371/journal.pmed.0020318
22. Fukuda-Parr S. Reducing inequality–The missing MDG: A content review of PRSPs and bilateral donor policy statements. IDS Bull. (2010) 41:26–35. doi: 10.1111/j.1759-5436.2010.00100.x
23. Amin S. The millennium development goals: A critique from the south. Monthly Rev. (2006) 57:1. doi: 10.14452/MR-057-10-2006-03_1
24. Haines A, Cassels A. Can the millennium development goals be attained? Br Med J. (2004) 329:394–7. doi: 10.1136/bmj.329.7462.394
25. Hill PS, Mansoor GF, Claudio F. Conflict in least-developed countries: challenging the Millennium Development Goals. SciELO Public Health. (2010) 2010:562. doi: 10.2471/BLT.09.071365
26. WHO U, UNFPA, World Bank Group and the United Nations Population Division. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF. UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO (2019).
27. Saad–Haddad G, DeJong J, Terreri N, Restrepo–Méndez MC, Perin J, Vaz L, et al. Patterns and determinants of antenatal care utilization: Analysis of national survey data in seven countdown countries. J Glob Health. (2016) 6:10404. doi: 10.7189/jogh.06.010404
28. Assefa E, Tadesse M. Factors related to the use of antenatal care services in Ethiopia: Application of the zero-inflated negative binomial model. Women Health. (2017) 57:804–21. doi: 10.1080/03630242.2016.1222325
29. Regassa N. Antenatal and postnatal care service utilization in southern Ethiopia: a population-based study. Afri Health Sci. (2011) 11.
30. Manyeh AK, Amu A, Williams J, Gyapong M. Factors associated with the timing of antenatal clinic attendance among first-time mothers in rural southern Ghana. BMC Pregn Childb. (2020) 20:1–7. doi: 10.1186/s12884-020-2738-0
31. Kawungezi PC, AkiiBua D, Aleni C, Chitayi M, Niwaha A, Kazibwe A, et al. Attendance and utilization of antenatal care (ANC) services: Multi-center study in upcountry areas of Uganda. Open J Prev Med. (2015) 5:132. doi: 10.4236/ojpm.2015.53016
32. Edward B. Factors influencing the utilisation of antenatal care content in Uganda. Australas Med J. (2011) 4:516. doi: 10.4066/AMJ.2011.849
33. Magadi MA, Madise NJ, Rodrigues RN. Frequency and timing of antenatal care in Kenya: Explaining the variations between women of different communities. Soc Sci Med. (2000) 51:551–61. doi: 10.1016/S0277-9536(99)00495-5
34. Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS ONE. (2017) 12:e0184934. doi: 10.1371/journal.pone.0184934
35. Tessema ZT, Akalu TY. Spatial pattern and associated factors of ANC visits in Ethiopia: Spatial and multilevel modeling of Ethiopian demographic health survey data. Adv Prev Med. (2020) 2020:4676591. doi: 10.1155/2020/4676591
36. Matsumura M, Gubhaju B. Women's status, household structure and the utilization of maternal. Asia Pacific Popul J. (2001) 16:23–44. doi: 10.18356/e8a4c9ed-en
37. Bbaale E. Factors influencing timing and frequency of antenatal care in Uganda. Australas Med J. (2011) 4:431. doi: 10.4066/AMJ.2011.729
38. Wang W. Levels and Trends in the Use of Maternal Health Services in Developing Countries. Calverton, MD: ICF Macro (2011).
39. Robson MG, Stephenson R, Elfstrom KM. Community influences on antenatal and delivery care in Bangladesh, Egypt, and Rwanda. Public Health Rep. (2012) 127:96–106. doi: 10.1177/003335491212700111
40. Verney A, Reed BA, Lumumba JB, Kung'u JK. Factors associated with socio-demographic characteristics and antenatal care and iron supplement use in Ethiopia, Kenya, and Senegal. Maternal Child Nutr. (2018) 14:e12565. doi: 10.1111/mcn.12565
41. Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregn Childb. (2016) 16:1–11. doi: 10.1186/s12884-016-1083-9
42. Owili PO, Muga MA, Chou Y-J, Hsu Y-HE, Huang N, Chien L-Y. Family structure types and adequate utilization of antenatal care in Kenya. Fam Commun Health. (2016) 39:188–98. doi: 10.1097/FCH.0000000000000109
43. Doctor HV. Intergenerational differences in antenatal care and supervised deliveries in Nigeria. Health Place. (2011) 17:480–9. doi: 10.1016/j.healthplace.2010.12.003
44. Ononokpono DN, Odimegwu CO, Imasiku E, Adedini S. Contextual determinants of maternal health care service utilization in Nigeria. Women Health. (2013) 53:647–68. doi: 10.1080/03630242.2013.826319
45. de Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, Oladapo OT, et al. Integrated person-centered health care for all women during pregnancy: Implementing World Health Organization recommendations on antenatal care for a positive pregnancy experience. Glob Health. (2017) 5:197–201. doi: 10.9745/GHSP-D-17-00141
46. Zamawe CO, Banda M, Dube AN. The impact of a community driven mass media campaign on the utilisation of maternal health care services in rural Malawi. BMC Pregn Childb. (2016) 16:1–8. doi: 10.1186/s12884-016-0816-0
47. Adewuyi EO, Auta A, Khanal V, Bamidele OD, Akuoko CP, Adefemi K, et al. Prevalence and factors associated with underutilization of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS ONE. (2018) 13:e0197324. doi: 10.1371/journal.pone.0197324
48. Ghaffar A, Pongponich S, Ghaffar N, Mehmood T. Factors associated with utilization of antenatal care services in Balochistan province of Pakistan: An analysis of the Multiple Indicator Cluster Survey (MICS) 2010. Pak J Medical Sci. (2015) 31:1447. doi: 10.12669/pjms.316.8181
49. Yesuf EA, Calderon-Margalit R. Disparities in the use of antenatal care service in Ethiopia over a period of fifteen years. BMC Pregn Childb. (2013) 13:1–10. doi: 10.1186/1471-2393-13-131
50. McCaw-Binns A, La Grenade J, Ashley D. Under-users of antenatal care: A comparison of non-attenders and late attenders for antenatal care, with early attenders. Soc Sci Med. (1995) 40:1003–12. doi: 10.1016/0277-9536(94)00175-S
51. Gupta S, Yamada G, Mpembeni R, Frumence G, Callaghan-Koru JA, Stevenson R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS ONE. (2014) 9:e101893. doi: 10.1371/journal.pone.0101893
52. Exavery A, Kanté AM, Hingora A, Mbaruku G, Pemba S, Phillips JF. How mistimed and unwanted pregnancies affect timing of antenatal care initiation in three districts in Tanzania. BMC Pregn Childb. (2013) 13:1–11. doi: 10.1186/1471-2393-13-35
53. Abosse Z, Woldie M, Ololo S. Factors influencing antenatal care service utilization in hadiya zone. Ethiop J Health Sci. (2010) 20:69432. doi: 10.4314/ejhs.v20i2.69432
54. Kumar G, Choudhary TS, Srivastava A, Upadhyay RP, Taneja S, Bahl R, et al. Utilisation, equity and determinants of full antenatal care in India: Analysis from the National Family Health Survey 4. BMC Pregn Childb. (2019) 19:1–9. doi: 10.1186/s12884-019-2473-6
55. Haruna-Ogun OA. Geographical differentials in uptake of antenatal care services in Nigeria. Health Care Women Int. (2018) 39:34–49. doi: 10.1080/07399332.2017.1388804
56. Dahiru T, Oche OM. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afri Med J. (2015) 22:6527. doi: 10.11604/pamj.2015.21.321.6527
57. Gebre E, Worku A, Bukola F. Inequities in maternal health services utilization in Ethiopia 2000–2016: Magnitude, trends, and determinants. Reprod Health. (2018) 15:1–9. doi: 10.1186/s12978-018-0556-x
Keywords: antenatal care, women, maternal mortality, low- and middle-income countries, reproductive-age women
Citation: Chilot D, Belay DG, Ferede TA, Shitu K, Asratie MH, Ambachew S, Shibabaw YY, Geberu DM, Deresse M and Alem AZ (2023) Pooled prevalence and determinants of antenatal care visits in countries with high maternal mortality: A multi-country analysis. Front. Public Health 11:1035759. doi: 10.3389/fpubh.2023.1035759
Received: 03 September 2022; Accepted: 06 January 2023;
Published: 30 January 2023.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Tores P. G. Theorell, Karolinska Institutet (KI), SwedenCopyright © 2023 Chilot, Belay, Ferede, Shitu, Asratie, Ambachew, Shibabaw, Geberu, Deresse and Alem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dagmawi Chilot,  ZGFnaW1jaGlsb3QyMUBnbWFpbC5jb20=
ZGFnaW1jaGlsb3QyMUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.