
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 02 March 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1024228
This article is part of the Research Topic Mental Health and Internalized Stigma in people with Severe Mental Illness View all 6 articles
Background: Giving care to someone who is experiencing mental distress is a difficult and challenging task that could be detrimental to the caregiver's overall quality of life. Numerous studies show that caregivers frequently experience mental distress and feel stigmatized. However, there is limited study done on this topic in our country.
Objective: To determine the magnitude and associated factors of perceived stigma and common mental disorder among primary caregivers of adults with mental illness in public hospitals at Harari regional state, Eastern Ethiopia, 2022.
Methods: A cross-sectional study design was conducted. A total of 419 participants were recruited by a systematic random sampling technique. The data was collected by using a face-to-face interview and by reviewing patients' charts. Perceived stigma and common mental disorder were assessed by Family Interview Schedule and Self-Reporting Questionnaire, respectively. Epi-data version 4.6.2 was used to enter data, and SPSS version 20 was used to analyze. Bivariable and multivariable logistic regression were performed. P-values < 0.05 were considered statistically significant.
Result: The magnitude of perceived stigma and common mental disorder were 42.5% (95% CI, 37.7–47.3) and 39.4% (95% CI, 34.8–44.0) respectively. Age of caregiver between 26 and 33 [AOR = 3.13, 95% CI: (1.71–8.93)], no formal education [AOR = 3.85, 95% CI: (1.81–8.15)], illness duration ≥7 years [AOR = 1.93, 95% CI: (1.04–3.57)], family history of mental illness [AOR = 1.92, 95% CI: (1.09–3.39)] and poor social support [AOR = 4.87, 95% CI: (3.74–12.71)] were significantly associated with perceived stigma. Being female [AOR = 1.92, 95% CI: (1.31–3.34)], having no formal education [AOR = 4.04, 95% CI: (2.15–10.01)], having a family history of mental illness [AOR = 2.26, 95% CI: (1.29–4.00)], having comorbid other illness [AOR = 2.13, 95% CI: (1.15–3.94)], and having poor social support [AOR = 4.58, 95% CI: (2.53–8.28)] were significantly associated with common mental disorder.
Conclusion: The magnitude of perceived stigma and common mental disorder was high among primary caregivers of patients with mental illness compared with other studies. Age of caregiver between 26 and 33, no formal education, duration of illness ≥7 years, family history of mental illness and poor social support were associated with perceived stigma and being female, no formal education, family history of mental illness, comorbid other illness and poor social support were associated with common mental disorder.
The most frequent and challenging issues in daily life are mental disorders, which are typically characterized by a combination of abnormal thoughts, perceptions, emotions, behavior, and interactions with others. They include: depression, bipolar disorder, schizophrenia and other psychoses, dementia, and developmental disorders. Their magnitude indicates that over 25% of people experience a mental disorder at some point in their lifespan (1–3).
A common mental disorder (CMD) is one of the most common mental illnesses in the world, and it refers to a set of illnesses that commonly include depression, anxiety, and somatoform disorders (4). A mental disorder is characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior. It is usually associated with distress or impairment in important areas of functioning. There are many different types of mental disorders. In most cases, they do not impair insight or cognition, but they do cause significant emotional pain and interfere with daily activities. The cumulative cost of CMDs to society is substantial despite the fact that they are typically less impairing than serious psychiatric diseases due to their higher prevalence (5).
Stigma is a social process that is characterized by separation, rejection, and blame or discrediting of an individual or group (6). It takes place on three levels: organizational, public, and individual. The stigma that exists at the individual level, or perceived stigma, refers to the respondent's perceptions that people with mental illness are typically stigmatized (7).
Caregivers are individuals who pay attention of others, often parents, spouses, or kids with special medical needs or disabilities (8). Caregiving is a broad responsibility that involves not only providing physical assistance and care but also emotional support. It is frequently a very stressful task that creates difficulties for the caregivers on the social, emotional, behavioral, and financial aspects, making them prone to common mental disorders like depression, anxiety, and somatic problems (9, 10).
The most prevalent cause of disability worldwide is mental illness, which includes common mental disorders, neurological disorders, substance use disorders, and suicide. Over 450 million people are thought to be affected by mental disorders internationally (11). CMD has recently been found to be 14% of the overall illness burden. It is anticipated that by 2030, it will rank as the primary cause of disease burden (12).
Studies have shown that family caregivers of patients with mental illness frequently receive insufficient support from mental health specialists and experience common mental disorder themselves. According to research from Latin America, 40% of caregivers met the criteria for being at risk of depression, compared to 13–18% of the general population (13). Nearly half (43.8%) of caregivers of psychiatric outpatients in Nigerian research experienced psychological distress (14).
One of the most difficult psychosocial challenges that family members or caregivers of people with mental illness must face is stigma. Evidence from around the world shows that the psychosocial burden on families of those with mental illnesses negatively affects both the family members and the patients they are caring for (15–17). One Moroccan study on family members of schizophrenia patients revealed significant levels of perceived stigma and burden on their families (18).
Among primary caregivers of patients with mental illness, a number of factors were consistently associated to common mental disorder, including the length and type of care provided, unemployment, the length of the illness, behavioral problems, cognitive and functional disabilities, feelings of isolation, anger, sadness, and guilt, poor social support, patient age, negative coping mechanisms, and real stigma (13, 14, 19).
Despite the fact that several studies have been conducted in the United States (US), Europe, and Africa. However, there have been few studies conducted in Ethiopia, and no study has been conducted in eastern Ethiopia regarding the magnitude of common mental disorders and perceived stigma among caregivers of patients with mental illness in Harari Regional State, eastern Ethiopia. Therefore, the purpose of this study is to assess the magnitude of perceived stigma, common mental disorders and associated factors among primary caregivers of adult patients with mental illness attending public hospitals, Harari Regional State, eastern Ethiopia.
Public hospitals in the Harari Regional State were used to perform the study. Harari Regional State is one of the 11 regions in Ethiopia, located in the eastern part of the country. The districts of Oromia regional state that form the borders of the region are Fedis district in the south, Gursum and Babile districts in the east, Haramaya district including Aweday in the west, and Kombolcha and Jarso districts in the north., which are the districts of Oromia regional state. The Harari Region is divided into six urban and three rural administrative districts in accordance with the present administrative system. The region had 183 344 people overall, 99 321 (54.2%) of whom lived in cities, and 84 023 (45.8%) of whom lived in rural areas. According to the Harari regional health bureau spokesperson, there are two public, one police, and two private hospitals. There are also eight (four urban and four rural) health centers, 19 health posts and 10 private clinics in the region. The study was conducted from April 01 to April 30, 2022.
An institutional-based quantitative cross-sectional study design was employed. All the primary caregivers of adult patients with mental illness attending public hospitals in Harari regional state, eastern Ethiopia who were available during the data collection period and whose age was ≥18 years were included in the study. Caregivers who were unable to communicate due to the severity of their health conditions were excluded.
The sample size for this study was calculated using the formula for estimation of single population proportion by considering the proportion of outcome variables of perceived stigma among primary caregivers studied in Jimma City was 54.7% (20), and Z value corresponding with a 95% confidence level (1.96); and d is the 5% desired precision.
Where:
Including 10% of the non-response rate, the final sample size was 419.
Concerning the sampling procedure, the estimated sample was proportionally allocated to each hospital based on the number/load of patients attending psychiatric units. Finally, a systematic random sampling technique was used to reach the actual primary care givers. The total number of patients attending psychiatric services at the psychiatric unit was 900 per month at HFSUH and 300 at Jugal hospital. Among these patients, 745 and 230 of the patients come with their care givers to HFSUH and Jugal, respectively. Then the total number of primary care givers was divided by the simple size and the interval (K = 2) was established. Then, based on the calculated K-value, the data was collected from both hospitals. Therefore, the sampling interval was 2. The first study participant was selected by a lottery method from each hospital independently, and the next study participants were chosen at a regular interval (every 2). They were interviewed by data collectors as shown in Figure 1.
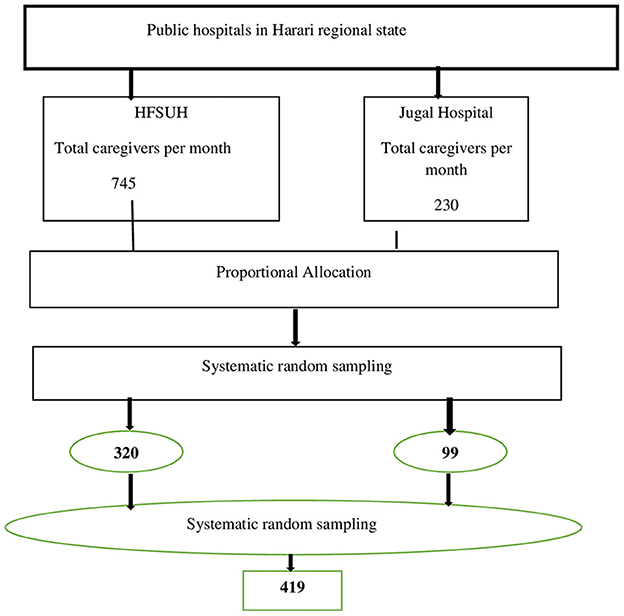
Figure 1. The schematic presentation of the sampling procedure for the study on magnitude of perceived stigma and CMD and associated factors among caregivers of patients with mental illness attending public hospitals of Harari regional state 2022.
An interview-based, pretested, and semi-structured questionnaire adapted from different literatures was administered. A face-to-face interview technique was used to collect the data. The questionnaire solicits information about the socio-demographic conditions, COVID-19 related variables, mental health problems and behavioral variables, the presence of suicidal behaviors, medication non-adherence, sleep disturbances, and quality of life among patients having mental illness.
An SRQ-20 that had been locally validated was used to measure CMD. The SRQ-20 consists of 20 yes/no questions on whether you have ever experienced depressive, anxiety, panic, or somatic symptoms in the preceding 30 days. The total score was dichotomized and score < 6 was regarded as no CMD and score greater or equal to 6 was regarded as having CMD, high scores indicating a high level of CMD. The tool was developed by World Health Organization and assesses primarily non-psychotic mental illness. It has 20 questions, answered by YES or NO with codes “1” represents the presence of a symptom, and “0” if the symptom is absent (21).
The WHO Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) test was used to evaluate the substance use behavior of primary care providers of patients with mental illness (22).
Social support was assessed using the Oslo 3-item Social Support Scale. This test measures the degree of social support in a very quick and cost-effective manner. A score of 3–8 represents poor social support, a score of 9–11 represents moderate support, and 12–14 represents strong support in this study (23).
The brief resilient coping scale (BRCS-4) was used to assess the coping strategies for difficult situations. Those primary care givers who scored 4–13 points were considered low-resilient coopers, 14–16 points were medium-resilient coopers, and 17–20 points were highly resilient coopers (24).
Family Interview Schedule: this is an instrument developed by WHO as part of the study on the course and outcome of schizophrenia. The stigma component of this instrument was used in different parts of Ethiopia; Jimma (20, 25), and Bahir Dare (26). The stigma part of this instrument has 14 items which can be rated on a four-level Likert scale of 0 means “not at all,” 1 means “sometimes,” 2 means “often” and 3 means “a lot.” In the 14 items, the sum of all scores ≥1 was computed. Those who scored below the mean were considered as “low stigma,” and those who scored above the mean were considered as “high stigma” (27). Data were collected by three trained BSc psychiatric nurses and supervised by one MSc in mental health professional. COVID-19 prevention protocol was completely applied during data collection.
The questionnaire was initially prepared in English, translated by experts into Afaan Oromo and Amharic, and then returned to English in order to maintain the consistency of the data. To ensure the quality of the data, we adapted standardized and validated tools specific to the research objectives. The supervisor and data collectors received intensive 1-day training. One week prior to the actual data collection a pre-test was conducted among 5% of the sample size in Jinela Health Center In order to evaluate the acceptability and applicability of the procedures and tools. The supervisors and investigators constantly monitored data collectors throughout the data collection process to maintain the consistency and completeness of the questionnaire. In order to reduce errors during data input, double data entry was done by two data clerks.
The gathered information was entered into EPI Data version 3.1, and SPSS version 20 was used for analysis. In order to describe categorical variables, frequency and percentage were used. After being evaluated for normality, continuous variables were described using the relevant summary measures and Bi-variable and multivariable binary logistic regression were carried out. The relationship between the dependent and independent variables was examined.
To identify significantly associated variables in the model, independent variables from bivariable logistic analysis with a p < 0.25 were fitted into multivariable logistic regression. The strength of the association was determined using the odds ratio with the 95% confidence interval, and association to be statistically significant if the p-value was < 0.05 at final model. In all of the models, the multi-collinearity of independent variables was tested using the variance inflation factor (VIF). In addition, model-goodness of fit was checked by using the Hosmer-Lemeshow test.
From a total of 419 samples, 414 participants were included in the study, with a response rate of 98.8%. Regarding the sex of both patient and caregiver, the majority of patients [231 (55.8%)] were male. However, both sexes equally participated regarding caregiving. The result of the age of both patients and caregivers showed that 113 (27.3%) patients were in the age range of 26–33 years and 120 (29%) of caregivers were in the age range of 34–41 years. Regarding the marital status and religion, about 186 (44.9%) of participants were married, and 184 (44.4%) were Islamic followers. Occupation and educational status were also studied variables, and the result showed that 113 (27.3%) were farmers and 173 (41.8%) had no formal education. Regarding the residence of participants, 195 (52.9%) came from urban areas and 107 (25.8%) earned a monthly income of < 1,000 ETB as shown in Table 1.
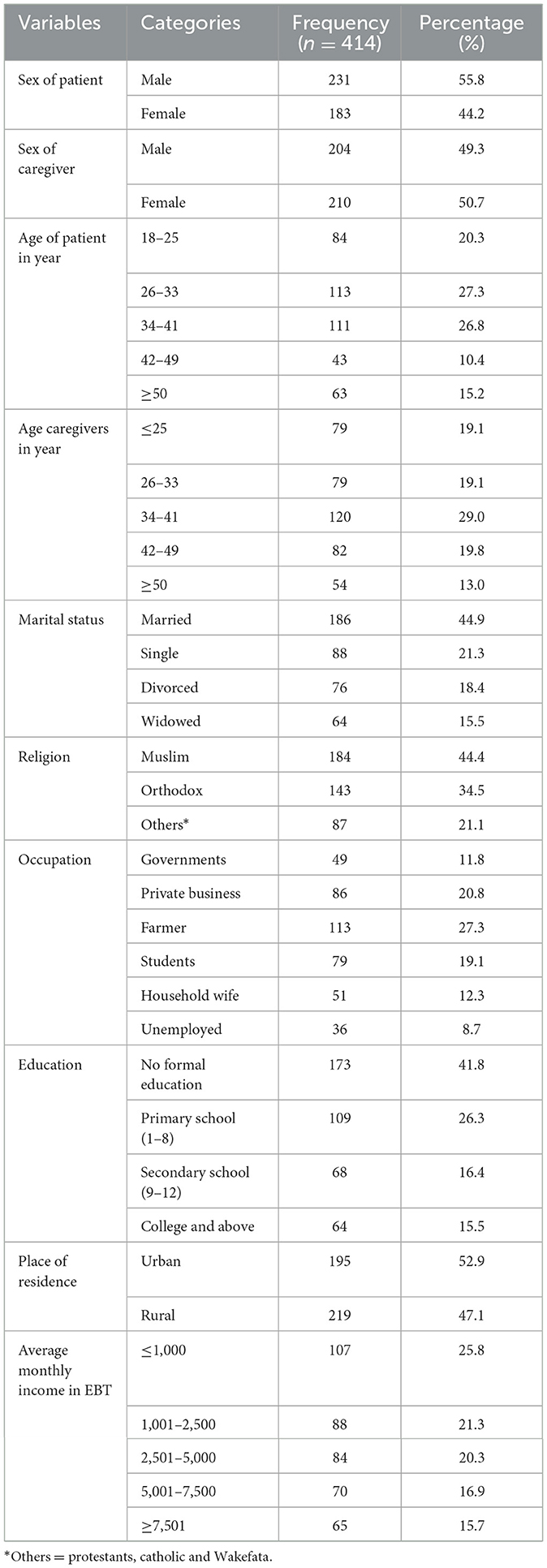
Table 1. Socio-economic distributions among primary caregivers of adult patients with mental illness attending at Harari region state public hospitals, Eastern Ethiopia, 2022 (n = 414).
Regarding the clinical characteristics of the respondents, about 85 (20.5%) had a family history of mental illness, 157 (37.9%) had a patient whose illness lasted for < 1 year, 153 (37%) spent the whole day giving care to the patient, 196 (47.3%) had a patient whose illness was a second episode, 109 (25.8%) had a comorbid illness, 123 (29.8%) had a patient who was not admitted to hospital, 123 (29.8%) had a patient who was diagnosed with schizophrenia, and 118 (28.5%) were given care for < 1 month. Regarding substance use, 193 (46.6%) had used any substance in their lifetime and 149 (36%) were current users. Regarding psychosocial factors, 159 (38.4%) had moderate social support and 128 (30.9%) had poor social support as shown in Table 2.
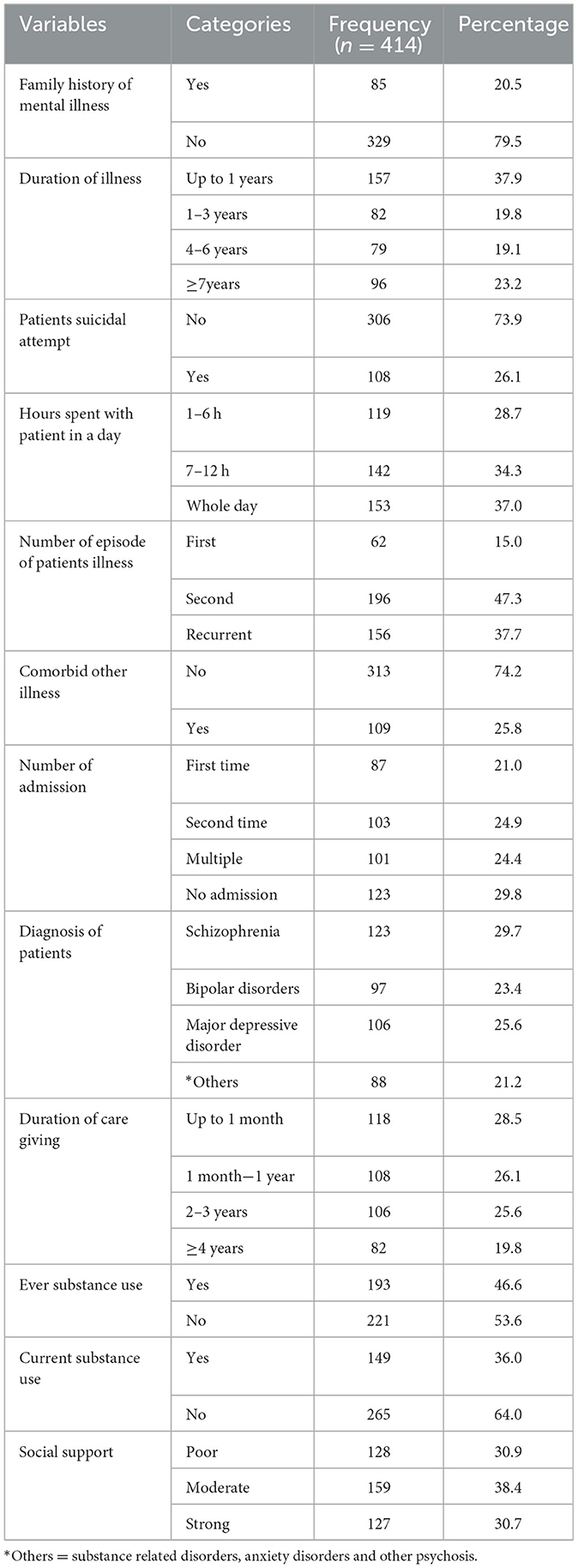
Table 2. Clinical, substance use, psychosocial characteristics among primary caregivers of adult patients with mental illness attending at Harari region state public hospitals, Eastern Ethiopia, 2022 (n = 414).
Magnitude of perceived stigma and common mental disorder among participants were 42.5% (95% CI, 37.7–47.3) and 39.4% (95% CI, 34.8–44.0), respectively.
In bivariable logistic analysis, variables; age of caregivers, educational status, number of admission, duration of illness, time spent with patient in day, family history of mental illness and social support were found to have a p-value < 0.25. These variables fulfilled minimum requirements for further multivariable logistic regression model.
From multivariable logistic regression variables; age of caregiver between 26 and 33, no formal education, duration of illness ≥7 years, family history of mental illness and poor social support were statistically significant with perceived stigma at p-value < 0.05.
In this study, the odds of perceived stigma among participants whose ages were between 26 and 33 years old was about 3.13 times higher as compared with age ≥50 years [AOR = 3.13, 95% CI: (1.71–8.93)].
The results of this study showed that the odds of perceived stigma among participants with no formal education was about 3.85 times higher as compared with educational status of college or above [AOR = 3.85, 95% CI: (1.81–8.15)].
The odds of perceived stigma among participants whose duration of illness was ≥7 years was about 1.93 times higher as compared with participants whose duration of illness was < 1 year [AOR = 1.93, 95% CI: (1.04–3.57)].
In this study, the odds of perceived stigma among participants with a family history of mental illness were 1.92 times higher as compared with participants without family history of mental illness [AOR = 1.92, 95% CI: (1.09–3.39)].
Social support was also another factor which was associated with perceived stigma. Participants with poor social support were 4.87 times more likely to perceive stigma as compared with participants with strong social support [AOR = 4.87, 95% CI: (3.74–12.71)] as shown in Table 3.
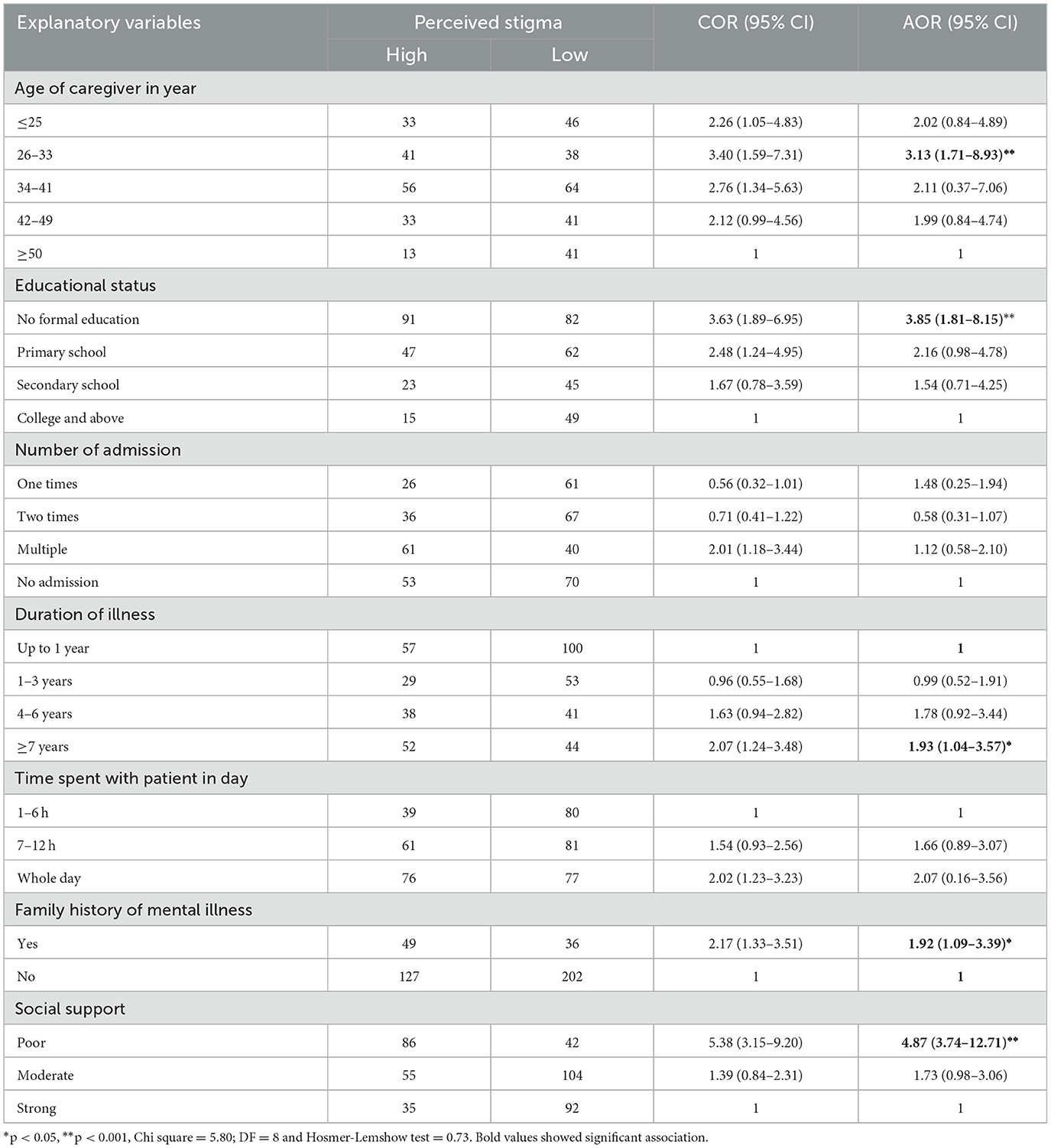
Table 3. Factors associated with perceived stigma in multivariate and bivariate logistic regression analysis among primary caregivers of adult patients with mental illness attending at Harari region state public hospitals, Eastern Ethiopia, 2022 (n = 414).
In bivariable logistic analysis, variables such as sex, marital status, educational status, family history of mental illness, duration of illness, comorbid other illness, and social support were found to have a p-value < 0.25. These variables fulfilled minimum requirements for further multivariable logistic regression model.
Being female, having no formal education, having a family history of mental illness, having comorbid illness, and having poor social support were statistically significant with common mental disorder at a p-value < 0.05.
Being female was associated with common mental disorder in this study. The odds of having a common mental disorder among female participants were about 1.92 times higher as compared to male participants [AOR = 1.92, 95% CI: (1.31–3.34)]. No formal education was also associated with common mental disorder in this study. The odds of having a common mental disorder among participants with no formal education was about 4.04 times higher as compared to those whose educational level is college or above [AOR = 4.04, 95% CI: (2.15–10.01)].
The results of this study also showed that the odds of having a common mental disorder among participants with a family history of mental illness was about 2.26 times higher as compared with participants without a family history of mental illness [AOR = 2.26, 95% CI: (1.29–4.00)]. The odds of having a common mental disorder participants with comorbid other illness were about 2.13 times higher as compared with participants without comorbidity [AOR = 2.13, 95% CI: (1.15–3.94)].
Social support was also another factor which was associated with common mental disorder. Participants with poor social support were 4.58 times more likely to have a common mental disorder as compared with participants with strong social support [AOR = 4.58, 95% CI: (2.53–8.28)] as shown in Table 4.
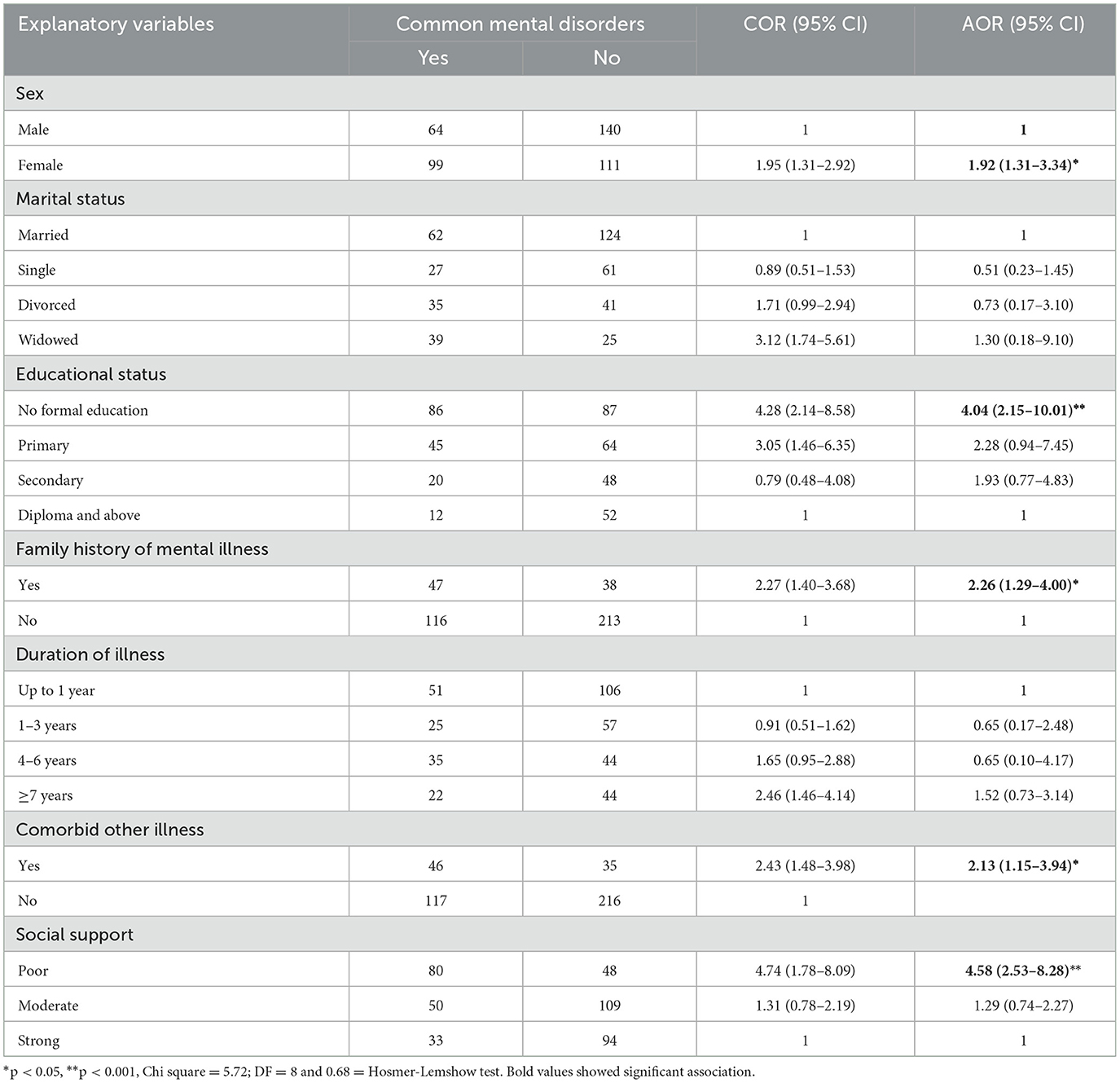
Table 4. Factors associated with common mental disorders in multivariate and bivariate logistic regression analysis among primary caregivers of adult patients with mental illness attending at Harari region state public hospitals, Eastern Ethiopia, 2022 (n = 414).
Caregiving for people with mental illness has a significant influence on families and is frequently accompanied by significant stress on family members, which can lead to a reduction in social activities and, over time, isolation. The most frequent impact of caring for people with serious mental diseases included behavioral disturbances, functional impairments, physical impairments, cognitive impairments, and concern that their relative may attempt suicide (28, 29). Caring itself is an independent risk factor for CMD independent of the other life stressors they have to deal with (30).
The reported magnitude of CMD among the primary caregivers in this study was 39.4 % (95% CI: 34.8–44.0). The result of this study is in line with cross-sectional studies conducted in Saudi Arabia (38.4%) among caregivers of patients with mental disorders (31) and with a study conducted in Nigeria (43.8%) (14).
However, the findings from this study revealed a lower magnitude of CMD among caregivers of patients with mental disorders when compared with studies conducted in India (80%) (32), Nigeria (79.8%) (33), and Ethiopia (56.7%) (34). This discrepancy could be attributed to a smaller sample size and being the primary caregiver for the most chronic form of mental disorder, schizophrenia, noted in the Indian and Nigerian studies, and in the Ethiopian study, where the study was conducted among caregivers of severe mental illness. Patients with severe mental disorders require a greater need for emotional support, assisting with maintenance of social and living skills, household chores and financial arrangements, supervising medication, and monitoring signs for illness and relapse prevention (35). This study revealed a higher prevalence of CMD among caregivers of patients with mental disorders when compared with another study conducted in Nigeria (36). This discrepancy could be attributed to the different tools, i.e., the Self-Reporting Questionnaire-20 was used in the current study, but the Patient Health Questionnaire, used in the Nigerian study (37).
On the other hand, this study also revealed that the magnitude of perceived stigma among the primary caregivers among patients with mental illness was 42.5% (95% CI, 37.7–47.3). The current finding was in line with the study conducted in America 43% (38) and Ethiopia 38.5% (39). However, the result of this study was lower than the studies conducted in Ethiopia, in Bahirdar 89% (26), Butajira 75% (40), Addis Ababa 62.6% (41), Jimma 54.7% (20), Nigeria 85.3% (42), Chile 90% (43), and Belgium 86% (44). The possible justification for the variation might be the tool difference used to assess the perceived stigma. For example, the Addis Ababa study used the standardized perceived devaluation and discrimination questionnaire to assess perceived stigma, whereas this study used Family Interview Schedule. The other possible reason might be that the studies conducted in Addis Ababa, Ethiopia, Belgium, and Chile were only among schizophrenic patients, whereas this study includes caregivers of all severely mentally ill patients. Caregivers of patients with schizophrenia reported significantly higher stigma than patients with bipolar disorder and recurrent depressive disorder (45). In addition to this, the Butajira, Ethiopia, and Belgium studies limit the caregivers to only family members, whereas this study includes any kind of caregiver who supports severely mentally ill patients, and the Butajira study was a community-based study, whereas this study is an institutional-based study. On the other hand, the finding of the current study was higher than that of the study done in India 21% (46). The possible reasons might be the difference in the study setting, socio-cultural backgrounds, and tool differences.
This study reported that being female had a statistically significant association with CMD that was in line with a study done in Nepal (47) and study done in Ethiopia and a review also revealed that female caregivers were more likely to suffer from mental distress than male counterparts (48). All over the world, informal care for family members with chronic conditions or disabilities including those elderly and those with mental illness provided most commonly by females (49). Providing care for family members often entails bearing emotional, physical, social, and financial burdens that make care givers suffer from more stressful life events (50).
This study revealed that those with low educational status had a statistically significant association with CMD. Studies done in the United States of America (51) and in Nepal (47) revealed that those caregivers who had low educational status were more likely to be associated with CMD than those with higher educational status. A systematic review also reported that there is a significant association between CMD and lower educational status (52). However, a study in India reported that lower mental distress was noted among primary caregivers who had lower education (32). This might be due to a significantly high number of participants with lower educational status who were included in the Indian study.
A family history of mental illness was significantly associated with the caregivers' CMD. Caregiving for family members with mental illnesses is usually undertaken on a full-time basis. This would result in intense stress and burnout among the family members. Furthermore, the family suffers from social stigma, which is associated with a high level of mental distress among the family caregivers (53). Though personal satisfaction, strengthening family ties, and saving resources could be seen as positive aspects of caring, the negative impact could be very significant, as they give up work and leisure. They feel overwhelmed and trapped, and that they suffer in silence (54).
In this study, the presence of comorbid medical illnesses had a statistically significant association with CMD. This is evidenced by the presence of comorbid medical conditions not only associated with common mental disorders but also increases the re-admission of patients with mental disorders (55) and the presence of common mental disorders was associated with the development and progression of medical conditions like heart failure (56). The presence of common mental disorders was also associated with the subsequence diagnosis of medical conditions like hypertension (57). The prevalence of common mental disorders was higher among patients with medical conditions (58).
Those caregivers who had poor social support had a statistically significant association with CMD and this fact is supported by a study conducted in Addis Ababa, Ethiopia (34). Moreover, lack of social support has a profound effect on caregivers' outcomes, and less social support corresponds to a higher symptomatology of caregivers. Provision of care is also associated with a decline in social support and increased isolation and withdrawal of caregivers (48).
In this study, the odds of experiencing perceived stigma were higher among the age group between 26 and 33 years compared to 50 years old. The possible reason might be that being sensitive to community rejection is more common than being adaptive. Caregivers who had no formal education were more likely to experience perceived stigma as compared to those who were educated to college or above. This might be because those who are educated caregivers might have a good coping mechanism to sigma and understand the role of caregivers for mentally ill patients and understand the nature of the illness.
The odds of having perceived stigma was higher among patients with a long duration of illness (more than 7 years) compared to a short duration (< 1 year). This finding was supported by a previous study carried out in Jimma and Bahirdar, Ethiopia (20, 26). The possible explanation might be that caregivers of mentally ill patients may perceive stigma when the duration of the illness increases. The burden of treating mentally ill patients will lie on the caregivers in every aspect of their lives, including economically, psychologically, and physically, especially when the illness becomes chronic or of long duration.
Respondents who had poor social support were more likely to experience perceived stigma as compared to those who had strong social support. This study is supported by studies of Ergetie et al. (26), Tesfaw et al. (41), and Chien et al. (59). The possible justification for this might be the caregivers who had mentally ill patients in the family member may ignore themselves from social activities and not able to share responsibilities and role in the community.
The prevalence of CMD and perceived stigma among the primary caregivers of patients with severe mental illness were high. Being female, low educational status, family history of mental illness, presence of comorbid medical illness and poor social support were significantly associated with CMD. Low educational status, family history of mental illness, being between 26 and 33 years old, having been ill for more than 7 years and poor social support were significantly associated with the perception of stigma among primary caregivers of patients with severe mental illnesses. Therefore, attention should be given, and essential psychosocial care should be provided, to maintain the mental health of primary caregivers of individuals with mental illness.
Since it was a cross-sectional study design, it cannot allow establishing a temporal relationship between outcome variable and independent variables. Some inquiries in the study have sensitive issues, which might leads to social desirability bias.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Haramaya University College of Health and Medical Sciences' Institutional Health Research Ethics Review Committee (IHRERC). The patients/participants provided their written informed consent to participate in this study.
KN, DT, TB, and HA were participated in inception of idea, proposal development, data collection, analysis, and final write up. HA and KN have participated on write up of the manuscript. All authors approved the final manuscript.
We want to sincerely thank our data collectors for their dedication and contributions, which are truly amazing. We also like to express our gratitude to the study participants who voluntarily participated in it.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ASSIST, Alcohol, Smoking and Substance Involvement Screening Test; CMD, Common Mental Disorder; HFSUH, Hiwot Fana Specialized University Hospital; NGO, None Governmental Organization; SRQ, Self-Reporting Questionnaire; SPSS, Statistical Package for Social Science; USA, United State of America; WHO, World Health Organization.
1. Roe J, Aspinall P. The restorative benefits of walking in urban and rural settings in adults with good and poor mental health. Health Place. (2011) 17:103–13. doi: 10.1016/j.healthplace.2010.09.003
2. Romaniuk P, Semigina T. Ukrainian health care system and its chances for successful transition from Soviet legacies. Global Health. (2018) 14:1–11. doi: 10.1186/s12992-018-0439-5
4. Risal A. Common mental disorders. Kathmandu Univ Med J. (2011) 9:213–7. doi: 10.3126/kumj.v9i3.6308
5. Stansfeld S, Clark C, Bebbington P, King M, Jenkins R, Hinchliffe S. Common mental disorders. NHS Digital. (2016).
6. Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Simon and Schuster (2009).
7. Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatising attitudes to depression: randomised controlled trial. Br J Psychiatry. (2004) 185:342–9. doi: 10.1192/bjp.185.4.342
8. Gupta A, Sharma R. Burden and coping of caregivers of physical and mental illnesses. Delhi Psychiatry J. (2013) 16:367–74. doi: 10.4103/jnrp.jnrp_312_17
9. Tabeleão VP, Tomasi E, Quevedo LdÁ. Burden on relatives of people with psychic disorder: levels and associated factors. Arch Clin Psychiatry (São Paulo). (2014) 41:63–6. doi: 10.1590/0101-60830000000012
10. Bello-Mojeed M, Omigbodun O, Ogun O, Adewuya A, Adedokun B. The relationship between the pattern of impairments in autism spectrum disorder and maternal psychosocial burden of care. OA Autism. (2013) 1:4. doi: 10.13172/2052-7810-1-1-430
11. Organization WH Control RfIT. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. Geneva: World Health Organization (2018).
12. WHO. Investing in Mental Health: World Health Organization. Geneva: World Health Organization (2018).
13. El-Tantawy AMA, Raya YM, Zaki A. Depressive disorders among caregivers of schizophrenic patients in relation to burden of care and perceived stigma. Curr Psychiatr. (2010) 17:15–25.
14. Oshodi Y, Adeyemi J, Aina O, Suleiman T, Erinfolami A, Umeh C. Burden and psychological effects: caregiver experiences in a psychiatric outpatient unit in Lagos, Nigeria. Afr J Psychiatry. (2012) 15:99–105. doi: 10.4314/ajpsy.v15i2.13
15. Larson JE, Corrigan P. The stigma of families with mental illness. Acad Psychiatry. (2008) 32:87–91. doi: 10.1176/appi.ap.32.2.87
16. Corrigan PW, Watson AC, Miller FE. Blame, shame, and contamination: the impact of mental illness and drug dependence stigma on family members. J Fam Psychol. (2006) 20:239. doi: 10.1037/0893-3200.20.2.239
17. Chang KH, Horrocks S. Lived experiences of family caregivers of mentally ill relatives. J Adv Nurs. (2006) 53:435–43. doi: 10.1111/j.1365-2648.2006.03732.x
18. Ciftci A, Jones N, Corrigan P, Jones N, Corrigan P. Mental health stigma in the Muslim community. J Muslim Ment Health. (2012) 7:17–32. doi: 10.3998/jmmh.10381607.0007.102
19. Grandón P, Jenaro C, Lemos S. Primary caregivers of schizophrenia outpatients: burden and predictor variables. Psychiatry Res. (2008) 158:335–43. doi: 10.1016/j.psychres.2006.12.013
20. Muhammed MS, Tesfaye M, Girma E, Birkie M. Level of perceived stigma among caregivers of persons with severe mental illness in Jimma City, Ethiopia: a cross-sectional study. Am J Clin Exp Med. (2021) 9:77. doi: 10.11648/j.ajcem.20210904.11
21. Beusenberg M Orley JH World Health Organization. A user's guide to the self-reporting questionnaire (SRQ No. WHO/MNH/PSF/948 Unpublished). Geneva: World Health Organization (1994).
22. WAW Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. (2002) 97:1183–94. doi: 10.1046/j.1360-0443.2002.00185.x
23. Kocalevent R-D, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. (2018) 6:1–8. doi: 10.1186/s40359-018-0249-9
24. Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. (2004) 11:94–101. doi: 10.1177/1073191103258144
25. Ayalew M, Workicho A, Tesfaye E, Hailesilasie H, Abera M. Burden among caregivers of people with mental illness at Jimma University Medical Center, Southwest Ethiopia: a cross-sectional study. Ann Gen Psychiatry. (2019) 18:1–11. doi: 10.1186/s12991-019-0233-7
26. Ergetie T, Yohanes Z, Asrat B, Demeke W, Abate A, Tareke M. Perceived stigma among non-professional caregivers of people with severe mental illness, Bahir Dar, northwest Ethiopia. Ann Gen Psychiatry. (2018) 17:1–8. doi: 10.1186/s12991-018-0212-4
27. Sartorius N, Janca A. Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol. (1996) 31:55–69. doi: 10.1007/BF00801901
28. Amir N, Freshman M, Foa EB. Family distress and involvement in relatives of obsessive-compulsive disorder patients. J Anxiety Disord. (2000) 14:209–17. doi: 10.1016/S0887-6185(99)00032-8
29. Eckardt JP. Caregivers of people with severe mental illness in the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:53. doi: 10.1016/S2215-0366(20)30252-2
30. Stansfeld S, Smuk M, Onwumere J, Clark C, Pike C, McManus S, et al. Stressors and common mental disorder in informal carers—an analysis of the English Adult Psychiatric Morbidity Survey 2007. Soc Sci Med. (2014) 120:190–8. doi: 10.1016/j.socscimed.2014.09.025
31. Alzahrani SH, Fallata EO, Alabdulwahab MA, Alsafi WA, Bashawri J. Assessment of the burden on caregivers of patients with mental disorders in Jeddah, Saudi Arabia. BMC Psychiatry. (2017) 17:1–8. doi: 10.1186/s12888-017-1368-1
32. Gupta A, Solanki R, Koolwal G, Gehlot S. Psychological well-being and burden in caregivers of patients with schizophrenia. Int J Public Health Res. (2015) 4:70–6. doi: 10.5455/ijmsph.2015.0817201416
33. Yusuf AJ, Nuhu FT. Factors associated with emotional distress among caregivers of patients with schizophrenia in Katsina, Nigeria. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:11–6. doi: 10.1007/s00127-009-0166-6
34. Sintayehu M, Mulat H, Yohannis Z, Adera T, Fekade M. Prevalence of mental distress and associated factors among caregivers of patients with severe mental illness in the outpatient unit of Amanuel Hospital, Addis Ababa, Ethiopia, 2013: cross-sectional study. J Mol Psychiatry. (2015) 3:1–10. doi: 10.1186/s40303-015-0014-4
35. Jeon YH, Brodaty H, Chesterson J. Respite care for caregivers and people with severe mental illness: literature review. J Adv Nurs. (2005) 49:297–306. doi: 10.1111/j.1365-2648.2004.03287.x
36. Inogbo C, Olotu S, James B, Nna E. Psychiatric disorders amongst caregivers who are first degree relatives of patients with schizophrenia. J Psychiatry Human Behav Sci. (2017) 1:1. doi: 10.11604/pamj.2017.28.284.11574
37. Husain N, Gater R, Tomenson B, Creed F. Comparison of the personal health questionnaire and the self-reporting questionnaire in rural Pakistan. J Pak Med Assoc. (2006) 56:366.
38. Struening EL, Perlick DA, Link BG, Hellman F, Herman D, Sirey JA. Stigma as a barrier to recovery: the extent to which caregivers believe most people devalue consumers and their families. Psychiatr Serv. (2001) 52:1633–8. doi: 10.1176/appi.ps.52.12.1633
39. Minichil W, Getinet W, Kassew T. Prevalence of perceived stigma and associated factors among primary caregivers of children and adolescents with mental illness, Addis Ababa, Ethiopia: cross-sectional study. PLoS ONE. (2021) 16:e0261297. doi: 10.1371/journal.pone.0261297
40. Shibre T, Negash A, Kullgren G, Kebede D, Alem A, Fekadu A, et al. Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol. (2001) 36:299–303. doi: 10.1007/s001270170048
41. Tesfaw G, Kibru B, Ayano G. Prevalence and factors associated with higher levels of perceived stigma among people with schizophrenia Addis Ababa, Ethiopia. Int J Mental Health Syst. (2020) 14(1):19. doi: 10.1186/s13033-020-00348-9
42. Verhaeghe M, Bracke P. Organizational and individual level determinants of stigmatization in mental health services. Commun Ment Health J. (2007) 43:375–400. doi: 10.1007/s10597-007-9083-x
43. Caqueo-Urízar A, Gutiérrez-Maldonado J. Burden of care in families of patients with schizophrenia. Qual Life Res. (2006) 15:719–24. doi: 10.1007/s11136-005-4629-2
44. Catthoor K, Schrijvers D, Hutsebaut J, Feenstra D, Persoons P, De Hert M, et al. Associative stigma in family members of psychotic patients in Flanders: an exploratory study. World J Psychiatry. (2015) 5:118. doi: 10.5498/wjp.v5.i1.118
45. Grover S, Avasthi A, Singh A, Dan A, Neogi R, Kaur D, et al. Stigma experienced by caregivers of patients with severe mental disorders: a nationwide multicentric study. Int J Soc Psychiatry. (2017) 63:407–17. doi: 10.1177/0020764017709484
46. Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination faced by family caregivers of people with schizophrenia in India. Soc Sci Med. (2017) 178:66–77. doi: 10.1016/j.socscimed.2017.01.061
47. Chang S, Zhang Y, Jeyagurunathan A, Lau YW, Sagayadevan V, Chong SA, et al. Providing care to relatives with mental illness: reactions and distress among primary informal caregivers. BMC Psychiatry. (2016) 16:1–9. doi: 10.1186/s12888-016-0786-9
48. Shah AJ, Wadoo O, Latoo J. Psychological distress in carers of people with mental disorders. Br J Med Pract. (2010) 3:a327.
49. Prince MJ. The 10/66 dementia research group-10 years on. Indian J Psychiatry. (2009) 51(Suppl1):S8.
50. Bush EC. Gender differences in specific caregiver burdens. Utah: University of Utah College of Nursing (1997).
51. Magaña SM, Ramirez Garcia JI, Hernández MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: the roles of burden and stigma. Psychiatr Serv. (2007) 58:378–84. doi: 10.1176/ps.2007.58.3.378
52. Patel V, Araya R, De Lima M, Ludermir A, Todd C. Women, poverty and common mental disorders in four restructuring societies. Soc Sci Med. (1999) 49:1461–71. doi: 10.1016/S0277-9536(99)00208-7
53. Kazakova O, Thomas F, Zrazikova V. Impact of relative mental illness on caregivers. Eur Psychiatry. (2021) 64:S369–S70. doi: 10.1192/j.eurpsy.2021.990
54. Borgo ELP, de Abreu Ramos-Cerqueira AT, Torres AR. Burden and distress in caregivers of patients with panic disorder and agoraphobia. J Nerv Ment Dis. (2017) 205:23–30. doi: 10.1097/NMD.0000000000000614
55. Šprah L, Dernovšek MZ, Wahlbeck K, Haaramo P. Psychiatric readmissions and their association with physical comorbidity: a systematic literature review. BMC Psychiatry. (2017) 17:1–17. doi: 10.1186/s12888-016-1172-3
56. Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harv Rev Psychiatry. (2018) 26:175. doi: 10.1097/HRP.0000000000000162
57. Stein DJ, Aguilar-Gaxiola S, Alonso J, Bruffaerts R, De Jonge P, Liu Z, et al. Associations between mental disorders and subsequent onset of hypertension. Gen Hosp Psychiatry. (2014) 36:142–9. doi: 10.1016/j.genhosppsych.2013.11.002
58. Gili M, Comas A, García-García M, Monzón S, Antoni S-B, Roca M. Comorbidity between common mental disorders and chronic somatic diseases in primary care patients. Gen Hosp Psychiatry. (2010) 32:240–5. doi: 10.1016/j.genhosppsych.2010.01.013
59. Chien W-T, Yeung FK, Chan AH. Perceived stigma of patients with severe mental illness in Hong Kong: Relationships with patients' psychosocial conditions and attitudes of family caregivers and health professionals. Admin Policy Mental Health Mental Health Serv Res. (2014) 41:237–51. doi: 10.1007/s10488-012-0463-3
Keywords: magnitude, caregivers, associated factors, perceived stigma, common mental disorders
Citation: Nigussie K, Tesfaye D, Bete T and Asfaw H (2023) Perceived stigma, common mental disorders and associated factors among primary caregivers of adult patients with mental illness attending at public hospitals, Harari regional state, Eastern Ethiopia: A multicenter cross-sectional study. Front. Public Health 11:1024228. doi: 10.3389/fpubh.2023.1024228
Received: 21 August 2022; Accepted: 02 February 2023;
Published: 02 March 2023.
Edited by:
Renato de Filippis, Magna Græcia University, ItalyReviewed by:
Arif Jamie, Harar Health Science College (HHSC), EthiopiaCopyright © 2023 Nigussie, Tesfaye, Bete and Asfaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henock Asfaw, eWFyZWRzYWZ3MzNAZ21haWwuY29t; Kabtamu Nigussie, a2FidGFtdWFsaUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.