- 1Department of Geriatrics, Jinhua Fifth Hospital, Jinhua, China
- 2Department of Geriatrics, Zhejiang Hospital, Hangzhou, China
- 3Department of Neurology, Zhejiang Hospital, Hangzhou, China
Background: This study aimed at investigating the prevalence and factors of the discordant attitudes toward advance care planning (ACP) among older patients and their family members toward patients' engagement in ACP in the primary medical and healthcare institution.
Methods: In a cross-sectional study, a total of 117 older patients and 117 family members from Jinhua Fifth Hospital in China were enrolled. The questionnaire included sociodemographic characteristics, functional capacity assessment, and attitudes toward patients' engagement in ACP. Functional capacity assessment scales included the Modified Barthel Index (MBI), the Short-Form Mini-Nutritional Assessment (MNA-SF), the 15-item Geriatric Depression Scale (GDS-15), the Mini-Mental State Examination (MMSE), the Clinical Frailty Scale (CFS), and the SARC-F questionnaire.
Results: The discordance attitudes toward patients' engagement in ACP between patients and family members accounted for 41(35.0%). In the multivariate logistic analysis, factors associated with higher odds of discordance attitudes toward patients' engagement in ACP included greater age differences between patients and family members (OR = 1.043, 95% CI: 1.007–1.081), lower educational level for family members (OR = 3.373, 95% CI: 1.239–9.181), the patient's higher GDS-15 score (OR = 1.437, 95% CI: 1.185–1.742), and patient's higher MNA-SF score (OR = 1.754, 95% CI: 1.316–2.338).
Conclusion: Older patients and their family members had little ACP knowledge, and factors that influence discordance attitudes toward patients' engagement in ACP included the age gaps between patients and family members, family members' educational level, patients' depressive symptoms, and patients' nutritional status.
1. Introduction
The acceleration of population aging in China has brought more challenges to elderly care services, medical and social resources. And end-of-life care issues such as living wills and place of death have become a problem that cannot be ignored. In order to promote death with dignity, it is an urgent task to build a healthy China under the current aging situation. Therefore, the Healthy China 2030 Plan and other far-reaching reforms released by the Chinese Government have pointed out the necessity of palliative care and hospice care including the implementation of advance care planning (ACP). ACP refers to a process wherein individuals with clearly aware decision-making capacity reflect upon personal life experience and values to make their future care goals and treatment preferences in advance (1, 2). As an important concept of ACP, advance directives (ADs) are usually in a legal formal written document that nominates a substitute decision proxy and/or determined life-sustaining treatment through a living will (3). The implementation of ACP is associated with realizing medical autonomy (3), relieving stress, anxiety, and depression in family members (4), reducing over-utilization of aggressive measures during the end of life (5–7), cutting down Medicare costs (8), and decreasing in-hospital mortality (9, 10).
Research on ACP for older adults in China is still in the early stage, and only one city on the mainland currently has such relevant local legal regulations. Of cognitively normal Chinese older adults from 140 nursing homes in Hong Kong, 88% of older residents preferred having ADs regarding their future medical treatments (11). A multicenter cross-sectional study from 25 hospitals throughout mainland China included 91.1% of older patients aged over 60 years, and the results reported that 38.3% of patients had heard about ACP, and 50.6% were willing to carry out ACP when being informed about relevant knowledge of ACP (12). The study clarified attitudes and preferences toward ACP in a relatively Chinese large sample mostly in tertiary hospitals but did not involve the elderly population in the primary medical and health care institution and the influence of functional status on ACP attitudes. Prior research has compared attitudes toward ACP between patients and family members, which has focused on specific diseases such as cancer and heart failure (13, 14). Different from the other specialized wards with a certain specific disease, older patients in the geriatric wards in the primary medical and health care institution, may have advanced age, complex multimorbidity, multiple functional loss, and a higher proportion at the final stage of the disease. It may be more common to hide the true condition of the patients and make medical decisions on behalf of their family members. Prior studies have suggested that despite their family members understanding the patient's wishes regarding end-of-life care, frequent disagreement between them about treatment preferences and goals of care often arises (15). However, medical decisions that are in concordance with seriously ill patients' values and goals are regarded as high-quality care (16, 17). Discordance with the patient's values, goals, and medical treatments has been shown to increase medical costs and prolong end-of-life difficulties (17–19). Additionally, other factors including health status, family support, physical functioning, and experiences of family or relatives rescuing may affect their perceptions of ACP and end-of-life care.
Thus, this study aimed at investigating the attitudes and preferences of older patients and their family members toward patients' engagement in ACP in a primary medical and healthcare institution. Moreover, this study integrated factors such as the functional capacity to explore the associated factors on discordance attitudes toward ACP between patients and their family members.
2. Methods
2.1. Study design and setting
A cross-sectional study was carried out in the Department of Geriatrics in Jinhua Fifth Hospital between October 2020 and August 2021. Jinhua Fifth Hospital, the first filed public hospital for old-age care in Jinhua City, Zhejiang Province, mainly serves the elderly with disability and multiple comorbidities. The medical and old-age care integration model in the primary medical and health care institution refers to integrating medical care, rehabilitation, nursing, and life care, and is an effective means to improve the quality of old-age care.
2.2. Participants
One hundred seventeen patients and 117 family members from Jinhua Fifth Hospital were enrolled by convenience sampling. Patients' inclusion criteria: (a) Age ≥ 60 years; (b) Patients with clear consciousness who have no communication barriers; (c) Patients who can sign informed consent voluntarily and cooperate in completing the investigation. Patients' exclusion criteria: unable to cooperate to complete the ACP questionnaire because of consciousness disorder, severe cognitive impairment, and other critical conditions. Family members' inclusion criteria: family members of hospitalized patients who voluntarily participated and were able to cooperate in completing the study.
This study was approved by the Medical Ethics Committee of Jinhua Fifth Hospital (number: 2021-04), and written informed consent was obtained from the patients and their family members prior to the data collection.
2.3. Measurements
Both patients and family members completed the questionnaires about sociodemographic and ACP attitudes, and functional capacity assessment by comprehensive geriatric assessment (CGA) was only investigated by the patients. Patients and family members separately expressed their own perspectives on ACP through face-to-face interviews.
Sociodemographic data including age, sex, marital status (categorized by married, divorced, widow, or single), educational level (classified as high school or below), medical insurance, religion, the relationship between patients and caregivers, self-reported family support (coded as poor, fair, and good), self-reported health status (coded as poor, fair, and good), concurrent diseases (including coronary artery disease, hypertension, diabetes, cerebrovascular disease, respiratory disease, and osteoarticular diseases), and prescription medications were recorded.
The functional capacity assessment was conducted by CGA based on the Chinese expert consensus recommendation (20). In this study, the activity of daily living was assessed by the Modified Barthel Index (MBI), and the higher the MBI score indicated the better the activity of daily living (21). The Short-Form Mini-Nutritional Assessment (MNA-SF) was used to ascertain the degree of malnutrition risk (22). Depressive symptoms were evaluated using the 15-item Geriatric Depression Scale (GDS-15), with higher scores indicating more depressive symptoms (23). Cognitive function was assessed using the Mini-Mental State Examination (MMSE) (24). Higher MMSE score indicated better cognitive function. Frailty was detected by the Clinical Frailty Scale (CFS) which was scored from 1 (very fit) to 9 (severely frail) (25). Based on the clinical judgment, a higher CFS score was considered a higher degree of frailty. The SARC-F questionnaire was used to screen sarcopenia, with higher values indicating a greater likelihood of sarcopenia (26).
A structured questionnaire about ACP attitudes was completed independently by patients and their family members. The questionnaire included prior experience with relatives and friends being rescued (coded as yes or no), attitudes toward death (categorized by fear, avoid discussing, and accept discussing), ACP knowledge, determination surrogate, value statement about end-of-life (coded as active treatment, relieving uncomfortable symptoms, maintenance of daily function, and quality of life or unknown), preferences for end-of-life treatments (including cardiopulmonary resuscitation, invasive mechanical ventilation support, non-invasive ventilation support, renal replacement therapy, gastrointestinal colostomy, nasal tube, deep vein catheterization, urinary catheter, and transfusion), and desired place of death. Discordance attitudes were defined based on patients' and family members' responses to the question about whether to consider ACP engagement of patients if patients cannot make decisions due to a medical condition (such as coma).
2.4. Data collection process
Patients and their family members were informed of the aim and the detailed process of the study when they visited the Department of Geriatrics. After obtaining their informed consent, they were interviewed by a trained researcher and the data were analyzed by another researcher.
2.5. Sample size calculation
A sample size of 111 patients was calculated to detect a discordance rate (p) of 32% according to a previous study (27), assuming a type I error (α) of 0.05, a desired precision (d) was 0.05, and a two-sided test. N represents the estimated annual cases of 165 new elderly patients admitted to the geriatrics department of the primary medical and healthcare institution. A non-response rate was set as 5%, and 117 pairs of patients and family members were required. The formula is as follows:
2.6. Statistical analysis
Data were analyzed using SPSS 18.0 software (SPSS, Chicago, IL, USA). The frequency and distribution tested by the normality test for all variables were evaluated. The continuous variables included patients' age, family members' age, the age gap between patients and family members, and functional capacities. These variables were presented as median (interquartile range, IQR) because they were not normally distributed, and the Mann-Whitney U tests were used to compare the differences between groups. Theχ2 tests were used to estimate differences in other variables between groups, and dichotomous variables are expressed as numbers (percentages). Furthermore, a multivariate logistic regression model to estimate odds ratios (ORs) and 95% confidence intervals (CIs) was conducted to identify associated influencing variables with discordance attitudes toward ACP between older patients and their family members. The variables with P < 0.2 in bivariate analysis were selected in the multivariate logistic regression analysis. A P-value of < 0.05 was considered statistical significance.
3. Results
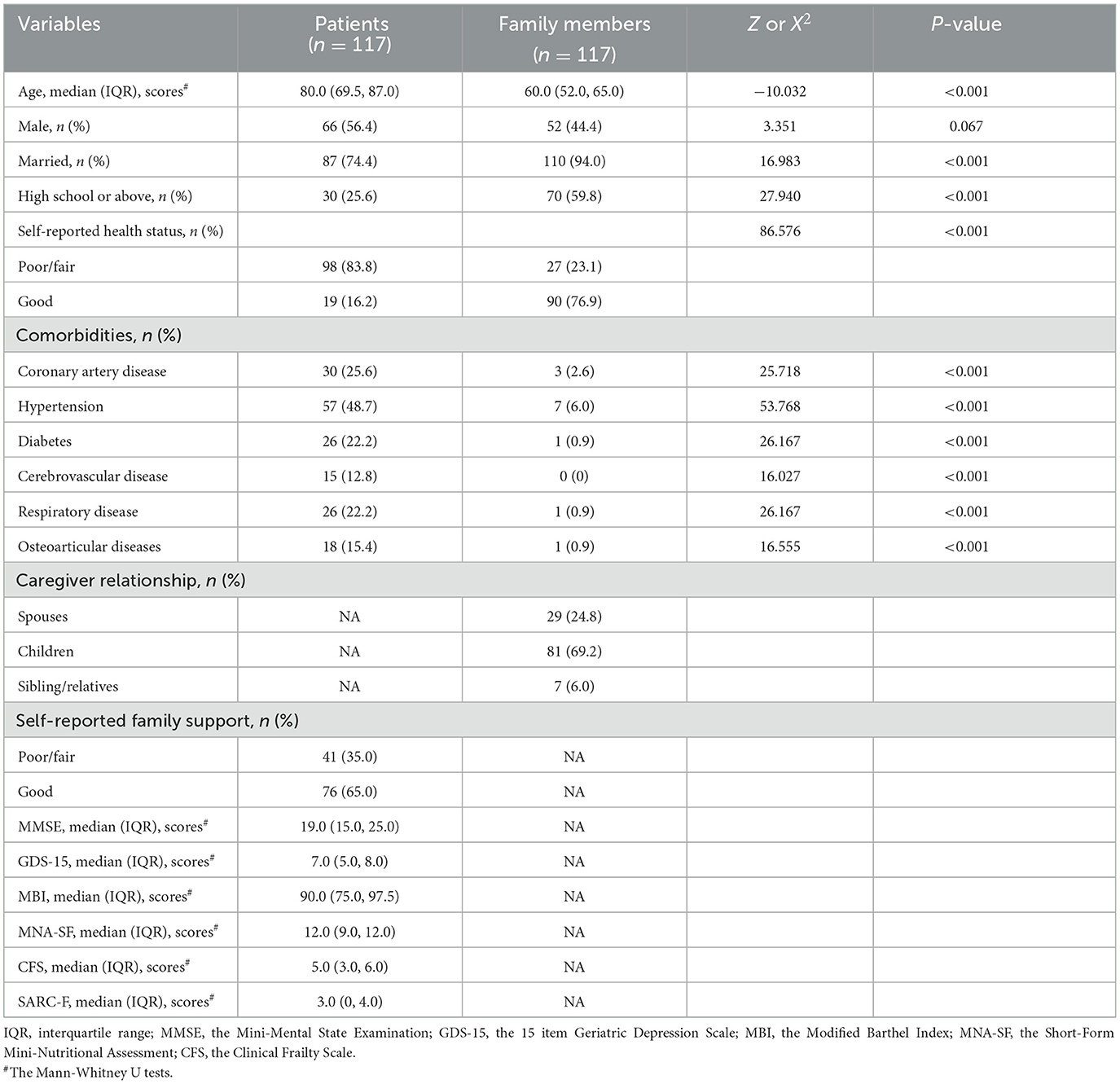
Table 1 presents the characteristics of 117 eligible pairs of patients and family members. Among patients, 66 (56.4%) were male, with a median age of 80 years. Among family members, 52 (44.4%) were males, with a median age of 60 years. Significant differences were found in age, marital status, educational level, self-reported health status, and comorbid diseases between patients and family members (all P < 0.05).
Table 2 displays the attitudes of older patients and their family members toward ACP and end-of-life treatments for the patients. About 84% of patients chose their children as their medical decision-making surrogates. Family members were more willing to actively discuss death with patients in order to cope with the subsequent irreversible final stage of life, but, in fact, family members preferred to choose active treatment for patients. In regards to the preferred place of death, there was no significance between patients and family members.
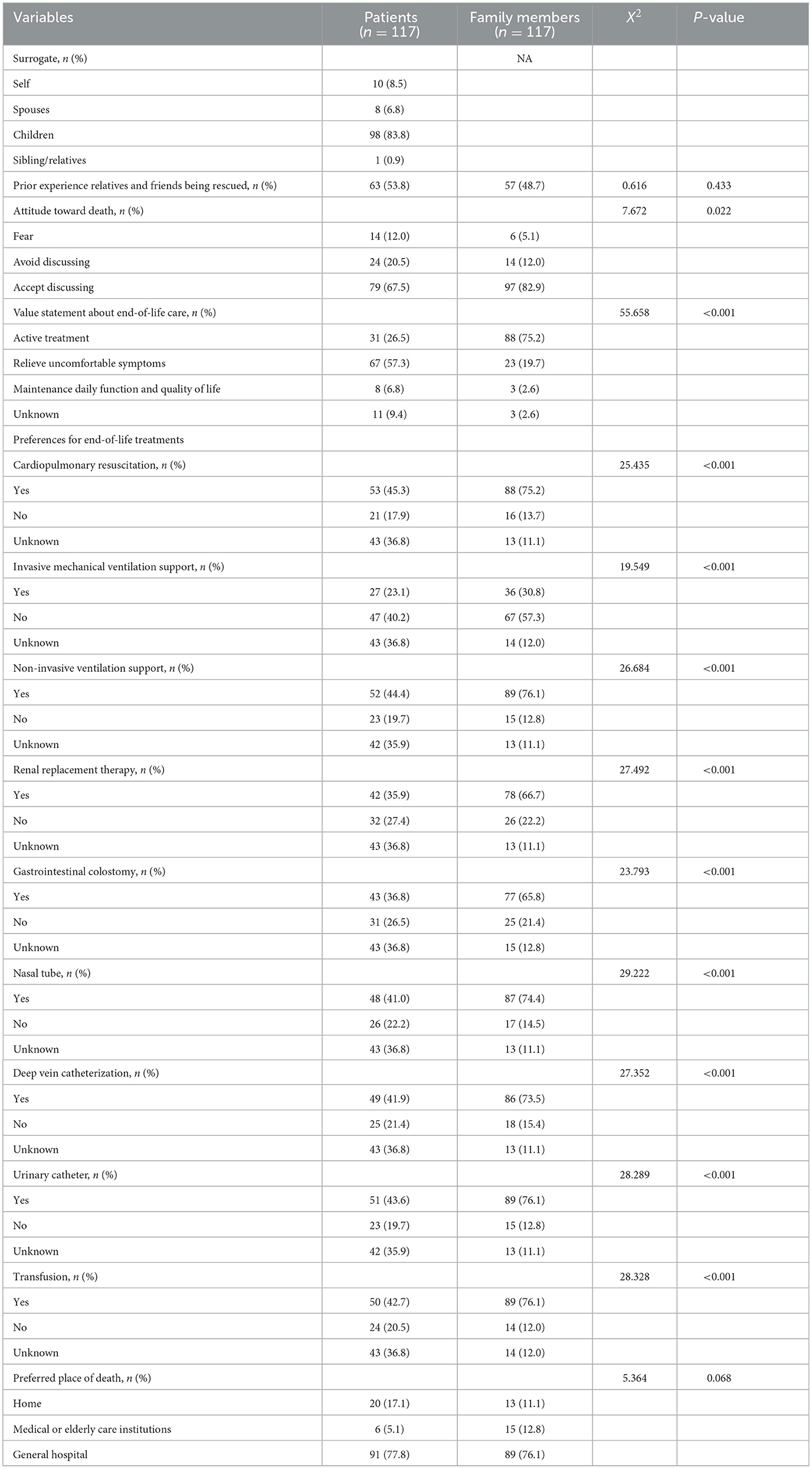
Table 2. Comparison of attitudes of older patients and their family members toward ACP and end-of-life treatments for the patients.
Only 4 patients (3.4%) and 14 family members (12.0%) heard of ACP. When the ACP was fully informed, the percentages of instituting ACP in the irreversible final stage of life increased to 51.3 and 78.6%, respectively. However, the discordant attitudes toward ACP between patients and family members accounted for 41 (35.0%). In the bivariate analysis, several patients' and family members' factors were associated with discordant attitudes toward ACP (Table 3). In the multivariate logistic analysis, factors associated with higher odds of discordance attitudes toward ACP included greater age differences between patients and family members (OR = 1.043, 95% CI: 1.007–1.081), higher GDS-15 score (OR = 1.437, 95% CI: 1.185–1.742), higher MNA-SF score (OR = 1.754, 95% CI: 1.316–2.338), and lower educational level for family members (OR = 3.373, 95% CI: 1.239–9.181) (Table 4).
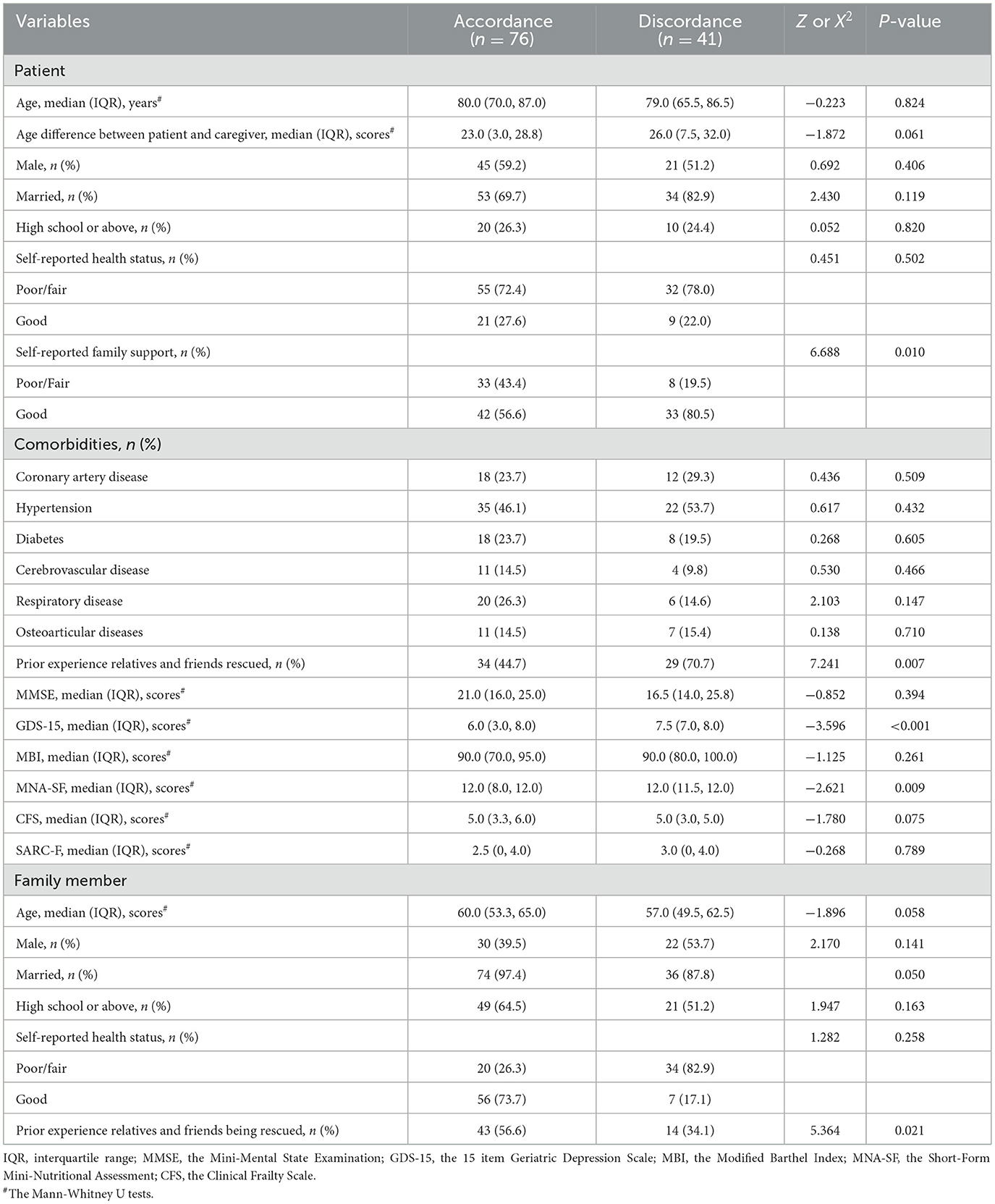
Table 3. The patient and family member factors associated with discordance attitudes toward ACP by bivariate analysis.
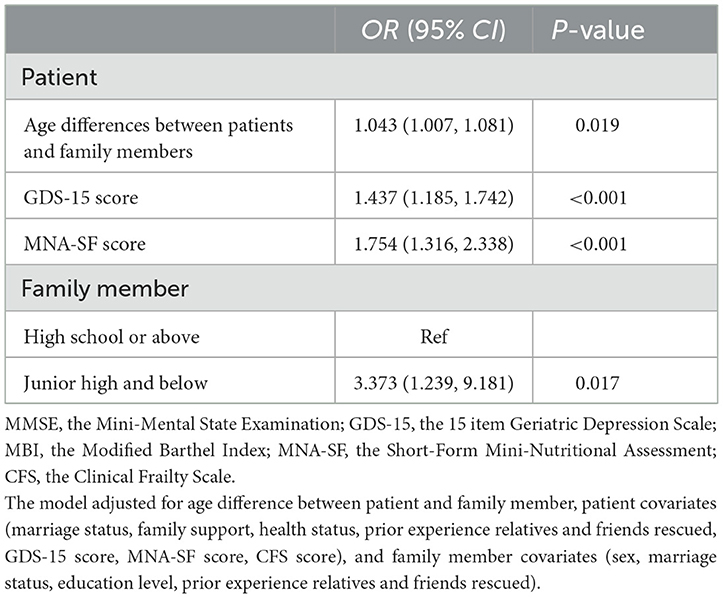
Table 4. The patient and family member factors associated with discordance attitudes toward ACP by multivariate logistic analysis.
4. Discussion
This study included older patients and their family members in the primary medical and healthcare institution, and identified that discordance attitudes toward patients' engagement in ACP between them were common, with the discordance rate accounting for ~35%. More specifically, most patients and their family members viewed general hospitals as the preferred location of death, but family members would choose more aggressive life-sustaining treatments for patients at the end of life than patients themselves. Indeed, multiple previous studies demonstrated poor patient-surrogate agreement about patients' end-of-life treatment preferences (15, 27, 28). One study showed that agreement between older persons and their surrogates regarding living will completion were 81%, while agreement about the other aspects of ACP including healthcare surrogates, attitudes toward life-sustaining treatments, and the quality and quantity of life was 62–68% (27). The low compliance of patients' end-of-life preferences may be attributed to the lack of ACP knowledge. The dissemination and implementation of ACP need to take into account cultural and ethical considerations (29, 30). It is well known that people in a Western culture attach great importance to patient autonomy and quality of life, partly because they have received death education since childhood, as well as the legislative power of patient autonomy and informed consent (31, 32). However, adult children in Chinese traditional culture often act on the patient's preferred surrogates for future medical decisions, they are endowed with important family responsibilities to make every effort to prolong their older patients' lives. And the collectivism of family and society is considered as having a higher value than patient autonomy in end-of-care decision-making, which prevents ACP discussion by families who are reluctant to inform patients of their true condition and discuss death (33). In addition, ethical conflicts about what is a reasonable decision for a patient end of life care often occur during ACP communication and the decision-making process (34, 35).
In addition to cultural and ethical considerations, our study found that discordance attitudes varied greatly with respect to age gaps between patients and family members, family members' educational level, patients' depressive symptoms, and patients' nutritional status. The smaller the age gap between the patient and his family member is, that is, they are both in advanced age, the easier the family members understand the patient's preference. On the contrary, the greater the age gap between the two, the younger family members may make decisions against the patient's will due to traditional culture, ethics, and other factors. There are no relevant studies to explore the association between the age gap and disagreement attitudes toward ACP activities between patients and their family members. Thus, the result of this study needs to be further warranted in a large sample study. Moreover, the awareness rates of ACP knowledge in both older patients and their family members in this study were obviously lower than the previously reported rates in tertiary general hospitals (12), and it may be supportive of the importance of promoting ACP education in the primary institutions. Except for ACP education, original educational level is known to influence individuals' attitudes toward ACP, and our study revealed that poorly educated family members were more prone to make decisions that were against the patients' end-of-life preferences than those with highly educated. In accordance with a recent study investigating factors influencing older married couples possessing an AD, the result clarified that older couples in which one or both spouses went to college were more prone to report AD concordance (36). Compared with poorly educated family members, highly educated family members may have more access to increase their knowledge and understanding of patients' wishes, and are more likely to joint communicate end-of-life treatment and care preferences with their elders, thus reducing the burden of making difficult end-of-life decisions on behalf of patients.
Functional capacity parameters, especially depressive symptoms and the nutritional status of patients were identified as important associated modifiable factors. Evidence showed that depression was associated with enhancing discussions about end-of-life care and declining cardiopulmonary resuscitation (37, 38), and a decrease in depressive symptoms, in turn, increased the likelihood of patients changing preferences from declining to desiring cardiopulmonary resuscitation (39). ACP discussion and intervention could facilitate alleviating anxiety and depressive symptoms of terminally ill patients and their surviving relatives, but neither improves the quality of life nor the end-of-life care decision-making process (4, 40). Fluctuations in patients' depressive symptoms and lack of communication may increase the possibility of inconsistent attitudes toward ACP. Furthermore, the patient's poor nutritional status was associated with an accordance attitude toward ACP. The observed association can be explained by the fact that older patients with malnutrition were accompanied by multiple comorbidities, reduced physical functioning, and dependence on activities of daily living (41). Poor physical condition and dependence synergistically make older patients a more self-perceived burden to their families (42). Older adults often have a perception that they do not want to burden others, including their families (43, 44). Moreover, prior studies of the perspective of the elderly on ACP have shown that ACP would ease the family burden (45). Hence, increasing family burdens seems to be an important factor in end-of-life decision-making for older adults. The discordant attitudes toward ACP between older patients and their family members were seen in older patients with good nutritional status in this context.
Studies have shown ACP focused more on improved concordance of care, particularly at the end of life, rather than improved clinical outcomes (46). Another study described the ACP process as part of chronic disease management (47). Based on these findings, the integration of ACP for older patients in the primary medical and health care institution into routine care may facilitate informed and shared decision-making in regard to complicated therapeutic options and palliative care that is in line with personal values and preferences. This study identified several modifiable and non-modifiable factors toward ACP discordance attitudes, which were important for good communication between older patients and their family members. It is suggested that clinicians need to pay close attention to the potentially vulnerable groups with discordant attitudes, and patient-family-clinician shared decision-making about end-of-life preferences should be adopted to achieve the goal of honoring patients' values, preferences, and wishes. In addition to ACP education, the ACP-related laws and regulations, and the robust healthcare system need to be supported at the national level in order to implement ACP smoothly.
However, this study also has some limitations. Firstly, this study recorded older patients and their family members' perceived attitudes toward future ACP engagement of patients, rather than actual discordance in medical care and treatments received. Attitudes toward end-of-life preferences would change during hospitalization for some patients and their family members, due to various reasons. Secondly, this study did not explore physician preferences for the patient's care goals and treatments. Thirdly, this study was conducted in a single institution with a relatively small sample, and the data were collected at one point in time. Thus, the findings were of limited generality, and no causality could be assumed. Fourth, the lack of collection of response rates and characteristics of non-responders may result in biased prevalence estimates and selection bias, and the results should be interpreted with caution.
5. Conclusion
This study indicated that older patients and their family members had little ACP knowledge, and factors that influence discordance attitudes toward patients' engagement in ACP included age gaps between patients and family members, family members' educational level, patients' depressive symptoms, and patients' nutritional status. Early ACP education for older patients and their family members may promote ACP communications, and thus facilitate patient-family-clinician shared decision-making in the primary medical and healthcare institution, which eventually achieves the goal of honoring patients' values, preferences, and wishes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Jinhua Fifth Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SS and SQ contributed to the conceptualization and methodology. LY and SS analyzed the data and wrote the original draft. LY, GJ, MC, and XX contributed to data collection. All authors contributed to implementing and revising the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Jinhua Science and Technology Project (2021-4-106), and the 1530 and 3060 personnel training projects from Zhejiang Hospital (2018-30-09 and 20203004).
Acknowledgments
We would like to acknowledge the staff from the Geriatric Department of Jinhua Fifth Hospital for their positive involvement in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. (2014) 28:1000–25. doi: 10.1177/0269216314526272
2. Rietjens JAC, Sudore RL, Connolly M, van Delden JJ, Drickamer MA, Droger M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. (2017) 18:e543–e51. doi: 10.1016/S1470-2045(17)30582-X
3. Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. (2010) 362:1211–8. doi: 10.1056/NEJMsa0907901
4. Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. (2010) 340:c1345. doi: 10.1136/bmj.c1345
5. Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. (2010) 153:256–61. doi: 10.7326/0003-4819-153-4-201008170-00008
6. Becker C, Lecheler L, Hochstrasser S, Metzger KA, Widmer M, Thommen EB, et al. Association of communication interventions to discuss code status with patient decisions for do-not-resuscitate orders: a systematic review and meta-analysis. JAMA Netw Open. (2019) 2:e195033. doi: 10.1001/jamanetworkopen.2019.5033
7. Guidelines for the appropriate use of do-not-resuscitate orders. Council on Ethical and Judicial Affairs, American Medical Association. JAMA. (1991) 265:1868–71. doi: 10.1001/jama.265.14.1868
8. Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. (2011) 306:1447–53. doi: 10.1001/jama.2011.1410
9. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am. (2015) 99:391–403. doi: 10.1016/j.mcna.2014.11.010
10. Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. (2013) 61:209–14. doi: 10.1111/jgs.12105
11. Chu LW, Luk JK, Hui E, Chiu PK, Chan CS, Kwan F, et al. Advance directive and end-of-life care preferences among Chinese nursing home residents in Hong Kong. J Am Med Dir Assoc. (2011) 12:143–52. doi: 10.1016/j.jamda.2010.08.015
12. Kang L, Liu XH, Zhang J, Shan PY, Wang JP, Zhong P, et al. Attitudes toward advance directives among patients and their family members in China. J Am Med Dir Assoc. (2017) 18:808.e7–e11. doi: 10.1016/j.jamda.2017.05.014
13. Feng C, Wu J, Li J, Deng HY, Liu J, Zhao S. Advance directives of lung cancer patients and caregivers in China: a cross sectional survey. Thorac Cancer. (2020) 11:253–63. doi: 10.1111/1759-7714.13237
14. Kim J, Shin MS, Park YM, Lee HN, Heo S, Ounpraseuth S. Associations of advance directive knowledge, attitudes, and barriers/benefits with preferences for advance treatment directives among patients with heart failure and their caregivers. J Card Fail. (2020) 26:61–9. doi: 10.1016/j.cardfail.2019.07.011
15. Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. (2006) 166:493–7. doi: 10.1001/archinte.166.5.493
16. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient's primary recovery goal for hospitalization? J Hosp Med. (2016) 11:615–9. doi: 10.1002/jhm.2569
17. Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. (2000) 284:2476–82. doi: 10.1001/jama.284.19.2476
18. Oo NM, Scott IA, Maggacis R, Rajakaruna N. Assessing concordance between patient preferences in advance care plans and in-hospital care. Aust Health Rev. (2019) 43:425–31. doi: 10.1071/AH18011
19. Unroe KT, Hickman SE, Torke AM, Group ARCW. Care consistency with documented care preferences: methodologic considerations for implementing the “measuring what matters” quality indicator. J Pain Symptom Manage. (2016) 52:453–8. doi: 10.1016/j.jpainsymman.2016.04.015
20. Chen X, Yan J, Wang J, Yu P, Geriatric GBoCMA. Chinese expert consensus on the application of comprehensive geriatric assessment for the elderly. Aging Med. (2018) 1:100–5. doi: 10.1002/agm2.12019
21. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. (1965) 14:61–5. doi: 10.1037/t02366-000
22. Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the mini nutritional assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. (2009) 13:782–8. doi: 10.1007/s12603-009-0214-7
23. Dennis M, Kadri A, Coffey J. Depression in older people in the general hospital: a systematic review of screening instruments. Age Ageing. (2012) 41:148–54. doi: 10.1093/ageing/afr169
24. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
25. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. (2005) 173:489–95. doi: 10.1503/cmaj.050051
26. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. (2016) 7:28–36. doi: 10.1002/jcsm.12048
27. Fried TR, Redding CA, Robbins ML, O'Leary JR, Iannone L. Agreement between older persons and their surrogate decision-makers regarding participation in advance care planning. J Am Geriatr Soc. (2011) 59:1105–9. doi: 10.1111/j.1532-5415.2011.03412.x
28. Pruchno RA, Lemay EP Jr, Feild L, Levinsky NG. Predictors of patient treatment preferences and spouse substituted judgments: the case of dialysis continuation. Med Decis Making. (2006) 26:112–21. doi: 10.1177/0272989X06286482
29. Master JF, Wu B, Ni P, Mao J. The compliance of end-of-life care preferences among older adults and its facilitators and barriers: a scoping review. J Am Med Dir Assoc. (2021) 22:2273–80.e2. doi: 10.1016/j.jamda.2021.05.007
30. Deng RL, Duan JZ, Zhang JH, Miao JR, Chen LL, Lee DT. Advance care planning for frail older people in China: a discussion paper. Nurs Ethics. (2019) 26:1696–706. doi: 10.1177/0969733018779177
31. Tanaka M, Kodama S, Lee I, Huxtable R, Chung Y. Forgoing life-sustaining treatment - a comparative analysis of regulations in Japan, Korea, Taiwan, and England. BMC Med Ethics. (2020) 21:99. doi: 10.1186/s12910-020-00535-w
32. Wiesing U, Jox RJ, Hessler HJ, Borasio GD. A new law on advance directives in Germany. J Med Ethics. (2010) 36:779–83. doi: 10.1136/jme.2010.036376
33. Ip M, Gilligan T, Koenig B, Raffin TA. Ethical decision-making in critical care in Hong Kong. Crit Care Med. (1998) 26:447–51. doi: 10.1097/00003246-199803000-00013
34. Poveda-Moral S, Rodriguez-Martin D, Codern-Bove N, Jose-Maria P, Sanchez-Valero P, Pomares-Quintana N, et al. Managing ethical aspects of advance directives in emergency care services. Nurs Ethics. (2021) 28:91–105. doi: 10.1177/0969733020952112
35. Mueller PS, Hook CC, Fleming KC. Ethical issues in geriatrics: a guide for clinicians. Mayo Clin Proc. (2004) 79:554–62. doi: 10.4065/79.4.554
36. Koss CS, Jensen D. Going it alone: advance directive discordance in older married couples. J Appl Gerontol. (2020) 39:1274–83. doi: 10.1177/0733464819884439
37. Fakhri S, Engelberg RA, Downey L, Nielsen EL, Paul S, Lahdya AZ, et al. Factors affecting patients' preferences for and actual discussions about end-of-life care. J Pain Symptom Manage. (2016) 52:386–94. doi: 10.1016/j.jpainsymman.2016.03.012
38. Stapleton RD, Nielsen EL, Engelberg RA, Patrick DL, Curtis JR. Association of depression and life-sustaining treatment preferences in patients with COPD. Chest. (2005) 127:328–34. doi: 10.1378/chest.127.1.328
39. Rosenfeld KE, Wenger NS, Phillips RS, Connors AF, Dawson NV, Layde P, et al. Factors associated with change in resuscitation preference of seriously ill patients. The SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Arch Intern Med. (1996) 156:1558–64. doi: 10.1001/archinte.1996.00440130104011
40. Tang ST, Chen JS, Wen FH, Chou WC, Chang JW, Hsieh CH, et al. Advance care planning improves psychological symptoms but not quality of life and preferred end-of-life care of patients with cancer. J Natl Compr Canc Netw. (2019) 17:311–20. doi: 10.6004/jnccn.2018.7106
41. Cereda E, Pedrolli C, Klersy C, Bonardi C, Quarleri L, Cappello S, et al. Nutritional status in older persons according to healthcare setting: a systematic review and meta-analysis of prevalence data using MNA((R)). Clin Nutr. (2016) 35:1282–90. doi: 10.1016/j.clnu.2016.03.008
42. Akazawa T, Akechi T, Morita T, Miyashita M, Sato K, Tsuneto S, et al. Self-perceived burden in terminally ill cancer patients: a categorization of care strategies based on bereaved family members' perspectives. J Pain Symptom Manage. (2010) 40:224–34. doi: 10.1016/j.jpainsymman.2009.12.015
43. Rehmann-Sutter C. Self-perceived burden to others as a moral emotion in wishes to die. A conceptual analysis. Bioethics. (2019) 33:439–47. doi: 10.1111/bioe.12603
44. Gudat H, Ohnsorge K, Streeck N, Rehmann-Sutter C. How palliative care patients' feelings of being a burden to others can motivate a wish to die. Moral challenges in clinics and families. Bioethics. (2019) 33:421–30. doi: 10.1111/bioe.12590
45. McPherson CJ, Wilson KG, Murray MA. Feeling like a burden to others: a systematic review focusing on the end of life. Palliat Med. (2007) 21:115–28. doi: 10.1177/0269216307076345
46. Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho AHY. Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manage. (2018) 56:436–59.e25. doi: 10.1016/j.jpainsymman.2018.05.016
Keywords: advance care planning, attitudes, older adults, geriatric assessment, advance directives
Citation: Ye L, Jin G, Chen M, Xie X, Shen S and Qiao S (2023) Prevalence and factors of discordance attitudes toward advance care planning between older patients and their family members in the primary medical and healthcare institution. Front. Public Health 11:1013719. doi: 10.3389/fpubh.2023.1013719
Received: 07 August 2022; Accepted: 06 February 2023;
Published: 23 February 2023.
Edited by:
Enno Nowossadeck, Robert Koch Institute (RKI), GermanyReviewed by:
Silke Tophoven, University of Applied Sciences Düsseldorf, GermanySunita Ghosh, University of Alberta, Canada
Copyright © 2023 Ye, Jin, Chen, Xie, Shen and Qiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shanshan Shen,  c2hlbnNoYW4zMDUmI3gwMDA0MDsxNjMuY29t; Song Qiao,
c2hlbnNoYW4zMDUmI3gwMDA0MDsxNjMuY29t; Song Qiao,  cWlhb3NvbmdpY3UmI3gwMDA0MDsxNjMuY29t
cWlhb3NvbmdpY3UmI3gwMDA0MDsxNjMuY29t
 Ling Ye1
Ling Ye1 Shanshan Shen
Shanshan Shen Song Qiao
Song Qiao