Abstract
Background:
Vulnerability to health-related poverty can predict the probability of families falling into poverty due to health risk impact. In this study, we measured the vulnerability to health-related poverty and examined the mediation path of physical multimorbidity on the vulnerability to health-related poverty of rural aging families in Ningxia, China.
Methods:
This cross-sectional study was conducted in Ningxia, China, in February 2019. A multi-stage stratified cluster-randomized design was used to obtain a representative sample in each county. We included participants aged 60 years and older, who had lived there for more than 1 year. A total of 3,653 rural residents older than 60 years old were selected as the research subjects. The three-stage generalized least square method was used to calculate the expected vulnerability to poverty. We used mediating effect model to test the mediation path of poverty vulnerability related to the physical multimorbidity.
Results:
Under different poverty line standards, i.e., $1.9/day as low vs. $3.1/day as the high poverty line, the proportion of families that could fall into poverty in the future was 5.3 and 53.7%, respectively. The prevalence of chronic diseases and physical multimorbidity among rural residents >60 years old was 64.62 and 21.24%, respectively. The results of mediating effect test showed that self-rated health status (indirect effect a × b = −0.0052), non-agricultural employment (a × b= −0.0046), household cattle production (a × b = 0.0004), housing type (a × b = −0.0008), gift expenses (a × b = 0.0006) and loan for illness (a × b = 0.0034) were the mediation paths of poverty vulnerability related to the physical multimorbidity.
Conclusions:
Concerted efforts are needed to reduce poverty vulnerability related to the physical multimorbidity. The strategy of alleviating poverty should emphasis on promoting non-agricultural employment of vulnerable groups sustainability and developing rural economy, which are important paths to reduce family's vulnerability to health-related poverty.
Background
In 2013, China proposed the concept of “targeted poverty alleviation,” where poverty caused by health problems was the primary factor (1). The state launched a series of Health Poverty Alleviation Policies, including signing management services for chronic diseases, paying attention to chronic disease prevention and control, and similar (1). It has been found that health-related poverty alleviation had an important role in overall poverty reduction, as in 2020, China completely eliminated absolute poverty (2). However, the problem of relative poverty still remains.
It has been estimated that nearly five million people might be at risk of returning to poverty during the 14th Five Year Plan period (3). The strategic plan for Rural Revitalization also proposes to further alleviate relative poverty by 2035 (4), as unstable poverty relief households and Marginal Poverty households could easily return to poverty again. In fact, different strategies are needed to safeguard this vulnerable groups (5). Focusing on safeguarding relatively poor people from encountering illness-induced poverty are of great significance for consolidation of the achievements of healthy poverty alleviation (6). In July 2017, Ningxia began to promote the alleviation of health-related poverty and implemented a comprehensive health poverty alleviation security policy for patients who become impoverished due to illness and who returned to poverty due to illness (7). According to available data, poverty induced by health problems accounted for 42% nationwide (8). A cluster sampling survey conducted in poor villages in Ningxia showed that 41.5% of the poverty cases were caused by diseases, which become the primary factor for rural families to return to poverty (9). In Guyuan, Ningxia, the patients with chronic diseases accounted for 60.59% of the total number of patients (10).
The economic burden of chronic diseases is an important part of health-related poverty (11). According to the World Health Organization, about 33% of the total disease burden among the elderly aged ≥60 years old in China is attributed to chronic diseases (12). The increasing prevalence of chronic diseases in the elderly and the decline of their ability to work do not only reduce the health capital and labor participation rate (13), but also significantly increase the medical expenditure of aging families (14). It has been estimated that by 2050, the population aging level will reach 30%, the elderly population will exceed 400 million, and the prevalence of chronic diseases among the elderly ≥60 years over in China will reach 75.8% (15). Physical multimorbidity (suffering from two or more chronic diseases at the same time) causes high economic costs to individuals and families, and more than one-third of the elderly are chronically illed (16, 17). Suffering from a variety of chronic diseases is significantly related to the increase of catastrophic medical expenditure (18). The high prevalence of chronic diseases and the burden of chronic diseases among the elderly have increased the probability of aging families returning to poverty due to illness, which has become the focus of a series of social policies such as “Healthy China” and “Population aging” (19). Vulnerability to health-related poverty is a prediction of the probability that families might encounter poverty in the future due to health-related issues. These individuals and groups usually share certain social and economic factors that increase their vulnerability to poverty. The vulnerability to health-related poverty can be used as a risk factor or early warning signal of returning to poverty due to illness.
According to previous studies, people living in Western rural areas of China, aging families, those with chronic diseases, and especially people prone to chronic diseases are at high risk of health-related poverty (20–23). The existing literature mainly explored the influencing factors of vulnerability to health-related poverty from the perspective of unexpected health risk (24–27), family resource endowments (28–34), risk response strategies (35–38), and health support system (39). Family resource endowment is the capital on which families depend for survival, including human capital, material capital, and social capital (40). Human capital is divided into education, health, and professional human capital. Previous studies have found that the role of educational human capital in reducing poverty vulnerability is the largest among human capital, which is of great significance for the long-term development of rural residents (4–49). Physical capital can also affect the impact of health risks. The occurrence of chronic diseases is often closely related to public health infrastructure (32). Previous studies have found that public health infrastructure such as clean drinking water and flushing toilets can improve residents' health to a certain extent (50–52).
At present, studies about mediation path of poverty vulnerability related to physical multimorbidity are limited. It is necessary to study the intensity and mode of mediation path. In this study, we measured the vulnerability to health-related poverty among aging families living in rural Western China, examined the net effect of physical multimorbidity on health-related poverty among aging families, and mediation path of vulnerability to poverty related to physical multimorbidity.
Methods
Data sources
A total of 5,643 rural residents from 171 villages in four counties of Ningxia, Western China, were surveyed in 2019. The investigation method involved multistage stratified random sampling. All administrative villages in each township of the four sample counties were divided into three levels according to the level of economic development, i.e., high, medium, and low. By using the random number table method, 40% of villages were selected as the sample villages, and 33 rural residents were systematically sampled as the survey samples. The survey method was a face-to-face inquiry survey. The survey subjects were all family members of the sample households. The subjects were rural residents aged >60 years old. People who met the following conditions were selected from the database for inclusion in the study: (1) permanent rural residents who have lived for more than 1 year in the area; (2) elderly ≥60 years old. Finally, 3,653 rural elderly were included in the study. Physical multimorbidity refers to the population with two or more chronic diseases previously diagnosed by doctors. The sample size calculation formula of counting data in descriptive research is , The significance test level α = 0.05 is usually adopted, and the allowable error δ = 0.1π is general. The prevalence of chronic diseases among the elderly in China in 2018 was 59.1% (53), means π = 59.1%, The required sample size is calculated to be 267, The subjects included in this study meet the requirements of sample size.
Model and variables
Explained variable (Y): The vulnerability to health-related poverty
Vulnerability to health-related poverty predicts the probability that families will fall into poverty in the future due to unexpected health issues. The most common measurement method is expected poverty vulnerability (VEP) (41), which mainly uses three-stage feasible generalized least squares (FGLS) to quantify the family's vulnerability to health-related poverty in three following steps:
First, Ordinary Least Square (OLS) is used to estimate the income equation:
where
Y it+1 refers to the income level of the rural population in the T+1 period, XM refers to a series of observable variables that affect the family income level, including family demographic characteristics, health risk variables, family resource endowment variables, risk response strategies, and health support system variables. Considering the heterogeneity of rural population in different counties, townships, and villages, the residual square is regarded as the approximate value of income variance , and the residual square is used as the explained variable to construct the regression model of residual square to individual characteristics:
The estimated value and residual estimated value of Yit+1 can be obtained through formulas (1) and (2).
Second, heteroscedasticity structure is constructed as a weight for weighted regression, and the expected value (3) and variance (4) of future income logarithm are estimated:
Finally, the poverty line is selected to estimate the vulnerability to poverty. This study used the international poverty line of $1.9/day and $3.1/day (34) as the poverty lines for measuring the vulnerability to poverty. The value of health poverty vulnerability was distributed between zero and one. Those who scored ≥0.5 were categorized as families highly vulnerable to poverty and those <0.5 as families with vulnerability to poverty (42, 43). The research subjects were aging rural families, so the lognormal distribution was more applicable. The logarithm of the poverty lineInlis in formula (5):
Tobit model identifies health poverty vulnerability risk factors:
The value of vulnerability to health-related poverty is a limited continuous dependent variable. Therefore, the Tobit model was selected to screen the significant influencing factors of vulnerability to poverty. The measured value of vulnerability to poverty was taken as the dependent variable (V), and family demographic characteristics, health risk impact, family resource endowment, family risk response strategy and health support system are taken as the explanatory variable (Xj).
Explanatory variable (X): Physical multimorbidity
Physical multimorbidity (suffering from two or more chronic diseases at the same time), The indicators of physical multimorbidity were obtained through the following questions in the questionnaire: “did you have a chronic disease diagnosed by a doctor in the past?”, “if so, what are the diseases, and fill in the names of the three most serious diseases.” We counted the number of chronic diseases in each participant to identify people who with physical multimorbidity.
Taking the elderly with physical multimorbidity as the treatment group and the elderly without physical multimorbidity as the control group, the propensity score matching method was used to match the two groups of Control Variables in order to maximize the control of confounding factors and data bias. First, the propensity scores of the treatment group and the control group were estimated. The logit model was used to calculate the tendency score, as follows:
Second, a balance test and common support test were performed. A balance test was used to test whether there was a significant difference in each covariate between the matched treatment group and the control group and whether there was a significant difference in the joint distribution of covariates before and after matching. A common support test was used to ensure that propensity scores overlapped more between the treatment group and the control group (44). Finally, the “average treatment on the treated (ATT)” was obtained, i.e., the net effect of physical multimorbidity on poverty vulnerability.
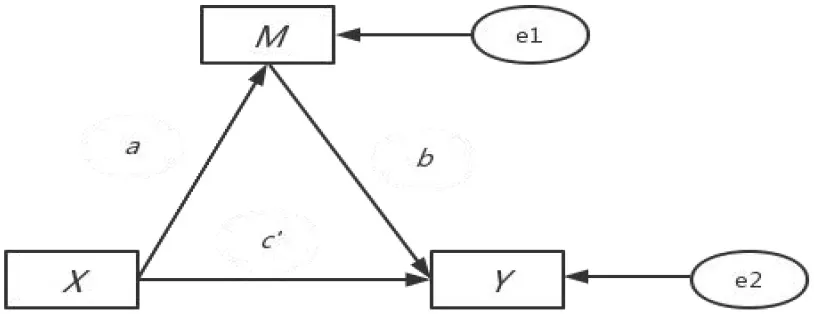
Mediating variable (M): Mechanism test of mediating effect model
The family's vulnerability to health-related poverty was used as the explanatory variable (Y), Physical multimorbidity as the explanatory variable (X), and human capital (Education level, The average length of education of family, Self-rating health, Non-agricultural workers), material capital (Household livestock ownership, Housing type, Type of drinking water, Toilet type, Separation of housing and kitchen) and social capital (Gift expenses) in resource endowment as the intermediary variable (M1) to test the possible path of family resource endowment in alleviating the impact of health risk on family's vulnerability to poverty. Taking the low insured households and medical assistance of risk response strategy as intermediary variables (M2), this study tested the role path of risk response strategy in alleviating health impact. Taking the transit time and chronic disease diagnosis and treatment institutions in the health support system as intermediary variables (M3), we tested their role in alleviating the health impact (Table 1).
Table 1
| Variables | Explanation | Code | |
|---|---|---|---|
| Explained variable (Y) | Health poverty vulnerability | Measure with expected poverty vulnerability (VEP) | |
| Explanatory variable (X) | Physical multimorbidity | 1 = treatment group, 2 = control group | |
| Control variable (C) | Gender | 1 = male, 2 = female | |
| Age | continuous variable | ||
| Marital status | 1 = unmarried, 2 = married, 3 = divorced, 4 = widowed, 5 = other | ||
| Family size | Household population | ||
| Number of the labor force | The family working-age population, 15–64 years old | ||
| Dependency ratio | 1–labor force / family size | ||
| Resource endowment (M1) | Human capital | Education level | 1 = no schooling, 2 = primary school, 3 = junior high school, 4 = senior high school or above |
| The average length of education of family(year) | No schooling = 0, primary school = 6, junior middle school = 9, senior high school and above = 12 | ||
| Self-rating health | 1 = very good, 2 = good, 3 = average, 4 = poor, 5 = very poor | ||
| Non-agricultural workers | 1 = yes, 2 = no | ||
| Material capital | Household livestock ownership (cattle) | continuous variable | |
| Housing type | 1 = brick soil concrete, 2 = brick wood, 3 = Civil Engineering, 4 = full brick, 5 = cave | ||
| Type of drinking water | 1 = tap water, 2 = mountain spring water, 3 = hand press well water, 4 = cellar water, 5 = well water, 6 = River and lake water, 7 = pond and ditch water | ||
| Toilet type | 1 = water flushing type, 2 = biogas, 3 = Double urn funnel type, 4 = deep pit, 5 = toilet, 6 = dry toilet, 7 = no toilet | ||
| Separation of housing and kitchen | 1 = yes, 2 = no | ||
| Social capital | Gift expenses(log) | Continuous variable (logarithm) | |
| Risk response strategy (M2) | Informal | Income from migrant workers | Continuous variable (logarithm) |
| loans because of illness | 1 = yes, 2 = no | ||
| Regular | Low-income households | 1 = yes, 2 = no | |
| Medical assistance | 1 = yes, 2 = no | ||
| Health support system (M3) | Health service accessibility | Physical accessibility | 1≤30 min, 2 = 30–60 min, 3 = 60–90 min, 4 = >90 min |
| Availability of health services | Chronic disease diagnosis and treatment institutions | 1 = village clinics, 2 = township hospitals, 3 = county hospitals, 4 = private clinics, 5 = others | |
Variable definition.
The intermediary effect model can analyze the process and mechanism of the influence between variables. When studying the influence of explanatory variable X (Physical multimorbidity) on the explained variable Y (The vulnerability to health-related poverty), Physical multimorbidity not only has a direct impact on the vulnerability to health-related poverty, but also an indirect impact on the vulnerability to health-related poverty through variable M (Mediating variable); thus, M can be called the intermediary variable, and the model X → M → Y reflecting the relationship between the three is called the intermediary effect model (45, 46). The mediating effect can be expressed as the product of coefficient b and coefficient a × b. This product term indicates how much of the effect of X on Y reaches Y through M. The independent variable of this study was category variable, so we used regression analysis to conduct intermediary analysis according to the stepwise method (54).
Control variable (C)
Gender, age, marital status, family size, labor force, and dependency ratio were used as control variables in family demographic characteristics (Table 1).
Results
Description of vulnerability to poverty among aging rural families
The vulnerability to poverty of aging rural elderly families calculated with the international poverty line of $1.9/day was 0.498 ± 0.001, and the proportion of vulnerable (VEP1) families was 5.3%. The vulnerability to poverty value of aging rural families calculated with the international poverty line of $3.1/day was 0.5 ± 0.001, and the proportion of vulnerable (VEP2) families was 53.7% (Table 2; Figure 1). Taking Poverty vulnerability value (3.1$) as the explanatory variable, family size, the number of the family labor force, dependency ratio, the toilet type in material capital and housing are separated from the kitchen, the logarithm of gift expenditure in social capital, the income of migrant workers in risk response strategy, loans due to illness, low-income households, the level of chronic disease diagnosis and treatment institutions providing medical assistance and health support system all resulted as the factors affecting vulnerability to poverty. The level of chronic disease diagnosis and treatment institutions providing the medical assistance and health support system resulted as factors affecting vulnerability to poverty (Table 3).
Table 2
| Variable | Observation | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Poverty vulnerability value1 () | 3,653 | 0.498 | 0.001 | 0.496 | 0.511 |
| Poverty vulnerability value2 () | 3,653 | 0.500 | 0.001 | 0.497 | 0.516 |
| VEP1* (%) | 3,653 | 0.053 | 0.225 | 0 | 1 |
| VEP2 (%) | 3,653 | 0.537 | 0.499 | 0 | 1 |
| poverty line1 (1.9$) (ln) | 3,653 | 8.390 | 0.000 | 8.390 | 8.390 |
| poverty line2 (3.1$) (ln) | 3,653 | 8.880 | 0.000 | 8.880 | 8.880 |
Description of basic family situation and vulnerability to poverty.
VEP1, the proportion of expected vulnerability to poverty calculated with the international poverty line of $1.9/day.
VEP2, the proportion of expected vulnerability to poverty calculated with the international poverty line of $3.1/day.
Figure 1
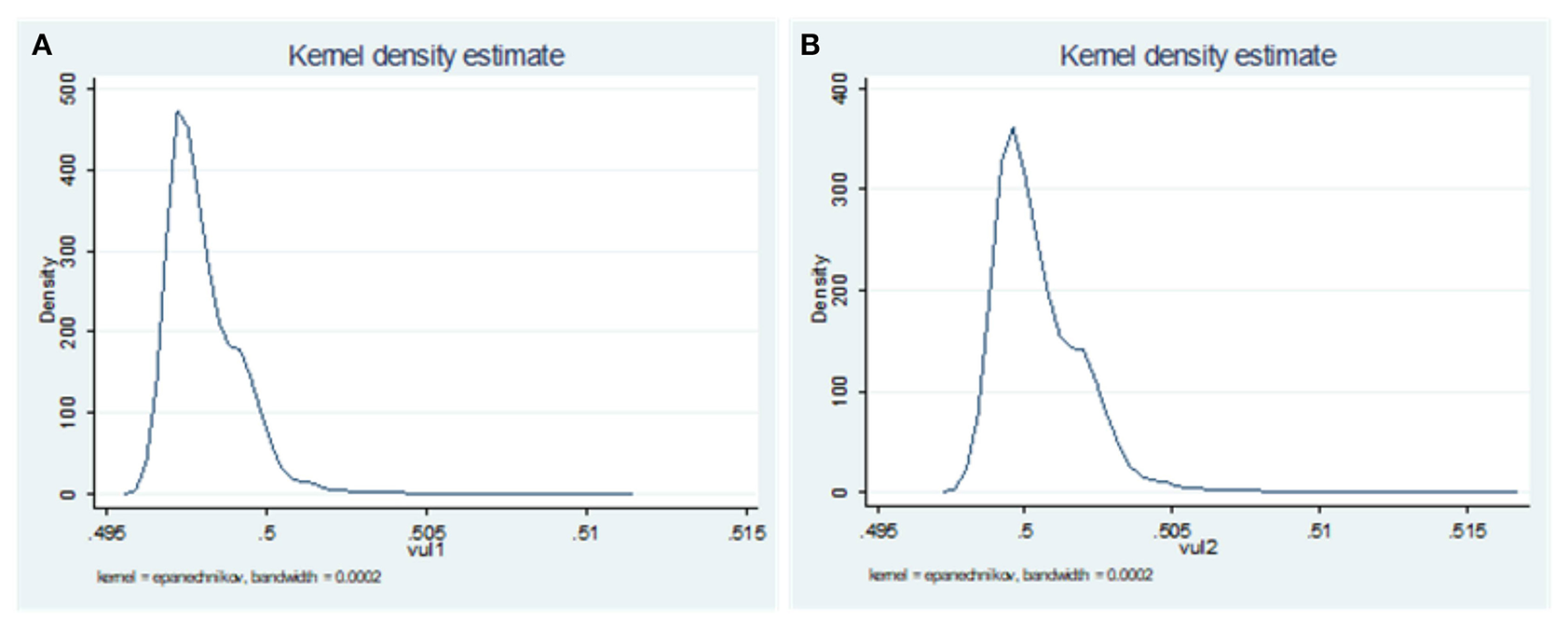
Kernel Density of vulnerability to poverty. (A) VEP1-poverty line = 1.9$; (B) VEP2-poverty line = 3.1$.
Table 3
| Poverty vulnerability value (3.1$) | OR | St. Err. | t-value | p-value | [95% Conf] | Interval | Sig |
|---|---|---|---|---|---|---|---|
| Gender | −0.009 | 0.007 | −1.29 | 0.196 | −0.022 | 0.005 | |
| Age | 0.000 | 0.001 | −0.60 | 0.552 | −0.001 | 0.001 | |
| Marital status | 0.003 | 0.005 | 0.57 | 0.571 | −0.006 | 0.012 | |
| Family size | 0.067 | 0.004 | 17.42 | < 0.001 | 0.059 | 0.075 | *** |
| Number of labor force | −0.049 | 0.006 | −7.76 | < 0.001 | −0.061 | −0.036 | *** |
| Dependency ratio | −0.147 | 0.019 | −7.89 | <0.001 | −0.183 | −0.11 | *** |
| Education level | 0.001 | 0.006 | 0.16 | 0.870 | −0.011 | 0.013 | |
| Average length of education of family | −0.002 | 0.002 | −1.43 | 0.152 | −0.006 | 0.001 | |
| Self–rating health | −0.001 | 0.004 | −0.29 | 0.775 | −0.008 | 0.006 | |
| Non–agricultural workers | 0.016 | 0.014 | 1.15 | 0.249 | −0.011 | 0.044 | |
| Household livestock ownership (cattle) | −0.001 | 0.001 | −1.23 | 0.220 | −0.004 | 0.001 | |
| Housing type | 0.003 | 0.003 | 1.04 | 0.300 | −0.002 | 0.008 | |
| Type of drinking water | 0.004 | 0.003 | 1.43 | 0.151 | −0.001 | 0.009 | |
| Toilet type | 0.010 | 0.003 | 3.61 | <0.001 | 0.004 | 0.015 | *** |
| Separation of housing and kitchen | 0.014 | 0.007 | 2.00 | 0.046 | 0.000 | 0.028 | ** |
| Gift expenses (log) | −0.032 | 0.001 | −31.25 | <0.001 | −0.034 | −0.03 | *** |
| Income from migrant workers | −0.003 | 0.001 | −3.48 | 0.001 | −0.004 | −0.001 | *** |
| Loans because of illness | 0.029 | 0.008 | 3.74 | <0.001 | 0.014 | 0.044 | *** |
| Low–income households | 0.018 | 0.007 | 2.81 | 0.005 | 0.006 | 0.031 | *** |
| Medical assistance | 0.029 | 0.011 | 2.72 | 0.007 | 0.008 | 0.050 | *** |
| Physical accessibility | 0.002 | 0.003 | 0.56 | 0.579 | −0.005 | 0.008 | |
| Chronic disease diagnosis and treatment institutions | −0.011 | 0.006 | −1.88 | 0.060 | −0.022 | 0.000 | * |
| Constant | 0.005 | 0.061 | 0.08 | 0.938 | −0.114 | 0.123 |
Analysis on influencing factors of poverty vulnerability (3.1$).
p < 0.01;
p < 0.05;
p < 0.1.
Analysis of tendency score matching results
The prevalence of chronic diseases among rural elderly people > 60 years old was 64.62%, and the prevalence of physical multimorbidity was 21.24%. Nearest neighbor matching (1:1 ratio) was used to calculate the average treatment effect (ATT) of the treatment group. Before calculating ATT, a balance test and common support test were performed. As shown in Figures 2, 3 depicting the balance test results, the covariate standardization deviation (% bias) of the matched post-processing group and the control group was greatly reduced (both <10%). Figure 4 shows the results of the common support test, where the two groups of samples were basically in the common support range, while 15 samples in the control group were not in the common support range vs. only two samples in the treatment group. As shown, most of the observed values were in the common value range (on support), and the tendency score had greater overlap in the processing group and the control group.
Figure 2
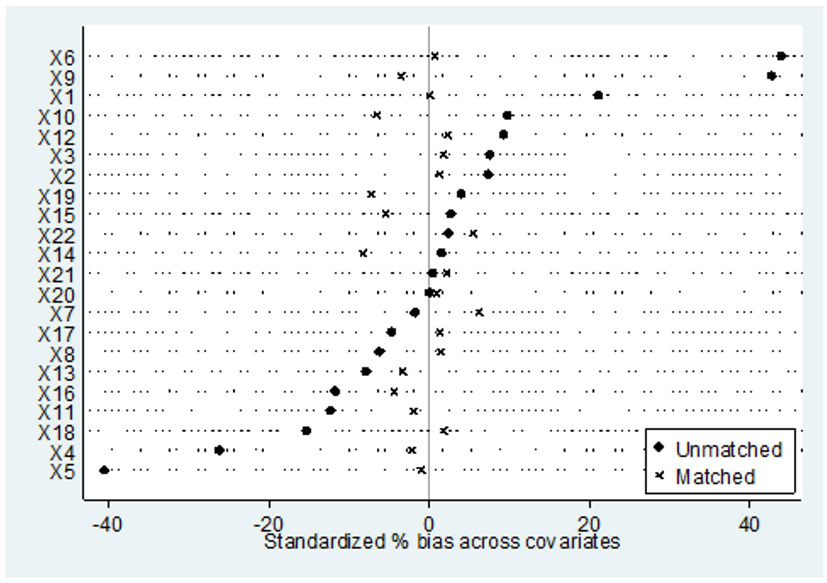
Standardized deviation diagram of covariates.
Figure 3
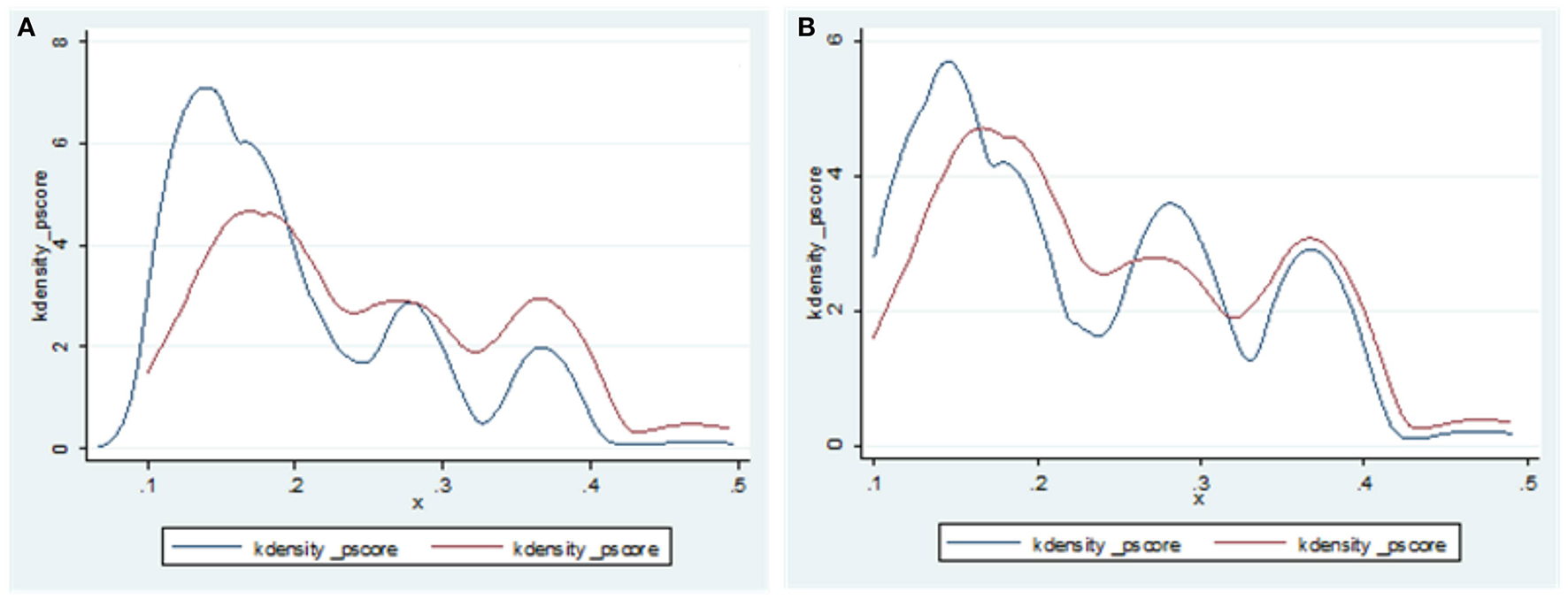
Balance test before (A) and after (B) matching between treatment group and control group.
Figure 4
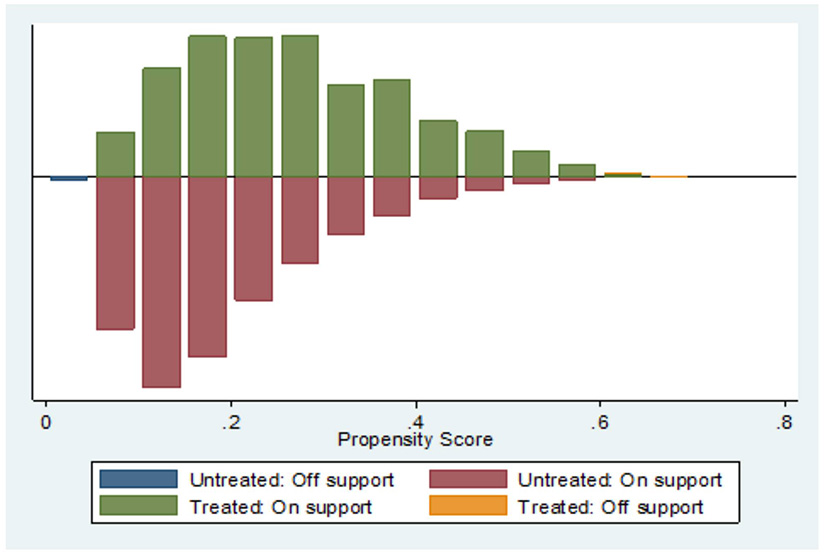
Common support test after matching between treatment group and control group. Untreated off support = 15; Treated off support = 2.
As shown in Table 4, for the vulnerability to poverty of aging rural families calculated at the international poverty line of $1.9/day, the vulnerability to poverty of the matched post-treatment group and the control group were 0.043 and 0.032, respectively. The difference was 0.011, i.e., the net effect of the coexistence of chronic diseases on the vulnerability to poverty of aging rural families was 0.011. According to the vulnerability to poverty value of rural aging families calculated at the international poverty line of $3.1/day, the vulnerability to poverty values of the matched post-treatment group and the control group were 0.486 and 0.474, respectively. The difference was 0.012, i.e., the net effect of physical multimorbidity on the vulnerability to poverty of rural elderly families was 0.012. The results show that the difference of vulnerability value between the treatment group and the control group was 0.012, that is, compared with the families without chronic diseases and with only one chronic disease, the poverty vulnerability value of families with physical multimorbidity will increase by 0.012. This shows that families with physical multimorbidity will increase the probability of poverty vulnerability.
Table 4
| Before and after matching | Treated | Controls | Difference | S.E. | T–stat | |
|---|---|---|---|---|---|---|
| VEP1 (poverty line = 1.9$) | Unmatched | 0.043 | 0.056 | −0.014 | 0.009 | −1.520 |
| ATT | 0.043 | 0.032 | 0.011 | 0.018 | 0.570 | |
| VEP2 (poverty line = 3.1$) | Unmatched | 0.486 | 0.551 | −0.065 | 0.020 | −3.210 |
| ATT | 0.486 | 0.474 | 0.012 | 0.042 | 0.280 |
The net effect of physical multimorbidity on poverty vulnerability [neighbor (K = 1)].
Analysis of intermediary effect of action path
Based on the analysis of the net effect of physical multimorbidity on poverty vulnerability, it is necessary to examine the mediation path further. As shown in Table 5, In the path with human capital as intermediary variable, the indirect effect of average level of family education was 0.0003, the contribution rate was 41.75%; self-rating health was −0.0052, the contribution rate was 82.80%; non-agricultural employment was −0.0046, the contribution rate was 2.57%. In the path with material capital as intermediary variable, the indirect effect of household cattle production was 0.0004, the contribution rate was 1.95%; Housing type was −0.0008, the contribution rate was 4.81%. In the path with social capital as intermediary variable, the indirect effect of gift expenses was 0.0006, the contribution rate was 0.8%; In the path with Risk Response Strategy as intermediary variable, the indirect effect of loans because of illness is 0.0034, the contribution rate was 2.17%. Analysis shows that self-rated health status, non-agricultural employment, household cattle production, housing type, gift expenses and loan for illness were the mediation paths of poverty vulnerability related to physical multimorbidity. These paths had a partial mediating role in the process of health-related vulnerability to poverty. Among these paths, the mediating effect of human health capital in family resource endowment was the largest, accounting for 82.8%; however, the total effect C was not significant. The sign of indirect effect a × b was opposite to that of direct effect C', indicating that the mediating effect of self-rated health results in vulnerability to poverty related to the physical multimorbidity existing in masking effect. The intermediary effect, direct effect, and total utility of non-agricultural employees in professional human capital in family resource endowment were statistically significant. Non-agricultural employment reduced the incidence of vulnerability to poverty. Household livestock ownership and housing type in physical capital, gift expenditure in social capital and disease-related lending in risk response strategy also had a part in the intermediary effect. Disease-related lending alleviated the vulnerability to health-related poverty.
Table 5
| VEP2 | a coefficient | b coefficient | Indirect effect (a*b) | Direct effect | Total effect | The proportion of total effect that is mediated |
|---|---|---|---|---|---|---|
| Education level | 0.0041 | 0.0658 | 0.0003 | −0.0808*** | −0.0805*** | −0.00335 |
| Average length of education of family | 0.0038 | 0.0647*** | 0.0003 | 0.0003 | 0.0006 | 0.4175 |
| Self–rating health | −0.0751*** | 0.0691*** | −0.0052*** | 0.0115 | 0.0063 | −0.8280 |
| Non–agricultural workers | −0.0677** | 0.0687*** | −0.0046* | 0.1851*** | 0.1805*** | −0.0257 |
| Household livestock ownership (cattle) | 0.006902 *** | 0.0580*** | 0.0004** | 0.0201 *** | 0.0205*** | 0.0195 |
| Housing type | −0.0130** | 0.0629*** | −0.0008* | −0.0162** | −0.0170** | 0.0481 |
| Type of drinking water | 0.0099* | 0.0622*** | 0.0006 | 0.0255*** | 0.0262*** | 0.0236 |
| Toilet type | −0.0021 | 0.0659*** | −0.0001 | 0.0659*** | 0.0658*** | −0.0021 |
| Separation of housing and kitchen | −0.0096 | 0.0666*** | −0.0006 | 0.1451*** | 0.1444*** | −0.0044 |
| Gift expenses (log) | 0 0.0060*** | 0.0935*** | 0.0006*** | −0.0711*** | −0.0705*** | −0.0080 |
| Income from migrant workers | 0.0019 | 0.0643*** | 0.0001 | 0.0024 | 0.0025 | 0.0482 |
| loans because of illness | 0.0617*** | 0.0547*** | 0.0034** | 0.1518*** | 0.1552*** | 0.0217 |
| Low–income households | −0.0134 | 0.0672*** | −0.0009 | 0.1228*** | 0.1219*** | −0.0074 |
| Medical assistance | 0.0001 | 0.0647*** | 0.000008 | 0.0476* | 0.0476* | 0.0002 |
| Physical accessibility | −0.0007 | 0.0649*** | −0.000043 | 0.0487*** | 0.0487*** | −0.0009 |
| Chronic disease diagnosis and treatment institutions | −0.0081 | 0.0636*** | −0.0005 | −0.0764*** | −0.0770*** | 0.0067 |
Intermediary effect test of vulnerability to poverty related to the physical multimorbidity.
p < 0.01;
p < 0.05;
p < 0.1.
Discussion
We measured the vulnerability to health-related poverty of aging rural families using two poverty lines and analyzed the mediation path of physical multimorbidity on poverty vulnerability based on the survey data obtained in 2019 from aging rural families in Ningxia, China. The empirical analysis showed that: first, Taking the high poverty line as the standard, more than half of the households were vulnerable; second, Families with physical multimorbidity were more vulnerable than those without chronic diseases or with one chronic disease; third, the test of intermediary effect mechanism revealed that self-rated health status, non-agricultural employment, household cattle production, housing type, gift expenses and loan for illness were important ways to reduce family's vulnerability to health-related poverty.
Taking the vulnerability to poverty measured by the high poverty line as the explanatory variable, households with large population had a higher probability of poverty vulnerability; Households with large household labor force are less vulnerable. The type of toilet and the separation of kitchen and housing were risk factors of poverty vulnerability. Previous studies have found that labor migration can significantly reduce the family's vulnerability to health-related poverty (55, 56). Our study also revealed that income of migrant workers was associated with the vulnerability to poverty of family. It has been reported that low-income households and medical assistance have no impact on the vulnerability to poverty (57), which was contrary to our results that low-income households and medical assistance could reduce vulnerability to health-related poverty. We also found that the level of chronic disease diagnosis and treatment institutions were risk factors of the vulnerability to poverty. Suppose grass-roots medical institutions cannot meet the medical needs of chronic patients, thus making a considerable number of patients seek medical help from institutions above the county level. In that case, this tends to increase the disease economic burden of families of chronic patients, affecting their vulnerability to health-related poverty (1).
Intermediary effect mechanism test revealed that family human capital, material capital, social capital, and private lending in risk response strategy were important ways to reduce family's poverty vulnerability related to physical multimorbidity. It has been found that the deterioration of residents' health levels makes them face higher vulnerability to poverty. For every 10% decline in residents' health level, the vulnerability to poverty increases by 6% (58). Some previous studies have also found that self-rated health status was associated with the vulnerability to health-related poverty (59), which is consistent with the results of the present study. Engaging in non-agricultural work and social capital can help to reduce farmers' the vulnerability to poverty. Individual differences in non-agricultural employment and health contribute the most to vulnerability to poverty (60). Our results revealed that non-agricultural employees was an important intermediary path to reduce the incidence of the vulnerability to health-related poverty. Material capital can also help to cope with the impact of health risks. The amount of household livestock and other realizable assets can be used to measure material capital, which reflects the economic situation of families to a certain extent and may alleviate effect on the vulnerability to health-related poverty (28). Gift spending in social capital also participates in the intermediary effect. Existing studies have reported that social capital has an external driving force on the family's livelihood capital (61). In the risk response strategy, lending due to illness also has a part of the intermediary effect, and it is an intermediary path to alleviates the vulnerability to health-related poverty. Some scholars have found that the intermediary effect of private lending is about 10%, which can reduce the vulnerability to poverty (36).
Implications for policy and practice
Understanding the intermediary path of poverty vulnerability related to physical multimorbidity of aging rural families may help to reduce the risk of vulnerable groups returning to poverty: first, To prevent the further development of chronic diseases and block the path of poverty, risk factors of multimorbidity such as dietary control, abstaining from tobacco, alcohol and physical activities should be targeted at an early state to prevent or delay the disease onset (62). The resource endowment of families is largely affected by the subjective initiative of family members through hard work, and non-agricultural employment, as improving labor skills can greatly enhance the family's ability to generate income (1), promote the development of rural labor economy and rural community construction, and form a good economic and social environment to improve farmers' ability to resist risks. Second, strategies for alleviation of systematic poverty should focus on promoting non-agricultural employment among vulnerable groups and continue to block the poverty trap through poverty alleviation in education and health. It is also necessary to focus on constructing rural family human capital. The higher the education level of rural residents, the lower their vulnerability to poverty (63). Education input-output is a relatively long-term process, and there is a lag effect on the embodiment of poverty alleviation effect. Third, the governance scheme for the health poverty vulnerability of rural elderly families should focus on improving the family coping ability. Primary care facilities should be strengthened to increase availability and accessibility while making the facilities affordable (64).
Strengths and limitations
Although we made a preliminary discussion on mediation path of the physical multimorbidity on vulnerability to poverty, due to the limited availability of data, the robustness of the conclusions of empirical research need to be further improved. With the emergence of higher quality data, the measurement of vulnerability to poverty or residents' vulnerability to health-related poverty and the discussion of relevant internal mechanisms could be further improved.
Conclusions
In the study, the health-related poverty vulnerability index was introduced as the risk warning signal of returning to poverty due to illness. In the process of poverty vulnerability related to the physical multimorbidity, self-rated health status, non-agricultural employment, household cattle production, housing type, gift expenses and lending due to illness were intermediary paths to alleviate vulnerability to poverty.
Funding
This paper was supported by the National Natural Science Foundation of China (No. 71864030).
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical approval was granted by the Ethics Committee of Ningxia Medical University, Approval number, No. 2018-114. The patients/participants provided their written informed consent to participate in this study.
Author contributions
HQ conceptualized the research idea and design. WG participated in the research design, drafted the manuscript, analyzed, and interpreted the data. JD helped revise the manuscript and interpreted the data. KC, WW, BG, and ZH helped clean the data. All authors contributed to the article and approved the submitted version.
Acknowledgments
This study is a population-based survey, and we thank all the respondents who volunteered to participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- VEP
expected poverty vulnerability
- FGLS
feasible generalized least squares
- OLS
Ordinary Least Square
- VEP1
the expected poverty vulnerability calculated with the international poverty line of $1.9/day
- VEP2
the proportion of expected poverty vulnerability calculated with the international poverty line of $3.1/day
- ATT
average treatment effect.
Abbreviations
References
1.
JW . Study on Health Risk Identification and Governance Strategy of Poverty Vulnerability of Rural Elderly Families in China. China Social Sciences Press (2020).
2.
Xinhua News Agency . Speech at the National Poverty Alleviation Summary and Commendation Conference. People's daily (2021).
3.
Xinhua News Agency . Available online at: http://www.cac.gov.cn/2020-03/06/c_1585039781415880.htm.
4.
Zhu ZF Cheng B Zhao DH Wang JY Cheng TZ . Research on the Connecting Path Between Healthy Poverty Alleviation and Rural Revitalization in China. China Health Econ. (2021) 40:9–13.
5.
Song YF . Research on the action mechanism and support path of inclusive finance blocking poverty return. Contemp Econ Policy. (2020) 7:41–5.
6.
Cheng B Zhu Z F Zhao DH Xu N Cheng TZ . Effectiveness, experience and challenges of healthy poverty alleviation in China. China Health Econ. (2021) 40:5–8.
7.
Wang YF . Study on the Problems and Countermeasures of Consolidating the Achievements of healthy poverty alleviation in Ningxia.Ningxia University (2021).
8.
China population and Development Research Center: National Health Poverty Alleviation Data Monitoring Report (2016-2020) October 2020 .
9.
Ningxia daily . Available online at: http://www.gov.cn/xinwen/2017-04/29/content_5189848.htm (accessed April 29, 2017).
10.
Zhu MJ . Study on disease burden and health poverty alleviation policy for patients with chronic diseases in Guyuan City. China Primary Health Care. (2019) 33:43–5. 10.3969/j.issn.1001-568X.2019.01.0015
11.
Tang SL . Plastic license Study on disease burden and health targeted poverty alleviation policy for poor patients with chronic diseases. J Health Policy. (2017) 10:64–7. 10.3969/j.issn.1674-2982.2017.06.012
12.
Yang G Kong L Zhao W . Emergence of chronic non-communicable diseases in China. Lancet. (2008) 372:1697–705. 10.1016/S0140-6736
13.
Urosević J Odović G Rapaić D Davidović M Trgovcević S Milovanović V . Quality-of life of the elderly in urban and rural areas in Serbia. Vojnosanitetski pregled. (2015) 72:968–74. 10.2298/VSP140831107U
14.
Liu E Zhang Q Feng Y . Elderly poverty risk of chronic diseases: theoretical mechanism and empirical test. Insurance Res. (2020) 11:63–78. 10.13497/j.cnki.is.2020.11.005
15.
Wang LM Chen ZH Zhang M Zhao ZP Huang ZJ Zhang X et al . Study of the prevalence and disease burden of chronic disease in the elderly in China. Zhonghua liuxingbingxue zazhi. (2019) 40:277–83. 10.3760/cma.j.issn.0254-6450.2019.03.005
16.
Barnett K Mercer SW Norbury M Watt G Wyke S Guthrie B . Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. 10.1016/S0140-6736
17.
Bloom DE Cafiero E Jané-Llopis E Abrahams-Gessel S Bloom LR Fathima S et al . The Global Economic Burden of Non-Communicable Diseases.Geneva: World Economic Forum (2011).
18.
Zhao Y Atun R Oldenburg B McPake B Tang S Mercer SW et al . Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. (2020) 8:e840–e9. 10.1016/S2214-109X
19.
Shu Z Tang YX Xiao JG Gong X . Analysis on the influencing factors of poverty caused by poverty and disease. China Public Health. (2019) 35:953–8. 10.11847/zgggws1116720
20.
Chen J Rong S Song MJSIR . Poverty Vulnerability and Poverty Causes in Rural China. (2020). p. 1-27. 10.1007/s11205-020-02481-x
21.
Liu JJ Wang GL Yan BL . Study on Influencing Factors of health poverty vulnerability of patients with chronic diseases. China Health Economy. (2019) 38:56–9.
22.
Ouadika SJPC . Health shocks and vulnerability to poverty in Congo. Humanit Soc Sci Commun. (2020) 7:1-8. 10.1057/s41599-020-00674-w
23.
Liu YL Zhu K Chen QY Li J Cai J He T et al . Impact of the COVID-19 Pandemic on farm households' vulnerability to multidimensional poverty in rural China. Sustainability. (2021) 13:1842. 10.3390/su13041842
24.
Han JS . Research on Equalization of Basic Public Expenditure From the Perspective of Benefit Destination. Central University of Finance and Economics (2016).
25.
He SY Huang WT . Poverty vulnerability of reservoir area migrants and reconstruction of accurate poverty alleviation strategy – Based on the analysis of 386 rural migrants in the reservoir area in the upper reaches of the Yangtze River. Rural Econ. (2018): 49–55.
26.
Zhong-Liang HU University GM . Gene, Cognitive Ability and Household Financial Decisions- Based on Analysis of the Literatures. (2016).
27.
Li H Zhang Z Yang X W . Does the health impact of the elderly squeeze out family education expenditure—Intermediary effect test based on medical expenditure. Educ Econ. (2019) 6:46–56.
28.
Chen CP . Evaluation of poverty vulnerability of the new generation of migrant workers in Western China – Based on the investigation of livelihood capital J Southwest. (2018) 39:127–32. 10.3969/j.issn.1004-3926.2018.05.020
29.
Liang F . Study on poverty vulnerability of farmers in Qinba Mountain Area: from the perspective of resource endowment and risk impact. Northwest University of agriculture and forestry science and technology (2018).
30.
Li L M Yang M Y Li Z . Research on the influence mechanism of educationon health. China Popul. Res. News. (2021). Available online at: https://115.com/101075/T1250373.html
31.
Jing ZY . Study on the Measurement and Dynamic Change of Health Poverty of Empty Nest Elderly Families in Rural Areas. Shandong University (2021).
32.
Yanqing MJ . Accessibility to Healthcare Resources and Farmers' Health: Evidence from Rural China. (2008).
33.
Ge XU Qian LU Jiang YL . Resources, Environment. Social Capital, Income Diversification and Households' Poverty Vulnerability. (2019).
34.
Wang Z Q . Study on the impact of family endowment and health risk impact on Farmers' poverty – A case study of Qinba Mountain Area Northwest University of agriculture and forestry science and technology (2019).
35.
Chalkiness Intergenerational upward mobility of private transfer payments and poverty vulnerability . Econ Manag. (2015) 37:170–9.
36.
Hu J Economics SO . Private Lending, Social Network and Poverty Vulnerability: Analysis Based on Test Procedure Of Mediating Effect. (2015).
37.
Zhang ML Li GP . Effect evaluation and mechanism analysis of commercial insurance policy on reducing family poverty vulnerability. Contemp Econ Res. (2020) 11:91–102.
38.
He X Y . he impact of Inclusive Finance on rural family poverty vulnerability from the perspective of multi intermediary. Shandong University (2021).
39.
Wei Y Li M.Q . Study on health poverty vulnerability and influencing factors of rural women. J Hubei Univer. (2021) 39:105–18. 10.13501/j.cnki.42-1328/c.2021.04.010
40.
Li L . Research on the Statistical Measurement and Occurrence Mechanism of Poverty Vulnerability and its Application in Poverty Alleviation Policies. Beijing: China financial and Economic Publishing House. (2020).
41.
Chaudhuri S Jalan J Suryahadi AJ . Assessing household vulnerability to poverty: a methodology and estimates for Indonesia. (2002).
42.
Abebe FE . Determinants of Rural Households' Vulnerability to Poverty in Chencha and Abaya Districts, Southern Ethiopia (Microeconometric Analysis). (2016).
43.
Nguyen LD Raabe K . Grote U. Rural–urban migration, household vulnerability, and welfare in Vietnam. World Dev. (2015) 71:79–93. 10.1016/j.worlddev.2013.11.002
44.
Rosenbaum PR Rubin DB . The central role of the propensity score in observational studies for causal effects. Biometrika. (1983) 70:41–55. 10.1093/biomet/70.1.41
45.
Wen Z L Ye B J . Intermediary effect analysis: method and model development. Adv psychol sci. (2014) 22:731–45. 10.3724/SP.J.1042.2014.00731
46.
Zhang H Kang F . Analysis method of multiple mediating effects based on bootstrap. Stat Decis Mak. (2016) 5:75–8. 10.13546/j.cnki.tjyjc.2016.05.019
47.
Yan HT Yang SP . Relative poverty governance effect of rural medical insurance system – An Empirical Analysis from the perspective of poverty vulnerability. J Hunan Agric Univer. (2021) 22:48–55. 10.13331/j.cnki.jhau(ss).2021.01.006
48.
Glewwe P . Hall G. Are some groups more vulnerable to macroeconomic shocks than others? Hypothesis tests based on panel data from Peru. J Dev Econ. (1998) 56:181–206. 10.1016/S0304-3878(98)00058–3
49.
Ligon E Schechter L . Measuring Vulnerability 2002 Annual meeting, July 28-31, Long Beach, CA.American Agricultural Economics Association Agricultural and Applied Economics Association, (2002)
50.
Yang S Guan R Jin Y . Public Health Infrastructure, Family Health Level and Poverty Vulnerability of Farmers—Based on the Data of 1458 Households in 8 Centralized Poverty-stricken Areas. (2019).
51.
Usman MA Nicolas G Joachim VB . The Impact of Drinking Water Quality and Sanitation on Child Health: Evidence from Rural Ethiopia. (2018). p. 1–19.
52.
Zhang J . The impact of water quality on health: evidence from the drinking water infrastructure program in rural China. J Health Econ. (2012) 31:122–34. 10.1016/j.jhealeco.2011.08.008
53.
Center for health statistics and information NHC . The Sixth National Health Service Statistical Survey Report in 2018.Beijing: People's medical publishing house (2018). p. 124–5.
54.
Fang Jie Wen Zhonglin Zhang Minqiang . Mediation effect analysis of categorical variables. Psychol Sci. (2017) 40:471–7.
55.
Xu C Gong B . Whether farmers' Entrepreneurship reduces poverty vulnerability. J Financ Econ. (2017) 37:46–59.
56.
Gao RC Li S . Is the migration of rural labor force conducive to the lasting poverty alleviation of left behind families—erability—Analysis Based on CFPS micro data. Accounting study. (2018). 4:132–140.
57.
Yao M D . Research on the impact of government transfer payment on family poverty vulnerability—Analysis Based on CFPS micro data. Rev Account Stud. (2018) 15:8–11.
58.
Huang XJ Economics . What leads to the rural household's risk of poverty—Measurement and decomposition of poverty vulnerability. J Guizhou Univ Financ Econ. (2018) 1:91–102. 10.3969/j.issn.1003-6636.2018.01.010
59.
Liang F Zhu YJ . Analysis of Farmer's Vulnerability to Poverty From the Perspective of Resource Endowment. (2018).
60.
Liu MY Feng XL Wang SG . Study on poverty vulnerability of relocated farmers in ex situ poverty alleviation. Rural Econ. (2019) 64–72.
61.
Zhang ZG . Study on the influencing factors of poverty vulnerability of rural families in China – Based on the analysis framework of sustainable livelihood. Rural Econ Technol. (2018) 29:144–7.
62.
Sinha A Kerketta S Ghosal S Kanungo S Pati S . Multimorbidity Among Urban Poor in India: Findings From LASI, Wave-1. Front Public Health. (2022) 10:881967. 10.3389/fpubh.2022.881967
63.
Li L Bai XM . Measurement and decomposition of poverty vulnerability of urban and rural households in China – An Empirical Study Based on CHNS micro data. Quant Econom. (2010) 27:61–73. 10.13653/j.cnki.jqte.2010.08.002
64.
Sinha A Kerketta S Ghosal S Kanungo S Lee JT Pati S . Multimorbidity and Complex Multimorbidity in India: findings from the 2017-2018 Longitudinal Ageing Study in India (LASI). Int J Environ Res Public Health. (2022) 19:9091. 10.3390/ijerph19159091
Summary
Keywords
physical multimorbidity, poverty vulnerability, propensity score matching, intermediary effect, cross-sectional study
Citation
Guo W, Du J, Chen K, Wang W, Gao B, Hu Z and Qiao H (2022) The mediation path of physical multimorbidity on the vulnerability to health-related poverty of rural aging families in Ningxia, China: A cross-sectional survey. Front. Public Health 10:993977. doi: 10.3389/fpubh.2022.993977
Received
14 July 2022
Accepted
26 September 2022
Published
18 October 2022
Volume
10 - 2022
Edited by
Mingsheng Chen, Nanjing Medical University, China
Reviewed by
Enver Envi Roshi, University of Medicine, Tirana, Albania; Krushna Chandra Sahoo, Regional Medical Research Center (ICMR), India; Dan Zhao, Shandong University, China
Updates
Copyright
© 2022 Guo, Du, Chen, Wang, Gao, Hu and Qiao.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Qiao qiaohui71@163.com
This article was submitted to Health Economics, a section of the journal Frontiers in Public Health
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.