- 1School of Public Health, Fudan University, Shanghai, China
- 2China Research Center on Disability, Fudan University, Shanghai, China
- 3Key Laboratory of Health Technology Assessment, National Health Commission, Fudan University, Shanghai, China
- 4Shanghai Jinshan District Health Service Management Center, Shanghai Jinshan District Municipal Health Commission, Shanghai, China
Background: As one of the countries with the most serious degree of aging, the incidence of potentially inappropriate drug use among the elderly is as high as 30. 4% in Chinese communities, and the lack of effective medication management and poor medication compliance at home are the main factors. Given these situations, we constructed a Rational Medication Management Mode based on family physician service, carried out an empirical research and evaluated the implementation effect.
Methods: A prospective cohort study was conducted from September to December 2021 to analyze the implementation effect of the Rational Medication Management Mode by comparing the outcome indicators between the intervention group and control group. The primary outcome of this study was medication number and polypharmacy (taking 5 or more medications) at 90 days. The secondary outcomes included the situation for behavioral self-management and knowledge-belief-behavior of rational medication use.
Results: A total of 618 elderly patients (309 in the intervention group and 309 in the control group) with multimorbidity were included in this study, those were all available at follow-up at 90 days. At 90 days, the number of medications was achieved by 3.88 (1.48), and patients with polypharmacy were reduced by 59.55% in the intervention group, having a significant difference compared with the control group (P < 0.001). Patients with medication reminders, intermittent medication and adverse drug reactions were achieved in 294 (95.15%), 47 (15.21%), and 51 (16.51%) respectively in the intervention group (P < 0.001). The knowledge, belief, behavior security and behavior compliance of rational medication use of elderly patients were all greatly improved in the intervention group at 90 days (P < 0.0001).
Conclusion: The Rational Medication Management Mode based family physician service, which provides the support of manuals and pillboxes, can decrease the elderly patients' number of drugs with multimorbidity, reduce the incidence of polypharmacy, enhance behavioral self-management, increase the knowledge and belief of rational medication use, and improve the security and compliance of medication usage behavior. In order to provide a practical basis for rational medication management of elderly patients with multimorbidity under the background of long-term prescriptions in China.
Introduction
The elderly have a high prevalence of chronic diseases, and often suffer from multimorbidity, requiring long-term medication (1). As the elderly often repeat treatment in multiple departments and hospitals, in this process of medical transfer and transition, several specialists may prescribe repetitive medicines using disease-specific guidelines due to the lack of information interconnection, resulting in patients' repeated medication. Relevant studies have found that the elderly visit 4 different medical institutions and 8 different doctors each year on average, and the average dosage is more than 5 times that of young people (2, 3). The combined use of these medicines may cause harm to patients if there is no professional drug integration (4, 5). In addition, irrational use of medications can stimulate inappropriate patient demand, and may lead to a loss of patient confidence in the health system (6).
The World Health Organization (WHO) put forward the concept of rational medication use in 1985, which refers to patients receiving medications appropriate to their clinical needs, in doses that meet their requirements, for an adequate period, and at the lowest cost to them and their community (6). Irrational use of medications in a way that is not compliant with rational use as defined above, which included polypharmacy, inappropriate use of antimicrobials, over-use of injections, inappropriate self-medication, etc. Worldwide, more than 50% of all medications are inappropriately prescribed, dispensed, or sold, while 50% of patients fail to take them correctly (6). Technology tools, such as electronic personal health records, mobile applications, paper versions of medication record forms, etc, could improve both patient experience and medication adherence, and potentially enable patients to be active participants in medication reviews (7). Some studies have revealed that technology/tool-based medication management modes (8–10), such as the doctor-patient participatory mode and the pharmacist-leading home-dwelling mode, have achieved good results in the management of hypertension, diabetes, osteoporosis and other chronic diseases (11, 12), which helps to standardize the prescription behavior of medical service providers and improve patients' medication compliance and health outcomes. Moreover, studies estimated that a total of USD$18 billion, 0.3% of the global total health expenditure, could be avoided by appropriate medication management (13).
As one of the countries with the most serious degree of aging, there are 182.17 million elderly people aged 65 and over who suffer from at least one chronic disease in China, with an average of 3.1 diseases per capita (14, 15). Relevant study shows that the incidence of potentially inappropriate drug use among the elderly is as high as 30.4% in Chinese communities, and the lack of effective medication management and poor medication compliance at home are the main factors (16). A study demonstrates that <50% of patients with chronic diseases can still strictly take medications at home according to doctor's advice 1 year after discharge (17). Since more than 90% of the elderly always live at home, and the family physician system has been developed in China for more than 10 years, community healthcare centers have become a key link and an important way to strengthen rational medication management at home for the elderly (18). However, previous studies have shown that primary medical institutions in China are incompetence of pharmaceutical personnel and weak in pharmaceutical care, making it difficult to realize whole-process pharmaceutical care for elderly patients with chronic diseases at home. The elderly themselves also have problems, such as lack of drug knowledge, incorrect drug concepts, poor drug compliance, and lack of supervision from doctors in-home medication, which emphasizes the problem of irrational drug use (19).
Given these situations, we constructed a rational medication management mode based on family physician service, carried out empirical research and evaluated the implementation effect, improving elderly patients' health outcomes and providing a reference for the policy-making of rational medication management for the elderly in China.
Materials and methods
Rational medication management mode in this current study
Based on family physician service, the Rational Medication Management Mode in this current study specifically refers to the joint participation of family physicians, pharmacists, family physician assistants, nurses, elderly and their family members to carry out medication reconciliation and drug use guidance through medication management manual and pillbox.
The medication management manual (tool) in this study contained “Basic information”, “Diagnosis and treatment”, “Medications list”, “Health care products list”, “Medications record weekly table”, “Health-related index record weekly table”, “Self-evaluation of medication use compliance” and “Medication management evaluation from family physician” eight functional modules, which are jointly recorded by the family physician team, elderly patients and their families (see Supplementary Table 1 for framework and content).
The operation process of Rational Medication Management Mode in this current study is shown in Figure 1.
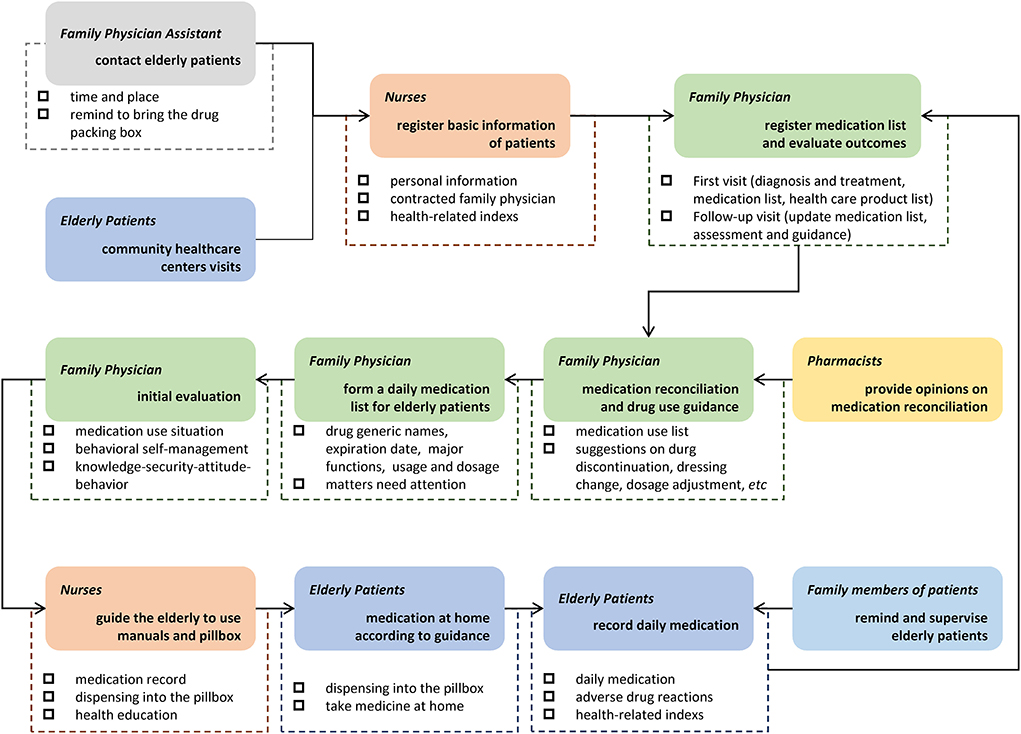
Figure 1. Operation process of Rational Medication Management Mode. Based on family physician service, the mode in this current study specifically refers to the joint participation of family physicians, pharmacists, family physician assistants, nurses, elderly and their family members to carry out medication reconciliation and drug use guidance through medication management manual and pillbox.
Empirical study design
In this study, two community healthcare centers were respectively selected in the central-city and countryside areas of Shanghai, divided into an intervention group and a control group. A prospective cohort study was conducted from September to December 2021 to analyze the implementation effect of the Rational Medication Management Mode by comparing the outcome indicators between the two groups.
Shanghai is a typical megacity in China, with developed economy and deep aging population. In 2011, Shanghai began to pilot the family physician system in community healthcare centers. In 2015, the “1+1+1” contract service mode was established, proposing to add pharmacists to the family physician team. In 2016, Shanghai took the lead in piloting the training of community clinical pharmacists. This series of explorations have provided a guarantee for the development of Rational Medication Management Mode for the elderly.
The selected community healthcare centers have the following characteristics: (i) complete functions with medication management, health monitoring, health education, etc; (ii) the family physician signing rate of the elderly aged 65 years old is more than 90%; and (iii) the family physician team organized well, equipping with general practitioners, nurses, pharmacists, family physician assistants, etc.
The target sample size is based on the calculation formula which compares 2 means with two groups:
where α is 0.05, Z value is two-sided, so Zα = 1.96; power of test is 0.9, so Zβ = 1.28. According to the pre-survey, the standard deviation (SD) of an average number of drugs was 1.71 (σ), and the difference value between the two groups was 0.49 (δ), so the calculated sample size was 256 per group. In this study, convenience sampling was used to select contracted elderly patients with comorbidity by family physician, and the propensity score matching was used to perform 1:1 matching on the baseline data of age, gender, living areas, marital status, education, living pattern, monthly income, insurance type, number of diseases and number of medication. Ultimately, 618 elderly patients with multimorbidity were enrolled in this study (309 in the intervention group and 309 in the control group) after propensity score matching. Considering the drop-out rates of 10%, the sample size still meets the calculation requirements. The flow chart of implementation effect research of the Rational Medication Management Mode is illustrated in Figure 2.
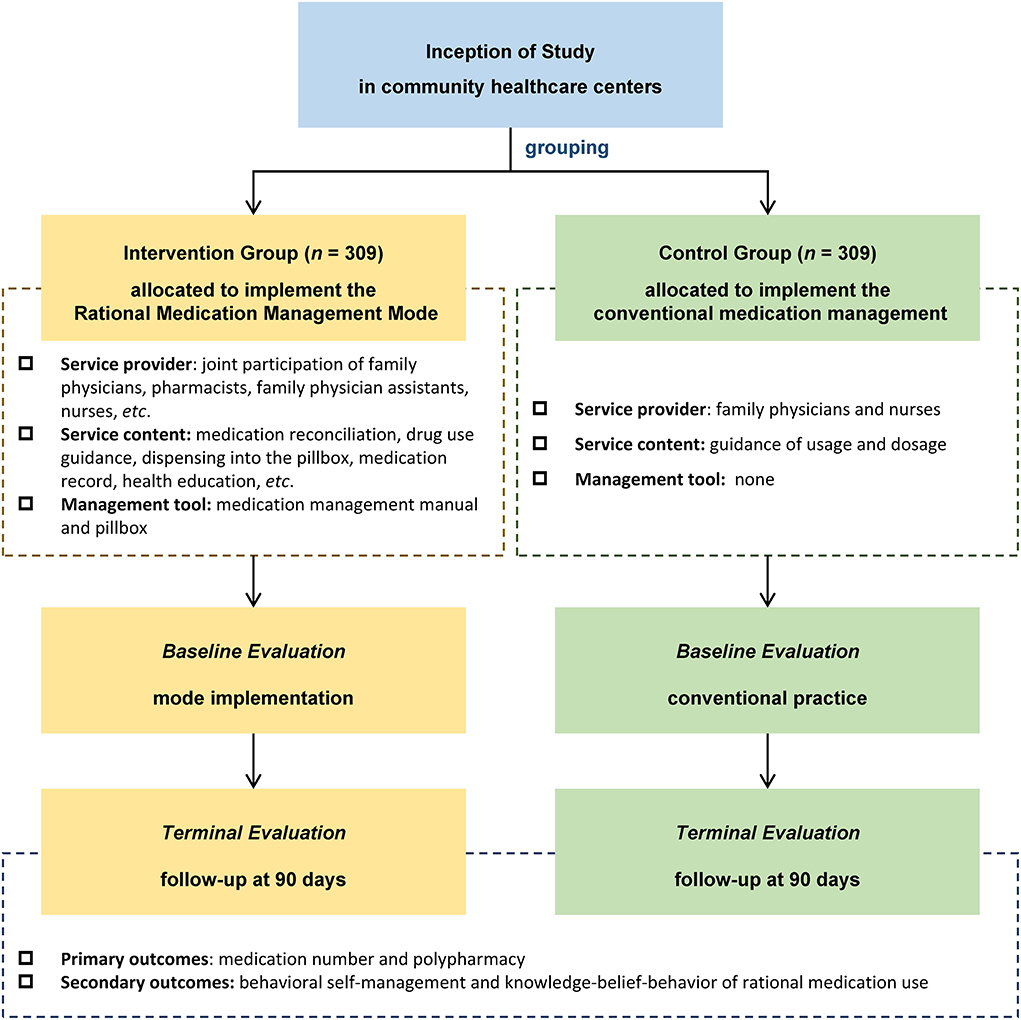
Figure 2. The flow chart of implementation effect research. A prospective cohort study was conducted from September to December 2021 to analyze the implementation effect of the Rational Medication Management Mode by comparing the outcome indicators between the intervention group and control group. The primary outcome of this study was medication number and polypharmacy (taking 5 or more medications) at 90 days. The secondary outcomes included the situation for behavioral self-management and knowledge-belief-behavior of rational medication use.
This study was approved by the Ethics Committee of School of Public Health, Fudan University (International Registration Number: IRB00002408 & FWA00002399; approval number: IRB#2021-11-0931).
Patients
Inclusion criteria
Referring to the screening criteria of relevant modes (20), this study included elderly patients with high demand for medication management services and the ability to collaborate in the implementation process. The inclusion criteria are as follows: (i) aged 65 ~ 75 years old; (ii) suffering from 2 or more common chronic diseases currently (hypertension, coronary heart disease, stroke, diabetes, chronic obstructive pulmonary disease, osteoporosis, etc.,); (iii) taking 2 or more drugs (including over-the-counter drugs); iv) require long-term medication; v) the condition is stable without acute symptoms; (vi) having health records in the community healthcare center and continuously visiting and prescribing drugs for more than 3 months; (vii) voluntarily participate in intervention projects and obtain informed consent.
Exclusion criteria
Patients with the following conditions were excluded: (i) consciousness disorders or communication difficulties; (ii) currently using medication reminder software; (iii) unstable condition; (iv) those who have plans to go out in the last 3 months, and the time of going out is more than 1 month; (v) not suitable to participate in this study from a specialist point of view (such as incapacity).
Elimination criteria
Those participants who dropped out and lost follow-up were excluded. If the subjects did not arrive at the community healthcare center within 3 months and could not be contacted, they were regarded as lost to follow-up.
Outcomes
The primary outcome of this study was medication number and polypharmacy (taking 5 or more medications) at 90 days.
The secondary outcomes included the situation for behavioral self-management and knowledge-belief-behavior of rational medication use. The behavioral self-management included the indicators of (i) medication reminders and its methods, (ii) intermittent medication and its reasons, and (iii) occurrence and handling of adverse drug reactions (ADRs).
The adapted scales were used for the evaluation of knowledge-belief-behavior for the rational medication (see Supplementary Table 2) (21, 22). According to the pre-survey, the rational medication knowledge scale and the medication behavior security scale optimized the expressions of the existing scales questions based on the opinions of the respondents. The rational medication belief scale and the medication behavior compliance scale were adapted from the existing scales, and the reliability and validity were tested based on the pre-survey. Cronbach's α coefficient was used to test the reliability of the scale, which demonstrated good consistency and reliability (Cronbach's α values were all > 0.7). Factorial analysis was used to test the validity of the scale (Kaiser-Meyer-Olkin value = 0.672; Bartlett's test of sphericity P value < 0.001), the cumulative variance interpretation rate was 67.30% when the eigenvalue is > 1, indicating good validity.
Statistical analysis
IBM SPSS Statistics 23.0 was used for data analysis. The data normality test was performed on the measurement data; the mean ± standard deviation was used to describe the measurement data with normal distribution; the quartiles were used to describe the measurement data with non-normal distribution; the composition ratio (%) was used to describe the count data. The differences between groups were analyzed by t-test for normally distributed measures, non-parametric tests for non-normally distributed measures, and chi-square test and Fisher exact probability method for counting data. A P value < 0.05 was considered significant.
Results
Baseline characteristics for elderly patients with multimorbidity
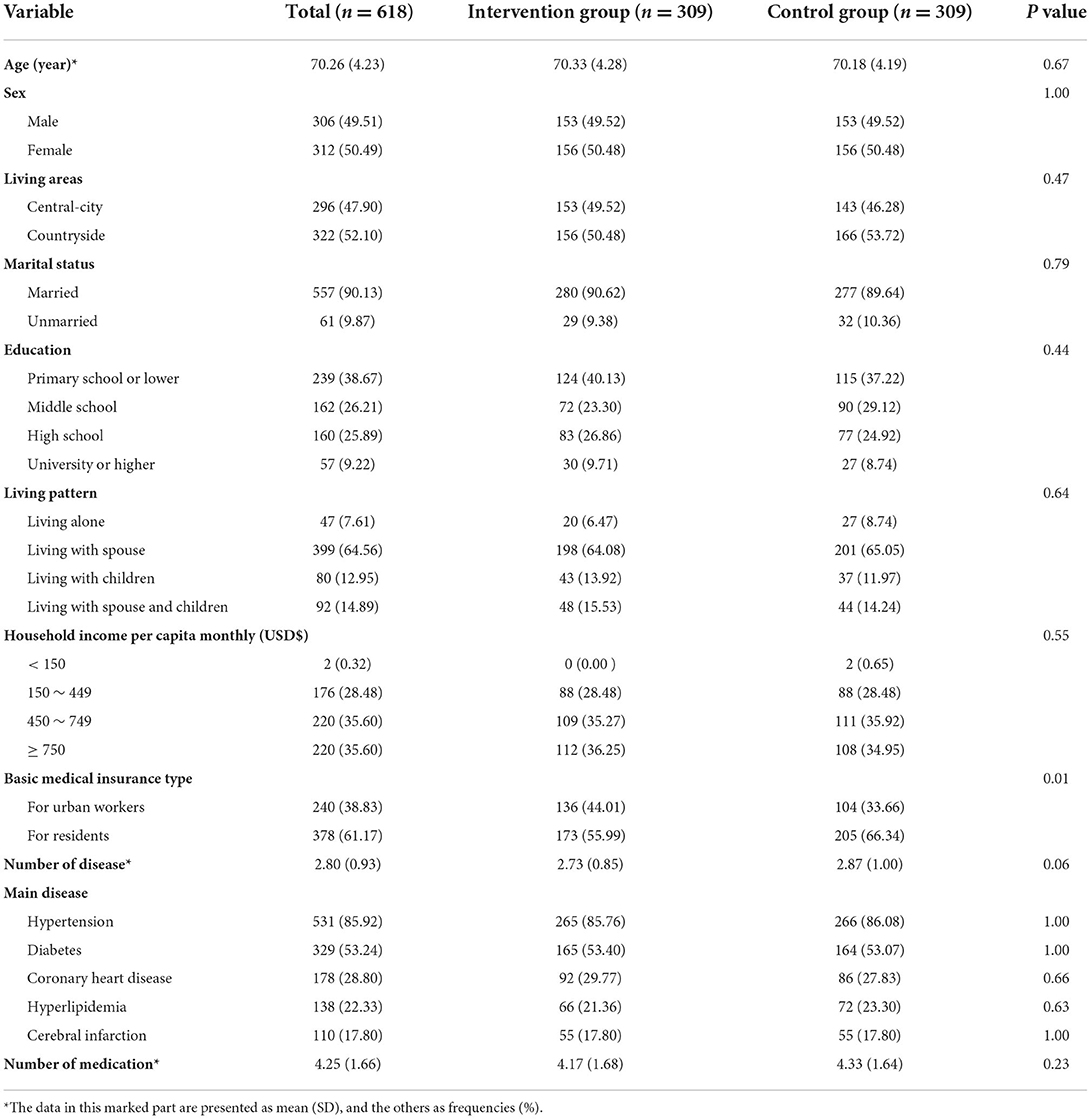
A total of 618 elderly patients (309 in the intervention group and 309 in the control group) with multimorbidity were included in this study, those were all available at follow-up at 90 days. Baseline characteristics of demographic and health status of the study participants are presented in Table 1.
There was no significant difference between the intervention group and the control group in age, gender, living area, marital status, education, living pattern, household income per capita monthly, the number of diseases, and the number of medications (P > 0.05). There was a statistical difference in the type of medical insurance between the two groups (P = 0.01). The homogeneity of baseline characteristics for the two groups is strong, especially the indicators of disease and medication, which were comparable.
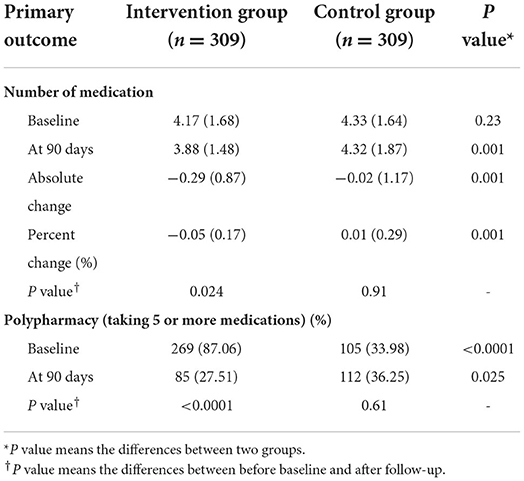
Primary outcome: Medication number and polypharmacy at 90 days
At 90 days, the number of medications was achieved by 3.88 (1.48) in the intervention group, while 4.32 (1.87) in the control group, which had a significant difference between the two groups (P = 0.001) (Table 2). And patients with polypharmacy were reduced by 59.55% in the intervention group at 90 days, having a significant difference compared with the control group (P < 0.001). The Rational Medication Management Mode had a positive effect on medication reconciliation (P = 0.024), while the conventional medication management was less effective (P = 0.91). Data on indicators are presented as the absolute change and percent change at 90 days from the baseline in each table.
Secondary outcomes: Behavioral self-management
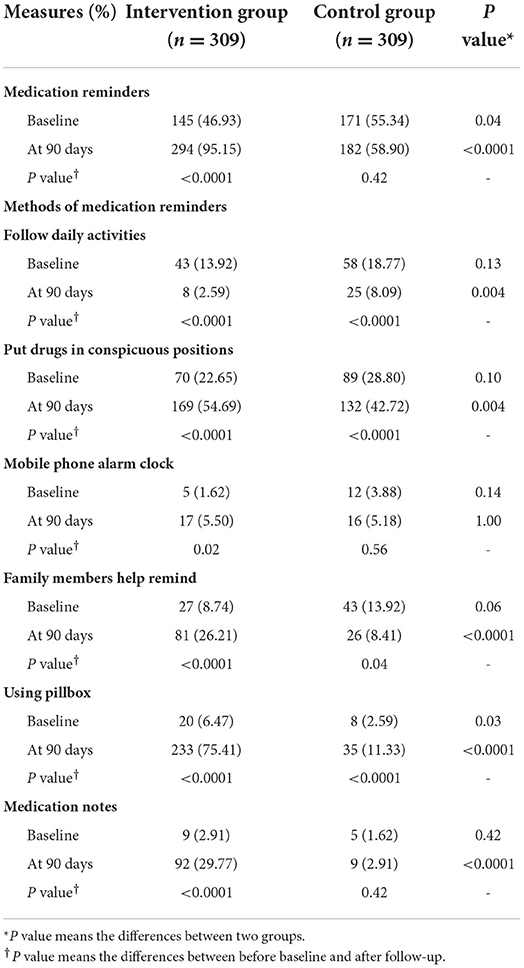
At 90 days, patients with medication reminders were achieved in 294 (95.15%) and 182 (58.90%) in the intervention group and control group respectively, which had a significant difference between the two groups (P < 0.001) (Table 3). For the methods of medication reminders, the main way in the intervention group was to use a pillbox (75.41%), while in the control group was to put drugs in conspicuous positions (42.72%).
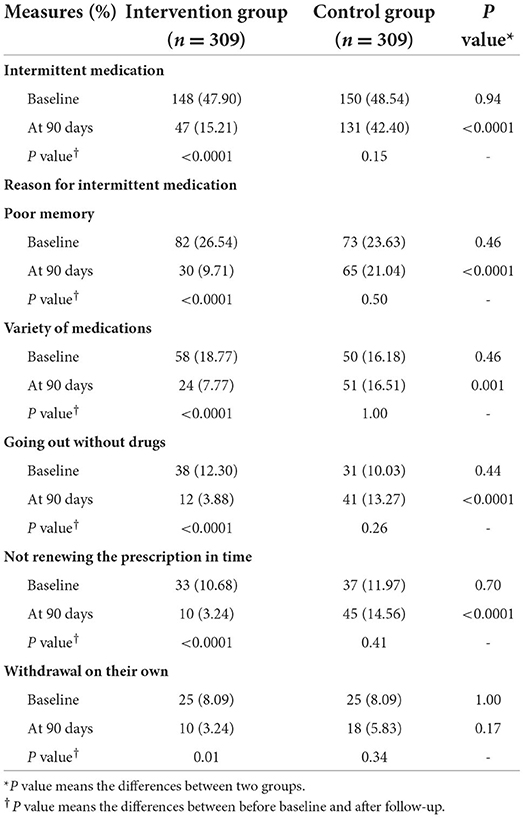
Patients with intermittent medication were reduced to 47 (15.21%) from 148 (47.90%) in the intervention group at 90 days, having a significant difference compared with the control group (P < 0.001) (Table 4). For the reason of reduction in intermittent medication, there were better improvements in poor memory, variety of drugs, withdrawal on their own, etc. in the experimental group (P < 0.05).
At 90 days, patients who occurred on ADRs were reduced to 51 (16.51%) from 88 (28.48%) in the intervention group, having a significant difference compared with the control group (P = 0.01) (Table 5). For the handling of ADRs, the way to ask family physicians increased remarkably in the intervention group (P < 0.0001).
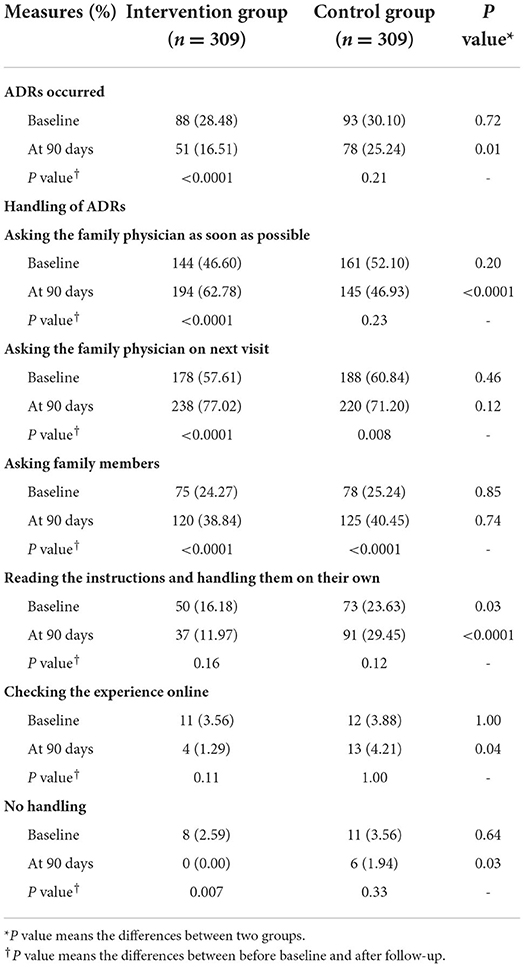
Table 5. Occurrence and handing of adverse drug reactions (ADR) of elderly patients with multimorbidity.
Secondary outcomes: Knowledge-belief-behavior evaluation
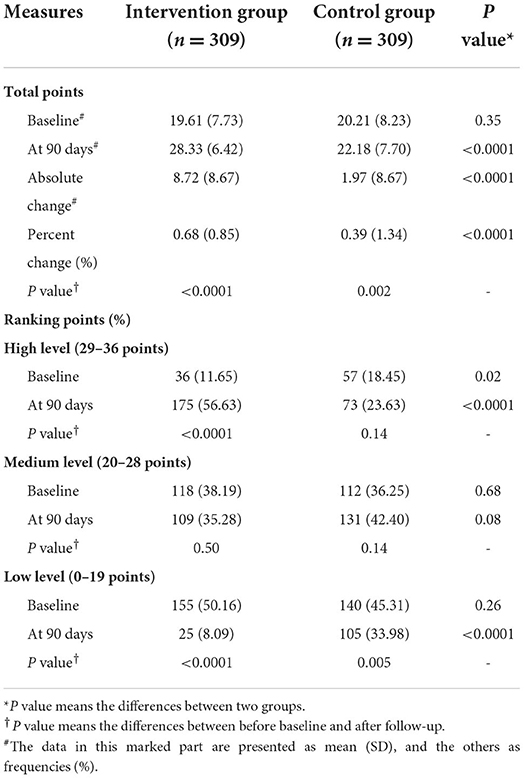
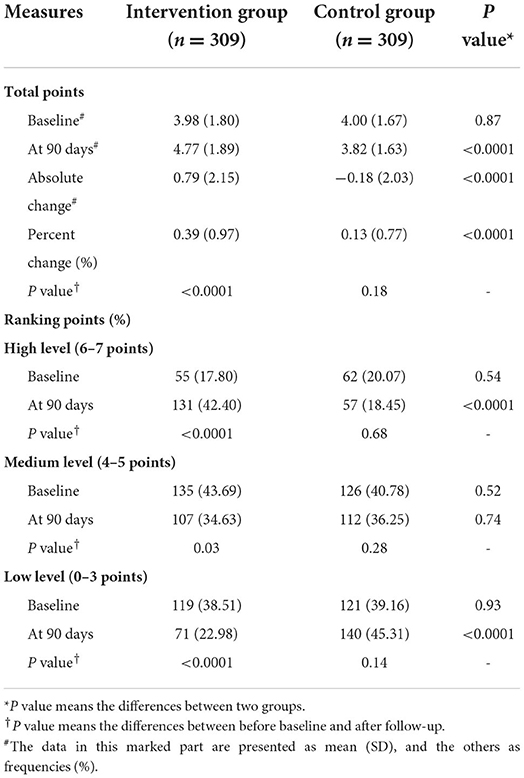
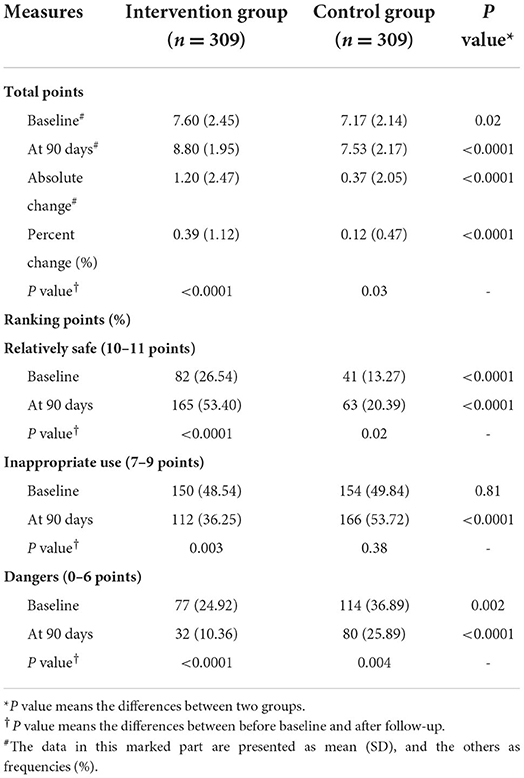
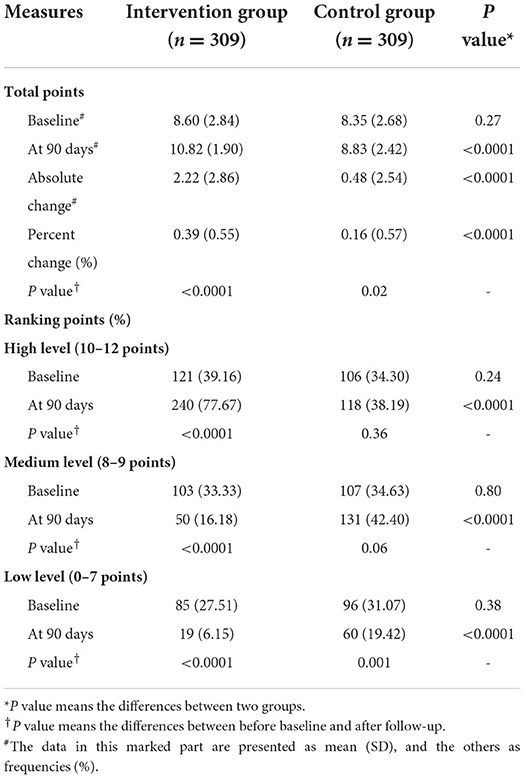
The knowledge, belief, behavior security and behavior compliance of rational medication use of elderly patients were all greatly improved in the intervention group at 90 days (P < 0.0001), which was statistically different compared with the control group (P < 0.0001), explaining the Rational Medication Management Mode had a positive effect on health education for elderly patients. Data on these measures are presented as the absolute change and percent change at 90 days from the baseline in Tables 6–9.
Discussion
With the acceleration of population aging and the changing in disease spectrum, the long-term medication demand of patients with chronic diseases is increasing (23). More practical research is required to evaluate the implementation effect of technology/tool-based mode and ensure they meet their potential and value in improving chronic disease management and rational medication use for patients (24).
The medication administration mode, which was widely used in countries with mature medication administration experience, comprised of drug administration tools, such as medication record form in the United States, the drug administration manual in Japan, etc., The effectiveness of medication management tools in improving patient compliance and health outcomes has been confirmed in relevant studies. A survey conducted by the Japanese Ministry of Health, Labor and Welfare showed that 50 ~ 90% of citizens of different ages were using the drug administration manual (25). A study has shown that the protocol-based pharmacotherapy management (PBPM) mode can effectively reduce the burden of doctors and nurses, and improve the safety of drug therapy for patients (26). Nevertheless, in the practice of medication management in China, there is a lack of tools to integrate patients' medication information. The existing medical records, health records, information systems, etc. are mostly used by medical staff, which is difficult to achieve joint records between doctors and patients, especially lacking ways for patients to report home medication situations. Based on the framework of medication record tools in the United States and Japan, and the medication management needs of the elderly, this study designed a tool of medication management manual for the elderly, which became the core technical support for the Rational Medication Management Mode.
Ensuring medication safety in polypharmacy is one of the key challenges for medication safety today. All stakeholders, including physicians, nurses, pharmacists, and even patients and their families, could have a vital role to play in driving change for the management of multiple drugs. Patients should be viewed as shared decision-makers on the use of medication, and health care professionals need to encourage and support patients and their families to disclose all the medications they are taking, including over-the-counter, traditional and complementary medicines, especially if they are suffering from multiple conditions and are being treated with polypharmacy (27–29). Family physicians and pharmacists should conduct medication reviews and medication reconciliation whenever possible in collaboration with the patient and their families, which has a positive impact on optimizing medicine use and improving health outcomes (30–32). The effect evaluation of this study found that after the implementation of Rational Medication Management Mode, the number of medications and the proportion of polypharmacy in the intervention group decreased significantly at 90 days, having a significant difference compared with the control group (P < 0.001).
Elderly chronic diseases and medication management need to pay attention to the establishment of an efficient interactive relationship with patients, strengthening the persistence of drug records and the self-management ability of patients (33–35). For example, family physicians and pharmacists help patients with complex medication regimens to clarify the usage and dosage of all kinds of drugs, reducing the occurrence of intermittent medication due to a variety of medications; patients are required to check the corresponding position after taking medication every day, helping to establish medication habits; dispensing into the pillbox can help patients take their medicines with them when they go out. The effect evaluation that, the proportion of elderly patients with medication reminders increased significantly, and the numbers of intermittent medication and ADR decreased significantly (P < 0.05).
If the elderly have weak awareness of rational drug use, it is hard to fully realize the value of medication management to improve their health status. Health education for patients plays a key role in the prevention and early detection of medication use and related health problems by raising their awareness of irrational drug use (4, 36–38). The knowledge-belief-behavior evaluation of rational medication use for patients can reflect the practical effect of the mode in health education (39). This study found that this mode can better improve patients' knowledge and belief in rational medication, and improve the security and compliance of medication behavior (P < 0.0001). It is worth noting that, for the evaluation of knowledge and behavior compliance, the proportion of low levels in the control group is significantly reduced compared with the baseline (P < 0.05), while there is no statistical difference in high levels. The evaluation of medication behavior security also showed a similar situation, the reduction degree of dangers level was greater than the improvement degree of the relatively safe level. This indicates that with the improvement of living standards and various health education, elderly patients began to enhance their awareness level of medication use, paying attention to knowledge learning and behavior improvement. However, in this process, it is difficult for elderly patients to find a scientific path of improvement by relying on their own experience and learning. Rational Medication Management Mode based on family physician services can help the elderly to learn drug use knowledge and adopt healthy behavior scientifically, and improve the long-term management efficiency of family physician teams, to maximize health effect gain and reduce the disease burden.
This study still has some limitations. First, some information on secondary outcomes was obtained through the self-reported questionnaire, which may constitute a reporting bias. However, this is likely to be an undifferentiated bias. Second, the experimental time of this study is short. And the mode needs certain application conditions, such as economically developed areas, mature family physician services, pharmacist equipment. However, after the effectiveness of this mode has been confirmed, we have begun to pilot promotion, and started to optimize the applicability of the mode, attempting to promote and apply it to other regions and key populations.
Conclusion
To sum up, this study constructed a Rational Medication Management Mode and carried out an empirical research to evaluate the implementation effect. The mode-based family physician service, which provides the support of manuals and pillboxes, can decrease the drug numbers of elderly patients with multimorbidity, reduce the incidence of polypharmacy, enhance behavioral self-management, increase the knowledge and belief of rational medication use, and improve the security and compliance of medication use behavior. In order to provide a practical basis for rational medication management of elderly patients with multimorbidity under the background of long-term prescriptions in China.
Data availability statement
The datasets presented in this article are not readily available because the datasets generated during and/or analyses during the current study are available from the authors on reasonable request. Requests to access the datasets should be directed to QT, dGFuZ3FpQGZ1ZGFuLmVkdS5jbg==.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of School of Public Health, Fudan University (International Registration Number: IRB00002408 & FWA00002399; approval number: IRB#2021-11-0931). The patients/participants provided their written informed consent to participate in this study.
Author contributions
JuL and GC conceived and designed the research and critically reviewed the manuscript. QT analyzed the data, wrote the initial manuscript and generated the tables and figures. LW revised the manuscript critically for important intellectual content. JiL, WW, and ZL helped in data collecting. SZ proofread the manuscript. CL supervised the research. All authors approved the final version of the paper and take responsibility for its content. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Major Project of National Social Science Foundation of China (Grant No. 17ZDA078), National Natural Science Foundation of China (Grant No. 72004030) and Policy Research Project of Shanghai Municipal Health Commission (Grant No. 2022HP53).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.992959/full#supplementary-material
References
1. Wang TC, Ku PJ, Lu HL, Hsu KC, Trezise D, Wang HY. Association between potentially inappropriate medication use and chronic diseases in the elderly. Int J Environ Res Public Health. (2019) 16:2189. doi: 10.3390/ijerph16122189
3. Wu JR, Chen QZ, Ye RL. Study on influencing factors of medication behavior in elderly patients. J Changgung Nurs. (2002) 13:166–74.
4. Molokhia M, Majeed A. Current and future perspectives on the management of polypharmacy. BMC Fam Pract. (2017) 18:70. doi: 10.1186/s12875-017-0642-0
5. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for healthcare, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/S0140-6736(12)60240-2
6. World Health Organization. Promoting Rational use of Medicines: Core Components. (2002). Available online at: https://apps.who.int/iris/bitstream/handle/10665/67438/WHO_EDM_2002.3.pdf (accessed March 12, 2022).
7. Baldwin JL, Singh H, Sittig D, Giardina TD. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other. Healthcare. (2017) 5:81–5. doi: 10.1016/j.hjdsi.2016.08.004
8. Pereira F, Gunten AV, Amoussou JR, Giorgi SID, Martins MM, Verloo H. Polypharmacy among home-dwelling older adults: the urgent need for an evidence-based medication management model. Patient Prefer Adherence. (2019) 13:2137–43. doi: 10.2147/PPA.S232575
9. Atkinson WL, Frey D. Integration of a medication management model into outcome-based quality improvement: a pilot program in a rural propriety home healthcare agency. Home Health Care Serv Q. (2005) 24:29–45. doi: 10.1300/J027v24n01_03
10. Prudencio J, Cutler T, Roberts S, Marin S, Wilson M. The effect of clinical pharmacist-led comprehensive medication management on chronic disease state goal attainment in a patient-centered medical home. J Manag Care Spec Pharm. (2018) 24:423–29. doi: 10.18553/jmcp.2018.24.5.423
11. Skinner JS, Poe B, Hopper R, Boyer A, Wilkins CH. Assessing the effectiveness of pharmacist-directed medication therapy management in improving diabetes outcomes in patients with poorly controlled diabetes. Diabetes Educ. (2015) 41:459–65. doi: 10.1177/0145721715587563
12. Murphy-Menezes M. Role of the pharmacist in medication therapy management services in patients with osteoporosis. Clin Ther. (2015) 37:1573–86. doi: 10.1016/j.clinthera.2015.03.023
13. Aitken M, Gorokhovich L. Advancing the Responsible use of Medicines: Applying Levers for Change. (2012). Available online at: https://ssrn.com/abstract=2222541 (accessed March 18, 2022).
14. General Office of the State Council of the People's Republic of China. Bulletin of the Seventh National Census. (2021). Available online at: http://www.gov.cn/guoqing/2021-05/13/content_5606149.htm (accessed April 06, 2022).
15. Yan W, Lu Y, Zhang Y, Chang F. Multimorbidity status of the elderly in China-research based on CHARLS data. Chin J Dis Control Prev. (2019) 23:426–30.
16. Wu HL, Ma XW, Wang N, Zhang WY. Progresses in researches on potentially inappropriate medication among elderly persons. Chin J Public Health. (2017) 33:324–27.
17. Mao JY, Liu LL, Pan YH. Enlightenment of American medication therapy management to Chinese pharmaceutical services. Drugs Clin. (2017) 32:2031–35.
18. China National Working Committee Office on Ageing. The Fourth Sample Survey on The Living Conditions of China's Urban and Rural Older Persons Datasets. Beijing: Xinhua Publishing House. (2018).
19. Tang Q, Wang C, Wu W, Cao Y, Chen G, Lu J. China should emphasize key issues inherent in rational medication management for the elderly. Biosci Trends. (2021) 15:262–5. doi: 10.5582/bst.2021.01254
20. Chisholm-Burns MA, SPivey CA, Tolley EA, Kaplan EK. Medication therapy management and adherence among US renal transplant recipients. Patient Prefer Adherence. (2016) 10:703–9. doi: 10.2147/PPA.S104646
21. Ma XQ. Study on the Situation of Illness and Medication of Elderly Patients With Chronic Disease in China. [dissertation/master's thesis].[Zhengzhou (HN)]: Henan University. (2015).
22. Chen XZ, Cai QF, Zhao E. Detection and evaluation of drug safety in community seniors. Univ Kang Ning J. (2019) 9:1–11.
23. Bao J, Zhou L, Liu G, Tang J, Lu X, Cheng C., et al. Current state of care for the elderly in China in the context of an aging population. Biosci Trends. (2022) 16:107–18. doi: 10.5582/bst.2022.01068
24. Schneider MP, Gertsch A, Bugnon O. Cyberhealth serving to support individual intake of medication. Swiss Med Wkly. (2013) 143:w13827. doi: 10.4414/smw.2013.13827
25. Tomoya T, Yoshihiro N. HitomiT. Literature review on the utilization of medication notebooks. Jpn J DrugInform. (2018) 20:1–11.
26. Bindu MA, Boban B, Karoor SA, Marimuthu K, Ramakrishnan SA, Xavier A. Medication therapy management (MTM): an innovative approach to improve medication adherence in diabetics. Drug Metab Pers Ther. (2016) 31:151–5. doi: 10.1515/dmpt-2016-0016
27. Richard C, Glaser E, Lussier MT. Communication and patient participation influencing patient recall of treatment discussions. Health Expect. (2017) 20:760–70. doi: 10.1111/hex.12515
28. Alpert PT, Gatlin T. Polypharmacy in older adults. Home Healthc Now. (2015) 33:524–9. doi: 10.1097/NHH.0000000000000299
29. Duerden M, Avery T, Payne R. Polypharmacy Medicines Optimization: Making it Safe Sound. London: The King's Fund. (2013). Available online at: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/polypharmacy-and-medicines-optimisation-kingsfund-nov13.pdf (accessed March 22, 2022).
30. Cutler DM, Everett W. Thinking outside the pillbox: medication adherence as a priority for health care reform. N Engl J Med. (2010) 362:1553–5. doi: 10.1056/NEJMp1002305
31. Hughes RG. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US). (2008).
32. Song P. Devoting attention to the management of community-acquired pneumonia for the elderly. Drug Discov Ther. (2020) 14:151–2. doi: 10.5582/ddt.2020.03055
33. Allegrante JP, Wells MT, Peterson JC. Interventions to support behavioral self-management of chronic diseases. Annu Rev Public Health. (2019) 40:127–46. doi: 10.1146/annurev-publhealth-040218-044008
34. Wei X, Zhang Z, Walley JD, Hicks JP, Zeng J, Deng S, et al. Effect of a training and educational intervention for physicians and caregivers on antibiotic prescribing for upper respiratory tract infections in children at primary care facilities in rural China: a cluster-randomised controlled trial. Lancet Global Health. (2017) 5:e1258–67. doi: 10.1016/S2214-109X(17)30383-2
35. Wei X, Zhang Z, Hicks JP, Walley JD, King R, Newell JN, et al. Long-term outcomes of an educational intervention to reduce antibiotic prescribing for childhood upper respiratory tract infections in rural China: follow-up of a cluster-randomised controlled trial. PLoS Med. (2019) 16:e1002733. doi: 10.1371/journal.pmed.1002733
36. Mair A, Fernandez-Limos F, Alonso A, Harrison C, Hurding S, Kempen T, et al. Polypharmacy Management by 2030: A Patient Safety Challenge, 2nd edition. (2017). Available online at: http://www.simpathy.eu/sites/default/files/Managing_polypharmacy2030-web.pdf (accessed April 19, 2022).
37. Norioka R, Tobisawa S, Nishigori R, Kuhara T, Yazaki M, Nagao M, et al. Saccharopinuria accompanied by hyperammonemia and hypercitrullinemia presented with elderly-onset epilepsy, progressive cognitive decline, and gait ataxia. Intractable Rare Dis Res. (2021) 10:126–30. doi: 10.5582/irdr.2021.01003
38. Shen L, Wang L, Liu C, Shi S, Takahashi T, Wang T. Community-acquired pneumonia: trends in and research on drug resistance and advances in new antibiotics. Biosci Trends. (2021) 15:266–75. doi: 10.5582/bst.2021.01342
Keywords: elderly, chronic disease, medication management, health education, family physicians, public health challenge
Citation: Tang Q, Wan L, Lu J, Wu W, Wu H, Liu Z, Zhao S, Li C, Chen G and Lu J (2022) Rational medication management mode and its implementation effect for the elderly with multimorbidity: A prospective cohort study in China. Front. Public Health 10:992959. doi: 10.3389/fpubh.2022.992959
Received: 13 July 2022; Accepted: 15 August 2022;
Published: 06 September 2022.
Edited by:
Qinghua Li, Guilin Medical University, ChinaCopyright © 2022 Tang, Wan, Lu, Wu, Wu, Liu, Zhao, Li, Chen and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Lu, bHVqdW5Ac2htdS5lZHUuY24=; Gang Chen, Z2NoZW5Ac2htdS5lZHUuY24=
†These authors have contributed equally to this work
 Qi Tang
Qi Tang Litao Wan1,2,3†
Litao Wan1,2,3† Sitang Zhao
Sitang Zhao