- 1Department of Pharmacy Practice, College of Pharmacy, Qassim University, Qassim, Saudi Arabia
- 2Department of Pharmacy Practice, College of Pharmacy, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
- 3Department of Clinical Pharmacy, College of Pharmacy, Taif University, Taif, Saudi Arabia
- 4Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
- 5Pharmacoeconomics Research Unit, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Background: Patients with prediabetes are at higher risk of developing type 2 diabetes. While intensive lifestyle modification is the primary approach to delaying diabetes, metformin has been shown to be effective, especially among patients younger than 60 years and obese (body mass index (BMI) > 35 kg/m2), patients with fasting blood glucose ≥ 6.1 mmol/L or HbA1c ≥ 6%, and women with history of gestational diabetes. Thus, metformin is now recommended as an option for diabetes prevention by the American Diabetes Association (ADA). The use of metformin among patients with prediabetes in Saudi Arabia and their adherence to the guideline's recommendation for the prevention of type 2 diabetes is unknown. This study aimed to identify the prevalence of metformin use among prediabetes patients overall and patients who are more likely to benefit from metformin use per the ADA guidelines.
Methods: A retrospective cohort study was conducted encompassing data from three tertiary care hospitals between January 2015 and June 2019. All patients aged 20 to 70 years with prediabetes (HbA1c of 5.7–6.4%) were included, while patients with an established diagnosis of diabetes, creatinine clearance <45 ml/min, using antihyperglycemic medications other than metformin, or on metformin for other indications were excluded. Prediabetes patients who are most likely to benefit from metformin for type 2 diabetes prevention are those younger than 60 years with a BMI ≥ 35 kg/m2, patients with fasting blood glucose ≥ 6.1 mmol/L or HbA1c ≥ 6%, and women with history of gestational diabetes. This study examined the prevalence of metformin use among all patients with prediabetes, as well as patients who would be more likely to benefit from metformin use per the ADA guidelines.
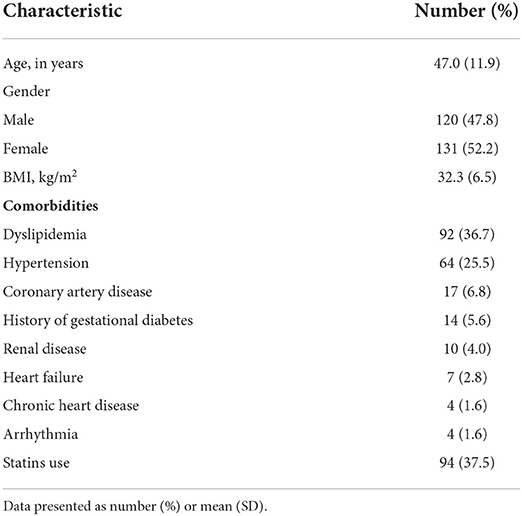
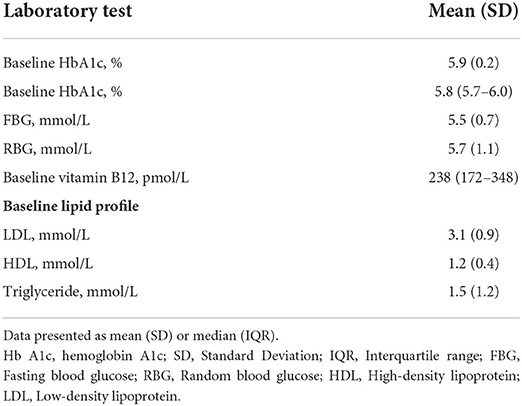
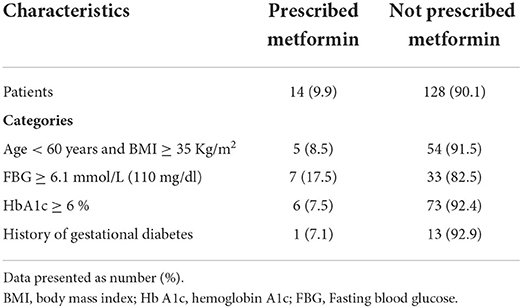
Results: A total of 251 patients were included in this study; 52.2% were female, with a mean age of 47.0 (11.9) years and BMI of 32.3 (6.5) kg/m2, and the median HbA1c at baseline was 5.8% (5.7–6.0). Among the overall sample, 18 patients (7.2%) received metformin for the prevention of type 2 diabetes, 14 of those were from the groups that are more likely to benefit from metformin use per the ADA guidelines (9.9%).
Conclusions: Among individuals with prediabetes in Saudi Arabia, metformin use was very low despite the evidence supporting its safety, convenience, and efficacy. Healthcare providers seemed hesitant to medicalize prediabetes; furthermore, the low use of metformin suggests the existence of several barriers that need to be identified and resolved. Increasing providers' knowledge and awareness regarding screening and management of prediabetes is highly encouraged.
Introduction
Patients with prediabetes are at a higher risk of developing type 2 diabetes (1). One major approach to delaying diabetes is through intensive lifestyle modifications that focus on weight loss and exercise (2, 3). The landmark trial of the diabetes prevention program (DPP) identified intensive lifestyle modification as the best intervention to delay the incidence of type 2 diabetes (2). Unfortunately, the translation of this experience outside the controlled setting of the clinical trial demonstrated inconsistent results (4, 5).
Although intensive lifestyle modification was shown to be superior to metformin in reducing the risk of diabetes (58 vs. 31%, respectively) in the DPP trial, metformin demonstrated a 53% reduction in the risk of diabetes among those who were obese, with a body mass index (BMI) of > 35 kg/m2, and younger than 60 years of age as well as women with a history of gestational diabetes compared to 51% with the intensive lifestyle modification (2). For metformin, the reduction in the incidence of type 2 diabetes compared to placebo was 31% in the DPP trial and 18% in 10-year and 15-year follow-up studies (2, 3). The standard of medical care in diabetes guidelines published by the American Diabetes Association (ADA) recommends the use of metformin as an option for diabetes prevention, especially among the aforementioned high-risk group (1). However, the use of metformin for this indication is off label according to the summary of product characteristics (SPC).
Despite the existing evidence, the use of lifestyle modifications and metformin for diabetes prevention remains underutilized (6–9). Mainous and colleagues found that lifestyle modifications or metformin were only initiated in 23% of patients with prediabetes (6, 7). Another study found that <5% of prediabetes patients were referred to lifestyle modification programs; furthermore, metformin was used in <1% of these patients. A related study found that among the eligible patients, only 7.8% received metformin (9). Several barriers to adopting a healthy lifestyle among people with obesity/newly diagnosed diabetes or prediabetes have been reported. For example, at the patient level, poor diet education, lack of adequate understanding of a healthy diet, lack of motivation, low socioeconomic status, emotional stress, presence of depression, and lack of symptoms have been reported to impact the initiation and maintenance of a healthy lifestyle. There are also factors at both physician and health system levels such as the limited resources, insufficient time for physicians, failure to identify patients' needs, hesitation to refer patients to other healthcare providers, limited integration of modern technologies, lack of a team-based approach, and limited community outreach (10). All those factors make it difficult for patients to adopt a healthy lifestyle.
The prevalence of prediabetes and type 2 diabetes in Saudi Arabia has been found to vary significantly in the available literature (11–13). Regardless of the true prevalence, type 2 diabetes remains a serious health issue that increases the burden on the Saudi healthcare system (14). The use of metformin among patients with prediabetes and their adherence to the clinical guidelines is unknown. Thus, in this study, we aimed to identify the prevalence of metformin use among prediabetes patients in three regions of Saudi Arabia, along with the prevalence of metformin use among patients with prediabetes who would be more likely to benefit from metformin use per the ADA guidelines.
Methods
Study design, setting, and participants
A retrospective cohort study was conducted, that considered data from three tertiary care hospitals in Saudi Arabia between January 2015 and December 2019. We included all patients aged 20 to 70 years with prediabetes (HbA1C of 5.7–6.4%) based on the ADA definition (15). Patients were excluded if they had an established diagnosis of diabetes, glomerular filtration rate or creatinine clearance < 45 ml/min, or were on antihyperglycemic medications other than metformin, as well as patients on metformin for other indications, such as polycystic ovary syndrome.
Data collection and outcome measures
Data collected from the electronic health records included demographic variables, BMI, comorbid conditions, laboratory values for HbA1c, fasting and random blood glucose (FBG and RBG, respectively), vitamin B12, and lipid profile at baseline, the follow-up value for HbA1c, and the name and strength of medications used by these patients—specifically, the use of metformin and statins—as well as the documentation of developing type 2 diabetes in the patient record. Prediabetes patients who are most likely to benefit from metformin for the prevention of type 2 diabetes are those aged < 60 years with BMI ≥ 35 kg/m2, patients with FBG ≥ 6.1 mmol/L or HbA1c ≥ 6%, and women with history of gestational diabetes. Thus, these factors were used to assess adherence to the ADA recommendations regarding the prevention of type 2 diabetes. The endpoints included the prevalence of metformin use among prediabetes patients overall and the prevalence of metformin use among patients who were more likely to benefit from metformin per the ADA guidelines.
Statistical analysis
Descriptive statistics, mean with standard deviation (SD) or median with interquartile range (IQR) and frequency with percentage (%) were used to describe continuous and categorical data, respectively. Patients' data were presented in tables based on the use of metformin according to the guidelines' recommendations: patients prescribed metformin and those not prescribed metformin. Data were collected and managed using Microsoft Excel, version 2010 (Microsoft Corp., Redmond, WA, USA), and all statistical analyses were conducted using the SAS® software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 251 patients with prediabetes were included in this study, of which 131 (52.2%) were female. The mean age of these patients was 47.0 (11.9) years, and their BMI was 32.3 (6.5) kg/m2. The most recorded comorbidity was dyslipidemia (36.7%), followed by hypertension (25.5%), and statin therapy was used in 37.5% of the sample (Table 1). The median HbA1c at baseline was 5.8% (5.7–6.0), and the mean FBG and RBG levels were 5.5 and 5.7 mmol/L, respectively (Table 2).
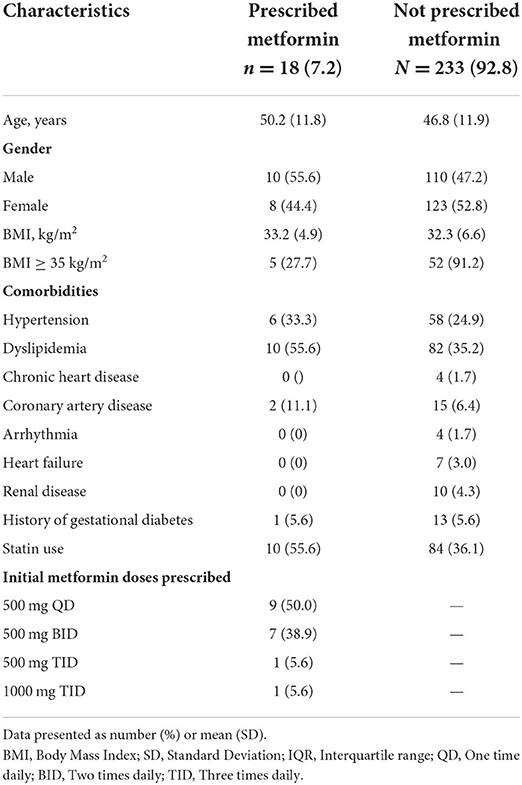
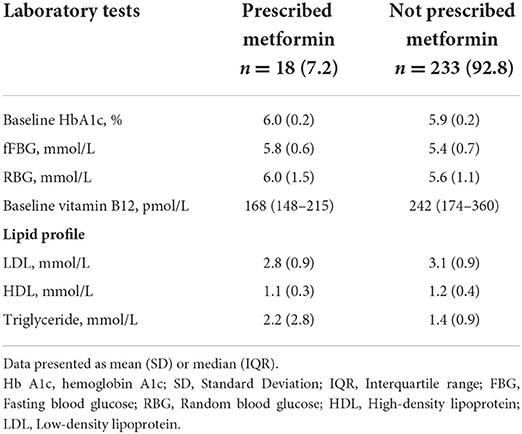
Among the entire sample of prediabetes patients, 18 (7.2%) received metformin for the prevention of type 2 diabetes (Table 3). Among those who received metformin, the most common comorbidities were dyslipidemia (55.6%), followed by hypertension (33.3%). The mean HbA1c, FBG, and RBG at baseline were 6.0%, 5.8 mmol/L, and 6.0 mmol/L, respectively, in those who received metformin, compared with 5.9%, 5.4 mmol/L, and 5.6 mmol/L in those who did not receive metformin (Table 4). The initial doses of metformin were 500 mg once daily in 9 patients (50%) and 500 mg twice a day in 7 patients (38.9%). Statins were used by 55.6% of these patients, compared to 36.1% of those who were not on metformin.
Regarding the group that was more likely to benefit from metformin and thus encouraged to receive metformin per the ADA recommendations, only 14 out of 142 patients (9.9%) received prescriptions for metformin. Among these, 17.5% of patients with FBG ≥ 6.1 mmol/L were prescribed metformin. In addition, only one out of 14 women with gestational diabetes were prescribed metformin (Table 5). Moreover, no clear trend toward the prescribing of metformin for diabetes prevention was observed during the study (Figure 1).
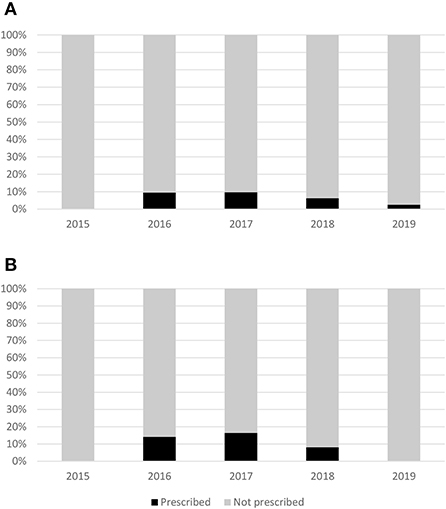
Figure 1. Trend of prescribing metformin for diabetes prevention for the overall population (A) and patients that are more likely to benefit from metformin (B).
Discussion
Although type 2 diabetes remains a serious health issue that increases the burden on the Saudi healthcare system, the use of metformin among patients with prediabetes is unknown. This study was conducted to identify the prevalence of metformin use among an overall sample of prediabetes patients and patients who were more likely to benefit from metformin use per the ADA guidelines. The prevalence of metformin use was only 7.2% in the overall sample and 9.9% among the subgroup of high-risk patients who were more likely to benefit from receiving metformin, based on the current evidence and the ADA guidelines' recommendations. Our study, which included individuals with prediabetes from three regions in Saudi Arabia, found metformin to be underused.
The observed underutilization of metformin for the prevention of type 2 diabetes is similar to the findings of two previous observational studies (8, 9). Schmittdiel and colleagues found that metformin was initiated in <1% of identified patients with prediabetes. Notably, the study included patients with confirmed prediabetes diagnoses between 2006 and 2010 (8). The ADA guidelines first began to recommend metformin as an option for diabetes prevention in 2008 (16). This timing might explain the extremely low rate of metformin use along with the use of data from a single electronic health record. Meanwhile, Moin et al. reported that 3.7% of working, insured adults with prediabetes received metformin. Moreover, in the subcategory of patients with a BMI of more than 35 kg/m2 or who had a history of gestational diabetes, 7.8% of patients received metformin. That study used a nationwide database for a large insurer in the United States that included data for working employees between 2010 and 2012 (9).
Research has shown that metformin is safe, convenient, and cost-effective when used for the prevention of type 2 diabetes (17, 18). For example, one metanalysis revealed the absolute risk reduction observed with metformin use ranged from 4.4 to 14.3% (17). From the population perspective, such numbers are critical in the case of a disease with a high prevalence, such as type 2 diabetes. Moreover, in a recent systematic review by Moin et al. the researchers suggested that metformin might be associated with higher absolute risk reduction, especially among certain higher-risk patients, such as those who were morbidly obese, as well as patients with higher HbA1c or Impaired FBG values (19). The difficulty in implementing lifestyle modification-based programs into real practice increases the importance of using metformin for diabetes prevention, at least among high-risk patients who are more likely to benefit from the use of metformin. Unfortunately, the low use of metformin indicates the existence of several barriers to implementing this approach.
As suggested by Moin et al. the lack of eligibility criteria as to who should receive metformin might have been an important challenge (19), especially since patients with prediabetes vary in their risk for developing type 2 diabetes. Health care providers' knowledge regarding prediabetes screening and treatment might be another barrier. Tseng et al. surveyed primary care providers to assess their knowledge of screening and managing prediabetes. The study findings revealed that only 6% managed to identify the correct risk factors to warrant prediabetes screening; in addition, only 11% of the primary health care providers mentioned that they would refer patients with prediabetes to a weight-loss program. moreover, only 17% managed to identify the correct lab values for diagnosing prediabetes (20). This study highlights a critical barrier that needs to be addressed, especially in primary care settings.
In Saudi Arabia, a study has been carried out to assess physicians' knowledge and attitudes regarding screening, diagnosing, or managing prediabetes (21). In that study, 115 primary care physicians (pcps) participated in a national survey. the study authors reported that only 27% of the study participants were aware of the risk factors for prediabetes. in addition, only 55.5 and 43.6% of the participants were aware of the HbA1c and FBG levels, respectively, for the diagnosis of prediabetes. Around 11.0% of the participating PCPs reported the use of metformin in more than half of their prediabetes patients. However, the participants were not asked about reasons for not starting metformin; that said, it is possible that the lack of an FDA indication for diabetes prevention on the metformin label and the possible side effects that might be associated with metformin use might have affected health care providers' attitudes toward prescribing metformin.
In order to overcome the previously mentioned barriers, it is highly recommended to educate health care providers about the screening and management of prediabetes. Increasing health care providers' knowledge regarding risk factors, diagnostic criteria, and the clinical guidelines' recommendations will promise great benefit, especially in primary care settings. Furthermore, healthcare institutions should develop clear criteria on who should be screened for diabetes; institutions should also have a clear eligibility criterion in place regarding who should receive metformin along with lifestyle modifications. Developing a simplified protocol for the use of primary care providers that includes metformin dosage instructions, monitoring, and patient education might help encourage physicians to medicalize prediabetes. In addition, patient-related factors that might hinder managing prediabetes can be overcome by increasing patients' awareness of diabetes prevention, and the benefits of lifestyle modification, and metformin might aid in these patients' acceptance of such interventions for prevention. Physicians' lack of time and limited staffing resources might be overcome by including clinical pharmacists as part of the multidisciplinary team in ambulatory care settings, which can play a vital role in the initiation and monitoring of metformin.
Although metformin is considered a very safe medication, it has some side effects, such as gastrointestinal disorders and B12 deficiency, that may hinder the prescribing or use of this medication as a protective measure (22). In addition, lactic acidosis is a rare side effect but it could occur with the chronic use of metformin, especially in patients with renal impairment (22). While the use of metformin can reduce the incidence of type 2 diabetes, it is still unclear whether the early introduction of metformin in patients with prediabetes may affect some of the patient outcomes in later stages, such as cardiovascular diseases or mortality (22). Thus, the lack of evidence about metformin's benefits on those outcomes might hinder its initiation by some healthcare providers (22). Therefore, the results of the ongoing VA-IMPACT study, investigating the potential impact of metformin vs. placebo among people with prediabetes on atherosclerotic cardiovascular disease and mortality might provide insight into the issue (23). Besides that, there is emerging evidence that new antidiabetic agents (SGLT2i and GLP-1 RA) may have favorable effects on the risk of progression of prediabetes to diabetes (24, 25). An exploratory analysis from DAPA-HF showed that the use of dapagliflozin in patients with heart failure reduces the incidence of new diabetes by 32% (24). Furthermore, in the SCALE obesity and prediabetes trial, the use of liraglutide among patients with prediabetes and obesity showed a reduction in the risk of diabetes during follow-up (25).
The overall small sample size included in this study is a limitation that must be noted. This aspect of the study might be a result of the low screening rate for diabetes overall, especially among the youthful segment of the population. The retrospective design of this study also imposes some limitations that must not be overlooked. The results of this study should be interpreted with caution, as only three regions of the country were included; thus, the findings from the study may not be generalized to other regions in Saudi Arabia. Also, larger study that include more regions are needed to assess the situation at the country level. Data regarding lifestyle modifications and referral to lifestyle modification-based programs were not reported in the database; thus, it was not clear whether patients were given these interventions in addition to metformin. Although this investigation represents the first multicenter study to address the rate of metformin use for diabetes prevention in Saudi Arabia, additional and larger studies are needed to investigate the reasons behind the low level of adherence to this guideline-based recommendation.
Conclusion
Among Saudi individuals with prediabetes, metformin use was very low despite the evidence supporting its safety, convenience, and efficacy. Health care providers seem to be hesitant to medicalize prediabetes, and the low use of metformin suggests the existence of possible barriers. increasing health care providers' knowledge and awareness regarding the screening and management of prediabetes is highly encouraged. The Ministry of Health, along with other healthcare settings and policymakers in saudi arabia, can utilize the results of this study to further promote the incorporation of evidence-based diabetes preventive measures into real-world practice, including referral of all patients to life style modification program and the use of metformin for patients who are more likely to benefit from it according to the ADA recommendations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board at King Abdullah International Medical Research Center. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
OMA, MA, and OAA contributed to the conception and design of this study. OAA conducted the statistical analysis and wrote the section Methods with inputs from OMA, MA, and OSA. AAA, AFA, FA, and OA-A did the data collection and wrote the section Results. OMA is the guarantor of this work. All authors contributed to writing the manuscript and revised and approved the final version of the manuscript.
Funding
This research was funded by the Researcher Supporting Project (RSP-2021/77), King Saud University, Riyadh, Saudi Arabia.
Acknowledgments
The authors would like to extend their appreciation to King Saud University for funding this work through the Researcher Supporting Project (RSP-2021/77), King Saud University, Riyadh, Saudi Arabia.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Prevention or delay of type 2 diabetes and associated comorbidities: standards of medical care in diabetes-2022. Diabetes Care. (2022) 45(Suppl. 1):S39–45. doi: 10.2337/dc22-S003
2. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. (2002) 346:393–403. doi: 10.1056/NEJMoa012512
3. Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. (2009) 374:1677–86. doi: 10.1016/S0140-6736(09)61457-4
4. Cardona-Morrell M, Rychetnik L, Morrell SL, Espinel PT, Bauman A. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? a systematic review and meta-analysis. BMC Public Health. (2010) 10:653. doi: 10.1186/1471-2458-10-653
5. Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff (Millwood). (2012) 31:67–75. doi: 10.1377/hlthaff.2011.1009
6. Mainous AG 3rd, Tanner RJ, Baker R. Prediabetes diagnosis and treatment in primary care. J Am Board Fam Med. (2016) 29:283–5. doi: 10.3122/jabfm.2016.02.150252
7. Mainous AG 3rd, Tanner RJ, Scuderi CB, Porter M, Carek PJ. Prediabetes screening and treatment in diabetes prevention: the impact of physician attitudes. J Am Board Fam Med. (2016) 29:663–71. doi: 10.3122/jabfm.2016.06.160138
8. Schmittdiel JA, Adams SR, Segal J, Griffin MR, Roumie CL, Ohnsorg K, et al. Novel use and utility of integrated electronic health records to assess rates of prediabetes recognition and treatment: brief report from an integrated electronic health records pilot study. Diabetes Care. (2014) 37:565–8. doi: 10.2337/dc13-1223
9. Moin T, Li J, Duru OK, Ettner S, Turk N, Keckhafer A, et al. Metformin prescription for insured adults with prediabetes from 2010 to 2012: a retrospective cohort study. Ann Intern Med. (2015) 162:542–8. doi: 10.7326/M14-1773
10. Koufakis T, Kotsa K, Papanas N. Remission of type 2 diabetes depends on prompt comprehensive lifestyle changes upon diagnosis: How can this “Road to Damascus” experience be supported? J Integr Med. (2022) 20:288–91. doi: 10.1016/j.joim.2022.04.001
11. Al-Rubeaan K, Al-Manaa H, Khoja T, Ahmad N, Al-Sharqawi A, Siddiqui K, et al. The Saudi abnormal glucose metabolism and diabetes impact study (SAUDI-DM). Ann Saudi Med. (2014) 34:465–75. doi: 10.5144/0256-4947.2014.465
12. Bahijri SM, Jambi HA, Al Raddadi RM, Ferns G, Tuomilehto J. The prevalence of diabetes and prediabetes in the adult population of Jeddah, Saudi Arabia: a community-based survey. PLoS ONE. (2016) 11:e0152559. doi: 10.1371/journal.pone.0152559
13. Aldossari KK, Aldiab A, Al-Zahrani JM, Al-Ghamdi SH, Abdelrazik M, Batais MA, et al. Prevalence of prediabetes, diabetes, and its associated risk factors among males in Saudi Arabia: a population-based survey. J Diabetes Res. (2018) 2018:2194604. doi: 10.1155/2018/2194604
14. Alhowaish AK. Economic costs of diabetes in Saudi Arabia. J Family Community Med. (2013) 20:1–7. doi: 10.4103/2230-8229.108174
15. Association AD. Introduction: Standards of Medical Care in Diabetes−2022. Diabetes Care. (2021) 45(Suppl. 1):S1–2. doi: 10.2337/dc22-Sint
16. Association AD. Standards of Medical Care in Diabetes−2008. Diabetes Care. (2008) 31(Suppl. 1):S12–54. doi: 10.2337/dc08-S012
17. Lily M, Godwin M. Treating prediabetes with metformin: systematic review and meta-analysis. Can Fam Physician. (2009) 55:363–9.
18. Long-term safety tolerability and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care. (2012) 35:731–7. doi: 10.2337/dc11-1299
19. Moin T, Schmittdiel JA, Flory JH, Yeh J, Karter AJ, Kruge LE, et al. Review of metformin use for type 2 diabetes prevention. Am J Prev Med. (2018) 55:565–74. doi: 10.1016/j.amepre.2018.04.038
20. Tseng E, Greer RC, O'Rourke P, Yeh HC, McGuire MM, Clark JM, et al. Survey of primary care providers' knowledge of screening for, diagnosing and managing prediabetes. J Gen Intern Med. (2017) 32:1172–8. doi: 10.1007/s11606-017-4103-1
21. Aljehani F, Alsulaiman A, Alqarni A, Almutairi F, Samkari M. Survey of primary care physicians' screening and treatment practices for prediabetes in saudi Arabia. Cureus. (2022) 14:e21475. doi: 10.7759/cureus.21475
22. Aroda VR, Ratner RE. Metformin and type 2 diabetes prevention. Diabetes Spectrum. (2018) 31:336–42. doi: 10.2337/ds18-0020
23. Investigation of metformin in pre-diabetes on atherosclerotic cardiovascular outcomes (VA-IMPACT). Available online at: https://clinicaltrials.gov/ct2/show/NCT02915198 (accessed August 11, 2022).
24. Inzucchi SE, Docherty KF, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, et al. Dapagliflozin and the incidence of type 2 diabetes in patients with heart failure and reduced ejection fraction: an exploratory analysis from DAPA-HF. Diabetes Care. (2020) 44:586–94. doi: 10.2337/dc20-1675
25. le Roux CW, Astrup A, Fujioka K, Greenway F, Lau DCW, Van Gaal L, et al. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet. (2017) 389:1399–409. doi: 10.1016/S0140-6736(17)30069-7
Keywords: prediabetes, diabetes prevention, metformin, type 2 diabetes, observational study
Citation: Alfayez OM, Alsallum AA, Aljabri AF, Almutairi FS, Al-Azzeh O, Almalki OS, Al Yami MS and Almohammed OA (2022) The use of metformin for type 2 diabetes prevention: Observational multicenter study from Saudi Arabia. Front. Public Health 10:989072. doi: 10.3389/fpubh.2022.989072
Received: 08 July 2022; Accepted: 19 August 2022;
Published: 08 September 2022.
Edited by:
Elaine Chow, The Chinese University of Hong Kong, ChinaReviewed by:
Roch A. Nianogo, University of California, Los Angeles, United StatesTheocharis Koufakis, Aristotle University of Thessaloniki, Greece
Copyright © 2022 Alfayez, Alsallum, Aljabri, Almutairi, Al-Azzeh, Almalki, Al Yami and Almohammed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Osamah M. Alfayez, b2FsZmF5ZXpAcXUuZWR1LnNh
 Osamah M. Alfayez
Osamah M. Alfayez Alanoud A. Alsallum2
Alanoud A. Alsallum2 Ola Al-Azzeh
Ola Al-Azzeh Ohoud S. Almalki
Ohoud S. Almalki Majed S. Al Yami
Majed S. Al Yami Omar A. Almohammed
Omar A. Almohammed