- 1Department of Operating Room, Qilu Hospital of Shandong University, Shandong University, Jinan, China
- 2Center for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 3National Health Commission of China, Key Laboratory of Health Economics and Policy Research, Shandong University, Jinan, China
Background: In recent decades, the prominence of medical errors (MEs) and adverse events (AEs) is fueled by several studies performed across the world. Correspondingly, a high prevalence of medical errors and adverse events have been reported. Operating room nurses (ORNs) were indispensable members of the operating process, and any kind of MEs or AEs from ORNs may cause serious results and even death to the patients. However, to the best of our knowledge, the prevalence and associated factors of MEs and AEs were never reported among ORNs in China, which is the largest country in population and health services quantity in the world.
Methods: This is a cross-sectional study, which was conducted among ORNs in China, and 787 valid questionnaires were analyzed in this study. MEs, AEs, gender, age, married status, religious belief, academic degree, manager or not, working years, working hours/week, physical disease, and mental health were evaluated in this study. MEs were evaluated by eight questions about the occurrence of eight kinds of MEs for the ORNs. For ORNs with MEs, further questions about clinical harm to the patients were interviewed, which analyzed AEs. Kessler 10 was used to evaluate the ORNs' mental health. Logistic regression was conducted to examine the factors associated with MEs and AEs.
Results: The prevalence of MEs and AEs was 27.7 and 13.9% among ORNs, respectively. The most frequent MEs that occurred among ORNs were from surgical instruments (9.1%), disinfection (9.0%), equipment and consumables (8.9%), and specimen management (7.8%). MEs were positively associated with lower working years, poor mental health, and physical disease. The physical disease was positively associated with AEs.
Conclusion: The prevalence of perceived MEs and AEs was at a higher level than other kinds of nurses. Fresh ORNs with physical and mental health problems were the risk population for MEs, and ORNs with physical disease were at a higher risk for AEs. All the findings implied that MEs and AEs were an important issue for ORNs, and ORNs with physical and mental health problems should be paid attention to control MEs and AEs.
Introduction
Medical errors (MEs) are defined as an incidence when there is an omission or commission in planning or execution that leads or could lead to unintended results (1), and adverse events (AEs) are a type of injury that most frequently is due to an error in medical or surgical treatment rather than the underlying medical condition of the patient (2). In recent decades, the prominence of MEs and AEs is fueled by several studies around the world, which reported a high prevalence of MEs and AEs (3–6). Although both MEs and AEs are inevitable because of imperfect humans (7), controlling MEs and AEs is a fundamental work to protect patient safety.
In the United States (US), MEs were the third leading cause of death (8). However, when we reviewed the studies regarding MEs in China, only a few studies reported the prevalence of MEs among emergency department nurses (9) and medical professionals (10). Regarding AEs in China, most studies focused on the AEs caused by some specific technologies and treatments (11–13). To the best of our knowledge, the prevalence of AEs among medical professionals was less reported in China. As we know, China is the largest country in population and health services quantity in the world (14), and studies about the prevalence and related factors of MEs and AEs were urgent to be conducted in China.
In recent decades, the operation has been one kind of important treatment for patients in the world. Operating room nurses (ORNs), as indispensable members of the operating process, often need to handle urgent situations, such as life-threatening, immediate decision-making. Any kind of MEs from ORNs may cause serious results and even death of the patients (15). However, to the best of our knowledge, the prevalence and associated factors of MEs and AEs were never reported among ORNs in China.
We should know that many previous studies had given us much information about the prevalence of MEs among nurses (16, 17), and many factors were also supported to be associated with MEs for nurses, such as occupational burnout (18), physical and mental health (19), and fatigue (20, 21). However, the differences between ORNs and other kinds of nurses should be considered when we interpret these findings. First, with the high-speed development of operation technologies, ORNs need to learn more new skills than other kinds of nurses. The non-proficient skills in the new technologies may cause them at a higher risk of MEs (22, 23). Second, with the higher concentration on the operating process, ORNs were also at higher risk of physical health than hospitalization nurses (24), which was also a risk factor for MEs (25). Further considering the possible serious outcomes of MEs caused by ORNs, MEs and AEs among ORNs should be explored.
As we introduced before, the prevalence and associated factors of MEs and AEs among ORNs were less reported in China. To fill this gap, we conducted a cross-sectional study among ORNs in China. The main aims of this study were to explore the prevalence and related factors of MEs and AEs among ORNs in China. It not only was helpful for us to learn the prevalence and related factors of MEs and AEs among ORNs in China but also could provide evidence to control MEs and AEs among ORNs in China and some other countries in the world.
Methods
Participants and data collection
This is a cross-sectional study conducted among operating room nurses (ORNs) from December 2021 to January 2022 in China. First, the online questionnaire was sent to three nursing supervisors who worked in the operating rooms of three hospitals. Second, they were asked to post the online questionnaire on the different Wechat groups regarding ORNs. Nurses working in the operating room were invited to fill out the online questionnaire anonymously after they agreed on the informed consent. A strict logical check was set for this online questionnaire to avoid logical problems and missing data. Finally, the online questionnaire was clicked 1,256 times during the survey period, and 787 eligible questionnaires were collected in this study with a completion rate of 62.7% (787/1,256).
Ethics approval and consent to participate
The institutional review board of Shandong University School of Public Health approved the study protocol before data collection. Informed consent was obtained from all participants of the study. All methods were performed in accordance with the Declaration of Helsinki.
Measures
Self-reported medical errors and adverse events
Self-reported medical errors (MEs) were evaluated by eight questions, which investigated the occurrence of eight kinds of MEs for the ORNs in this study. The eight kinds of MEs were about patients or body parts, medication or blood transfusion, specimen management, surgical instruments, equipment and consumables, disinfection, implantable device, and others. For each question, the answers can be chosen from yes or no. In this study, ORNs without any kinds of MEs were coded as without self-reported medical errors (NME), and other ORNs with any positive answers were coded as with self-reported medical errors (YME). For ORNs with MEs, we further asked them if these errors caused clinical harm to the patients, which can be defined as adverse events (AEs) (2). ORNs with MEs responded the negative answers were coded as medical errors without clinical harm (MENH).
Social-demographic variables
In this study, the analyzed social-demographic variables included gender, age, married status, religious belief, and academic degree. Gender was coded as male (1) and female (0). Age was analyzed as a continuous variable by the ORNs' years old. Married status was evaluated by one question about the married status for the ORNs. The answers were single, married, divorced, widowed, and others. As there was a small percentage for the last three answers, we recorded it into ever married (1) and never married (0), which the last one contained the last four answers. Religious belief was coded as yes (1) and no (0). The academic degree was evaluated by one question about the highest degree, that the ORNs obtained. The answers were doctors, master, bachelor, junior college, technical secondary school, and others. As most of the ORNs obtained a bachelor's degree, we recorded it as a bachelor's or above (1) and below bachelor's (0).
Work-related variables
The work-related variables analyzed in this study contained the professional title, manager, working years, and working hours/week. The professional title was coded as senior (3), medium (2), and junior (1). The manager was evaluated by the question “do you have a management position in their worked hospitals.” Working years were measured by the years they worked in their hospitals. Working hours per week were calculated by two questions about the working day per week and averaged working hours per day.
Mental health
Mental health was measured by the Chinese version of the Kessler 10 (K10) scale (26). The Chinese version of K10 was also identified with nice reliability and validity in different populations (27, 28). In the K10 scale, there were 10 items with a 5-point Likert-type response. It was also translated and used to measure mental health and psychological distress in different countries (29, 30). The Cronbach's alpha of K10 in this study was 0.964.
Physical disease
The physical disease was evaluated by the question “Were you diagnosed with any kinds of physical diseases?” The answers could be chosen from yes (1) and no (0).
Statistical analysis
In this study, IBM SPSS Statistics 24.0 (Web Edition) was used to analyze the data. Student t-tests or Chi-square tests were performed to compare the differences between ORNs with or without MEs and AEs. Logistic regression was further conducted to examine the factors associated with MEs and AEs. All the tests were two-tailed, and a p < 0.05 was considered statistically significant.
Results
Totally, 787 ORNs finished the questionnaires in this study. Detailed information could be found in the second column of Table 1. In this table, single analyses were also conducted to analyze the factors associated with MEs, and the results supported that the associated factors of MEs were working hours/week (t = 2.76, p < 0.01), mental health (t = 3.35, p < 0.001), and physical disease (χ2 = 20.91, p < 0.001) among ORNs. For the differences between AEs and NMEs, the same factors with MEs were supported. Working hours/week (t = 2.58, p < 0.01), mental health (t = 2.48, p < 0.05), and physical disease (χ2 = 12.15, p < 0.001) were also associated with AEs. However, when we compared the differences between AEs and MENH, all the analyzed factors were not statistically significant (p > 0.05). The detailed information is shown in the last three columns of Table 1.
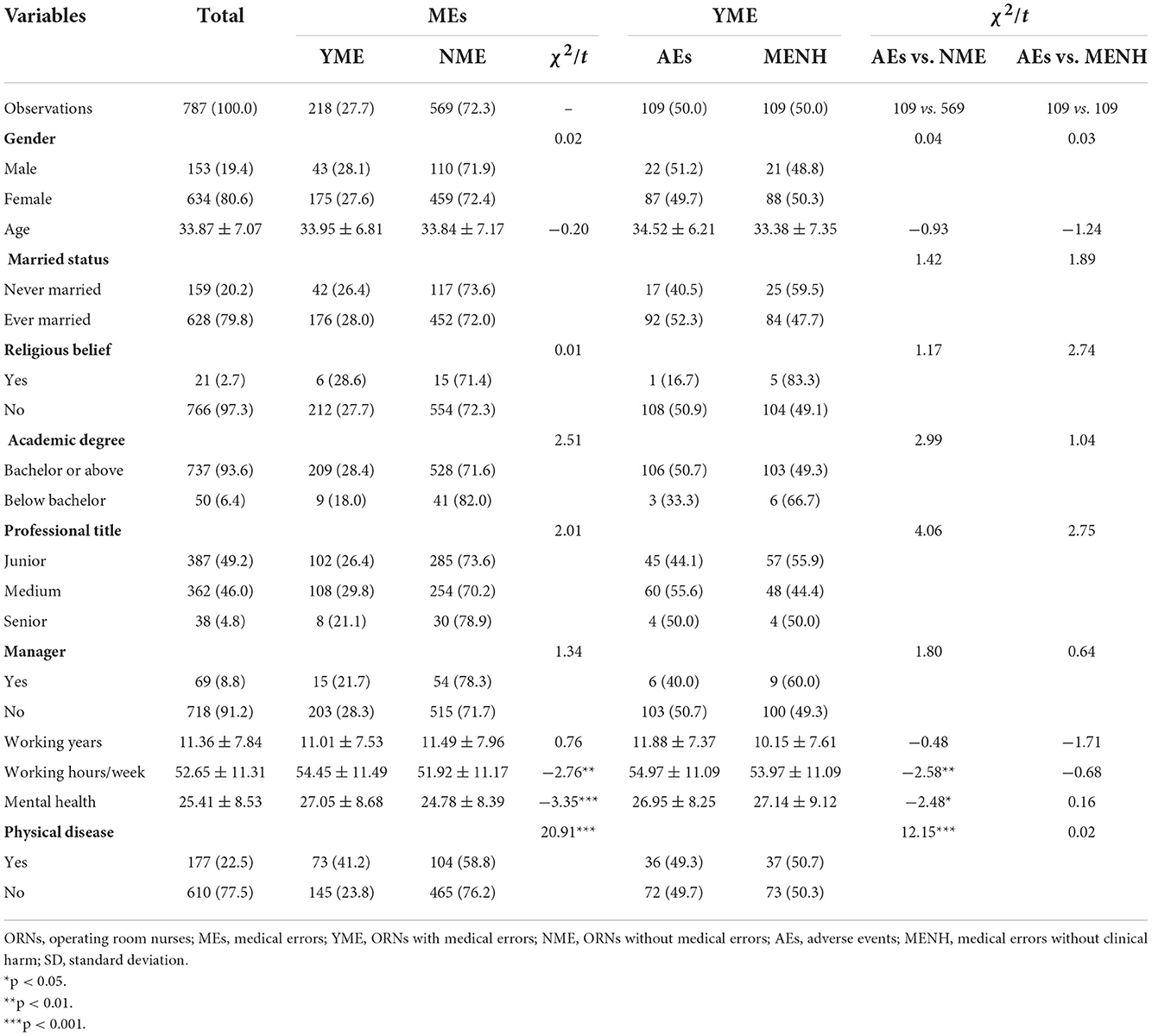
Table 1. Sample characteristics and single analyses for the factors associated with MEs and AEs among ORNs [n (%)/Mean ± SD].
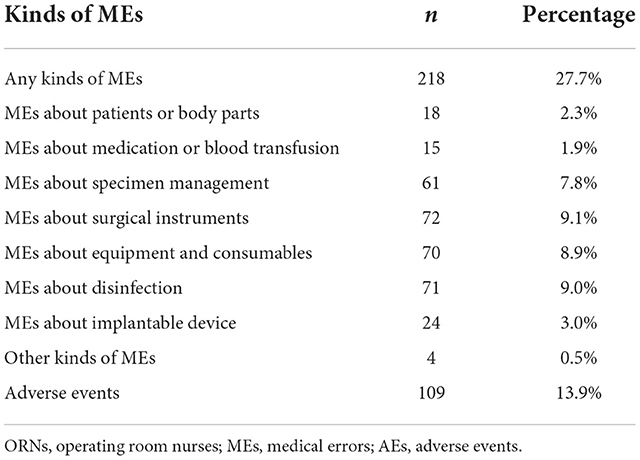
The prevalence of different kinds of MEs and AEs is shown in Table 2. In this table, we could find that 27.7% (218/787) of ORNs reported MEs. Among these ORNs with MEs (218 ORNs), 50.0% of ones (109/218) reported the experience of AEs, and the prevalence of AEs among ORNs was 13.9% (109/787). We also analyzed the percentage of different kinds of MEs. The results showed that the prevalence of MEs in patients or body parts, medication or blood transfusion, specimen management, surgical instruments, equipment and consumables, disinfection, implantable device, and others were 2.3, 1.9, 7.8, 9.1, 8.9, 9.0, 3.0, and 0.5%, respectively.
In Table 3, logistic regressions were further conducted to analyze the factors associated with MEs and AEs. The results showed that MEs were positively associated with lower working years (OR = 0.94, p < 0.01), poor mental health (OR = 1.02, p < 0.001), and physical disease (OR = 2.14, p < 0.001). When we compared the difference between AEs and NME, only physical disease (OR = 1.89, p < 0.01) was positively associated with AEs. However, any analyzed factors were not supported to be associated with MEs (p > 0.05), compared with MENH.
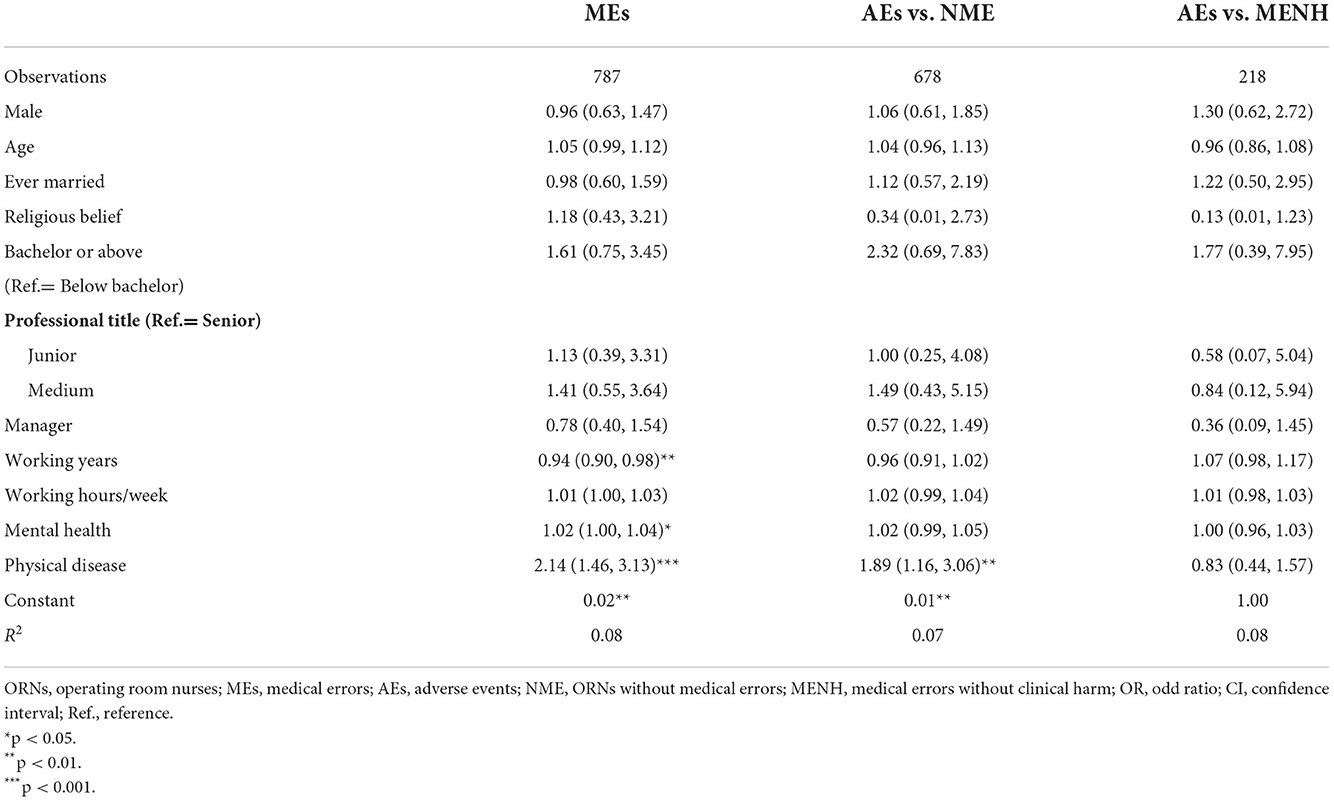
Table 3. Logistic regressions for the factors associated with medical errors and adverse events among ORNs [OR (95% CI)].
Discussion
In this study, our main aims were to analyze the prevalence and associated factors of MEs and AEs among ORNs in China, and there were several critical findings in this study. First, the prevalence of MEs and AEs was 27.7 and 13.9% among ORNs, respectively. Second, MEs about surgical instruments, disinfection, equipment and consumables, and specimen management were the most frequent errors that occurred among ORNs. Third, factors associated with MEs were lower working years, poor mental health, and physical disease among ORNs. Fourth, the physical disease was positively associated with the occurrence of AEs, and no statistically significant factors were supported between AEs and MENH among ORNs experienced with MEs.
We found that the prevalence of MEs was 27.7% among ORNs. As we know, the reported prevalence of MEs among nurses varied from 37 to 50% in different countries (31–33), which was higher than our findings. The different prevalence of MEs in different countries may be explained by the different healthcare systems and quality (34–36). In China, to our knowledge, this is the first study, which explored the prevalence of MEs among ORNs. However, compared with other kinds of nurses, our findings were similar to the previous findings among emergency department nurses (25.28%) (9) but higher than the findings among the nurses in other departments (17, 37). The higher prevalence of MEs among ORNs and emergency department nurses may be explained by the complicated and urgent work among ORNs and emergency department nurses, which were risk factors for MEs (32, 38).
For the prevalence of AEs among ORNs, we found that 13.9% of ORNs reported the experience of AEs. A study conducted among nursing students found the incidence of AEs was 17.8% (39). In other countries, several studies reported a high prevalence of AEs. In Turkey, a study showed that the prevalence of AEs was 37.3% (40), and the prevalence varied from 51.2 to 63.0% in Iran (41). The main reason for the different prevalence may be caused by the different definitions of AEs in previous studies. In these studies, AEs included all the injury events to patients, and they did not consider if these events were caused by MEs, and MEs were also included in AEs in these studies. The other reason may be caused by the difference between operating room and other departments. Although AEs caused by ORNs may result serious outcomes, the prevalence of AEs may be in lower level. Because nurses in other departments need to serve the patients in a longer time, which is a risk factor for AEs (42).
We also found that lower working years, poor mental health, and physical disease were positively associated with MEs among ORNs. Actually, all these factors were also supported by other kinds of medical professionals in previous studies (43–46), which further reminded us that we should pay attention to fresh ORNs with physical and mental health problems. The reasons may be that ORNs with physical and mental health problems cannot fully engage with patients or the operating process. One of the interesting findings was that working years were not associated with medical errors. Previous supported that burnout was not associated with medical errors (47). Working years, an important factor associated with burnout (48), may also not be associated with medical errors because of the weak association between MEs and burnout. Social-demographic variables were also not associated with MEs, which was also supported in a previous review study (49).
For the associated factors of AEs, we found that physical disease was positively associated with the occurrence of AEs. However, when we compared AEs and MENH among ORNs experienced with MEs, no statistically significant factors were supported. The reasons for the association between physical disease and AEs were similar to the explanation about MEs, which were also supported in other studies (50). The association between social-demographic variables, mental health, and AEs were not supported in this study, it may be caused by the small sample size of ORNs with AEs. Similar reasons also can explain why no factors were supported for the differences between AEs and MENH in this study.
There were also some limitations when we interpret the findings in this study. First, as this is a cross-sectional study, we cannot get any causal relationships between the associated factors and MEs. Second, MEs, AEs, and all the factors analyzed in this study were collected by self-report, and some bias cannot be avoided. For example, some ORNs did not want to report their MEs and AEs (51, 52), and the prevalence of MEs and AEs may be underestimated in this study. Third, the factors analyzed in this study included social-demographic characteristics, worked-related variables, physical disease, and mental health. Although we considered these factors, and there were many factors, which were not analyzed in this study, such as occupational stress (53), patient safety culture (54). In further studies, some other factors should be explored to make a comprehensive understanding of MEs and AEs among ORNs.
Conclusion
The prevalence of perceived MEs and AEs was at a higher level than other kinds of nurses. Fresh ORNs with physical and mental health problems were the risk population for MEs, and ORNs with the physical disease were at a higher risk for AEs. All the findings implied that MEs and AEs were an important issue for ORNs, and ORNs with physical and mental health problems should be paid attention to control MEs and AEs. Some strategies or policies should be applied to protect the ORNs' health status, which may also play positive roles in patient safety.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of School of Public Health, Shandong University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
QS analyzed the data and drafted the manuscript. JT and ZW collected the data and commented on the draft of this manuscript. LS designed the study and revised the draft. All authors read and approved the final manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (71974114). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgments
We would like to thank all the participants for their participation in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. Treasure Island: StatPearls (2022).
3. Ock M, Jo MW, Choi EY, Lee SI. Patient safety incidents reported by the general public in Korea: a cross-sectional study. J Patient Saf. (2020) 16:e90–6. doi: 10.1097/PTS.0000000000000509
4. Heyland DK, Ilan R, Jiang X, You JJ, Dodek P. The prevalence of medical error related to end-of-life communication in Canadian hospitals: results of a multicentre observational study. BMJ Qual Saf. (2016) 25:671–9. doi: 10.1136/bmjqs-2015-004567
5. James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. (2013) 9:122–8. doi: 10.1097/PTS.0b013e3182948a69
6. Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. (1991) 324:377–84. doi: 10.1056/NEJM199102073240605
7. American IoMCoQoHCi. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press (2000).
8. Makary MA, Daniel M. Medical error-the third leading cause of death in the US. Br Med J. (2016) 353:i2139. doi: 10.1136/bmj.i2139
9. Wang J, Mu K, Gong Y, Wu J, Chen Z, Jiang N, et al. Occurrence of self-perceived medical errors and its related influencing factors among emergency department nurses. J Clin Nurs. (2022) 2022:16200. doi: 10.1111/jocn.16200
10. Wei Z, Wang Y, Yang S, Sun L. Association between perceived medical errors and suicidal ideation among Chinese medical staff: the mediating effect of depressive symptoms. Front Med. (2022) 9:807006. doi: 10.3389/fmed.2022.807006
11. Zhou X, Yao Z, Bai H, Duan J, Wang Z, Wang X, et al. Treatment-related adverse events of PD-1 and PD-L1 inhibitor-based combination therapies in clinical trials: a systematic review and meta-analysis. Lancet Oncol. (2021) 22:1265–74. doi: 10.1016/S1470-2045(21)00333-8
12. Hua W, Wang S, Wang X, Shao Y, Wang Y, Ye J, et al. Neuropsychiatric adverse events during 12 months of treatment with Efavirenz in Treatment-Naive HIV-infected patients in China: a prospective cohort study. Front Psychiatry. (2021) 12:579448. doi: 10.3389/fpsyt.2021.579448
13. Zhang T, Du J, Yin X, Xue F, Liu Y, Li R, et al. Adverse events in treating smear-positive tuberculosis patients in China. Int J Environ Res Public Health. (2015) 13:10086. doi: 10.3390/ijerph13010086
14. United Nations Department of Economic Social Affairs PD. Global Population Growth and Sustainable Development. New York, NY: United Nations (2021). Available online at: https://data.worldbank.org/indicator/SP.POP.TOTL?end=2020&most_recent_value_desc=true&start=2020&view=map (accessed November 29, 2022).
15. Jung JJ, Elfassy J, Juni P, Grantcharov T. Adverse events in the operating room: definitions, prevalence, and characteristics. A systematic review. World J Surg. (2019) 43:2379–92. doi: 10.1007/s00268-019-05048-1
16. Suliman WF, Al-Hammouri MM, Ta'an A. Prevalence of medical errors and barriers to report among nurses and nursing students in Jordan: a cross-sectional study. Nurs Forum. (2021) 56:284–90. doi: 10.1111/nuf.12542
17. Xu M, Wang Y, Yao S, Shi R, Sun L. One-year prevalence of perceived medical errors or near misses and its association with depressive symptoms among Chinese medical professionals: a propensity score matching analysis. Int J Environ Res Public Health. (2022) 19:63286. doi: 10.3390/ijerph19063286
18. Chan MF, Al Balushi AA, Al-Adawi S, Alameddine M, Al Saadoon M, Bou-Karroum K. Workplace bullying, occupational burnout, work-life imbalance and perceived medical errors among nurses in Oman: a cluster analysis. J Nurs Manag. (2021) 2021:13432. doi: 10.1111/jonm.13432
19. Nelson R. Rate of medical errors higher among critical care nurses in poor health. Am J Nurs. (2021) 121:13. doi: 10.1097/01.NAJ.0000767744.75988.75
20. Kiymaz D, Koc Z. Identification of factors which affect the tendency towards and attitudes of emergency unit nurses to make medical errors. J Clin Nurs. (2018) 27:1160–9. doi: 10.1111/jocn.14148
21. Jankowska-Polanska B, Czyrnianska M, Sarzynska K, Swiatoniowska-Lonc N, Chabowski M. Impact of fatigue on nursing care rationing in paediatric haematology and oncology departments - a cross-sectional study. BMC Nurs. (2021) 20:139. doi: 10.1186/s12912-021-00663-7
22. Gohal G. Models of teaching medical errors. Pak J Med Sci. (2021) 37:2020–5. doi: 10.12669/pjms.37.7.4506
23. Kahriman I, Ozturk H, Bahcecik N, Sokmen S, Kucuk S, Calbayram N, et al. The effect of theoretical and simulation training on medical errors of nurse students in Karadeniz Technical University, Turkey. J Pak Med Assoc. (2018) 68:1636–43.
24. Marti-Ejarque MDM, Guiu Lazaro G, Juncal RC, Perez Paredes S, Diez-Garcia C. Occupational diseases and perceived health in operating room nurses: a multicenter cross-sectional observational study. Inquiry. (2021) 58:469580211060774. doi: 10.1177/00469580211060774
25. Melnyk BM, Tan A, Hsieh AP, Gawlik K, Arslanian-Engoren C, Braun LT, et al. Critical care nurses' physical and mental health, worksite wellness support, and medical errors. Am J Crit Care. (2021) 30:176–84. doi: 10.4037/ajcc2021301
26. Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. (2003) 33:357–62. doi: 10.1017/S0033291702006700
27. Zhou C, Chu J, Wang T, Peng Q, He J, Zheng W, et al. Reliability and validity of 10-item Kessler Scale (K10) Chinese version in evaluation of mental health status of Chinese Population. Chin J Clin Psychol. (2008) 16:627–9.
28. Bu XQ, You LM, Li Y, Liu K, Zheng J, Yan TB, et al. Psychometric properties of the Kessler 10 scale in Chinese parents of children with cancer. Cancer Nurs. (2017) 40:297–304. doi: 10.1097/NCC.0000000000000392
29. Bougie E, Arim RG, Kohen DE, Findlay LC. Validation of the 10-item Kessler psychological distress scale (K10) in the 2012 aboriginal peoples survey. Health Rep. (2016) 27:3–10.
30. Pereira A, Oliveira CA, Bartolo A, Monteiro S, Vagos P, Jardim J. Reliability and factor structure of the 10-item Kessler psychological distress scale (K10) among Portuguese adults. Cien Saude Colet. (2019) 24:729–36. doi: 10.1590/1413-81232018243.06322017
31. Kahriman I, Öztürk H. Evaluating medical errors made by nurses during their diagnosis, treatment and care practices. J Clin Nurs. (2016) 25:2884–94. doi: 10.1111/jocn.13341
32. Melnyk BM, Orsolini L, Tan A, Arslanian-Engoren C, Melkus GD, Dunbar-Jacob J, et al. A national study links nurses' physical and mental health to medical errors and perceived worksite wellness. J Occup Environ Med. (2018) 60:126–31. doi: 10.1097/JOM.0000000000001198
33. Khammarnia M, Ansari-Moghaddam AR, Setoodehzadeh F, Rezaei K, Clark CCT, Peyvand M, et al. Systematic review and meta-analysis of the medical error rate in Iran: 2005-2019. Qual Manag Health Care. (2021) 30:166–75. doi: 10.1097/QMH.0000000000000304
34. Wu DTY, Deoghare S, Shan Z, Meganathan K, Blondon K. The potential role of dashboard use and navigation in reducing medical errors of an electronic health record system: a mixed-method simulation handoff study. Health Syst. (2019) 8:203–14. doi: 10.1080/20476965.2019.1620637
35. Kaprielian V, Ostbye T, Warburton S, Sangvai D, Michener L. A system to describe and reduce medical errors in primary care. In:K Henriksen, JB Battles, MA Keyes, ML Grady, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 1: Assessment). Rockville, MD: The Agency for Healthcare Research and Quality Publication (2008). p. 1–11.
36. Andel C, Davidow SL, Hollander M, Moreno DA. The economics of health care quality and medical errors. J Health Care Finance. (2012) 39:39–50.
37. Topcu I, Türkmen AS, Sahiner NC, Savaser S, Sen H. Physicians' and nurses' medical errors associated with communication failures. J Pak Med Assoc. (2017) 67:600–4.
38. Isci N, Altuntas S. Effect of professionalism level on tendency to make medical errors in nurses. Florence Nightingale Hemsire Derg. (2019) 27:241–52. doi: 10.26650/FNJN397503
39. Li H, Kong X, Sun L, Zhu Y, Li B. Major educational factors associated with nursing adverse events by nursing students undergoing clinical practice: a descriptive study. Nurse Educ Today. (2021) 98:104738. doi: 10.1016/j.nedt.2020.104738
40. Yesilyaprak T, Demir Korkmaz F. The relationship between surgical intensive care unit nurses' patient safety culture and adverse events. Nurs Crit Care. (2021) 2021:12611. doi: 10.1111/nicc.12611
41. Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, et al. Nurses' perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. (2021) 20:60. doi: 10.1186/s12912-021-00571-w
42. Patel DM, Walker HC, Brooks R, Omar N, Ditty B, Guthrie BL. Adverse events associated with deep brain stimulation for movement disorders: analysis of 510 consecutive cases. Neurosurgery. (2015) 11(Suppl.2):190–9. doi: 10.1227/NEU.0000000000000659
43. Arakawa C, Kanoya Y, Sato C. Factors contributing to medical errors and incidents among hospital nurses —nurses' health, quality of life, and workplace predict medical errors and incidents. Ind Health. (2011) 49:381–8. doi: 10.2486/indhealth.MS968
44. Arimura M, Imai M, Okawa M, Yamada TFaN. Sleep, mental health status, and medical errors among hospital nurses in Japan. Indus Health. (2010) 48:811–7. doi: 10.2486/indhealth.MS1093
45. Hall LH, Johnson J, Watt I, Tsipa A, O'Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. (2016) 11:e0159015. doi: 10.1371/journal.pone.0159015
46. Noland CM, Carmack HJ. “You never forget your first mistake”: Nursing socialization, memorable messages, and communication about medical errors. Health Commun. (2015) 30:1234–44. doi: 10.1080/10410236.2014.930397
47. Garrouste-Orgeas M, Perrin M, Soufir L, Vesin A, Blot F, Maxime V, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. (2015) 41:273–84. doi: 10.1007/s00134-014-3601-4
48. Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. (2015) 52:649–61. doi: 10.1016/j.ijnurstu.2014.11.004
49. Kerari A, Innab A. The influence of nurses' characteristics on medication administration errors: an integrative review. SAGE Open Nurs. (2021) 7:23779608211025802. doi: 10.1177/23779608211025802
50. Kable A, Kelly B, Adams J. Effects of adverse events in health care on acute care nurses in an Australian context: a qualitative study. Nurs Health Sci. (2018) 20:238–46. doi: 10.1111/nhs.12409
51. Nasiri T, Bahadori M, Ravangard R, Meskarpour Amiri M. Factors affecting the failure to report medical errors by nurses using the analytical hierarchy process (AHP). Hosp Top. (2020) 98:135–44. doi: 10.1080/00185868.2020.1796555
52. Aljabari S, Kadhim Z. Common barriers to reporting medical errors. ScientificWorldJournal. (2021) 2021:6494889. doi: 10.1155/2021/6494889
53. Kakemam E, Kalhor R, Khakdel Z, Khezri A, West S, Visentin D, et al. Occupational stress and cognitive failure of nurses and associations with self-reported adverse events: a national cross-sectional survey. J Adv Nurs. (2019) 75:3609–18. doi: 10.1111/jan.14201
Keywords: self-reported medical errors, self-reported adverse events, prevalence, risk factors, operating room nurse
Citation: Song Q, Tang J, Wei Z and Sun L (2022) Prevalence and associated factors of self-reported medical errors and adverse events among operating room nurses in China. Front. Public Health 10:988134. doi: 10.3389/fpubh.2022.988134
Received: 13 September 2022; Accepted: 14 November 2022;
Published: 08 December 2022.
Edited by:
Sahar Geravandi, Asadabad School of Medical Sciences, IranReviewed by:
Kourosh Zarea, Ahvaz Jundishapur University of Medical Sciences, IranKatalin D. Papp, University of Debrecen, Hungary
Copyright © 2022 Song, Tang, Wei and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Long Sun, c3VubG9uZ0BzZHUuZWR1LmNu
 Qi Song1
Qi Song1 Juan Tang
Juan Tang Long Sun
Long Sun