- 1Health Management Center, General Practice Center, West China Hospital, Sichuan University, Chengdu, China
- 2Biliary Surgery, West China Hospital, Sichuan University, Chengdu, China
Introduction: Current studies have found that the incidence of masked hypertension is high in Asian countries, but the use of ambulatory blood pressure monitoring (ABPM) in Asian countries is very limited, especially in primary health care. We compared the ABPM and office blood pressure (OBP) in primary health care of a high-risk population of hypertension.
Methods: The study included participants with at least one risk factor for hypertension who received primary health care. Demographic data, present medical history, personal history, and family history were collected by questionnaire.
Results: A total of 823 subjects were included in the study. There were 531 (64.5%) subjects with hypertension by ABPM and 316 patients (38.4%) by OBP. A paired chi-square test showed that the positive rate of ABPM in the diagnosis of hypertension was significantly higher than that of OBP (chi-square value 174.129, P < 0.0001). There were 24 (2.9%) patients with white coat hypertension, 239 (29.0%) with masked hypertension, 504 (52.9%) with a non-dipping pattern, 135 (16.9%) with nocturnal hypertension and 18 (2.2%) with high ambulatory BP variability. Concordance correlation coefficient showed there was a poor correlation between OBP and awake average BP. Scatter plot displayed there was a positive correlation between OBP and awake average BP, but the degree of fitting was not high. The Bland Altman plot showed that OBP and awake average BP were consistent.
Conclusions: Although OBP and ABPM have some consistency, ABPM can screen for masked hypertension and nocturnal hypertension in primary care of populations at high risk of hypertension. Therefore, ABPM is necessary in the primary health care of populations at high risk of hypertension and can be used as a routine screening.
1. Background
Hypertension is an important risk factor leading to cardiovascular disease and stroke, and it is an important public health problem (1). Risk factors for hypertension include age, smoking, alcoholism, low physical activity, high salt diet, family history of hypertension and overweight or obese (2). At present, office blood pressure (OBP) is still an important means of hypertension screening and management and is especially suitable for primary health care because of its convenience and economy (3, 4). However, OBP has great limitations. OBP is easily affected by the operation method, and variability is great (3). Multiple OBP measurements can minimize the impact of the limitations, but white-coat hypertension and masked hypertension are difficult to detect by OBP (3). A study involving 14,143 people in 27 countries showed that the prevalence rates of white coat hypertension and occult hypertension were 23% and 10%, respectively (5). With the sufficient understanding of the limitations of OBP and the importance of ambulatory blood pressure monitoring (ABPM), an increasing number of scholars are paying attention to the role of ABPM in the diagnosis, prognosis and management of hypertension. ABPM can evaluate BP at multiple time points in daily life and automatically calculate average BP, including 24-h average BP, daytime average BP and nighttime average BP. It can also evaluate the circadian rhythm of BP, which contains abundant BP parameters and is more conducive to finding masked hypertension (4, 6). Current studies have found that the incidence of masked hypertension, morning hypertension and nocturnal hypertension in Asian countries is higher than that in Western countries (7–9). However, the use of ABPM in Asian countries, including China, is very limited, especially in primary health care (10). The purpose of this study was to compare OBP with ABPM in high hypertension-risk Asian individuals in primary care.
2. Methods
2.1. Subjects
The population at high risk of hypertension who received primary health care in West China Hospital Health Management Center from November 2020 to October 2021 was included.
2.1.1. Inclusion criteria
At least one of the following risks of hypertension was met (2). (1) Age ≥ 40 years old; (2) Smoking; (3) Alcoholism; (4) Low physical activity (11); (5) High salt diet; (6) Family history of hypertension; (7) Overweight or obese.
2.1.2. Exclusion criteria
Patients with hypertension, severe cardiovascular and cerebrovascular diseases, severe liver and kidney diseases, severe mental illness and malignant tumors.
This study was approved by the Ethics Committee of West China Hospital, and the subjects signed the informed consent form.
2.2. Data collection and indicator measurement
Basic information was collected by questionnaire. The questionnaire included demographic data, present medical history, personal history and family history. The present medical history consisted of hypertension, diabetes, hyperlipidemia, cardiovascular and cerebrovascular diseases, malignant tumors, liver and kidney diseases, and mental illness. Personal history included smoking history, drinking history, exercise, and salt intake. Family history included a family history of hypertension. Height, weight, OBP and ABPM were measured on the same date.
2.2.1. Height and weight measurement method
The subjects only wore single clothes and took off their shoes and socks. Height and weight were measured by a calibrated electronic meter (Seca 287, Germany).
2.2.2. OBP measurement method
The subjects rested for at least 5 min, and no smoking, tea or coffee was taken within 30 min. BP was measured twice by a calibrated electronic sphygmomanometer (Omron HBP-9021, Japan) by professional nurses, and the average value was taken (12).
2.2.3. ABPM method
ABPM is the gold standard measure of BP. ABPM equipment (SPACELABS, 90217A, America) was used to monitor 24-h BP and outputted average BP, average pulse pressure, average daytime BP, average nighttime BP and circadian rhythm. The ABPM equipment was installed by professional nurses in the hospital. Then, subjects took the device home, and the nurse removed it the next day. The hour between waking up and going to bed was defined as daytime, and the hour between going to bed and waking up was defined as nighttime (13).
2.3. Diagnostic criteria
2.3.1. Phenotype hypertension
(1) Hypertension
OBP ≥140/90 mm Hg or ambulatory BP was elevated (24-h average BP ≥130/80 mm Hg or daytime average BP ≥135/85 mm Hg or nighttime average BP ≥120/70 mm Hg) (2).
(2) White-coat hypertension
Office BP ≥140/90 mm Hg and ambulatory BP were normal (24-h average BP < 130/80 mm Hg and daytime average BP < 135/85 mm Hg) (2).
(3) Masked hypertension
Office BP < 140/90 mm Hg and ambulatory BP were elevated (24-h average BP ≥130/80 mm Hg or daytime average BP ≥135/85 mm Hg) (2).
(4) Non-dipping pattern
Diel rhythm was < 10% (2).
(5) Nocturnal hypertension
Nighttime ambulatory BP average ≥120/70 mm Hg, 24-h average BP < 130/80 mm Hg and daytime average BP < 135/85 mm Hg (2).
(6) High ambulatory BP variability
Diel rhythm was more than 20% (2).
2.3.2. Overweight and obesity
Overweight: 24 kg/m2 ≤ body mass index (BMI) < 28 kg/m2 (14);
Obesity: BMI ≥ 28 kg/m 2 (14).
2.3.3. High salt diet
Salt consumption was investigated in a questionnaire. Taste for salty food was divided into very light, light, average, salty, and very salty. The average level of salt intake was 6 g/d. The taste for salty or very salty food (salt intake >6 g/d) was defined as a high salt diet (15).
2.4. Statistical methods
IBM SPSS 26.0 and MedCalc 19.8 software were used for statistical analysis. The continuity variable was expressed as the mean value () ± standard deviation (S). Qualitative data were described by absolute numbers and rates. The rates of the two groups were compared using the paired chi-square test. The two continuity variables were compared using paired t tests. Concordance correlation coefficient, scatter chart, Bland Altman plot, ROC curve and area under the curve were used to compare OBP and awake average BP. α = 0.05.
3. Results
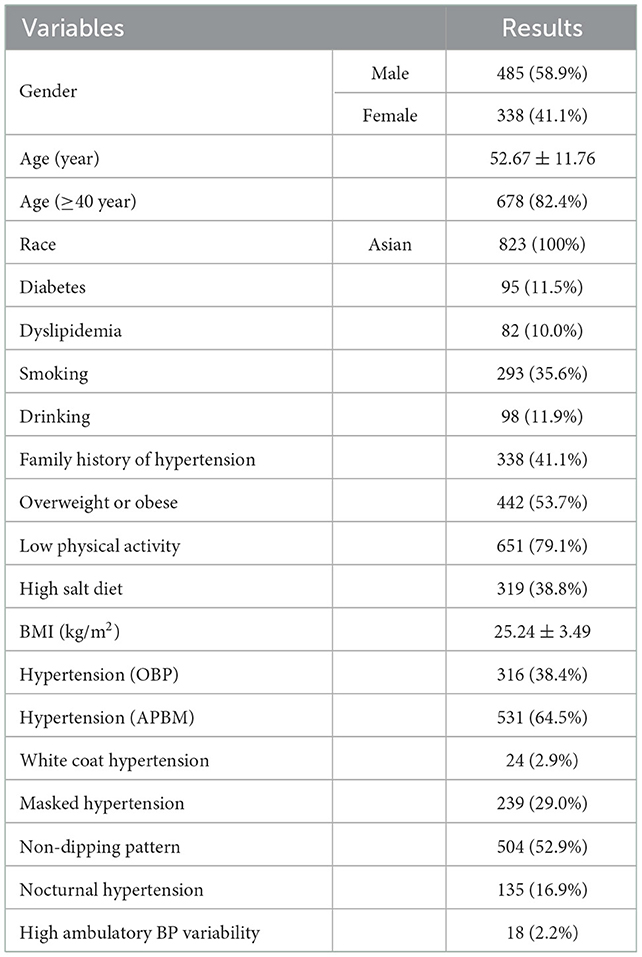
We screened 1,286 cases and excluded 463 cases according to the inclusion and exclusion criteria. A total of 823 subjects were included in the study, including 485 (58.9%) males and 338 (41.1%) females. The average age was 52.67 ± 11.76 (30–81) years old. There were 678 (82.4%) subjects aged 40 or older. The subjects were all Chinese. There were 95 (11.5%) patients with diabetes and 82 (10.0%) patients with dyslipidemia. Two hundred ninety-three (35.6%) subjects had a history of smoking, 98 (11.9%) had a history of drinking, 338 (41.1%) had a family history of hypertension, 442 (53.7%) were overweight or obese, 651 (79.1%) had low physical activity, and 319 (38.8%) had a high-salt diet. The number of hypertension cases was 316 (38.4%) by OBP and 531 (64.5%) by ABPM, and the paired chi-square test showed that the difference was statistically significant (chi-square value 174.129, P < 0.0001). There were 24 (2.9%) patients with white coat hypertension, 239 (29.0%) with masked hypertension, 504 (52.9%) with a non-dipping pattern, 135 (16.9%) with nocturnal hypertension and 18 (2.2%) with high ambulatory BP variability. The details are shown in Table 1.
The BP results of the included subjects are shown in Table 2. OBP was 136.06 ± 16.25/81.61 ± 12.30 mm Hg. The 24-h average BP was 126.88 ± 15.42/80.48 ± 11.25 mm Hg, the awake average BP was 130.56 ± 14.69/84.48 ± 12.60 mm Hg, and the nighttime average BP was 119.59 ± 16.33/75.50 ± 11.44 mm Hg.
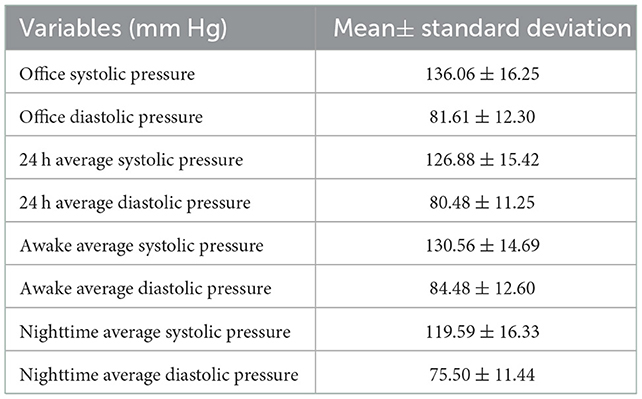
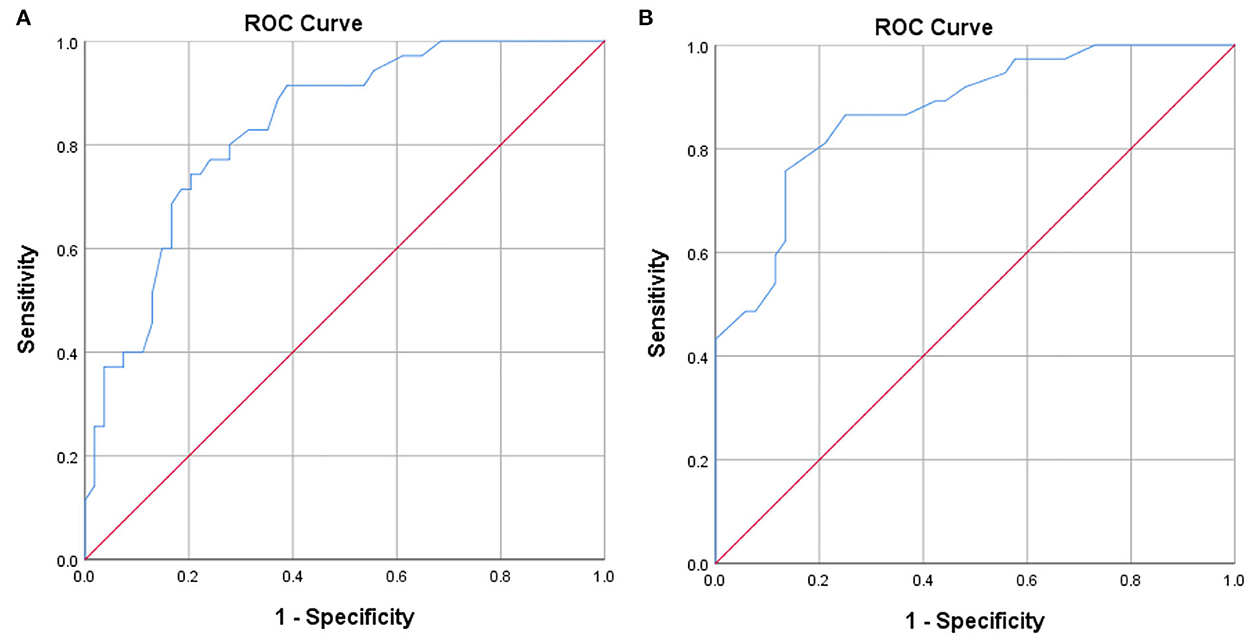
The correlation between office systolic pressure and awake average systolic pressure was poor (Concordance correlation coefficient = 0.606), and the same relationship was observed between office diastolic pressure and awake average diastolic pressure (Concordance correlation coefficient = 0.650). The scatter plot indicates that there was a positive correlation between office systolic pressure and awake average systolic pressure, but the degree of fitting was not high (R2 = 0.420, Figure 1A). There was a positive correlation between office diastolic pressure and awake average diastolic pressure, but the degree of fitting was also not high (R2 = 0.445, Figure 1B). The Bland Altman plot showed that office systolic pressure and awake average systolic pressure were consistent (P < 0.0001, Figure 2A), as were office diastolic pressure and awake average diastolic pressure (P < 0.0001, Figure 2B). The ROC curves of office systolic pressure and awake average systolic pressure is shown in Figure 3A, office diastolic pressure and awake average diastolic pressure in Figure 3B, and the areas under the ROC curves were 0.834 and 0.872, respectively.
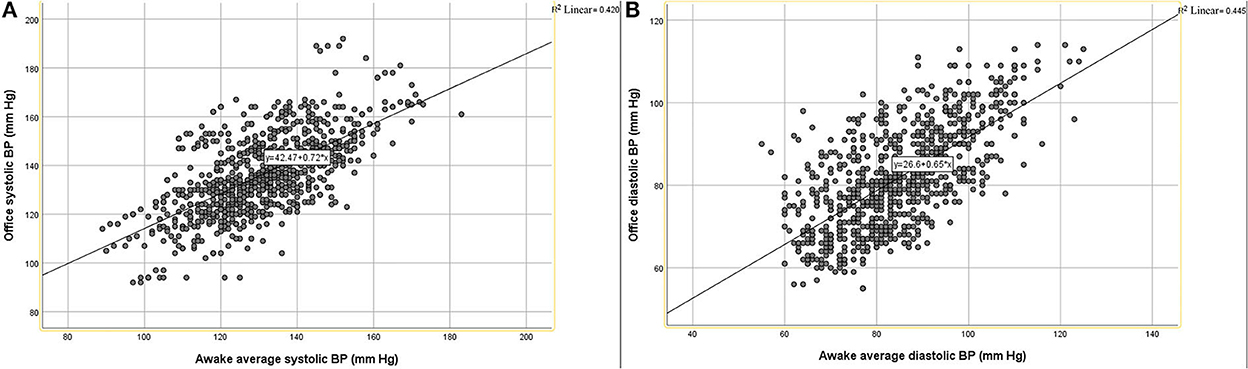
Figure 1. Scatter diagram of OBP and awake average BP. (A) Systolic pressure, (B) diastolic pressure.
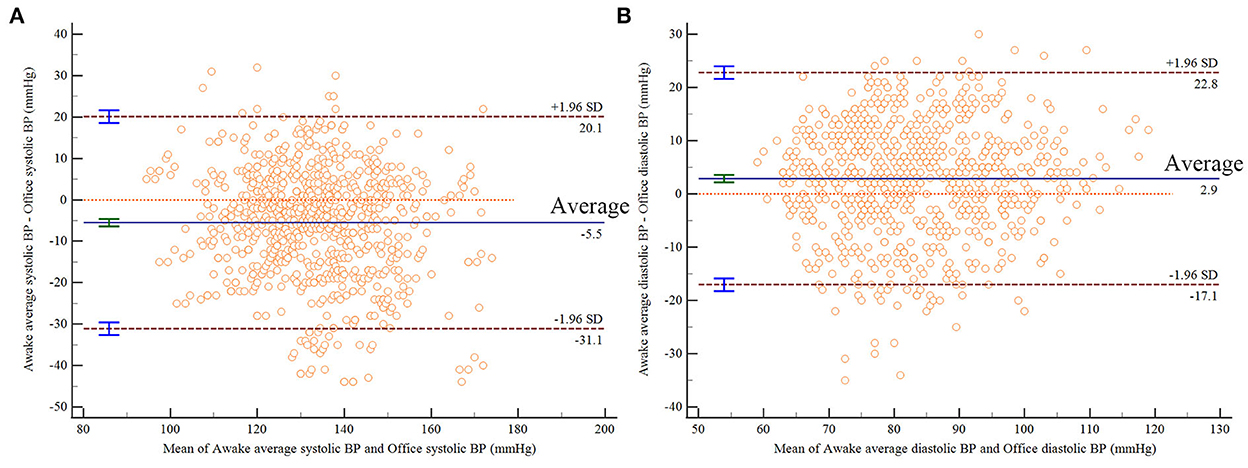
Figure 2. Bland Altman plot results of OBP and awake average BP. (A) Systolic pressure, (B) diastolic pressure.
4. Discussion
Previous studies on ABPM have mainly focused on outpatients or inpatients (16–18), and the number of studies on the population receiving primary health care is very limited. ABPM is not routinely used in primary health care due to its high cost and limited resources (10).
In this study, by comparing the values of OBP and ambulatory BP, it was found that there was a poor correlation between them, with consistency, and there was a linear relationship, but the degree of fit was not high. Although the OBP and ABPM have consistency, the positive rate of ABPM (64.5%) for screening hypertension was significantly higher than that of OBP (38.4%). In this study, the subjects were the high-risk population of hypertension, which may be the reason for the higher prevalence of hypertension than in the previous study (19).
ABPM screened out 24 (2.9%) patients with white coat hypertension, 239 (29.0%) with masked hypertension, 504 (52.9%) with a non-dipping pattern, 135 (16.9%) with nocturnal hypertension and 18 (2.2%) with high ambulatory BP variability. Previous studies have reported that the prevalence of white coat hypertension was 13% in untreated people (20, 21), the prevalence rate of masked hypertension in China is 17.8% (20), and the prevalence of nocturnal hypertension was approximately 10% in the Chinese population and 6.0% ~ 7.9% in Europe and America (22). This may be associated with salt-sensitive hypertension in the Chinese population (23). We hypothesize that the differences from previous studies are mainly due to race and the differences in the included population.
Although the cost increases at present, it will save the cost in the long run (24). The 24-h mean BP and nocturnal BP can better predict the morbidity and mortality of cardiovascular and cerebrovascular diseases (25). Patients with masked hypertension and nocturnal hypertension can receive intervention treatment as soon as possible, and some of them can be alleviated only by lifestyle intervention, which can greatly reduce the incidence and mortality of complications such as cardiovascular and cerebrovascular diseases, which can reduce the economic burden of patients' families and society in the long run (26–28). This study provides an important basis for the application of ABPM in the primary care of high-risk hypertension populations.
This study has some advantages. The population included in this study was at high risk for hypertension receiving primary care, and this population has been less studied in previous studies. This study is a prospective study design and is relatively more reliable than the results of cross-sectional studies. Of course, there are some drawbacks to this study. The study did not include a long follow-up period, and the sample size of this study was not large enough. Therefore, high-quality studies with a larger sample size and long-term follow-up are needed to further confirm the role and significance of ABPM in primary care.
5. Conclusion
Although OBP and ABPM haves some consistency, ABPM can screen for masked hypertension and nocturnal hypertension in primary care of populations at high risk of hypertension. Therefore, ABPM is necessary in the primary health care of populations at high risk of hypertension and can be used as a routine screening.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by West China Hospital, Sichuan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
WG was responsible for the study design, data collection, statistical analysis, and manuscript writing. YJ contributed to data collection. TB contributed to statistical analysis. YH was responsible for the study design and manuscript revision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by 1•3•5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYJC21056) and the Science and Technology Bureau of Sichuan Province (grant numbers: 2020YFS0099, 2021YJ0139, and 2019YFS0306).
Acknowledgments
We thank the participants in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. (2021) 18:785–802. doi: 10.1038/s41569-021-00559-8
2. Viera AJ, Shimbo D. Ambulatory blood pressure phenotypes and the risk for hypertension. Curr Hypertens Rep. (2014) 16:481. doi: 10.1007/s11906-014-0481-5
3. Stergiou GS, Palatini P, Parati G, O'Brien E, Januszewicz A, Lurbe E, et al. 2021 european society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. (2021) 39:1293–302. doi: 10.1097/HJH.0000000000002843
4. Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
5. Omboni S, Aristizabal D, Sierra AD, Dolan E, Head G, Kahan T, et al. Hypertension types defined by clinic and ambulatory blood pressure in 14 143 patients referred to hypertension clinics worldwide. Data from the ARTEMIS study. J Hypertens. (2016) 34:2187–98. doi: 10.1097/HJH.0000000000001074
6. Kario K, Park S, Chia Y-C, Sukonthasarn A, Turana Y, Shin J, et al. 2020 Consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich). (2020) 22:351–62. doi: 10.1111/jch.13751
7. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic diurnal blood pressure variability between Japanese and American treatment-resistant hypertensive populations. Circ J. (2017) 81:1337–45. doi: 10.1253/circj.CJ-16-1237
8. Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. (2013) 61:278–83. doi: 10.1161/HYPERTENSIONAHA.111.00217
9. Shin J, Kario K, Chia Y-C, Turana Y, Chen C-H, Buranakitjaroen P, et al. Current status of ambulatory blood pressure monitoring in Asian countries: a report from the HOPE Asia Network. J Clin Hypertens (Greenwich). (2020) 22:384–90. doi: 10.1111/jch.13724
10. Mahmud A, Alahaideb R, Alshammary H, Abanumay M, Alfawwaz A, Alhelabi S, et al. Prevalence and clinical correlates of ambulatory blood pressure phenotypes in a Saudi hypertensive population. J Clin Hypertens (Greenwich). (2020) 22:2372–6. doi: 10.1111/jch.14059
11. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
12. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. (2020) 75:1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
13. Kario K, Hoshide S, Chia Y-C, Buranakitjaroen P, Siddique S, Shin J, et al. Guidance on ambulatory blood pressure monitoring: a statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). (2021) 23:411–21. doi: 10.1111/jch.14128
14. Zeng Q, Yang Y, Jia W, Li Y, Zhu Y, Zhang P, et al. Expert consensus & standard on weight management for overweight or obese people. Chin J Health Manage. (2018) 12:200–7.
15. Ha SK. Dietary salt intake and hypertension. Electrolyte Blood Press. (2014) 12:7–18. doi: 10.5049/EBP.2014.12.1.7
16. Hinderliter AL, Voora RA, Viera AJ. Implementing ABPM into clinical practice. Curr Hypertens Rep. (2018) 20:5. doi: 10.1007/s11906-018-0805-y
17. Salagre SB, Khobragade AP. Clinical utility of ambulatory blood pressure monitoring (ABPM) in newly diagnosed hypertensive patients. J Assoc Physicians India. (2020) 68:52–6.
18. Harianto H, Valente M, Hoetomo S, Anpalahan M. The clinical utility of ambulatory blood pressure monitoring (ABPM): a review. Curr Hypertens Rev. (2014) 10:189–204. doi: 10.2174/157340211004150319121321
19. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. (2018) 137:2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380
20. Kang Y-Y, Li Y, Huang Q-F, Song J, Shan X-L, Dou Y, et al. Accuracy of home versus ambulatory blood pressure monitoring in the diagnosis of white-coat and masked hypertension. J Hypertens. (2015) 33:1580–7. doi: 10.1097/HJH.0000000000000596
21. Fagard RH. and Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. (2007) 25:2193–8. doi: 10.1097/HJH.0b013e3282ef6185
22. Li Y, Staessen JA, Lu L, Li L-H, Wang G-L, Wang J-G. Is isolated nocturnal hypertension a novel clinical entity? Findings from a Chinese population study. Hypertension. (2007) 50:333–9. doi: 10.1161/HYPERTENSIONAHA.107.087767
23. Zou T, Yao S, Du M-F, Mu J-J, Chu C, Hu G-L, et al. Associations of corin genetic polymorphisms with salt sensitivity, blood pressure changes, and hypertension incidence in Chinese adults. J Clin Hypertens (Greenwich). (2021) 23:2115–23. doi: 10.1111/jch.14401
24. O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. (2013) 31:1731–68. doi: 10.1097/HJH.0b013e328363e964
25. Yang W-Y, Melgarejo JD, Thijs L, Zhang Z-Y, Boggia J, Wei F-F, et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA. (2019) 322:409–20. doi: 10.1001/jama.2019.9811
26. Douros A, Tölle M, Ebert N, Gaedeke J, Huscher D, Kreutz R, et al. Control of blood pressure and risk of mortality in a cohort of older adults: the Berlin Initiative Study. Eur Heart J. (2019) 40:2021–28. doi: 10.1093/eurheartj/ehz071
27. Bowling CB, Davis BR, Luciano A, Simpson LM, Sloane R, Pieper CF, et al. Sustained blood pressure control and coronary heart disease, stroke, heart failure, and mortality: An observational analysis of ALLHAT. J Clin Hypertens (Greenwich). (2019) 21:451–9. doi: 10.1111/jch.13515
Keywords: ambulatory blood pressure monitoring (ABPM), office blood pressure, hypertension, primary health care, high-risk population
Citation: Gao W, Jin Y, Bao T and Huang Y (2023) Comparison of ambulatory blood pressure monitoring and office blood pressure in primary health care of populations at a high risk of hypertension. Front. Public Health 10:985730. doi: 10.3389/fpubh.2022.985730
Received: 04 July 2022; Accepted: 19 December 2022;
Published: 11 January 2023.
Edited by:
Jose Vilela-Martin, Faculdade de Medicina de São José do Rio Preto, BrazilReviewed by:
Juan Yugar, Faculdade de Medicina de São José do Rio Preto, BrazilMarco Antonio Vieira Da Silva, Universidade Federal do Triângulo Mineiro, Brazil
Copyright © 2023 Gao, Jin, Bao and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Huang,  amtnbHp4MjAwNkAxNjMuY29t
amtnbHp4MjAwNkAxNjMuY29t
 Wei Gao
Wei Gao Yanwen Jin2
Yanwen Jin2 Yan Huang
Yan Huang