
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 01 December 2022
Sec. Environmental Health and Exposome
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.985445
A correction has been applied to this article in:
Corrigendum: Association of household fuel with acute respiratory infection (ARI) under-five years children in Bangladesh
 Md. Aminul Islam1,2*†
Md. Aminul Islam1,2*† Mohammad Nayeem Hasan3,4*†
Mohammad Nayeem Hasan3,4*† Tanvir Ahammed3
Tanvir Ahammed3 Aniqua Anjum3
Aniqua Anjum3 Ananya Majumder5
Ananya Majumder5 M. Noor-E-Alam Siddiqui3
M. Noor-E-Alam Siddiqui3 Sanjoy Kumar Mukharjee1
Sanjoy Kumar Mukharjee1 Khandokar Fahmida Sultana1
Khandokar Fahmida Sultana1 Sabrin Sultana6
Sabrin Sultana6 Md. Jakariya7
Md. Jakariya7 Prosun Bhattacharya8*
Prosun Bhattacharya8* Samuel Asumadu Sarkodie9
Samuel Asumadu Sarkodie9 Kuldeep Dhama10
Kuldeep Dhama10 Jubayer Mumin11
Jubayer Mumin11 Firoz Ahmed1
Firoz Ahmed1In developing countries, acute respiratory infections (ARIs) cause a significant number of deaths among children. According to Bangladesh Demographic and Health Survey (BDHS), about 25% of the deaths in children under-five years are caused by ARI in Bangladesh every year. Low-income families frequently rely on wood, coal, and animal excrement for cooking. However, it is unclear whether using alternative fuels offers a health benefit over solid fuels. To clear this doubt, we conducted a study to investigate the effects of fuel usage on ARI in children. In this study, we used the latest BDHS 2017–18 survey data collected by the Government of Bangladesh (GoB) and estimated the effects of fuel use on ARI by constructing multivariable logistic regression models. From the analysis, we found that the crude (the only type of fuel in the model) odds ratio (OR) for ARI is 1.69 [95% confidence interval (CI): 1.06–2.71]. This suggests that children in families using contaminated fuels are 69.3% more likely to experience an ARI episode than children in households using clean fuels. After adjusting for cooking fuel, type of roof material, child's age (months), and sex of the child–the effect of solid fuels is similar to the adjusted odds ratio (AOR) for ARI (OR: 1.69, 95% CI: 1.05–2.72). This implies that an ARI occurrence is 69.2% more likely when compared to the effect of clean fuel. This study found a statistically significant association between solid fuel consumption and the occurrence of ARI in children in households. The correlation between indoor air pollution and clinical parameters of ARI requires further investigation. Our findings will also help other researchers and policymakers to take comprehensive actions by considering fuel type as a risk factor as well as taking proper steps to solve this issue.
Acute respiratory infection (ARI) is the leading cause of death among children under-five years in underdeveloped countries (1). It is a severe infection that makes it difficult to breathe normally (2). Yet, it is nearly impossible to prove whether the main risk factors for developing an ARI from viruses and bacteria originate from the nose, trachea (windpipe), or lungs (3–5). Children, elderly, and people with immune system abnormalities are especially vulnerable (6–9).
Generally, anyone from neonatal to old may be affected by ARI, with diverse clinical symptoms such as runny nose, cough, nasal congestion, sore throat, fatigue, body aches, obstruction, dysphasia, or respiratory distress, accompanied by or without fever (10). The World Health Organization (WHO) confirmed a global alarm for pneumonia called severe acute respiratory syndrome (SARS) on 12 March 2003 (11). ARI causes 15% of the global under-five deaths in children, especially in low- and middle-income countries (LMICs) (12). About 98% of children in LMICs under the age of five are exposed to levels of ambient air pollution that exceed WHO recommendations (13). For children in high-income countries, the figure is 52% (13). Bangladesh is LMIC with almost 166 million people (63%) living in rural regions (14). However, the precise magnitude of ARI which is already doubling at a very large scale in Bangladesh is unknown. Unlike cholera or acute malnutrition, there are no acceptable benchmarks for ARI, making it difficult to measure case management quality using established criteria. Several research studies reported high correlations between environmental risk parameters and developing ARI, such as smoke produced from indoor cooking, different types of outdoor air pollution, passive smoking, and overcrowding (15, 16). These risk factors in children under-five years cause various severe problems, such as low birth weight, malnutrition, measles, pneumonia, and problems in breastfeeding mothers (16). In addition to that, different types of cooking fuel, poor toilet facilities, percentage of mother's literacy, adequate medication for the intestinal parasite, place of residence, body mass index (BMI) of mother and children, and wealth index are also potential risk factors for pneumonia/ARI in developing countries (17–23). Recent studies from India and Guatemala indicated that children born in households using high-polluting solid fuels were 73 and 63 g underweight, respectively, lower in birth weight as compared with children born in households using low-polluting fuels (24, 25).
In rural areas of developing countries, the main risk factors for ARI considered are lack of sanitation system, malnutrition, cooking smoke, and acute respiratory diseases, which are related to the low income and illiteracy (25–27). The burning of cooking fuel is not necessarily the only source of indoor air pollution, although it is considered the major source. Pollutants from dirty contaminated fuel sources used for indoor space heating and lighting are among the other sources (1). Children in the city stay inside their home being exposed to indoor air pollution from biomass fuel due to outdoor space scarcity. Underlying risk factors such as malnutrition among children may also aggravate the problems significantly (28). Because of the scarcity and difficulty in obtaining non-solid or clean fuels such as electricity and natural gas, low-income families in many developing countries rely on the use of low-cost but high-pollution solid fuels, such as wood, coal, straws, and animal dung, as their primary sources of energy for cooking and heating (29–32). Yet, even when access to electricity was available, 19.0, 6.8, and 50.9% of households in Bangladesh used crops, animal dung, and wood, respectively, as fuels for cooking, heating, and lighting (18). The fuels are primarily used in simple, inefficient, and mostly unvented family cooking stoves, resulting in enormous amounts of indoor smoke accumulation due to poor ventilation (33). The number of doors and windows is pertinent in improving house ventilation and is also associated with children's ARI. The odds of ARI in children living in poorly ventilated houses were four times higher than in those living in houses with good ventilation (34).
In Bangladesh, 80% of households use various solid fuel sources for cooking (coal/lignite, charcoal, wood, straw/shrubs/grass, crops, and animal dung), while 20% use clean fuel (electricity and liquid petroleum gas/natural gas/biogas) (35). In addition, the main reason for mortality and morbidity in Bangladesh for diarrhea has been successfully mitigated now, while the relative risk factors for ARI have been increasing day by day (36–39). However, no study to our knowledge has investigated the link between ARI in children and solid fuel exposure in Bangladesh. Thus, using the most up-to-date data available, this study examines the relationship between exposure to solid fuels and ARI in Bangladeshi children under the age of five.
Bangladesh is a developing country and is one of the most highly densely populated countries in the world, with a delta of rivers that flows down into the Bay of Bengal (40). It is a low-lying, riverine country in South Asia's tropical monsoon region, with an average elevation of 85 meters above sea level and a climate marked by high temperatures, heavy rainfall, cyclones, tidal bores, often excessive humidity, and fairly marked seasonal variations (41, 42).
Bangladesh is a tropical-moist climate-based area characterized by seasonal diversity in precipitation, moderate ambient temperature, and high relative humidity (43). The country has four climatic seasons in a year: lower temperature in the winter (from December to February); higher temperature in the summer (from March to May), the rainy season (from June to September), and the post-monsoon autumn (from October to November) (44). From the observation of daily temperature data in the last 61 years (1960–2021), the average temperature of 25.2°C occurs in July, a minimum temperature of 12.9°C occurs in January while the maximum temperature of 33.5°C is observed in April. We also observed maximum precipitation of 496 mm in July and a minimum of 4 mm in January (43).
This study utilized data from the BDHS 2017–18, a government-organized national survey. In the first step, 675 enumeration areas (EA) were chosen with a probability proportionate to EA size of 250 in urban regions and 425 in rural areas. A calculated sample size of 30 households per EA was selected in the second step of sampling to give statistically credible estimates of key demographic and health characteristics. A total of 20,250 households were selected based on this concept. Since three EAs (two rural and one urban) were severely affected by floodwater, the survey was completed in 672 EAs. We observed that about 20,100 were never-married women aged 15 to 49 who were expected to complete the interviews. Mothers of 8,347 children younger than 5 years were questioned about demographic, economic, pregnancy, postnatal care, immunization, and health issues including ARI symptoms. After limiting our samples to children for whom complete data on the outcome and predictors included in the study were available, we ended up with 8,321 (weighted) children for analysis after eliminating ineligible cases (such as other fuel types, guests, and non-surviving based children) as well as cases with missing survey information on the age of selected children. Figure 1 illustrates the sampling technique. The 2017–18 BDHS report includes a detailed discussion of the sample design and technique. In this study, we used the outcome variable of interest as ARI in children under the age of five. According to 2017–18 BDHS, ARI is known as a mother's or caregiver's acuity whether children with ARI symptoms need to follow proper treatment. In that survey, the ARI symptoms define as, short, rapid breathing that is chest-related and/or difficult breathing. Children under age five with ARI symptoms in the 2 weeks before the survey were included as a sample in this study. The ARI variable was classified as 1, if respondents answered “yes”, or coded as 0 when they responded “no”.
The exposure variable is solid fuel, which is determined by the type of fuel used for cooking or heating. Each household's type of cooking fuel is collected by the BDHS. Survey respondents were asked “What type of fuel does your home primarily use for cooking?” (35). Fuel types are classified into coal/lignite, charcoal, wood, straw/shrubs/grass, crops, animal dung, electricity, and liquid petroleum gas/natural gas/biogas. The exposure variable is a binary variable that indicates types of cooking fuel: clean fuel vs. solid fuel. Coal/lignite, charcoal, wood, straw/shrubs/grass, crops, and animal dung are considered solid fuels. The use of electricity and liquid petroleum gas/natural gas/biogas is classified as clean fuels. The fuel type variable is coded as 1 if the household uses clean fuel, otherwise 0 (solid fuel).
By reviewing the existing literature, the most potentially related and assumed variables associated with ARI were included in this study, such as household-related factors (i.e., place of residence, region, mass media, source of potable water, availability of toilet facility, wealth status, electricity, types of materials for flooring, type of wall material, type of roof material, and the number of household members), parents/caregivers related factors (i.e., having vaccination card, mother's age, education level, BMI, the total count of living children, mother's occupation, mother's work for, household head's occupation, proper education, and type of household head's education), and child-related factors (i.e., child's age, sexual category, time of birth, delivery place, birth weight, C-section delivery, treatment for intestinal diseases, vitamin A supplementation, and nutritional history) (25).
Participants were asked about their history of listening to radio or watching television, and those who replied at least once in 7 days were counted to be routinely exposed to that type of social media (35). Sources of drinking water, supplied piped water sources (piped in dwellings, piped to a yard/plot, public tap water/standpipe water), tube well water (borehole), and other sources of drinking water, were listed (e.g., rainwater and river water, well) (45). Some of the toilet facilities used in this study include improved (flush toilets, flush in a piped sewer system, flush in septic tanks, flush from pit latrines, pit latrines with slabs, and ventilated pit latrines), shared (but improved) toilets with other households, and not advanced (no flush toilet), no flush in the piped sewer facility, no flush in the septic tank (e.g., hanging toilet, open hole) (46). The wealth index was reclassified into upper economic class (above 20% asset value), middle economic class (within 40% asset value), and lower economic class (below 40% asset value) (47). We also observed the main material of the floor/roof/wall of the dwelling. The floor/roof/wall is classified as natural (earth/sand and dung), rudimentary (wood planks and palm/bamboo), and finished (vinyl or asphalt strips, ceramic tiles, cement, and carpet) (35).
The BDHS obtained vaccination coverage data in 2017–2018 using two methods namely immunization cards provided to interviewers and from mothers' verbal remarks (48, 49). In this study, wealth index categorized into three variables where Richer and Richest converted to “Rich” and Poorer and Poorest to “Poor.” The interviewers transcribed the vaccination dates straight into the questionnaire if the cards were available. The respondents were asked to recollect the immunizations administered to their child if there was no vaccination card for the child or if a vaccine was not mentioned as administered in the vaccination card (8, 31, 35, 50–52). Mother's/household head's occupation is categorized as agricultural/skilled worker (farming/agricultural work and semi-skilled labor/service), household/unskilled worker (unskilled labor, home-based manufacturing, domestic service, and other), and industrial worker (professional/technical, business, factory work or blue-collar service, poultry, or cattle raising).
The weight at birth was classified as low if the weight of the child was <2.5 kg and normal if >2.5 kg. The z-scores of three anthropometric indices namely height-for-age, weight-for-age, and weight-for-height were used to assess a child's nutritional status as suggested by WHO (9). The z-score indicates how far a given result deviates from the mean, and it is commonly used to normalize data. The z-score is used in this study to compare stunting and wasting in children under-5 years by gender and age group. If a child's weight-for-height z-score is <-2, it is labeled as wasted, weight-for-age z-score is <-2, it is labeled as underweight, and the z-score of height-for-age <-2 is classified as stunted.
To illustrate the distribution of variables, descriptive statistics were utilized whereas numbers and percentages were used for categorical variables. We used chi-square tests to identify factors associated with ARI in children, and P < 0.05 was considered statistically significant. We fit the design-based binary logistic regression (53) to assess the association between child ARI and types of cooking fuel in a household. For the adjusted association, the model was adjusted for the type of cooking fuel, type of roof material, child's age (months), and sex of the child. The COR and AOR were calculated and reported with the 95% CI and p-values (54). The specified predictor variables are used in multiple logistic regression. A survey package in R was used to conduct the statistical analyses and data management in this study. (55).
The variables were selected using the Rao and Scott chi-squared test (a design-adjusted variation of the Pearson chi-squared test) (56) which was employed to account for the data's cluster-design effect. In total, 13 variables were significant with ARI at p < 0.05 (Table 1). Bivariate and multivariable logistic regression were carried out independently for each of the selected variables. A cutoff value of 4.00 was used as the variance inflation factor (VIF) value to analyze multicollinearity in the final model (Table 2). The area under the curve (AUC) of the receiver operating characteristic curve is used to verify the prediction accuracy of the final model (Table 3). We also utilized the Hosmer and Lemeshow goodness-of-fit test to examine the overall fit of the final model (Table 3).
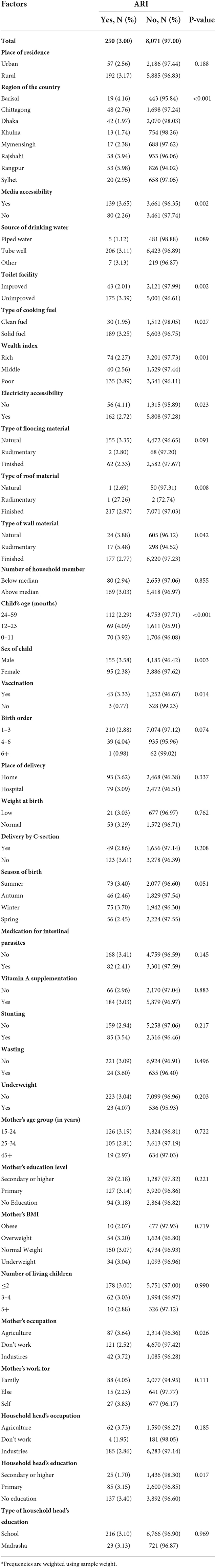
Table 1. Frequency distribution (weighted*) of ARI among children younger than 5 years in Bangladesh.
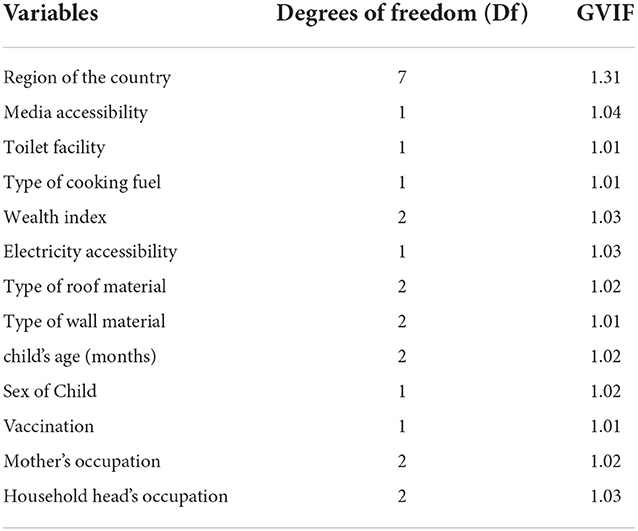
Table 2. Generalized variance inflation (GVIF) value of the final model of ARI among under-5 years children in Bangladesh.
A total number of 20,160 households were eligible for the interview although 20,250 houses were approached. Floodwater undermined three clusters, resulting in the loss of 90 households. As such, 20,160 households with 8,347 children were enrolled in the study. Of those enrolled, 26 children were eliminated due to visitors and non-surviving children. Finally, 8,321 observations were obtained for conducting this study (Figure 1).
In the public health sector, despite many challenges in socio-demographic conditions, Bangladesh coined huge success from the liberation of 1971, decreasing pregnancy and maternal deaths (39). Table 1 presents the results of the chi-square analysis for identifying household factors associated with ARI. The results of the chi-square analysis indicate the regional distribution, media accessibility, toilet facility, types of cooking fuel, wealth index, electricity accessibility, types of roof material, and types of wall material are statistically significant (p < 0.05) factors. Among 8,321 children, 73.04% were from rural areas and 26.96% from urban areas. By region of the country, 25.38% were from Dhaka, 20.99% from Chittagong, 11.67% from Rajshahi, 10.56% from Rangpur, 9.23% from Khulna, 8.48% from Mymensingh, 8.15% from Sylhet, and 5.55% from Barisal. We also found that 51.76% of the household has media accessibility and 48.24% does not have any type of media accessibility in their household. Furthermore, 90.30% used tube well sources of water, 6.63% of respondents used piped sources of water, and 3.07% used other sources of water. From our results, we observed that 70.52% has unimproved toilet facilities, and 29.48% had improved toilet facilities. According to wealth status, 41.77% are from the poorest households, 44.68% were from the 25–34 years age group and 7.86% were from the 45 years or above age group. By wealth status, 41.77% are from the lower wealth category families, 39.36% are children from higher wealth category families, and 18.86% are from middle-class families. About 78.97% used solid cooking fuel, and 82.32% has electric accessibility.
Most mothers (79.68%) of the children were from the 15–24 years age group, 44.68% were from the 25–34 years age group, and 7.86% were from the ≥45 years age group. A large group of mothers (79.68%) was vaccinated, whereas a few (20.32%) were not. As for parents' education characteristics, 48.64% of respondents had primary education, 15.81% had secondary or higher education, and 35.55% of respondents were uneducated. According to mothers' education status, 77.89% of household heads were industrial workers, 19.89% were agricultural workers, and only 2.22% were unemployed. Among all household heads, 49.29% of household heads had no education (Table 1). In total, 58.47, 20.19, and 21.34% of children were included from the 24–59 months, 12–23 months, and 0–11 months age groups, respectively. There were 52.16% of male children, and 30.72% were stunted. The birth order distribution of children was 87.5% in the 1–3 group, 59.3% were born at a health facility, 69.95% were delivered at a normal weight, and 66.61% and 47.84% were female children delivered by normal delivery (Table 1).
Table 1 shows the relationship between the incident of ARI with different household, maternal, and child characteristics. From our chi-square test, region of the country, media accessibility, toilet facility, type of cooking fuel, wealth index, electricity availability, roof materials type, vaccination, mothers' occupation, education of household head, child age, and sex of the child showed a statistically significant effect on ARI (P < 0.05). This study found that the highest prevalence (5.98%) of ARI was observed in children living in Rangpur–those who were infected by ARI in the last 2 weeks of the survey, and was the lowest (1.74%) in Khulna. ARI depends on the Child's household with media accessibility. Children who live with media access had ARI at a rate of 3.65% but those children who live without media accessibility (2.26%) had lower ARI. Toilet facility and wealth index significantly influence ARI diseases. The proportion of getting ARI among children and households with poor and unhygienic toilets was 3.39% whereas with hygienic toilets was 2.01%. The proportion of exposure to ARI was relatively lower (2.27%) in children with a high family wealth index compared to the middle or poor. This infers wealthy families spend more money to improve the health and nutritional standards of their children and acquire clean energy sources for cooking and heating purposes, thus reducing exposure to ARI.
According to Aziz et al. (57), about 19% of households used clean cooking while WHO guidelines described proper fuel usage without much air pollution (58). The wider access to clean cooking systems for all people by 2030 is one of the important targets in the Sustainable Development Goal (SDG) 7. In total, 86.3% of households consume solid fuels whose children suffer from ARI–among them, 3.4% use wood/straw, and 2.3% use animal dung (Figure 2). Currently, 2.7 billion households lack access to use clean cooking around the world, while the maximum number of people uses solid fuels, including charcoal, peat, wood, coal, corn, rye, wheat, and other grains.
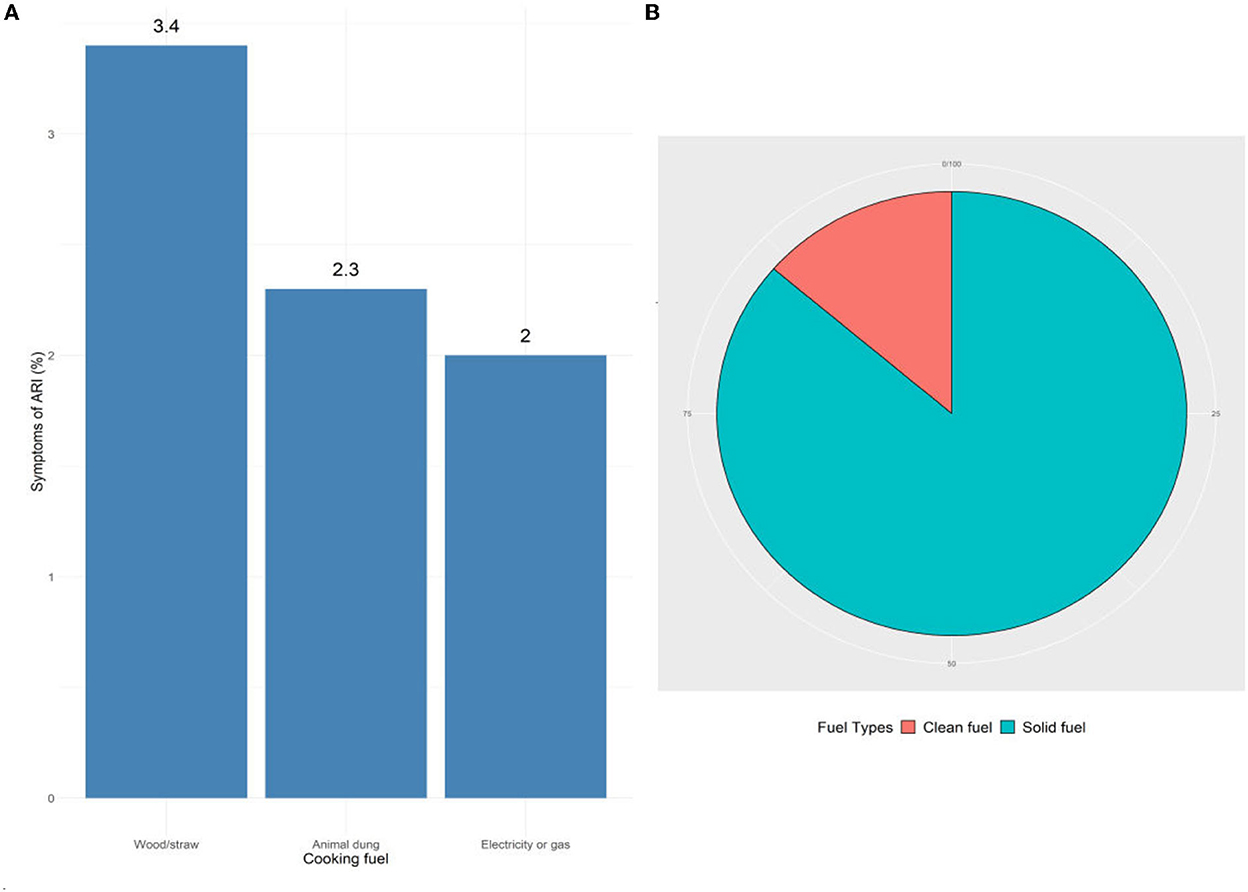
Figure 2. Fuel types used in ARI-infected children's household in the study area. (A) All fuel types, (B) clean and solid fuel.
Solid fuel is found in a variety of forms and is comparatively easier to use and cheaper but heavier to transport than liquid fuel. The Rangpur and Barisal regions of Bangladesh have the highest prevalence of solid fuel consumption, whereas the Dhaka region has the lowest prevalence (Figure 3). The northern division of Bangladesh Rangpur shows the maximum ARI infection rate, while the capital of Bangladesh Dhaka and the southern part of Khulna reveals the lowest infection with ARI. The results show the ARI infection rate is moderate in Rajshahi and Barisal.
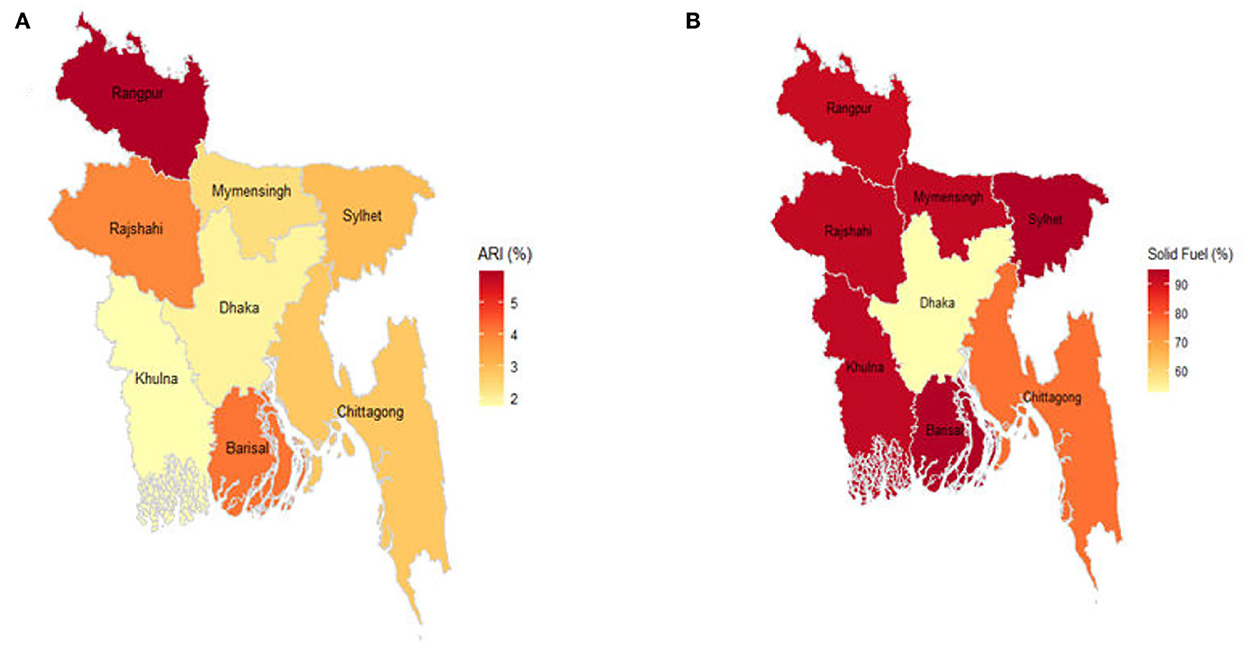
Figure 3. Prevalence of ARI and solid fuel (%) in different regions of Bangladesh. (A) ARI. (B) Solid fuel.
According to the results of the Rao-Scott chi-squared independence test, the prevalence of ARI is significantly associated (P < 0.05) with the type of fuel used in the home (Table 1).
The VIF results demonstrated no multicollinearity in the final multivariable logistic model (Table 2). The classification accuracy is acceptable with an AUC value of 0.61. The model also passed the Hosmer and Lemeshow goodness-of-fit test (value = 8.2419, degrees of freedom = 8, P = 0.760), indicating no lack of fit (Tables 2, 3; Figure 4).
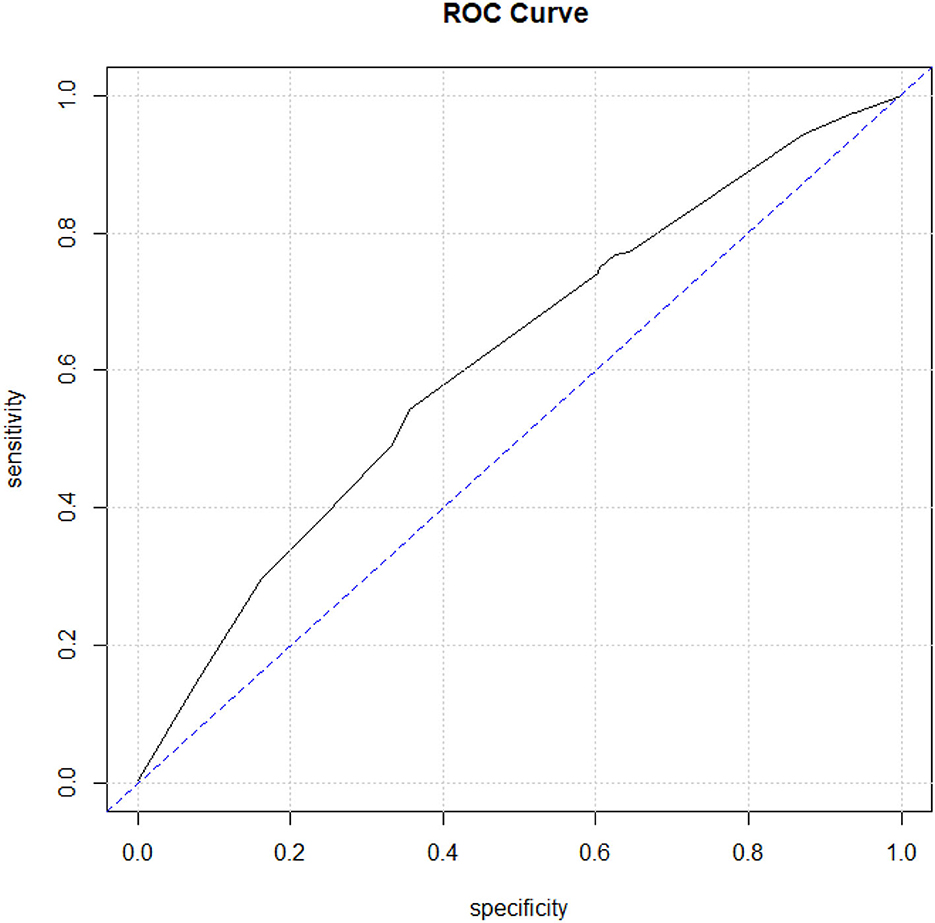
Figure 4. Model evaluations using the receiver operating characteristic curve (ROC curve). X-axis indicates specificity, whereas Y-axis indicates sensitivity.
According to (18), about 50,320 (4.9%) child deaths are attributed annually to fuel in Ethiopia (28). This cross-section-based research study also proved that biomass fuel and ARI were correlated in 422 households in the slum of Addis Ababa from January to February 2012. Table 4 demonstrates the crude and adjusted association between household fuel use and ARI among children under-5 years in Bangladesh. In crude analysis, the solid fuel risk group in household fuel type is associated with 1.69 times higher odds of ARI than the clean fuel risk group (COR: 1.69; 95% CI: 1.06–2.71). After adjusting the model for potential confounders and risk factors, we observe 1.69 times the odds of ARI among those children from the solid fuel risk group in households than those from clean fuel (AOR: 1.69; 95% CI: 1.05–2.72) (Table 4).
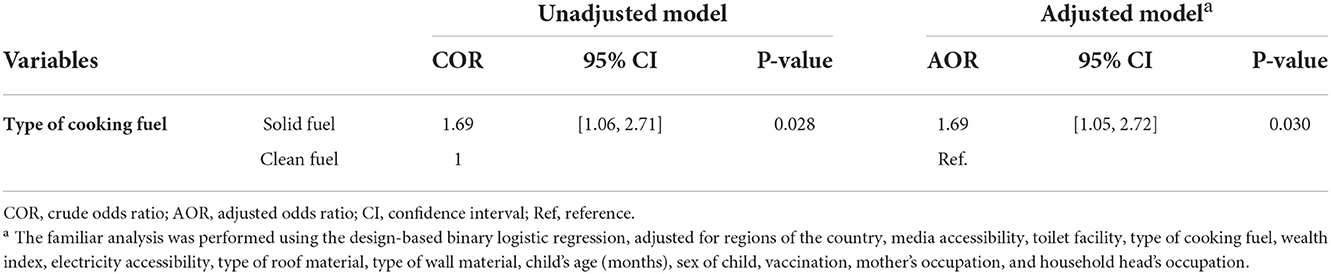
Table 4. Association between the household type of fuel use and ARI among under-5 years children in Bangladesh.
Human respiratory-related infections (RTIs) are known as the most familiar human infections, while ARIs are found in the upper and lower side of respiratory tract. The population compactness of Bangladesh is 1,265 sq/km with a total of 165 million as of 04 July 2022 (56, 59). Of the study households, solid fuel (i.e., coal/lignite, charcoal, wood, straw/shrubs/grass, agricultural crops, and animal dung) is the most widely used fuel for cooking in Bangladesh. Biomass burning inside homes generates high-magnitude concentrations of harmful substances, such as CO (an 8-h average: about 40.7 ppm SD: 40.0 ppm), PM 2.5, and PM 10, exceeding WHO Indoor Air Quality Standards (57). This stimulates an inflammatory response in the airways (60) and greater tissue damage favoring the development of respiratory diseases (61).
These findings show an association between solid fuel consumption in households and ARI episodes in children under-5 years old, which is consistent with previous studies (62). A few studies, however, have failed to establish a relationship between smoke and ARI (63). A follow-up study in Kenya developed an exposure-response function between exposure to particles from biomass fuel combustion and ARI (21). The prevalence of ARI is greater in children who live in households that use solid fuel. A national representative sample of a Bangladesh Urban Health Survey conducted in 2013 reported 39.5% of solid fuel users in urban areas while 60.5% as clean fuel users (64). More than half of households in India and Nepal use 54% (2015–2016) and 66% (2016) solid fuel for cooking.
In our study, we observe that ARI is more frequent in the case of children of uneducated mothers. According to a study conducted by Johns Hopkins University's Department of International Health, most mothers believe that a “wind-carrying sickness” may kill their children, but ARI is deemed to be more controllable, and this is due to illiteracy (65). The government's effort to educate girls beyond the secondary level is a requirement to improve future health literacy and childcare management. In this instance, the government's free primary and secondary education program is extremely important, and it should be strengthened and expanded (66). This is likely because mothers who use vaccination programs are more aware of healthcare facilities and are more likely to seek out early consultation for children's illnesses, which may perhaps curb morbidity and mortality (67).
Our findings show that women in older age cohorts and children with higher birth order have a lower prevalence of ARI. This can be due to childcare expertise and experience acquired by older women, which is unmistakably advantageous over younger women (66). Household wealth is defined according to the respondent's reported household assets, which were assigned a standardized score and categorized into three categories, namely lower, middle, and higher. Being overweight or obese (BMI ≥ 25 kg/m2) is a rising issue connected with the risk of ARIs (68).
In our study, the incidence of ARI was found superior in stunted infants, wasted infants, and infants with low birth weight. Stunting is linked to a long period spent in poor environmental circumstances alongside a low socioeconomic level as a child (69). ARI bouts that are more frequent and long-lasting may cause growth retardation. Moreover, other nutritional disorders were also found to be associated with ARI. Malnutrition was found to be strongly related to ARI in this investigation, as it has been in prior studies (19). A study in the Philippines included age-stratified risks in children ≤ 23 months of age and reported the highest risk of deaths from ARI due to malnutrition among those aged 12–22 months (18). A study conducted in New Delhi, India, exposed severe malnutrition as the forecaster of mortality in ARI in 2-week to 5-year-old children. Overall, malnutrition is associated with a 2- to 3-fold increase in ARI mortality (70).
The studies differ in terms of the plan, exposure dimension, and result evaluation, and the recent findings concerning the relationship between solid fuel consumption and the occurrence of acute respiratory diseases are parallel to most research findings in India (OR 4.0, 95% CI 2.0–7.9), Zimbabwe (OR 2.1, 95% CI 1.5–3.1), Nepal (OR 2.3, 95% CI 1.8–2.9), Gambia (OR 5.2, 95% CI 1.7–15.9), and a meta-analysis-based research studies (OR 2.3, 95% CI 1.9–2.7) (17–23). The safe fuel and adapting to it necessitating significant behavioral changes and other factors must be considered as part of broader initiatives, such as reforming kitchen structure, upgrading knowledge, as well as boosting the adequate and satisfactory level of awareness among household family members and broader communities, which can facilitate lowering the risk of air pollution and concomitant childhood ARI prevalence.
This is the first research that assesses the association between exposure to solid fuel and ARI episodes in children aged under-5 years in Bangladesh. We used a sufficiently large nationally representative dataset that reflects Bangladesh's whole population. We also considered a wide range of factors that influence the public's knowledge of the issue. We also looked at model-fitting criteria, which were mostly absent in the literature. Despite this, there were certain limitations to our research. Because we used secondary data, we had no control over the variable selection, data quality, or measurement indication. Besides, environmental and behavioral factors were missing, which are important in exposure assessment. Furthermore, the fluctuating economic performance in Bangladesh could have shifted the level of fuel used among households.
This study shows that solid fuel is significantly associated with an increased risk of ARI in children under the age of five in Bangladesh, which underscores the demand for clean and alternative cooking fuels to reduce the occurrences of ARI diseases, especially in rural and poor households. Even though such association requires further investigation using more specific measures of exposure to smoke and clinical measures of ARI, this study has crucial implications for the preventative measures of ARI among children in Bangladesh as a significant portion of households use solid fuel for cooking in the country's rural areas. Short-term measures such as using efficient burners and instructing mothers about keeping children away while cooking might help lower the prevalence of ARI and accompanying morbidity and death. Long-term interventions for shifting to cleaner and safer fuels could be established, which may include infrastructural and economic progress. Our study also shows that ARI, which is currently prevalent on a wide scale, is on the rise. Hence, the government could devote high attention to ARI control and prevention as a top priority.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
AA: formal analysis and writing—original draft. AM and SM: data curation. MS and SM: writing and reviewing. SM: methodology. KS, AM, AA, and KD: reviewing and editing. All authors contributed to the article and approved the submitted version.
This study was funded by KTH Royal Institute and supported by President Abdul Hamid Medical College Hospital, Kishoreganj, Bangladesh.
We acknowledge MEASURE DHS, NIPORT, and Bangladesh Bureau of Statistics for allowing us to use the data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.985445/full#supplementary-material
1. Ahmed F, Islam MA, Kumar M. First detection of SARS-CoV-2 genetic material in the vicinity of COVID-19 isolation centre in Bangladesh:variation along the sewer network. Sci Total Environ. (2021) 776:145724. doi: 10.1016/j.scitotenv.2021.145724
2. Chan-Yeung M, Yu WC. Outbreak of severe acute respiratory syndrome in Hong Kong Special Administrative Region: Case report. BMJ. (2003) 326:850–2. doi: 10.1136/bmj.326.7394.850
3. Sehgal V, Sethi GR, Satyanarayana L. Predictors of mortality in subjects hospitalized with acute lower respiratory tract infections. Indian Pediatr. (1997) 34:213–9.
4. Rashid SF, Hadi A, Afsana K, Ara Begum S. Acute respiratory infections in rural Bangladesh: Cultural understandings, practices and the role of mothers and community health volunteers. Trop. Med Int Heal. (2001) 6:249–55. doi: 10.1046/j.1365-3156.2001.00702.x
5. Juvonen R, Bloigu A, Peitso A. Risk factors for acute respiratory tract illness in military conscripts. Respirology. (2008) 13:575–80. doi: 10.1111/j.1440-1843.2008.01299.x
6. Chakraborty S, Chandran D, Mohapatra RK, Islam MA, Alagawany M, Bhattacharya M, et al. Langya virus, a newly identified Henipavirus in China - Zoonotic pathogen causing febrile illness in humans, and its health concerns: Current knowledge and counteracting strategies – Correspondence. Int J Surg. (2022) 105:106882. Available online at: https://linkinghub.elsevier.com/retrieve/pii/S1743919122006598
7. Chakraborty S, Mohapatra RK, Chandran D, Alagawany M, Sv P, Islam MA, et al. Monkeypox vaccines and vaccination strategies: Current knowledge and advances. An update – Correspondence. Int J Surg. (2022) 105:106869. Available online at: https://linkinghub.elsevier.com/retrieve/pii/S174391912200646X
8. Chakraborty S, Chandran D, Mohapatra RK, Yatoo MI, Islam A, Sharma AK, et al. Marburg virus disease – A mini-review. J Exper Biol Agri Sci. (2022) 10:689–96. doi: 10.18006/2022.10(4).689.696
9. Chandran D, Dhama K, Aslam M. Monkeypox : an Update on current knowledge and research advances. J Exp Biol Agric Sci. (2022) 10:679–88. doi: 10.18006/2022.10(4).679.688
10. Campe H, Heinzinger S, Hartberger C, Sing A. Clinical symptoms cannot predict influenza infection during the 2013 influenza season in Bavaria, Germany. Epidemiol. Infect. 144, no. 5:1045–1051, Apr. (2016). doi: 10.1017/S0950268815002228
11. Gonzales R, John Bart G. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med. (2001) 134:490–4. doi: 10.7326/0003-4819-134-6-200103200-00015
12. IHME. University of Washington: GBD, 2021. (2021). Available online at: https://vizhub.healthdata.org/gbd-compare/.
13. WHO. World health statistics 2019: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization. (2019).
14. Shaddick G, Thomas ML, Mudu P, Ruggeri G, Gumy S. Half the world's population are exposed to increasing air pollution. NPJ Clim Atmos Sci. (2020) 3:23. doi: 10.1038/s41612-020-0124-2
15. Cowley L, Afrad M, Rahman S. Genomics, social media and mobile phone data enable mapping of SARS-CoV-2 lineages to inform health policy in Bangladesh. Nat Microbiol. (2021) 6:1271–8. doi: 10.1038/s41564-021-00955-3
16. Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. (2001) 33:757–62. doi: 10.1086/322627
17. Zhang L, Mendoza-Sassi R, Santos JCH, Lau J. Accuracy of symptoms signs in predicting hypoxaemia among young children with acute respiratory infection: a meta-analysis. Int J Tuberc. Lung Dis. (2011) 3:317–25. doi: 10.3390/cli2020028
18. Sanbata H, Asfaw A, Kumie A. Association of biomass fuel use with acute respiratory infections among under- five children in a slum urban of Addis Ababa, Ethiopia. BMC Public Health. (2014) 14:1. doi: 10.1186/1471-2458-14-1122
19. Janjua NZ, Mahmood B, Dharma VK, Sathiakumar N, Khan MI. Use of biomass fuel and acute respiratory infections in rural Pakistan. Public Health. (2012) 126:855–62. doi: 10.1016/j.puhe.2012.06.012
20. da Fonseca Lima EJ, Mello M, de Albuquerque M, Lopes M, Serra G, Lima D, et al. Risk factors for community-acquired pneumonia in children under five years of age in the post-pneumococcal conjugate vaccine era in Brazil: a case control study. BMC Pediatr. (2016) 16:1–9. doi: 10.1186/s12887-016-0695-6
21. Mishra V. Indoor air pollution from biomass combustion acute respiratory illness in preschool age children in Zimbabwe. Int J Epidemiol. (2003) 32:847–53. doi: 10.1093/ije/dyg240
22. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ. (2008) 86:390–94. doi: 10.2471/BLT.07.044529
23. De Francisco A, Morris J, Hall AJ, Schellenberg JA, Greenwood BM. Risk factors for mortality from acute lower respiratory tract infections in young Gambian children. Int J Epidemiol. (1993) 22:1174–82. doi: 10.1093/ije/22.6.1174
24. Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. (2008) 86:5. doi: 10.2471/BLT.07.048769
25. Sreeramareddy CT, Shidhaye RR, Sathiakumar N. Association between biomass fuel use and maternal report of child size at birth - an analysis of 2005-06 India Demographic Health Survey data. BMC Public Health. (2011) 11:403. doi: 10.1186/1471-2458-11-403
26. Jakariya M, Ahmed F, Islam M, Wastewater Wastewater based surveillance system to detect SARS-CoV-2 genetic material for countries with on-site sanitation facilities: an experience from Bangladesh. medRxiv. (2021). doi: 10.1101/2021.07.30.21261347
27. Hossain M, Saiha T, Rahman A. Novel Mutations Identified from Whole-Genome Sequencing of SARS-CoV-2 Isolated From Noakhali, Bangladesh [Preprint]. (2021). doi: 10.21203/rs.3.rs-437228/v1
28. Goyal R, Khare M. Indoor air pollution and health effects. In: Air Pollution: Health and Environmental Impacts [Preprint]. Marcel Dekker. (2010) p. 109–134. doi: 10.1201/EBK1439809624-c4
29. Islam A, Hossen F, Rahman A, Sultana KF, Hasan MN, Haque A, et al. An opinion on wastewater-based epidemiological monitoring (WBEM) with clinical diagnostic test (CDT) for detecting high-prevalence areas of community COVID-19 Infections. Curr Opin Environ Sci Health. (2022) 100396. doi: 10.1016/j.coesh.2022.100396 [Epub ahead of print].
30. Tiwari A, Adhikari S, Kaya D, Islam MA, Malla B, Sherchan SP, et al. Monkeypox outbreak: Wastewater and environmental surveillance perspective. Sci Total Environ. (2023) 856:159166. doi: 10.1016/j.scitotenv.2022.159166
31. Chakraborty C, Bhattacharya M, Sharma AR, Roy SS, Deep Deep learning research should be encouraged for diagnosis treatment of antibiotic resistance of microbial infections in treatment associated emergencies in hospitals. Int J Surg. (2022) 105:106857. doi: 10.1016/j.ijsu.2022.106857
32. Islam A, Rahman A, Jakariya, Bahadur NM, Hossen F, Mukharjee SK, et al. A 30-day follow-up study on the prevalence of SARS-CoV-2 genetic markers in wastewater from the residence of COVID-19 patient and comparison with clinical positivity. Sci Total Environ. (2022) 159350. doi: 10.1016/j.scitotenv.2022.159350
33. Siddiky CIA. Energy scenario of Bangladesh. Geopolit. Energy South Asia. (2021) 96–110. doi: 10.4324/9781003110057-5
34. Wichmann J, Voyi KVV. Impact of cooking heating fuel use on acute respiratory health of preschool children in South Africa. South. African J Epidemiol Infect. (2006) 21:48–54. doi: 10.1080/10158782.2006.11441264
35. Bangladesh: DHS, 2017-18 - Final, Report. (2018). Available online at: https://dhsprogram.com/publications/publication-FR344-DHS-Final-Reports.cfm
37. Hossain FE, Islam S, Islam MA, Islam S, Ahmed F. Detection of virulence genes of APEC (avian pathogenic Escherichia coli) isolated from poultry in Noakhali, Bangladesh. Bioresearch Commun. (2021) 7:967–972. doi: 10.3329/brc.v7i1.54253
38. Rakib SH, Masum S, Patwari MRI, Fahima RA, Farhana A, Islam MA. Design and Development of a low cost Ultraviolet Disinfection system to reduce the cross infection of SARS-CoV-2 in ambulances. In: 2021 International Conference on Electronics, Communications and Information Technology (ICECIT). (2021) p. 1–4. doi: 10.1109/ICECIT54077.2021.9641131
39. Sakib MMH, Nishat A, Tarequl M. Computational screening of 645 antiviral peptides against the receptor-binding domain of the spike protein in SARS-CoV-2. Comput. Biol. Med.. 136, p. 104759, Sep. (2021). doi: 10.1016/j.compbiomed.2021.104759
40. Islam A, Marzan A, Sydul M, Sex-specific Sex-specific epidemiological and clinical characteristics of COVID-19 patients in the southeast region of Bangladesh. MedRxiv [Preprint]. (2021). doi: 10.1101/2021.07.05.21259933
41. BBC. Bangladesh country profile - BBC News. BBC. (2019). Available online at: https://www.bbc.com/news/world-south-asia-12650940
42. Climate, - Banglapedia,. National Encyclopedia of Bangladesh. Available online at: https://en.banglapedia.org/index.php/Climate
43. Geography of Bangladesh (Wikipedia). Wikipedia. (2017). Available online at: https://en.wikipedia.org/wiki/Geography_of_Bangladesh
44. Kamruzzaman M, Mandal T, Rahman TMS A, Abdul Khalek M, Alam GMM, Rahman MS. Climate Modeling, Drought Risk Assessment and Adaptation Strategies in the Western Part of Bangladesh. Climate Vulnerability and Resilience in the Global South (2021). p. 21–54. doi: 10.1007/978-3-030-77259-8_2
45. Shahid S, Khairulmaini OS. Spatio-temporal variability of rainfall over Bangladesh during the time period 1969-2003. Asia-Pacific J Atmos. Sci. (2009) 43:375–89.
46. DHS. Household Drinking Water. Guide to DHS Statistics DHS-7. (2019). Available online at: https://dhsprogram.com/data/Guide-to-DHS-Statistics/Household_Drinking_Water.htm
49. Roy S, Rahman MA, Begum R. Arachidonic acid supplementation attenuates adipocyte inflammation but not adiposity in high fat diet induced obese mice. Biochem Biophys Res Commun. (2022) 608:90–95. doi: 10.1016/j.bbrc.2022.03.089
50. Roy S, Bhowmik DR, Begum R. Aspirin attenuates the expression of adhesion molecules, risk of obesity, and adipose tissue inflammation in high-fat diet-induced obese mice. Prostaglandins Other Lipid Mediat. (2022) 162:106664. doi: 10.1016/j.prostaglandins.2022.106664
51. Chakraborty S, Chandran D, Mohapatra„, Langya virus a newly identified Henipavirus in China - Zoonotic pathogen causing febrile illness in humans its health concerns: Current knowledge counteracting strategies – Correspondence. Int J Surg. (2022) 105:106882. doi: 10.1016/j.ijsu.2022.106882
52. Chakraborty S, Mohapatra RK, Chandran D, Alagawany M. Monkeypox vaccines vaccination strategies: Current knowledge advances. An update – Correspondence. Int J Surg. (2022) 105:106869. doi: 10.1016/j.ijsu.2022.106869
53. De Onis M, Blössner M. WHO Global Database on Child Growth and Malnutrition. Geneva: Program Nutr World Heal Organ. (1997).
54. Hasan MN, Abdul Baker Chowdhury M, Jahan J, Jahan S, Ahmed NU, Uddin MJ. Cesarean delivery and early childhood diseases in Bangladesh: An analysis of Demographic and Health Survey (BDHS) and Multiple Indicator Cluster Survey (MICS). PLoS ONE. (2020) 15:1–13. doi: 10.1371/journal.pone.0242864
55. Haque MA, Wang F, Chen Y. Bacillus spp. contamination: a novel risk originated from animal feed to human food chains in South-Eastern Bangladesh. Front Microbiol. (2022) 12. doi: 10.3389/fmicb.2021.783103
56. Jakariya M, Ahmed F, Islam A. Wastewater-based epidemiological surveillance to monitor the prevalence of SARS-CoV-2 in developing countries with onsite sanitation facilities. Environ Pollut. (2022) 119679. doi: 10.1016/j.envpol.2022.119679
57. Aziz S, Barua S, Chowdhury SA. Cooking energy use in Bangladesh: Evidence from technology and fuel choice. Energy. (2022) 250:123696. doi: 10.1016/j.energy.2022.123696
58. Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: Chi-squared tests for goodness of fit independence in two-way tables. J Am Stat Assoc. (1981) 76:221–30. doi: 10.1080/01621459.1981.10477633
59. Ahmed F, Aminul Islam M, Kumar M, Hossain M, Bhattacharya P, Tahmidul Islam M, et al. First detection of SARS-CoV-2 genetic material in the vicinity of COVID-19 isolation centre through wastewater surveillance in Bangladesh. medRxiv [Preprint]. (2020). doi: 10.1101/2020.09.14.20194696
60. Woolley K, Bartington SE, Pope FD, Price MJ, Thomas GN, Kabera T. Biomass cooking carbon monoxide levels in commercial canteens in Kigali, Rwanda. Arch Environ Occup Health. (2021) 76:75–85. doi: 10.1080/19338244.2020.1761279
61. Juginović A, Vuković M, Aranza I, Biloš V. Health impacts of air pollution exposure from 1990 to 2019 in 43 European countries. Sci Rep. (2021) 11:22516. doi: 10.1038/s41598-021-01802-5
62. Andualem Z, Nigussie Azene Z, Dessie A, Dagne H, Dagnew B. Acute respiratory infections among under-five children from households using biomass fuel in Ethiopia: systematic review and meta-analysis. Multidiscip Respir Med. (2020) 15:710. doi: 10.4081/mrm.2020.710
63. Po JYT, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. (2011) 66:232–9. doi: 10.1136/thx.2010.147884
64. Ezzati M, Kammen DM. Indoor air pollution from biomass combustion and acute respiratory infections in Kenya: an exposure-response study. Lancet. (2001) 358:619–24. doi: 10.1016/S0140-6736(01)05777-4
65. NIPORT. Bangladesh Urban Health Survey 2013 Final Report — MEASURE Evaluation.” (2015). Available online at: https://www.measureevaluation.org/publications/tr-15-117.html
66. Srivastava P, Mishra AK, Kumar Roy A. Predisposing factors of community acquired pneumonia in under-five children. J Lung Dis Treat. (2015) 1:1. doi: 10.4172/2472-1018.1000101
67. Bbaale E. Determinants of diarrhoea and acute respiratory infection among under-fives in uganda. Australas Med J. (2011) 4:400–9. doi: 10.4066/AMJ.2011.723
68. Mengistie B, Berhane Y, Worku A. Prevalence of diarrhea associated risk factors among children under-five years of age in Eastern Ethiopia: a cross-sectional study. Open J Prev Med. (2013) 03:446–53. doi: 10.4236/ojpm.2013.37060
69. Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infectious Dis. (2002) 2:1. doi: 10.1016/S1473-3099(01)00170-0
Keywords: developing countries, solid fuels, clean fuels, under-five children, acute respiratory infection (ARI)
Citation: Islam MA, Hasan MN, Ahammed T, Anjum A, Majumder A, Siddiqui MN-E-A, Mukharjee SK, Sultana KF, Sultana S, Jakariya M, Bhattacharya P, Sarkodie SA, Dhama K, Mumin J and Ahmed F (2022) Association of household fuel with acute respiratory infection (ARI) under-five years children in Bangladesh. Front. Public Health 10:985445. doi: 10.3389/fpubh.2022.985445
Received: 04 July 2022; Accepted: 17 October 2022;
Published: 01 December 2022.
Edited by:
Atin Adhikari, Georgia Southern University, United StatesReviewed by:
M. Nazmul Hoque, Bangabandhu Sheikh Mujibur Rahman Agricultural University, BangladeshCopyright © 2022 Islam, Hasan, Ahammed, Anjum, Majumder, Siddiqui, Mukharjee, Sultana, Sultana, Jakariya, Bhattacharya, Sarkodie, Dhama, Mumin and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Prosun Bhattacharya, cHJvc3VuQGt0aC5zZQ==; Mohammad Nayeem Hasan, bmF5ZWVtNTg0N0BnbWFpbC5jb20=; Md. Aminul Islam, YW1pbnVsbWJnQGdtYWlsLmNvbQ==; YW1pbnVsQHBhaG1jLmVkdS5iZA==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.