- 1Department of Clinical Midwifery School of Midwifery, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Maternity Case Team, Metema General Hospital, Amhara Regional Health Bureau, Bahir Dar, Ethiopia
Background: Iron deficiency accounts for about half of anemia cases worldwide. Iron and folate supplementation can effectively control and prevent anemia during pregnancy. Despite the efforts to reduce iron deficiency anemia during pregnancy, only a few women took an iron supplement as recommended. The aim of this study is to assess adherence to iron-folic acid supplementation and associated factors.
Methods: A facility-based cross-sectional study was conducted from April 1 to May 31, 2021, among pregnant women attending the antenatal care clinic at Metema district governmental health institutions. Data was collected through face-to-face interviews with an interviewer-administered questionnaire. Epi info version 7.1 and SPSS 20 were used for data entry and analysis. Binary logistic regression analysis was done to identify factors associated with iron-folic acid supplementation for pregnant women. Significant associations were determined based on the adjusted odds ratio (AOR) and 95% confidence, with a p-value < 0.05.
Results: The proportion of pregnant women adhering to iron-folic acid supplementation was 34.9% (95% CI: 31, 38.8%). Maternal educational status [AOR = 6.09, 95% CI (3.26, 11.4)], time of first antenatal consultation [AOR = 1.95, 95% CI (1.25, 3.06)], having good knowledge of iron with folic acid supplementation [AOR = 2.80, 95% CI (1.83, 4.28)], having a good understanding of anemia [AOR = 1.61, 95% CI (1.06, 2.43)], and a history of anemia during current pregnancy [AOR = 2.31, 95% CI (1.36, 3.94)] were factors affecting iron-folic acid supplementation adherence.
Conclusions: Iron-folic acid supplementation adherence was low in the study area. Increasing maternal awareness, having good knowledge about the benefits of iron-folate supplements, and early registration to antenatal care were positive determinants of iron with folic acid adherence.
Introduction
Iron with folic acid (IFA) adherence measures how closely clients comply with the dosage and timing of iron-folate supplements as advised by their healthcare providers (1). If a woman takes 65% or more of the iron-folic acid supplement, which equates to taking the supplement at least 4 days a week, she is considered adherent to the supplement (2).
Iron deficiency anemia is a disorder where the body produces fewer red blood cells due to a lack of iron. A necessary nutrient for the production of hemoglobin is iron (1). Anemia occurs when the blood's hemoglobin concentration is lower than usual due to a lack of one or more crucial nutrients (3). Anemia is pervasive in public health issues and linked to a higher risk of morbidity and mortality, particularly in young children and pregnant women. More than 2 billion people, or over 30% of the world's population, suffer from iron insufficiency, the most common nutrient shortage in the world, especially in developing nations (4). Due to their increased nutritional needs, pregnant women are especially at risk of iron deficiency. Anemia caused by iron deficiency has consequences on both mother and child health. Folic acid deficiency during conception and early pregnancy causes a higher risk of neural tube abnormalities and other poor pregnancy outcomes like orofacial clefts (5).
According to the Ethiopian Demographic and Health Survey (EDHS) 2016, 23% of Ethiopian women between the ages of 15 and 49 are anemic. One-seventh of the population (15%) is slightly anemic, 5% are seriously anemic, and < 1% are severely anemic. In rural settings, 25% of women have some form of anemia, compared to 16% in urban areas (6). Since it is hard to meet the need for iron during pregnancy solely by dietary intake, iron-folic acid supplementation is a widely advised intervention to address this problem (7).
Therefore, giving iron and folic acid in the form of tablets to pregnant women is the most effective mass intervention for iron supplementation. These increase hemoglobin levels, allowing for the possible reduction in the level of anemia at term (8).
All pregnant women have been advised to take a daily supplement containing 400 μg of folic acid and 30–60 mg of elemental iron for 6 months by the World Health Organization. Supplemental iron and folic acid should be used with malaria prevention, detection, and treatment strategies (9).
The main issue with iron-folate supplementation during pregnancy is adherence because women frequently forget to take the supplements regularly as directed by their healthcare providers. This is the probable cause of the high prevalence of anemia among pregnant mothers.
Methods
Study design and setting
A facility-based cross-sectional study was conducted in Metema district governmental health institutions located in the West Gondar Zone of the Amhara Regional State, Ethiopia, from April 1 to May 31, 2021. Metema district is 897 km north of Addis Ababa and 197 km from Gondar town. The district has one general hospital and five health centers.
Sample size determination and sampling technique
The sample size was calculated by single population proportion formula using a 95% confidence level, a 5% margin of error, a prevalence of 37.2% (5), a design effect of 1.5, and a non-response rate of 10%. Four health centers (Gendawuha, Kokit, Metema Yohannes, and Shinfa) were selected randomly for the study by lottery method. Study participants were selected using a systematic and simple random sampling method. Reports of the 2 months of the study period were taken from each selected health institution to allocate the sample proportionally. The total number of pregnant women attending the antenatal care (ANC) clinic was 1,318. The required minimum sample size in the institutions was n = 593; an interval of k = N/n = 1,318/593 = 2 was used to select the study participants. The first study participant was selected using the lottery method and then every other woman was included. All pregnant women attending routine antenatal care follow-up for the current pregnancy and who took IFA supplementation (IFAS) at least for a month during the study period were the study population. All pregnant women who took IFAS at least for a month and had ANC follow-ups at Metema district governmental health centers were included in the study. Adherence to IFAS was defined as pregnant women taking IFAS tablets at least four times per week in the previous month preceding the study (2, 5, 8).
Data collection method
Face-to-face interviews were used to gather data using a pretested questionnaire. The questionnaire was prepared after reviewing the literature (3–7, 9). To make the questionnaires clear, it was first prepared in English and translated into the local (Amharic) language to make them simple and understandable, and then back to English to check the consistency. Five percent of the sample size in Metema primary hospital pretested the questionnaire, based on which the questionnaire underwent necessary corrections.
Four BSc nurses and two supervisors collected the data. The data collectors and supervisors received a one-day training. The pregnant women were interviewed before they got their regular service/examination.
Statistical analysis
Epi-info version 7.1 software was used to enter the data which was exported into SPSS version 20 software for statistical analysis and interpretation. The sociodemographic variables of pregnant women were analyzed with descriptive statistics. Binary logistic regression analysis was used to determine the association of independent variables with IFAS as a dependent variable. Variables that were significant in binary logistic regression with a p-value < 0.25 were considered for multivariable logistic regression analysis. To demonstrate the strength of the association, crude odds ratio (COR) and adjusted odds ratio (AOR), together with the 95 percent confidence interval, were calculated. Variables having a p-value of 0.05 or lower were deemed statistically significant in the multivariable logistic regression analysis.
Ethical consideration
The institutional review board (IRB) of the University of Gondar College of Medicine and Health Sciences granted ethical approval with the reference number (SMidw/53/2013). A permission letter was also obtained from the Metema district health office. Anonymity was used to protect the confidentiality of the study participant's data. Written informed consent was taken from the study participants. The data was not used for any other purpose other than the designed study.
Results
Sociodemographic characteristics of pregnant women
A total of 575 pregnant mothers took part in the study yielding a 97% response rate. The average age of the pregnant women was 27.1 with (SD) ±5.57 years old. More than half of the participants 300 (52.2%) were in the age group of 25–34 years. About 367 (63.8%) were Orthodox Christian followers and two-thirds (383, 66.6%) were urban residents. About 322 (56%) of the mothers had >1,000 birr monthly income (Table 1).
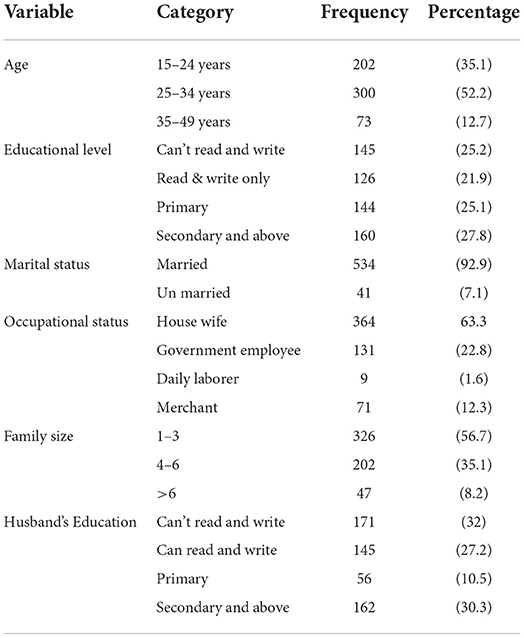
Table 1. Socio-demographic characteristics of pregnant women attending ANC clinic in governmental health institutions of Metema district, Northwest Ethiopia, May, 2021 (N = 575).
Obstetric and health facility-related characteristics of pregnant women
The average gestational age of participants during the interview was 26.1 ±5.3 weeks. About 324 (56.3%) participants were in their second trimester. About two-fifths (229, 39.8%) of participants were primigravida. A majority (345, 60%) had a history of anemia, and an equal number t 340 (59.1%) visited the ANC clinic within 12 weeks of gestation. About two-thirds (393, 68.3%) of the respondents spent < 30 min reaching the health facility.
Adherence rate to IFAS
The adherence rate to IFA supplementation was 34.9% (95%CI, 31.0–38.8%). The leading reason for IFAS adherence was counseling (65.6%), followed by fear of illness if they missed the supplement (21.9%), and finally, family support (17.2%). Among mothers who missed the IFAS doses, the leading reason was fear of side effects (83.3%) followed by forgetfulness (40.9%).
Factors associated with adherence to IFA supplementation
Maternal education, time of ANC registration, history of anemia, the prevalence of anemia during the current pregnancy, counseling on IFA, knowledge of anemia, and knowledge of IFAS were associated with IFAS adherence in bivariable analysis at p-value < 0.25 and entered multivariable logistic regression analysis. In the multivariate logistic regression analysis, there were significant relationships between IFAS adherence and the timing of ANC registration, the prevalence of anemia during the current pregnancy, maternal education, awareness of anemia, and knowledge of IFAS.
The odds of pregnant mothers with a secondary level school education and above were six times more likely to adhere to IFAS than those who cannot read and write [AOR = 6.09 95% CI (3.26, 11.4)]. The odds of pregnant women registering earlier for ANC were 1.9 times more likely to adhere to IFAS than those who registered late [AOR = 1.95, 95% CI (1.25, 3.06)]. The odds of pregnant women who were knowledgeable about anemia were 1.6 times more likely to adhere to IFAS than those who were less knowledgeable [AOR = 1.61, 95% CI (1.06, 2.43)]. Pregnant women who were knowledgeable about IFAS were 2.8 times more likely to adhere to IFAS than those less knowledgeable about IFAS [AOR = 2.80, 95% CI (1.83, 4.28)]. The odds of pregnant women who had a history of anemia during current pregnancy were 2.3 times more likely to adhere to IFAS than those who had no anemia [AOR = 2.31, 95% CI (1.36, 3.94)] (Table 2).
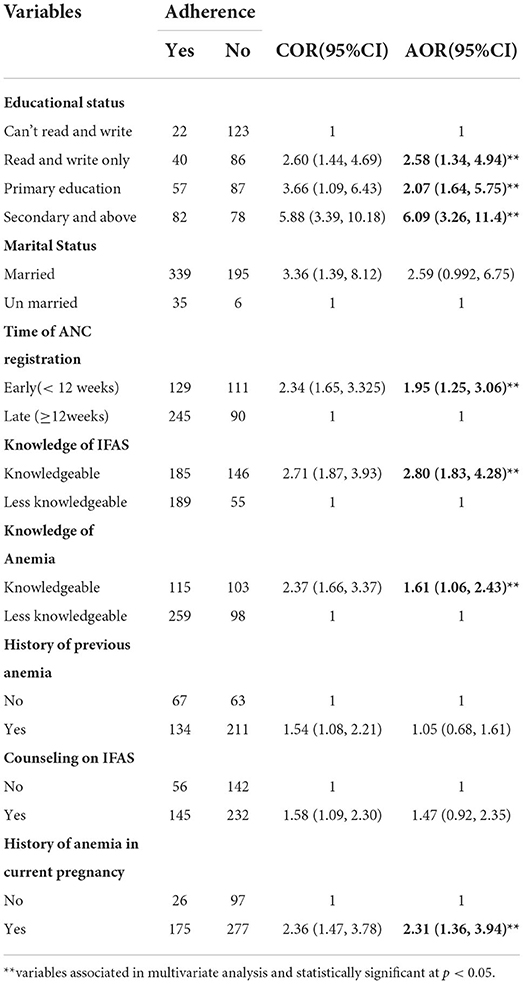
Table 2. Factors associated with adherence to IFAS among pregnant women attending ANC Clinics at Metema woreda governmental health institutions, North west Ethiopia, May 2021 (N = 575).
Discussion
Iron-folic acid supplementation adherence among pregnant mothers attending ANC clinics was 34.9% (95% CI 31.0–38.8%). The finding of this study is consistent with the findings in Tigray, Ethiopia (37.2%) (5). This might be due to the similarities in the study population, settings, and service delivery of the institutions.
However, it is higher compared with the studies done in Mecha district, Northwest Ethiopia (20.4%) (10), Afar region (22.9%) (11), Goba woreda (18%) (12), Bihar, India (24%) (13), Moshi, Tanzania (16.1%) (14) and Kiambu county, Kenya (24.5%) (15). The reason might be increased knowledge among pregnant mothers over time regarding anemia and IFA supplementation through health education, counseling, media, improved ANC service coverage, and the time difference between studies.
However, the adherence levers were lower than the studies done in Mizan Aman town (70.6%) (16), Misha district, South Ethiopia (39.2%) (17), eight rural districts of Ethiopia (74.9%) (18), Siem Reap and Kampong Cham Provinces, Cambodia (47%) (19), Indonesia (53.7%) (20), and Mangalore city, India (64.7%) (8). The variation may be dissimilarity in the design of the studies done in Misha district, South Ethiopia, and eight rural districts of Ethiopia which were community-based. The others could be explained by differences in health service delivery and the socio-economic status of study populations for the studies done in Cambodia, Indonesia, and India.
Iron-folic acid adherence was better observed among pregnant mothers who had attended secondary school and above. This finding is similar to other findings in urban slums in India, and Mecham district, Northwest Ethiopia (7, 10, 21). The reason behind this might be that educated women have good knowledge regarding the benefit of IFAS for their health and the health of the fetus. Plus, educated women have better knowledge of anemia and its effect on the health of the mother and their fetus.
Early registration for ANC services had a better effect on IFAS adherence among pregnant mothers than those who registered late. This finding is similar to several other studies done in urban slums in India, Tigray, and other areas in Ethiopia (5, 13, 21, 22). The reason may be pregnant women who had early registration for ANC services probably had more ANC visits leading to better counseling and ultimately enhancing their knowledge about anemia and IFAS.
The prevalence of anemia during the current pregnancy was another factor that increased adherence to IFAS. This finding is consistent with other studies on Mecha district, Tigray, Kiambu county, Kenya, and Moshi, Tanzania (5, 10, 14, 15). This might be due to the attention given to counseling anemic women, which increased their awareness and knowledge of iron and folic acid supplementation, and therefore they took the supplements regularly to avoid complications.
Having good knowledge about iron-folic acid supplementation led mothers to take the tablets regularly. This finding is similar to other studies done in Siem Reap and Kampong Cham Provinces in Cambodia, urban slums in India, Misha district of Ethiopia, and Mecha (10, 17, 19, 21). The possible reason is that being knowledgeable about IFAS made mothers more aware of the tablet's importance, its side effects, how to take them, and complications if missed. Being knowledgeable about anemia made the mothers adhere to iron-folic acid supplementation. A similar result was reported in Mecha district, Western Amhara (10). The probable reason could be knowledge of pregnant women about causes, consequences, and methods of prevention of anemia affected their adherence to IFA. In addition, being knowledgeable about iron and folic acid encourages individuals to prevent iron deficiency anemia and helps women to adopt a good attitude about the benefits of taking IFA supplements.
Conclusion
This study found that IFA supplementation adherence among pregnant mothers attending antenatal care is low. This study also found that maternal education, knowledge of IFAS, history of anemia in the current pregnancy, time of ANC registration, and knowledge of anemia were significant factors that were associated with adherence to IFAS during pregnancy. Therefore, antenatal care providers should continue to advise pregnant mothers to register earlier for ANC and counsel them on the importance of IFAS. Also, the district health offices should promote IFAS and anemia prevention strategies in the community through community health task forces.
Limitations
Electronic pill counting which, is the gold standard method of measuring adherence had not been used as it is expensive. Being cross-sectional, this study might not show cause-effect relations. It was also important if the nutritional assessment had been included.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the University of Gondar College of Medicine and Health Sciences. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AY conceived and designed the experiments. HT, FK, and BA contributed in investigation, analyzed and interpreted the data, and wrote the article. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank the University of Gondar for the approval of ethical clearance. Our gratitude to the Amhara regional health bureau and Metema woreda Health Office for providing the necessary information and facilitating conditions while carrying out this study. Above all, the authors' heartfelt thanks go to the study participants, who gave us their precious time. All data collectors and supervisors are highly acknowledged for the effort they put into this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, Antenatal Care; AOR, Adjusted Odds Ratio; CI, Confidence interval; COR, Crude Odds Ratio; IFA, Iron Folate Acid; IFAS, Iron Folate Acid Supplimentaion; SPSS, Statistical Package for Social Science.
References
2. Marcewicz LH, Anderson BL, Byams VR, Grant AM, Schulkin J. Screening and treatment for iron deficiency anemia in women: results of a survey of obstetrician-gynecologists. Matern Child Health J. (2017) 21:1627–33. doi: 10.1007/s10995-016-2252-1
4. WHO CfD. “Prevention Ca, Atlanta. Worldwide prevalence of anaemia 1993–2005”. In: WHO Global Database on Anaemia, eds B. de Benoist, E. McLean, I. Egli, M. Cogswel (2008).
5. Abel Gebre AM. Belachew E. Assessment of factors associated with adherence to iron-folic acid supplementation among urban and rural pregnant women in North Western zone of Tigray, Ethiopia: comparative study. Int J Nutr Food Sci. (2015) 4:161. doi: 10.11648/j.ijnfs.20150402.16
6. CSA. ETHIOPIA Demographic and Health Survey2016. Ethiopia: Central Statistical Agency Addis Ababa (2016).
7. Godara S, Hooda R, Nanda S, Mann S. To study compliance of antenatal women in relation to iron supplementation in routine ante-natal clinic at a tertiary health care center. J Drug Delivery Therapeut. (2013) 3:71–5. doi: 10.22270/jddt.v3i3.520
8. Mithra P, Unnikrishnan B, Rekha T, Nithin K, Mohan K, Kulkarni V, et al. Compliance with iron-folic acid (IFA) therapy among pregnant women in an urban area of south India. Afr Health Sci Dec. (2013) 13:880–5. doi: 10.4314/ahs.v13i4.3
9. WHO. Who Guideline: Daily Iron and Folic Acid Supplementation in Pregnant Women. Geneva: World Health Organization (2012).
10. Taye B, Abeje G, Mekonen A. Factors associated with compliance of prenatal iron folate supplementation among women in Mecha district, Western Amhara: a cross-sectional study. Pan Afr Med J. (2015) 20:43. doi: 10.11604/pamj.2015.20.43.4894
11. Gebre A. Determinants of compliance to iron-folic acid supplementation among pregnant women in pastoral communities of Afar region: the cases of Mille and Assaita districts, Afar, Etiopia. Med. Res. Chron. (2015) 4:352–62.
12. Haile MT, Jeba AB, Hussen MA. Compliance to prenatal iron and folic acid supplement and associated factors among women during pregnancy in South East Ethiopia: a cross-sectional study. J Nutr Health Food Eng. (2017) 7:00235. doi: 10.15406/jnhfe.2017.07.00235
13. Wendt A, Stephenson R, Young M, Webb-Girard A, Hogue C, Ramakrishnan U, et al. Individual and facility-level determinants of iron and folic acid receipt and adequate consumption among pregnant women in rural Bihar, India. PLoS ONE. (2015) 10:e0120404. doi: 10.1371/journal.pone.0120404
14. Ogundipe O, Hoyo C, Østbye T, Oneko O, Manongi R, Lie RT, et al. Factors associated with prenatal folic acid and iron supplementation among 21,889 pregnant women in Northern Tanzania: a cross-sectional hospital-based study. BMC Public Health. (2012) 12:481. doi: 10.1186/1471-2458-12-481
15. Dinga L, Mwangi A, Abong G. Factors Associated With Adherence to Iron/Folate Supplementation Among Pregnant Women Attending Antenatal Clinic. Kiambu County, Kenya: Thika District Hospital (2013).
16. Shewasinad NS. Adherence-and-associated-factors-of-prenatal-iron-folic-acid-supplementationamong-pregnant-women-who-attend-ante-natal-care-in-Health Facility at Mizan-Aman Town. Bench Maji Zone, Ethiopia, 2015. J Pregnancy Child Health. (2015) 4:1–5.
17. Abinet AS, Abebe Gebretsadik L, Aman Hussen M. Compliance with iron-folate supplement and associated factors among antenatal care attendant mothers in Misha District, South Ethiopia: community based cross-sectional study. J Environ Public Health. (2015) 2015:781973. doi: 10.1155/2015/781973
18. Gebremedhin S, Samuel A, Mamo G, Moges T, Assefa T. Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: a cross-sectional study. BMC Public Health. (2014) 14:607. doi: 10.1186/1471-2458-14-607
19. Lacerte P, Pradipasen M, Temcharoen P, Imamee N, Vorapongsathorn T. Determinants of adherence to iron/folate supplementation during pregnancy in two provinces in Cambodia. Asia-Pacific J Public Health. (2011) 23:315–23. doi: 10.1177/1010539511403133
20. Dibley T. Factors associated with not using antenatal iron/folic acid supplements in Indonesia. Asia Pacific J Clin Nutr. (2015) 23:678–90.
21. Alpanarani J, Dutta PP, Bansal RK. Compliance to iron supplementation among pregnant women: a cross-sectional study in Urbanslum. Natl J Commun Med. (2014) 5:457–62.
Keywords: iron-folic acid, pregnant women, adherence, anemia, metema
Citation: Yismaw AE, Tulu HB, Kassie FY and Araya BM (2022) Iron-folic acid adherence and associated factors among pregnant women attending antenatal care at Metema District, Northwest Ethiopia. Front. Public Health 10:978084. doi: 10.3389/fpubh.2022.978084
Received: 25 June 2022; Accepted: 30 September 2022;
Published: 18 November 2022.
Edited by:
Rabina Shrestha, Dhulikhel Hospital, NepalReviewed by:
Abdurahman Kedir Roble, Jigjiga University, EthiopiaPeter Mac Asaga, Freiburg University Medical Center, Germany
Copyright © 2022 Yismaw, Tulu, Kassie and Araya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayenew Engida Yismaw, YXllbmV3ZTA3QGdtYWlsLmNvbQ==
 Ayenew Engida Yismaw
Ayenew Engida Yismaw Helen Bekele Tulu2
Helen Bekele Tulu2 Fisseha Yetwale Kassie
Fisseha Yetwale Kassie