
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 11 October 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.977072
This article is part of the Research Topic Global Excellence in Public Mental Health: Asia and Australasia Volume II View all 13 articles
Background: In 2022, Shanghai was seriously affected by the coronavirus disease 2019 (COVID-19) pandemic. The government implemented citywide static management for 2 months, as well as all universities in Shanghai, which changed the normal learning and living style of sports students and led to a decline in physical activity level. As the physical activity has a strong correlation with mental health, this study aimed to investigate the current state of physical activity (PA) and mental health of the students in Shanghai University of Sport. It will try to reveal the correlation between PA and depressive symptoms, anxiety symptoms, fear of COVID-19 and smartphone addiction.
Methods: A cross-sectional survey was conducted on a random sample of 400 students who came from six different majors in May 2022 at the Shanghai University of Sport. Respondents completed the International Physical Activity Questionnaire Short Form (IPAQ-SF), the Chinese version of the 9-item Patient Health Questionnaire (PHQ-9), the Chinese version of the Generalized Anxiety Disorder Scale (GAD-7), the Chinese version of the COVID-19 Fear Scale (FCV- 19S), and the Smartphone Addiction Scale (SAS-SV). Demographics, PA, depressive symptoms, anxiety symptoms, fear of COVID-19, and smartphone addiction were compared. A binary logistic regression model was used for the further analysis.
Results: A total of 376 college students were included in the final analysis. Binary logistics analysis showed that moderate physical activity (MPA) was negatively correlated with depression (OR = 0.95, 95%CI = 0.93–0.98), anxiety (OR = 0.97, 95%CI = 0.95–0.99), fear of COVID 19(OR = 0.99, 95%CI = 0.98–0.99)and smartphone addiction (OR = 0.94, 95%CI = 0.9–0.98) (all P < 0.05). Sedentary behavior was positively correlated with smartphone addiction (OR = 1.01, P < 0.01, 95%CI = 1.001–1.004).
Conclusion: There was an association between the presence of MPA and depressive symptoms, anxiety symptoms, fear of COVID-19, smartphone addiction, and sedentary behavior associated with smartphone addiction levels. Clarifying the causal relationship between PA and mental health will require further research.
In late February 2022, a round of SARS-CoV-2 infection broke out in Shanghai. According to the Shanghai Health Commission, as of May 4, 2022, there have been more than 593,336 cumulative cases of SARS-CoV-2 infection, of which 538,450 were asymptomatic, with 503 cumulative deaths (1). COVID-19 spread rapidly on a large scale, leading to strict and comprehensive pandemic control strategies throughout the city for 2 months. The lockdown resulting in closing public places, primary and secondary schools. Universities implemented school closures and residents implemented a policy of quarantine at homes under strict control and isolation-related measures that the epidemic was effectively controlled. However, this dramatic lifestyle change might affect the wellbeing of different age groups (2). According to previous studies, measures including restriction of movement and isolation can lead to varying degrees of increased mental health problems. For instance, the prevalence of major depressive disorder and anxiety disorders during the COVID-19, respectively, reached 27.6 and 25.6%, with much higher prevalence than before the COVID-19 (3). A Canadian study of anxiety and depression symptoms in adults during the COVID-19 also found that the proportion of respondents with high to very high levels of anxiety increased from 5 to 20%, and the number of respondents reporting high levels of depression increased from 4 to 10% (4). Not only that, confinement and lockdown also tended to cause problems such as insufficient physical activities, increased sedentary behavior, excessive use of electronics, and increased fear of COVID-19 infection (5–8). Moreover, the increase of these undesirable behaviors and mental health problems may further aggravate the symptoms of depression and anxiety in the epidemic. It may seriously affect people's mental health (9–11).
As a group in society vulnerable to mental health disorders and sudden changes, the mental health of college students during the pandemic has attracted widespread attention (12). Sun et al. investigated the mental health of 1912 Chinese college students during the pandemic. They found that 46.55 and 34.73% of college students had symptoms of depression and anxiety, respectively (13). Lockdown and quarantine have led to a decrease in personal physical activity and an increase in sedentary, game-obsessed, and college students' excessive use of electronic devices. Huang et al. found in a survey of 10,357 medical college students that the rate of smartphone addiction was as high as 59.42%, accompanied by sedentary, reduced PA, and poor mental health (10). A study from Spain found that physical activities among college students during the lockdown period of COVID-19 decreased by 29.5 and 18.3% for moderate-intensity and high-intensity PA, respectively. However, the sedentary time increased by 52.7% compared to the period before the pandemic (14). It leads to cognitive impairment, depression negative emotions and other mental health problems. Therefore, it becomes very relevant about how to effectively solve college students' mental health problems during the pandemic.
With the rise of evidence-based research on the relationship between physical activities and mental health, PA showed the association with the rise of general wellbeing and enhanced perception of quality of life and mood, and could significantly alleviate anxiety and depressive symptoms (15, 16). The evidence of a significant and positive association between PA and mental health was also successively and strongly confirmed in COVID-19 pandemic (17–19). A review of previous studies implied that many studies have been conducted to investigate the PA and mental health aspects of general college students during the pandemic (13, 20–22). however, few studies have been conducted on the relationship between PA and mental health of students at sports universities. Students from sports universities belong to a special group, these students usually have better physical quality and habit of participating in sports, and their PA level is higher than that of students from ordinary universities. Some of them take courses that get involved in theoretical and practical aspects of different sports, and they have mastered certain methods of physical exercise and the ability to design training contents (23). Beyond that, some studies found that there is a significant difference in the social adaptability psychological quality between sports college students and non-sports college students, in which sports college students could cope with various stimulis and influences exerted on them by others or the external environment and have greater acceptance and carrying capacity stronger stress coping power (24), Hence, whether such populations were able to engage in regular physical activities during the COVID-19 confinement and whether they had the same mental health problems faced by the average college student should be further explored.
During this outbreak, for positive response to the epidemic prevention policy, Shanghai University of Sport implemented the most strict control measures. In addition to the epidemic control and security personnel, students could not leave the dorms without a special reason. The university was responsible for providing daily meals and deliver to every dorm, so as to reduce the personnel flow and contact, which could minimize the risk of transmission. The strict lockdown limited students' activities to their rooms. They could not process normal travel and exercise, which led to a sharp reduction in physical activity and the possibility of psychological problems that were often seen in mental health studies during the pandemic, such as depression, anxiety, excessive use of electronic products and fear of COVID-19. Therefore, whether the physical education students can process regular physical activities in a limited space and whether they have to face the same mental health problems as the ordinary university students need to be further explored. As a result, the purpose of this study was to conduct a questionnaire survey on undergraduate students at the Shanghai University of Sport during the lockdown period of the pandemic in 2022, in hope of better understanding the current situation of PA and mental health of the students and the association between different physical activity levels and mental health. It will provide basic data reference for sports colleges and universities to carry out health education, PA advice and psychological guidance for college students during the special epidemic period and the post-epidemic period.
In this study, a cross-sectional questionnaire survey of current undergraduate students with confinement was conducted at the Shanghai University of Sport from May 5 to 15, 2022, 4 weeks after strict and comprehensive pandemic control strategies for the whole area. The Shanghai University of Sport is the earliest sports university created after the founding of China, with a variety of disciplines and majors within it, and its Kinesiology program is one of the best sports majors in the country, with many students from athletes having high PA levels and exercise habits. With the consent of the university, this study randomly selected 400 students from six different majors from the 2019 to 2021 grades of Shanghai University of Sport. The selection criteria included: (a) undergraduate students; (b) Not volunteering or working for the university during the pandemic. Compared to graduate students, undergraduate students reported higher rates of emotions and behaviors related to poor mental health (25, 26). While volunteers or staff were required to complete tasks assigned by the university every day, such as meals delivery and nucleic acid testing, etc., which were not suitable for this study.
To guarantee the validity of questionnaires and ensure that respondents were able to understand the content of the questionnaires (detailed instructions are included in the measurement), the study was conducted through the students' teacher in charge who specifically administered and interpreted the questionnaires with an initial sample size of 400 students. After excluding respondents with incomplete and missing data, the information from 376 college students was finally valid.
Considering the safety issues during the pandemic, all respondents completed the questionnaires via the WeChat “Questionnaire Star” survey platform with descriptions of the survey instructions. The questionnaires included physical activity scales, depressive symptoms, anxiety symptoms, smartphone addiction, and the fear of COVID-19 scale, as well as some sociodemographic information. The respondents' guardians have been informed about the survey through the respondents' counselors prior to data collection. Subsequently, informed consent forms were sent to the respondents and their parents. After obtaining their consent, the survey was started. The purpose of this study was explained to all respondents and it was emphasized that all data collected would be analyzed in an aggregated manner and that personal information would be kept strictly confidential. This study was based on the Declaration of Helsinki and it was approved by the Ethics Review Committee of Shanghai University of Sport.
Daily PA time and sitting time were self-reported using the International Physical Activity Questionnaire Short Form (IPAQ-SF), which was developed as a surveillance instrument to measure multiple domains of PA (27, 28). The IPAQ-SF is considered a reliable instrument to assay the total amount of PA obtained in the 15–65 years people (28). The IPAQ-SF required respondents to report the frequency and duration of each PA (vigorous-intensity activities, moderate-intensity activities, and walking), as well as the duration of daily sitting during the last 7 days. The Chinese version of the IPAQ-SF has been confirmed adequately reliable and valid in previous studies (27).
Anxiety symptoms were measured using the Chinese version of the Generalized Anxiety Disorder scale (GAD-7) (29). Each item has four response options with scores ranging from 0 to 3 (0 = Not at all to 3 = Nearly every day). Each respondent could obtain a total score that ranged from 0 to 21, with a higher score indicating more severe anxiety symptoms. Total scores of 5, 10, 15, and 20 were identified as mild, moderate, moderately severe, and severe anxiety, respectively. Thus, with the cut-off point set at 5, respondents were categorized into two groups: no anxiety symptoms (GAD-7 score < 5) and anxiety symptoms (GAD-7 score ≥5). The Chinese version of GAD-7 has been widely used and well-validated in multiple studies (29), In this study, the Cronbach alpha coefficient of the GAD-7 scale = 0.895 and the correlation coefficients of the GAD-7 and PHQ-9 were 0.751 and 0.934, respectively, with acceptable reliability and convergent validity (30).
The Chinese version of the 9-item Patient Health Questionnaire (PHQ-9) was applied to measure the severity of depressive symptoms (31). A total score ranged from 0 to 27 (higher points indicating more severe depressive symptoms), with each item that could earn 0–3 points (0 = Not at all to 3 = Nearly every day). Total scores of 5, 10, 15, and 20 were identified as mild, moderate, moderately severe, and severe depressive symptoms, respectively (31). Thus, a total score of 5 was set as a cut-off point to categorize respondents into two groups: no depressive symptoms (PHQ-9 score < 5) and depressive symptoms (PHQ-9 score ≥ 5). The Chinese version of PHQ-9 has been widely used and well-validated in Chinese adolescents (32), which would be further supported by this study. The Chinese version of the PHQ-9 has been extensively used and validated among Chinese adolescents. The overall reliability coefficients Cronbach s α and McDonald's ω of this scale in this study were 0.824 and 0.86, respectively, and the correlation coefficient between PHQ-9 and GAD-7 was 0.751, implying that its reliability and convergent validity were good (33).
COVID-fear was measured via the Chinese version of the Fear of COVID-19 Scale (FCV-19S) (34, 35). It consisted of seven items, with each item that can be responded to on a five-point Likert scale (strongly disagree=1 to strongly agree = 5), with higher scores indicating a greater COVID-fear level. The scale was widely used in several countries, and a systematic review with the evidence from 16 papers including 21 countries and 16 language versions of the FCV-19S found that the different language versions of the FCV-19S were a powerful and valid tool for assessing fear of COVID-19 and did not differ significantly by age and gender (36). Beyond that, the psychometric properties of the FCV-19S have been confirmed in the Chinese population, and some scholars examined the applicability of the FCV-19S in 2,445 Chinese students, and the findings manifested good reliability (reliability and index) where item separation reliability = 1.00, item separation index = 18.44, person separation reliability = 0.88, and person separation index = 2.77. The validity of the FCV-19S was also favorable. The validity of the FCV-19S was also ideal, The mean significant correlation values for FCV-19SC and depression, anxiety, and stress were |r| = 0.467, 0.482, and 0.469, respectively (37). Thus, the FCV-19S-C was shown to be a valid measure of Chinese students' fear of COVID-19. The internal consistency of this study was good, with a Cronbach s alpha coefficient of 0.86, and its construction and criterion validity remained the acceptable limits (38).
The Smartphone Addiction Scale short version (SAS-SV) was adopted to measure the extent of smartphone addiction (39, 40). The scale contains 10 items related to smartphone addiction, with a score of 1 to 6 on a scale of “strongly disagree” to “strongly agree” (6 levels). The higher the total score, the higher the degree of smartphone addiction, using ≥33 (females) and ≥31 (males) as their classification criteria for smartphone addiction. A 2019 study showed that the SAS-SV scale was a valid scale for assessing excessive smartphone use among children and adolescents in Hong Kong, and its results indicated that the scale had good convergent validity and the CFA confirmed that the model had acceptable goodness of fit (comparative fit index = 0.96, Tucker Lewis index = 0.95, root mean square error of approximation = 0.06) (41). The scale had good reliability in this study (α = 0.81; ω = 0.78) (42).
Data analysis was performed via SPSS 26.0 software. The basic conditions of college students who attended the questionnaire survey were depicted. Then, the descriptive data were expressed as the mean and standard deviation (SD) of continuous variables, and logistic regression equations were used to analyze the association and strength between physical activity and mental health of sports university students with different degrees of physical activity as independent variables, depression, anxiety, fear of COVID-19, and smartphone addiction as dependent variables, respectively, controlling for confounding factors gender, grade, major, family residence, whether they were only children, parents' educational level, and family economic status, and so on, so as to delve into the association and strength between physical activities and mental health of students at sports universities. The test level α = 0.05.
In this study, a total of 376 questionnaires from students that were around 20 years old (20 ± 1.3) in Shanghai University of Sport were valid, including 144 (38.3%) male students and 232 (61.7%) female students. According to the result, the average scores of long sedentary time (M = 497.4, SD = 524.9), depression (M = 6.7, SD = 5.1), smartphone addiction (M = 34.1, SD = 9.2) were above the normal range. The mean value of anxiety (M = 4.5, SD = 4.4) was kept in the normal range. The average scores in fear of COVID-19 was 2.2 ± 0.8. The daily mean time to perform low to moderate intensity PA was 5.5 (SD = 20.1) min, 12.7 (SD = 23.4) min, and 12 (SD = 21.9) min, respectively, as detailed in Table 1.
Binary logistic regression analysis showed that moderate-intensity physical activities was negatively associated with depression (OR = 0.95, 95% CI = 0.93–0.98), anxiety (OR = 0.97, 95% CI = 0.95–0.99), COVID-19 (OR = 0.99, 95% CI = 0.98–0.99) fear and smartphone addiction (OR = 0.94, 95% CI = 0.9–0.98) were negatively associated (all P-values < 0.05), and sedentary behavior was positively associated with smartphone addiction (OR = 1.01, P < 0.01, 95% CI = 1.001–1.004), after adjusting the model to control for statistically significant characteristic variables such as grade, whether the child was an only child, parental literacy, and family economic status. The results did not change significantly, as detailed in Table 2.
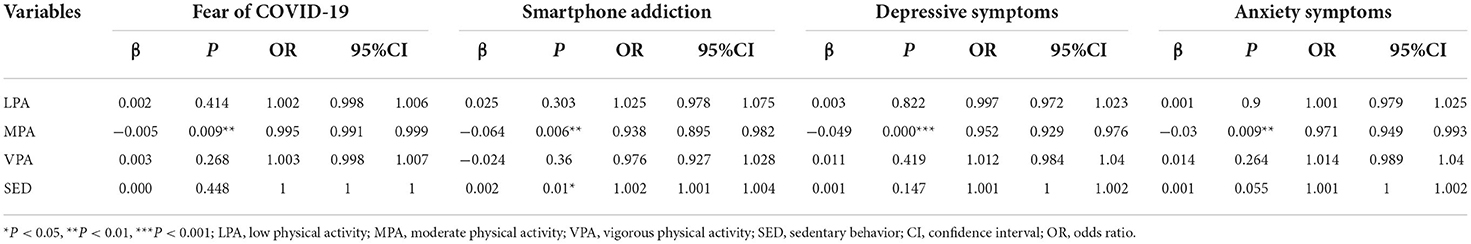
Table 2. Associations between LPA, MPA, VPA, and SED with fear of COVID-19, smartphone addition, depressive symptoms and anxiety symptoms.
Upholding data from a sample of college students at the Shanghai University of Sport during the confinement period of Shanghai from May 5 to May 15, 2022, the purpose of this study was to determine the relationship between PA and depressive symptoms, anxiety symptoms, COVID-19 fear, and smartphone addiction. It was found that MPA was negatively associated with depressive symptoms, anxiety symptoms, smartphone addiction, COVID-19 fear, and a positive association between sedentary and smartphone addiction. Possible explanations for these results were discussed below.
Shanghai has implemented a series of strict and comprehensive pandemic control strategies to reduce the transmission and infection rate of COVID-19 in 2022. With the purpose of making sure the gathering and contact of people, the university arranged three meals per day by building, time and area during the control period, with uniform delivery to the door of the dormitory, and all school students could not leave the dormitory under the control of the strict policy. The adoption of such a closed management policy may lead to higher levels of depression, anxiety, and stress and lower levels of subjective wellbeing among school students (43). In this context, this study found that students' MPA was negatively associated with depressive symptoms, this result could be supported by previous studies conducted by Herbert which validated the effectiveness of exercise in preventing and reducing depressive symptoms at university students populations, that exercise interventions comprising aerobic exercises of low- to moderate intensity may work best to improve mental health among university students after a few weeks of intervention (44). and the role of moderate-to-vigorous physical activity (MVPA) in alleviating depressive symptoms has also been widely recognized (45–47).
A study showed that during the pandemic, people who regularly engaged in MVPA were 12–32% less likely to experience symptoms of depression. A single 20–60 min session of physical activities 1–5 times per week had the significant positive effect on depression (48) while high-frequency exercise (3–5 times per week) interventions were more effective in alleviating depression symptoms than low frequency (1 time per week) (49). Compared with previous findings, this study realized no significant difference between the effects of low- and high-intensity physical activity on depressive symptoms, and moderate-intensity physical activities were effective in alleviating depression. Some scholars have used restricted cubic spline model analysis to identify an approximate “U” shaped dose-effect relationship between weekly MVPA time, total physical activities and the risk of developing depressive symptoms. With the increase of weekly MVPA time and total physical actibity, the risk of developing depressive symptoms showed a tendency to decrease then increase (50). It could be seen that exercise intensity and total physical activities should be maintained at an appropriate intensity and level for alleviating and preventing the occurrence of depressive symptoms (51); another important reason may be that it was difficult to perform strenuous physical activities during the closure control period due to the policy of preventing from leaving home and the lack of corresponding exercise equipment for college students in physical education (17), and moderate-intensity exercises, such as jumping gymnastics, self-weight strength training and other moderate-intensity physical activities are commonly chosen by students and have produced good alleviating effects on depression.
In this study, MPA was also negatively associated with anxiety symptoms, a result was consistent with a large body of research and showed that physical activities had a positive effect on improving mood and wellbeing, reducing anxiety and promoting mental health (52). From the neurobiological mechanism hypothesis, PA enhanced mental health and alleviated anxiety symptoms by changing the structural and functional organization of the brain (53) while the behavioral mechanism hypothesis suggested that physical activities improved self-regulation and coping skills, thus helping people to stay mentally active effectively (54). Physical activities of appropriate intensity and frequency could release psychological tension and increase mental stability (55). In 2020, the World Health Organization gave more specific recommendations that for adults aged 18–64 years, at least 150 min of moderate-intensity aerobic exercise or at least 75 min of high-intensity aerobic exercise per week may reduce the risk of anxiety (56). Promoting mental health by maintaining and improving PA levels have already became a critical and highly effective measure with effects comparable to those of medication and psychotherapy, and it is widely recognized (56–58).
Prolonged lockdown and removal from the constraints of the normal group environment may be accompanied by changes in various behavioral habits of college students, including the frequency of smartphone use. Smartphone addiction is a new type of behavioral addiction in which individuals use smartphones excessively and have no control over the behavior, resulting in impaired social functioning and bringing about psychological and behavioral problems (59). In this study, the average score of smartphone addiction for the sample as a whole was 34 (over 33 for female students and over 31 for male students as having symptoms of smartphone addiction), implying that most students are in a state of smartphone addiction during the epidemic control period, just like students who came from general universities, and that smartphone addiction might affect physical activities during the day (60, 61). This study found that students engaging in moderate-intensity PA were negatively associated with smartphone addiction, and sedentary behavior were positively linked with smartphone addiction. A study last year has the similar results, in which smartphone addicted college students resulted in the increased sedentary time and decreased physical activity time compared to the pre-COVID-19 outbreak. It meant that long sedentary time and low moderate physical activity time were positively associated with smartphone addiction among college students (10). Also, a 2020 US study also showed that during the early restriction period of COVID-19, a reduction in PA and increased time spent using smartphone screens led to poorer mental health outcomes (62), the longer the sedentary time was, the poorer mental health and wellbeing would be (9). This study validated previous studies in some respects that performing moderate-intensity PA can reduce the level of smartphone addiction, and that sedentary behavior is a risk factor for smartphone addiction. Therefore, it can be suggested that reducing sedentary behaviors and maintaining moderate to high PA levels during self-quarantine of the COVID-19 pandemic should be an important measure to avoid smartphone addiction and promote physical and mental health among college students.
Furthermore, this study found a negative correlation between MPA and fear on the COVID-19, which is also consistent with previous studies that found a negative correlation between fear scores and physical activity levels on the COVID-19 (higher fear was associated with lower physical activity levels), with each increase in scale score decreasing the odds of engaging in strenuous physical activity 3% (63). Engaging in moderate-intensity physical activities contributes to and alleviates fear of COVID-19 and can be explained by theories of stress and maladaptive coping as well as health behavior theories because COVID-19 global spread exceeds an individual's psychosocial resources (e.g., social support; self-regulatory skills) and exacerbates an individual's fear of COVID-19 and thus may be reduced by using maladaptive coping strategies to respond, thereby reducing time spent participating in physical activities.
In interpreting the results of the above study, some limitations of this study were noted. First of all, this study made use of a cross-sectional study design, which only allowed for correlational analysis and did not allow for causal inference, and it was more difficult to collect questionnaires and had a smaller sample size during the school closure period of the pandemic. Future studies should be able to consider larger sample sizes and use longitudinal designs and randomized controlled trials to help establish causal relationships between physical activities, depression, anxiety symptoms, smartphone addiction, and fear of COVID-19. Another limitation of this study was the self-reported nature of the data, which was heavily influenced by potential recall bias and current subjective mood. For example, people who have experienced poor mental health problems may be more inclined to participate in research because they find the topic more relevant. This may lead to an overestimation of depressive and anxiety symptoms. Future studies should use more objective measures. Furthermore, the mechanisms associated with why only moderate-intensity PA can be a significant influence on depression, anxiety symptoms, smartphone addiction, and fear of COVID-19 factors in this study remained an open question for future research.
Despite these limitations, our findings still have clinical and policy implications. First of all, university psychology counselors could further evaluate the psychological problems of the students based on the result of the investigation, in order to implement effective intervention, which will help students to alleviate mental health problems in the lockdown. In addition, moderate intensity exercise seems to be a better choice in the relatively small space. The students could choose to do some self-weight strength training, jumping gymnastics, rope skipping and other moderate-intensity physical activities (64). It is recommended to have exercises for 20 min a day, adjust life schedule and reduce sedentary behaviors, so as to alleviate mental health problems caused by the epidemic lockdown.
There was a significant association between moderate-intensity physical activities and depression, anxiety, fear of COVID-19, and smartphone addiction, and a significant association between sedentary behavior and smartphone addiction among sports college students during the lockdown. The findings again demonstrated that physical activities and reduction of sedentary behavior could contribute to the mental health of college students, but further longitudinal studies should be needed to elucidate the causal relationship between moderate-intensity physical activities and mental health among sports college students. This study suggested that during the pandemic, current college students in closure management should be encouraged to overcome difficulties such as space limitations, actively engage in moderate-intensity physical activity, and reduce sedentary behaviors, which are beneficial for alleviating mental health problems, such as depression, anxiety symptoms, fear of COVID-19, and smartphone addiction.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Review Committee of Shanghai University of Sport. The patients/participants provided their written informed consent to participate in this study.
YW: conceptualization, methodology, investigation, data curation, and writing—original draft. YL: validation, supervision, formal analysis, writing—reviewing and editing, and funding acquisition. Both authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Zhang X, Zhang W, Chen S. Shanghai's life-saving efforts against the current omicron wave of the COVID-19 pandemic. Lancet. (2022) 399:2011–2. doi: 10.1016/S0140-6736(22)00838-8
2. Brailovskaia J, Margraf J. Predicting adaptive and maladaptive responses to the coronavirus (COVID-19) outbreak: a prospective longitudinal study. Int J Clin Health Psychol. (2020) 20:183–91. doi: 10.1016/j.ijchp.2020.06.002
3. Santomauro DF, Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
4. Dozois DJ Mental Health Research Canada. Anxiety and depression in canada during the COVID-19 pandemic: a national survey. Can Psychol. (2021) 62:136–42. doi: 10.1037/cap0000251
5. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
6. Katewongsa P, Widyastari DA, Saonuam P, Haemathulin N, Wongsingha N. The effects of the COVID-19 pandemic on the physical activity of the Thai population: evidence from Thailand's Surveillance on Physical Activity 2020. J Sport Health Sci. (2021) 10:341–8. doi: 10.1016/j.jshs.2020.10.001
7. Paterson DC, Ramage K, Moore SA, Riazi N, Tremblay MS, Faulkner G, et al. Exploring the impact of COVID-19 on the movement behaviors of children and youth: a scoping review of evidence after the first year. J Sport Health Sci. (2021) 10:675–89. doi: 10.1016/j.jshs.2021.07.001
8. Tulchin-Francis K, Stevens W Jr, Gu X, Zhang T, Roberts H, Keller J, et al. The impact of the coronavirus disease 2019 pandemic on physical activity in U.S. children. J Sport Health Sci. (2021) 10:323–32. doi: 10.1016/j.jshs.2021.02.005
9. Faulkner J, O'Brien WJ, McGrane B, Wadsworth D, Batten J, Askew CD, et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: a multi-country cross-sectional analysis. J Sci Med Sport. (2021) 24:320–6. doi: 10.1016/j.jsams.2020.11.016
10. Huang Z, Tan J, Xu H, Huang B, Chen Q, Li Z, et al. Association of smartphone addiction with daily behaviors and mental health during the COVID-19 pandemic among medical college students. Chin J School Health. (2021) 42:713–8. doi: 10.16835/j.cnki.1000-9817.2021.05.018
11. Sun Y, Liu W, Xiong L, Qu Y, Chen S, Wu D, et al. Relationship between moderate to vigorous physical activity, screen time and depressive symptoms among middle school students in Guangzhou. Chin J School Health. (2021) 1499–503. doi: 10.16835/j.cnki.1000-9817.2021.10.013
12. Chi X, Becker B, Yu Q, Willeit P, Jiao C, Huang L, et al. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front Psychiatry. (2020) 11:803. doi: 10.3389/fpsyt.2020.00803
13. Sun S, Goldberg SB, Lin D, Qiao S, Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Global Health. (2021) 17:15. doi: 10.1186/s12992-021-00663-x
14. Rodríguez-Larrad A, Mañas A, Labayen I, González-Gross M, Espin A, Aznar S, et al. Impact of COVID-19 confinement on physical activity and sedentary behaviour in Spanish University students: role of gender. Int J Environ Res Public Health. (2021) 18:369. doi: 10.3390/ijerph18020369
15. Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. (2013). doi: 10.1016/j.amepre.2013.08.001
16. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am J Psychiatry. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
17. Maugeri G, Castrogiovanni P, Battaglia G, Pippi R, D'Agata V, Palma A, et al. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. (2020) 6:e04315. doi: 10.1016/j.heliyon.2020.e04315
18. Haider S, Smith L, Markovic L, Schuch FB, Sadarangani KP, Lopez Sanchez GF, et al. Associations between physical activity, sitting time, and time spent outdoors with mental health during the first COVID-19 lock down in Austria. Int J Environ Res Public Health. (2021) 18:9168. doi: 10.3390/ijerph18179168
19. Wolf S, Seiffer B, Zeibig JM, Welkerling J, Brokmeier L, Atrott B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. (2021) 51:1771–83. doi: 10.1007/s40279-021-01468-z
20. Duclos-Bastías D, Vallejo-Reyes F, Giakoni-Ramírez F, Parra-Camacho D. Impact of COVID-19 on sustainable university sports: analysis of physical activity and positive and negative affects in athletes. Sustainability. (2021) 13:6095. doi: 10.3390/su13116095
21. Shen S, Suzuki K, Kohmura Y, Fuku N, Someya Y, Miyamoto-Mikami E, et al. Associations of voluntary exercise and screen time during the first wave of COVID-19 restrictions in japan with subsequent grip strength among University Students: J-Fit(+) Study. Sustainability. (2021) 13:13648. doi: 10.3390/su132413648
22. Roldan A, Raul R. Are self-efficacy gains of university students in adapted physical activity influenced by online teaching derived from the COVID-19 pandemic? Front Psychol. (2021) 12:654157. doi: 10.3389/fpsyg.2021.654157
23. Mosquera-González MJ, Ríos-de-Deus MP, Rego-Agraso L, Rodicio-García ML, Penado Abilleira M. Physical activity of sport sciences students during COVID-19 home confinement. Sport Soc. (2022) 25:1359–72. doi: 10.1080/17430437.2021.2016705
24. Liu L. Enlightenment of social adaptability of sports major college students on physical education in colleges. J Beijing Sport Univ. (2017) 40:78–83+95. doi: 10.19582/j.cnki.11-3785/g8.2017.01.013
25. Wyatt T, Oswalt SB. Comparing mental health issues among undergraduate and graduate students. Am J Health Educ. (2013) 44:96–107. doi: 10.1080/19325037.2013.764248
26. Dial LA, DeNardo FA, Fevrier B, Morgan AL, Du C, Tucker RM, et al. Comparing mental health and well-being of US undergraduate and graduate students during the early stages of the COVID-19 pandemic. J Am Coll Health. (2021) 0:1–11. doi: 10.1080/07448481.2021.1996372
27. Macfarlane DJ, Lee CC, Ho EY, Chan KL, Chan DT. Reliability and Validity of the Chinese Version of IPAQ (Short, Last 7 Days). J Sci Med Sport. (2007) 10:45–51. doi: 10.1016/j.jsams.2006.05.003
28. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire:12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
29. He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
30. Dhira TA, Rahman MA, Sarker AR, Mehareen J. Validity and reliability of the generalized anxiety disorder-7 (GAD-7) among University Students of Bangladesh. PLoS ONE. (2021) 16:e0261590. doi: 10.1371/journal.pone.0261590
31. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
32. Leung DY, Mak YW, Leung SF, Chiang VC, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in chinese adolescents. Asia Pac Psychiatry. (2020) 12:e12381. doi: 10.1111/appy.12381
33. Rahman MA, Dhira TA, Sarker AR, Mehareen J. Validity and reliability of the patient health questionnaire scale (PHQ-9) among university students of Bangladesh. PLoS ONE. (2022) 17:e0269634. doi: 10.1371/journal.pone.0269634
34. Chi X, Chen S, Chen Y, Chen D, Yu Q, Guo T, et al. Psychometric evaluation of the fear of COVID-19 scale among Chinese population. Int J Ment Health Addict. (2022) 20:1273–88. doi: 10.1007/s11469-020-00441-7
35. Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Mental Health Addict. (2020) 20:1537–45. doi: 10.1007/s11469-020-00270-8
36. Alimoradi Z, Lin CY, Ullah I, Griffiths MD, Pakpour AH. Item response theory analysis of the fear of COVID-19 scale (FCV-19S): A systematic review. Psychol Res Behav Manag. (2022) 15:581–96. doi: 10.2147/PRBM.S350660
37. Chen W, Liang Y, Yin X, Zhou X, Gao R. The factor structure and rasch analysis of the fear of COVID-19 scale (FCV-19S) among Chinese students. Front Psychol. (2021) 12:678979. doi: 10.3389/fpsyg.2021.678979
38. Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Armesilla MD, Latorre JM. The fear of COVID-19 scale: validation in Spanish university students. Psychiatry Res. (2020) 293:113350. doi: 10.1016/j.psychres.2020.113350
39. Chen B, Liu F, Ding S, Ying X, Wang L, Wen Y, et al. Gender differences in factors associated with smartphone addiction: a cross-sectional study among medical college students. BMC Psychiatry. (2017) 17:341. doi: 10.1186/s12888-017-1503-z
40. Luk TT, Wang MP, Shen C, Wan A, Chau PH, Oliffe J, et al. Short version of the smartphone addiction scale in Chinese adults: psychometric properties, sociodemographic, and health behavioral correlates. J Behav Addict. (2018) 7:1157–65. doi: 10.1556/2006.7.2018.105
41. Cheung T, Lee RL, Tse AC, Do CW, So BC, Szeto GP, et al. Psychometric properties and demographic correlates of the smartphone addiction scale-short version among Chinese children and adolescents in Hong Kong. Cyberpsychol Behav Soc Netw. (2019) 22:714–23. doi: 10.1089/cyber.2019.0325
42. Andrade AL, Scatena A, Martins GD, de Oliveira Pinheiro B, da Silva AB, Enes CC, et al. Validation of smartphone addiction scale – short version (SAS-SV) in Brazilian Adolescents. Addict Behav. (2020) 110:106540. doi: 10.1016/j.addbeh.2020.106540
43. Quarta S, Levante A, García-Conesa MT, Lecciso F, Scoditti E, Carluccio MA, et al. Assessment of Subjective Well-Being in a Cohort of University Students and Staff Members: Association with Physical Activity and Outdoor Leisure Time during the COVID-19 Pandemic. Int J Environ Res Public Health. (2022) 19:4787. doi: 10.3390/ijerph19084787
44. Herbert C. Enhancing mental health, well-being and active lifestyles of university students by means of physical activity and exercise research programs. Front Public Health. (2022) 10:849093. doi: 10.3389/fpubh.2022.849093
45. Joshi S, Mooney SJ, Kennedy GJ, Benjamin EO, Ompad D, Rundle AG, et al. Beyond METs: types of physical activity and depression among older adults. Age Ageing. (2016) 45:103–9. doi: 10.1093/ageing/afv164
46. Chang YC, Lu MC, Hu IH, Wu WC, Hu SC. Effects of different amounts of exercise on preventing depressive symptoms in community-dwelling older adults: a prospective cohort study in Taiwan. BMJ Open. (2017) 7:e014256. doi: 10.1136/bmjopen-2016-014256
47. Chi X, Liang K, Chen ST, Huang Q, Huang L, Yu Q, et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. (2021) 21:100218. doi: 10.1016/j.ijchp.2020.100218
48. Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. (2008) 62:25–9. doi: 10.1080/08039480802315640
49. Legrand F, Heuze JP. Antidepressant effects associated with different exercise conditions in participants with depression: a pilot study. J Sport Exerc Psychol. (2007) 29:348–64. doi: 10.1123/jsep.29.3.348
50. Kuwahara K, Honda T, Nakagawa T, Yamamoto S, Akter S, Hayashi T, et al. Associations of leisure-time, occupational, and commuting physical activity with risk of depressive symptoms among Japanese workers: A cohort study. Int J Behav Nutr Phys Activity. (2015) 12:119. doi: 10.1186/s12966-015-0283-4
51. Lin J, Guo T, Becker B, Yu Q, Chen ST, Brendon S, et al. Depression is associated with moderate-intensity physical activity among college students during the COVID-19 pandemic: differs by activity level, gender and gender role. Psychol Res Behav Manag. (2020) 13:1123–34. doi: 10.2147/PRBM.S277435
52. Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C, et al. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. (2015) 9:366–78. doi: 10.1080/17437199.2015.1022901
53. Lin TW, Kuo YM. Exercise benefits brain function: the monoamine connection. Brain Sci. (2013) 3:39–53. doi: 10.3390/brainsci3010039
54. Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. (2016) 138:e20161642. doi: 10.1542/peds.2016-1642
55. Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. (2020) 26:e924085. doi: 10.12659/MSMBR.924085
56. Okely AD, Kontsevaya A, Ng J, Abdeta C. 2020 WHO guidelines on physical activity and sedentary behavior . Sports Med Health Sci. (2021) 3:115–8. doi: 10.1016/j.smhs.2021.05.001
57. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: A meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36:846–58. doi: 10.1002/da.22915
58. Teychenne M, White RL, Richards J, Schuch FB, Rosenbaum S, Bennie JA, et al. Do we need physical activity guidelines for mental health: what does the evidence tell us? Mental Health Phys Act. (2020) 18:100315. doi: 10.1016/j.mhpa.2019.100315
59. Liu Q, Yang Y, Lin Y, Yu S, Zhou Z. Smartphone addiction: concepts, measurements, and factors. Chin J Clin Psychol. (2017) 25:82–7. doi: 10.16128/j.cnki.1005-3611.2017.01.019
60. Lepp A, Barkley JE, Sanders GJ, Rebold M, Gates P. The relationship between cell phone use. Physical and sedentary activity, and cardiorespiratory fitness in a sample of US college students. Int J Behav Nutr Phys Activity. (2013) 10:79–79. doi: 10.1186/1479-5868-10-79
61. Towne T, Ory SD, Smith MG, Peres ML, Pickens SC, Mehta AW, et al. Accessing physical activity among young adults attending a university: the role of sex, race/ethnicity, technology use, and sleep. BMC Public Health. (2017) 17:721. doi: 10.1186/s12889-017-4757-y
62. Meyer J, Mcdowell C, Lansing J, Brower C, Smith L, Tully M, et al. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3052 US Adults. Int J Environ Res Public Health. (2020) 17:6469. doi: 10.3390/ijerph17186469
63. Cummings C, Humiston T, Cohen LB, Lansing AH. The role of COVID-19 fears and related behaviors in understanding daily adolescent health behaviors during the pandemic. J Health Psychol. (2022) 27:1354–64. doi: 10.1177/13591053211044533
Keywords: COVID-19, confinement, physical activities, mental health, sports university students
Citation: Wang Y and Li Y (2022) Physical activity and mental health in sports university students during the COVID-19 school confinement in Shanghai. Front. Public Health 10:977072. doi: 10.3389/fpubh.2022.977072
Received: 24 June 2022; Accepted: 02 September 2022;
Published: 11 October 2022.
Edited by:
Liye Zou, Shenzhen University, ChinaReviewed by:
Sitong Chen, Victoria University, AustraliaCopyright © 2022 Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youqiang Li, eW91bWVjaXR5QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.