- 1Department of Radiology, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
- 2Medical Imaging Center, Affiliated Drum Tower Hospital, Medical School of Nanjing University, Nanjing, China
- 3Institute of Medical Imaging and Artificial Intelligence, Nanjing University, Nanjing, China
- 4Department of Pulmonary and Critical Care Medicine, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
- 5Department of Infectious Disease, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
- 6Department of Infectious Diseases, The Second Hospital of Nanjing, The Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, China
- 7Institute of Brain Science, Nanjing University, Nanjing, China
Background: The coronavirus disease (COVID-19) pandemic, which has been ongoing for more than 2 years, has become one of the largest public health issues. Vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is one of the most important interventions to mitigate the COVID-19 pandemic. Our objective is to investigate the relationship between vaccination status and time to seroconversion.
Methods: We conducted a cross-sectional observational study during the SARS-CoV-2 B.1.617.2 outbreak in Jiangsu, China. Participants who infected with the B.1.617.2 variant were enrolled. Cognitive performance, quality of life, emotional state, chest computed tomography (CT) score and seroconversion time were evaluated for each participant. Statistical analyses were performed using one-way ANOVA, univariate and multivariate regression analyses, Pearson correlation, and mediation analysis.
Results: A total of 91 patients were included in the analysis, of whom 37.3, 25.3, and 37.3% were unvaccinated, partially vaccinated, and fully vaccinated, respectively. Quality of life was impaired in 30.7% of patients, especially for mental component summary (MCS) score. Vaccination status, subjective cognitive decline, and depression were risk factors for quality-of-life impairment. The chest CT score mediated the relationship of vaccination status with the MCS score, and the MCS score mediated the relationship of the chest CT score with time to seroconversion.
Conclusion: Full immunization course with an inactivated vaccine effectively lowered the chest CT score and improved quality of life in hospitalized patients. Vaccination status could influence time to seroconversion by affecting CT score and MCS score indirectly. Our study emphasizes the importance of continuous efforts in encouraging a full vaccination course.
Introduction
The coronavirus disease (COVID-19) pandemic, which has been ongoing for more than 2 years, has become one of the largest public health issues and has affected the lives of most people worldwide (1). Quality of life domains and wellbeing outcomes have been worsened due to the pandemic in several parts of the world. Vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is one of the most important interventions to mitigate the COVID-19 pandemic (2). Available evidence has demonstrated that COVID-19 vaccines are effective in the prevention of severe complications of COVID-19 and death (2, 3), moreover, these vaccines are effective against infection with the different variants of COVID-19 (4). Clinical trials have demonstrated that vaccine efficacy can significantly affect disease outcomes, as vaccination can prevent symptomatic COVID-19 in 65.9–83% of people and severe illness or intensive care unit (ICU) admission in 90% to 100% of infected patients (5–7). A previous study reported that the 28-day seroconversion rate in subjects exceeded 80% (8). Additionally, the incidence of COVID-19 in the unvaccinated population was more than double (20.07%) that in the fully vaccinated population (9).
In China, people are generally vaccinated with inactivated vaccines (2). Accumulated evidence suggests that inactivated vaccines can efficiently, although not fully, protect against SARS-CoV-2 infection and, more importantly, prevent severe illness progression (10). Previous studies have confirmed the protective effect of the inactivated vaccine against the pathogenesis of SARS-CoV-2 mutant strains (2, 9), such as the Delta Variant (B.1.617.2).
COVID-19 infection directly affects not only overall survival but also central nervous system function, leading to acute neuropsychiatric symptoms (11). COVID-19 also indirectly affects the neuropsychiatric state (12). The contraction of the COVID-19 virus, spectrum of infection, environment and social situations, and social isolation also significantly affect the mental state of patients. COVID-19 patients have reported an increased sense of anxiety and reduced quality of life 6 months after hospital admission (13).
Whether vaccination status with an inactivated vaccine affects the seroconversion time in patients during hospital admission remains unclear. Thus, we performed a real-world study that analyzed patients' clinical, neuropsychiatric assessment, laboratory examination and chest CT image data in a designated hospital in Nanjing. Our study aimed to describe how the relationship between vaccination status and seroconversion time is affected by mental health and chest CT imaging findings during hospitalization and its effect on the pathogenesis of SARS-CoV-2 mutant strains.
Methods
Patients
This study was conducted between July 21, 2021, and September 15, 2021. Ninety-one COVID-19 patients with SARS-CoV-2 B.1.617.2 infection were enrolled at the Second Hospital of Nanjing, which is a specialized hospital for infectious diseases that was responsible for the admission of infected patients throughout Jiangsu Province during the SARS-CoV-2 B.1.617.2 variant pandemic. The inclusion criteria were as follows: (a) confirmed COVID-19 diagnosis via nasopharyngeal or oropharyngeal swab; (b) confirmation of the presence of the B.1.617.2 (Delta) variants by high-throughput whole-genome sequencing; (c) hospital admission and disease management; and (d) age ≥18 years. Patients were excluded from the study if they met any of the following exclusion criteria: (a) an unconfirmed etiology of pneumonia; (b) no available computed tomography (CT) scans; (c) an unconfirmed vaccination status (d) refusal to provide consent or (e) unable to complete questionnaires. The vaccination detail of 21 subjects was unknown. Fifteen subjects were excluded due to illiterate or unable to complete questionnaires. Finally, a total of 91 patients were enrolled in this study. The severity of disease was classified into three grades: mild, moderate, and severe, according to the Chinese management guideline for COVID-19 (14). None of the patients in the acute phase exhibited progression to severe disease, and all cases were mild or moderate. All patients received adequate medical support during hospitalization. This study was approved by the ethics committee of the Second Hospital of Nanjing, Nanjing, China (Nr: 2021-LS-ky031). Written informed consent was obtained from all participants.
Clinical evaluation
The baseline day was defined as the day of the initial positive for new coronavirus nucleic acid by using the SARS-CoV-2 specific RT-PCR test. Nasal swabs were sampled at an interval of 24 h for examination of viral titer during hospitalization. The diagnostic criteria for viral seroconversion were two consecutive nasal swab samples negative by the SARS-CoV-2 RT-PCR test. Time to seroconversion was defined as the time from baseline day to viral seroconversion. All patients completed a structured electronic questionnaire independently within three days of hospital admission. The contents of the questionnaire included basic information (age, sex, education level, date of birth, height, weight, smoking status), medical history, and neuropsychological tests (cognition, quality of life, anxiety, depression and posttraumatic stress). The investigator was blinded to medical history during the data acquisition to avoid selection bias. Clinical symptoms, treatments, initial laboratory indicators, and chest CT imaging were extracted from the electronic medical system. Initial laboratory and imaging results were defined as the first-time examination within 24 h after admission.
Definition of vaccination status
We categorized the patients into 3 groups, unvaccinated, partially vaccinated, and fully vaccinated, according to their immunization history (15). Patients were considered unvaccinated if they had never been vaccinated or had received 1 dose of the vaccine with a time interval between the first dose and illness onset of <14 days. Patients who had received 1 vaccine dose with an interval of more than 14 days or received 2 vaccine doses with an interval between the second dose and illness onset of <14 days were considered partially vaccinated. Patients were considered fully vaccinated if they received 2 doses of the vaccine and the time interval between the last vaccine dose and illness onset was more than 14 days.
Cognition, quality of life, and emotional state evaluations
Cognitive impairment was evaluated both objectively and subjectively. Objective cognitive impairment was assessed by the Mini Mental Status Examination (MMSE), a widely used psychological test of global cognitive function among elderly individuals; it includes tests for orientation, attention, memory, language and visual-spatial skills (16). The maximum MMSE score is 30 points, and a score below 25 suggests cognitive impairment. Subjective cognitive decline (SCD) was assessed by a newly developed questionnaire consisting of nine items (17), that examine global memory functioning and the ability to perform daily activities. Higher scores indicate a higher risk of SCD.
Health-related quality of life was evaluated with the 36-item Short Form (SF-36), a well-validated 36-item questionnaire (18). The questionnaire includes one multi-item scale that assesses eight health concepts: physical function, role physical, bodily pain, general health, validity, social function, role-emotional and mental health. The total scores of the physical component summary (PCS) and mental component summary (MCS) range from 0 to 100 points each, with higher levels indicating a better health condition. Total scores below 117 are considered to indicate impairment according to norm-based scoring in elderly Chinese individuals.
Posttraumatic stress was assessed by the Posttraumatic Stress Disorder Checklist-5 (PCL-5) (19). The PCL-5 is a self-report instrument for the assessment of distress associated with the 20 symptoms of posttraumatic stress disorder (PTSD), with scores > 32 indicating clinically relevant PTSD. Depression and anxiety were evaluated with the Hospital Anxiety and Depression Scale (HADS) (20). This score consists of anxiety (HADS-A) and depression (HADS-D) subscales, each of which contains seven items scored from 0 to 3 points. The scores of each subscale range from 0 to 21, with higher scores indicating a larger number of intensive anxiety- and depression-related symptoms. Scores >7 indicate mild disorder, and scores >10 indicate clinically meaningful anxiety disorder or depression.
CT protocol
Chest CT scans were performed using a 64-MDCT scanner (Brilliance 64, Philips Healthcare, Cleveland, Ohio, USA) or a 16-MDCT scanner (Aquilion TSX-101A, Toshiba, Tokyo, Japan). All chest CT scans were obtained with the patient in the supine position and scanning was performed at end-inspiration. The following parameters were used: tube voltage of 120 kVp, automatic tube current modulation (ATCM), reconstruction matrix of 512 × 512 pixels, section thickness of 1.5 mm, and interval of 1.5 mm.
Evaluation of the CT score
The CT score, a widely used evaluation method by radiologists to quantify the extent of lung abnormalities, was determined for every CT scan (21, 22). Each lung lobe was scored from 0 to 5 based on the percentage of infection: score of 0, no involvement; score of 1, <5% involvement; score of 2, 6–25% involvement; score of 3, 26–49% involvement; score of 4, 50–75% involvement; and score of 5, >75% involvement. The CT score was derived from the sum of the individual lobar scores, resulting in CT scores ranging from 0 to 25 for each CT scan.
Statistical analysis
Statistical analyses were performed with IBM SPSS Statistics Software (version 26; IBM, New York, USA). Categorical variables are expressed as frequencies, and continuous variables are described as means ± standard deviations (SDs). The chi-square or Fisher's exact test was used to compare categorical variables. We used analyses of covariance (ANCOVA) to compare the group differences in laboratory findings, chest CT scores, and multiple psychological assessments. Risk factors related to impaired quality of life were analyzed by univariate regression. Variables that were significantly associated with the dependent variable in the univariate analyses (P < 0.05) were included in a multivariable regression model. Odds ratios (ORs) were reported with 95% confidence intervals (CIs). The SF-36 total score, PCS score, and MCS score were correlated with the CT score and time to seroconversion using partial correlation analyses. Partial correlation is a method used to describe the relationship between two variables whilst taking away the effects of another variable, or several other variables, on this relationship. To ensure our results are not affected by demographic features, age, sex and education levels were controlled as covariates in partial correlation analyses (23). After establishing that vaccination status has effects on the chest CT score, SF-36 scale scores and time to seroconversion (Figure 1), we applied mediation model analyses to test the hypothesis that the relationship between vaccination status and time to seroconversion are mediated by chest CT score or SF-36 scale scores. Mediation analyses are employed to understand a known relationship by exploring the underlying mechanism or process by which one variable influences another variable through a mediator variable (24). Mediation analysis was performed using the PROCESS SPSS macro toolbox. The indirect effect in the mediation model was estimated using 5,000 bias-corrected bootstraps with 95% CIs, and P < 0.05 indicated statistical significance.
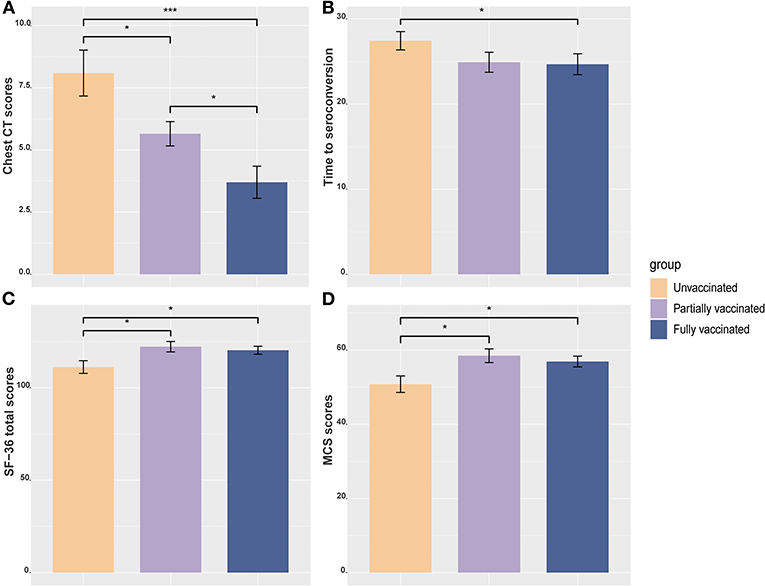
Figure 1. Bar plots among different vaccination status groups with the mean and standard error of the mean are shown. (A) Between-group differences in chest CT scores. (B) Between-group differences in time to seroconversion. (C) Between-group differences in SF-36 total score. (D) Between-group differences in MCS score. *P < 0.05; ***P < 0.001. MCS, mental component summary.
Results
Characteristics of the patients
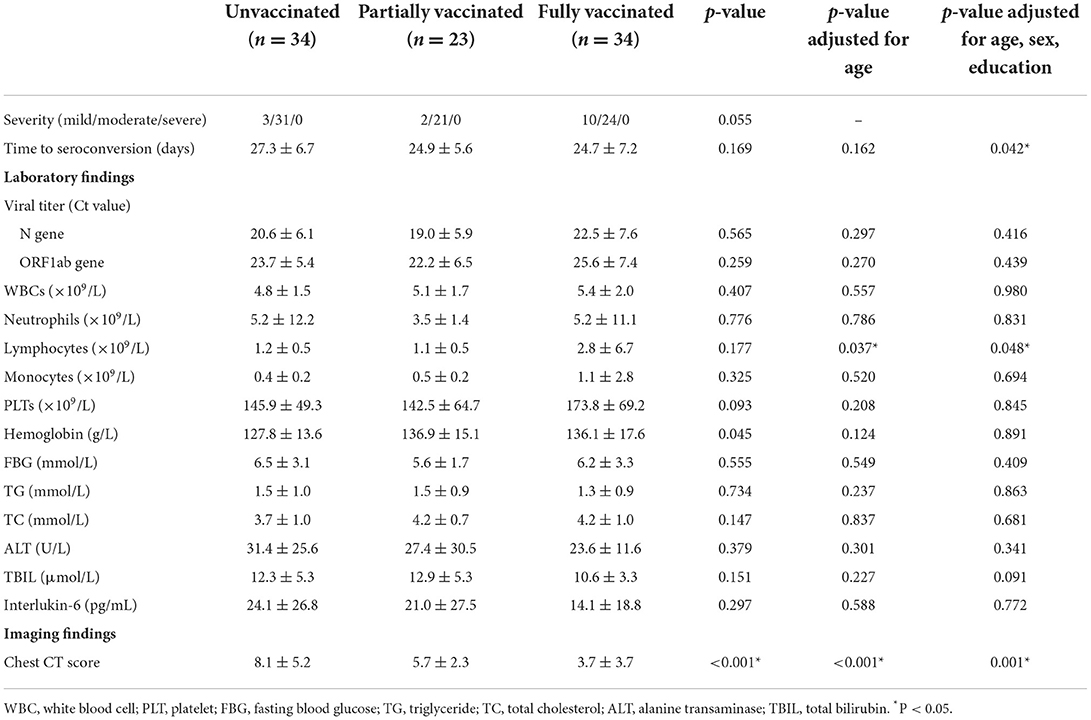
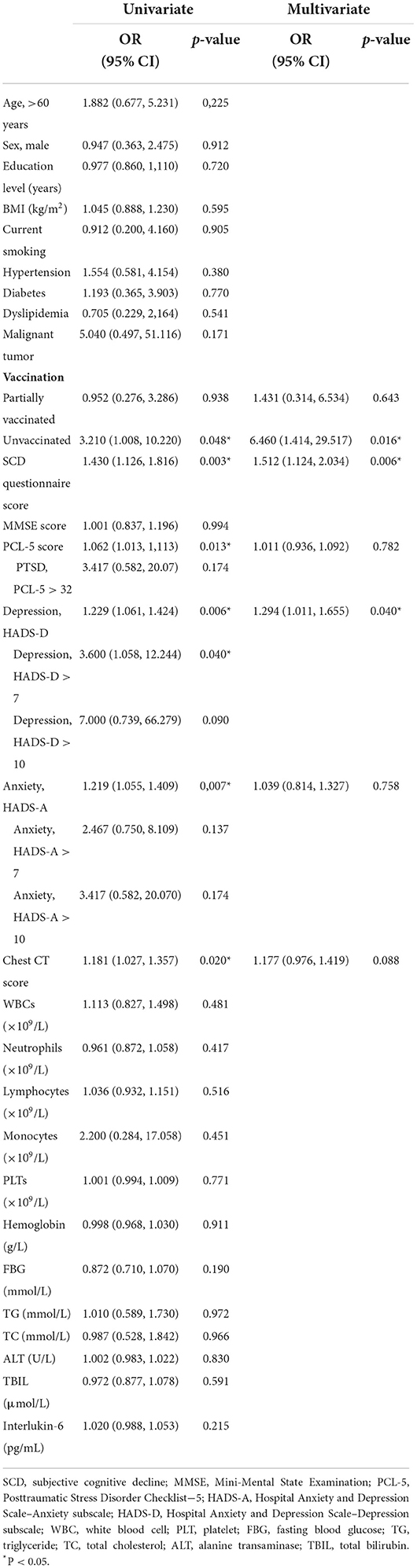
A total of 91 patients were included in the analysis, of whom 34 (37.3%), 23 (25.3%), and 34 (37.3%) were unvaccinated, partially vaccinated, and fully vaccinated, respectively. The inactivated vaccines used were the CoronaVac (Sinovac Biotech, Beijing, China), BBIBP-CorV (Sinopharm, Beijing, China), and KCONVAC (BioKangtai, Shenzhen, China) vaccines, accounting for 57.4, 33.8, and 8.8% of the vaccine doses, respectively. There was no significant difference in sex, education level, smoking status, alcohol consumption, medical history or major symptoms of COVID-19 (Table 1) among the groups. Fully vaccinated patients were younger and had higher diastolic blood pressure (DBP) than unvaccinated patients. Vaccinated patients had a higher lymphocyte level, shorter time to seroconversion, and lower chest CT score during the immediate hospitalization period after adjustment for age, sex and education than the other vaccination status groups (Table 2 and Figures 1A,B). There was no significant difference in the viral load between unvaccinated and fully vaccinated patients, represented by the PCR Ct value of the N gene (P = 0.297) or ORF1ab gene (P = 0.270).
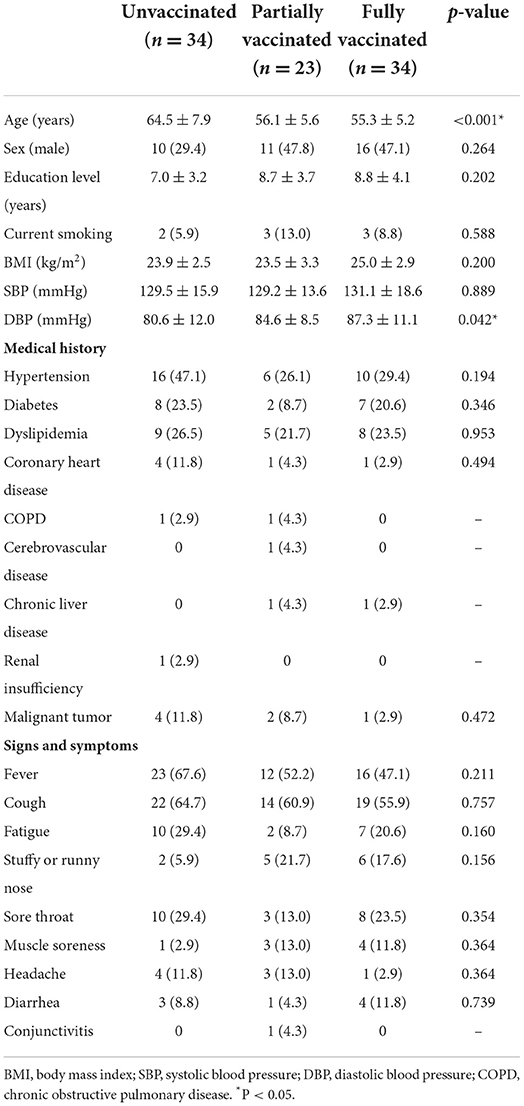
Table 1. Characteristics and clinical features of COVID-19 patients with different vaccination statuses.
Cognition, quality of life, and mental health evaluations
The results of the neuropsychological assessments are shown in Table 3. Cognitive impairment (MMSE < 25) was found in 15.4% of patients (26.5% of unvaccinated patients, 8.7% of partially vaccinated, and 5.6% of fully vaccinated patients). There was no significant difference in the MMSE score among the three groups with adjustment for age, sex, and education (P = 0.076). Quality of life was impaired in 30.7% of patients (38.2% of unvaccinated patients, 26.1% of partially vaccinated, and 26.5% of fully vaccinated). Among the three groups, unvaccinated patients had the lowest SF-36 total score (P = 0.042), especially in the MCS (P = 0.019) (Figures 1C,D). PTSD was diagnosed in 6.6% (6/91) of patients. Depression and anxiety were reported in 5.5% (5/91) and 6.6% (6/91) of patients, respectively. However, there was no significant difference in the incidence of PTSD, depression, or anxiety among the three groups.
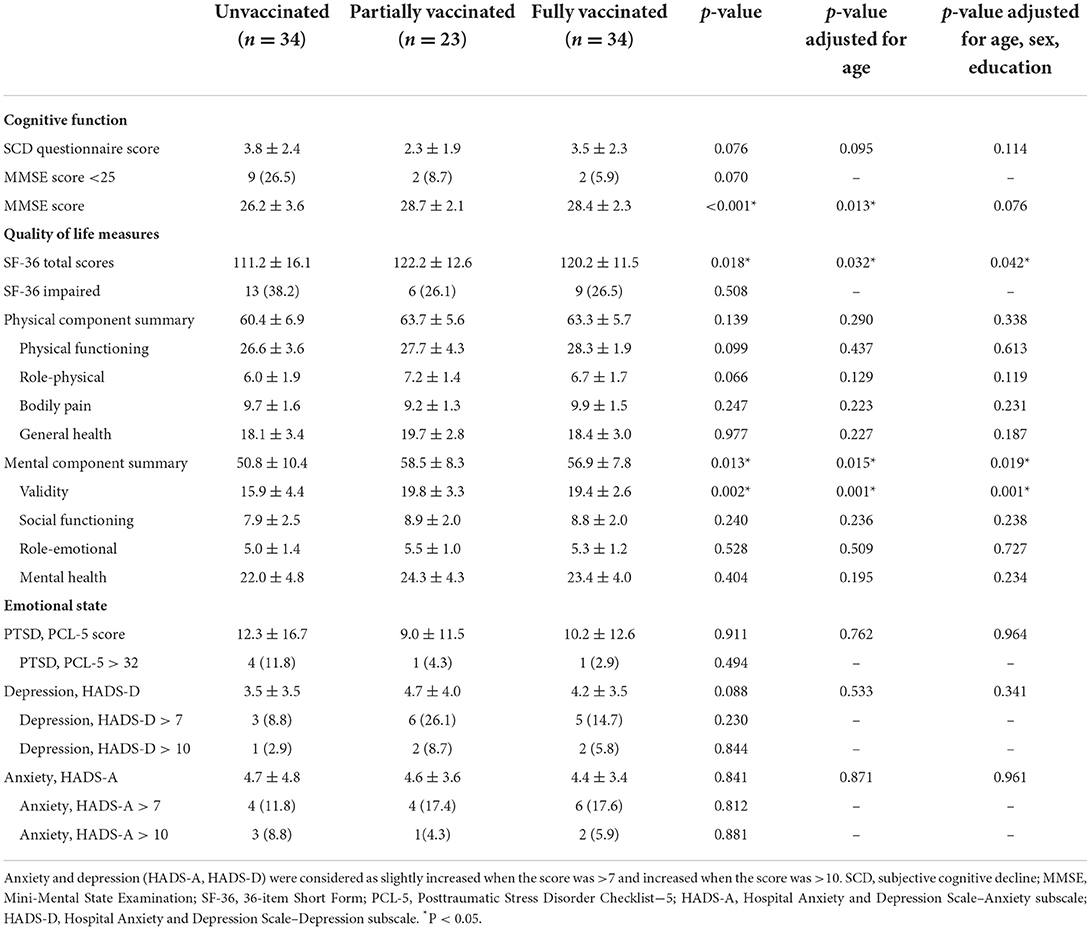
Table 3. Cognition, quality of life and emotional state in COVID-19 patients with different vaccination statuses.
Risk factors related to impaired quality of life
A total of 28 (30.7%) patients had impaired quality of life. Compared with fully vaccinated group, the unvaccinated group had a significantly higher risk of impaired quality of life (OR: 3.210, 95% CI: 1.008–10.220, P = 0.048). In addition, higher scores on the SCD questionnaire (OR: 1.430, 95% CI: 1.126–1.816, P = 0.003), HADS-D (OR: 1.229, 95% CI: 1.061–1.424, P = 0.006), HADS-A (OR: 1.219, 95% CI: 1.055–1.409, P = 0.007), and PCL-5 (OR: 1.062, 95% CI: 1.013–1.113, P = 0.013) were all associated with impaired quality of life. Higher chest CT scores were also related to impaired quality of life (OR: 1.181, 95% CI: 1.027–1.357, P = 0.02) (Table 4). In the multivariable model, the risk of impaired quality of life was more significant in the unvaccinated group than in the vaccinated groups (OR: 6.460, 95% CI: 1.414–29.517, P = 0.016). Higher scores on the SCD questionnaire (OR: 1.512, 95% CI: 1.124–2.034, P = 0.006) and HADS-D (OR: 1.294, 95% CI: 1.011–1.655, P = 0.04) were also associated with impaired quality of life. No significant effect of partial vaccination was found in either the univariable model or multivariable model (Table 4).
Relationships of quality of life with the chest CT score and time to seroconversion
Results of partial correlation analyses are shown in Figure 1. There were significantly negative associations of SF-36 scores with chest CT scores (r = −0.350, P = 0.003) and time to seroconversion (r = −0.419, P < 0.001) (Figures 2A,D). The same correlation was seen either in the PCS or MCS scores (Figures 2B,C,E,F). These results suggest that better quality of life was correlated with less severe lung lesions and shorter time to seroconversion during hospitalization.
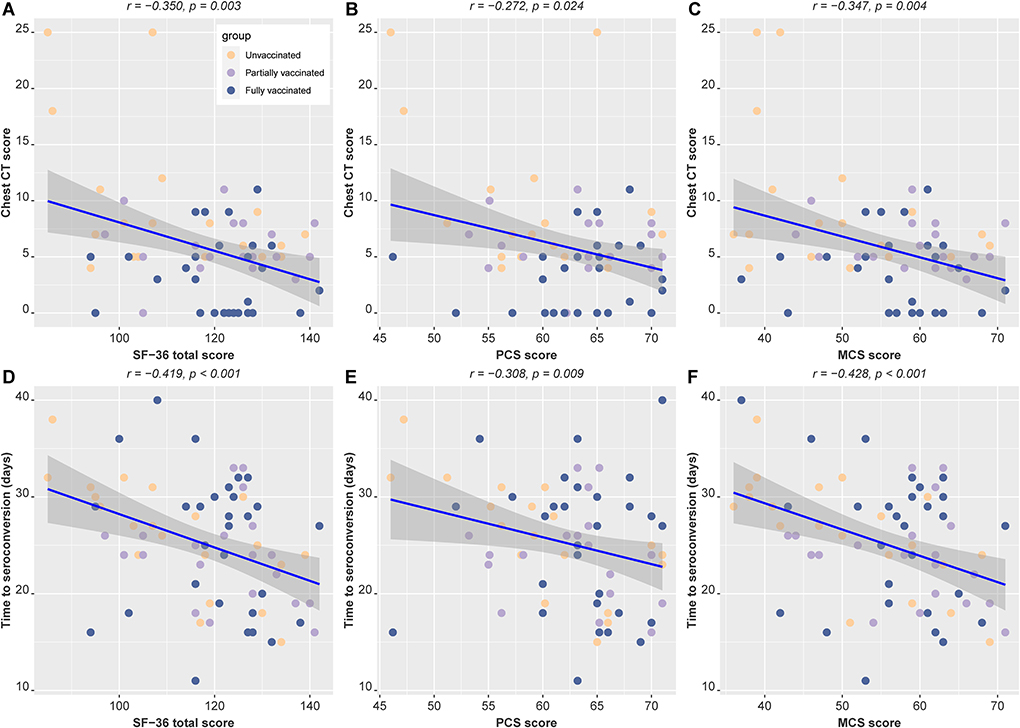
Figure 2. Partial correlation analyses of quality of life with the chest CT score and time to seroconversion, with age, sex and education as covariables. The color of point represents vaccination status. The regression line for all subjects (blue line) and upper and lower 95% CIs (gray shades) are shown. (A–C) Partial correlation analysis between chest CT scores and SF-36 total score, PCS score, and MCS score. (D–F) Partial correlation analysis between seroconversion time and SF-36 total score, PCS score, and MCS score. PCS, physical component summary; MCS, mental component summary.
Mediation analysis
Mediation analyses with correction for age, sex and education were performed to determine the associations of vaccination status with quality of life, chest CT score, and time to seroconversion. Figure 3 showed that chest CT score mediated the correlation between vaccination status and MCS score [indirect effect = 1.5461; 95% bootstrap CI (0.1131, 3.2745)]. Meanwhile, MCS score also mediated the association between chest CT score and time to seroconversion [indirect effect = 1.1825; 95% bootstrap CI (0.0451, 0.3198)] (Figure 3). In our current samples, there is no evidence of direct effect of vaccination status on the time to seroconversion, but vaccination could influence time to seroconversion by affecting CT score and MCS score indirectly.
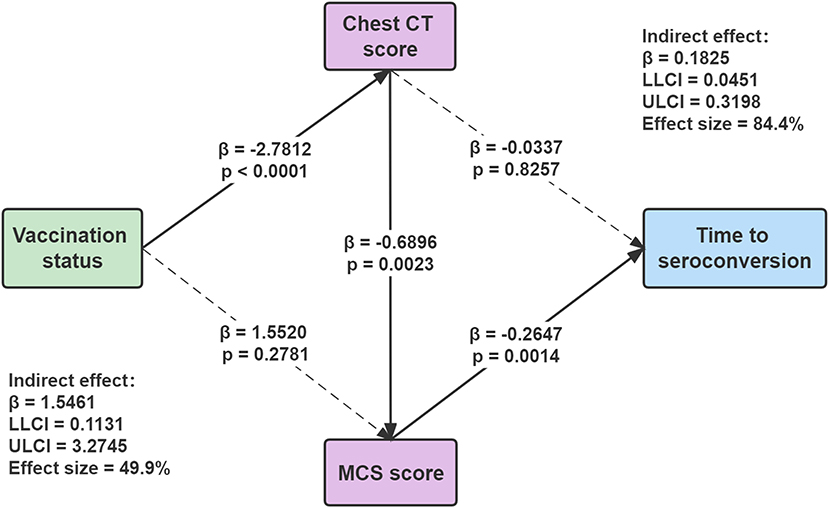
Figure 3. Mediation analyses for the association among vaccination status, chest CT score, MCS score, and time to seroconversion. Standardized β-coefficient was derived from mediation models controlling for age, sex, and education. Values are standardized path coefficients with 95% CIs in parentheses. The effect size of mediation was estimated from the proportion of indirect effect in the total effect. MCS, mental component summary. ULCI, upper limit of the 95% confidence interval; LLCI, lower limit of the 95% confidence interval.
Discussion
The rapid spread and mutation of SARS-CoV-2 have attracted significant public attention, with concerns about increased transmissibility, increased severity of disease, and reduced diagnostic capacity. The mutation frequency and transmission speed of SARS-CoV-2 have rapidly increased. Breakthrough infections due to new variants after vaccination have been increasingly reported, even in mass-vaccination regions (25, 26), especially during the Delta variant epidemic. Therefore, there is a question about whether herd immunity bolstered by vaccination with an inactivated vaccine in China can protect against new variants and help promote rapid recovery with few COVID-19 complications.
Previous work on the long-term impact of COVID-19 on mental health is extensive (27–29) and has shown that functional mobility impairment, pulmonary abnormalities, and mental health disorders are the most common postacute sequelae of COVID-19 infection (30). However, these studies were usually meta-analyses and did not consider vaccination status. Additionally, short-term SARS-CoV-2 vaccine effectiveness in hospitalized patients has been rarely reported. In this study, we focused on vaccination effects in patients who had recently been admitted to the hospital. Our results indicated that fully immunized patients had significantly less severe chest CT findings, as represented by CT scores, than unvaccinated patients. It is possible that the vaccine protected against the progression of the disease from mild to severe (31).
After adjustment of age, sex and education, the three groups have no difference on the MMSE scores. However, the SF-36 scores and MCS scores of the three groups still had significant differences after correcting for age, sex, and education. The unvaccinated group had the lowest SF-36 total score and MCS score compared with the vaccinated group. Among patients recently infected with SARS-CoV-2 and who are under a closed management environment in the hospital, unvaccinated patients may suffer more mental stress, causing quality of life changes. Studies have revealed that vaccination-related stress levels significantly decrease after vaccination (32), and our data support this finding. The univariate and multivariate analyses revealed that vaccination status, cognitive impairment, depression, anxiety, and the chest CT score were significant risk factors for quality of life impairment in hospitalized patients.
The major outcome of this study was the relationship between vaccination status and seroconversion time. The negative associations between quality of life (SF-36 score) with the chest CT score indicated that better quality of life was correlated with less severe lung lesions. COVID-19 causes a wide impairment of diffusion capacity and restrictive ventilatory defects, which exist even at the time of hospital discharge (23, 33). Moreover, the negative correlations between the SF-36 score and time to seroconversion suggest that quality of life at baseline can significantly affect disease prognosis. Mediation analysis (24, 34) allowed us to observe the direct and indirect effects of each variable and explore whether vaccination status was independently associated with the effects of imaging and mental health. The mediation model suggested that vaccination status could influence time to seroconversion by affecting CT score and MCS score indirectly. It can be speculated that a higher quality of life at the outset leads to fewer lung lesions and shorter seroconversion time. Overall, full vaccination showed positive effects on viral clearance and the patient's recovery.
There are some limitations of our study. First, we confirmed that both the chest CT score and MCS score had mediating effects on the relationship between vaccination status and seroconversion time, but the observation windows were narrow because they were restricted to the hospitalization period. Follow-up data may be needed to confirm the persistence of the mediation effects in the long term. Second, only vaccination with inactivated vaccines were considered in this study, and whether this mediating effect exists for other kinds of vaccines still needs to be explored. Third, the sample size was relatively small due to the long period of neuropsychological assessments.
In conclusion, we found a full immunization course with an inactivated vaccine effectively decreases the chest CT score and improves the quality of life in hospitalized patients. Vaccination status could influence time to seroconversion by affecting CT score and MCS score indirectly. Our study highlights the importance of continuous efforts in encouraging a full vaccination course.
Data availability statement
The raw data used and analyzed in the current study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Hospital of Nanjing, Nanjing, China (Nr: 2021-LS-ky031). The patients/participants provided their written informed consent to participate in this study.
Author contributions
WZ contributed to the study design and statistical analyses and wrote the manuscript. QC and JLu contributed to the revision of the manuscript. JD, JLi, and YY contributed to participants' recruitment and data collection. LF, XL, JLiu, JLiuf, and CL contributed to the data collection. BZ is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, supervised the entire study, and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Jiangsu Funding Program for Excellent Postdoctoral Talent, the National Natural Science Foundation of China (81720108022), the Fundamental Research Funds for the Central Universities, Nanjing University (2020-021414380462), the Key Scientific Research Project of Jiangsu Health Committee (K2019025), Industry and Information Technology Department of Nanjing (SE179-2021), Educational Research Project of Nanjing Medical University (2019ZC036), and the Project of Nanjing Health Science and Technology Development (YKK19055). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to thank all the heroic people who actively contributed to ending the COVID-19 outbreak.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mouratidis K. How COVID-19 reshaped quality of life in cities: a synthesis and implications for urban planning. Land Use Policy. (2021) 111:105772. doi: 10.1016/j.landusepol.2021.105772
2. Hu Z, Tao B, Li Z, Song Y, Yi C, Li J, et al. Effectiveness of inactivated COVID-19 vaccines against severe illness in B.1.617.2 (Delta) variant-infected patients in Jiangsu, China. Int J Infect Dis. (2022) 116:204-9. doi: 10.1016/j.ijid.2022.01.030
3. Henry DA, Jones MA, Stehlik P, Glasziou PP. Effectiveness of COVID-19 vaccines: findings from real world studies. Med J Aust. (2021) 215:149. doi: 10.5694/mja2.51182
4. Vasileiou E, Simpson CR, Shi T, Kerr S, Agrawal U, Akbari A, et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet. (2021) 397:1646–57. doi: 10.1016/S0140-6736(21)00677-2
5. Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, et al. Effect of 2 inactivated SARS-CoV-2 vaccines on symptomatic COVID-19 infection in adults: a randomized clinical trial. JAMA. (2021) 326:35–45. doi: 10.1001/jama.2021.8565
6. Jara A, Undurraga EA, González C, Paredes F, Fontecilla T, Jara G, et al. Effectiveness of an inactivated SARS-CoV-2 vaccine in Chile. N Engl J Med. (2021) 385:875–84. doi: 10.1056/NEJMoa2107715
7. Tanriover MD, Doganay HL, Akova M, Güner HR, Azap A, Akhan S, et al. Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey. Lancet. (2021) 398:213–22. doi: 10.1016/S0140-6736(21)01429-X
8. Xing K, Tu X-Y, Liu M, Liang Z-W, Chen J-N, Li J-J, et al. Efficacy and safety of COVID-19 vaccines: a systematic review. Zhongguo Dang Dai Er Ke Za Zhi. (2021) 23:221–8. doi: 10.7499/j.issn.1008-8830.2101133
9. Mahumud RA, Ali MA, Kundu S, Rahman MA, Kamara JK, Renzaho AM. Effectiveness of COVID-19 vaccines against delta variant (B. 1617 2): A meta-analysis. Vaccines. (2022) 10:277. doi: 10.3390/vaccines10020277
10. Benjamanukul S, Traiyan S, Yorsaeng R, Vichaiwattana P, Sudhinaraset N, Wanlapakorn N, et al. Safety and immunogenicity of inactivated COVID-19 vaccine in health care workers. J Med Virol. (2022) 94:1442–9. doi: 10.1002/jmv.27458
11. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immunity. (2020) 87:34–9. doi: 10.1016/j.bbi.2020.04.027
12. Babicki M, Malchrzak W, Hans-Wytrychowska A, Mastalerz-Migas A. Impact of vaccination on the sense of security, the anxiety of COVID-19 and quality of life among polish. A nationwide online survey in Poland. Vaccines. (2021) 9:1444. doi: 10.3390/vaccines9121444
13. Liu CH, Zhang E, Wong GTF, Hyun S. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for US young adult mental health. Psychiatry Res. (2020) 290:113172. doi: 10.1016/j.psychres.2020.113172
14. The Novel Coronavirus Pneumonia Emergency Response Epidemiology T. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) - China, 2020. China CDC Wkly. (2020) 2:113–22. doi: 10.46234/ccdcw2020.032
15. Li XN, Huang Y, Wang W, Jing QL, Zhang CH, Qin PZ, et al. Effectiveness of inactivated SARS-CoV-2 vaccines against the Delta variant infection in Guangzhou: a test-negative case-control real-world study. Emerg Microbes Infect. (2021) 10:1751–9. doi: 10.1080/22221751.2021.1969291
16. Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
17. Gifford KA, Liu D, Romano R III, Jones RN, Jefferson AL. Development of a subjective cognitive decline questionnaire using item response theory: a pilot study. Alzheimers Dement. (2015) 1:429–39. doi: 10.1016/j.dadm.2015.09.004
18. Ware JEJr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I Conceptual framework and item selection. Med Care. (1992) 30:473–83. doi: 10.1097/00005650-199206000-00002
19. Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. (2011) 28:596–606. doi: 10.1002/da.20837
20. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
21. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. (2020) 295:200463. doi: 10.1148/radiol.2020200463
22. Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing. Radiology. (2020) 296:E41–5. doi: 10.1148/radiol.2020200343
23. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. (2021) 397:220–32. doi: 10.1016/S0140-6736(20)32656-8
24. VanderWeele TJ. Mediation analysis: a practitioner's guide. Annu Rev Public Health. (2016) 37:17–32. doi: 10.1146/annurev-publhealth-032315-021402
25. Campbell F, Archer B, Laurenson-Schafer H, Jinnai Y, Konings F, Batra N, et al. Increased transmissibility and global spread of SARS-CoV-2 variants of concern as at June 2021. Eurosurveillance. (2021) 26:2100509. doi: 10.2807/1560-7917.ES.2021.26.24.2100509
27. Elkan M, Dvir A, Zaidenstein R, Keller M, Kagansky D, Hochman C, et al. Patient-reported outcome measures after hospitalization during the COVID-19 pandemic: a survey among COVID-19 and non-COVID-19 patients. Int J Gen Med. (2021) 14:4829. doi: 10.2147/IJGM.S323316
28. Sanchez-Ramirez DC, Normand K, Zhaoyun Y, Torres-Castro R. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines. (2021) 9:900. doi: 10.3390/biomedicines9080900
29. Walle-Hansen M, Ranhoff A, Mellingsæter M, Wang-Hansen M, Myrstad M. Health-related quality of life, functional decline, and long-term mortality in older patients following hospitalisation due to COVID-19. BMC Geriatr. (2021) 21:199. doi: 10.1186/s12877-021-02140-x
30. Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. (2021) 4:e2128568. doi: 10.1001/jamanetworkopen.2021.28568
31. Katal S, Pouraryan A, Gholamrezanezhad A. COVID-19 vaccine is here: practical considerations for clinical imaging applications. Clin Imaging. (2021) 76:38–41. doi: 10.1016/j.clinimag.2021.01.023
32. Zheng Y-B, Sun J, Liu L, Zhao Y-M, Yan W, Yuan K, et al. COVID-19 vaccine-related psychological stress among general public in China. Front Psychiatry. (2021) 12:774504. doi: 10.3389/fpsyt.2021.774504
Keywords: COVID-19, SARS-CoV-2, B.1.617.2 Delta variant, vaccination, mental health, seroconversion time
Citation: Zhang W, Chen Q, Dai J, Lu J, Li J, Yi Y, Fu L, Li X, Liu J, Liufu J, Long C and Zhang B (2022) Mental health and chest CT scores mediate the relationship between COVID-19 vaccination status and seroconversion time: A cross-sectional observational study in B.1.617.2 (Delta) infection patients. Front. Public Health 10:974848. doi: 10.3389/fpubh.2022.974848
Received: 23 June 2022; Accepted: 03 October 2022;
Published: 19 October 2022.
Edited by:
Shuko Nojiri, Juntendo University, JapanReviewed by:
Chun Huai Luo, Johns Hopkins University, United StatesLi Fan, Shanghai Changzheng Hospital, China
Yuta Kawakami, Yokohama National University, Japan
Hojat Dehghanbanadaki, Tehran University of Medical Sciences, Iran
Copyright © 2022 Zhang, Chen, Dai, Lu, Li, Yi, Fu, Li, Liu, Liufu, Long and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Zhang, emhhbmdiaW5nX25hbmppbmdAbmp1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Wen Zhang
Wen Zhang Qian Chen1,2,3†
Qian Chen1,2,3† Jinghong Dai
Jinghong Dai Jie Li
Jie Li Yongxiang Yi
Yongxiang Yi Cong Long
Cong Long Bing Zhang
Bing Zhang