
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 05 January 2023
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.968281
This article is part of the Research Topic Promoting Self-Care Education and Empowerment in the Management of Chronic Disease View all 8 articles
Introduction: This study assessed the relevance, value, and effectiveness of “Taking Charge of My Life and Health” (TCMLH), a patient wellbeing peer group program for U.S. veterans focused on empowering them to identify what really matters in their lives and to work toward health goals that align with their mission, aspirations, or purpose in life. The potential of TCMLH to empower veterans to engage in self-care behaviors, make health behavior changes, and participate in health care decision making is important, as veterans are more likely than the general population to suffer from multiple chronic conditions that require ongoing self-management.
Methods: We conducted individual semi-structured interviews with 19 TCMLH facilitators serving in eight U.S. Veteran's Health Administration medical centers. Data were analyzed using an inductive approach to identify salient themes in facilitators' experiences.
Results: Facilitators reported that TCMLH participants demonstrated positive attitude changes (e.g., greater confidence and hope) and behavior changes (e.g., making healthcare appointments and implementing self-care practices) by program completion. Further, findings show that mindful awareness practices, the peer group setting, Whole Health assessment tools, and goal setting tools were perceived as the most impactful program elements leading to positive health behavior change.
Conclusion: Overall, findings suggest that this non-clinical peer group program can enhance patient wellbeing, and that there are certain program elements of TCMLH that are driving key attitudinal and behavioral changes.
The U.S. Veteran's Health Administration (VHA), the largest integrated health care system in the country, serves a patient population with higher rates of chronic illness and comorbidities than the general population (1, 2). Health outcomes for patients with common chronic conditions like diabetes and hypertension hinge on patients' ongoing self-care to manage their health conditions (3–5), which often involves learning, implementing, and sustaining substantial behavior changes (5, 6). Patients with chronic conditions have better health outcomes and reduced health care costs if they are more engaged, activated, and empowered—meaning they have knowledge, skills, self-efficacy, and motivation to effectively manage their health needs and health care interactions (7–13). To better serve its patients, the VHA implemented a Whole Health framework, a patient-centered care paradigm wherein veterans' personal values and goals—what patients want their health for—are central to care (14–17). Whole Health emphasizes a comprehensive patient-centered approach to health care that addresses mental, physical, emotional, and social drivers of health in a way that is personalized, proactive, and patient-driven. The goal is to foster greater patient engagement within a system of care that takes a preventive and proactive approach focused on wellbeing rather than one that is reactionary and disease-centric (14–16, 18–20).
The VHA's effort to transform its health care system into one grounded in Whole Health began in 2010 and has since expanded nationwide (15, 17). Implementation of Whole Health involved clinician and staff training, care redesign, cultivating champions, expansion of complementary and alternative health care, and offering aligned patient wellness programs (14, 21–26). The patient wellness program “Taking Charge of My Life and Health” (TCMLH) is a centerpiece for disseminating Whole Health to patients, aiming to foster patient engagement and motivation to make health behavior changes.
TCMLH provides a non-clinical, peer group environment for veterans to learn about Whole Health, the importance of self-care, and ways to achieve values-based health and wellness goals (21).1 A standard TCMLH group program involves weekly 90-min meetings over a 2 month period. Drawing from research demonstrating the beneficial impact of peer-based patient education programs on patients' health management, knowledge, and self-efficacy (27–32), learning occurs in a peer group setting that enables shared experience, social support, and accountability. TCMLH is not disease-specific; rather, the program aims to empower participants to identify motivators and provide tools and skills that align with their mission, aspirations, or purpose in life, ultimately bolstering their overall health and wellbeing.
Each TCMLH group program is led by a trained facilitator who is typically also a veteran, and who helps provide a safe, supportive group environment while guiding group participants through an experiential and interactive curriculum. Facilitators, who can be volunteers or VHA staff, go through a didactic and experiential 3-day training, where they learn about Whole Health concepts, tools, and skills and practice facilitating small groups through key session components (21). The facilitator role is designed to foster participants' own efforts in making meaningful health behavior changes—removed from the clinical context of advice-giving and clinical directives. Facilitators do not tell participants what they should be doing or give health recommendations. As Veterans in a given TCMLH group typically have a variety of health challenges, diagnoses, and overall needs, the group is designed to support each individual in taking steps toward improving their self-care and managing their health based on their own reflections on personal values, health and wellness needs, and what efforts are feasible and realistic.
Our multi-component evaluation of TCMLH was part of a larger project to design, implement, and evaluate Whole Health educational and wellness programming throughout the VHA system from 2013 to 2020 (VA777-12-C-002; Rychener, PI). We evaluated the TCMLH program from 2016 to 2018, assessing facilitator trainings (21), site implementation (33), and participant outcomes (34, 35). Our studies of veteran participant outcomes after attending TCMLH found significant improvements from baseline to program conclusion in outcomes related to patient self-management (patient activation, patient motivation, and self-care behaviors) and health indicators (global mental health, perceived stress, and quality of life) (34, 35). Two months post program, participants reported significant improvements in another patient self-management outcome (health care empowerment) and health indicator (global physical health), notably among a sample characterized by very high burden of chronic illnesses (34).
To better understand what may be driving these crucial outcomes, we undertook qualitative research to gain a richer understanding of what, how, and why aspects of TCMLH were beneficial. We conducted individual, semi-structured interviews with experienced TCMLH group program facilitators to explore (a) the most important or valuable aspects of TCMLH in helping veterans implement changes for improved health and wellness, and (b) the changes in attitudes and behaviors endorsed by participants. In this article, we present our findings, focusing on key program elements and their linkages to attitudinal and behavior changes.
The standard TMCLH program involves 9 weekly in-person 90-min meetings, but has been adapted for completion in shorter time periods, such as 6 weeks or an intensive weekend-long program (21, 34, 35).2 Trained facilitators serve as peer guides (not medical experts) for small groups of veterans, and foster a non-judgmental, safe, and supportive environment while guiding veterans through an experiential-heavy curriculum (34, 36). Each meeting includes at least one facilitator-led 5–10-min mindful awareness (MA) practice, such as mindful breathing and guided imagery exercises (36). MA attitudes – including non-judging, being present, having a beginner's mind, and patience – set the framework within which veterans explore their health and wellbeing. MA practices are evidence-based skills to manage stress and promote emotional and psychological wellbeing (37–39).
Throughout TCMLH, participants utilize Whole Health tools – the Circle of Health (Figure 1) and Personal Health Inventory (PHI) – and an action-oriented goal planning strategy to: (a) explore their “Mission, Aspirations, or Purpose;” (b) reflect on their personal values; (c) self-assess health and wellbeing strengths and needs; (d) learn about self-care; (e) set goals; and (f) take action to implement health-related changes (21, 34, 35, 41). The Circle of Health (Figure 1) is a visual touchstone for TCMLH, summarizing how different areas of life are interrelated and may impact one's health (40). The Circle of Health depicts the veteran (“Me”) as central, encircled by the key self-care practice of “Mindful Awareness,” signifying that identifying what matters most starts with reflection and observation. Eight areas of self-care surround the center: Working Your Body; Surroundings; Personal Development; Food and Drink; Recharge; Family, Friends and Coworkers; Spirit and Soul; and Power of The Mind. The outermost rings of the Circle of Health represent the veteran's professional care team and wider community as surrounding supports (14, 40). The second tool, the PHI, is a five-page booklet that operationalizes the eight areas of self-care in the form of a patient self-assessment tool, and is designed to facilitate reflection on areas of needs as well as strengths, and set the course for health behavior change action planning (42). The PHI provides space for veterans to reflect on their values, and then asks them to reflect on and assess each self-care area in terms of where they are now and where they would like to be. The PHI prompts veterans to consider how these assessments connect to their personal motivations and priorities.
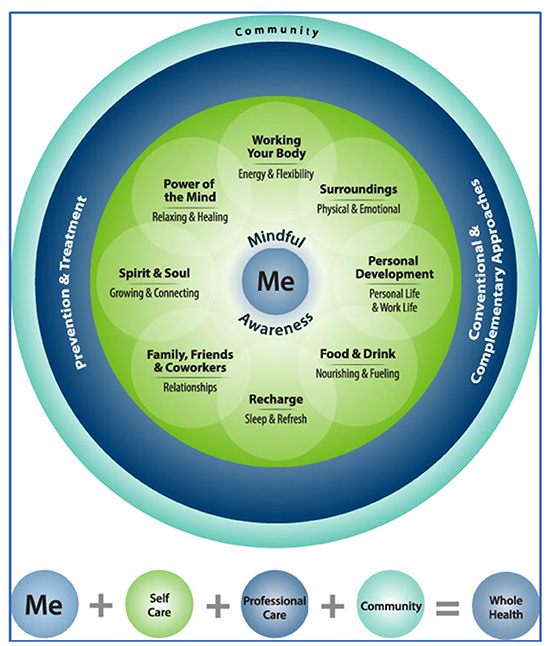
Figure 1. Circle of Health (40).
Once veterans have determined the self-care area in which they want to focus their efforts, TCMLH participants embark on goal setting. The program uses the “S.M.A.R.T.” goals format, learning to establish a goal that is Specific, Measurable, Action-oriented, Realistic, and Time-specific. Facilitators next guide participants in planning their action steps—thinking through the individual actions that are necessary to make progress toward the goal. Along with goal setting and action planning, TCMLH encourages participants to explore potential barriers to goal achievement and to plan how they can respond to and overcome those barriers. At subsequent sessions, facilitators initiate discussions wherein participants share about their progress as well as challenges they encountered, consider adjustments to their goals or action plans, and gain support from their peers who are doing similar work (36, 41).
Facilitators were eligible to participate in interviews if they had: (a) attended one of 12 facilitator trainings held between 2016 and 2018 that were within the scope of our programmatic evaluation (21), and (b) had facilitated at least one complete TCMLH program at their home VHA site. Considering research on the number of interviews necessary to reach thematic saturation (43, 44), we aimed to recruit 16–20 trained facilitators with varying levels of program delivery experience (i.e., 8–10 facilitators who had implemented fewer than five TCMLH programs and 8–10 who had delivered five or more) (43). The research team recruited facilitators via an email describing the interview purpose, length, topics, and confidentiality procedures. Those who expressed interest were scheduled for phone interviews based on their time and date preferences. As we desired to interview a sample of facilitators with a wide range of experience conducting TCMLH groups, we recruited a convenience sample until we reached saturation in terms of facilitation experience.
At the start of each interview, participants were reminded of the purpose, confidentiality procedures, voluntary nature of interview, and that the interviews would be audio-recorded for transcription. No incentives were provided. The research team was external to the VA, and VA staff did not have access to interview data. The authors' Institutional Review Board deemed this study exempt due to low risk, and the VHA's IRB designated this as a quality improvement evaluation.
The semi-structured, ~30-min phone interview involved questions about facilitators' observations and experiences with delivering the TCMLH program to veterans. The interview guide was informed by research on health behavior change, and drew on the authors' knowledge of the VA medical system and TCMLH curriculum. To ascertain facilitators' experiences with how TCMLH program components fostered veterans' development of skills, knowledge, and self-efficacy for health behavior change, we asked:
• What Whole Health tools or strategies did you use most often when facilitating the group(s)?
• What skills did you see veterans developing in the program?
• What knowledge do you think the veteran participants gained through the program?
• What would you say was the overall impact/value of TCMLH on the veterans you worked with?
• How would you describe veteran participants at the beginning and end of the program?
To gain broader perspective and fully saturate our data on topics related to potential program impacts, we also asked, ‘How would you describe the role that TCMLH serves within the broader VHA system?' Interviews were conducted in 2018 by BOR, an experienced qualitative researcher, and were audio-recorded.
The audio files from the interviews were transcribed and de-identified, then uploaded into Dedoose for qualitative analysis (45); all analysis steps were completed by two analysts trained in qualitative analysis methods with knowledge of TCMLH (BOR, RB) and were reviewed by the evaluation lead (MHA). First, transcripts were segmented into domains corresponding with interview topics, allowing for responses from any point in the interview to be grouped with the appropriate topic(s) (46). Next, the team reviewed the content for each interview topic and inductively generated a coding scheme wherein codes were descriptive of content themes (47, 48). Analysts applied codes to text, maintaining intercoder reliability through frequent meetings to review coding, reconcile code application disagreements, hone code definitions, and ensure concept stability. Such processes ensured codes represented concise and mutually exclusive concepts, and that content was comprehensively represented by codes. The combination of (a) interview topics guided by program goals and quantitative findings, (b) content-driven inductive analysis, (c) the iterative process of review and honing, and (d) the analysts' knowledge of TCMLH, provides a strong foundation for authenticity and trustworthiness of our analysis (49).
Nineteen TCMLH facilitators completed interviews ranging from 23 to 50 min long, averaging 37 min. Facilitators represented eight VA medical systems located throughout the eastern and midwestern U.S. (range 1–5 participants per system). The majority were veterans, and all were VA staff, most commonly in patient-facing non-clinical roles such as Health Coaches and Peer Support Specialists (see Table 1). Those interviewed were evenly split between men and women and averaged 49 years old (range 29–63). Just over half of the facilitators had led five or more TCMLH group programs. Most facilitated nine- or 6-week TCMLH program formats.
Facilitators' experiences and perceptions were grouped into two domains: (1) TCMLH program elements most important, beneficial, or impactful for veterans in cultivating health behavior change, and (2) observations of attitude and behavior changes among veterans while participating in TCMLH. Within the first domain, crucial elements of the program that fostered behavior change were (a) MA practices, (b) peer group environment, (c) Whole Health tools—specifically the Circle of Health and Personal Health Inventory (PHI), and (d) the S.M.A.R.T. goal setting process (see Table 2). In the second domain, facilitators described the ways in which they observed veterans change, which were grouped into two broad types: (a) attitudinal improvements (e.g., increased confidence and hopefulness); and (b) improved health behaviors (e.g., addressing health and wellbeing needs with providers, increasing physical activity, and practicing MA) (see Table 3). We present these findings in the following sections, and provide exemplary quotes for each. To preserve anonymity, quotes are not labeled with participant characteristics. To achieve representation across the sample, we reviewed the sources of all quotes to prevent heavy reliance on any one or a few participants, and ensure that quotes provided for each theme came from different participants and that all participants are represented in the results.
Facilitators emphasized that MA practices were a crucial element of the program that had a positive and meaningful impact on participants. According to facilitators, MA practice helped veterans address or improve upon a variety of everyday challenges, including insomnia, strong emotions, and PTSD symptoms, as well as pinpointing sources of increased physical pain during daily activities and identifying other wellness barriers. MA practice also helped veterans find creative ways to improve their environments to support better health, and was a coping strategy for managing stressors and improving communications. Facilitators explained:
“Learning to be more mindful and paying attention more, that has really seemed to hit it with a lot of them, you know, learning to be aware.”
“[MA] helps them to kind of step back, take a breath, and look at things for how they are, maybe not for how their emotions are telling them the way things are. ”
“I've had a lot of veterans just talk about how [MA is] just helping to calm them, just practicing some of the mindfulness skills, you know, they're able to really apply those in a lot of real-life situations.”
“[Program participant] would be in a work environment … with people bringing issues to him that would really just get under his skin. He just adapted doing [an MA practice] … and it just stopped affecting him. He would just rub his thumb and forefinger and remember, like, ‘I don't have to react to this.”'
“From talking to prior group members, they still practice it and I was really surprised by the benefits that they've achieved by practicing mindful awareness.”
Facilitators also asserted that the peer group environment was an essential aspect of the program. Exploring ones' health needs and developing goals took place in the context of a small group of people with similar experiences and challenges, an environment that facilitators were trained to foster as safe and non-judgmental (34). One facilitator described that in the group, “there was this sense of comradery in there...there's a deeper sense of connection with each other.” Participants have unique challenges, health needs, and goals, but they create shared experiences by working through the self-assessment and behavior change processes together. As a facilitator stated, “Where one was lacking, the other was strong, and they helped each other, you know, kind of help figure out their goals and how to best reach their goals. It was really cool to watch.”
The group setting of peers with relatable experiences provided an environment of support, respect, and emotional safety to veterans as they considered their current health and wellbeing, developed goals, and took action. The peer group provided personalized accountability that was attentive to each individual's values and priorities. Veterans enjoyed coming back each week to this meaningful community. Facilitators explained:
“Probably about starting the third or fourth [meeting] they're happy, they want to come... they want to be connected to the other veterans, and by the end they don't want the groups to stop because it's where they're coming to get their support to make healthy changes.”
“I think when they first come in, they don't really know what to expect and they're kind of reluctant... By the end of week two they're comfortable with each other. By week four... they're holding each other accountable, they're asking each other even before class, ‘How are you doing on your goal?”'
Facilitators asserted that they frequently used and referred back to the Whole Health program tools Circle of Health (Figure 1) and PHI (42), which portray one's overall wellbeing as multi-faceted. Facilitators stated they frequently referenced the Circle of Health to reinforce the concept that these various aspects of one's life are interrelated and influence wellbeing and health. One explained, “They started realizing, ‘Wow, this really does matter to me because I never gave it thought'...they're realizing how much it really does matter.” Further, this tool reinforces self-care as a priority, since it encourages reflection on how they care for themselves could have implications for others: “It helps them to understand that...they need to be the most important person—they need to take care of themselves before they can take care of anyone else.” Facilitators noted that the Circle of Health validates the importance of each participants' chosen goals for their health, even if they are areas of self-care not routinely discussed in a clinical context. For example, a participant knew they needed to improve on both mental and physical health, but by reflecting on the Circle of Health, realized that excess clutter around their home was negatively affecting their mental wellbeing (causing anxiety) and hindering their physical health (there was no space to incorporate a needed home exercise regimen). Thus, the veteran decided to address the “surroundings” area of the Circle of Health, setting a goal around cleaning and organizing their home.
Facilitators also pointed to the importance, value, and relevance of the PHI for veterans in their groups. A facilitator explained, “Everything that they're doing comes back to their PHI, really—what matters to them. …The PHI helps that veteran explore ‘What really matters to me most in this present moment, what am I really ready to tackle right now?”' These realizations helped veterans prioritize and set relevant goals, as well as gain awareness of their strengths and weaknesses. The PHI helps participants gain “self-recognition of their needs as well as their assets, and being comfortable with asking for assistance,” as one facilitator explained. Facilitators said that they could see participants gaining greater understanding of themselves as they worked through the PHI. Further, with the PHI including the eight areas of life from the Circle of Health, it gave them opportunities to choose a place to start that felt more feasible. One facilitator stated: “They're motivated to do the things that they know they can actually do. …They get that extra boost in their self-esteem, you know, ‘OK, I know I can do this; if I start with this, I know I'll have success.”'
Learning an effective goal-achievement process in TCMLH was another crucial element to the program according to facilitators. Participants learned how to set values-based goals, and to plan out actions needed to be successful. Learning how to examine the process for achieving goals was particularly relevant for veterans as their military experience often focused on carrying out orders rather than planning. Goal achievement tools in TCMLH enhanced self-efficacy as participants experienced their progress toward a goal. Facilitators explained:
“As a soldier … we tend to look at the final act, we just charge ahead. … I think when we break that down into small pieces for them, that helps them be able to realize that even some of the goals that they thought were a little bigger might be reachable. … That really helps them a lot.”
“I've had quite a few tell me that they didn't realize that they could do this; these are areas that they thought they would never be able to achieve again. … They understand now that, yes, this is still achievable and with baby steps, that you can have a quality life.”
A component to the goal-setting process in TCMLH is identifying barriers to goal progress and figuring out ways to overcome them. According to facilitators, the concept of planning for how to overcome barriers was new to many participants. As participants worked on taking steps toward their goals during TCMLH, they followed-up each week with their peers and considered how to overcome challenges. The process normalized setbacks, turning the focus away from failure toward learning from these experiences and planning ways to overcome challenges going forward. The attention to identifying and planning for barriers helped veterans stay motivated and build self-efficacy. Facilitators reported:
“A lot of times you hear, ‘Oh, barriers, I didn't even think about barriers.' Like, yep, life happens, there's going to be barriers.”
“Every week I would have them go back and review what their goals were or what went well, what their challenges were—I think that was a vital part. …I think that really was motivating to go, ‘Hey, when I come back next week I want to be able to say I did this or I did that.”'
Facilitators observed changes in group participants' attitudes toward themselves, their health, and the VA. They reported that veterans developed hope in themselves, gained self-efficacy in making changes and in managing their healthcare, developed a positive sense of self-worth, increased their confidence, and had a more positive view of the VA. Such changes are important to the VA's goal of providing patient-driven care, which requires patients to be involved as collaborators with their providers and clinical staff. Facilitators described how TCMLH changed attitudes:
“Number one for a lot of them is hope, a re-instilled hope that they can change, hope that maybe the whole VA system and healthcare system is going to shift to better meet their needs.”
“It's that they do have worth and they do have a purpose. It's that they matter to—not just to everybody else that they've been giving to their entire lives—but that they matter to themselves.”
“I have noticed... the ones that have been very... upset with the VA, that those have all been—they're very grateful, they changed to being grateful.”
“[TCMLH] provides veterans with a means of connecting with their provider and then ownership for their health... versus., ‘I'm going to do this because my doctor says I need to do this,' [instead] saying, ‘I'm going to do this because I think it is important to do.”'
Facilitators also described a variety of health and wellbeing behavior changes veterans had undertaken during the group program. Facilitators explained that TCMLH helped veterans re-orient their view of health through identifying their own motivations and priorities for taking health-related action. One facilitator noted he found his role in TCMLH rewarding because it helped participants connect their health needs to their personal motivations in life, saying, “the behavior changes only happen whenever it matters to them.” Facilitators described many participants' implementation of fitness activities, including walking, swimming, and yoga. A facilitator explained,
“Today one of my veterans from one of my first groups stopped by. …He had a new walking partner with him today. And so, not only are they doing the self-care, they're promoting it to their fellow veterans which is wonderful.”
Facilitators reported that veterans in their groups had implemented a variety of health-related behavior changes that covered all areas of the Circle of Health. Prominent examples included stress management with MA or tai chi classes, volunteering in the community, taking steps toward professional development, improving dietary habits, and working on strained relationships.
A vignette illustrates how the program helps veterans start making changes that lead to broader health impacts. In a facilitator's first TCMLH group, a veteran with severe COPD decided that her goal would be to clean and de-clutter her house. As she continued with TCMLH, she soon realized, in the words of the facilitator, “Wait—I've got to de-clutter my health!” As she reflected on her complex health challenges with her peers, she realized that the fundamental barrier to progress was her mobility – she had trouble walking and therefore avoided going to healthcare appointments in the expansive medical complex. With the group's support, she pursued eligibility for a power wheelchair and was successful in obtaining one, following which, she embarked on a process of engaging with her providers and learning about her health. The facilitator explained:
“[The power chair] gave her the opportunity to get to some more providers more often and go, ‘Tell me about COPD, tell me about this diagnosis, tell me about that.' She went back to every single one of them and got information about it so she knew. …Now she'll go into the yoga class and park her chair and grab her oxygen and just sit it down and do some yoga.”
This was a veteran who went from not knowing where to start with her cluttered home and complex health challenges, to finding the confidence to seek assistance, increase her knowledge about how to better manage her health conditions, and even try out yoga despite her body's difficulties.
Findings from our facilitator interviews suggest that key program elements were valuable in helping TCMLH participants implement changes to improve their health and wellbeing, and may suggest pathways toward achieving the health outcomes observed in our other studies (34, 35). MA practice was very prominent in facilitators' responses on the value and positive impact of TCMLH for veterans, as well as in the attitude and behavior changes they observed. The growing evidence base on positive outcomes of MA practice includes stress reduction, improved emotional regulation, and decreased experience of negative emotions (37–39, 50–52); facilitators observed similar outcomes and noted they were integral to some of the mental health issues the veterans were experiencing. Indeed, the VA has implemented MA within other aspects of health care delivery, as clinical trials demonstrated significant benefits of MA in decreasing veterans' PTSD and depression symptoms (53, 54). In terms of behavior change, learning MA through practice in each TCMLH session may foster positive outcome expectations and self-efficacy to practice MA on their own (55–60). MA provides veterans with a method through which they can self-monitor, or be more “aware” of their emotions, physical feelings, and external stimuli, which can also help them to sustain other health behavior changes (57–59).
Facilitators' observations of the benefits of the peer group environment also align with research demonstrating the efficacy of peer group programs in promoting self-management and health behavior change for individuals with chronic illnesses (30, 61–66). Studies suggest that being with peers while learning and attempting new or changed behaviors to better address health needs may increase patients' self-efficacy for enacting health promoting behaviors (57, 58, 67, 68). Indeed, facilitators observed that TCMLH participants found common ground in their needs to make changes and in the challenges they faced when attempting to implement changes, and in turn, became supportive resources to one another. Facilitators observed that this environment fostered skill-building and confidence.
Facilitators explained that the Circle of Health and PHI support veterans in realistic self-assessment of their health and help them connect their personal motivations to what aspects of their health they would like to change, leading to development of behavior change intentions. This approach is similar to that of health coaching with its incorporation of motivational interviewing, which can be effective in establishing readiness to make changes for a variety of health concerns (23, 69–74). Focusing on motivations and developing intentions are commonly recognized as important to initial phases of health behavior change, in order to prime the individual toward implementing a new or changed behavior (75). Facilitators noted that group participants tended to view health-related actions as doctors' orders, which left them unmotivated to implement challenging changes in their lives; as such, the time spent in TCMLH reflecting on motivations and the connection of personal values to behavior change intentions was important foundational work for this population.
According to facilitators, setting a S.M.A.R.T. goal in TMCLH and action planning, including planning for challenges, was very effective in spurring veterans toward implementing new or changed behaviors. Research suggests that this type of goal setting is most effective when combined with action planning (76), and TCMLH facilitators' feedback affirmed the benefits of this approach. TCMLH goal setting was effective in helping participants to undertake planned actions, and by making goals feasible, small successes bolstered their confidence.
Many theories of health behavior change emphasize the important role of self-efficacy in undertaking the actions necessary to improve one's own health, which is a recurring outcome of these key program elements according to facilitators (75). The Health Action Process Approach (HAPA) delineates three different types of self-efficacy for behavior change (77), which aligns with facilitators' experiences with TCMLH impacts. These forms of self-efficacy are: “action self-efficacy” (confidence in one's ability to implement the desired change), “maintenance self-efficacy” (confidence in one's ability to overcome barriers), and “recovery self-efficacy” (confidence in one's ability to move forward after experiencing setbacks) (58, 78). In TCMLH, working through the PHI may foster veterans' action self-efficacy; facilitators explained that it helped veterans think of their health more clearly and concretely—as opposed to confronting a complex set of dismaying needs and challenges—and prioritize needs based on their own values. Further, goal setting in TCMLH involves action planning, which also helps participants develop action self-efficacy as small steps seem feasible. Goal setting also involves reflection on challenges and planning how to overcome them, which addresses maintenance self-efficacy; facilitators reported that this was new to many participants and very relevant to their experiences. Finally, reviewing and reflecting on efforts, setbacks, and lessons learned within a supportive group of peers may help participants develop recovery self-efficacy as they can normalize their struggles and encourage one another in moving forward after setbacks (58, 61, 66).
Facilitators observed that TCMLH had positive attitudinal impacts on participants who lacked a sense of hope or had low self-confidence when starting the program. In previous research, we found that at the start of the program TCMLH participants averaged a “very low” score for sense of meaning and purpose in life in comparison to the general population (34). Facilitators reported that veterans gained hope that things can improve, confidence in themselves to make positive health changes and to handle adversity, and felt more empowerment regarding their healthcare. Beyond attitudinal shifts, in our research on patient outcomes, we found that following TCMLH participation, veterans reported statistically significant improvements in measures of self-care behaviors and goal progress (34), which facilitators affirmed as behavioral outcomes they observed in veterans they worked with. Facilitators described a variety of behaviors that participants had undertaken to the benefit of their wellbeing.
Finally, patients' increased involvement in their health care, such as by asking questions of providers to learn about their health conditions, adhering to appointments, and making changes in their daily lives, is crucial for improved outcomes for those with chronic illness. Research underscores the importance for patients with chronic illness to be actively involved in their health care - such patients are more likely to experience better health outcomes and care satisfaction, and have lower health care costs (7, 8, 79–82). Patients' enhanced knowledge and self-management is consistent with the theoretical underpinning of high-quality primary care and chronic disease management, suggesting TCMLH is aligned with clinical efforts to improve health outcomes (12, 83). Further, when providers affirm patients' personal priorities from a whole person perspective, this may encourage patients to improve their self-management, which can ultimately lead to improved health outcomes (13, 82, 84–87). The PHI can help patients communicate with healthcare providers about their personal values and motivations, and the VA has encouraged providers to integrate the PHI in their clinical work with patients. However, it can be difficult for providers to find enough time to engage patients in the discussion and reflection necessary for filling it out during standard appointments (26, 88). TCMLH provides ample time and an ideal environment for introspection and discussion of one's PHI, which they can bring to their next healthcare appointment. In this way, the program can serve as a crucial bridge to providers' efforts to integrate the PHI in patient care. TCMLH is thus an effective mechanism for integrating best practices—such as patient-centered communication, patient engagement, and shared decision-making—to enhance overall wellbeing.
Participation in interviews was voluntary and was not incentivized, thus it is possible that self-selection led to bias toward facilitators who were more enthusiastic about TCMLH. The potential for selection bias in findings is lessened due to the wide range of facilitators' characteristics, including amount of experience facilitating TCMLH. Further, the purpose of the interview as an evaluation component aimed at program improvement was emphasized before and during the interview to discourage social desirability bias. As the evaluation team was external to the VHA, this also provided another degree of separation from facilitators' workplaces.
In most cases, facilitators have limited experience with participants and cannot verify participants' attitudes and behaviors prior to TCMLH; their observations rely on what participants share throughout the program, and in some cases afterwards, as noted in the findings. Additionally, TCMLH participation is voluntary; those who participate through the entirety of the program may be more likely to benefit from it than those who decline to participate or attend infrequently. Facilitators may be more aware of the impacts on veterans who attend regularly and through the entirety of the program because of greater time spent with those veterans. Further, as a VHA program, TCMLH is situated within a large, integrated health care organization providing primary and specialty care, which is connected to further social welfare services and benefits. Such a context may also impact outcomes because program participants all received health care through the same system, perhaps making it easier for some participants to learn to navigate the health system and services through one another's experiences.
This study was conducted before the COVID-19 pandemic which led to alterations in access to patient programming and healthcare, and initiated substantial broadening of access to services via telehealth. Facilitators in this study spoke from their experiences offering the TCMLH group program in person; future research should evaluate implementation and outcomes of TCMLH programs offered remotely via web-based conferencing systems.
The goal of this study was to gain greater insight into how the TCMLH peer-led group program impacts veteran patient participants, using qualitative data from interviews with experienced TCMLH facilitators, many of whom were also veterans. Facilitator perspectives coalesced around the important roles of MA, the peer group context, the Whole Health tools, and S.M.A.R.T. goal-setting technique in supporting veterans in creating behavior change intentions, gaining self-efficacy, and moving forward with intended actions. Facilitators reported observing and receiving reports from participants of positive changes in attitudes and behaviors, which demonstrated the ways that TCMLH helped participants. Findings reinforce the relevance of the Whole Health paradigm for the U.S. veteran population, which emphasizes the inter-connectedness of different domains of wellbeing, the benefits of self-care, the utility of MA, and the importance of patients' personal values (14, 15, 18, 54, 71). Our findings illuminate mechanisms that may foster the gains observed in physical and mental health, patient motivation, and patient engagement among program participants in our pilot outcomes evaluations (34, 35), and underscore the potential for TCMLH to effectively engage a patient population with a substantial chronic illness burden in health self-management behaviors.
Identification of impactful program elements may be applied to solidifying program fidelity criteria especially given the desire for modified formats (21, 33, 89). This study can be applied to planning future research on program outcomes, including development of measures for various types of outcomes that occur during the process of behavior change, including the different types of self-efficacy, social identification, and empowerment, in addition to outcomes in physical and mental health. Future studies should also consider the broader implementation context (e.g., an integrated healthcare system implementing aligned programming throughout its system) to understand how it may help or hinder outcomes.
The raw data supporting the conclusions of this article will be made available by the authors, upon reasonable request.
In accordance with U.S. law, The Institutional Review Boards of the Pacific Institute for Research and Evaluation and the Veterans Health Administration deemed this study exempt from human subjects review due to its classification as quality improvement evaluation. As exempt research, written informed consent was not required.
DR lead development of the Taking Charge of My Life and Health program and facilitator training. MA and CD also contributed to program and training development. MA led program evaluation. Interviews were developed by MA and BR with input from DR. BR conducted interviews and led the analysis. MA, RB, and BR analyzed the interview data, in consultation with DR and CD. BR led manuscript development and writing, with RB, MA, and CD as contributing writers. All authors carefully reviewed the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the Veterans Health Administration Office of Patient Centered Care and Cultural Transformation [VA777-12-C-0002; DR, PI]. This study was also supported in part by the National Heart, Lung, And Blood Institute (NHLBI) of the National Institutes of Health (NIH) under Award Number K12HL138030 (CD) and by the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) (CIN 13-410) at the Durham VA Health Care System (CD).
We are deeply appreciative of the TCMLH facilitators who shared their time and insights for this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed in this article are those of the authors and do not necessarily represent the views of the U.S. Department of Veterans Affairs or NIH.
1. ^DR led TCMLH program development and facilitator trainings. MHA and CDD were also involved in the development of TCMLH and pilot facilitator trainings.
2. ^For further information about the TCMLH program, facilitator training, and program implementation, see our other publications (21, 33–35).
1. Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs associated with multimorbidity among VA patients. Med Care. (2014) 52:S31–S6. doi: 10.1097/MLR.0000000000000061
2. Eibner C, Krull H, Brown KM, Cefalu M, Mulcahy AW, Pollard M, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Quart. (2016) 5.
3. Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. (2014) 104:e25–31. doi: 10.2105/AJPH.2014.302041
4. Bodenheimer T, Lorig K, Holman H, Grumback K. Patient self-management of chronic disease in primary care. JAMA. (2002) 288:2469–75. doi: 10.1001/jama.288.19.2469
5. Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. (2003) 26:1–7. doi: 10.1207/S15324796ABM2601_01
6. Lorig KR, Sobel DS, Stewart AL, Brown BW. Jr, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. (1999) 37:5–14. doi: 10.1097/00005650-199901000-00003
7. Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff. (2015) 34:431–7. doi: 10.1377/hlthaff.2014.0452
8. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences) fewer data on costs. Health Aff. (2013) 32:207–14. doi: 10.1377/hlthaff.2012.1061
9. Hibbard JH, Mahoney ER, Stock R. Do increases in patient activation result in improved self-management behaviors? Health Serv. (2007) 3:669. doi: 10.1111/j.1475-6773.2006.00669.x
10. Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, et al. The patient centered medical home. A systematic review. Ann Intern Med. (2013) 158:169–78. doi: 10.7326/0003-4819-158-3-201302050-00579
11. Rosenthal MB, Alidina S, Friedberg MW, Singer SJ, Eastman D, Li Z, et al. A difference-in-difference analysis of changes in quality, utilization and cost following the colorado multi-payer patient-centered medical home pilot. J Gen Intern Med. (2016) 31:289–96. doi: 10.1007/s11606-015-3521-1
12. Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. (2001) 20:64–78. doi: 10.1377/hlthaff.20.6.64
13. Liddy C, Blazkho V, Mill K. Challenges of self-management when living with multiple chronic conditions: systematic review of the qualitative literature. Canadian Family Physician. (2014) 60:1123–33.
14. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. (2014) 52:S5–8. doi: 10.1097/MLR.0000000000000226
15. Gaudet T, Kligler B. Whole health in the whole system of the veterans administration: how will we know we have reached this future state? J Alternat Complement Med. (2019) 25:S7–S11. doi: 10.1089/acm.2018.29061.gau
16. Taylor SL, Bolton R, Huynh A, Dvorin K, Elwy AR, Bokhour BG, et al. What should health care systems consider when implementing complementary and integrative health: lessons from veterans health administration. J Alternat Complement Med. (2019) 25:S52–60. doi: 10.1089/acm.2018.0445
17. Bokhour BG, Fix GM, Mueller NM, Barker AM, Lavela SL, Hill JN, et al. How can healthcare organizations implement patient-centered care? Examining a large-scale cultural transformation. BMC Health Serv Res. (2018) 18:168. doi: 10.1186/s12913-018-2949-5
18. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the veterans affairs to a whole health system of care: time for action and research. Med Care. (2020) 58:295–300. doi: 10.1097/MLR.0000000000001316
19. Rindfleisch JA. Passport to Whole Health A Personal Health Planning Reference Manual. (2016). Available online at: http://projects.hsl.wisc.edu/SERVICE/key-resources/PDF%20Passport%20to%20Whole%20Health%20FINAL%2011-10-16.pdf (accessed August 14, 2019).
20. Bell IR, Caspi O, Schwartz GE, Grant KL, Gaudet TW, Rychener D, et al. Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med. (2002) 162:133–40. doi: 10.1001/archinte.162.2.133
21. Abadi MH, Drake C, Richard BO, Schweinhart A, Rychener D, Shamblen SR, et al. An evaluation of the facilitator training to implement “Taking Charge of My Life and Health”, a peer-led group program to promote self-care and patient empowerment in Veteran participants. Patient Educ Couns. (2020) 103:2489–98. doi: 10.1016/j.pec.2020.06.014
22. Collins DA, Shamblen SR, Atwood KA, Rychener DL, Scarbrough WH, Abadi MH, et al. Evaluation of a health coaching course for providers and staff in Veterans Health Affairs medical facilities. J Prim Care Community Health. (2015) 6:250–5. doi: 10.1177/2150131915591154
23. Collins DA, Thompson K, Atwood KA, Abadi MH, Rychener DL, Simmons LA. Integration of health coaching concepts and skills into clinical practice among VHA providers: a qualitative study. Glob Adv Health Med. (2018) 7:2164957X18757463. doi: 10.1177/2164957X18757463
24. Shamblen SR, Atwood K, Scarbrough W, Collins DA, Rindfleisch A, Kligler B, et al. Perceived behavioral control as a key to integrative medicine. J Evid Based Integrat Med. (2018) 23:2515690X18801581. doi: 10.1177/2515690X18801581
25. Atwood KA, Shamblen SR, Gaudet T, Rindfleisch A, Collins DA, Milovani C, et al. Impact of a clinical educational effort in driving transformation in health care. Fam Med. (2016) 48:711–9. Available online at: https://www.stfm.org/FamilyMedicine/Vol48Issue9/Atwood711
26. Simmons LA, Drake CD, Gaudet TW, Snyderman R. Personalized health planning in primary care settings. Fed Pract. (2016) 33:27–34.
27. Sallinen M, Kukkurainen ML, Peltokallio L. Finally heard, believed and accepted–Peer support in the narratives of women with fibromyalgia. Patient Educ Couns. (2011) 85:e126–e30. doi: 10.1016/j.pec.2011.02.011
28. Drake C, Meade C, Hull SK, Price A, Snyderman R. Integration of personalized health planning and shared medical appointments for patients with type 2 diabetes mellitus. South Med J. (2018) 111:674–82. doi: 10.14423/SMJ.0000000000000892
29. Stenberg U, Haaland-Øverby M, Fredriksen K, Westermann KF, Kvisvik T. A scoping review of the literature on benefits and challenges of participating in patient education programs aimed at promoting self-management for people living with chronic illness. Patient Educ Couns. (2016) 99:1759–71. doi: 10.1016/j.pec.2016.07.027
30. Fisher EB, Ballesteros J, Bhushan N, Coufal MM, Kowitt SD, McDonough AM, et al. Key features of peer support in chronic disease prevention and management. Health Aff. (2015) 34:1523–30. doi: 10.1377/hlthaff.2015.0365
31. Ramchand R, Ahluwalia SC, Xenakis L, Apaydin E, Raaen L, Grimm G, et al. systematic review of peer-supported interventions for health promotion and disease prevention. Prev Med. (2017) 101:156–70. doi: 10.1016/j.ypmed.2017.06.008
32. Lovell MR, Luckett T, Boyle FM, Phillips J, Agar M, Davidson PM. Patient education, coaching, and self-management for cancer pain. J Clin Oncol. (2014) 32:1712–20. doi: 10.1200/JCO.2013.52.4850
33. Drake C, Abadi MH, Batchelder HR, Richard BO, Balis LE, Rychener D. National implementation of a group-based program promoting patient engagement and peer support in the veterans health administration: a multi-methods evaluation. Int J Environ Res Public Health. (2022) 19:8333. doi: 10.3390/ijerph19148333
34. Abadi M, Richard B, Shamblen S, Drake C, Schweinhart A, Bokhour B, et al. Achieving whole health: a preliminary study of TCMLH, a group-based program promoting self-care and empowerment among veterans. Health Educ Behav. (2022) 49:347–57. doi: 10.1177/10901981211011043
35. Abadi MH, Barker A, Rao S, Orner M, Rychener D, Bokhour BG. Examining the impact of a peer-led group program for veteran engagement and well-being. J Alternat Complement Med. (2021) 27:S37–44. doi: 10.1089/acm.2020.0124
36. Office Office of Patient Centered Care & Cultural Transformation (OPCC&CT) Pacific Institute for Research and Evaluation (PIRE). Whole Health Facilitated Group: Taking Charge of My Life and Health Facilitator Guide: Veterans Health Administration, U.S. Department of Veterans Affairs. (2019). Available online at: https://www.va.gov/WHOLEHEALTHLIBRARY/docs/courses/TCMLH-Facilitator-Guide-2019-508.pdf (accessed November 27, 2022).
37. Carlson KJ, Silva SG, Langley J, Johnson C. Mindful-Veteran: the implementation of a brief stress reduction course. Complement Ther Clin Pract. (2013) 19:89–96. doi: 10.1016/j.ctcp.2012.12.003
38. Hempel S, Taylor S, Marshall N, Miake-Lye I, Beroes J, Shanman R, et al. Evidence map of mindfulness. In: Service HSRaD. Department of Veterans Affairs (2014).
39. Eberth J, Sedlmeier P. The effects of mindfulness meditation: a meta-analysis. Mindfulness. (2012) 3:174–89. doi: 10.1007/s12671-012-0101-x
40. Office of Patient Centered Care and Cultural Transformation (OPCC&CT). The Circle of Health: Veterans Health Administration, U.S. Department of Veterans Affairs. (2020). Available online at: https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp (accessed September 1, 2021).
41. Office Office of Patient Centered Care and Cultural Transformation (OPCC&CT) Pacific Institute for Research and Evaluation (PIRE). Whole Health Facilitated Group: Taking Charge of My Life and Health Participant Workbook: Veterans Health Administration, U.S. Department of Veterans Affairs. (2019). Available online at: https://www.va.gov/WHOLEHEALTHLIBRARY/docs/courses/TCMLH-Participant-Workbook-508.pdf (accessed November 27, 2022).
42. Office of Patient Centered Care and Cultural Transformation (OPCC&CT). Personal Health Inventory: Veterans Health Administration, U.S. Department of Veterans Affairs. (2019). Available online at: https://www.va.gov/WHOLEHEALTH/docs/10-773_PHI_July2019_508.pdf (accessed September 1, 2021).
43. Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Meth. (2006) 18:59–82. doi: 10.1177/1525822X05279903
44. Namey E, Guest G, McKenna K, Chen M. Evaluating bang for the buck: a cost-effectiveness comparison between individual interviews and focus groups based on thematic saturation levels. Am J Evaluat. (2016) 37:425–40. doi: 10.1177/1098214016630406
45. Dedoose version 8.3.45. Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Los Angeles, CA: SocioCultural Research Consultants, LLC (2021).
46. Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociol Methods Res. (2013) 42:294–320. doi: 10.1177/0049124113500475
47. Bernard HR. Social Research Methods: Qualitative and Quantitative Approaches, 2nd ed. Thousand Oaks, CA: Sage (2013).
48. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed. Thousand Oaks, CA: Sage (1994).
49. Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and Authenticity in Naturalistic Evaluation. In:Williams DD, , editor. Naturalistic Evaluation. New Directions for Program Evaluation. San Francisco: Jossey-Bass (1986). p. 73–84. doi: 10.1002/ev.1427
50. Cardaciotto L, Herbert JD, Forman EM, Moitra E, Farrow V. The assessment of present-moment awareness and acceptance: the Philadelphia mindfulness scale. Assessment. (2008) 15:204–23. doi: 10.1177/1073191107311467
51. Teper R, Segal ZV, Inzlicht M. Inside the mindful mind. Curr Dir Psychol Sci. (2013) 22:449–54. doi: 10.1177/0963721413495869
52. Smith BW, Shelley BM, Dalen J, Wiggins K, Tooley E, Bernard J, et al. pilot study comparing the effects of mindfulness-based and cognitive-behavioral stress reduction. J Altern Complement Med. (2008) 14:251–8. doi: 10.1089/acm.2007.0641
53. Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. (2015) 314:456–65. doi: 10.1001/jama.2015.8361
54. Possemato K, Bergen-Cico D, Treatman S, Allen C, Wade M, Pigeon W, et al. Randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. J Clin Psychol. (2016) 72:179–93. doi: 10.1002/jclp.22241
55. Keller J, Gellert P, Knoll N, Schneider M, Ernsting A. Self-efficacy and planning as predictors of physical activity in the context of workplace health promotion. Appl Psychol Health Well-Being. (2016) 8:301–21. doi: 10.1111/aphw.12073
56. Zhang CQ, Zhang R, Schwarzer R, Hagger MS, A. meta-analysis of the health action process approach. Health Psychol. (2019) 38:623–37. doi: 10.1037/hea0000728
57. Bandura A. Health promotion from the perspective of social cognitive theory. Psychology Health. (1998) 13:623–49. doi: 10.1080/08870449808407422
58. Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the health action process approach (HAPA). Rehabil Psychol. (2011) 56:161–70. doi: 10.1037/a0024509
59. McAlister AL, Perry CL, Parcel GS. How Individuals, Environments, and Health Behaviors Interact: Social Cognitive Theory. In:Glanz K, Rimer BK, Viswanath K, , editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th Edition ed. San Francisco: Jossey-Bass (2008). p. 169–88.
60. Luszczynska A, Tryburcy M, Schwarzer R. Improving fruit and vegetable consumption: a self-efficacy intervention compared with a combined self-efficacy and planning intervention. Health Educ Res. (2007) 22:630–8. doi: 10.1093/her/cyl133
61. Embuldeniya G, Veinot P, Bell E, Bell M, Nyhof-Young J, Sale JE, et al. The experience and impact of chronic disease peer support interventions: a qualitative synthesis. Patient Educ Couns. (2013) 92:3–12. doi: 10.1016/j.pec.2013.02.002
62. Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World psychiatry. (2012) 11:123–8. doi: 10.1016/j.wpsyc.2012.05.009
63. Lee S, Schorr E, Hadidi NN, Kelley R, Treat-Jacobson D, Lindquist R. Power of peer support to change health behavior to reduce risks for heart disease and stroke for african american men in a faith-based community. J Racial Ethn Health Disparities. (2018) 5:1107–16. doi: 10.1007/s40615-018-0460-7
64. Gomez-Pardo E, Fernandez-Alvira JM, Vilanova M, Haro D, Martinez R, Carvajal I, et al. A comprehensive lifestyle peer group-based intervention on cardiovascular risk factors: the randomized controlled fifty-fifty program. J Am Coll Cardiol. (2016) 67:476–85. doi: 10.1016/j.jacc.2015.10.033
65. Burke E, Pyle M, Machin K, Varese F, Morrison AP. The effects of peer support on empowerment, self-efficacy, and internalized stigma: a narrative synthesis and meta-analysis. Stigma and health. (2019) 4:337–56. doi: 10.1037/sah0000148
66. Arney JB, Odom E, Brown C, Jones L, Kamdar N, Kiefer L, et al. The value of peer support for self-management of diabetes among veterans in the empowering patients in chronic care intervention. Diabet Med. (2020) 37:805–13. doi: 10.1111/dme.14220
67. Willis E. Patients' self-efficacy within online health communities: facilitating chronic disease self-management behaviors through peer education. Health Commun. (2016) 31:299–307. doi: 10.1080/10410236.2014.950019
68. Cameron JE, Voth J, Jaglal SB, Guilcher SJT, Hawker G, Salbach NM. “In this together”: Social identification predicts health outcomes (via self-efficacy) in a chronic disease self-management program. Soc Sci Med. (2018) 208:172–9. doi: 10.1016/j.socscimed.2018.03.007
69. Linden A, Butterworth SW, Prochaska JO. Motivational interviewing-based health coaching as a chronic care intervention. J Eval Clin Pract. (2010) 16:166–74. doi: 10.1111/j.1365-2753.2009.01300.x
70. Simmons LA, Wolever RQ. Integrative health coaching and motivational interviewing: synergistic approaches to behavior change in healthcare. Glob Adv Health Med. (2013) 2:28–35. doi: 10.7453/gahmj.2013.037
71. Purcell N, Zamora K, Bertenthal D, Abadjian L, Tighe J, Seal KH. How VA whole health coaching can impact veterans' health and quality of life: a mixed-methods pilot program evaluation. Glob Adv Health Med. (2021) 10:1–13. doi: 10.1177/2164956121998283
72. VanBuskirk KA, Wetherell JL. Motivational interviewing with primary care populations: a systematic review and meta-analysis. J Behav Med. (2014) 37:768–80. doi: 10.1007/s10865-013-9527-4
73. Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. (2013) 93:157–68. doi: 10.1016/j.pec.2013.07.012
74. Long H, Howells K, Peters S, Blakemore A. Does health coaching improve health-related quality of life and reduce hospital admissions in people with chronic obstructive pulmonary disease? A systematic review and meta-analysis. Br J Health Psychol. (2019) 24:515–46. doi: 10.1111/bjhp.12366
75. Sheeran P, Klein WM, Rothman AJ. Health behavior change: moving from observation to intervention. Annu Rev Psychol. (2017) 68:573–600. doi: 10.1146/annurev-psych-010416-044007
76. Bailey RR. Goal setting and action planning for health behavior change. Am J Lifestyle Med. (2019) 13:615–8. doi: 10.1177/1559827617729634
77. Schwarzer R. Self-efficacy in the adoption and maintenance of health behaviors: Theoretical approaches and a new model. In:Schwarzer R, , editor. Self-Efficacy: Thought Control of Action. Washington, DC: Hemisphere (1992). p. 217–43.
78. Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
79. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs) delivery systems should know their patients' “scores”. Health Aff. (2013) 32:216–22. doi: 10.1377/hlthaff.2012.1064
80. El Miedany Y, El Gaafary M, Youssef S, El Aroussy N. Meaningful patient engagement in inflammatory arthritis: development of the patient motivation questionnaire. Clin Rheumatol. (2017) 1–9. doi: 10.1007/s10067-017-3605-x
81. Ivey SL, Shortell SM, Rodriguez HP, Wang YE. Patient engagement in ACO practices and patient-reported outcomes among adults with co-occurring chronic disease and mental health conditions. Med Care. (2018) 56:551–6. doi: 10.1097/MLR.0000000000000927
82. Pages-Puigdemont N, Mangues MA, Masip M, Gabriele G, Fernandez-Maldonado L, Blancafort S, et al. Patients' perspective of medication adherence in chronic conditions: a qualitative study. Adv Ther. (2016) 33:1740–54. doi: 10.1007/s12325-016-0394-6
83. Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Vonkorff M. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. (2005) 11:S7–15. doi: 10.1089/acm.2005.11.s-7
84. Kristensen MAT, Guassora AD, Arreskov AB, Waldorff FB, Holge-Hazelton B. 'I've put diabetes completely on the shelf till the mental stuff is in place'. How patients with doctor-assessed impaired self-care perceive disease, self-care, and support from general practitioners a qualitative study. Scand J Prim Health Care. (2018) 36:342–51. doi: 10.1080/02813432.2018.1487436
85. Coventry PA, Small N, Panagioti M, Adeyemi I, Bee P. Living with complexity marshalling resources: a systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Fam Pract. (2015) 16:171. doi: 10.1186/s12875-015-0345-3
86. Bratzke LC, Muehrer RJ, Kehl KA, Lee KS, Ward EC, Kwekkeboom KL. Self-management priority setting and decision-making in adults with multimorbidity: a narrative review of literature. Int J Nurs Stud. (2015) 52:744–55. doi: 10.1016/j.ijnurstu.2014.10.010
87. Coventry PA, Fisher L, Kenning C, Bee P, Bower P. Capacity, responsibility, and motivation: a critical qualitative evaluation of patient and practitioner views about barriers to self-management in people with multimorbidity. BMC Health Serv Res. (2014) 14:536. doi: 10.1186/s12913-014-0536-y
88. Howe RJ, Poulin LM, Federman DG. The personal health inventory: current use, perceived barriers, and benefits. Fed Pract Health Care Prof VA DoD PHS. (2017) 34:23–6.
Keywords: patient education, peer support, behavior change, veterans, self-care
Citation: Richard BO, Abadi MH, Drake CD, Rychener D and Bauer R (2023) “A reinstilled hope that they can change”: Facilitator perspectives on a self-care and health promotion peer group program for veterans. Front. Public Health 10:968281. doi: 10.3389/fpubh.2022.968281
Received: 13 June 2022; Accepted: 21 November 2022;
Published: 05 January 2023.
Edited by:
Raúl Juárez-Vela, University of La Rioja, SpainReviewed by:
Naomi Lee, Northern Arizona University, United StatesCopyright © 2023 Richard, Abadi, Drake, Rychener and Bauer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bonnie O. Richard, YnJpY2hhcmRAcGlyZS5vcmc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.