- 1Department of Social and Behavioral Studies, University West, Trollhättan, Sweden
- 2Department of Sociology and Work Science, Gothenburg University, Gothenburg, Sweden
- 3Campus Västervik, Västervik, Sweden
- 4Department of Psychology, Université de Poitiers, Univ Rennes, Univ Angers, Univ Brest, RPPSY, Poitiers, France
Background: The prevalent, neuropsychiatric, deficit perspective on children and youth diagnosed with ADHD prohibits a multidimensional approach where socio-economic status, family stress and relationships within the families are relevant factors to examine. Assessments of ADHD through the use of rating scales and short-term interventions may lead not only to overdiagnosis but also to a reductionistic approach in the psychiatric field. This literature review aims to address research outside the prevailing discourse on ADHD as an organic brain dysfunction and broaden the perspectives on children's behavioral difficulties.
Methods: The articles included in this applied, mixed-method, systematic review includes 26 peer-reviewed articles, both English and French, with a search focus on ADHD in children and youth related to Attachment styles and relationships.
Results: In the studies reported, researchers approached correlations between ADHD and attachment in different ways, and in most cases, there was a caution to address causality. The role of parents was found to be both buffering and aggravating for the appearance of ADHD. In the French case studies, the diagnosis was conceptualized as a relational phenomenon where the child's behavior was inseparable from family member's suffering.
Discussion: This review article illustrates how children's difficulties in terms of ADHD symptoms can be addressed through a paradigm where emotional and cognitive dysregulation is understood through psychosocial factors rather than as a neurological condition. In our view, to avoid an overly reductionistic and medicalized approach to children's behavioral difficulties, it is time to reiterate the value of the biopsychosocial perspective.
Conclusion: Professionals and researchers need to acknowledge that becoming diagnosed with ADHD has a strong connection to economic disadvantage, social status, and familial care. The academic discourse of addressing brain dysfunctions might serve the unintended purpose of masking emotional stress and social disadvantage that manifests across generations. A biopsychosocial approach to ADHD including family, emotional history, and socio-economic issues could imply a lesser focus on medical treatment as a first choice.
Introduction
In the relatively short history of psychiatry and mental health care, there are numerous examples of diagnoses, interventions, and explanations of human suffering that later has been questioned (1). Today, large resources are invested in research on the role of genetic and neurological factors in the etiology of Attention Deficit Hyperactivity Disorder (ADHD) [see for example (2), whereby neuropsychiatric assessment and treatment with central stimulant drugs are favored]. Faraone and Larssson's (2) view on future research advances implies a focus on unraveling the genetics of ADHD, leading to a breakthrough regarding etiology, diagnostics, and pharmacological intervention. As a consequence of the present focus on neurobiology in the discourse of ADHD symptoms, there is a risk that families seeking help for a child's behavioral problems tend to be recommended pharmacological treatment, at the expense of family therapy and individual child psychotherapy (3). The remarkably increased use of psychotropic medication can partly be explained by the fact that more and more children receive an ADHD diagnose, and some researchers have warned of a lack of knowledge about the effects on prefrontal cortex of central stimulants in children who are prescribed such medication, especially at an early age (4, 5). Consequently, it is important to address that even pre-school children (i.e., 3–5 years of age) are becoming a target of ADHD diagnostics, for example in the USA where there this group is on the rise, from 1.0 % in 2007 and 2008, to 2.4 % in 2016 (6).
It has been proven difficult to differentiate ADHD from normal variation (7). Since symptoms of the diagnosis is continuously distributed within the population – without thresholds – the prevalence is ultimately dependent on social consensus regarding the boundaries of deviation. In other words, a “natural” prevalence cannot be found out there, regardless of scientific rigor. Studies indicating that individuals with ADHD have a brain volume that is smaller compared to individuals without a diagnosis (8) has been met with criticism for shortcomings in implementation and conclusions (9). Many authors [cf. (10–12)] argue that ADHD is a heterogeneous, multifactorial problem and often with comorbidities, why the search for one explanatory factor must be abandoned. Such a view is not new, however. For more than half a century ago Anna Freud (13) shared her view on children who were perceived as having improper behavioral problems and sent to a psychiatric clinic, usually after a long series of complaints from home or from school. Freud underscored the importance of understanding the child's developmental process and suggested that the outbursts of rage and irrational behavior must be compared with the pattern of behavior within the family. Furthermore, she proposed a diagnostic procedure including a meta-psychological profile of the child, i.e., an image of dynamic, genetic, economic, structural, and adaptive data. In a recent article, Peter (14) draws our attention to the psychoanalytical view on ADHD as a complex phenomenon, requiring a multimodal approach. The author describes an uneven situation, where a well-functioning partnership between psychotherapy and medication is perceived as preferable, while critical views against the powerful, medical approach is “treated as potentially sensitive or problematic” (ibid, s. 40).
In modern times, some authors [e.g., (15–17) have advocated a biopsychosocial model in order to transcend dichotomies such as nature/nurture or individual/context, in the understanding of ADHD. While such a proposal is eligible, it is at the same time important not to throw important analytical categories – “unhelpful polarities” to quote Cooper - out with the bathwater. When it comes to psychiatric diagnoses, the gene-environment distinction is too often seemingly evaded through vague statements on “interaction.” The problem is that in the current neuro-era, any model that intertwines its components too thoroughly, risks an explanatory imbalance where “the brain” is given interpretive precedence: a BIO-psychosocial model. Cooper (16), for example, delivers a proposal for a biopsychosocial perspective by criticizing five (what we believe are partly relevant) claims that (1) there is an absence of neuro-scientific evidence for ADHD, (2) ADHD is an example of determinism, (3) ADHD rest on culturally specific judgements, (4) ADHD legitimizes the use of stimulant drugs, (5) ADHD is a medicalization of defiant behaviors. Despite his ambition of criticizing the polarity in itself, he almost exclusively criticizes one pole (e.g., constructionistic, sociological, cultural) from the position of the other pole (e.g., positivistic, materialistic, biological).
Our proposal for an application of a biopsychosocial approach rather strives to recognize the psychosocial conditions that are associated with getting an ADHD diagnosis. Such a take is needed due to the very uneven power dimensions within research paradigms and clinical discourse. A pubmed. search performed on March 3rd, 2022, on ADHD and the relationship to genetics, genes or hereditary or inherited, resulted in a total of 46.994 articles published between 1990 and 2022. Research on adverse psychosocial circumstances and the presence of high stress in families where these children grow up is sparse in comparison with the organic/synaptic discourse. This regime of biased knowledge production also manifests in clinical practice where, as Singh (15) noted already 20 years ago, methylphenidate is often being used without supporting interventions. Despite decades old evidence that early interaction patterns when infants are 6 months old is a more powerful predictor of distractibility and hyperactivity than biological or temperament factors (18), both research and clinical practice tend to be biased toward inherent organic traits rather than learned behavioral skills. Accordingly, Richard (17) discusses findings on how trauma and attachment impacts brain development and notes that psychosocial factors has been neglected in the development of ADHD symptoms: “Clinicians, when told that a child had a diagnosis of ADHD, have been found to underestimate the presence of psychosocial factors, and are less likely to ask about the possibility of neglect or abuse” (p. 483). A diversity of perspectives regarding etiology, diagnostics, and choice of therapy in children being investigated for ADHD is therefore required.
Social disadvantage, early attachment, and emotional regulation
As Cooper (16) notes, even if ADHD is socially constructed, some persons are more likely than others to be diagnosed. An important question of course is what makes this likeliness unevenly distributed. Despite observations on how gene-environment interaction in ADHD is complex (19) and how genetic risks tend to have small effect sizes (11), there is arguably a genetic emphasis in the dominant understanding of ADHD symptoms (20). At the same time, a Swedish population-based study confirmed the link between low family income and an increased risk for psychiatric disorders, including ADHD, even after adjusting for variables concerning parental psychiatric disorders (21, 22). So, what are the implications of the neuro-discourse on how to comprehend the association between ADHD and low income? The relationship between psychiatric disorder and social disadvantage, is associated with two main hypotheses: social drift and social causation (23). The more ADHD symptoms are conceptualized as a genetic syndrome, the more the social drift hypothesis is accentuated, portraying social conditions as a dependent variable rather than a cause of symptoms, through mediating factors (24). To put it bluntly: Social disadvantage is seen as genetically inherited.
The current biological discourse may point out that individuals and families to a greater extent end up in socioeconomically unfavorable conditions due to neuropsychiatric characteristics, rather than vice versa. However, a large epidemiological study of all individuals in Sweden between 5 and 60 years old, examined the prevalence of ADHD through stratified analysis (25). While native Swedes had a higher absolute risk of ADHD than immigrants, the stratified analysis illustrated a certain complexity, where the highest prevalence was found among 10–14 years old immigrant boys from families in the middle-income group. In the light of such data, it is difficult to adhere to a social drift hypothesis and claim that children to a greater extent have an immigrant background as a result of neuropsychiatric characteristics. Rather, it is apparent that there is a social causation where these individuals' difficulties are a result of their history of stress being more pronounced.
Additionally, in an article on a psychoanalytical perspective on the inner world of ADHD children, Salomonsson points to epigenetics as a “third way” that can “highlight and recognize the influence of experience on a neural level without disqualifying the predictive capacity of genes” [(26), p. 1]. Considering ADHD, epigenetics may contribute to valuable knowledge about the interplay between the proposed genetic heritage and the environment, literally the impact of social context on brain development (27). Conceptually, this includes both early-life experience and how epigenetic pathways responsible for detecting the input from the environment act, and what influences phenotypic variations have across generations. Bielawski and co-authors (28) reviewed a total of 65 human preclinical and clinical studies investigating the role of epigenetic processes, the so called “protein machines” on the development of several psychiatric disorders and proposed that the alterations of epigenetic processes can have a considerable effect on mental health.
To undertake a one-sided neuropsychiatric perspective on children and youth showing behavioral problems prohibits a multidimensional, clinical approach where socioeconomic factors, family stress, and relationships within the families are relevant factors in the understanding of how symptoms develop. Research have shown that <10% in children diagnosed with ADHD has a secure attachment (29). Shifting the locus of children's difficulties from the brain to the sphere of relations is not about blaming caregivers, but rather to illuminate the inequalities in parenting, illustrated in the correlation between socioeconomic status and (some) psychiatric diagnoses (cf. Richards, 2008). Individuals from a socially disadvantaged context simply have a higher risk of experiencing stress within the family. Accordingly, Murdock and Fagundes (30) have illustrated how attachment can work as a mediator between socioeconomic disadvantage during childhood and negative health outcomes in adulthood. Wylock et al. (12) conducted a systematic literature review aimed to clarify the nature of the relationship between ADHD and child attachment and the results showed that the link still seems to remain unclear. One explanation was that many studies tend to consider ADHD as a homogeneous disorder, but the observed differences among studies could also be a matter of the methodology used to measure attachment.
Emotional self-regulation, linked to the child's attachment behavior, is mainly organized during early childhood, and developed in relationships with others, i.e., foremost caregivers (31). Difficulties with emotional dysregulation are arguably hallmark features in both attachment and ADHD discourse (32, 33), why examining correlations between attachment difficulties and ADHD-symptoms might seem irrelevant or even tautological. Yet it is important to further investigate and discuss in what way these two conditions relate to each other, since psychiatric diagnoses seldom are a result of scientific discoveries but a question of how symptoms and behaviors are interpreted and conceptualized (34). The point of departure of this review article is that the well evaluated, theoretical framework of Attachment Theory (35) could play a more prominent role, not only in the understanding of ADHD and its strong linkages to social disadvantage (36), but also in a truly biopsychosocial model of psychiatric research and clinical practice.
Aims
An applied, mixed-method, systematic review was utilized to extend beyond the present medical ADHD discourse. Our goal was to synthesize quantitative and qualitative research focusing on early relations/attachment in association with children diagnosed with ADHD. In consideration with an ethical and empathic attitude to children's behavioral problems the prevailing biomedical view demands to be interrogated and replaced with a biopsychosocial disease model. The main goal of this article was:
To investigate the relationship between ADHD and attachment. Secondly, to discuss the results in relation to how psychosocial factors are required in the understanding of ADHD symptoms. In line with this goal our research question was: How does symptoms of ADHD relate to psychosocial conditions such as attachment, emotional growth, and family stress?
Method and procedure
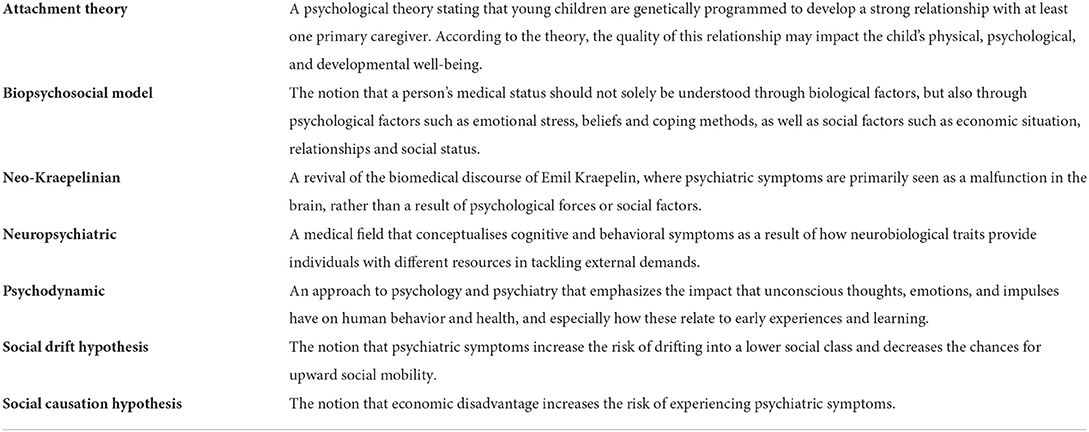
For guidance in performing this literature review we used the J. Briggs Institute's Methodology for Mixed Methods Systematic Reviews (MMSR), (37), based on two research paradigms, i.e., positivism and constructivism, of which we followed the latter paradigm. According to the authors, MMSRs has become an important method in health care research but is still under development. The mixed method can bring together quantitative and qualitative evidence “to create a breadth and depth of understanding that can confirm or dispute evidence and ultimately answer the review question posed” (ibid). Hong and colleagues (38) identified two types of frameworks that were dominant in mixed method reviews, referred to as the convergent and the sequential approach. We have adopted a convergent, integrated approach, which allows for a combination of quantitative and qualitative data. Allowing for an inductive and a deductive approach as in the mixed-method systematic review has the advantage of providing a well-founded view of the research subject. Terminology used throughout the text is clarified as Key terms (see Table 1).
Search history and eligibility criteria
For the search of articles according to the research question, the following databases was used: Psychlitt., Psychinfo, and Cairn. The searches were performed on March 24th (APA Psychinfo), April 1st (Psychlitt.), April 21st (Cairn) and May 4th (Psychlitt. and Psychinfo). Thesis, short, descriptive studies, and articles in other languages than English and French were initially removed from the records. Criteria for inclusion were empirical studies, systematic review studies published in peer-reviewed journals and studies that were eligible for ADHD in children and youth. The results of the searches were organized and specified as the following profile:
Peer-reviewed articles (English-spoken) with the search terms: ADHD or attention deficit hyperactivity disorder, Children or kids or youth or child, Attachment styles and relationships, or attachment styles in child development. Peer-reviewed articles (French-spoken) with the search terms: hyperactivité (hyperactivity), TDAH (ADHD), enfant (children), adolescent, famille (family).
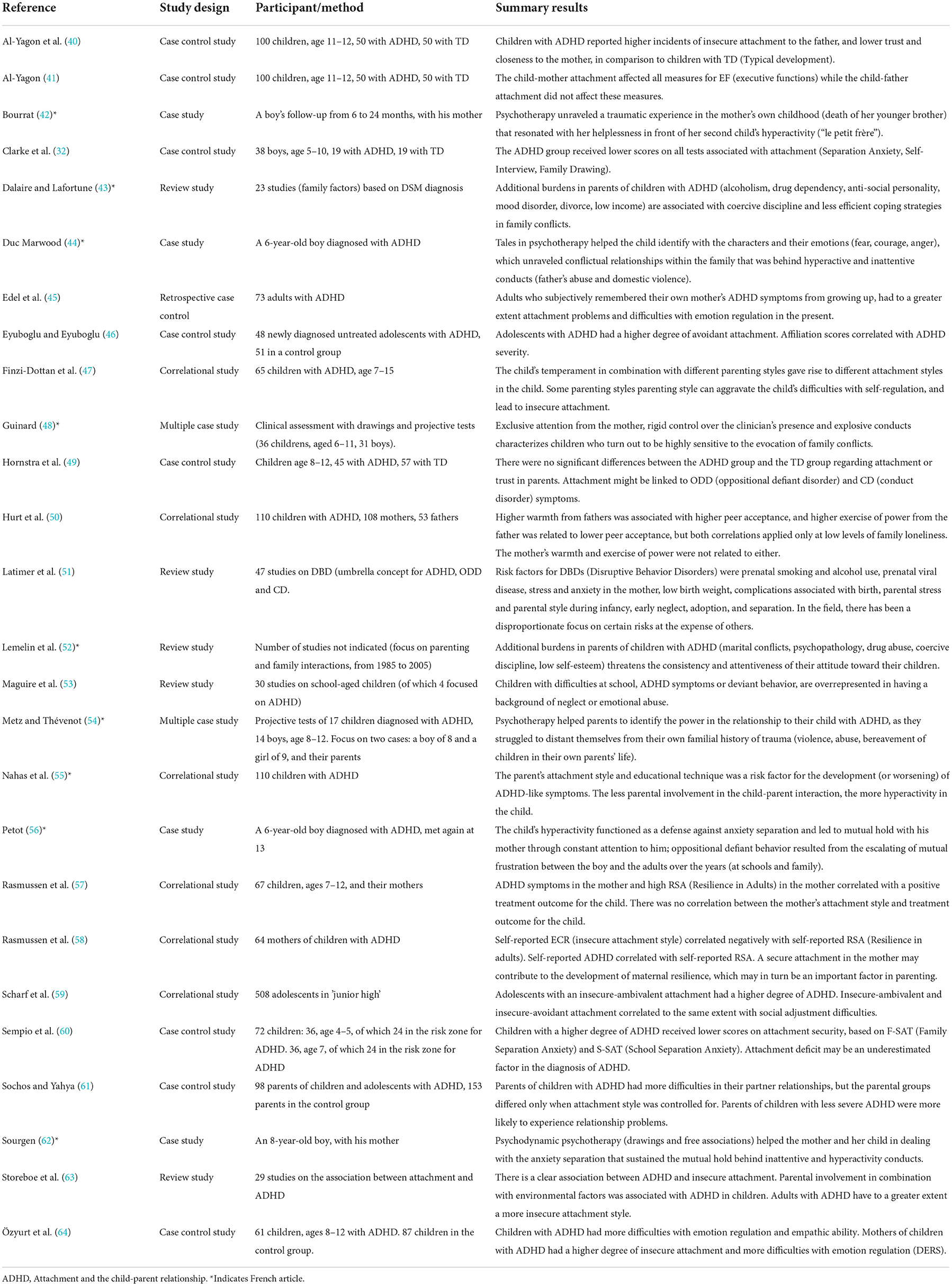
The total records identified after the initial database searches were 492. Removal of duplicates left 483 articles. The vast majority of articles written in French referred to a biomedical or neurodevelopmental perspective on ADHD. Articles that did not focus on psychosocial factors associated with child and family, such as opinion and theoretical articles, were excluded. Furthermore, some articles were excluded due to irrelevant content, i.e., focusing on other diagnoses or on treatment evaluation. Full-text articles assessed for eligibility amounted to 72 articles. In order to decide on eligibility the authors examined the full-text articles (n = 72). In total, 26 articles were found eligible for being included. The procedural steps taken throughout the review process are shown in Figure 1.
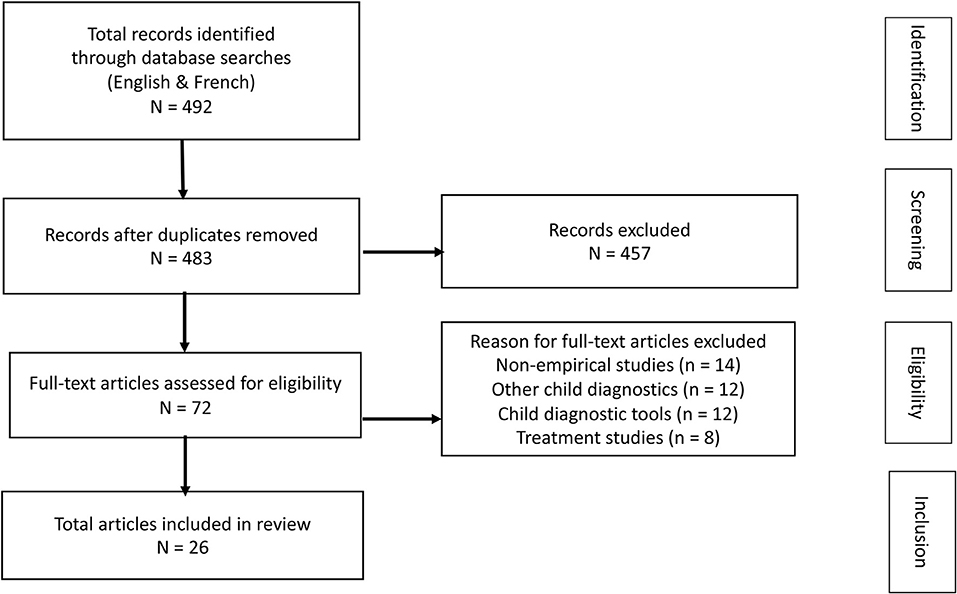
Figure 1. PRISMA Flow Diagram used in the review is adapted from Moher et al. (39).
Quality appraisal and synthesis of data
Throughout a narrow reading of included articles, the authors made their quality assessments after careful considerations and agreements improved by the research team. This implied a main focus on methodological rigor, i.e., if research questions were clearly formulated and could be answered with the data presented. Articles that did not meet with these criteria were sorted out. In the next step, the main findings of each of the articles were summarized and displayed in Table 2, where authors, research methodology and a brief summary of the content appear. The distribution of methodology of studies included were: Retrospective/Case control studies (9) – Case/multiple case studies (6) – Correlational studies (6) – Review studies (5).
Whether qualitative or quantitative, all eligible articles were converted into a text. To reach an approved level of structure and synthesis of the reviewed articles a comprehensive, close reading of each part were made by two authors (SIE, CH). The next step implied to characterize the content by searching for common denominators, i.e., themes describing those denominators, a process undertaken by the first author (SIE). Searching for themes was guided by Braun and Clarke (65) who declared that “a theme capturers something important about the data in relation to the research question.” Furthermore, a theme should represent a level of “patterned response or meaning within the data set” (ibid, p.82). In the final stage of the outline of the results, the themes were approved by all other participating authors. In order to give the reader's access to the French-spoken literature included in the review, abstracts of the French articles were translated into English by one author (ND), see Supplementary material including abstracts of 8 such articles.
Results
The main focus of the results in the review is how ADHD relate to attachment, including the family environment. Included articles had varying research methods and focuses (see Table 2), and were themed (65) with the following headings and sub-headings:
• ADHD, attachment, and the family environment
Competing discourses about the interaction between ADHD and attachment
ADHD, early development, and interactions with environmental stimuli
Narratives of family bonds in parents of children with ADHD
ADHD, attachment, and the family environment
In focus of this review, attachment difficulties were associated with ADHD symptoms in a different number of ways (63). Children diagnosed with ADHD had lower scores on tests associated with secure attachment (32), reported higher incidents of insecure attachment to the father, and lower trust and closeness to the mother (40). These attachment patterns were transferred to other contexts such as the school environment, where ADHD symptoms correlated with separation anxiety (60). However, Hornstra and colleagues (49), in a study of children between 8–12 years of age, found no connection between attachment and ADHD, but on the other hand that attachment can be an important factor for the development of ODD (Oppositional Defiant Disorder) and CD (Conduct Disorder). One systematic review of children with difficulties in school and behavioral problems (among them ADHD symptoms), showed that these children more often have a background of relational trauma, such as neglect or emotional abuse (53).
Competing discourses about the interaction between ADHD and attachment
In the studies found in this review, the researchers approached correlations between ADHD and attachment in different ways, and in most cases, there was a caution to address causality. However, differences in how results were interpreted and formulated could indicate disparate basic assumptions among researchers. Scharf and coworkers (59) thus found that adolescents with an insecure-ambivalent attachment had a higher degree of ADHD symptoms, suggesting that relational patterns can be a developmental precursor for ADHD and adjustment problems in school. Eyuboglu and Eyuboglu (46) on the other hand found that avoidant attachment issues among adolescents correlated with ADHD severity but framed this as an indication of how ADHD affects other aspects of life. In a similar way, several studies investigated the relationship between child and parent characteristics but emphasized different aspects when it came to the direction of influence. Özyurt and coworkers (64) found that mothers of children diagnosed with ADHD had a higher degree of insecure attachment and suggested that the emotion regulation skills of the mother are vital for the child's development process. Likewise, Nahas and fellow researchers (55) stated that both parent attachment style and parental educational techniques were risk factors for the development or worsening of ADHD symptoms. In that study, less parental involvement and supervision was associated with a heightened extent of hyperactivity in the child.
In a review by Weissenberger and colleagues (66) parenting style was found to be both buffering and aggravating for the appearance of ADHD. Parenting style including warmth, communication, and clear boundaries for the child (authoritative parenting) was associated with better educational outcome, less symptom severity and lower rates of drug abuse and addiction for the child diagnosed with ADHD. Parenting including harshness, neglect, and strict parenting behaviors (authoritarian parenting) was associated with exacerbated symptoms with inferior academic performance and an increased risk of being diagnosed with CD. Other researchers approached correlations between parental behavior and ADHD in an opposite way. Finzi-Dottan and colleagues (47) thus argued that temperament factors among children with ADHD evoke certain reactions among parents, which aggravate the child's regulation difficulties and lead to an insecure attachment. Another study found that parents of children with ADHD had more difficulties in their partner relationships, especially if they also had high attachment avoidance, making parents more unable to enjoy satisfaction in adult relationships (61). These kind of studies focuses on parent stress due to managing the child's behavior rather than how family aspects contribute to ADHD symptomatology in the child (67). Such a discourse is in line with older observational studies, which have shown that mothers of hyperactive children initiate less interaction, and are more critical and disapproving toward the child, suggesting that hyperactivity evoke negative behaviors from the mother (68). One of the studies in this review found that ADHD adults who from their own up-bringing subjectively remember ADHD symptoms in their mother, are at a greater risk of experiencing difficulties with emotion regulation in the present (45). Attachment difficulties among individuals with ADHD are thus seen as an effect of (undiagnosed) ADHD among primary caregivers since this had implications for parental style during childhood.
In summary, the results illustrated competing discourses about the interaction between ADHD and attachment. Correlations between parental behavior and difficulties expressed from a child could mean either that the former contributes to the latter, or the other way around, i.e., that inherent dysfunction in the brain of the child affects the interaction and the behavior of caregivers. Clarke and coworkers (32) point out that research on ADHD tends to focus on the latter, where psychosocial contributors are regarded as peripheral to the development of the disability. In the review of Storebø and coworkers, the relationship between attachment security and ADHD was described as follows: “ADHD and insecure attachment … are mutual risk factors; when one of the conditions occurs, there is an increased risk for developing the other” [(63), p. 193]. Thus, while the results mostly support a tangible connection between insecure attachment and ADHD symptoms, there are differing interpretations when it comes to the direction of influence between the characteristics of the child and the behavior of the caregivers.
ADHD, early development, and interactions with environmental stimuli
Lemelin and coworkers (52) found that marital conflicts, psychopathology, drug abuse, coercive discipline, and low self-esteem in parents of children with ADHD seriously impacted their relationship with the child. Dalaire and Lafortune (43) reported similar behavioral strain (alcoholism, drugs dependency, and mood disorder) in parents of ADHD children, associated with more coercive discipline on their children, and less efficient coping strategies in dealing with family conflicts. While most of the literature on ADHD and attachment focuses on emotional development, Al-Yagon with colleagues (40, 41) explored how attachment relates to executive functions, i.e., cognitive skills associated with goal-directed behavior. According to some research, the development of these higher cortical functions requires interactions with environmental stimuli (69). In one of the studies, impairments in executive functioning among the children was affected by the relationship with the mother (41).
Other results showed that high resilience in the mother was associated with a positive treatment outcome in the child (57). In one study, self-reported maternal resilience significantly correlated with attachment style, suggesting that attachment security may contribute to the perception of resilience, which may in turn be an important factor for children's developmental outcome (58). Rasmussen and colleagues also found that maternal resilience correlated with ADHD symptoms in the mother, and that these symptoms was associated with a positive treatment outcome in the child. This might be due to the fact that parent and child ADHD similarity is associated with the parent being more empathic with the child's difficulties (70).
Even when ADHD is mostly considered a neurological disorder, there seem to be several environmental factors affecting the condition. One study found that parent style from the father was associated with peer functioning of boys diagnosed with ADHD, but only among boys that experienced low levels of family loneliness (50). As Sempio and coworkers [39, p. 70–71] write: “Factors such as temperament and arousal … are not, on their own, powerful predictors of an insecurity pattern of behavior … they seem to have a significant impact only when other risk factors, such as poor parenting, economic hardship or difficulties of attachment are also present.” In a study of risk factors for Disruptive Behavior Disorders (which at the time of the study included both ADHD, ODD, and CD), Latimer and coworkers (51) found links to prenatal smoking and alcohol use, prenatal viral disease, stress and anxiety in the mother, low birth weight, complications associated with birth, parental stress and parental style during infancy, early neglect, adoption, and separation. The authors conclude that in this area of research, there has been a disproportionate focus on certain risks at the expense of others.
In summary, several studies confirmed the relationship between adverse psychosocial circumstances and ADHD symptoms. Results suggest that some factors only have a significant impact in combination with certain other factors. Also, instead of only investigating the correlation or the direction of influence between attachment and ADHD, attachment can pose as an independent variable that contributes to resilience, having a moderating impact on the genesis of symptoms.
Narratives of family bonds in parents of children with ADHD
Among the eight studies included in this review, some commonalities can be identified in the family dynamics within the French community. The authors describe a mutual and paradoxical hold between the child and the parents. The dynamics of ADHD is presented in the following way by Petot [60, p. 97]: “the more the child is inattentive, lacking in foresight and impulsive, the more his parents must be watchful, provident and vigilant instead of him” (original italics). Having to pay continuous attention, the parents are deprived of their own thoughts and feelings in their relationship to the child, and can hardly be involved personally in the interaction, as they most of the time only react to his lack of self-regulation. Petot (56) reported the case of a 6-year-old-boy diagnosed with ADHD, who subsequently developed ODD. The family bonds associated with ADHD was defined as a self-perpetuating process, in which the child's inattentiveness and the parents' required control over him resulted in escalating frustration on both sides, with subsequent punishments and provocations. As a consequence of this self-perpetuating process, Metz and Thévenot (54) suggest that parents feel discouraged to interact with their child, who repeatedly ignore their words and their own feelings. Moreover, the parents see the child as a stranger in the family, who is driven out of control by the disorder. Unwittingly, and instead of psychotherapy, they adopt a discourse that reify their child as having a biological disorder. Petot (56) and Sourgen (62) identified anxiety separation as a core threat to which both parents and their child defend themselves against, unconsciously turning it into turmoil, worries and frustration, which could lead to a highly seductive attitude. Accordingly, Guinard (48) reported examples of relational demands from children with ADHD, requiring an immediate attention drawn back to them when other interactions were initiated.
Families encountered in consultation for ADHD were afflicted by traumatic events in the family history, where the parents' helplessness in front of their child's behavior resonated with past circumstances they were not able to make sense of. Bourrat (42) reported the case of a 6 months old boy, whose mother felt overwhelmed by guilt for not being able to temper and interact with him (her second child). The childbirth had been painful, and the boy had to be hospitalized, after which both parents worried for the unrest and inattentiveness in the little boy. In her own childhood, the mother witnessed the death of her younger brother who died in a traffic accident. The psychotherapy process helped the mother identify her fears for her second child, that resonated unconsciously with the horror of her younger brother's death and interactions with the boy was restored. As suggested by Metz and Thévenot (54), parents who from their own family history face struggles without closure, may feel resourceless when it comes to raising a child diagnosed with ADHD. In psychotherapy, parents could process unconscious emotions that interfered with contemporary relations between parents and children. For instance, a father could express his reluctance to exert authority with his child, remembering how violent his own father was. The authors suggest that these kind of events have a powerful impact on the parents' relationship to their child. Duc Marwood (44) suggested that inattentiveness and disruptive behaviors sometimes can function as an unconscious strategy to avoid thoughts and feelings connected to violence witnessed in the family. In line with Metz and Thévenot (54) the author considered that, in some instances, hyperactivity should draw the attention of health professionals to emotional suffering that the child is unable to contain and speak about.
Furthermore, the authors suggest that family members, and especially the child with ADHD, are highly sensitive to words that may evoke inner conflicts. Sourgen (62) and Duc Marwood (44) describe boys who display strong reluctance in talking about themselves. Metz and Thévenot (54) met parents who were distant from feelings and thoughts about their own relationships, apart from the frustration their child with ADHD evoked in them. The children didn't want to talk or listen to the clinicians, and behaved in an aggressive manner, claiming that they could not narrate their feelings. Similarly, Guinard (48) observed that a majority of the children she met were reluctant to share their imagination or play with their inner fantasies when being shown pictures they were expected to comment on (like the Rorschach Inkblot test). Instead, the children wanted to control the activities and give order to the clinician, as if they were authoritative adults. For instance, one daughter would immediately ask the clinician to mind her business, requiring her mother to shut up, when the latter recalled a period of hospitalization during which the daughter and the mother were separated from one another. In doing so, the child seemed to defend herself from painful emotions associated with the separation.
In summary, the psychodynamic case studies illustrated how the “ADHD behaviors” of the child were inseparable from ongoing relational processes within the family. Both children's and parent's behavior sometimes functioned as defenses from unpleasant emotions, and these were sometimes connected to earlier events in the family history. Through psychotherapy, both children and parents could receive help in becoming aware of and processing emotions (i.e., learning to self-regulate, instead of acting out dysfunctional behaviors as an automated avoidance strategy).
Discussion
There is a noticeable risk of over-diagnosis when the treatment paradigm primarily targets the child's individual traits and overlooks contextual factors such as economic hardships and complications in family life. This review article has given examples of how the later are important variables in the understanding of ADHD symptoms. Several of the case studies based on psychotherapy explore the relationships between the parents' stress and their children's behavior (43, 52, 54, 61). Dalaire and Lafortune describe the presence of severe distress in families of children with ADHD, such as divorce, drug dependency and economic disadvantage. Early relationships also seem to have implications for how some cognitive skills develop in children with ADHD (41). Important to note is that while several studies in this review identified correlations between attachment deficits and ADHD, Hornstra and colleagues (49), found no such connection, but on the other hand that attachment related to ODD and CD. In the light of these findings, one might ask whether some behavioral difficulties are more connected to attachment and environmental conditions than others. Or if the findings rather illustrate the complexity of environment-behavior relations, and the fallacy of sorting children's adjustment difficulties into medical boxes.
Being recognized as someone who have ADHD is not seldom felt as a relief and a sense of social belonging (71, 72). The experience of “belonging” underlines the importance of a socially inclusive treatment of children who risk ending up outside normality. Contrary, there is a risk that children with deviant behavior might become recipients of an individualized discourse where the focus lies on vague labels rather than on the lifeworld of the person. As an example, a child with behavioral misconducts was helped in psychotherapy to express strong emotions being tied to hyperactivity and inattentiveness associated to abuse and domestic violence (44). According to such a treatment paradigm, a child's inability to conform to the prevailing pattern of behavior might be a way of expressing an important message, which can contribute to recognizing unhealthy and pathogenic modes in society, school, or family (13). We argue that the mainstream discourse on ADHD, despite scholarly ambitions of describing a “multifactorial” condition, tends to shift the focus from a relational perspective on the subject, to a focus on the object, where phenomena such as attention, impulsivity, and executive functioning, are regarded as static traits of the brain, rather than a reflection of stress, social disadvantage, or lack of learned skills.
To avoid an overly reductionistic approach to children with behavioral problems, it is high time to reiterate the value of a biopsychosocial perspective, that gives equal attention to all its components. In a published essay in Lancet Psychiatry, Gask (73) describes the emergence and dismantling of the biopsychosocial model and highlights the importance of time, i.e., why the patient is applying for professional help at a specific moment in life. She emphasizes the importance of recording how the biological, psychological, and social factors vary, not only between disease episodes but also over time and circumstances in the patient's life. This is a highly important aspect in the understanding of ADHD symptoms, especially in an era where young people who have been diagnosed in childhood are beginning to request their “neuro-disorder” to be reconsidered [for a Swedish context, see (74, 75)]. Previous research on health in adults has shown how attachment can be highly relevant for a biopsychosocial model, since it can work as a mediator between “the social” (low SES) and “the bio” (symptoms) (30). Accordingly, we argue that the relational perspective inherent in the attachment paradigm can contribute to a holistic understanding of children's emotional and behavioral difficulties by addressing how external circumstances can have impact on the development of the child's “internal working models, which reflect the outer lived experiences on an inner level” [(63), p. 187]. When it comes to ADHD, the academic discourse of overemphasizing the brain, might in fact serve the unintended purpose of masking the emotional stress and social disadvantage that manifests across generations.
As Latimer and coworkers (51) concludes, in the research area of disruptive behavior disorders, which at the time of their study included ADHD, there has been a disproportionate focus on certain risks at the expense of others. Our main argument here is that academic discourse is not solely based on scientific facts, but on how researchers across time and space choose to focus on different empirical arenas and theoretical models, due to different core assumptions. The difference between developmental paradigms such as attachment or psychodynamic theory on the one hand, and the neuropsychiatric discourse on the other, is that the former to a greater extent emphasizes how psychological characteristics (e.g., impulse control, executive functions, ability to concentrate, relationships) develop in harmony with the social environment. At the same time, it is important not to land in a simplified either/or approach to “organic” syndromes such as ADHD vs. “learned” behaviors such as attachment difficulties since research illustrates how these (along with sociological variables) are tightly interwoven (63). Despite this, we argue that the view on the relationship between neuropsychiatric traits and environmental factors needs to be much more nuanced. To illustrate, it would most certainly be far more acceptable in contemporary academic discourse to claim that attachment difficulties could accentuate ADHD symptoms, than to claim that it actually creates them. Such a discourse contains a puzzling view on the link between brain and environment. Since ADHD is continuously distributed in the population, where getting a diagnosis is the same as passing the clinical threshold or cut-off, any accentuation of ADHD traits must be equivalent to etiological cause.
Strengths and limitations
The present review article demonstrates how complicated the phenomenon of ADHD is. We believe that it is both an opportunity and a duty as researchers to present the breadth of knowledge that different scientific disciplines can offer. One of the strengths of this contribution is that the everyday life of those most affected by ADHD diagnoses have been given attention, which may offer a more integrated and broad view on the research area. Additionally, alternative explanatory models for children's inattention and hyperactivity and the importance of family relationships were invoked in the French studies. While all authors have a research affiliation within behavioral and social science and three authors are experienced in clinical psychology, there is a width among the researchers' scientific backgrounds including sociology, medical anthropology, psychoanalysis, and the interdisciplinary field of child and youth studies. Some limitations of the study must also be disclosed. Many of the studies included in this review have small samples and the limited number of reviewed articles may jeopardize the conclusions that can be drawn. Furthermore, leaning on a review method like the mixed-method systematic review implies a number of procedural steps, of which we have been able to follow some, and not others. We have, however clarified in detail how the review process was carried out.
Implications for future research
No doubt, the vast majority of research on ADHD continues to rest on neurological assumptions about children's attributes as a unified and inherent, biological body. Given the unequal allocation of resources available in contemporary ADHD research, there is reason to consider the long-term consequences that the lack of a biopsychosocial research paradigm has for scientific discourse and reliability. But also, what the effect is for those youngsters who are expected to live their lives with a label that implies that to fit into society they need to be dependent on drugs. Future research and clinical practice can benefit from more openness and less rigid beliefs in the understanding of behavioral difficulties in children (and adults). Such a paradigm shift includes more resources for the humanities and social sciences in studies of hyperactivity, concentration and emotional regulation. Otherwise, there is a risk of another 40 years with a continuing, rising curve of even younger children who are medicalized and defined as having a disease/disorder. To perceive children as subjects whose development is dependent on a secure and trustful social context can raise parents' (and society's) sensitivity to children's needs of sharing their feelings of frustration. The child psychiatrist Sami Timimi has offered a treatment option “The Rational Awareness Program” for parents and their children struggling with challenging behavior (76). This family therapy prioritizes building relationships, over controlling the behaviors and symptoms of the child. Instead of medicalizing the child's behavior through a diagnosis of the brain, focus is on giving support and help to the parents, which serves as a treatment also for the child. In accordance with this view, psychotherapeutic techniques (26, 77–79) could be alternatives to the current, often first-of-choice, central-stimulant medication. Within a psychotherapeutic framework, children diagnosed with ADHD can receive unique attention allowing them to communicate what they perceive as most disturbing in their life.
Conclusions
This review article has investigated and discussed how children's behavioral difficulties labeled as ADHD can be understood through factors such as attachment, family relations and emotional history (and indirectly also broader sociological variables). Such a focus does not deny that individuals have differing genetic vulnerabilities for developing psychiatric symptoms, but rather strives to re-establish a biopsychosocial model that has become vaguer in a neo-Kraepelinian era. Even though Anna Freud (13) wrote her book more than half a century ago, her way of comprehending a child with severe behavioral problems is remarkably inclusive when it comes to etiological considerations, and it has none of the reductionistic ambitions guiding much of the biomedical theorizing that dominates the view on ADHD today. Such a position opposes the prevailing biomedical view, not because it denies that we are biological creatures, but because it refuses to reduce behavioral issues into a biological disturbance and advocates a model that puts equal attention on biological, psychological, and social factors in understanding and treating ADHD symptoms.
Author contributions
SE wrote the first draft and was responsible for guidance in the process of writing the paper. The search for publications was done by SE, CH, and ND. All authors participated in reading and summarizing the review articles and writing the result section. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.966900/full#supplementary-material
References
1. Erlandsson SI, Punzi E. (2017). A biased ADHD discourse ignores human uniqueness. Int J Qual Stud Health Well-being. (2017) 12:1319584. doi: 10.1080/17482631.2017.1319584
2. Faraone SV, Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol Psychiatry. (2019) 24:562–75. doi: 10.1038/s41380-018-0070-0
3. LeFever Watson G, Powell A, Antonuccio DO, Healy D. Shooting the messenger: the case of ADHD. J Contemp Psychother. (2014) 44:43–52. doi: 10.1007/s10879-013-9244-x
4. Urban KR, Gao WJ. Evolution of the study of methylphenidate and its actions on the adult versus juvenile brain. J Atten Disord. (2015) 19:603. doi: 10.1177/1087054712455504
5. Bouziane C, Filatova OG, Schrantee A, Caan MWA, Vos FM, Reneman L, et al. White matter by diffusion MRI following methylphenidate treatment: a randomized control trial in males with Attention Deficit/Hyperactivity Disorder. Radiology. (2019) 293:186–92. doi: 10.1148/radiol.2019182528
6. Froelich TE. Comparison of medication treatments for preschool children with ADHD: a first step toward addressing a critical gap. JAMA. (2021) 325:2049–50. doi: 10.1001/jama.2021.5603
7. Takahashi N, Ishizuka K, Toshiya I. Peripheral biomarkers of attention-deficit hyperactivity disorder: current status and future perspective. J Psychiatric Res. (2021) 137:465–70. doi: 10.1016/j.jpsychires.2021.03.012
8. Hoogman M, Bralten J, Hibar DP, Mennes M, Zwiers MP, Schweren LSJ, et al. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis. Lancet Psychiatry. (2017) 4:310–9. doi: 10.1016./52215-0366(17)30049-4
9. Batstra L, Meerman S, Conners K, Frances A. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults. Lancet Psychiatry. (2017) 4:439. doi: 10.1016/S2215-0366(17)30107-4
10. Moynihan R, Doust J, Henry D. Preventing overdiagnosis: how to stop harming the healthy. BMJ. (2012) 344:e3502. doi: 10.1136/bmj.e3502
11. Thapar A, Cooper M, Eyre O, Langley K. Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry. (2013) 54:3–16. doi: 10.1111/j.1469-7610.2012.02611.x
12. Wylock JF, Borghini A, Slama H, Delvenne V. Child attachment and ADHD: a systematic review. Euro Child Adolesc Psychiatry. (2021) doi: 10.1007/s00787-021-01773-y
14. Peter S. An (un)happy marriage: chilad psychology with children who are medicated for ADHD. J Child Psychother. (2021) 47:32–53. doi: 10.1080/0075417X.2021.1945657
15. Singh I. Biology in context: social and cultural perspectives on ADHD. Children and Society. (2002) 16:360–7. doi: 10.1002/chi.746
16. Cooper P. Like alligators bobbing for poodles? a critical discussion of education, ADHD and the biopsychosocial perspective J Philosophy Educ. (2008) 42:457–74. doi: 10.1111/j.1467-9752.2008.00657.x
17. Richards LME. It is time for a more integrated bio-psycho-social approach to ADHD. Clin Child Psychol Psychiatry. (2012) 18:483–503. doi: 10.1177/1359104512458228
18. Carlson EA, Jacobvitz D, Sroufe LA. A developmental investigation of inattentiveness and hyperactivity. Child Dev. (1995) 66:37–54. doi: 10.1111/j.1467-8624.1995.tb00854.x
19. Nigg J, Nikolas M, Burt A. Measured gene-by-environment interaction in relation to attention-deficit/hyperactivity disorder. J Am Acad Child Adeolsc Psychiatry. (2010) 49:863–73. doi: 10.1016/j.jaac.2010.01.025
20. Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, et al. The World federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neurosci Biobehav Rev. (2021) 128:789–818. doi: 10.1016/j.neubiorev.2021.01.022
21. Björkenstam E, Cheng S, Bjurström B, Pebley AR, Björkenstam C, Kosidou K. Association between income trajectories in childhood and psychiatric disorder: a Swedish population-based study. Mental Health. (2017) 71:648–54. doi: 10.1136./jech-2016-208513
22. Björkenstam E, Björkenstam C, Jablonska B, Kosidou K. Cumulative exposure to childhood adversity and treated attention deficit/hyperactivity disorder: a cohort study of 543 650 adolescents and young adults in Sweden. Psychol Med. (2018) 48:498–507. doi: 10.1017/S0033291717001933
23. Topor A, Ljungqvist I. Money. Social relationships and the sense of self: the consequences of an improved financial situation for persons suffering from serious mental illness. Commun Mental Health J. (2017) 53:823–31. doi: 10.1007/s10597-017-0146-3
24. Draine J. Mental health, mental illnesses, poverty, justice, and social justice. American J Psychiatric Rehabil. (2013) 16:87–90. doi: 10.1080/15487768.2013.789684
25. Axrud R. Socioeconomic Disparities in Attention Deficit Hyperactivity Disorder (ADHD) in Sweden: A Cross-Sectional Social Epidemiological Study using Analyses of Individual Heterogeneity and Discriminatory Accuracy (AIHDA) [Unpublished master's thesis]. Department of Clinical Sciences, Lund University (2019).
26. Salomonsson B. Interpreting the inner world of ADHD children: psychoanalytic perspectives. Int J Qual Stud Health Well-being. (2017) 12:1298269. doi: 10.1080/17482631.2017.1298269
27. Gerhardt S. Why Love Matters: How Affection Shapes a Baby's Brain. New York, NY: Routledge (2004).
28. Bielawski T, Misiak B, Moustafa A, Frydecka D. Epigenetic mechanisms, trauma, and psychopathology: targeting chromatic remodeling complexes. Rev Neurosci. (2019) 30:595–604. doi: 10.1515/revneuro-2018-0055
29. Storebø OJ, Gluud C, Winkel P, Simonsen E. Social-skills and parental training plus standard treatment vs. standard treatment for children with ADHD: the randomised SOSTRA trial. PLoS ONE. (2012) 7:e37280. doi: 10.1371/journal.pone.0037280
30. Murdock KW, Fagundes CP. Attachment orientations, respiratory sinus arrhythmia, and stress are important for understanding the link between childhood socio-economic status and adult self-reported health. Ann Hebav Med. (2017) 51:189–98. doi: 10.1007/s12160-016-9842-4
31. Brumariu LE. Parent–child attachment and emotion regulation. New Dir Child Adolesc Dev. (2015) 148:31–45. doi: 10.1002/cad.20098
32. Clarke L, Ungerer J, Chahoud K, Johnson S, Stiefel I. Attention deficit hyperactivity disorder is associated with attachment insecurity. Clin Child Psychol Psychiatry. (2002) 7:179–98. doi: 10.1177/1359104502007002006
33. Franc N, Maury M, Purper-Ouakil D. Trouble déficit de l'attention/hyperactivité (TDAH): quels liens avec l'attachement? [ADHD and attachment processes: are they related?]. L'Encéphale. (2009) 35:256–61. doi: 10.1016/j.encep.2008.04.007
34. Conrad P, Potter D. From hyperactive children to ADHD adults: observations of the expansion of medical categories. Soc Probl. (2000) 47:559–82. doi: 10.2307/3097135
35. Ainsworth MDSJ, Bowlby J. An ethological approach to personality development. Am Psychol. (1991) 46:331–41. doi: 10.1037/0003-066X.46.4.333
36. Russell G, Ford T, Rosenberg R, Kelly S. The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: alternative explanations and evidence. J Child Psychol Psychiatry. (2014) 55:436–45. doi: 10.1111/jcpp.12170
37. Cindy S, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. (2021) 19:120–9. doi: 10.1097/XEB.0000000000000282
38. Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. (35). Mixed Methods Appraisal Tool (MMAT). User guide. McGill. Department of Family Medicine, Canada (2018).
39. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
40. Al-Yagon M, Forte D, Avrahami L. Executive functions and attachment relationships in children with ADHD: links to externalizing/internalizing problems, social skills, and negative mood regulation. J Attent Disord. (2017) 24:1876–90. doi: 10.1177/1087054717730608
41. Al-Yagon M. Models of child-parent attachment in attention deficit hyperactivity disorder: links to executive functions. Pers Relatsh. (2018) 25:280–98. doi: 10.1111/pere.12232
42. Bourrat MM. Hyperexcitabilité, hyperactivité et traumatisme [Hyperexcitement, hyperactivity and traumatism]. Neuropsychiatrie de l'Enfance et de l'Adolescence. (2004) 52:210–8. doi: 10.1016/j.neurenf.2004.03.006
43. Dalaire S, Lafortune D. Trouble de déficit d'attention: facteurs génétiques et familiaux. Une rescension des écrits [Attention deficit disorder: genetic and familial factors An inventory of writings on the subject]. La psychiatrie de l'enfant. (2008) 51:275–312. doi: 10.3917/psye.511.0275
44. Duc Marwood A. Les contes en thérapie avec des enfants souffrant d'hyperactivité et de déficit de l'attention [Tales in therapies with children who have been diagnosed with ADHD]. Thérapie Familiale. (2020) 41:73–84. doi: 10.3917/tf.201.0073
45. Edel MA, Juckel G, Brüne M. Interaction of recalled parental ADHD symptoms and rearing behavior with current attachment and emotional dysfunction in adult offspring with ADHD. Psychiatry Res. (2010) 178:137–41. doi: 10.1016/j.psychres.2010.04.004
46. Eyuboglu M, Eyuboglu D. Emotional regulation and attachment style in previously untreated adolescents with attention deficit and hyperactivity disorder. Dusunen Adam J Psychiatry Neurol Sci. (2020) 33:228–36. doi: 10.14744/DAJPNS.2020.00086
47. Finzi-Dottan R, Manor I, Tyano S. ADHD, temperament, and parental style as predictors of the child's attachment patterns. Child Psychiatry Hum Dev. (2006) 37:103–114. doi: 10.1007/s10578-006-0024-7
48. Guinard, M. Le travail du pulsionnel et ses différentes figures chez des enfants dits ”TDAH” [The working through of drives and its different facets in children diagnosed with ”ADHD”]. La psychiatrie de l'Enfant. (2012) 55:97–224. doi: 10.3917/psye.551.0197
49. Hornstra R, Bosmans G, van den Hoofdakker BJ, Meyer D, van der Oord HS. Self-reported attachment styles in children with and without Attention-Deficit/Hyperactivity Disorder (ADHD). Euro Child Adolesc Psychiatry. (2019) 28:1277–80. doi: 10.1007/s00787-019-01288-7
50. Hurt EA, Hoza B, Pelham WE Jr. Parenting, family loneliness, and peer functioning in boys with attention-deficit/hyperactivity disorder. J Abnorm Child Psychol. (2007) 35:543–55. doi: 10.1007/s10802-007-9111-x
51. Latimer K, Wilson P, Kemp J, Thompson L, Sim F, Gillberg C, et al. Disruptive behaviour disorders: a systematic review of environmental antenatal and early years risk factors. Child Care Health Dev. (2012) 38:611–28. doi: 10.1111/j.1365-2214.2012.01366.x
52. Lemelin G, Lafortune D, Fortier I. Les caractéristiques familiales des enfants présentant un trouble déficitaire de l'attention avec ou sans hyperactivité: recension critique des écrits [Charactetistics of the families with children diagnosed with ADHD–a critical review of the literature]. Can Psychol. (2006) 47:211–28. doi: 10.1037/cp2006011
53. Maguire SA, Williams B, Naughton AM, Cowley LE, Tempest V, Mann MK, et al. A systematic review of the emotional, behavioural and cognitive features exhibited by school-aged children experiencing neglect or emotional abuse. Child Care Health Dev. (2015) 41:641–53. doi: 10.1111/cch.12227
54. Metz C, Thevenot A. Instabilité psychomotrice des enfants : trouble ou symptôme ? [Hyperactivity in children– disorder or symptom?] Psychologie Clinique. (2010) 30:34–48. doi: 10.1051/psyc/2010302034
55. Nahas N, Normandeau S, Lapointe JG. Liens entre les pratiques éducatives. le style d'attachement du parent et les comportements d'inattention et d'hyperactivité /impulsivité [Links between educational techniques, parents' attachment style and inattentive or hyperactive/compulsive behaviors]. La Psychiatrie de l'Enfant. (2017) 60:329–49. doi: 10.3917/psye.602.0329
56. Petot D. Pourquoi l'hyperactivité infantile évolue t-elle fréquemment vers le ”trouble oppositionnel avec provocation” [Why does attention-deficit/hyperacitivity disorder often turn into oppositional defiant disorder]? Neuropsychiatrie de l'Enfance et de l'Adolescence. (2004) 52:97–103. doi: 10.1016/j.neurenf.2003.11.001
57. Rasmussen PD, Storebø OJ, Shmueli-Goetz Y, Bojesen AB, Simonsen E, Bilenberg N, et al. Childhood ADHD and treatment outcome: the role of maternal functioning. Child and Adolesc Psychiatry Mental Health. (2018) 12:1–13. doi: 10.1186/s13034-018-0234-3
58. Rasmussen PD, Blienberg N, Kirubakaran R, Storebø OJ. Mapping factors facilitating resilience in mothers: potential clinical relevance for children with ADHD. Nordic J Psychiatry. (2020) 74:541–4. doi: 10.1080/08039488.2020.1748899
59. Scharf M, Oshri A, Eshkol V, Pilowsky T. Adolescents' ADHD symptoms and adjustment: the role of attachment and rejection sensitivity. Am J Orthopsychiatry. (2014) 84:209–17. doi: 10.1037/h0099391
60. Sempio OL, Fabio RA, Tiezzi P, Cedro C. Parental and teachers attachment in children at risk of ADHD and with ADHD. Life Span and Disability. (2016) 19:57–77.
61. Sochos A, Yahya F. Attachment style and relationship difficulties in parents of children with ADHD. J Child Fam Stud. (2015) 24:3711–22. doi: 10.1007/s10826-015-0179-6
62. Sourgen JL. La thérapie familiale psychanalytique a-t-elle sa place dans le traitement du TDAH? Un enfant au destin grandiose [Is there room for psychoanalytic family therapy in the approach to ADHD? Meeting a child with a great destiny]. Le divan Familiale. (2017) 39, 105–120. doi: 10.3917/difa.039.0105
63. Storebø OJ, Rasmussen PD, Simonsen E. Association between insecure attachment and ADHD: environmental mediating factors. J Atten Disord. (2016) 20:187–96. doi: 10.1177/1087054713501079
64. Özyurt G, Öztürk Y, Akay A. Relation of emotion regulation and empathy skills with maternal emotion regulation and attachment in children diagnosed with ADHD. Anadolu Psikiyatri Derg. (2017) 18:611–20. doi: 10.5455/apd.247800
65. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
66. Weissenberger S, Ptacek R, Klicperova-Baker M, Erman A, Schonova K, Raboch J, et al. ADHD, lifestyles and comorbidities: a call for a holistic perspective – from medical to societal intervening factors. Front Psychol. (2017) 8:454. doi: 10.3389/fpsyg.2017.00454
67. Johnston C, Behrenz K. Childrearing discussions in families of non-problem children and ADHD children with higher and lower levels of aggressive-defiant behavior. Can J School Psychol. (1993) 9:53–65. doi: 10.1177/082957358500900106
68. Danforth JS, Barkley RA, Stokes TF. Observation of parent-child interactions with hyperactive children: research and clinical implications. Clin Psychol Rev. (1991) 11:703–27. doi: 10.1016/0272-7358(91)90127-G
70. Johnston C, Williamson D, Noyes A, Stewart K, Weiss MD. Parent and child ADHD symptoms in relation to parental attitudes and parenting: testing the similarity-fit hypothesis. J Clin Child Adolesc Psychol. (2018) 47:127–36. doi: 10.1080/15374416.2016.1169538
71. Brinkmann S. Psychiatric diagnoses as semiotic mediators: the case of ADHD. Nordic Psychology. (2014) 66:121–34. doi: 10.1080/19012276.2014.926227
72. Nielsen, M. (2017). My ADHD and me: identifying with and distancing from ADHD. Nordic Psychol. 69:33–46. doi: 10.1080/19012276.2016.1267916
73. Gask L. In defence of the biopsychosocial model (Essay). Lancet Psychiatry. (2018) 5:548–9. doi: 10.1016./S2215.0366(18)30165-2
74. Dagens Medicin,. Ungdomar Vill Återkalla Sina Diagnoser. (2018). Available online at: https://www.dagensmedicin.se/specialistomraden/psykiatri/ungdomar-vill-aterkalla-sina-diagnoser/
75. Jernberg M. Fler vill slippa ADHD-diagnos. Psykologtidningen. Available online at: https://psykologtidningen.se/2021/04/29/fler-vill-slippa-adhd-diagnos/ (accessed April 29, 2021).
76. Timimi S. Non-diagnostic based approaches to helping children who could be labelled ADHD and their families. Int J Qual Stud Health and Well-Being. (2017) 12:1298270. doi: 10.1080/17482631.2017.1298270
77. Günter M. Attention deficit hyperactivity disorder (ADHD): an affect-processing and thought disorder? Int J Psychoanal. (2014) 95:43–66. doi: 10.1111/1745-8315.12081
78. Conway F, Lyon S, Silber M, Donath S. Cultivating compassion ADHD project: a mentalization informed psychodynamic approach. J Infant Child Adolesc Psychother. (2019) 18:212–22. doi: 10.1080/15289168.2019.1654271
Keywords: ADHD, overdiagnosis, attachment, family relations, social disadvantage, biopsychosocial
Citation: Erlandsson SI, Hornborg C, Sorbring E and Dauman N (2022) Is ADHD a way of conceptualizing long-term emotional stress and social disadvantage? Front. Public Health 10:966900. doi: 10.3389/fpubh.2022.966900
Received: 11 June 2022; Accepted: 10 October 2022;
Published: 03 November 2022.
Edited by:
Martin Whitely, Curtin University, AustraliaReviewed by:
Athanasios Koutsoklenis, Democritus University of Thrace, GreeceJuho Honkasilta, University of Helsinki, Finland
Copyright © 2022 Erlandsson, Hornborg, Sorbring and Dauman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Soly I. Erlandsson, c29seS5lcmxhbmRzc29uQGh2LnNl
 Soly I. Erlandsson
Soly I. Erlandsson Christoffer Hornborg
Christoffer Hornborg Emma Sorbring
Emma Sorbring Nicolas Dauman
Nicolas Dauman