- 1Mandura District Health Office, Beneshangul Gumuz, Asosa, Ethiopia
- 2School of Nursing and Midwifery, College of Health and Medical Science, Haramaya University, Harar, Ethiopia
- 3School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Maternal mortality from pregnancy and childbirth remains a major public health problem. Increasing access to institutional delivery is one of the key strategies to reduce childbirth-related maternal mortality. Despite all the efforts, institutional deliveries in Ethiopia remain low. Understanding factors associated with institutional delivery is important to devise strategies to improve facility based child birth. Hence, this study assessed the prevalence of institutional delivery and associated factors to bridge the gap.
Methods: A community-based cross-sectional study was employed from March-April 2020. Multi-stage sampling was employed to select 500 mothers who gave birth within the last 12 months in Mandura district, Benishangul Gumuz Region, Ethiopia. Data were collected using pre tested structured questionnaire through face-to-face interview. Logistic regression models were fitted to assess the predictors of institutional delivery. Adjusted Odds ratios with 95% CI was used to show associations and statistical significance was set at a p < 0.05.
Results: This study indicated that the prevalence of institutional delivery was 28.8% CI (25–33.3%). Having a positive attitude (AOR = 9.6,95%CI:2.5–35.9), attending antenatal care (ANC) at least once (AOR = 16.1,95%CI:9.6–22), attending ANC more than three times (AOR = 17.2, 95% CI:13.5–43.8), having good knowledge (AOR = 11.1, 95%CI: 2.7–45.4), and facing complications during pregnancy (AOR = 4.04, 95%CI: 1.0–16.0) were significantly associated with institutional delivery.
Conclusion: The prevalence of institutional delivery in this study was low. Positive attitude toward institutional delivery, attending ANC, having good knowledge about institutional delivery, and facing complications during pregnancy were identified predictors of institutional delivery. Strategies with a focus on increasing ANC uptake, improving mothers' knowledge, and promoting institutional delivery at the community level are critical.
Background
Maternal mortality from pregnancy and child birth remains a major public health problem globally. Approximately 295,000 women died in 2017; related to pregnancy and childbirth. The large number of these deaths (94%) happened in developing countries, and Sub-Saharan Africa alone accounted for roughly two-thirds (196,000) of maternal deaths (1, 2).
Averting maternal death remains the priority agenda of Sustainable Development Goal (SDG-3) with the plan to reduce maternal mortality ratio (MMR) to global target of 70 per 100,000 livebirths or less by 2030. However, maternal mortality worldwide dropped by 38% between 2000 and 2017; with this progress, the SDG-3 will not be achieved at the expense of millions of lives (1, 3).
Globally more than three fourth of maternal deaths are due to direct obstetric complications which includes hemorrhage, infection, complication of unsafe abortion, pregnancy induced hypertension and obstructed labor. Post-partum hemorrhage alone accounts for 25% of maternal death with the vast majority occurring within 24 h after delivery (4, 5). Most of these deaths could have been averted if the women have received basic maternal health care from skilled care provider.
Increasing access to institutional delivery is one key approach to reduce maternal deaths related to childbirths in developing countries, such as Ethiopia. Institutional delivery warrants safe childbirth, reduce post-partum complications, enhance survival ‘of mothers and newborns. It is predicted that delivery at health facilities could decrease 16–33% of maternal death (4, 6).
Ethiopia is one of the big contributors of global maternal death among 10 countries that comprised 58% of maternal deaths following India, Nigeria, and Democratic Republic of Congo (7). The Ethiopian demographic health survey report indicated that maternal mortality rate dropped by 39% from 676 in 2011 to 412 per 100,000 live births in 2016 (8, 9). More ever, the proportion of skilled birth attendance have been increased from 28 % in 2016 to 48% in 2019 and still majority of the women are giving birth at home without any skilled professional assistance (9, 10).
Studies showed that numerous factors affect institutional delivery services. Socioeconomic/demographic factors, health facility factors, obstetric factors, maternal preference of birth places, knowledge about the benefits of institutional delivery, knowledge about pregnancy danger signs, pregnancy plan, family size, birth preparedness and complication readiness are some factors influencing delivery service utilization (11–13).
To achieve the target of SDGs, Ethiopian government has developed various interventions to improve access to maternal health services. For instance, deployment of health extension workers (HEWs) working in the rural set up across all regions of the country to provide basic maternal health services (14). In addition, federal ministry of health (FMOH) put a national goal to scale up facility-based childbirth to 70% by 2025 (15). Despite all these efforts, institutional deliveries remain low.
Although institutional delivery has been widely investigated in Ethiopia, most of the studies relied on the data from national/regional surveys whereas studies on predictors of institutional delivery in the particular study area were limited. Understanding factors associated with institutional delivery in particular set up is important to devise strategies to improve facility based child birth in the study area. Thus, this study assessed prevalence and associated factors of institutional delivery among mothers who gave birth in Mandura district, Benishangul Gumuz Region, Ethiopia.
Methods and material
Study design, setting and period
A community based cross-sectional study was carried out among women who gave birth in Mandura district.
Mandura is one of the districts or woredas found in the Metekel Zone of Benishangul-Gumuz Region in Ethiopia; located 546 KM from Addis Ababa. According to 2007 national survey this woreda had a total population of 40,746, of whom 21,241 were men and 19,505 were women; 45% (8776) were reproductive age groups. The district had 3 urban and 17 rural kebeles (small administrative units in the district) (16). The study was conducted from March-April 2020.
Source and study population
All reproductive age group women residing in Mandura district were the source population where as those women who gave birth within the last 12 months in the selected kebeles of the study area were study population. Critically ill mothers who were unable to respond were excluded from the study.
Sample size determination and sampling technique
The sample size was determined using single population formula; n = (Zα/2)2 × P (1 - p)/d2 with the following assumptions: The proportion of institutional delivery P = 18% (17), degree of precision (d) = 0.05, 95% confidence interval, and design effect of 2. Considering 10% non-response rate, the final sample size was 500. Multi-stage sampling technique was used to select nine kebeles (three urban kebeles and six rural kebeles) in the district. The kebeles were selected by lottery method. Proportional allocation was made to give equal chance for each kebele. All eligible households from each kebele were selected by systematic random sampling. The list of households was obtained from the health post (health extension workers). If more than one eligible woman were in the selected household, only one of them was interviewed.
Data collection instrument and procedures
Data were collected using a structured questionnaire through face-to-face interview. The questionnaire was prepared by reviewing various literatures (17–24). The questionnaire contains socio-demographic characteristics, health facility/service-related factors, obstetric characteristics and participants' knowledge and attitude toward institutional delivery. Four health extension workers and two Bsc midwives were recruited for data collection and supervision. A two-day training was given for data collectors and supervisors on the contents of the tools and aim of the study. The pretest was conducted on 5% of the sample (25 participants) outside the study area. Some modifications and adjustments were made to questions based on lessons obtained during the pretest. The collected data was checked daily by supervisors and principal investigators for its completeness and consistency.
Operational definitions
Institutional delivery
Refers to if the woman gave birth at were minimal facilities and skilled professionals to diagnose, manage or refer obstetric complications are available (13, 18).
Knowledge about institutional delivery
The woman was categorized as having good knowledge if she scored 50% and above for knowledge questions, otherwise poor knowledge (13, 18).
Attitude toward institutional delivery
The women was considered as having positive attitude toward institutional delivery, if she scored 50% and above on attitude questions and negative attitude if not (18).
Data processing and analysis
Data were entered into computer, cleaned and coded using Epi-Data 3.1, then exported to SPSS version 22 for analysis. Descriptive statistics were computed to determine the frequencies and means. Model fitness was checked using Hosmer and Lemeshow's test for goodness of fit. Binary logistic regression analysis was performed to identify predictors of institutional delivery. Variables with p < 0.25 in bivariable analysis were retained into multivariable logistic regression model and adjusted odds ratio with 95% confidence interval was used to measure strength of association. Statistical significance was set at p < 0.05.
Ethical consideration
The ethical approval for the study was sought from Institutional Health Research Review Committee of Haramaya University, College of health and medical science. Voluntary, written and signed consent was obtained from study participants, from a parent and/or legal guardian for the participants under 18, and from legally authorized representatives for illiterate participants. Confidentiality was maintained and all basic rights of participants were respected.
Results
Socio-demographic characteristics of study participants
A total of 500 women participated in the study, with 100% response rate. The mean age of study participants was 28.85(SD ± 5.79). Majority (93.8%) of the respondents were married and from rural 377 (75.4%). The highest proportion 366 (73.2%) of study participants were illiterate (Table 1).
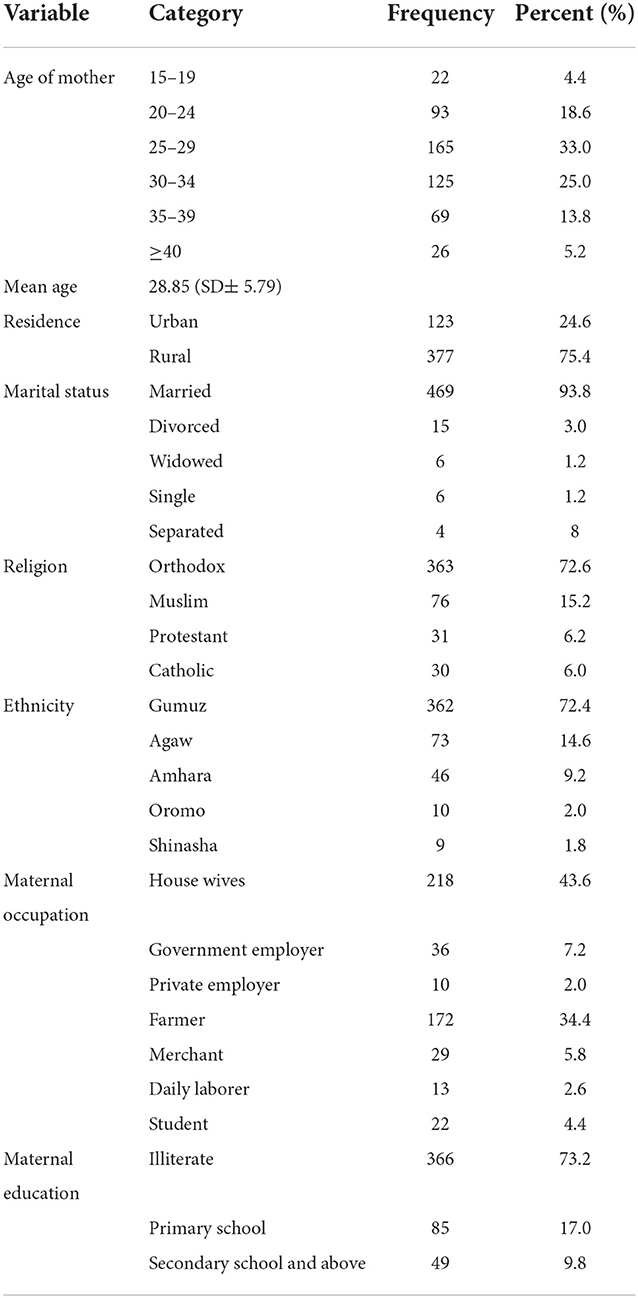
Table 1. Socio-demographic characteristics of women who gave birth in the past 12 months in Mandura district, Benishangul Gumuz region, Ethiopia, 2020 (n = 500).
Obstetric characteristics of the respondents
More than one third 176 (35.2%) of study participants attended ANC for their current pregnancy and 139(27.8%) of participants reported that their current pregnancy was planned. More than half 291(58.2%) of women had poor knowledge about institutional delivery, whereas 365(73%) of them had negative attitude toward institutional delivery (Table 2).
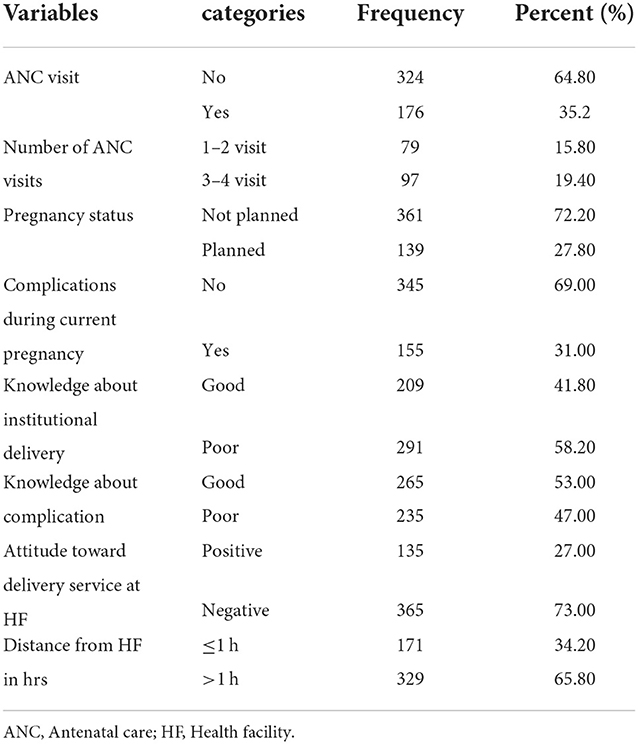
Table 2. Obstetric conditions of women who gave birth in the past 12-months in Mandura district, Benishangul Gumuz region, Ethiopia, 2020 (n = 500).
Institutional delivery among study participants
The prevalence of institutional delivery in this study was 28.8% (95% CI: 25, 33.2%) (Figure 1).
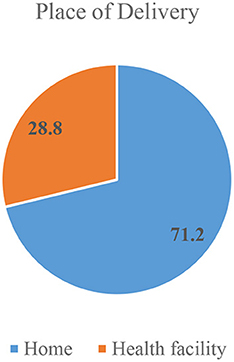
Figure 1. Place of delivery among women who gave birth in the past 12 months in Mandura district, Benishangul Gumuz, Ethiopia, 2020 (n = 500).
With regard to place of delivery a significant number of participants 356(71.2%) delivered at home. The major reported reasons for home delivery were: feel more comfortable at home (32%), good family care at home (40.6%), previous usual practice (25%) and others (2.4%) %) (Figure 2).
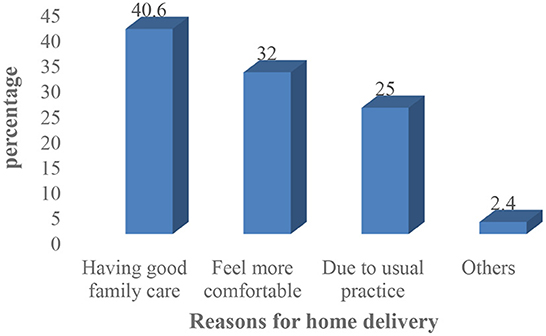
Figure 2. Reasons for home delivery in Mandura district, Benishangul Gumuz, Ethiopia, 2020 (n = 356).
Predictors of institutional delivery
The multi-variable analysis showed that complications faced during pregnancy, knowledge about institutional delivery, attitude toward institutional delivery and antenatal care visit were strong predictors of institutional delivery. Women who faced complications during current pregnancy were 4.04 times more likely to give birth at health facility compared to their counterparts (AOR = 4.04, 95% CI:1.02–16.04, P = 0.04). Mothers with at least one ANC visit during the recent pregnancy were 16.1 times more likely to give birth at health facility compared to those who had no ANC follow up (AOR = 16.1, 95% CI:9.6–22, P = 0.001). The odds of institutional delivery were 11.1 times higher among mothers who had good knowledge compared to those who had poor knowledge (AOR = 11.1, 95% CI: 2.7–45.4, P = 0.001). The odds of institutional delivery were 9.6 times higher among mothers with positive attitude than mothers who had negative attitude toward child birth at HF (AOR = 9.6, 95% CI: 2.5–35.9, P = 0.001) (Table 3).
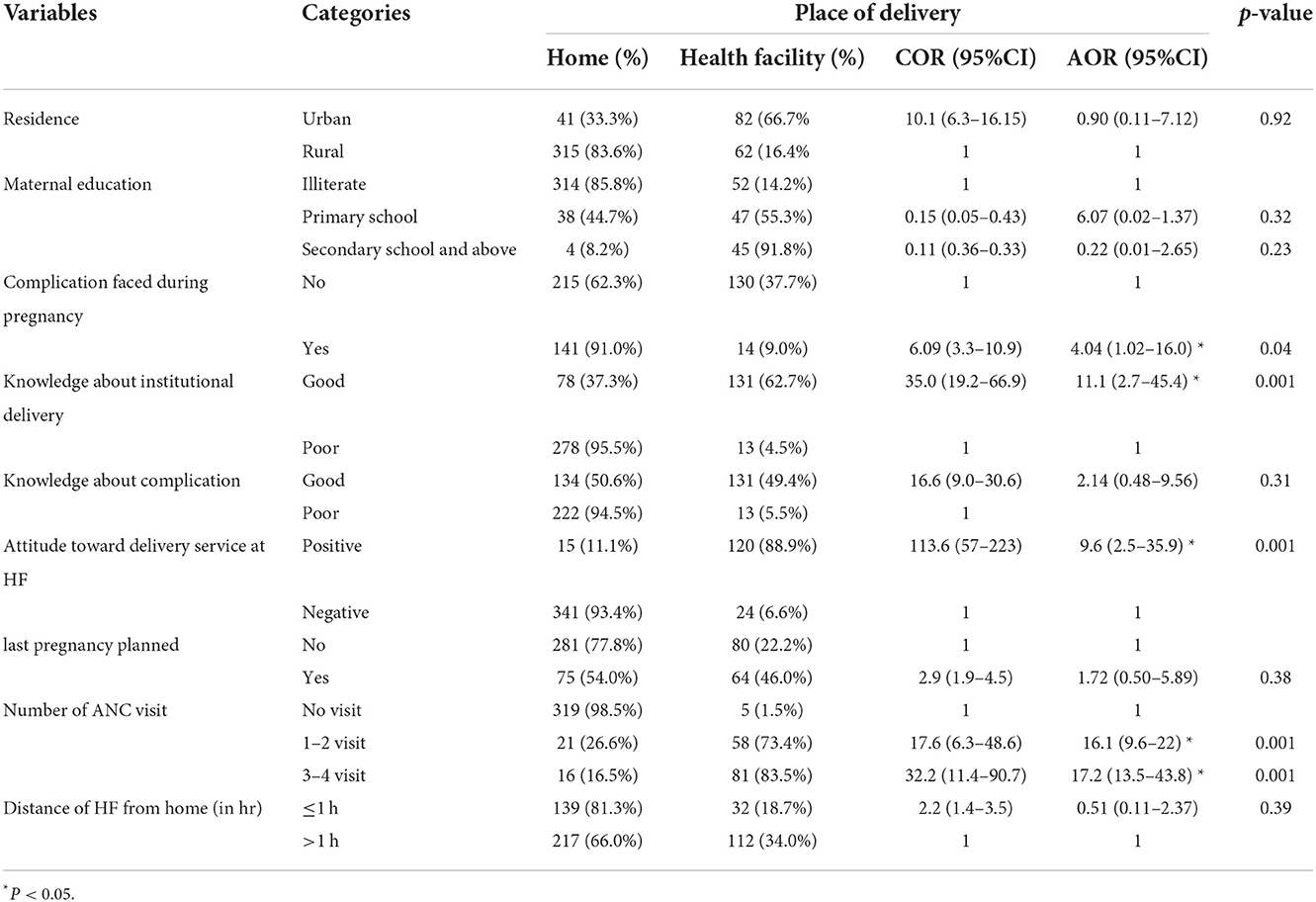
Table 3. Factors associated with institutional delivery among mothers who gave birth in the past 12 months in Mandura district, Benishangul Gumuz, Ethiopia, 2020 (n = 500).
Discussion
This study assessed institutional delivery and associated factors among women who gave birth in Mandura District of Benishangul gumuz, Ethiopia. The study revealed the prevalence of institutional delivery was 28.8% (95% CI: 25–33.3%). Good knowledge about institutional delivery, positive attitude toward institutional delivery, complication faced during pregnancy, and having ANC follow up were found to be significant predictors of institutional delivery.
The prevalence of institutional delivery in this study is consistent with that of a study done in Cheha district, Gurage zone, SNNPR (31%), systematic review report from Ethiopia (31%) and other national study in Ethiopia (26.2%) (19–21). But it is higher than studies conducted in Liban District (13.9%), Guji Zone, Oromia, Southern Ethiopia (22), Dangla (18.3%), Northern Ethiopia (23), and Awi zone (18.8%), North West Ethiopia (24). The difference might be due to the length of time interval between the studies. At present there is improved exposure to health education and increased access to maternal health care services with the involvement of health extension workers.
However, this study finding was lower compared to Ethiopian Demographic Health Survey report (EDHS, 2019) which was 48% (10), studies conducted at Arbaminch Town, southern Ethiopia 73.2% (25), Woldia Town, Ethiopia 74.7% (26) and Bench maji Zone, South West Ethiopia 78.30% (27). The difference might be explained by sample size difference, sociodemographic variation, study setting and accessibility of the service.
This study revealed that women who faced complications during current pregnancy were 4 times (AOR = 4.04, 95% CI:1.02–16.04) more likely to had institutional delivery compared to those women who did not faced complications. This finding is in agreement with other studies conducted in Ayssaita District, North East Ethiopia (28), and Benchi Maji, Southwest Ethiopia (27). This imply that those mothers who recognized the problem during pregnancy could have greater fear of the possible adverse birth outcomes. Therefore, they would be encouraged and motivated to deliver at health facility.
This study revealed that ANC visits was strong predictor of institutional delivery. Mothers with at least one ANC visit during the recent pregnancy were 16 times (AOR = 16.1, 95% CI:9.6–22) more likely to give birth at health facility compared to those who had no ANC follow up. This finding agreed with different studies conducted in Nepal, Tanzania and Ethiopia (29–34). This might be because the women would be counseled about complication readiness and birth preparedness during their ANC follow up which will encourage the women to deliver at health facility.
The odds of institutional delivery were 11 times (AOR = 11.1, 95% CI: 2.7–45.4) higher among mothers who had good knowledge compared to those who had poor knowledge. This finding was congruent with other studies in Ethiopia and some developing countries (29, 30, 32, 35). This might be because women with good knowledge about institutional delivery would know the benefits of institutional delivery and can predict the possible consequences of childbirth; Hence, they are more likely to give birth at the health facilities.
Women's attitude toward childbirth at health facility was another important predictor which affects institutional delivery service utilization. Women with positive attitude were 9.6 time (AOR = 9.6, 95% CI: 2.5–35.9) more likely to give birth at health facility compared to those with negative attitudes. The finding is similar with other studies conducted in Afar, Northeast Ethiopia, in Bench Maji zone, South West Ethiopia, and evidence from meta-analysis in Ethiopia (19, 27, 36). This can be justified as attitude is the most important aspect which affects the health care seeking habits of the women.
Finally, as limitation of this study recall bias may be introduced because the women were asked information about their exposure and delivery status retrospectively. Furthermore, since the study was cross sectional, it was not possible to establish the temporal relationship of variables.
Conclusion
The magnitude of institutional delivery in the study area was low. Positive attitude toward institutional delivery, attending ANC, having good knowledge about institutional delivery, and facing a problem during pregnancy were strong predictors of facility-based childbirth. Community mobilization and health education on maternal health service is needed to increase uptake of antenatal care, ensure women's knowledge toward institutional delivery and promote benefits of institutional delivery to increase the number of institutional deliveries.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Health Research Review Committee of Haramaya University, College of health and medical science. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TA is the primary author who initiated the study. IM and MD involved in the study design, supervision, and analysis. TM and AA drafted the manuscript. All authors have conceived, critically revised, read, and approved the final manuscript.
Funding
Haramaya University provided technical support for this study.
Acknowledgments
We gratefully acknowledge the study participants, data collectors, supervisors, facility administrators and staff for their willingness and cooperation to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Maternal Mortality: Evidence Brief . World Health Organization (2019). Available online at: https://apps.who.int/iris/bitstream/handle/10665/329886/WHO-RHR-19.20-eng.pdf
2. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2019). Available online at: https://apps.who.int/iris/handle/10665/327596
3. United Nations. Transforming our world: the 2030 agenda for sustainable development. Division for Sustainable Development Goals. New York, NY: World Health Organization (2015). Available online at: https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf
4. Ronsmans C, Graham WJ. Maternal mortality: who, when, where and why. Lancet. (2016) 368:1189–200. doi: 10.1016/S0140-6736(06)69380-X
5. Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. (2005) 365:977–88. doi: 10.1016/S0140-6736(05)71088-6
6. Graham WJ, Bell JS, Bullough CHW. Can skilled attendance at delivery reduce maternal mortality in developing countries? In: De Brouwere V, Van Lerberghe W, ediors. Safe Motherhood Strategies: A Review of the Evidence. Studies in Health Services Organisation and Policy (2001).
7. WHO UNICEF UNFPA World Bank United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva: WHO (2014). Available online at: https://apps.who.int/iris/bitstream/10665/112697/1/WHO_RHR_14.13_eng.pdf
8. Central Statistical Agency [Ethiopia], ICF, International,. Ethiopia Demographic Health Survey 2011. Addis Ababa, Ethiopia Calverton, Maryland, USA: Central Statistical Agency ICF International (2012). Available online at: https://dhsprogram.com/pubs/pdf/fr255/fr255.pdf
9. Central Statistical Agency(CSA) ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF. (2016). Available online at: https://www.usaid.gov/sites/default/files/documents/1860/Ethiopia%20DHS%202016%20KIR%20-%20Final%2010-17-2016.pdf
10. EPHI (Ethiopian public health institute). Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, Maryland, USA: EPHI and ICF (2019). Available online at: https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf
11. Andargie AA, Abebe M. Factors associated with utilization of institutional delivery care and postnatal care services in Ethiopia. J Public Health Epidemiol. (2018) 10:108–22. doi: 10.5897/JPHE2017.0989
12. Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia : analysis of the. EDHS. (2011) 2014:1–13. doi: 10.1186/1471-2393-14-161
13. Mitikie KA, Wassie GT, Beyene MB. Institutional delivery services utilization and associated factors among mothers who gave birth in the last year in Mandura district, Northwest Ethiopia. PLoS ONE. (2020) 15:e0243466. doi: 10.1371/journal.pone.0243466
14. Ministry of Health. Essential Health Services Package of Ethiopia. Addis Ababa (2019). Available online at: https://www.uib.no/sites/w3.uib.no/files/attachments/essential_health_service_package_ethiopia_2019_0.pdf
15. FMOH. Health Sector Transformation Plan II (HSTP II) 2020/21–2024/25 (2013 EFY-2017 EFY) Ministry of Health-Ethiopia (2021). Available online at: http://repository.iifphc.org/handle/123456789/1414
16. Agency CS,. 2007 Population Housing Census of Ethiopia. Central Statistical Agency Addis Ababa, Ethiopia (2007). Available online at: https://rise.esmap.org/data/files/library/ethiopia/Documents/Clean%20Cooking/Ethiopia_Census%202007.pdf
17. Ahmed M, Demissie M, Medhanyie AA, Worku A, Berhane Y. Utilization of institutional delivery Service in a Predominantly Pastoralist Community of Northeast Ethiopia. Ethiop J Health Sci. (2018) 28:403–12. doi: 10.4314/ejhs.v28i4.6
18. Mohammed MJ, Mohammed YE, Reddy PS. Institutional delivery service utilization and associated factors among mothers in Afambo District, Afar, Ethiopia-2016. Community based cross sectional study. Med Res Chron. (2017) 4:363–79.
19. Nigusie A, Azale T, Yitayal M. Institutional delivery service utilization and associated factors in Ethiopia: a systematic review and META-analysis. BMC Pregnancy Childbirth. (2020) 20:1–25. doi: 10.1186/s12884-020-03032-5
20. Ketemaw A, Tareke M, Dellie E, Sitotaw G, Deressa Y, Tadesse G, et al. Factors associated with institutional delivery in Ethiopia: a cross sectional study. BMC Health Serv Res. (2020) 20:1–6. doi: 10.1186/s12913-020-05096-7
21. Habte F, Demissie M. Magnitude and factors associated with institutional delivery service utilization among childbearing mothers in Cheha district, Gurage zone, SNNPR, Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. (2015) 15:1–12. doi: 10.1186/s12884-015-0716-8
22. Wako WG, Kassa DH. Institutional delivery service utilization and associated factors among women of reproductive age in the mobile pastoral community of the Liban District in Guji Zone, Oromia, Southern Ethiopia: a cross sectional study. BMC Pregnancy Childbirth. (2017) 17:1–10. doi: 10.1186/s12884-017-1325-5
23. Demilew YM, Gebregergs GB, Negusie AA. Factors associated with institutional delivery in Dangila district, North West Ethiopia: a cross-sectional study. Afr Health Sci. (2016) 16:10–7. doi: 10.4314/ahs.v16i1.2
24. Alemayehu M, Mekonnen W. The prevalence of skilled birth attendant utilization and its correlates in North West Ethiopia. BioMed Res Int. (2015) 2015:436938. doi: 10.1155/2015/436938
25. Kelebore WG, Asefa A, Tunje A, Shibiru S, Hassen S, Getahun D, et al. Assessment of factors affecting institutional delivery service utilization among mother who gave birth in last two years, Arbaminch town, Gamo Gofa zone, Snnpr, Ethiopia. Sci J Public Health. (2016) 4:458. doi: 10.11648/j.sjph.20160406.17
26. Gedefaw G, Abebe E, Nigatu R, Mesfin B, Addisu A. Institutional delivery service utilization and its factors influencing among mothers who gave birth in Woldia Town, Ethiopia. A Community-Based Cross-Sectional Study. Gynecol Obstet (Sunnyvale). (2018) 8:484. doi: 10.4172/2161-0932.1000484
27. Tadele N, Lamaro T. Utilization of institutional delivery service and associated factors in Bench Maji zone, Southwest Ethiopia: community based, cross sectional study. BMC Health Serv Res. (2017) 17:1–10. doi: 10.1186/s12913-017-2057-y
28. Yilma F, Olgira L, Mengiste B, Surender Reddy P, Gebre A. Magnitude and associated factors for institutional delivery service among women who gave birth in the last 12 months in ayssaita district, north east ethiopia: a community based cross sectional study-2015. Med Res Chron. (2018) 5:202–23. Available online at: https://medrech.com/index.php/medrech/article/view/306
29. Bhaskar RK, Deo KK. Determinants of utilization of institutional delivery services in East Nepal: a community-based cross-sectional study. J Natl Med Coll. (2018) 3:6–15. doi: 10.3126/medphoenix.v3i1.20755
30. Bishanga DR, Drake M, Kim YM, Mwanamsangu AH, Makuwani AM, Zoungrana J, et al. Factors associated with institutional delivery: findings from a cross-sectional study in Mara and Kagera regions in Tanzania. PLoS ONE. (2018) 13:e0209672. doi: 10.1371/journal.pone.0209672
31. Amentie M, Abera M, Abdulahi M. Utilization of institutional delivery care services and influencing factors among women of child bearing age in Assosa District, Benishangul Gumuz Regional State, West Ethiopia. Glob J Med Res. (2016). 16:3. doi: 10.11648/j.sjcm.20150403.11
32. Eshete T, Legesse M, Ayana M. Utilization of institutional delivery and associated factors among mothers in rural community of Pawe Woreda northwest Ethiopia, 2018. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4450-6
33. Anteneh KT, Gebreslasie KZ, Nigusie TS, Aynalem GL, Yirdaw BW. Utilization pattern of institutional delivery among mothers in North-western Ethiopia and the factors associated; A community -based study. Clin Epidemiol Glob Health. (2021) 10:100675. doi: 10.1016/j.cegh.2020.100675
34. Gashaye A, Kibret GD, Bazezew Y, Mengist B. Factors affecting institutional delivery in Ethiopia: a multi-level analysis. Int J Afr Nurs Sci. (2021) 15:100331. doi: 10.1016/j.ijans.2021.100331
35. Yaya S, Bishwajit G, Ekholuenetale M. Factors associated with the utilization of institutional delivery services in Bangladesh. PLoS ONE. (2017) 12:e0171573. doi: 10.1371/journal.pone.0171573
Keywords: predictors, institutional delivery, Mandura, Benishangul Gumuz, Ethiopia
Citation: Arega T, Mulatu T, Alemayehu A, Mussa I and Dheresa M (2022) Institutional delivery and associated factors among women who gave birth in Benishangul Gumuz region, South West Ethiopia. Front. Public Health 10:965524. doi: 10.3389/fpubh.2022.965524
Received: 09 June 2022; Accepted: 23 November 2022;
Published: 09 December 2022.
Edited by:
Sunjoo Kang, Yonsei University, South KoreaReviewed by:
Vasuki Rajaguru, Yonsei University Health System, South KoreaTrang Thi Thuy Ho, Hue University of Medicine and Pharmacy, Vietnam
Copyright © 2022 Arega, Mulatu, Alemayehu, Mussa and Dheresa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Teshale Mulatu, d295ZXNhZ0BnbWFpbC5jb20=
 Temesgen Arega1
Temesgen Arega1 Teshale Mulatu
Teshale Mulatu Afework Alemayehu
Afework Alemayehu Ibsa Mussa
Ibsa Mussa Merga Dheresa
Merga Dheresa