- 1The Children's Hospital, Zhejiang University School of Medicine, National Clinical Research Centre for Child Health, Hangzhou, China
- 2School of Public Health, Shanghai Medical College, Fudan University, Shanghai, China
- 3Department of Philosophy, Beijing Normal University, Beijing, China
Background: Chinese pediatricians are facing challenges, and there is a need to examine the issue of negative emotions, namely, stress, anxiety and depression, among front-line pediatric residents in clinical settings. Understanding the current situation and influencing factors of negative emotions among pediatric residents in China and exploring the formation mechanism can lay a foundation for psychological interventions.
Methods: A total of 138 pediatric residents in the Children's Hospital, Zhejiang University School of Medicine, China, were surveyed using the Depression Anxiety Stress Scale-21 (DASS-21), Social Support Rating Scale (SSRS), Connor-Davidson Resilience Scale (CD-RISC), and Maslach Burnout Inventory-General Survey (MBI-GS).
Results: (1) The incidence of abnormal stress, anxiety, and depression among pediatric residents was 18.8%, 47.8%, and 47.8% respectively. (2) Negative emotions were significantly negatively correlated with social supports and psychological resilience, and positively correlated with burnout. (3) The chain-mediating effect of resilience and burnout between social supports and negative emotions was significant.
Conclusion: Psychological resilience and burnout played a chain-mediating role between social supports and negative emotions. Measures should be taken to improve the mental health of Chinese pediatric residents.
1. Introduction
In recent years, pediatricians in China have been confronted with a crisis with regards to long working hours, the frequency of medical disputes, and a shortage of pediatricians, which has caused widespread concern among the public. Despite intense workloads and high levels of risk, they earn less income than other senior healthcare providers (1, 2). The turnover rate of pediatricians in China is as high as 12.6%, and largely includes young doctors (3). In China, the standardized training system for residents has been established in recent years. All clinicians, including pediatricians, should undergo a 3-year residency training after graduating from medical school. During these 3 years, residents will study in different departments of the training base in turn. Pediatric residents work on the front line in healthcare settings, have direct interaction with children and their families, and are close to graduating from medical school and embarking on their careers in clinical practice. It is necessary to pay attention to their negative emotions caused by above crisis, because addressing negative emotions is not only the key to improving quality of life (4), but also patient safety (5). Anxiety and depression are the most common negative emotions in the general population (6). Anxiety and depression are usually external manifestations of stress (7). Therefore, we proposed the following hypotheses and verified the mechanisms.
Social supports describe the actual or perceived material, emotional and spiritual supports that an individual can access in their external world (8). The social support buffering hypothesis holds that social supports can mitigate the negative impact of stress on mental health (9). Lower levels of social support have been found to be associated with more mental health issues (10, 11), and individuals with less social support are about five times more likely to experience symptoms of anxiety and depression than those that have greater social supports (12). People with low levels of social support are at a higher risk of psychological stress, while higher levels of social support can help to alleviate anxiety and depression (13–15). Accordingly, the first hypothesis (H1) is proposed: social support can predict negative emotions among pediatric residents.
Psychological resilience is the ability to flexibly deal with challenges and overcome adversity, and it is accompanied by personal growth and transformation (16, 17). Some studies have pointed out that there is a significant positive correlation between social support and psychological resilience (18, 19), and people who receive more social support tend to have a higher level of psychological resilience. Psychological resilience can negatively predict anxiety (20) and alleviate depressive symptoms (21). High levels of resilience are associated with optimism and tenacity (22). Thus, the second hypothesis (H2) is proposed: among pediatric residents, social support could influence negative emotions through the mediating effect of psychological resilience.
Burnout is a psychological condition or a response to chronic emotional and interpersonal stressors on the job (23), and burnout among pediatricians may pose a danger to both doctors and patients (24). Negative emotions are closely related to job burnout (25, 26). Previous study has shown that social support has a negative predictive effect on job burnout among nurses (27). Support from leaders and colleagues could alleviate burnout and contribute to lower turnover intentions (28). Studies in different environments (29) and in different populations (30) seem to have found that social support may have a positive effect on burnout. Accordingly, the third hypothesis (H3) is proposed: among pediatric residents, social support can influence negative emotions through the mediating effect of burnout.
High psychological resilience often enables individuals to cope more effectively with their work environment, improve their work involvement and alleviate symptoms of burnout (31). Resilience can be regarded as the other side of the burnout coin (32) and could protect people from workplace stress (33). Researchers who have examined the relationship between resilience and burnout among nurses (34, 35) have shown that these two factors are negatively correlated, suggesting that higher levels of resilience might protect nurses from emotional exhaustion and contribute to personal accomplishment. Combining the relationship between resilience and social support, and the relationship between burnout and negative emotions, the fourth hypothesis (H4) is put forward: among pediatric residents, social support can affect negative emotions through the chain-mediating effect of resilience and burnout.
By verifying the above hypotheses, it would help exploring the psychological intervention for Chinese pediatric residents to improve their mental health, and reduce the turnover rate of pediatric professionals.
2. Methods
2.1. Investigation site and participants
The study was conducted at the Children's Hospital, Zhejiang University School of Medicine, Zhejiang Province, Eastern China in January 2022. A total of 138 pediatric residents participated in the investigation. This study was approved by the Ethics Committee of the children's hospital, Zhejiang University school of medicine (No. 2022-IRB-107).
2.2. Questionnaire tool
2.2.1. Socio-demographic information
The socio-demographic information questionnaire covered information related to gender, age, working years, education level, annual income, category, qualification, and clinical practice area.
2.2.2. Depression Anxiety Stress Scale-21
The Depression Anxiety Stress Scale-21 (DASS-21) is used to measure an individual's negative mood and the severity of symptoms in the previous week (36). The scale includes three subscales of anxiety, depression, and stress. Each subscale contains seven items, and a total of 21 items. Four grades ranging from 0 to 3 were used: “completely inconsistent,” “partially consistent,” “mostly consistent,” and “completely consistent.” Higher scores indicated more intense negative emotions. Each subscale is divided into asymptomatic, mild, moderate, severe, and extremely severe according to the score. In this study, the overall Cronbach's (37) alpha value was 0.956, and the Cronbach's alpha coefficients of each subscale were 0.880, 0.879, and 0.892, respectively.
2.2.3. Social Support Rating Scale
The Social Support Rating Scale (SSRS) (38) compiled by Chinese scholar Shuiyuan Xiao consists of ten items and three dimensions: objective social support (four items), subjective social support (four items), and utilization of social support (three items). Items 1–5 and 8–10 were scored on a four-point Likert scale, ranging from 1 (“not at all”) to 4 (“very much”). For items 6 and 7, the response “no source” was assigned 0 points and the response “have a source” was assigned 1 point for each source. Overall, higher scores indicated higher levels of personal social support. A total score of <20 signifies less social support, a total score of 20–30 signifies general social support, and a total score of more than 30 signifies satisfactory social support. In this study, the scale's Cronbach's alpha value was 0.940.
2.2.4. Connor-Davidson Resilience Scale
The Connor-Davidson Resilience Scale (CD-RISC), developed by Connor and Davidson (17), consists of 25 items that were assessed using a five-point Likert scale ranging from 0 to 4: incorrect, rarely correct, sometimes correct, usually correct, and correct. Higher scores indicated higher levels of resilience (39). The questionnaire was divided into three dimensions: tenacity, strength and optimism (40). In this study, the CD-RISC overall Cronbach's alpha value was 0.962.
2.2.5. Maslach Burnout Inventory-General Survey
We adopt the revised Chinese version of Maslach Burnout Inventory-General Survey (MBI-GS) (41, 42). The MBI-GS (Chinese version) consists of three subscales: emotional exhaustion (five items), cynicism (four items) and reduced personal accomplishment (six items). The scale was evaluated using a seven-point Likert scoring method, with scores from 0 to 6 indicating the frequency of their own feelings. For emotional exhaustion and cynicism, higher scores were associated with high levels of burnout. In the case of reduced personal accomplishment, higher scores indicated lower levels of burnout. The total Cronbach's alpha value of the burnout scale was 0.846, and the Cronbach's alpha values of the three subscales were 0.949, 0.945, and 0.937, respectively.
2.3. Statistical analysis
SPSS version 26.0 (IBM SPSS Statistics, USA) was used for data sorting and analysis. The measurement data are expressed as means ± standard deviations. For the basic situation of the data, a chi-square test was performed to assess the balance of grouping. If the data of both groups were normally distributed, a t-test was carried out for inter-group comparison; otherwise, the Mann-Whitney test was applied. For more than two groups, if the data satisfied a normal distribution and the variance was homogeneous, a one-way analysis of variance (ANOVA) was performed for inter-group comparison, and the least significant difference procedure was carried out for post-hoc comparison; otherwise, the data were analyzed by the Kruskal-Wallis test. The Spearman rank correlation method was used to analyze the correlation between social support, psychological resilience, burnout, stress, anxiety and depression. SPSS 26.0 (IBM SPSS Statistics, USA) software and its process program were used to analyze the intermediary effect, and the bootstrap method with deviation correction was used to test the regression coefficient to obtain the 95% deviation-corrected confidence interval. The confidence interval did not contain zero, indicating that the effect was statistically significant. For the homogeneity of variance test, the test level was 0.10, whereas the test level of the others were set at 0.05; that is, p < 0.05 indicated a statistically significant difference.
3. Results
3.1. Common method bias test
Exploratory factor analysis was performed on all items of the four scales using Harman's one-factor test for common method bias (43). The results showed that the explanation rate of the first principal component variation extracted by unrotated factors was 28.20%, which was less than the critical value standard of 40% (44), and there were 16 factors with eigenvalues >1. It was inferred that homologous variance was not the main reason for the co-variation among the variables. The synthetic reliability, the Omega coefficient, was also calculated (45, 46). The Omega coefficient used in this questionnaire was above 0.834, which performed well, and further data analysis was carried out.
3.2. General characteristics of the study sample
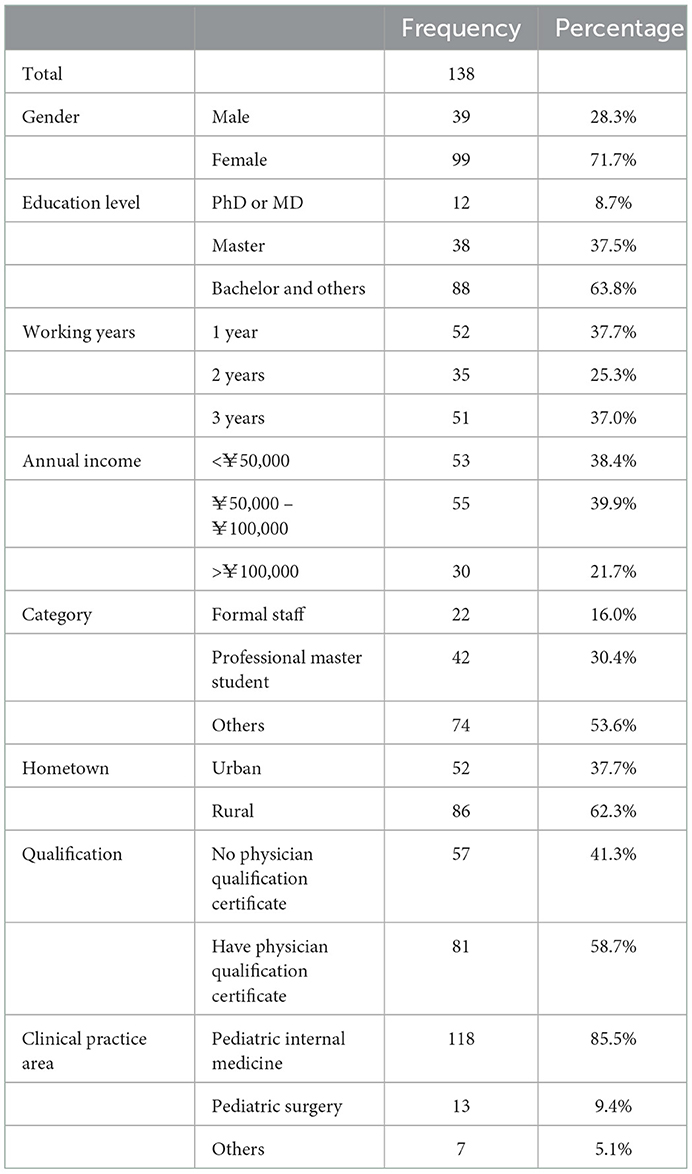
A total of 138 pediatric residents were included in the data analysis, of which the oldest was 36 years old and the youngest 22 years old. The average age was (26.25 ± 2.61) years old. See Table 1 for socio-demographic characteristics.
3.3. The status of negative emotions, social supports, psychological resilience, and burnout among pediatric residents
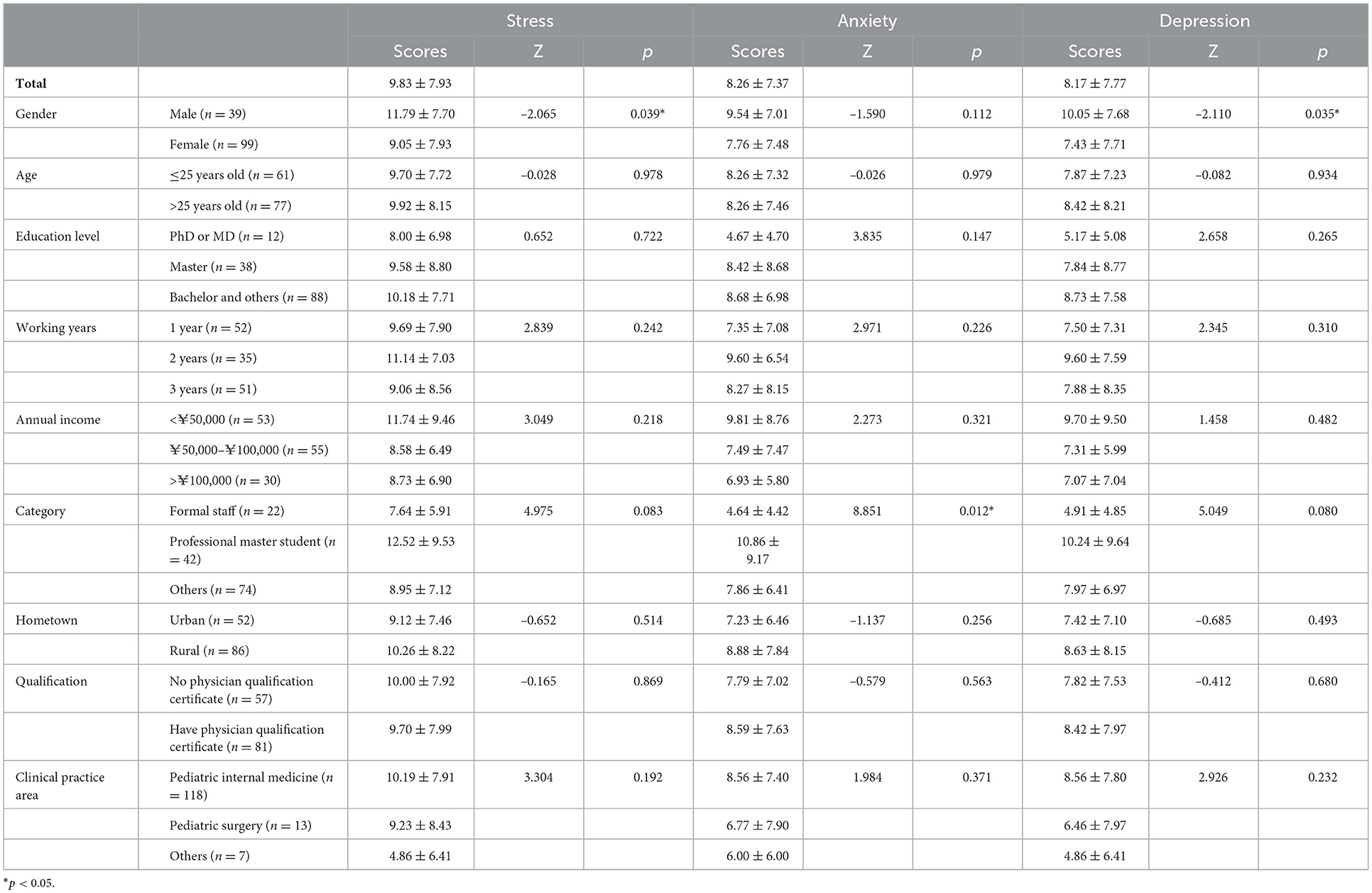
Analysis of the DASS-21 showed that the average scores of the subscales of stress, anxiety and depression were (9.83 ± 7.93), (8.26 ± 7.37), and (8.17 ± 7.77), respectively. The abnormal rate of stress was 18.8% (26/138), of which very severe stress, severe stress, moderate stress and mild stress accounted for 0.7% (1/138), 5.1% (7/138), 5.1% (7/138), and 7.9% (11/138), respectively. The incidence of anxiety was 47.8% (66/138), of which very severe anxiety, severe anxiety, moderate anxiety, and mild anxiety accounted for 7.9% (11/138), 7.9% (11/138), 22.9% (30/138), and 10.1% (14/138), respectively. The incidence of depression was 47.8% (67/138), of which very severe depression, severe depression, moderate depression, and mild depression accounted for 3.6% (5/138), 2.2% (3/138), 18.8% (26/138), and 20.3% (28/138), respectively. See Table 2 for details.
The lowest SSRS score was 17, the highest was 57, and the average score was (32.21 ± 6.83). Among them, two respondents (1.4%) reported that they had received little social support, 53 (38.5%) had general social support and 83 (60.1%) had satisfactory social support. The objective support score was (5.92 ± 2.63), the subjective support score was (19.03 ± 4.282), and the support utilization score was (7.26 ± 1.86). The average score of the CD-RISC was (58.26 ± 15.66), including tenacity (42.56 ± 8.74), strength (28.54 ± 5.32) and optimism (13.16 ± 2.47). The overall average score of MBI-GS was (50.87 ± 20.59), of which emotional exhaustion accounted for (15.88 ± 7.11), cynicism (7.89 ± 5.50), and reduced personal accomplishment (20.62 ± 7.53). The incidence of burnout among pediatric residents was 51.4% (71/138), of which the incidences of severe burnout, moderate burnout, and mild burnout were 2.2% (3/138), 9.4% (13/138), and 39.8% (55/138), respectively.
3.4. Correlation analysis and mediating effect analysis
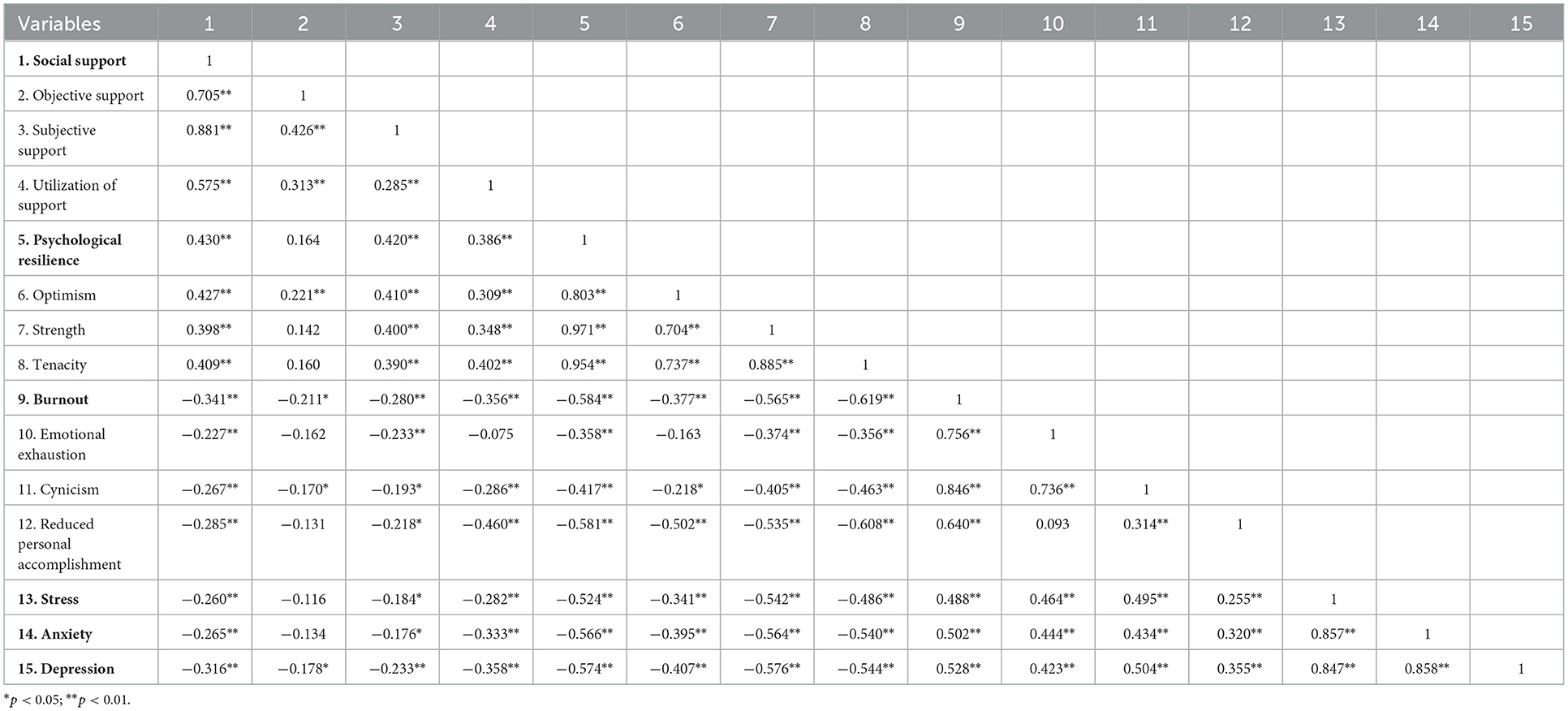
Stress among pediatric residents was negatively correlated with social support (r = −0.260, p < 0.01) as well as psychological resilience (r = −0.542, p < 0.01), but positively correlated with burnout (r = 0.488, p < 0.01); their anxiety was negatively correlated with social support (r = −0.265, p < 0.01) and psychological resilience (r = −0.566, p < 0.01), whereas positively correlated with burnout (r = 0.502, p < 0.01); depression, similarly, was negatively correlated with social support (r = −0.316, p < 0.01) and psychological resilience (r = −0.574, p < 0.01), but positively correlated with burnout (r = 0.528, p < 0.01). The correlation analysis of social support, psychological resilience, burnout, stress, anxiety and depression is shown in Table 3, indicating that H1 was verified.
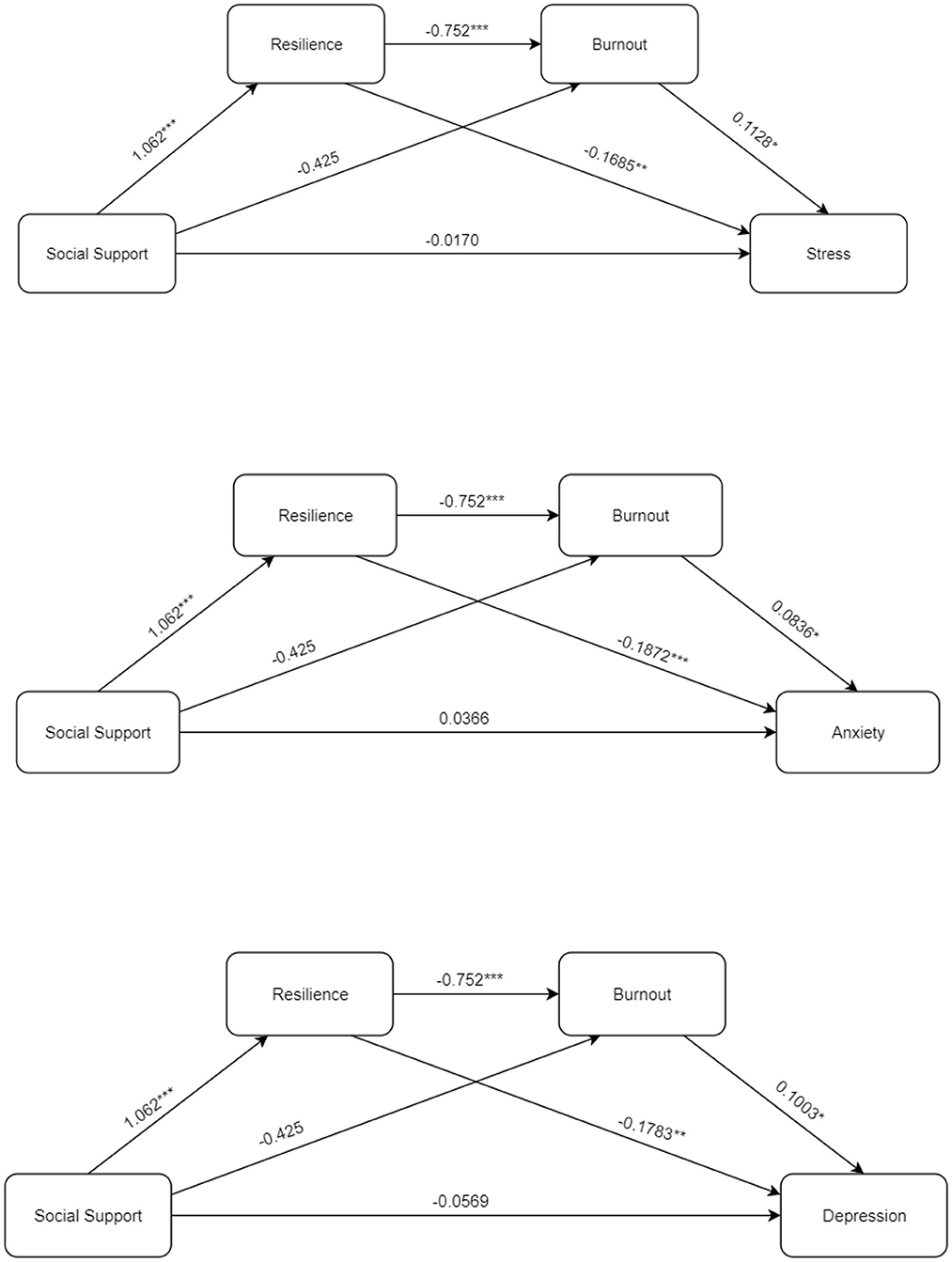
Taking the levels of stress, anxiety, and depression as dependent variables; social supports as independent variables, and psychological resilience and burnout as mediating independent variables; a chain-mediating effect analysis was carried out. The beta values obtained from the analysis are shown in Figure 1. Social support positively predicted resilience (β = 1.062, p < 0.001); psychological resilience negatively predicted burnout (β = 0.752, p < 0.001), stress (β = −0.1684, p < 0.001), anxiety (β = −0.1872, p < 0.001) and depression (β = −0.1783, p < 0.001); while burnout positively predicted stress (β = 0.1128, p < 0.05), anxiety (β = 0.0836, p < 0.05) and depression (β = 0.1003, p < 0.05).
It can be seen from Table 4 that the mediating effect of resilience between social supports and negative emotions was significant, indicating that H2 was verified; the mediating effect of burnout was not significantly associated with social supports and negative emotions, indicating that H3 was not verified; the chain-mediating effect of resilience and burnout was significantly associated with social supports and negative emotions, and it was a complete mediating role, which verified H4.
4. Discussion
The abnormal rate of stress among the 138 pediatric residents in this study was 18.8%, and nearly half developed anxiety and depression. The residency period is the initial stage at which medical professionals embark on their formal career path, and stress may be related to excessive medical disputes and patients' high expectations (25). Tense doctor-patient relationships have a significant effect on mental health, job satisfaction, burnout and rates of drop-out among physicians (47, 48). In addition to intense clinical work, the income of residents is generally lower, more than 70% of pediatric residents in this study earning < ¥100,000 per year. Residency trainees also include many highly educated medical graduates. Some of these doctors may be over 30 years old when they start their training and may also be responsible for supporting their parents and other family expenses. Therefore, their financial pressure cannot be ignored, and improving the treatment of residents is still something that needs to be addressed at this time.
At present, it is believed that longer working hours are associated with greater work pressures, which may contribute to negative emotions (49). Some scholars constructed an effort-reward-imbalance model of occupational stress (50), which can be used to explain the occurrence of negative emotions. Negative emotions are not only detrimental to the mental health of physicians, but may also increase the incidence of medical errors (51). Screening out physicians with psychological abnormalities and encouraging them to seek help and treatment through educational actions may be a feasible way to help medical staff to reduce negative emotions (52). Psychological interventions had a positive and significant effect on negative emotions (53). The Vila Sana Program, which was established by the Norwegian Medical Association to provide free individual and group counseling services for all doctors in the country, improved the mental health of clinicians (54). There is also an urgent need in China to establish a psychological support service system for pediatric residents and for all physicians, to improve their mental health.
The results of this study showed that negative emotions among pediatric residents were significantly inversely associated with social support. Previous studies suggested that social support had preventive and regulatory effects on stress and depressive symptoms (55, 56), and social support can help residents to deal with stressors more effectively (57), which may be attributed to the way in which social support can shape brain activity (58). As seen in Table 3, male residents exhibited higher levels of stress and were more likely to suffer from depression. This suggested that the mental health of male pediatric residents should not be neglected. In China, female pediatricians far outnumber male pediatricians, which was also confirmed in this study. It was observed on a daily basis that female pediatricians are more likely to form partnerships and support each other, whereas Chinese men were less good at expressing emotions in traditional culture, which results in emotional problems. We also found that professional master's students are a relatively special group of residents, and anxiety is more obvious in this group, which might also be related to the current professional master's training model in China. Unlike other residents who only need clinical rotations to improve clinical theory and practice, professional master's students are required to engage in scientific research in addition to clinical work, which increases the risk of negative emotions. Considering the points outlined above, government authorities should reform the training of professional master's students.
Our study found that psychological resilience was one of the most important factors that mediated the relationship between social support and negative emotions, and that negative emotions among pediatric residents were significantly and negatively correlated with psychological resilience, similar to previous findings in other populations (35). Individuals with higher levels of psychological resilience were highly adaptable when confronted with adversities and work-related pressures, and they also demonstrated an ability to make decisions that were most favorable in the current situation, which enhances subjective wellbeing and quality of life (22). We also found that burnout was also an important factor in mediating the relationship between resilience and negative emotions. This is consistent with the conservation of resources theory (59) which holds that burnout arises from an imbalance between an employee's perceived levels of job investment and job reward. Moreover, burnout can cause employees to negatively evaluate themselves and others, and can also cause negative reactions. Therefore, in addition to increasing social supports for pediatric residents, it is also necessary to strengthen psychological resilience and reduce burnout, thereby alleviating negative emotions.
Some studies have explored how psychological resilience can be enhanced among doctors, and the most mainstream method involves providing mindfulness training (60–62). Before and after the implementation of some intervention measures, an improvement has been observed in resilience test scores (63, 64), although not all physicians showed a significant improvement, and some even exhibited decreased levels of resilience. However, these physicians nonetheless felt that similar interventions could encourage better peer relationships and play a positive role in strengthening resilience (61). Mindfulness-based interventions tend to focus on building resilience at the individual level, which is now believed to be determined by a combination of internal and external factors rather than a single intrinsic factor (33, 65), as confirmed by this study, and social support, as an external factor, can directly affect psychological resilience. Therefore, the results of the current study indicate that external supports, such as family support and peer support, play an equally important role in promoting psychological resilience. Some scholars have started to examine how external environments, such as organizations, affects individual resilience, proposing that it is possible to improve an individual's levels of resilience within an organization by addressing organizational-level issues (66). In China, literature that focuses on improving the psychological resilience of medical staff is scarce. As such, we need to learn from relevant foreign studies and develop psychological resilience intervention programs targeted at Chinese pediatric residents.
This paper presented a preliminary study on the current situation and multiple mediating paths of negative emotions among pediatric residents in China, and highlighted the role of social supports, psychological resilience and burnout in generating negative emotions. We call on the Chinese society to pay attention to the negative emotions of Chinese pediatric residents. Three ways to reduce negative emotions by strengthening social support, improving resilience, and alleviating burnout could be considered, which provides a basis for governmental policies on pediatric residents' occupational health. In the future, we can continue to study the factors affecting the negative emotions at different levels, such as individual, organization and society. The clinical intervention trial will be designed to explore the psychological intervention to improve the mental health of Chinese pediatricians.
This study had some limitations. The bootstrap analysis of the mediating effect of social supports and anxiety revealed that the total beta effect was smaller than the total indirect beta effect, although there may have been a masking effect. Therefore, future studies should increase the sample size to further examine the relationship between social supports and anxiety. Some of the conclusions presented in this paper were largely consistent with existing studies involving other populations, but further intervention studies should be carried out among the Chinese pediatric resident population to verify the findings. Self-report scales were used, and the results may have been impacted by social desirability bias.
5. Conclusion
Psychological resilience and burnout played a chain-mediating role between social supports and negative emotions. The whole society and government departments should pay attention to the emotional problems of pediatric residents, especially professional master's students and male residents. Strengthening social support, increasing psychological resilience, and relieving burnout may be the ways to reduce negative emotions. There is an urgent need to establish a psychological support service system to improve the mental health of pediatric residents. In conclusion, measures should be taken to improve the mental health of Chinese pediatric residents.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study was approved by the Ethics Committee of the children's hospital, Zhejiang University school of medicine (No. 2022-IRB-107). Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CS recruited participants, collected questionnaires, and wrote the draft. X-TD and J-HM performed the statistical analysis. Y-XH conceived the study and revised the draft. J-HM contributed to recruiting the participants and collecting the questionnaires. J-HM and WZ participated in the revision of the paper. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the Major Project of New Generation Artificial Intelligence, Scientific and Technological Innovation 2030 (Ministry of Science and Technology of the People's Republic of China) (2021ZD0113505), the Second Batch of Industry–University-Education Collaboration Projects (Ministry of Education of the People's Republic of China) (202102177013), and 2020 Education Reform Project of Zhejiang University School of Medicine (jgyb20202037).
Acknowledgments
We sincerely thank all the respondents who volunteered to participate in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hu KJ, Sun ZZ, Rui YJ, Mi JY, Ren MX. Shortage of paediatricians in China. Lancet. (2014) 383:954. doi: 10.1016/S0140-6736(14)60482-7
2. Xu W, Zhang SC. Chinese pediatricians face a crisis: should they stay or leave? Pediatrics. (2014) 134:1045–7. doi: 10.1542/peds.2014-1377
3. Zhang Y, Huang L, Zhou X, Zhang X, Ke Z, Wang Z, et al. Characteristics and workload of pediatricians in China. Pediatrics. (2019) 144:e20183532. doi: 10.1542/peds.2018-3532
4. Zhang H, Jiang X, Da H, Dai R, Zhao N, Pan W, et al. Effect of comprehensive psychosomatic promotion in hypertension patients with anxiety and depression based on community: a randomized parallel controlled trial. Medicine (Baltimore). (2020) 99:e21451. doi: 10.1097/MD.0000000000021451
5. Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. (2018) 178:1317–30. doi: 10.1001/jamainternmed.2018.3713
6. El Archi S, Cortese S, Ballon N, Réveillère C, De Luca A, Barrault S, et al. Negative affectivity and emotion dysregulation as mediators between ADHD and disordered eating: a systematic review. Nutrients. (2020) 12:3292. doi: 10.3390/nu12113292
7. Maier T, Kugelmann M, Rhee DS, Brill S, Gündel H, Friemert B, et al. Structural equation modeling of a global stress index in healthy soldiers. J Clin Med. (2021) 10:1799. doi: 10.3390/jcm10081799
8. Sun J, Sun R, Jiang Y, Chen X, Li Z, Ma Z, et al. The relationship between psychological health and social support: evidence from physicians in China. PLoS ONE. (2020) 15:e0228152. doi: 10.1371/journal.pone.0228152
9. Hur NW, Kim HC, Waite L, Youm Y. Is the relationship between depression and c reactive protein level moderated by social support in elderly?-Korean Social Life, Health, and Aging Project (KSHAP). Psychiatry Investig. (2018) 15:24–33. doi: 10.4306/pi.2018.15.1.24
10. Levine JW, Ferrer P, De Witte AJ, Levitt FH, Castro G, Varella M, et al. The association between social support and psychological distress in Latina mothers living in Miami-Dade County, Florida. Cureus. (2020) 12:e10848. doi: 10.7759/cureus.10848
11. Vaughan C, Trail TE, Mahmud A, Dellva S, Tanielian T, Friedman E. Informal caregivers' experiences and perceptions of a web-based peer support network: mixed-methods study. J Med Internet Res. (2018) 20:e257. doi: 10.2196/jmir.9895
12. Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. doi: 10.1017/S2045796020000931
13. Santini ZI, Stougaard S, Koyanagi A, Ersbøll AK, Nielsen L, Hinrichsen C, et al. Predictors of high and low mental well-being and common mental disorders: findings from a Danish population-based study. Eur J Public Health. (2020) 30:532–8. doi: 10.1093/eurpub/ckaa021
14. Guo J, Liu L, Zhao B, Wang D. Teacher support and mental well-being in Chinese adolescents: the mediating role of negative emotions and resilience. Front Psychol. (2020) 10:3081. doi: 10.3389/fpsyg.2019.03081
15. Mukhtar S., Mahmood Z. Moderating role of perceived social support between perceived parenting styles and relational aggression in adolescents. J Aggress Maltreatment Trauma. (2018) 27:831–845. doi: 10.1080/10926771.2018.1468842
16. Topiwala A, Suri S, Allan C, Valkanova V, Filippini N, Sexton CE, et al. Predicting cognitive resilience from midlife lifestyle and multi-modal MRI: a 30-year prospective cohort study. PLoS ONE. (2019) 14:e0211273. doi: 10.1371/journal.pone.0211273
17. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
18. Yldrm M, Celik F. Social support, resilience and subjective well-being in college students. J Posit School Psychol. (2020) 5:127–35. doi: 10.47602/jpsp.v5i2.229
19. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
20. Chen S, Bagrodia R, Pfeffer CC, Meli L, Bonanno GA. Anxiety and resilience in the face of natural disasters associated with climate change: a review and methodological critique. J Anxiety Disord. (2020) 76:102297. doi: 10.1016/j.janxdis.2020.102297
21. Beck AT, Bredemeier K. A unified model of depression: integrating clinical, cognitive, biological, and evolutionary perspectives. Clin Psychol Sci. (2016) 4:596–619. doi: 10.1177/2167702616628523
22. Zou G, Shen X, Tian X, Liu C, Li G, Kong L, et al. Correlates of psychological distress, burnout, and resilience among Chinese female nurses. Ind Health. (2016) 54:389–95. doi: 10.2486/indhealth.2015-0103
23. Puranitee P, Stevens FF, Pakakasama S, Plitponkarnpim A, Vallibhakara SA, Busari JO, et al. Exploring burnout and the association with the educational climate in pediatric residents in Thailand. BMC Med Educ. (2019) 19:245. doi: 10.1186/s12909-019-1687-7
24. Kushnir T, Levhar C, Cohen AH. Are burnout levels increasing? The experience of Israeli primary care physicians. Isr Med Assoc J. (2004) 6:451–5.
25. Zhou J, Yang Y, Qiu X, Yang X, Pan H, Ban B, et al. Relationship between anxiety and burnout among chinese physicians: a moderated mediation model. PLoS ONE. (2016) 11:e0157013. doi: 10.1371/journal.pone.0157013
26. Khamisa N, Peltzer K, Ilic D, Oldenburg B. Work related stress, burnout, job satisfaction and general health of nurses: a follow-up study. Int J Nurs Pract. (2016) 22:538–45. doi: 10.1111/ijn.12455
27. Ariapooran S. Compassion fatigue and burnout in Iranian nurses: the role of perceived social support. Iran J Nurs Midwifery Res. (2014) 19:279–84.
28. Van der Heijden B, Brown Mahoney C, Xu Y. Impact of job demands and resources on nurses' burnout and occupational turnover intention towards an age-moderated mediation model for the nursing profession. Int J Environ Res Public Health. (2019) 16:2011. doi: 10.3390/ijerph16112011
29. Bezerra Cde M, Assis SG, Constantino P. Psychological distress and work stress in correctional officers: a literature review. Cien Saude Colet. (2016) 21:2135–46. doi: 10.1590/1413-81232015217.00502016
30. Özmen S, Yurttaş A. Determination of care burden of caregivers of patients with multiple sclerosis in Turkey. Behav Neurol. (2018) 2018:7205046. doi: 10.1155/2018/7205046
31. Guo YF, Luo YH, Lam L, Cross W, Plummer V, Zhang JP. Burnout and its association with resilience in nurses: a cross-sectional study. J Clin Nurs. (2018) 27:441–9. doi: 10.1111/jocn.13952
32. McKnight J, Nzinga J, Jepkosgei J, English M. Collective strategies to cope with work related stress among nurses in resource constrained settings: an ethnography of neonatal nursing in Kenya. Soc Sci Med. (2020) 245:112698. doi: 10.1016/j.socscimed.2019.112698
33. Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. Eur Psychol. (2013) 18:12–23. doi: 10.1027/1016-9040/a000124
34. Kelly LA, Gee PM, Butler RJ. Impact of nurse burnout on organizational and position turnover. Nurs Outlook. (2021) 69:96–102. doi: 10.1016/j.outlook.2020.06.008
35. Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care. (2015) 24:412–20. doi: 10.4037/ajcc2015291
36. Zanon C, Brenner RE, Baptista MN, Vogel DL, Rubin M, Al-Darmaki FR, et al. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress scale-21 (DASS-21) Across Eight Countries. Assessment. (2021) 28:1531–44. doi: 10.1177/1073191119887449
37. Aravena PC, Astudillo P, Miranda H, Manterola C. Reliability and validity of measuring scale for postoperative complications in third molar surgery. BMC Oral Health. (2018) 18:25. doi: 10.1186/s12903-018-0486-6
38. Xiao SY. The theoretical basis and research application of “Social Support Rating Scale”. J Clin Psychiatry. (1994) 4:98–100.
39. Fu C, Leoutsakos JM, Underwood C. An examination of resilience cross-culturally in child and adolescent survivors of the 2008 China earthquake using the Connor-Davidson resilience scale (CD-RISC). J Affect Disord. (2014) 155:149–53. doi: 10.1016/j.jad.2013.10.041
40. Yu XN, Lau JT, Mak WW, Zhang J, Lui WW, Zhang J. Factor structure and psychometric properties of the Connor-Davidson Resilience Scale among Chinese adolescents. Compr Psychiatry. (2011) 52:218–24. doi: 10.1016/j.comppsych.2010.05.010
41. Wu L, Ren L, Wang Y, Zhang K, Fang P, Liu X, et al. The item network and domain network of burnout in Chinese nurses. BMC Nurs. (2021) 20:147. doi: 10.1186/s12912-021-00670-8
42. Hou J, Xu B, Zhang J, Luo L, Pen X, Chen S, et al. Psychological status and job burnout of nurses working in the frontline of the novel coronavirus in China during the delta variant outbreak: a cross-sectional survey. Psychol Res Behav Manag. (2022) 15:533–46. doi: 10.2147/PRBM.S343749
43. Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
44. Wilson LC, Scarpa A. Childhood abuse, perceived social support, and posttraumatic stress symptoms: a moderation model. Psychol Trauma. (2014) 6:512–8. doi: 10.1037/a0032635
45. Peters GJY. The alpha and the omega of scale reliability and validity: why and how to abandon Cronbach's alpha and the route towards more comprehensive assessment of scale quality. Eur Health Psychol. (2014) 16:56–69. doi: 10.31234/osf.io/h47fv
46. Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. (2014) 105:399–412. doi: 10.1111/bjop.12046
47. Wáng YX, Káplár Z, Li YT. AME survey-003 A1-part 2: the motivation factors of medical doctors in China. Quant Imaging Med Surg. (2015) 5:917–24. doi: 10.3978/j.issn.2223-4292.2015.12.01
48. Du L, Xu J, Chen X, Zhu X, Zhang Y, Wu R, et al. Rebuild doctor-patient trust in medical service delivery in China. Sci Rep. (2020) 10:21956. doi: 10.1038/s41598-020-78921-y
49. Beschoner P, von Wietersheim J, Jarczok MN, Braun M, Schönfeldt-Lecuona C, Jerg-Bretzke L, et al. Changes in working conditions and mental health among intensive care physicians across a decade. Front Psychiatry. (2020) 11:145. doi: 10.3389/fpsyt.2020.00145
50. Loerbroks A, Weigl M, Li J, Angerer P. Effort-reward imbalance and perceived quality of patient care: a cross-sectional study among physicians in Germany. BMC Public Health. (2016) 16:342. doi: 10.1186/s12889-016-3016-y
51. Mata DA, Loureiro SR. Crippa JA, Bolsoni LM, Sen S. Association between physician Depressive symptoms and medical errors: a systematic review and meta-analysis. JAMA Netw Open. (2019) 2:e1916097. doi: 10.1001/jamanetworkopen.2019.16097
52. Collier R. Physician suicide too often “brushed under the rug”. CMAJ. (2017) 189:E1240–1. doi: 10.1503/cmaj.1095498
53. Körver S, Geurtsen GJ, Hollak CEM, van Schaik IN, Longo MGF, Lima MR, et al. Depressive symptoms in Fabry disease: the importance of coping, subjective health perception and pain. Orphanet J Rare Dis. (2020) 15:28. doi: 10.1186/s13023-020-1307-y
54. Rø KE, Gude T, Tyssen R, Aasland OG. Counselling for burnout in Norwegian doctors: one year cohort study. BMJ. (2008) 337:a2004. doi: 10.1136/bmj.a2004
55. Ioannou M, Kassianos AP, Symeou M. Coping with depressive symptoms in young adults: perceived social support protects against depressive symptoms only under moderate levels of stress. Front Psychol. (2019) 9:2780. doi: 10.3389/fpsyg.2018.02780
56. Ouyang M, Gui D, Cai X, Yin Y, Mao X, Huang S, et al. Stressful life events and subjective well-being in vocational school female adolescents: the mediating role of depression and the moderating role of perceived social support. Front Psychol. (2021) 11:603511. doi: 10.3389/fpsyg.2020.603511
57. Zhang H, Chen D, Cui N, Zou P, Shao J, Wang X, et al. Explaining job satisfaction among residents in standardized residency training programs: a serial multiple mediation model. Risk Manag Healthc Policy. (2021) 14:4073–81. doi: 10.2147/RMHP.S330217
58. Hostinar CE, Gunnar MR. Social support can buffer against stress and shape brain activity. AJOB Neurosci. (2015) 6:34–42. doi: 10.1080/21507740.2015.1047054
59. Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Appl Psychol. (2001) 50:e62. doi: 10.1111/1464-0597.00062
60. Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med. (2013) 11:412–20. doi: 10.1370/afm.1511
61. Bird AN, Martinchek M, Pincavage AT. A curriculum to enhance resilience in internal medicine interns. J Grad Med Educ. (2017) 9:600–4. doi: 10.4300/JGME-D-16-00554.1
62. Schroeder DA, Stephens E, Colgan D, Hunsinger M, Rubin D, Christopher MS, et al. Brief mindfulness-based intervention for primary care physicians: a pilot randomized controlled trial. Am J Lifestyle Med. (2016) 12:83–91. doi: 10.1177/1559827616629121
63. Mache S, Danzer G, Klapp B, Groneberg DA. An evaluation of a multicomponent mental competency and stress management training for entrants in surgery medicine. J Surg Educ. (2015) 72:1102–8. doi: 10.1016/j.jsurg.2015.06.018
64. Mache S, Bernburg M, Baresi L, Groneberg DA. Evaluation of self-care skills training and solution-focused counselling for health professionals in psychiatric medicine: a pilot study. Int J Psychiatry Clin Pract. (2016) 20:239–44. doi: 10.1080/13651501.2016.1207085
65. Rutter M. Resilience in the face of adversity. Protective factors and resistance to psychiatric disorder. Br J Psychiatry. (1985) 147:598–611. doi: 10.1192/bjp.147.6.598
Keywords: social support, psychological resilience, stress, anxiety, depression, burnout, chain-mediating effect, pediatrician
Citation: Song C, Du X-T, Hong Y-X, Mao J-H and Zhang W (2023) Association between social supports and negative emotions among pediatric residents in China: The chain-mediating role of psychological resilience and burnout. Front. Public Health 10:962259. doi: 10.3389/fpubh.2022.962259
Received: 06 June 2022; Accepted: 27 December 2022;
Published: 23 January 2023.
Edited by:
Oriol Yuguero, Lleida Institute for Biomedical Research (IRBLleida), SpainReviewed by:
Zhaoqiang Jiang, Hangzhou Medical College, ChinaAh Yusuf, Airlangga University, Indonesia
Copyright © 2023 Song, Du, Hong, Mao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun-Xia Hong,  Y2hieWhqeWJAemp1LmVkdS5jbg==; Jian-Hua Mao,
Y2hieWhqeWJAemp1LmVkdS5jbg==; Jian-Hua Mao,  bWFvamg4OEB6anUuZWR1LmNu
bWFvamg4OEB6anUuZWR1LmNu
 Chao Song
Chao Song Xiao-Tian Du2
Xiao-Tian Du2 Yun-Xia Hong
Yun-Xia Hong Jian-Hua Mao
Jian-Hua Mao