
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 03 August 2022
Sec. Family Medicine and Primary Care
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.952710
This article is part of the Research Topic Improving Symptom Outcomes and Quality of Life in Breast Cancer Survivors View all 4 articles
Background: Currently, few studies have explored the heterogeneity of symptoms and functions in patients with breast cancer. This study aimed to identify the subgroups of symptoms and functions in women receiving chemotherapy for breast cancer and determine whether the subgroups differed in demographic and clinical characteristics.
Methods: A cross-sectional multicenter survey involving five hospitals in Zhejiang, Shanghai, Shandong, and Guangxi provinces of Mainland China was implemented between August 2020 to December 2021. Participants completed questionnaires that included the PROMIS-57, PROMIS cognitive function short form, and demographic and clinical characteristics. Latent class analysis was performed, followed by chi-square test and analysis of variance. Subsequently, significant variables were included in multinomial logistic regression.
Results: A total of 1,180 patients were investigated, with an average age of 48.9 years. Three classes were identified: low symptom burdens and functions group (26.2%, Class 1), moderate symptom burdens and functions group (16.9%, Class 2), and low symptom burdens and high functions group (56.9%, Class 3). Compared with patients in Class 1 and 3, those in Class 2 consistently showed a higher tendency of having urban employee health insurance (odds ratio = 2.506, P < 0.05) and rural health insurance (odds ratio = 2.207, P < 0.05). Additionally, patients in Class 2 tended to be in their fourth cycle of chemotherapy. However, receiving chemotherapy and surgery increased the likelihood of belonging to Class 1.
Conclusions: A high proportion of patients experienced varying degrees of symptom and function issues, suggesting that attention is warranted for women with breast cancer undergoing chemotherapy. Patients with the urban employee basic medical system, the new rural cooperative medical system and in the early stage of chemotherapy cycles were more likely to have symptom burdens. Middle-aged postmenopausal women reported varying degrees of cognitive issues. Additionally, surgery increased the presence of potential long-term effects in functional levels.
Breast cancer may present with persistent and distressing symptoms caused by disease and treatment (1, 2). For example, anticipating chemotherapy can be a stressful experience accompanied with multiple symptoms and dysfunction (3–5). Considerable evidence has shown that fatigue, pain, sleep disturbance, anxiety, and depression often manifest as a symptom cluster in women with breast cancer (6–8). Symptom clusters are sets of interrelated symptoms that share a common etiology or variance, and might cause more impact on health outcomes when compared with isolated symptoms (9). In contrast to symptoms of patients without cancer diagnosis, symptom clusters are relatively more severe and are closely related to chronic syndrome (10). Additionally, physical, social, and cognitive impairment are commonly reported in the course of chemotherapy, and can be the consequence of symptom clusters (11, 12). As the crux of patient-reported outcomes, perception of symptoms and dysfunctions prompt individuals to obtain medical treatment and care. Given that many patients experience symptoms and function issues during chemotherapy, a comprehensive approach to identify high-risk subgroups and address these care needs should be implemented.
Assessment of symptoms and functions can be obtained directly from the patients' perspective. The Patient-Reported Outcomes Measurement Information System (PROMIS) is an initiative to promote standardization and validation of multiple self-reported outcome measures across different health conditions (12). PROMIS measures are calibrated based on the item response theory model, which makes it possible to quantify a health domain based on its severity. Therefore, PROMIS measures are ideal instruments for reporting symptoms and functions.
Some efforts have been made to explore the symptom experiences of patients with breast cancer. However, variable-centered methods might dilute the heterogeneity by using total scores of the symptoms for evaluation purposes. Latent class analysis (LCA) is a commonly used person-centered approach to distinguish heterogeneous entities compared with a variable-centered method (13). It allows inter-individual variability, identifies the class-specific probability of response profiles and characteristics, and assigns similar individuals into corresponding subgroups (13). Therefore, LCA is useful for clinical and research purposes, as it elaborates the inter-individual relationship and enables health professionals to perform targeted guidance and interventions for specific groups. The mean age of diagnosis for breast cancer is 45–55 years in China, which is almost 10 years younger than the average for western patients (14). Additionally, middle-aged women accounted for a large proportion of patients with breast cancer in China (14). Given no prior attention has been given to heterogeneity for symptoms and functions in women receiving chemotherapy for breast cancer in China, it is important to understand distinct clusters and predict high-risk individuals with symptoms and function issues. Additionally, few study have adopted PROMIS measures in patients with breast cancer to identify their symptoms and functions experiences, especially in those receiving chemotherapy. Therefore, the purpose of this study was to examine the heterogeneity of symptoms and functions using the LCA approach and delineate the class characteristics using PROMIS measures in women receiving chemotherapy for breast cancer in China.
A cross-sectional research design, which adhered to the STROBE guidelines, was adopted. Using convenience sampling method, patients with breast cancer who were hospitalized in five tertiary hospitals in Zhejiang, Shanghai, Shandong, and Guangxi provinces were recruited from August 2020 to December 2021. The inclusion criteria for participants were as follows: women aged 18 years old or above, diagnosed with breast cancer, receiving chemotherapy, and were able to write or speak Chinese. Patients who were in critical or terminal condition, had other cancers or serious diseases, refused to participate, and had psychiatric illnesses were excluded. More than 50 samples are recommended for LCA for each subgroup (13). Therefore, we included more than 1,000 patients to ensure the accuracy of the classification.
Demographic data included age, marital status, children, educational level, employment status, annual household income, and medical insurance. The health condition characteristics were cancer stage, therapeutic regimen, and chemotherapy cycle.
PROMIS-57 is a commonly used instrument to assess multidimensional symptoms and functions (15). The instrument consists of seven domains, including physical function (eight items), anxiety (eight items), depression (eight items), fatigue (eight items), sleep disturbance (eight items), pain interference and intensity (eight items for pain interference and a single item for pain intensity), and ability to participate in social roles and activities (eight items) (16). The total scores range from 8 to 40 and all items are rated on a five-point Likert scale, except for pain intensity, which is assessed using a numeric rating scale ranging from 0 to 10. Raw scores of all domains are transformed into T-scores, with a mean of 50 and a standard deviation of 10, indicating the reference level of the general US population (http://www.healthmeasures.net). A higher score indicates a higher level of the trait being measured, i.e., either higher degrees of function or worse symptom burden. Therefore, higher scores for anxiety, depression, fatigue, and sleep disturbance domains reflect more symptom severity. By contrast, higher scores for physical function and ability to participate in social roles and activities domains reflect better functioning (15). The psychometric properties of the PROMIS-57 had been validated in multiple studies on patients with chronic diseases including breast cancer (15, 16). The Cronbach's α of the PROMIS-57 ranged from 0.85 to 0.95 in this study.
PROMIS cognitive function short form is a self-reported instrument of perceived cognitive difficulties (17). The instrument consists of four items, which are rated on a five-point Likert scale during the previous 7 days (1 = very often to 5 = never). Raw score of the four items ranges from 4 to 20 and is transformed to T-scores (M = 50, SD = 10), and lower scores indicate greater subjective cognitive difficulty (17). The Cronbach's α of the scale was 0.93 in this study.
Ethical approval of this study was obtained from the Institutional Review Boards of Fudan University Cancer Hospital (no 1810192-22) and Fudan University Zhongshan Hospital (no 2020-076R). The multicenter survey was supported by a mobile application named “intelligent intervention system for chronic disease follow-up,” which aimed to combine intelligent follow-up and intervention for medical staff and was available for symptom management, follow-up, health education, and visit notice. The application had been utilized to maintain long-term contact between patients and medical staff and improve patients' compliance and treatment experience in clinical settings in Affiliated Hospital of Medical School of Ningbo University for years. In this study, demographic and clinical characteristics, PROMIS-57, and PROMIS cognitive function short form were incorporated into the application.
To ensure standardization of data collection, all research assistants were previously trained to use the application. All patients completed written informed consent forms that assured the voluntariness and confidentiality of participation and their right to withdraw from the study without any penalty. Patients were also required to click on the “agree” button in the application before completing the survey if they agreed to participate. The research assistants verified the clinical characteristics of the patients to ensure consistency of the results with their medical records, and clarified any questions raised by the participants.
Data were analyzed using SPSS version 25.0 and Mplus version 8.0. Frequencies and percentages were adopted to describe demographic and clinical characteristics. Means and standard deviations were used to delineate subscale scores.
T-scores of the PROMIS-57 and PROMIS cognitive function short form were dichotomized as 0 or 1 according the cutoff score for clinical difference according to PROMIS guidelines (https://www.healthmeasures.net/). Subsequently, LCA from one to six classes was performed to identify the subtypes in terms of symptoms and functions. For model selection, low Akaike information criterion (AIC), Bayesian information criterion (BIC), and sample size-adjusted Bayesian information criterion (aBIC) were used to assess information criterion. Entropy was utilized to evaluate the accuracy of classifications. Additionally, Lo-Mendell-Rubin likelihood-ratio test (LMR-LRT) and bootstrap likelihood-ratio test (BLRT) were also performed (18). Lower AIC, BIC, aBIC, larger entropy, and statistically significant LMR-LRT and BLRT were indicators of good model fit (13). Subsequently, the difference in demographic and clinical variables among the subgroups was analyzed using a chi-square test and analysis of variance.
After best-fitting models were determined, multinomial logistic regression analysis was conducted to examine whether the above-mentioned significant variables had mutually adjusted associations with latent class membership. Odds ratios (ORs) and 95% confidence intervals were calculated. Statistical significance was set at P < 0.05.
Of the 1,350 participants, 170 were excluded due to missing items. A total of 1,180 patients were finally included in the final analysis. The mean age of the patients was 48.9 years (SD = 10.1, ranging from 24 to 85). Furthermore, 92.5% of them were married, and 54.5% had one child. Most participants had more than secondary school education: 19.5% received a high school diploma and 27.3% had completed a university degree or above. Most of the patients (60.5%) had an annual household income of ≥¥60,000 (approximately USD $9,240) and had urban employee health insurance (71.0%), and were unemployed (37.5%). With regard to clinical characteristics, most of them were in the early stage of cancer (37.2%). The majority received chemotherapy and surgery (39.8%) and had undergone more than five cycles of chemotherapy treatment (50.8%).
The goodness-of-fit index comparison is listed in Table 1. As more classes were included, the values of AIC, BIC, and aBIC decreased. LMR-LRT and BLRT results favored the three-class model over the higher-class models. The three-class model also obtained the highest entropy value. Thus, based on model fit indices and consideration of clinical interpretability, a three-class model was determined to be the optimal solution.
Probability for the three-class model is shown in Figure 1. Of the 1,180 patients, 26.2, 16.9, and 56.9% were classified into one, two, and three classes, respectively. Class 1 was characterized by featuring the low probability of symptom and function domains, and was labeled “low symptom burdens and functions group.” Class 2 was labeled as “moderate symptom burdens and functions group” since patients in this group were more likely to feature moderate probability of both symptom and function domains. Class 3 was characterized by featuring the lowest probability of symptoms but the highest function domains, and was labeled “low symptom burdens and high functions group.”
Table 2 shows the scores of the eight domains in each class. Patients in Class 3 obtained the highest scores in the physical, social, and cognitive function domains. By contrast, patients with more symptom burdens were more likely to belong to Class 2.
Differences in demographic characteristics among latent classes are reported in Table 3, and statistically significant differences were found in age, medical insurance, cancer stage, therapeutic regimen, and chemotherapy cycle (P < 0.05). These variables were included in multinomial logistic regression analysis.
Multinomial regression analysis was performed with Class 1 as reference. The reference groups were 20–39 years old, free medical insurance, cancer stage I, chemotherapy and surgery, and first chemotherapy cycle. Association of demographics and clinical characteristics with Classes 2 and Class 3 compared with Class 1 were shown in Figure 2, 3. Table 4 shows that patients with urban employee health insurance and rural health insurance were at increased risk for experiencing moderate symptoms compared with those with free or no medical insurance (OR = 2.506, P = 0.013; OR = 2.207, P = 0.038). These patients were also more likely to be in their fourth cycle of chemotherapy treatment (OR = 3.040, P = 0.008). Patients with chemotherapy and surgery treatment were more likely to have impaired functions compared with those with other therapeutic regimens. No significant associations were found between age and cancer stage with the risk of symptoms and function issues.
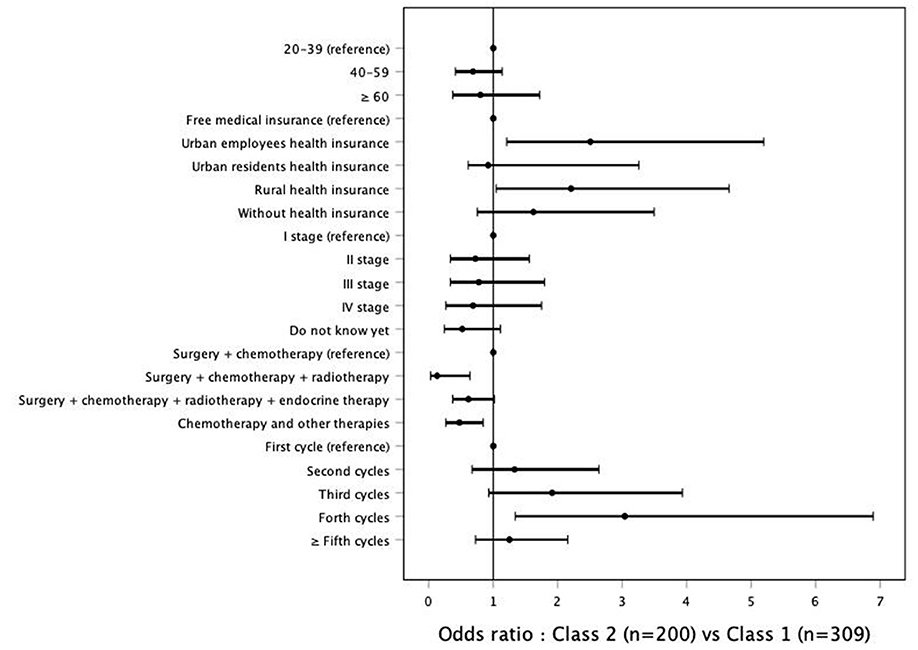
Figure 2. Association of demographics and clinical characteristics with Classes 2 compared with Class 1.
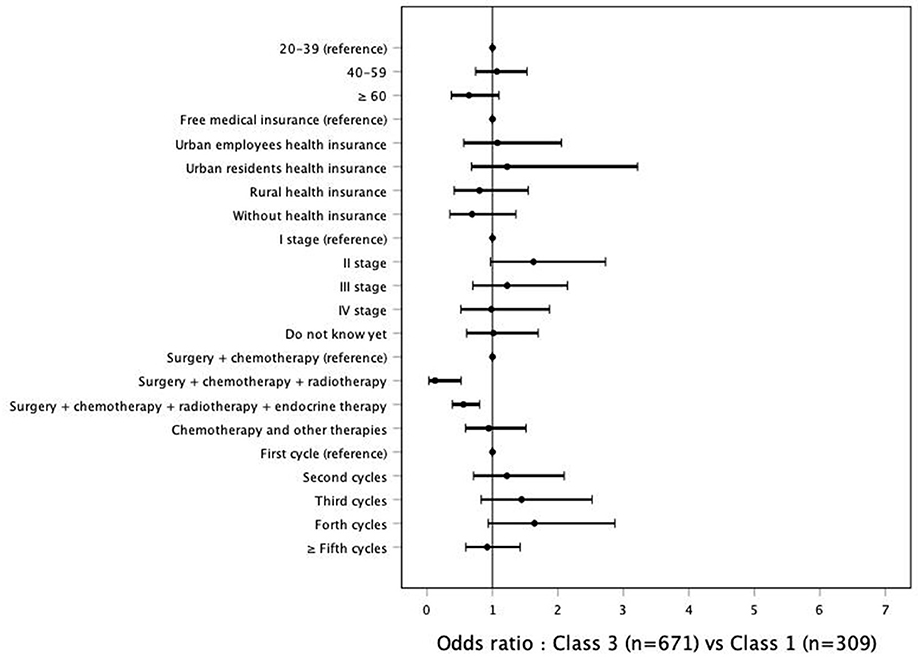
Figure 3. Association of demographics and clinical characteristics with Classes 3 compared with Class 1.
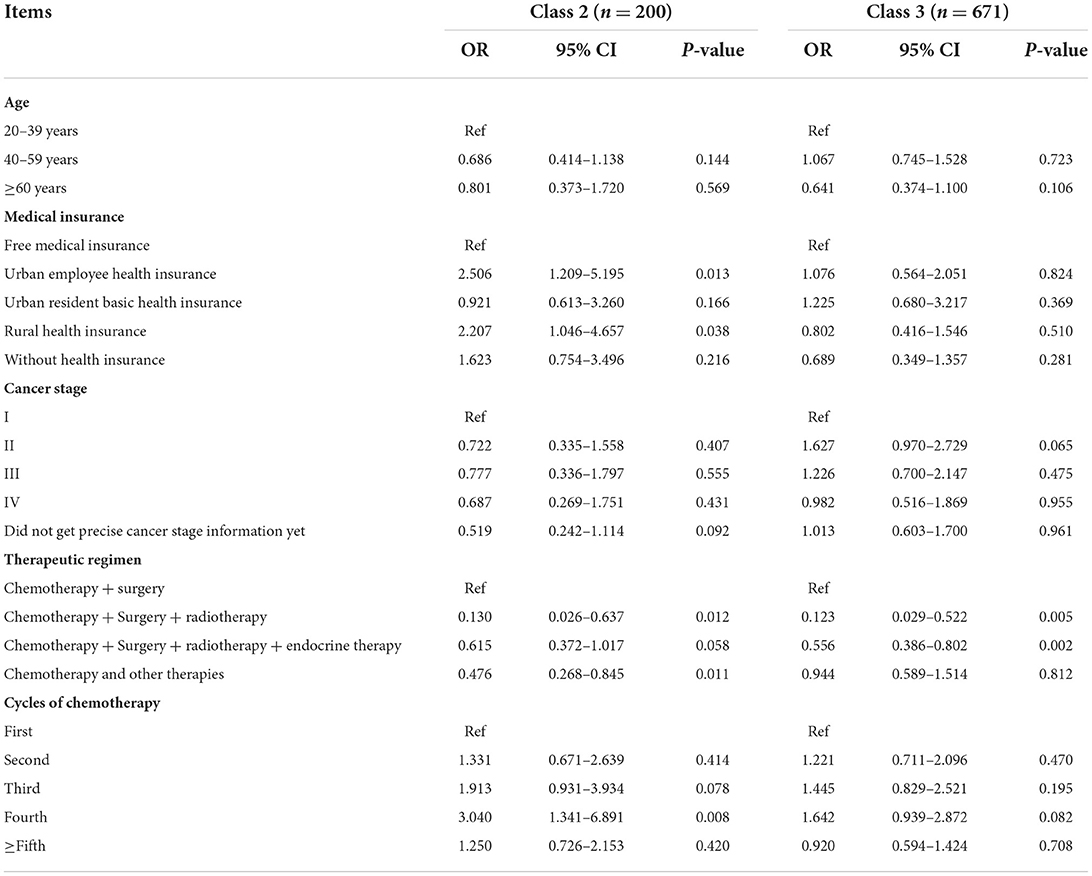
Table 4. Selected results of multinomial logistic regression: Potential prediction of latent class membership.
This study identified the heterogeneity for symptoms and functions in women with breast cancer undergoing chemotherapy by performing a person-centered cluster statistical analysis. Three latent classes were identified: low symptom burdens and functions group, moderate symptom burdens and functions group, and low symptom burdens and high functions group. Notably, 43.14% of the participants belonged to classes with symptom or function issues, suggesting that early detection should be considered to identify patients at risk and provide patient group-specific interventions.
Consistent with the findings of Kyranou and Li et al. (19, 20), the present study found that the symptom cluster showed similar trends of severity, especially in anxiety and depression, fatigue, and sleep disturbance domains. Although not always consistent with the tendency of symptoms, a consistent pattern was found for the function domains (21, 22). Patients in Class 3 were more likely to report low levels of symptoms but high function and were a relatively small burden group, accounting for the largest proportion. Although the patients in Class 1 had low symptoms, they had impaired functions physically and socially. In contrast, the patients in Class 2 were more concerned with their symptoms. Therefore, nurses should prioritize assessment and interventions to patients in Class 1 and 2.
The type of health insurance was found to be correlated with symptom and function levels. Patients in Class 2 were more likely to have urban employee health insurance and rural health insurance. Currently, China has three public health insurance systems, namely the urban resident basic medical system, the urban employee basic medical system, and the new rural cooperative medical system (23). However, the current tiered basic medical insurance scheme cannot cover all the health services. Patients with urban employee health insurance suffer from long-term follow-up costs and the loss of some employment-based insurance benefits due to the inability to work (24, 25). For patients with new rural cooperative medical insurance, their economic burden is higher than those with urban residents and urban employee medical insurance, and they have to pay for relatively high costs out-of-pocket after a cancer diagnosis. For example, the proportion of medical expenses coverage for the urban residents is 70–90% while there is only 50–60% for the rural residents (26). Additionally, patients who live in rural areas may face disproportionate financial problems due to higher transportation costs, higher rates of uninsured and other factors (26). Therefore, they have less access to symptom management and suffer from more perceived financial hardship due to the disease and the treatment, which might be the reason for more symptoms and dysfunction (26).
Consistent with the literature (26), patients in the early stage of chemotherapy cycles were more likely to be in the group characterized by higher symptom severity, and patients in Class 2 tended to be in their fourth cycle of chemotherapy treatment. Browall et al. (27) reported that the fatigue and pain symptoms significant affected functional status of patients with stage I–IIIa breast cancer at three to five cycles of their chemotherapy, and these symptoms were not major concerns after the 6 cycles. Therefore, our results were not against the broader literature.
Previous studies reported that age is an important and unmodifiable risk factor for functional status such as cognitive and physical function, and the prevalence of cancer-related cognitive impairment is high among females aged 60 years or above (28, 29). Mandelblatt et al. (30) explored trajectories of self-reported cognitive function over time in older women with breast cancer who received chemotherapy for 6 years, and found that less than one in 10 patients had a steep decline with accelerated aging for cognitive function. However, only 12.4% of the patients in this study were aged 60 years or older, and critically ill patients or patients who were unwilling to use the mobile application were excluded, which may have influenced the results and made the proportion of patients with cognitive decline or physical function smaller overall. Interestingly, middle-aged postmenopausal women in this study reported varying degrees of cognitive issues. A recent study in China suggested that electrophysiological cognitive impairments mainly occur in younger patients receiving chemotherapy for breast cancer (31). This status would last for years after the treatment, highlighting the importance of early detection and intervention for relatively young patients. Additionally, the largest proportion of middle-aged patients was found in groups with more symptom burdens. Middle-aged women take on important roles at work and in their families and may be an essential provider of family income (32). The impact of cancer diagnosis and the long-term effects of treatment such as chemotherapy can lead to functional limitations, physical and psychological symptoms in these patients. It may cause dilemma in balancing work, social activities, and family responsibilities (33). Therefore, a relatively high occurrence of symptoms in middle-aged women could be understandable.
The findings also provided valuable information in terms of cancer-treatment details. Receiving chemotherapy and surgery treatment was found to be associated with Class 1, which was a group with more dysfunction. In our study, most patients had undergone more than five cycles of chemotherapy treatment, and were not shortly after surgery, and they did not report significant symptoms in this stage. Therefore, our results suggested that surgery increased the presence of more potential long-term late effects in functional levels, and the results were not against previous studies (30, 34). Our study did not particularly investigate the effect of different surgery types in the functional status. Fontes et al. (35) investigated women with breast cancer surgery or without breast cancer, and assessed the impact of surgical treatment on physical activity, functional capacity, and quality of life in patients with breast cancer. The results indicated that patients who underwent breast reconstruction reported better physical activity and quality of life than patients who received breast-conserving surgery or mastectomy alone. Therefore, future research would benefit from considering these variables and increase the external validity of the results in this study.
Our study has several limitations. First, the cross-sectional design failed to explore the trajectory of class memberships. The results required further testing by using a longitudinal study design. Second, the patients were recruited in tertiary hospitals, which might limit the generalization of the findings in other clinical settings. More predictors that differentiate at-risk subgroups need to be investigated further.
The person-centered approach used in this study identified the discrete heterogeneity of symptoms and functions, which leaned close to the natural convergence of the interaction patterns from a patient perspective and shed light on inter-group differences. Understanding how these groups vary during the chemotherapy treatment helped to identify subgroups of patients at risk for elevated symptoms and dysfunction. A high proportion of patients experienced varying degrees of these issues, suggesting that more attention is warranted for women with breast cancer undergoing chemotherapy. Patients with the urban employee basic medical system, the new rural cooperative medical system and in the early stage of chemotherapy cycles were more likely to have symptom burdens. Middle-aged postmenopausal women in China reported varying degrees of cognitive issues. Additionally, surgery increases the presence of potential long-term effects in functional levels. These patients may benefit from additional assessment and early intervention.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval of this study was obtained from the Institutional Review Boards of Fudan University Cancer Hospital (no 1810192-22) and Fudan University Zhongshan Hospital (no 2020-076R). The patients/participants provided their written informed consent to participate in this study.
TC and TZ: drafted the manuscript, contributed to the design of the study, completed the acquisition and analysis of data for the work. ChaY: contributed to the interpretation and critical revision of the manuscript. ZS, TC, and ChuY: completed the acquisition of data for the work, made the interpretation of data for the work. FN: involved in the analysis of data for the work, revised the manuscript critically for important intellectual content. ZS: contributed to the conception, design, interpretation and critical revision of the manuscript. All authors have read and approved the final manuscript.
This study was supported by the Major Project for Science & Technology Innovation 2025 in Ningbo, China (2019B10035). The funding aided in the questionnaire collection process and open access publication fees of the manuscript.
The authors wish to extend their sincere thanks to the data collectors for their contributions and thank the participants of the study for their cooperation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cai T, Qian J, Huang Q, Yuan C. Distinct dyadic coping profiles in Chinese couples with breast cancer. Support Care in Cancer. (2021) 29:6459–68. doi: 10.1007/s00520-021-06237-2
2. Jones JM, Olson K, Catton P, Catton CN, Fleshner NE, Krzyzanowska MK, et al. Cancer-related fatigue and associated disability in post-treatment cancer survivors. J Cancer Surviv. (2015) 10:51–61. doi: 10.1007/s11764-015-0450-2
3. Hansen JA, Feuerstein M, Calvio LC, Olsen CH. Breast cancer survivors at work. J Occup Environ Med. (2008) 50:777–84. doi: 10.1097/JOM.0b013e318165159e
4. Cai T, Huang Q, Yuan C. Profiles of instrumental, emotional, and informational support in Chinese breast cancer patients undergoing chemotherapy: a latent class analysis. BMC Women's Health. (2021) 21:183. doi: 10.1186/s12905-021-01307-3
5. Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. (2001) 28:465–70.
6. Kenne SE, Ohlén J, Odén A, Gaston-Johansson F. Experience and predictors of symptoms, distress and health-related quality of life over time in postmenopausal women with recurrent breast cancer. Psycho-Oncology. (2008) 17:497–505. doi: 10.1002/pon.1258
7. Trudel-Fitzgerald C, Savard J, Ivers H. Which symptoms come first? Exploration of temporal relationships between cancer-related symptoms over an 18-month period. Ann Behav Med. (2013) 45:329–37. doi: 10.1007/s12160-012-9459-1
8. Ho SY, Rohan KJ, Parent J, Tager FA, McKinley PS. A longitudinal study of depression, fatigue, and sleep disturbances as a symptom cluster in women with breast cancer. J Pain Symptom Manag. (2015) 49:707–15. doi: 10.1016/j.jpainsymman.2014.09.009
9. Sanford SD, Beaumont JL, Butt Z, Sweet JJ, Cella D, Wagner LI. Prospective longitudinal evaluation of a symptom cluster in breast cancer. J Pain Symptom Manag. (2014) 47:721–30. doi: 10.1016/j.jpainsymman.2013.05.010
10. Al Qadire M, Alsaraireh M, Alomari K, Aldiabat KM, Al-Sabei S, Al-Rawajfah O, et al. Symptom clusters predictive of quality of life among Jordanian women with breast cancer. Semin Oncol Nurs. (2021) 37:151144. doi: 10.1016/j.soncn.2021.151144
11. Howell D, Molloy S, Wilkinson K, Green E, Orchard K, Wang K, et al. Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol. (2015) 26:1846–58. doi: 10.1093/annonc/mdv181
12. Rothrock NE, Cook KF, O'Connor M, Cella D, Smith AW, Yount SE. Establishing clinically-relevant terms and severity thresholds for Patient-Reported Outcomes Measurement Information System® (PROMIS®) measures of physical function, cognitive function, and sleep disturbance in people with cancer using standard setting. Qual Life Res. (2019) 28:3355–62. doi: 10.1007/s11136-019-02261-2
13. Choi EPH, Huang J, Chau PH, Wan EYF. Health-related quality of life among Chinese primary care patients with different lower urinary tract symptoms: a latent class analysis. Qual Life Res. (2021) 30:1305–15. doi: 10.1007/s11136-020-02731-y
14. Song QK Li J, Huang R., Fan JH, Zheng RS, Zhang BN, et al. Age of diagnosis of breast cancer in china: almost 10 years earlier than in the United States and the European Union. Asian Pac J Cancer Prev. (2014) 15:10021–5. doi: 10.7314/APJCP.2014.15.22.10021
15. Rimehaug SA, Kaat AJ, Nordvik JE, Klokkerud M, Robinson HS. Psychometric properties of the PROMIS-57 questionnaire, Norwegian version. Qual Life Res. (2022) 32:269–80. doi: 10.1007/s11136-021-02906-1
16. Cai T, Fu L, Huang Q, Yu C, Yang Y, Ni F., Yuan C. Validity and reliability of the Chinese version of the patient-reported outcomes measurement information system adult profile-57 (PROMIS-57). Health Qual Life Out. (2022) 20:1–12. doi: 10.1186/s12955-022-01997-9
17. Valentine TR, Weiss DM, Jones JA, Andersen BL. Construct validity of PROMIS® Cognitive Function in cancer patients and noncancer controls. Health Psychol. (2019) 38:351–8. doi: 10.1037/hea0000693
18. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. (2007) 14:535–69. doi: 10.1080/10705510701575396
19. Kyranou M, Puntillo K, Dunn LB, Aouizerat BE, Paul SM, Cooper BA, et al. Predictors of initial levels and trajectories of anxiety in women before and for 6 months after breast cancer surgery. Cancer Nurs. (2014) 37:406–17. doi: 10.1097/NCC.0000000000000131
20. Li J, Zhang H, Shao D, Xue JM, Bai H, Sun JW, et al. Depressive symptom clusters and their relationships with anxiety and posttraumatic stress disorder symptoms in patients with cancer: the use of latent class analysis. Cancer Nurs. (2019) 42:388–95. doi: 10.1097/NCC.0000000000000624
21. Fox RS, Ancoli-Israel S, Roesch SC, Merz EL, Mills SD, Wells KJS, et al. Sleep disturbance and cancer-related fatigue symptom cluster in breast cancer patients undergoing chemotherapy. Support Care Cancer. (2020) 28:845–55. doi: 10.1007/s00520-019-04834-w
22. Tang V, Zhao S, Boscardin J, Sudore R, Covinsky K, Walter LC, et al. Functional status and survival after breast cancer surgery in nursing home residents. JAMA Surg. (2018) 153:1090–6. doi: 10.1001/jamasurg.2018.2736
23. Mitra S, Gao Q, Chen W, Zhang Y. Health, work, and income among middle-aged and older adults: a panel analysis for China. J Econ Ageing. (2020) 21:376. doi: 10.1016/j.jeoa.2020.100255
24. Mols F, Tomalin B, Pearce A, Kaambwa B, Koczwara B. Financial toxicity and employment status in cancer survivors: a systematic literature review. Support Care Cancer. (2020) 28:5693–708. doi: 10.1007/s00520-020-05719-z
25. Zahnd WE, Davis MM, Rotter JS, Vanderpool RC, Perry CK, Shannon J, et al. Rural-urban differences in financial burden among cancer survivors: an analysis of a nationally representative survey. Support Care Cancer. (2019) 27:4779–86. doi: 10.1007/s00520-019-04742-z
26. Jing J, Feng R, Zhang X, Li M, Gao J. Financial toxicity and its associated patient and cancer factors among women with breast cancer: a single-center analysis of low-middle income region in China. Breast Cancer Res Treat. (2020) 181:435–43. doi: 10.1007/s10549-020-05632-3
27. Browall M, Brandberg Y, Nasic S, Rydberg P, Bergh J, Rydén A, et al. A prospective exploration of symptom burden clusters in women with breast cancer during chemotherapy treatment. Support Care Cancer. (2017) 25:1423–9. doi: 10.1007/s00520-016-3527-1
28. Ng T, Dorajoo SR, Cheung YT, Lam YC, Yeo HL, Shwe M, et al. Distinct and heterogeneous trajectories of self-perceived cognitive impairment among Asian breast cancer survivors. Psychooncology. (2018) 27:1185–92. doi: 10.1002/pon.4635
29. Bødtcher H, Bidstrup PE, Andersen I, Christensen J, Mertz BG, Johansen C, et al. Fatigue trajectories during the first 8 months after breast cancer diagnosis. Qual Life Res. (2015) 24:2671–9. doi: 10.1007/s11136-015-1000-0
30. Mandelblatt J, Clapp J, Luta G, Faul LA, Tallarico MD, McClendon TD, et al. Long-term trajectories of self-reported cognitive function in a cohort of older breast cancer survivors. Cancer. (2016) 122:3555–63. doi: 10.1002/cncr.30208
31. Xu Z, Luo F, Wang Y, Zou B, Man Y, Liu JS, et al. Cognitive impairments in breast cancer survivors treated with chemotherapy: a study based on event-related potentials. Cancer Chemother Pharmacol. (2020) 5:61–7. doi: 10.1007/s00280-019-03994-0
32. Zhang W, Sun H, Li X. The Association between chronic conditions and non-agricultural work productivity loss among the middle-aged Chinese population. J Occup Environ Med. (2018) 60:832–8. doi: 10.1097/JOM.0000000000001348
33. Zeng Y, Cheng ASK, Feuerstein M. Cognitive limitations at work among employed breast cancer survivors in China. Rehabil Nurs. (2017) 42:347–53. doi: 10.1002/rnj.279
34. Junghaenel DU, Cohen J, Schneider S, Neerukonda AR, Broderick JE. Identification of distinct fatigue trajectories in patients with breast cancer undergoing adjuvant chemotherapy. Support Care Cancer. (2015) 23:2579–87. doi: 10.1007/s00520-015-2616-x
Keywords: breast cancer, chemotherapy, heterogeneity, latent class analysis, patient-reported outcomes
Citation: Cai T, Zhou T, Yuan C, Yu C, Ni F and Sheng Z (2022) Heterogeneity of symptoms and functions among women receiving chemotherapy for breast cancer in China: A multicentre, cross-sectional study. Front. Public Health 10:952710. doi: 10.3389/fpubh.2022.952710
Received: 25 May 2022; Accepted: 15 July 2022;
Published: 03 August 2022.
Edited by:
Zeng-Jie Ye, Guangzhou University of Chinese Medicine, ChinaReviewed by:
Mustafa Bayraktar, Atatürk University, TurkeyCopyright © 2022 Cai, Zhou, Yuan, Yu, Ni and Sheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiren Sheng, c2hlbmd6aGlyZW45MEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.