
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 October 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.951544
This article is part of the Research Topic Mental Health Promotion and Protection View all 34 articles
Background: Low prescription rates of antipsychotic long-acting injections (LAIs) may be a major challenge in the prevention and treatment of schizophrenia. However, there are few studies on the usage and attitude toward LAIs among community-based patients with schizophrenia.
Methods: A large community-based cross-sectional investigation was conducted among 6,336 patients with schizophrenia from Shanghai, China from March 1 to June 30, 2021. The structured Attitude and Status toward Treatment of Community Patients with Schizophrenia Questionnaire (AST-CSQ) was used to investigate the attitude and influencing factors of community-dwelling patients with schizophrenia toward LAIs.
Results: Among the 6,336 participants, the average age was 49.28 ± 11.23. The rate of agreement to LAI antipsychotics among participants was 3.16% (n = 200). The family financial resources, care ability, and disease course of the LAIs group were less than those of the non-LAIs group. However, the LAIs group had higher immediate family guardianship, social activity, previous hospitalization, number of hospitalization, outpatient adherence, previous antipsychotic use, antipsychotic adherence, and attitude toward oral antipsychotics than the non-LAIs group, with significant differences between the two groups (p < 0.05). Furthermore, age (β = −0.036, OR 0.964, 95% CI 0.947–0.982), marital status (β = 0.237, OR 1.267, 95% CI 1.002–1.602), care ability (β = 0.709, OR 2.032, 95% CI 1.437–2.875), outpatient adherence (β = −0.674, OR 0.510, 95% CI 0.358–0.725), antipsychotic adherence (β = 0.920, OR 2.509, 95% CI 1.092–5.764), and attitude toward oral antipsychotics (β = −1.357, OR 0.258, 95% CI 0.103–0.646) were significant predictors of attitude toward LAI antipsychotics (p < 0.05).
Conclusions: The community-dwelling patients with schizophrenia in China had a low willingness to use LAIs. Patients of a younger age, more hospitalizations, and a shorter course of disease were prone to be more willing to accept LAIs. The patients' age, marital status, care ability, outpatient adherence, antipsychotic adherence, and attitude toward oral antipsychotics were important predictor of patients' attitudes toward LAIs. Under the global deinstitutionalized management model of mental disorders, these results highlight an urgent problems for public mental health service providers and policy-makers and provide more solutions for them.
The prevention of relapse and hospitalization in individuals with schizophrenia is a major public mental health challenge (1). To date, the problems of multiple relapses in the course of schizophrenia are difficult to solve and have attracted extensive attention worldwide (2, 3). According to a WHO report in 2018, the number of patients with schizophrenia in the world reached 24 million, with a prevalence of 3.8 to 8.4 ‰ and a 10-year recurrence rate of 75% (4). In Europe, estimates of the excess costs of relapse in schizophrenia range from $8665 to 18,676 over periods of 6–12 months, while in the US, it can reach $16,000 to 33,000 over a period of 6–15 months (5). Most studies have shown that poor treatment adherence has become an important factor in multiple relapses of schizophrenia (6, 7).
Long-acting injectable (LAI) antipsychotics have been shown to improve treatment adherence in patients with schizophrenia and decrease the rate of relapse and hospitalization, which makes them superior to their oral counterparts in this regard (8). LAIs are a new medical controlled-release technology that can reduce the number of times patients take medicine, so they can effectively improve medication adherence (9). Subotnik et al. (10) showed that the relapse rate and/or psychotic exacerbation of first episode of schizophrenia was lower for the LAIs group than for the oral group, and the relative risk was reduced by 84.7%. A meta-analysis of 147 studies suggests that LAIs are more beneficial than oral antipsychotics in terms of insight, efficacy, effectiveness, safety and quality of life (11).
However, the clinical use rate of LAIs has not reached expectations, especially for community-dwelling patients with schizophrenia, which puts forward new problems for public mental health (12). In European countries, the second-generation antipsychotic LAI prescription rate is lower than 30%, while that in the United States is only 10% (13). The limited use of LAIs appears to be related to the negative attitudes of clinicians and inpatients toward this treatment (14). A total of 17.6% of physicians declared feeling more pressure to offer LAI antipsychotics than oral antipsychotics (15). Most patients believed that LAIs were less effective, more expensive and had more serious side effects than oral antipsychotics (16).
At present, there are few studies on the usage of and attitude toward LAIs among community-dwelling patients with schizophrenia. We do not know the factors related to the low use of LAIs in community-dwelling patients. According to the data of the mental health center of the Chinese Center for Disease Control and Prevention, the number of patients with schizophrenia in China has exceeded 6.4 million (17). In the future, the rehabilitation of schizophrenia will be gradually deinstitutionalized and the community rehabilitation model will be realized (18). This large community-based cross-sectional investigation explored the attitude and influencing factors of Chinese community-dwelling patients with schizophrenia toward LAIs.
This study was conceptualized as a community-based cross-sectional investigation. It was conducted by the Mental Health subcentre of Shanghai Pudong New Area Center for Disease Control and Prevention, Shanghai Pudong New Area Mental Health Center, Tongji University School of Medicine, which has been dedicated to fully functioning community mental health prevention and research since 2010. The sample size of the study was calculated using the PASS version 21.0.3 (NCSS LLC, Utah, USA), a sample size and power analysis software. Taking the significance level (α) was 0.05, the confidence level (1-α) was 0.95, the allowable error (δ) was 0.03, and the proportion (p) was 0.5, and the calculated sample size was 1,098. Considering the special population, the loss rate was set at 40%, the calculated sample size was at least 1,830. A total of 10,305 paper informed consent forms and questionnaires were distributed to patients with schizophrenia in 23 residential districts and 32 community health service centers in Pudong New Area, Shanghai. A total of 6,336 individuals agreed to participate in and complete the questionnaires from March 1 to June 30, 2021. The attrition rate of participants was 38.52%. This study was ethically reviewed by the Research Ethics Committee of the Shanghai Pudong New Area Mental Health Center and Tongji University Mental Health Center.
All participants were community-based psychiatric patients from Pudong New Area, Shanghai from March 1 to June 30, 2021. The following inclusion criteria were employed: (1) patients meeting the DSM-5 (19) diagnostic criteria for schizophrenia; (2) age ≤ 65 years old; (3) certain visual and auditory resolution without cognitive disorders; (4) currently living in the community and not hospitalized; and (5) both the participants and guardians agreed to participate in the investigation and signed the informed consent. The following exclusion criteria were employed: (1) severe visual or hearing impairment, physical disability, extracranial trauma or history of surgery; (2) obvious excitement impulse, serious negativity, self-harm or suicidal ideation; (3) dementia or developmental delay diagnosed as behavioral disorder; and (4) participants or guardians who did not sign the informed consent form, or withdrew halfway.
This investigation was conducted using the self-made AST-CSQ. To ensure the quality and rationality of the survey, three measures were taken to finalize the questionnaire. First, referring to the Medication Adherence Rating Scale (MARS) (20, 21), Drug Attitude Inventory (DAI) (22), and Multidimensional Scale of Perceived Social Support (MSPSS) (23), the expert consultation determined the questionnaire items. Second, after three rounds of expert committee argumentation, the first version of the questionnaire is determined. Third, the revised version of the questionnaire were determined according to the pre- survey problems. The expert committee consisted of four psychiatrists, four public health experts, two psychopharmacologists, one health economists, and one health statistician.
The structured AST-CSQ was used to investigate the attitude and status toward treatment of community patients with schizophrenia. The questionnaire consists of four sections and twenty questions (Table 1). The first part is demographic characteristics, including age, gender, marriage, residence, education, and occupation. The second part deals with the social support of the respondents, including economic status, medical expenses, guardians, care ability, and social activities. The third part is related to the treatment experience, including course of disease, number of episodes, inpatient or outpatient experience. The last part focuses on attitude toward oral and long-acting injectable antipsychotics (24). In addition, attitudes toward antipsychotics refer to agreement or disagreement to receive oral or long-acting injectable antipsychotics. The questionnaire was completed by 32 community psychiatric public health physicians through face-to-face interviews with respondents. All investigators were trained for consistency.
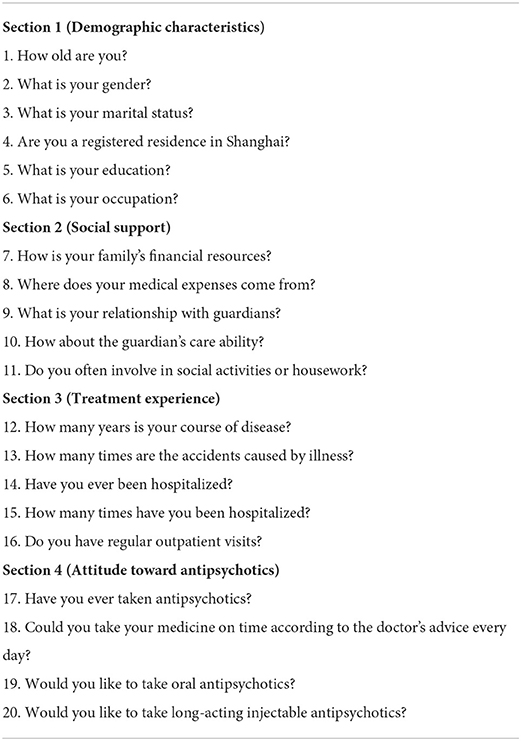
Table 1. Attitude and status toward treatment of community patients with schizophrenia questionnaire (AST-CSQ).
Data were analyzed using SPSS version 25.0 statistical software (SPSS, Inc., Chicago, IL, USA). We first identified the patients' attitude acceptance rate of LAIs and divided them into an LAIs group and a non-LAIs group. Descriptive analysis was performed for sociodemographic data. All continuous variables are first tested for normality, and the variables with normal distribution were described by the mean mean ± standard deviation. The continuous variables were compared between groups using the independent samples t test. For classified data, the frequency (percentage) was used for statistical description, and the chi-square (χ2) test was used for intergroup comparison. Binary logistic regression analysis was used to explore the predictors of influencing factors for attitude toward LAI antipsychotics. The difference was statistically significant at p < 0.05.
The demographic characteristics of community-based patients with schizophrenia, including age, gender, marital status, residence, education and occupation, are shown in Section Demographic characteristics of Table 2. Among the 6,336 participants, the average age was 49.28±11.23 years, and the proportion of females was higher (52.53%). In addition, most of the respondents were unmarried (50.45%), registered a residence in the city (96.65%), had a junior high school education (43.58%), and were unemployment (52.10%). Respondents of the LAIs group were younger and less employed than those of the non-LAIs group, and there were significant difference between the two groups (p < 0.001). But there was no significant difference in other control variables of demographic characteristics (p > 0.05).
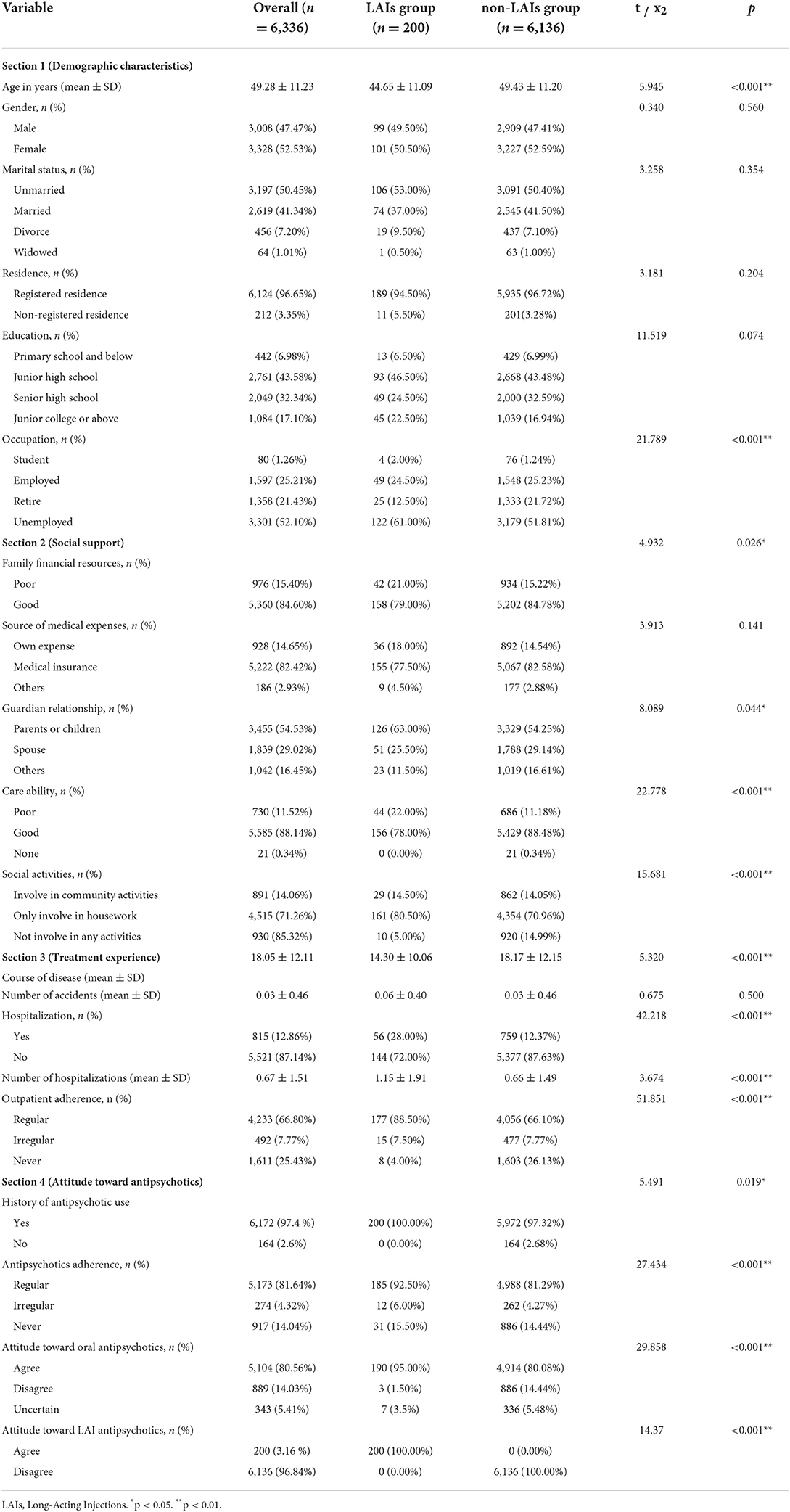
Table 2. Demographic characteristics, social support, treatment experience, and attitude toward antipsychotics of participants.
The social support, treatment experience, and attitude toward antipsychotics among participants from the overall and the two groups in this study are reported in Section Social support to Attitude toward antipsychotics of Table 2. The rate of agreement to LAI antipsychotics among participants was 3.16% (n = 200), and there was a significant difference between the two groups (χ2 = 14.37, p < 0.001). The family financial resources, care ability, and disease course of the LAIs group were less than those of the non-LAIs group, and there were significant differences between the two groups (p < 0.05). However, the LAIs group had higher immediate family guardianship, social activity, previous hospitalization, number of hospitalization, outpatient adherence, previous antipsychotic use, antipsychotic adherence, and attitude toward oral antipsychotics than the non-LAIs group, with significant differences between the two groups (p < 0.05). There was no significant difference in the source of medical expenses and the number of accidents (p > 0.05).
The independent variables were different influencing factors of treatment attitude among community-based patients with schizophrenia; attitude toward LAI antipsychotics was the dependent variable for binary logistic regression analysis (Table 3). Age (β = −0.036, OR 0.964, 95% CI 0.947–0.982), marital status (β = 0.237, OR 1.267, 95% CI 1.002–1.602), care ability (β = 0.709, OR 2.032, 95% CI 1.437–2.875), outpatient adherence (β = −0.674, OR 0.510, 95% CI 0.358–0.725), antipsychotic adherence (β = 0.920, OR 2.509, 95% CI 1.092–5.764), and attitude toward oral antipsychotics (β = −1.357, OR 0.258, 95% CI 0.103–0.646) were significant predictors of attitude toward LAI antipsychotics (p < 0.05).
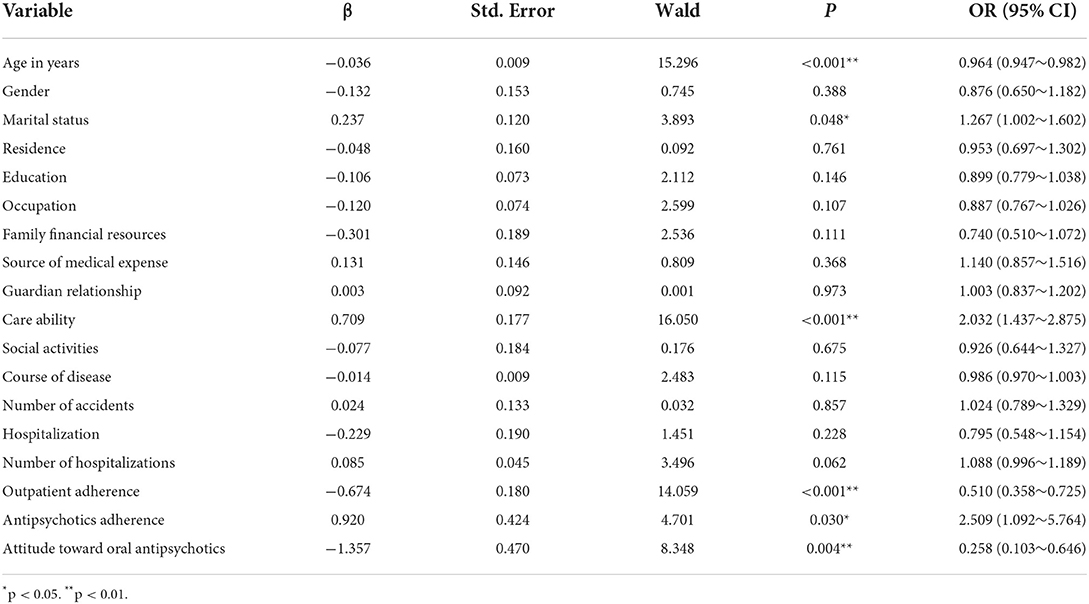
Table 3. Binary logistic regression analysis of different influencing factors on attitude toward LAIs.
We examined the attitude and influencing factors of community-based patients with schizophrenia toward LAIs by the AST-CSQ, which is based on a large community-based cross-sectional investigation. To date, our study is the largest survey of community patients-dwelling with schizophrenia, and it can address the relevant factors of patients' attitudes toward LAIs more comprehensively, which is an original research direction. We found that Chinese community-based patients with schizophrenia had a low willingness to use LAIs, only 3.16%. There is a huge gap, with a 30% prescription rate of LAIs in the clinical setting of European countries and an 18.2% utilization rate for outpatients in Japan (13, 25). Regarding attitudes toward oral antipsychotics, 80.56% of the participants agreed with their use. This is also similar to the results of a study conducted by Grover et al. (26), 78.8% of patients in India are still willing to choose oral tablets.
On the other hand, this study also found that there were significant differences in age, hospitalization, and course of disease between the LAIs group and the non-LAIs group, that is, patients of a younger age, more hospitalizations, and a shorter course of disease were prone to be more willing to accept LAIs. This may be related to the high demand for social function recovery of patients or guardians of a younger age, more hospitalizations, or a short course of disease and their obvious desire to reduce recurrence (27). In contrary, older patients with schizophrenia suffer from long-term disease, and their social function and insight are greatly damaged, which seriously affects their expectation of the efficacy of LAIs. These results were consistent with the study of Xiao et al. (28). Perhaps this suggests that it is necessary to develop a personalized intervention plan for the population of this age and disease course structure and carry out targeted medication guidance (29).
Furthermore, the attitude toward and willingness to use LAIs of community-based patients with schizophrenia will also be affected by the characteristics of family monitoring and the coexistence of disease outcome (30, 31). Our study showed that patients' age, marital status, care ability, outpatient adherence, antipsychotic adherence, and attitude toward oral antipsychotics were important predictor of patients' attitudes toward LAI antipsychotics. Consistent with the results of this study, Grover et al. found that patients with low antipsychotic adherence were less willing to accept LAI treatment (26). Interestingly, most studies have found that patients with poor care ability were more likely to choose LAI treatment (32). These patients hope to reduce the cost of monitoring by reducing the number of oral antipsychotics used (33, 34). The antipsychotic adherence of patients with antipsychotics directly affects their motivation and understanding in choosing LAIs (35, 36).
Understanding the attitudes and influencing factors of real-world community-dwelling patients toward LAIs and formulating targeted drug publicity plans may be an effective method for mental health control and prevention of schizophrenia in the future (37). Most previous studies were based on inpatients or outpatients with clinical schizophrenia. In contrast, our study was on a natural sample population of community-based patients (38). Because patients' attitudes toward LAIs are easily influenced by psychiatrists, this may lead to study bias (39). Grover et al. (40) suggested that psychiatrists' attitudes toward LAIs play an important role in the prescription rate of LAIs. Communicating and explaining according to the characteristics of different patients can effectively change their attitudes toward LAIs (41). In the context of deinstitutionalization of global mental disorder management, mental health managers and psychiatrists should participate together to optimize mental health management techniques and strengthen health education for patients with mental disorders in the community (42). This could form a more open relationship and stronger mutual trust to improve patients' support for long-term drugs and reduce the risk of disease recurrence.
We also note several limitations. First, we were unable to conduct a nationwide multicentre study because of the COVID-19 pandemic. Second, we did not expand the use of measurement tools to measure psychiatric symptoms or social support systems. Future studies should explore the final outcome of community-based patients with schizophrenia using oral antipsychotics and LAIs by a long-term longitudinal study. This could provide more treatment options for clinical psychiatrists or public health practitioners to prevent the recurrence of mental diseases.
In this study, community-dwelling patients with schizophrenia in China had a low willingness to use LAIs. Patients of a younger age, more hospitalizations, and a shorter course of disease were prone to be more willing to accept LAIs. The patients' age, marital status, care ability, outpatient adherence, antipsychotic adherence, and attitude toward oral antipsychotics were important predictor of patients' attitudes toward LAIs. Under the global deinstitutionalized management model of mental disorders, these results highlight an urgent problems for public mental health service providers and policy-makers and provide more solutions for them.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Research Ethics Committee of the Shanghai Pudong New Area Mental Health Center and Tongji University Mental Health Center (No. PDJWLL2019008). The patients/participants provided their written informed consent to participate in this study.
YF, HF, TJ, and LZ recruited participants and collected the data. QW recommended the scales used in the study. YS, JT, and YY completed the scales data entry, analyzed the data of scales, and wrote the manuscript. YY and QW designed the study and revised the paper. All authors have read and approved the manuscript.
This study was supported by grants from the following institutions: Shanghai Pudong New Area Science and Technology Development Fund (No. PKJ2021-Y78), Construction of characteristic disciplines of Public Mental Health of Shanghai Pudong New Area (No. PWYgts2021-01), and the Outstanding Clinical Discipline Project of Shanghai Pudong (No. PWYgy2021-02).
The authors would like to thank the Shanghai Pudong Municipal Commission of Health and Family Planning, the Outstanding Clinical Discipline Project of Shanghai Pudong for funding support. We would also like to thank Xudong Zhao, Chengping Hu, and Xirong Sun for their teaching and insight. The authors would also like to thank the participants that took part in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kane JM, Schooler NR, Marcy P, Correll CU, Achtyes ED, Gibbons RD, et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry. (2020) 77:1217–24. doi: 10.1001/jamapsychiatry.2020.2076
2. Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. (2013) 13:50. doi: 10.1186/1471-244X-13-50
3. Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. (2012) 139:116–28. doi: 10.1016/j.schres.2012.05.007
4. Schizophrenia. World Health Organization (2018). Available online at: http://www.who.int/mental_health/management/schizophrenia/en/
5. Pennington M, McCrone P. The cost of relapse in schizophrenia. Pharmacoeconomics. (2017) 35:921–36. doi: 10.1007/s40273-017-0515-3
6. Tiihonen J, Tanskanen A, Taipale H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am J Psychiatry. (2018) 175:765–73. doi: 10.1176/appi.ajp.2018.17091001
7. Spaniel F, Novak T, Bankovska Motlova L, Capkova J, Slovakova A, Trancik P, et al. Psychiatrist's adherence: a new factor in relapse prevention of schizophrenia. a randomized controlled study on relapse control through telemedicine system. J Psychiatr Ment Health Nurs. (2015) 22:811–20. doi: 10.1111/jpm.12251
8. Uchida H, Suzuki T, Takeuchi H, Arenovich T, Mamo DC. Low dose vs standard dose of antipsychotics for relapse prevention in schizophrenia: meta-analysis. Schizophr Bull. (2011) 37:788–99. doi: 10.1093/schbul/sbp149
9. Rubio JM, Schoretsanitis G, John M, Tiihonen J, Taipale H, Guinart D, et al. Psychosis relapse during treatment with long-acting injectable antipsychotics in individuals with schizophrenia-spectrum disorders: an individual participant data meta-analysis. Lancet Psychiatry. (2020) 7:749–61. doi: 10.1016/S2215-0366(20)30264-9
10. Subotnik KL, Casaus LR, Ventura J, Luo JS, Hellemann GS, Gretchen-Doorly D, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. a randomized clinical trial. JAMA Psychiatry. (2015) 72:822–9. doi: 10.1001/jamapsychiatry.2015.0270
11. Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry. (2021) 8:387–404. doi: 10.1016/S2215-0366(21)00039-0
12. Huang CY, Fang SC, Shao YJ. Comparison of long-acting injectable antipsychotics with oral antipsychotics and suicide and all-cause mortality in patients with newly diagnosed schizophrenia. JAMA Netw Open. (2021) 4:e218810. doi: 10.1001/jamanetworkopen.2021.8810
13. Patel MX, Haddad PM, Chaudhry IB, McLoughlin S, Husain N, David AS. Psychiatrists' use, knowledge and attitudes to first- and second-generation antipsychotic long-acting injections: comparisons over 5 years. J Psychopharmacol. (2010) 24:1473–82. doi: 10.1177/0269881109104882
14. Llorca PM, Bobes J, Fleischhacker WW, Heres S, Moore N, Bent-Ennakhil N, et al. Baseline results from the European non-interventional antipsychotic long acting injection in schizophrenia (ALTO) study. Eur Psychiatry. (2018) 52:85–94. doi: 10.1016/j.eurpsy.2018.04.004
15. Patel MX, Bent-Ennakhil N, Sapin C, di Nicola S, Loze JY, Nylander AG, et al. Attitudes of European physicians towards the use of long-acting injectable antipsychotics. BMC Psychiatry. (2020) 20:123. doi: 10.1186/s12888-020-02530-2
16. Lauriello J, Weiden PJ, Gleeson CD, Shah A, Boulanger L, Jariwala-Parikh K, et al. Real-world outcomes and costs following 6 months of treatment with the long-acting injectable (LAI) aripiprazole lauroxil for the treatment of schizophrenia. CNS Drugs. (2021) 35:1123–35. doi: 10.1007/s40263-021-00849-2
17. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
18. Krieger I, Bitan DT, Sharon-Garty R, Baloush-Kleinman V, Zamir L. The effect of community-based mental health rehabilitation services for schizophrenia: a retrospective cohort study. Psychiatr Q. (2020) 91:1453–63. doi: 10.1007/s11126-020-09772-z
19. Roehr B. American psychiatric association explains DSM-5. BMJ. (2013) 346:f3591. doi: 10.1136/bmj.f3591
20. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new medication adherence rating scale (MARS) for the psychoses. Schizophr Res. (2000) 42:241–7. doi: 10.1016/S0920-9964(99)00130-9
21. Fialko L, Garety PA, Kuipers E, Dunn G, Bebbington PE, Fowler D, et al. A large-scale validation study of the medication adherence rating scale (MARS). Schizophr Res. (2008) 100:53–9. doi: 10.1016/j.schres.2007.10.029
22. Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophr Bull. (1993) 19:609–18. doi: 10.1093/schbul/19.3.609
23. Dambi JM, Corten L, Chiwaridzo M, Jack H, Mlambo T, Jelsma J, et al. systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health Qual Life Outcomes. (2018) 16:80. doi: 10.1186/s12955-018-0912-0
24. Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. (2013) 74:957–65. doi: 10.4088/JCP.13r08440
25. Sugawara N, Kudo S, Ishioka M, Sato Y, Kubo K, Yasui-Furukori N. Attitudes toward long-acting injectable antipsychotics among patients with schizophrenia in Japan. Neuropsychiatr Dis Treat. (2019) 15:205–11. doi: 10.2147/NDT.S188337
26. Grover S, Sahoo S, Bn S, Malhotra N, Dua D, Avasthi A. Attitude and perceptions of patients towards long acting depot injections (LAIs). Asian J Psychiatr. (2019) 44:200–08. doi: 10.1016/j.ajp.2019.07.052
27. Kane JM, Schooler NR, Marcy P, Achtyes ED, Correll CU, Robinson DG. Patients with early-phase schizophrenia will accept treatment with sustained-release medication (long-acting injectable antipsychotics): results from the recruitment phase of the PRELAPSE trial. J Clin Psychiatry. (2019) 80:18m12546. doi: 10.4088/JCP.18m12546
28. Xiao L, Xie YFJPP, Remedies C. Influencing factors for medication adherence of patients with schizophrenia to paliperidone palmitate and its effect on the recurrence of schizophrenics. Pract Pharm Clin Remedie. (2019) 22:282–85.
29. Zhu J, Chen Y, Lu W, Huang Q, Li B, Xu Y, et al. Attitudes and willingness to accept long-acting injections for patients with schizophrenia in beijing: a cross-sectional investigation based on samples from the communities. Front Public Health. (2021) 9:770276. doi: 10.3389/fpubh.2021.770276
30. Lee Y, Lee MS, Jeong HG, Youn HC, Kim SH. Medication adherence using electronic monitoring in severe psychiatric illness: 4 and 24 weeks after discharge. Clin Psychopharmacol Neurosci. (2019) 17:288–96. doi: 10.9758/cpn.2019.17.2.288
31. Nagai N, Tani H, Yoshida K, Gerretsen P, Suzuki T, Ikai-Tani S, et al. Drug attitude, insight, and patient's knowledge about prescribed antipsychotics in schizophrenia: a cross-sectional survey. Neuropsychiatr Dis Treat. (2020) 16:781–87. doi: 10.2147/NDT.S240377
32. Jaeger M, Rossler W. Attitudes towards long-acting depot antipsychotics: a survey of patients, relatives and psychiatrists. Psychiatry Res. (2010) 175:58–62. doi: 10.1016/j.psychres.2008.11.003
33. Ascher-Svanum H, Peng X, Faries D, Montgomery W, Haddad PM. Treatment patterns and clinical characteristics prior to initiating depot typical antipsychotics for nonadherent schizophrenia patients. BMC Psychiatry. (2009) 9:46. doi: 10.1186/1471-244X-9-46
34. Dolder CR, Lacro JP, Dunn LB, Jeste DV. Antipsychotic medication adherence: is there a difference between typical and atypical agents? Am J Psychiatry. (2002) 159:103–8. doi: 10.1176/appi.ajp.159.1.103
35. Rauch AS, Fleischhacker WW. Long-acting injectable formulations of new-generation antipsychotics: a review from a clinical perspective. CNS Drugs. (2013) 27:637–52. doi: 10.1007/s40263-013-0083-9
36. Chan HW, Huang CY, Yen YC. Clinical outcomes of paliperidone long-acting injection in patients with schizophrenia: a 1-year retrospective cohort study. BMC Psychiatry. (2021) 21:507. doi: 10.1186/s12888-021-03513-7
37. Sathienluckana T, Tiangpattanawong P, Chaiyasukthananoan K, Jittayanan P, Sawetwangsing H, Puchsaka P. Comparison of efficacy and safety between long-acting injectable antipsychotic monotherapy and combination of long-acting injectable and oral antipsychotics in patients with schizophrenia. Schizophr Res Treatment. (2021) 2021:8403986. doi: 10.1155/2021/8403986
38. Lindenmayer JP, Glick ID, Talreja H, Underriner M. Persistent barriers to the use of long-acting injectable antipsychotics for the treatment of schizophrenia. J Clin Psychopharmacol. (2020) 40:346–49. doi: 10.1097/JCP.0000000000001225
39. Guinart D, Taipale H, Rubio JM, Tanskanen A, Correll CU, Tiihonen J, et al. Risk factors, incidence, and outcomes of neuroleptic malignant syndrome on long-acting injectable vs oral antipsychotics in a nationwide schizophrenia cohort. Schizophr Bull. (2021) 47:1621–30. doi: 10.1093/schbul/sbab062
40. Grover S, Sahoo S, Mehra A. Perceptions of psychiatrists toward the use of long-acting injectable antipsychotics: an online survey study from India. J Clin Psychopharmacol. (2019) 39:611–19. doi: 10.1097/JCP.0000000000001109
41. Ciglar M, Bjedov S, Maleković H. Attitudes of croatian psychiatrists towards long-acting injectable antipsychotics. Psychiatr Danub. (2016) 28:273–77.
Keywords: long-acting injections, LAIs, schizophrenia, community, China
Citation: Sun Y, Tong J, Feng Y, Fang H, Jiang T, Zhao L, Wang Q and Yang Y (2022) Attitude and influencing factors of patients with schizophrenia toward long-acting injections: A community-based cross-sectional investigation in China. Front. Public Health 10:951544. doi: 10.3389/fpubh.2022.951544
Received: 24 May 2022; Accepted: 22 September 2022;
Published: 10 October 2022.
Edited by:
Harshavardhan Sampath, Sikkim Manipal University, IndiaReviewed by:
Hiroyoshi Takeuchi, Keio University School of Medicine, JapanCopyright © 2022 Sun, Tong, Feng, Fang, Jiang, Zhao, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Yang, eWFuZ3lAc2hzcGRqdy5jb20=; Qiang Wang, MTM1MjQxMTQ4MjhAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.