- 1Department of Nutrition Hygiene and Toxicology, School of Public Health, Medical College, Academy of Nutrition and Health, Wuhan University of Science and Technology, Wuhan, China
- 2Wuhan Centers for Disease Prevention and Control, Wuhan, China
- 3Wuhan Municipal Health Commission, Wuhan, China
Objective: This study aimed to examine the relationship between social support and its sub-domains and cognitive performance, and the association with cognitive impairment among older adults in China.
Design: A cross-sectional study.
Setting and participants: We included 865 community-based individuals aged 65 and above from Hubei province, China.
Methods: The level of social support was evaluated using the social support rating scale (SSRC). The Mini-Mental State Examination was adopted to assess cognitive function, and its cut-offs were used to determine cognitive impairment among the participants. Multiple linear regression models and logistic regression models were used to estimate the β and odds ratios (ORs) and their 95% CIs, respectively.
Results: The participants were divided into quartiles 1–4 (Q1–Q4), according to the total scores of SSRC. After adjusting for sociodemographic characteristics, lifestyle factors, and history of diseases, for MMSE scores, compared to these in Q1, the β of Q2–Q4 were −0.22 (−0.88, 0.43), 0.29 (−0.35, 0.94), and 0.86 (0.19, 1.53), respectively; For cognitive impairment, the ORs of Q2–Q4 were 1.21 (0.80, 1.82), 0.62 (0.40, 0.94), and 0.50 (0.32, 0.80), respectively. Considering SSRC scores as the continuous variable, per 1-unit increase, the β was 0.05 (0.02, 0.09) for the cognitive score, and the OR was 0.95 (0.92, 0.98) for cognitive impairment. In addition, higher levels of both subjective support and support utilization were related to better MMSE performance and lower risks of cognitive impairment.
Conclusion and implications: Among the older adults in China, as expected, there is a positive relationship between social support and cognitive performance, and high levels of social support, particularly in support utilization, were related to low risks of cognitive impairment. More social support should be provided in this population to improve cognitive function and reduce the risks of cognitive impairment.
Introduction
With the rapid aging of the population over the world, the diseases of cognitive impairment, including mild cognitive impairment (MCI) and dementia, are causing a tremendous burden on the economy and health (1, 2). MCI is a disorder characterized by impairment of memory, learning difficulties, and reduced ability to concentrate on a task for more than brief periods, and has a high risk of progressing to dementia (3). It is estimated that there are 15.07 million people with dementia and 38.77 million people with MCI in China (4). Given no effective treatment for dementia, the efforts on modifiable influencing factors are important for improving cognitive function and preventing diseases of cognitive impairment among older adults.
For an individual, social support is the composition of material and spiritual support from various people and organizations, including family members, friends, neighbors, colleagues, and governmental and non-governmental organizations. Given that the resources to keep alive, such as food, daily supplies, and emotional support, largely depend on the family members and other for older adults, social support may play a crucial role in the health outcomes of older adults. In addition, a previous study showed that common comorbidities, such as hypertension, diabetes, glycemic variability, and dyslipidemia were linked to cognitive decline (5–7). Social support in the older adult may be beneficial to controlling blood pressure and lipids well and keeping blood glucose stable (8–11). Several studies have explored the associations of emotional and instrumental support with cognitive function and brain image among adults in the US (12–15), UK (16), Dutch (17), Mexican (18), and South Africa (19). The results from these studies (12–23) were conflicting due to the heterogeneities in study design, sample size, and study population. In addition, social support was often divided into different aspects (24), such as objective support from living materials, subjective support from emotional networks, and support utilization indicating the ability to get others' support. However, there were limited studies investigating the relationship between social support and cognition in China.
In this study, by a specialized questionnaire for assessing different aspects of social support, we conducted a cross-sectional study and examined the association of social support and its sub-domains with cognition among older adults aged 65 and above in China.
Methods
Study population and data collection
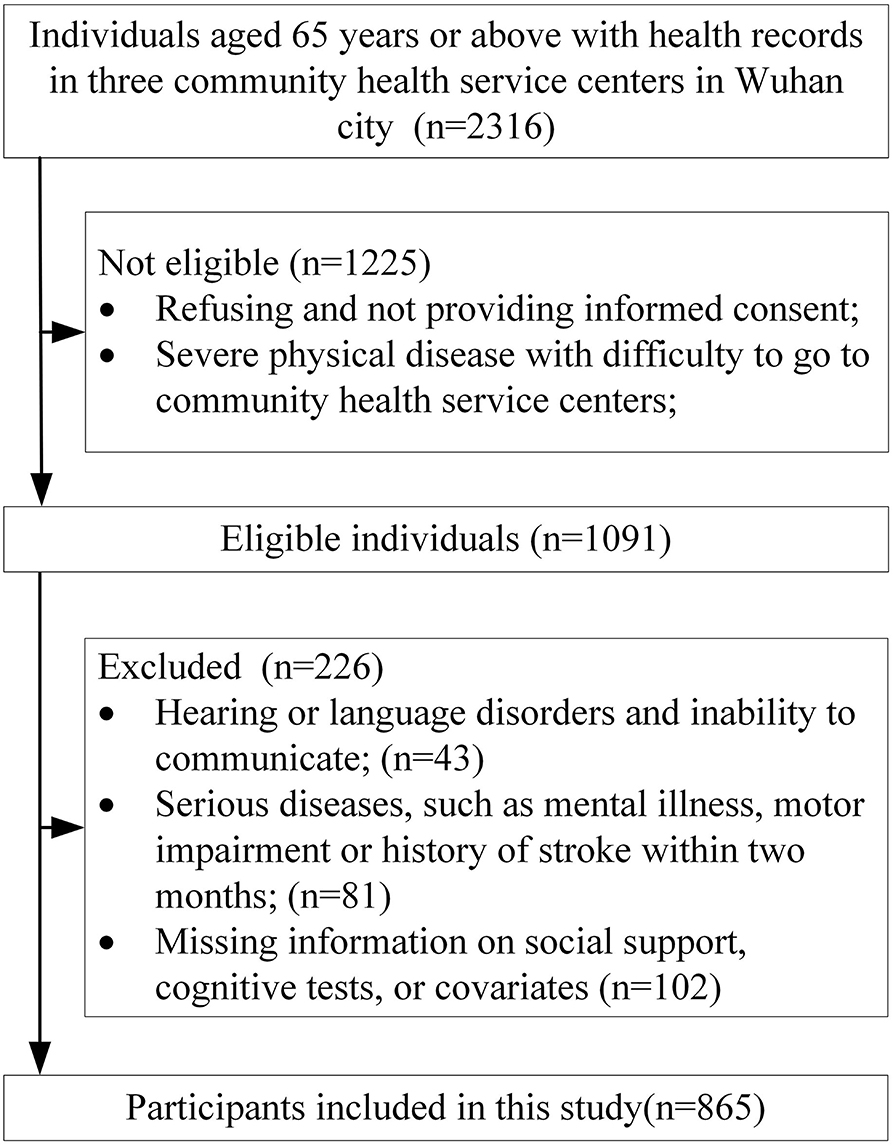
Participants were recruited from Wuhan city, China. Eligible participants aged 65 and above volunteered to participate in this study and could provide informed consent and did not have severe physical diseases and were able to go to community health service centers. The following exclusion criteria were applied: (1) Hearing or language disorders and inability to communicate. (2) Severe diseases, such as mental illness, motor impairment, or history of stroke within two months. (3) Missing information on social support, cognitive test, or other covariates. We used following method to calculate the sample size, n = Z a/2 2 * P * (1-P) / δ 2. According to previous studies (25, 26) on cognitive function among older adults in Hubei province, China, the prevalence of cognitive impairment was set as 25% in this study. In addition, Z a/2 was set as 1.96, δ (allowable error) was set as 3%, and the required sample size was calculated to be 800. Cluster sampling methods were used for the survey. We first performed random sampling methods to select three community health service centers in Wuhan city, the residents whose health records were registered in health service centers were recruited. With the inclusion and exclusion criteria, a total of 865 older adults aged 65 and above were used as the final analytic sample. The detailed flowchart was presented in Figure 1.
Baseline data on socio-demographic and background variables (including general demographic characteristics, lifestyle factors, and history of diseases) were collected using a self-made questionnaire. The interviewers underwent extensive training as well as periodic certification. One-to-one interview in a quiet room was employed to complete all questionnaires. This study was approved by the Medical Ethics Committee of Medical College, Wuhan University of Science and Technology (No. WUSTMC-201942). Written informed consent was obtained from all participants.
Assessment of cognitive function
Mini-Mental State Examination (MMSE) originated from Folstein et al. in 1975 (27), and has 13 items, including orientation, attention, language, immediate recall, delayed recall, and construction, and the scores range from 0 to 30 points. High scores indicate good cognitive performance. The Chinese version of MMSE was employed to assess the cognitive function of participants in this study. The previous study has shown good reliability (28) and validity (29) of the Chinese version of the Mini-Mental State Examination. According to a previous validation study on the Chinese version of MMSE (29), the cut-off points of dementia and MCI were set as 16/17 and 19/20 for illiteracy, 19/20 and 24/25 for primary school, and 23/24 and 27/28 for junior high school and above in this population. The participants screened with dementia and MCI were considered to be with cognitive impairment.
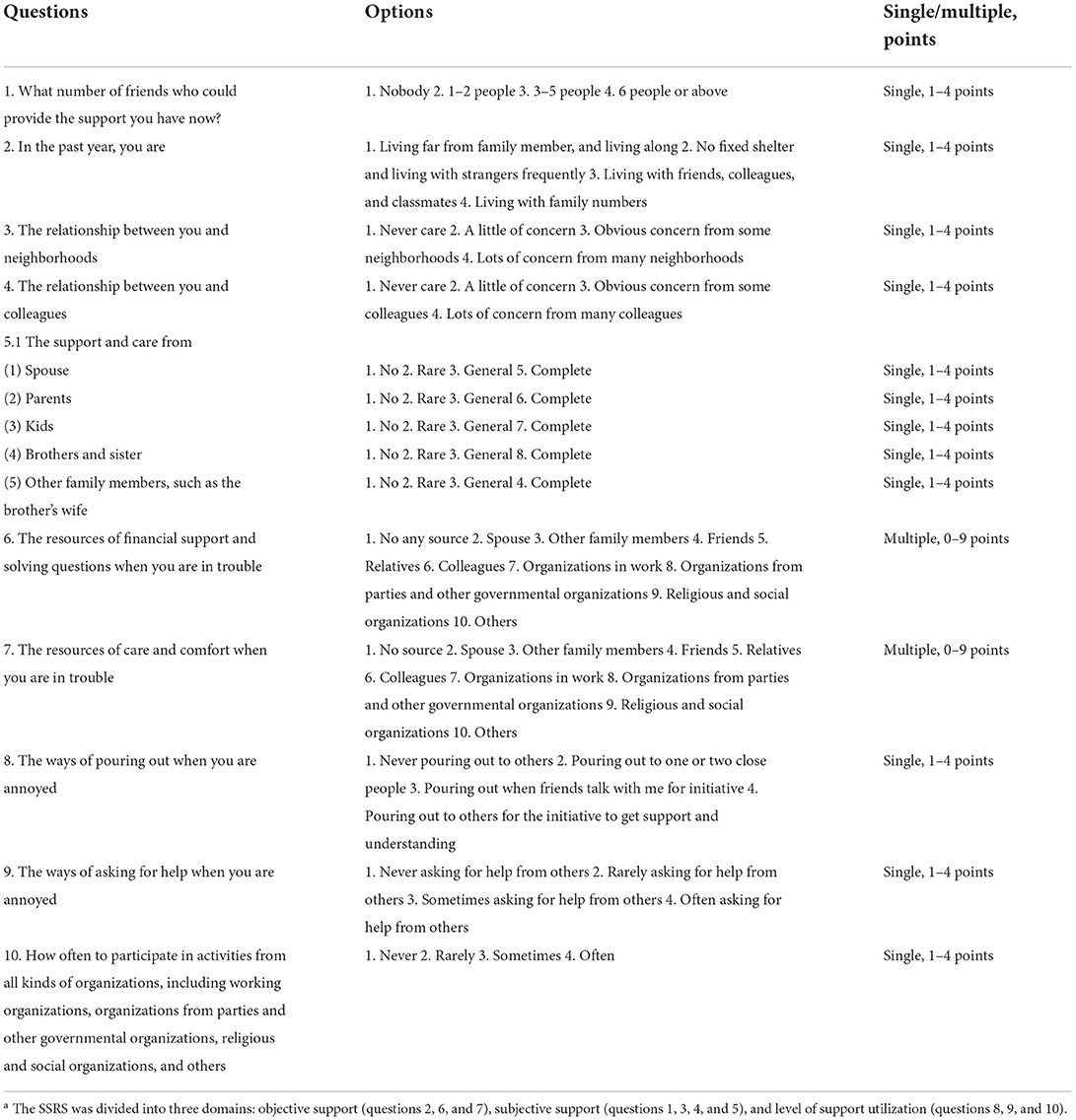
Measurement of social support score
The score of social support was measured by the social support rating scale (SSRS) (24). As shown in Table 1, the SSRS consists of three sub-domains such as objective support, subjective support, and support utilization, its total scores range from 12 to 66, and higher scores indicate better social support. Cronbach's a coefficient, split-half correlation coefficient, and test-retest correlation coefficient of SSRS were 0.821, 0.875, and 0.829, respectively, indicating high reliability (30). A previous study also showed high-construct validity and content validity (31). As a questionnaire to evaluate social support, SSRC has been widely accepted and used in epidemiological studies across China (32).
Socio-demographic characteristics, lifestyle factors, and history of diseases
According to the previous studies (33, 34), the socio-demographic characteristics, lifestyle factors, and history of diseases were considered covariates. Socio-demographic characteristics included age, sex, education level, and marital status. Education levels were divided into three categories: 0–6 years, 7–9 years, and ≥10 years. Marital status was categorized as married and non-married (single, divorced, or widowed). Lifestyle factors included smoking status and alcohol intake, which were defined as yes or no based on self-reported information. History of disease included obesity, hypertension, and diabetes. Body mass index (BMI) was calculated using weight to divide the square of height, and participants with a BMI < 18.5 kg/m2 were considered underweight, between 18.5 and 23.9 kg/m2 were considered normal, between 24 and 27.9 kg/m2 were considered overweight, and ≥ 28 kg/m2 were considered obese (35). Hypertension was defined as at least one of followed conditions: self-reported history of diagnosed hypertension, having anti-hypertension drugs or measured systolic blood pressure ≥140 mm Hg, or diastolic blood pressure ≥90 mm Hg (36). Diabetes was defined as at least one of the following conditions: self-reported history of diagnosed diabetes, having glucose-lowering medications or fasting blood glucose level of ≥7 mmol/L (37).
Statistical analysis
Differences between groups in demographic variables were examined using ANOVA analysis for continuous variables, and Pearson's chi-square test for categorical variables. Multiple linear regressions were performed to calculate the partial regression coefficient between the social support and MMSE scores. Unconditional logistic regression models were used to examine the association of social support with cognitive impairment by evaluating the odds ratio. Besides, the linear relationship and odds ratio between scores of three domains of social support were also examined. The covariates were controlled in model 1: adjusted for age and sex; model 2, further adjusted for education level, marriage, smoking, and drink; model 3, further adjusted for BMI categories, hypertension, and diabetes. All reported P–values were two-tail, and P < 0.05 was considered to be statistically significant. All statistical analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics of participants
The mean age in this study was 70.44 years old, and 53.18% were women. There were 264 participants with cognitive impairment, with a 30.52% of cognitive impairment prevalence. The demographic data and lifestyle factors were presented in Table 2 according to the participants with the quartiles 1–4 of social support scores. The participants with higher support scores were more likely to have lower age, higher MMSE scores, higher education levels, and be married. There was no significant difference in sex, smoking, drinking, BMI, hypertension, and diabetes among these groups.
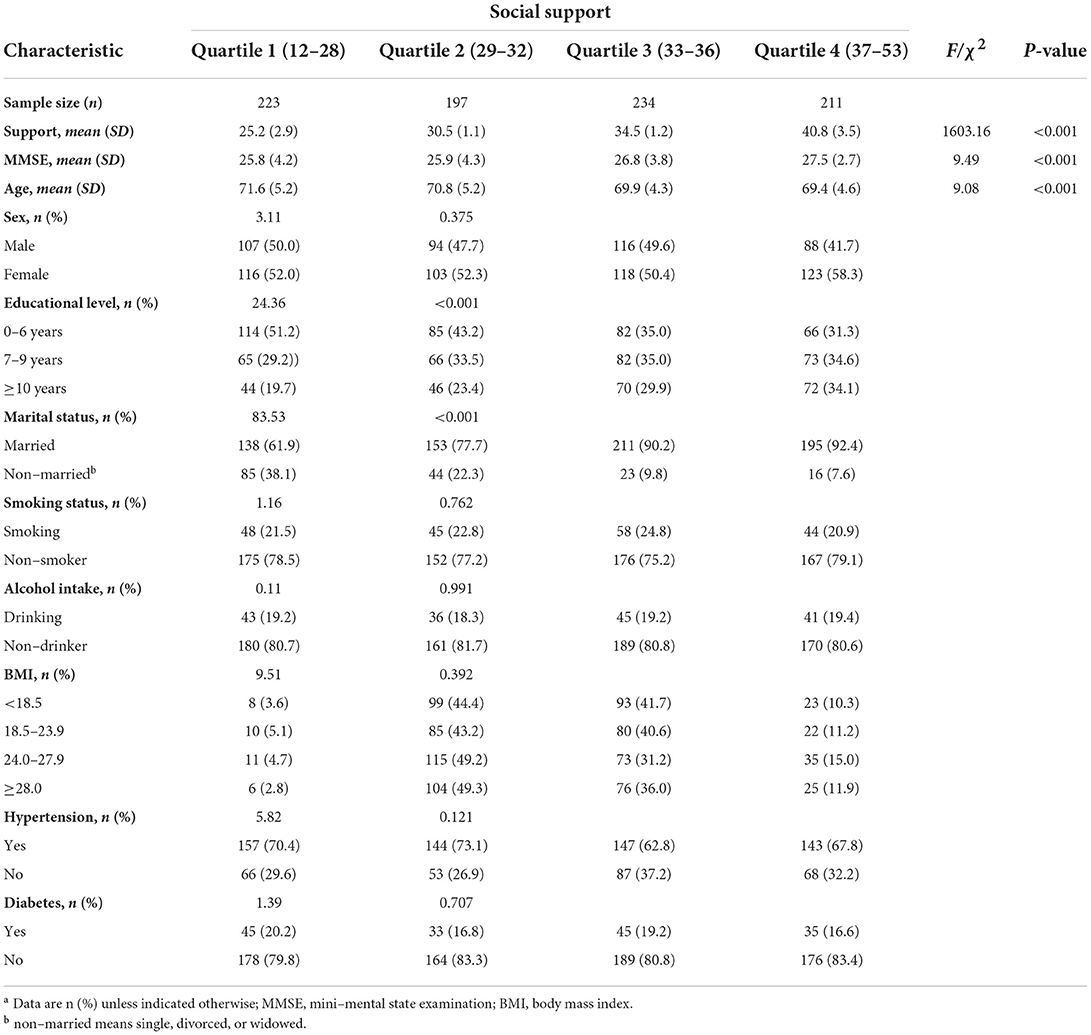
Table 2. Baseline characteristics of study population according to quartiles of social support scoresa.
The relationship between social support and cognitive function
As shown in Table 3, in multiple linear regression analysis of controlling the demographic characteristics, lifestyle, and history of diseases, compared to the participants with the lowest quartile of social support score (Q1), those with the highest quartile of social support score (Q4) was positively related to MMSE score (β = 0.86, 95% CI: 0.19, 1.53). The β for 1-unit increment of social support was 0.05 (95% CI: 0.02, 0.09; P < 0.001) for MMSE, showing a positive relationship between social support and MMSE scores. In addition, objective support and subjective support scores were not related to the MMSE scores. The support utilization score was positively related to MMSE scores, and the β was 0.14 (95% CI: 0.04, 0.24) for 1-unit increment (Table 4).
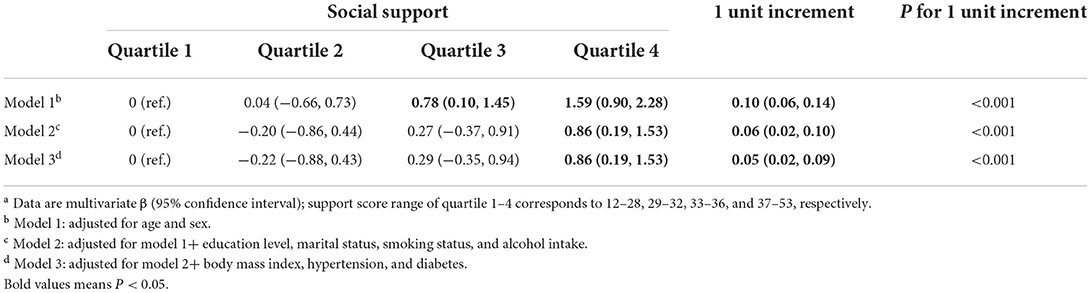
Table 3. Relationship between the social support and score in MMSE in multiple linear regression analysisa.
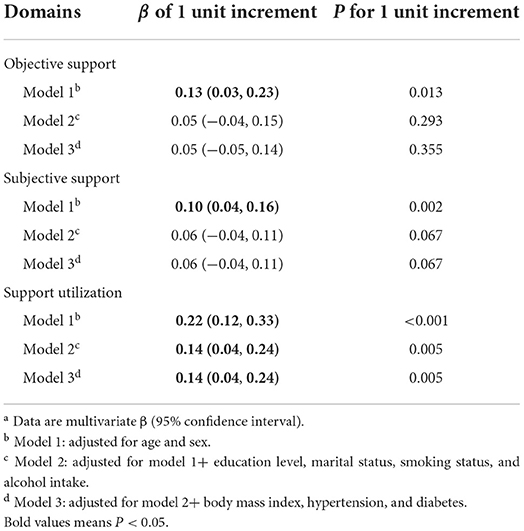
Table 4. The relationship between three domains of social support and MMSE score in multiple linear regressiona.
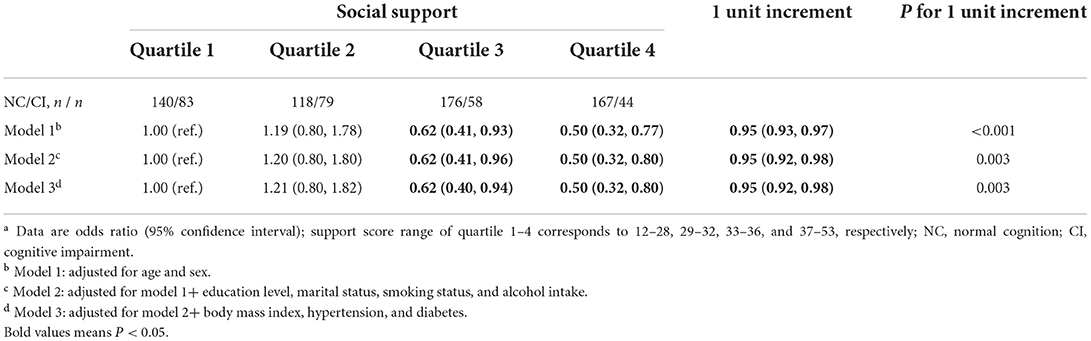
Association of social support with cognitive impairment
As shown in Table 5, by the logistic regression model, the associations of social support with cognitive impairment were examined after adjusting the covariates. In the analysis of adjusted model 3, compared to the participants with Q1, those with Q4 have a reduced odds ratio (OR = 0.50, 95% CI: 0.32, 0.80). With the 1-unit increment of social support score, there was a 5% decreased risk (OR = 0.95, 95% CI: 0.92, 0.98; P = 0.003) for cognitive impairment. Moreover, the higher scores in support utilization were associated with lower risks of CI, with a 10% decreased risk (OR = 0.90, 95% CI: 0.84, 0.96) for a 1-unit increment (Table 6).
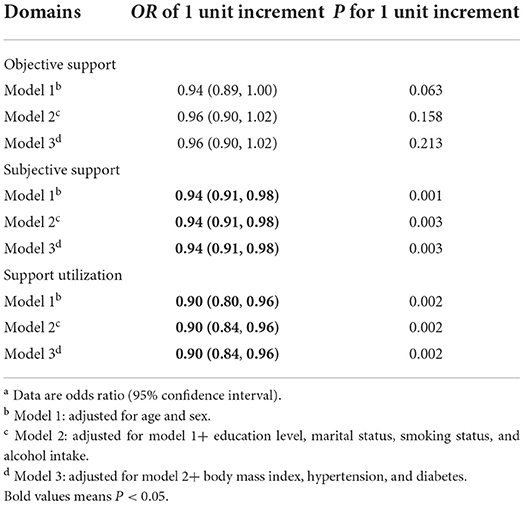
Table 6. The association of three domains of social support with cognitive impairment in logistic regressiona.
Discussion
We examined the relationship between social support and cognition among older adults in China, and found that the level of social support, particularly in support utilization, was positively associated with cognitive function. In addition, higher levels of social support, subjective support, and support utilization were associated with reduced risks of cognitive impairment, after controlling the socio-demographic characteristics, lifestyle factors, and history of diseases.
Our results are in accordance with previous studies (12, 17–22), investigating the link between social support and cognitive function. A cohort study of 624 older adults using the structural equation model showed that social support at baseline was negatively related to cognitive function 2 years later (22). A longitudinal study, including 2,255 participants aged 55–85 over 6 years of follow-up, found that high levels of emotional and instrumental support were related to better cognitive performance (17). A cross-sectional study also showed the positive relationship between social support and cognitive function in middle-aged African Americans (12), older adults in China (20), Mexican adults aged 50 and older (18), and middle-aged and older adults in rural South Africa (19). Another study, consisting of 623 middle-aged adults with a family history of Alzheimer's disease, reported that a higher level of social support was associated with better performance on tests of speed and flexibility (21). A large-scale brain image study found that individuals with social isolation had lower gray matter volumes in several brain regions temporal, such as the temporal lobe, frontal lobe, and hippocampus, and the gray matter volumes partly explained the association of baseline social isolation with cognition (16). However, several studies indicated different results from this study. Prospective studies (13, 23) have explored the temporal associations between cognitive function and social support and showed that poor cognitive function might have a negative effect on social support, and social support in mid-life was not associated with outcomes of cognitive impairment in late life. Further interventional studies and long-term observational studies are needed to prove the causal association and temporal relationship between social support and cognitive function.
The present study also indicated the inverse relationship between cognitive impairment and both subjective support and support utilization in older adults. The items of subjective support reflected the magnitude of emotional support from friends, neighbors colleagues, and family members (38). Consistent with our results, a longitudinal study with over 7.5 years of follow-up found a significant relationship between the high level of emotional support and change in global cognitive function. The aforementioned longitudinal (17) and cross-sectional (12, 19) studies also showed similar associations between emotional support with cognitive function. The items of support utilization describe the degree of voluntarily seeking others' help and understanding and attending social activities, which may involve the willingness to communicate and collaborate with others. In addition, the objective support was not related to cognition function. These associations of the sub-domain of social support and cognitive function highlighted the importance of emotional support and support utilization, suggesting that facilitating the emotional support and support utilization of participants may be beneficial to the prevention of poor cognitive performance and cognitive impairment.
Some interpretations may increase the understanding of the relationship between social support and cognitive function. Accumulating evidence demonstrated that social support was associated with a reduced risk of depression (39, 40) and well-being (41). Several large prospective studies proved that these improvements in mental health might delay the progression of cognitive impairment and Alzheimer's disease (42). Moreover, social support also means the degree of feedback when older adults ask for needs and help. For instance, foods to eat and drugs to perform always need to be provided and prepared for older adults. The loss of these may cause accelerating cognitive decline. Importantly, as vulnerable people, older adults have more benefits from social support than younger. In addition, social support could reflect long-term care from others, which may increase the management of blood lipids and glucose (8–11) and reduce the risk of Alzheimer's disease and dementia in late life for the benefit of controlling blood glucose and lipids well.
The biological mechanisms that social support is beneficial to cognitive function are feasible. Social interaction was considered as a pathway of mental stimulation, which could contribute to cognitive reserves by activating and strengthening neurobiological activities (18, 43). Animal studies also indicated that the level of brain-derived neurotrophic factor (BDNF) playing a beneficial role in the brain was related to social support in rats (44, 45). Interestingly, another human study showed that social support from others was associated with BDNF, which alleviates the stress response (46). The evidence from human studies and animal experiments suggested that tDNF may explain the links between social support and cognitive function.
In addition, the specialized questionnaire was important to evaluate the level of social support. This study used the SSRC to assess the social support of participants. The items of SSRC consist of objective support, perceived social support, and support utilization, which comprehensively represent the level of social support. SSRC was confirmed with good reliability and α's coefficient (47, 48). Epidemiological studies among the Chinese population have widely used SSRC to examine the relationship between social support and diseases (32, 49). Over past decades, studies across the world have employed various tests to determine social support. However, there are some differences between the various versions of social support due to the distinction of culture and language among different countries and areas (13, 17, 19). Thus, future studies using approximate questionnaires will contribute to providing empirical evidence to evaluate the association of social support with diseases.
This study has several limitations to report. First, given the cross-sectional nature of this study, we could not examine the temporal association between social support and cognitive function. Second, the MMSE, as the assessment of cognitive function, was used in this study. Further epidemiological studies employing a battery of multi-domain cognitive tests and clinical diagnosis of MCI and dementia as outcomes are promising. Third, all participants in this study were recruited from Hubei province, and the results may not apply to older adults in other parts of China. Fourth, we did not test the biomarkers associated with support and cognition, such as BDNF. Further studies based on blood or brain biomarkers are needed to confirm the findings in this study. Fifth, although we have adjusted for many potential confounders in this study, we are unable to completely rule out residual confounders from unmeasured factors.
Conclusions and implications
In this cross-sectional study, we found that social support and support utilization were positively related to cognitive function. In addition, social support, subjective support, and support utilization were negatively associated with the risk of cognitive impairment. The improvement of social support, particularly in support utilization, from health care policies, society, and family numbers may have a protective effect on late-life cognition among old adults in China.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Medical College, Wuhan University of Science and Technology. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SR and XL proposed and designed the study. SR and BL drafted this article. YG and BL completed the statistical analysis. SR supervised the data acquisition, statistical analysis, and interpretation of results. All authors critically revised the manuscript for important intellectual content.
Funding
This work was supported by the Health Commission of Hubei Province's Scientific Research Project (Grant No. WJ2019H306) and the National Natural Science Foundation of China (No. 81941016). The funders of the study had no role in the study design, data interpretation, writing of the report, or decision of a publication.
Acknowledgments
The authors are grateful to all the subjects who participated in this study and the interviewers who helped us during the study procedures.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jia J, Wei C, Chen S, Li F, Tang Y, Qin W, et al. The cost of Alzheimer's disease in China and re-estimation of costs worldwide. Alzheimers Dement. (2018) 14:483–91. doi: 10.1016/j.jalz.2017.12.006
2. Alzheimer's Disease facts and figures. Alzheimers Dement. (2021) 17:327–406. doi: 10.1002/alz.12328
3. World Health Organization. Risk Reduction of Cognitive Decline and Dementia. Who Guidelines (2019.
4. Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. (2020) 5:e661–e71. doi: 10.1016/S2468-2667(20)30185-7
5. Alster P, Dunalska A, Migda B, Madetko N, Krolicki L. The rate of decrease in brain perfusion in progressive supranuclear palsy and corticobasal syndrome may be impacted by glycemic variability-a pilot study. Front Neurol. (2021) 12:767480. doi: 10.3389/fneur.2021.767480
6. Pal K, Mukadam N, Petersen I, Cooper C. Mild cognitive impairment and progression to dementia in people with diabetes, prediabetes and metabolic syndrome: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:1149–60. doi: 10.1007/s00127-018-1581-3
7. van Vliet P. Cholesterol and late-life cognitive decline. J Alzheimers Dis. (2012) 30 Suppl 2:S147–62. doi: 10.3233/JAD-2011-111028
8. Shirom A, Melamed S, Rogowski O, Shapira I, Berliner S. Workload, control, and social support effects on serum lipids: a longitudinal study among apparently healthy employed adults. J Occup Health Psychol. (2009) 14:349–64. doi: 10.1037/a0015283
9. King DK, Glasgow RE, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, et al. Self-Efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care. (2010) 33:751–3. doi: 10.2337/dc09-1746
10. Rees CA, Karter AJ, Young BA. Race/ethnicity, social support, and associations with diabetes self-care and clinical outcomes in Nhanes. Diabetes Educ. (2010) 36:435–45. doi: 10.1177/0145721710364419
11. Ing CT, Zhang G, Dillard A, Yoshimura SR, Hughes C, Palakiko DM, et al. Social support groups in the maintenance of glycemic control after community-based intervention. J Diabetes Res. (2016) 2016:7913258. doi: 10.1155/2016/7913258
12. Sims RC, Levy SA, Mwendwa DT, Callender CO, Campbell AL. Jr. The Influence of functional social support on executive functioning in middle-aged African Americans. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. (2011) 18:414–31. doi: 10.1080/13825585.2011.567325
13. Kats D, Patel MD, Palta P, Meyer ML, Gross AL, Whitsel EA, et al. Social support and cognition in a community-based cohort: the atherosclerosis risk in communities (aric) study. Age Ageing. (2016) 45:475–80. doi: 10.1093/ageing/afw060
14. Kotwal AA, Kim J, Waite L, Dale W. Social function and cognitive status: results From a Us Nationally Representative Survey of Older Adults. J Gen Intern Med. (2016) 31:854–62. doi: 10.1007/s11606-016-3696-0
15. Salinas J, O'Donnell A, Kojis DJ, Pase MP, DeCarli C, Rentz DM, et al. Association of social support with brain volume and cognition. JAMA Netw Open. (2021) 4:e2121122. doi: 10.1001/jamanetworkopen.2021.21122
16. Shen C, Rolls E, Cheng W, Kang J, Dong G, Xie C, et al. Associations of social isolation and loneliness with later dementia. Neurology. (2022). doi: 10.1212/WNL.0000000000200583
17. Ellwardt L, Aartsen M, Deeg D, Steverink N. Does loneliness mediate the relation between social support and cognitive functioning in later life? Soc Sci Med. (2013) 98:116–24. doi: 10.1016/j.socscimed.2013.09.002
18. Zamora-Macorra M, de Castro EF, Avila-Funes JA, Manrique-Espinoza BS, Lopez-Ridaura R, Sosa-Ortiz AL, et al. The association between social support and cognitive function in Mexican adults aged 50 and older. Arch Gerontol Geriatr. (2017) 68:113–8. doi: 10.1016/j.archger.2016.10.005
19. Harling G, Kobayashi LC, Farrell MT, Wagner RG, Tollman S, Berkman L. Social contact, social support, and cognitive health in a population-based study of middle-aged and older men and women in rural South Africa. Soc Sci Med. (2020) 260:113167. doi: 10.1016/j.socscimed.2020.113167
20. Zhu S, Hu J, Efird JT. Role of social support in cognitive function among elders. J Clin Nursing. (2012) 21:2118–25. doi: 10.1111/j.1365-2702.2012.04178.x
21. Zuelsdorff ML, Engelman CD, Friedman EM, Koscik RL, Jonaitis EM, Rue AL, et al. Stressful events, social support, and cognitive function in middle-aged adults with a family history of Alzheimer's disease. J Aging Health. (2013) 25:944–59. doi: 10.1177/0898264313498416
22. McHugh Power JE, Lawlor BA, Kee F. Social support mediates the relationships between extraversion, neuroticism, and cognitive function in older adults. Public Health. (2017) 147:144–52. doi: 10.1016/j.puhe.2017.02.015
23. Liao J, Muniz-Terrera G, Head J, Brunner EJ. Dynamic longitudinal associations between social support and cognitive function: a prospective investigation of the directionality of associations. J Gerontol B Psychol Sci Soc Sci. (2018) 73:1233–43. doi: 10.1093/geronb/gbw135
24. Shuiyuan X. Theoretical foundation and research application about the social support rating scale. J Clin Psychiatr. (1994) 4:98–100.
25. Liu D, Li L, An L, Cheng G, Chen C, Zou M, et al. Urban-Rural disparities in mild cognitive impairment and its functional subtypes among community-dwelling older residents in central China. Gen Psychiatr. (2021) 34:e100564. doi: 10.1136/gpsych-2021-100564
26. Deng Y, Zhao S, Cheng G, Yang J, Li B, Xu K, et al. The prevalence of mild cognitive impairment among Chinese people: a meta-analysis. Neuroepidemiology. (2021) 55:79–91. doi: 10.1159/000512597
27. Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
28. Li G, Shen YC, Chen CH, Zhao YW Li SR, Lu M. An epidemiological survey of age-related dementia in an urban area of Beijing. Acta Psychiatr Scand. (1989) 79:557–63. doi: 10.1111/j.1600-0447.1989.tb10303.x
29. Li H, Jia J, Yang Z. Mini-Mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
30. Zhang. L, Kong. L, Zhang. Q, Tao. F, Ma. A, Liu. Y, et al. Development of Chinese people's social support scale and test of reliability and validity. J Clin Psychosomatic Dis. (2014) 20:36–40. doi: 10.3969/j.issn.1672-187X.2014.06.015-0036-05
31. Liu J, Li F, Lian Y. Investigation of reliability and validity of the social support scale. J Xinjiang Med Univer. (2008) 1:1–3.
32. Xiao P, Zhou Y. Factors associated with the burden of family caregivers of elderly patients with femoral neck fracture: a cross-sectional study. J Orthop Surg Res. (2020) 15:234. doi: 10.1186/s13018-020-01749-9
33. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
34. Sommerlad A, Ruegger J, Singh-Manoux A, Lewis G, Livingston G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry. (2018) 89:231–8. doi: 10.1136/jnnp-2017-316274
35. Zhou BF. Cooperative Meta-Analysis Group of the Working Group on Obesity in C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese Adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. (2002) 15:83–96.
36. Joint Committee for Guideline R. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
37. American Diabetes A. 2. classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. (2021) 44(Suppl 1):S15–33. doi: 10.2337/dc21-S002
38. Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: macarthur studies of successful aging. Health Psychol. (2001) 20:243–55. doi: 10.1037/0278-6133.20.4.243
39. Gariepy G, Honkaniemi H, Quesnel-Vallee A. Social support and protection from depression: systematic review of current findings in Western Countries. Br J Psychiatry. (2016) 209:284–93. doi: 10.1192/bjp.bp.115.169094
40. Tengku Mohd TAM, Yunus RM, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in asia: a systematic review. BMJ Open. (2019) 9:e026667. doi: 10.1136/bmjopen-2018-026667
41. Kafetsios K, Sideridis GD. Attachment, social support and well-being in young and older adults. J Health Psychol. (2006) 11:863–75. doi: 10.1177/1359105306069084
42. Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF. 3rd. late-life depression and risk of vascular dementia and Alzheimer's Disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. (2013) 202:329–35. doi: 10.1192/bjp.bp.112.118307
43. Hsiao YH, Hung HC, Chen SH, Gean PW. Social interaction rescues memory deficit in an animal model of Alzheimer's disease by increasing Bdnf-dependent hippocampal neurogenesis. J Neurosci. (2014) 34:16207–19. doi: 10.1523/JNEUROSCI.0747-14.2014
44. Zaletel I, Filipovic D, Puskas N. Hippocampal Bdnf in physiological conditions and social isolation. Rev Neurosci. (2017) 28:675–92. doi: 10.1515/revneuro-2016-0072
45. Viana Borges J, Souza de. Freitas B, Antoniazzi V, de Souza Dos Santos C, Vedovelli K, Naziaseno Pires V, et al. Social isolation and social support at adulthood affect epigenetic mechanisms, brain-derived neurotrophic factor levels and behavior of chronically stressed Rats. Behav Brain Res. (2019) 366:36–44. doi: 10.1016/j.bbr.2019.03.025
46. Ma DY, Chang WH, Chi MH, Tsai HC, Yang YK, Chen PS. The correlation between perceived social support, cortisol and brain derived neurotrophic factor levels in healthy women. Psychiatry Res. (2016) 239:149–53. doi: 10.1016/j.psychres.2016.03.019
47. Guoyu Y, Zhengzhi F, Benli X. The reliability, validity and national norm of social support scale in servicemen. Chin Mental Health J. (2006) 20:309–12.
48. Changfei L, Cunxian J, Jiyu Z, Xinxin W, Dongfang W, Liyuan L. Reliability and validity of social support rating scale in rural suicides. Chin Mental Health J. (2011) 25:218–22.
Keywords: cognitive function, cognitive impairment, older adults, social support, cross-sectional study
Citation: Li B, Guo Y, Deng Y, Zhao S, Li C, Yang J, Li Q, Yan Y, Li F, Li X and Rong S (2022) Association of social support with cognition among older adults in China: A cross-sectional study. Front. Public Health 10:947225. doi: 10.3389/fpubh.2022.947225
Received: 19 May 2022; Accepted: 29 August 2022;
Published: 26 September 2022.
Edited by:
Katherine Henrietta Leith, University of South Carolina, United StatesReviewed by:
Edite Teixeira-Lemos, Instituto Politecnico de Viseu, PortugalAgustín Aibar-Almazán, University of Jaén, Spain
Copyright © 2022 Li, Guo, Deng, Zhao, Li, Yang, Li, Yan, Li, Li and Rong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaonuan Li, MzI2NjMzMTg4QHFxLmNvbQ==; Shuang Rong, cm9uZ3NodWFuZ3d1c3RAeWVhaC5uZXQ=
†These authors have contributed equally to this work and share first authorship
 Benchao Li1†
Benchao Li1† Shuang Rong
Shuang Rong