- 1Department of Health Care Management, National Taipei University of Nursing and Health Sciences, Taipei City, Taiwan
- 2Department of Health Promotion and Health Education, National Taiwan Normal University, Taipei City, Taiwan
- 3Department of Endocrinology and Metabolism, Zhongxiao Branch, Taipei City Hospital, Taipei City, Taiwan
- 4Department of Family Medicine, Far Eastern Memorial Hospital, New Taipei City, Taiwan
Objective: Health literacy plays a crucial role in managing chronic health conditions. Previous studies have revealed the positive relationship between health literacy and diabetes knowledge but few studies have focused on peripheral vascular disease (PVD) in diabetes in relation to health literacy in diabetes management. This study investigated the relationship between the risk for PVD and health literacy level with other determining factors among patients with type 2 diabetes.
Method: We conducted a survey on health literacy using the Mandarin Multidimensional Health Literacy Questionnaire in the department of metabolism and endocrine systems at a regional hospital in northern Taiwan from December 2021 to May 2022 and obtained data from the hospital's health information system (HIS) from 2013 to 2020 to identify occurrences of PVD (n = 429). We performed logistic regression analysis to identify the relationship between PVD events and health literacy levels (overall and in five separate subdimensions) adjusted with other variables.
Results: A longer duration of diabetes increased the risk for PVD events (P = 0.044 and 0.028). In terms of health literacy, the overall level was not significant; however, the dimension of higher levels of health literacy in acquiring health information increased the risk for PVD events (P = 0.034). Other variables were not significantly associated with the risk for PVD events.
Conclusion: This study examined the risk for PVD events in terms of the duration of diabetes and provided evidence across the range of dimensions of health literacy concerning the ability to control diabetes. Those with a higher level of health literacy may be more aware of their disease situation, seek and cooperate with their healthcare providers earlier, and have more opportunities to be made aware of their health status from regular checkups than those with inadequate health literacy. These results may help providers make available more self-management tools that are adequate and sustainable for diabetes patients with poor health literacy.
Introduction
Type 2 diabetes mellitus (T2DM) is a serious public health issue prevalent in aging societies, especially when the condition is not well-controlled. It increases the risk for micro- and macro-complications (such as retinopathy, dialysis, and peripheral vascular disease [PVD]) (1). The first step in diabetes management involves lifestyle changes in diet and physical activities (e.g., taking regular exercise) together with self-monitoring of blood glucose (SMBG) and medication adherence. These efforts in diabetes management involve long-term work and require patients to cooperate with medical teams or with their healthcare providers to obtain the optimal glycemic level. Studies show that patients with T2DM can enjoy a good quality of life and a lower risk for future complications if they follow diabetes management guidelines well (2, 3).
Chronic disease management studies have found that health literacy, defined as the capability to acquire, understand, and apply health knowledge, plays a crucial role in managing chronic health conditions (4, 5). Better outcomes are identified in patients with higher health literacy levels (6, 7). Furthermore, the performance of basic reading and numerical tasks requires them to function in the healthcare environment, which helps patients take the wheel in their disease condition. Low (or inadequate) health literacy may lead to a gap in communication with the medical team, an information gap in the use of medical devices for SMBG, or a functional gap in diabetes management in daily life. These gaps could lead to poor diabetes management (e.g., worse glycemic control), create a risk for diabetes-related problems (such as hypoglycemia), or contribute to worse outcomes, especially in terms of chronic diseases. In addition, studies have identified a connection between low health literacy and poor knowledge in terms of diabetes (8), which is also associated with poor self-related health (9) and more utilization of healthcare (10, 11).
The risk for PVD in diabetic patients is occurring earlier at an increasing rate and is becoming more severe and diffuse (12). The high blood sugar levels commonly associated with diabetes can, over time, damage the blood vessels. Poor diabetes management leads to increased morbidity and mortality in PVD due to dysfunction, inflammation, and hypercoagulability in the vascular system. One study in the UK found that 1.2% of newly diagnosed patients with T2DM also had PVD (13), suggesting that intensive targeting of glycemic control is needed. Few studies have focused on the prevalence of PVD in diabetes concerning issues of health literacy in diabetes management and the consequences of PVD, which leads patients to control their diabetes better.
We hypothesize that, in patients with type 2 diabetes, having better health literacy may enhance their diabetes care management and reduce the risk of complications (such as PVD) in the future. Therefore, this study investigated the relationship between the risk for PVD at different health literacy levels among patients with T2DM. The results may be useful for medical teams caring for patients with T2DM who otherwise have poor health literacy to conceive useful strategies in diabetes care.
Methods
Population
This was a cross-sectional survey conducted in a department of metabolism and endocrine systems at a northern regional hospital in Taiwan from December 2021 to May 2022. Before the survey, all patients provided written informed consent, which included the use of medical records from the hospital's health information system (HIS) for the analysis. All participating patients had T2DM and answered the questionnaire voluntarily; those with mental disorders or cognitive impairments, who were unable to provide informed consent or participate in the survey, were excluded. After completing the survey, we compensated the participants with NTD 100 gift cards. In all, after data correction (missing or double ID), 429 patients from the interview by trained staff were used in the analysis. The Institutional Review Board of the hospital approved the study design, which conformed to the ethical principles of the 2008 Declaration of Helsinki.
Variables
The outcome variable
The outcome we used in this study was the record of pulse volume recording for each patient from 2013 to 2020, as applicable, drawn from the hospital's HIS to identify events of PVD. Because participants had multiple medical records over the study period, we defined PVD events as those occurring when participants had PVD records in the abnormal figure throughout the study period. The abnormal range of PVD was defined as ankle brachial index <0.8.
Independent variable
We not only used using the Mandarin Multidimensional Health Literacy Questionnaire (MMHLQ) for the measurement of health literacy, but also collected participant demographic, and diabetes-related information. The demographic variables included age, sex, education, and marital status. The diabetes-related information included SMBG (Do you regularly monitor your blood glucose when not in hospital? Yes/No), diabetes control methods (medication, insulin, diet [following the suggestions of the medical team], in terms of regular exercise [three times a week for at least 30 min per session], smoking behavior [Yes/No], and drinking behavior [Yes/No]), diabetes duration (<1 year, 1–5 years, 6–10 years, or >11 years), any family history of diabetes (Yes/No), ability to takeregular exercise, ability to follow a diet plan, ability to follow treatments, ability to perform SMBG, and responses to the Diabetes Knowledge Questionnaire (DKQ).
To assess their ability to follow regular exercise and diet plans, we asked the participants to evaluate the degree of comprehension in understanding the diabetes control plans (in diet and exercise) from the medical teams on a scale of 0–10. To assess the ability to follow treatment and perform SMBG, we asked participants to respond to the following items: understanding the treatment plan (Yes/No), knowing how to take the medicine (Yes/No), understanding the drug information (Yes/No), knowing how to use the glucometer (Yes/No), identifying the device information from the glucometer (Yes/No), and knowing the level of fasting plasma glucose (Right/Wrong). The DKQ is a 24-item questionnaire that records the understanding of the cause of diabetes with complications, blood glucose levels, diet, and physical activity, has three response options “yes,” “no,” and “don't know” and has been reported to have optimal reliability and validity (14). The higher the score, the better the knowledge of the disease (The highest achievable score was 24). In addition, the Cronbach's alpha reliability of DKQ-24 was 0.796 (alpha if item deleted was 0.784–0.797) which represented an acceptable range (15).
To test health literacy, we used the MMHLQ, which includes 20 items in 5 dimensions (acquiring, understanding, assessing, applying, and communication). Every item has four scales (very difficult 1, difficult 2, easy 3, and very easy 4), and a transforming formula was used to obtain scores ranging from 0 to 50 in the five dimensions and the total. Later, we cataloged these scores into four levels: inadequate (≤25), limited/problematic (25 ≤ 33), sufficient (33 ≤ 42), and excellent (42 ≤ 50). Several studies have demonstrated that the MMHLQ is an adequate tool for health literacy (16–18). In addition, the Cronbach's alpha reliability of MMHLQ was 0.79 (alpha if item deleted was 0.77–0.94) which represented an acceptable range.
Statistics
To better understand the distribution of health literacy, we provided the original response to every item in the five dimensions across the four-level distribution. We were also interested in the factors associated with health literacy, and we used the chi-square test and ANOVA to test for significant differences. Finally, we performed logistic regression to explore the relationship between PVD events and health literacy levels (both overall and across the five sub-dimensions) adjusted for other variables. Note that we only considered a high correlation between education and health literacy; thus, we only included health literacy in the logistic regression model. All statistical data were analyzed using SAS 9.3.1 (SAS Institute, Cary, NC) and SPSS 20.0 (SPSS Inc., Chicago, IL). The significance level was set to P < 0.05.
Results
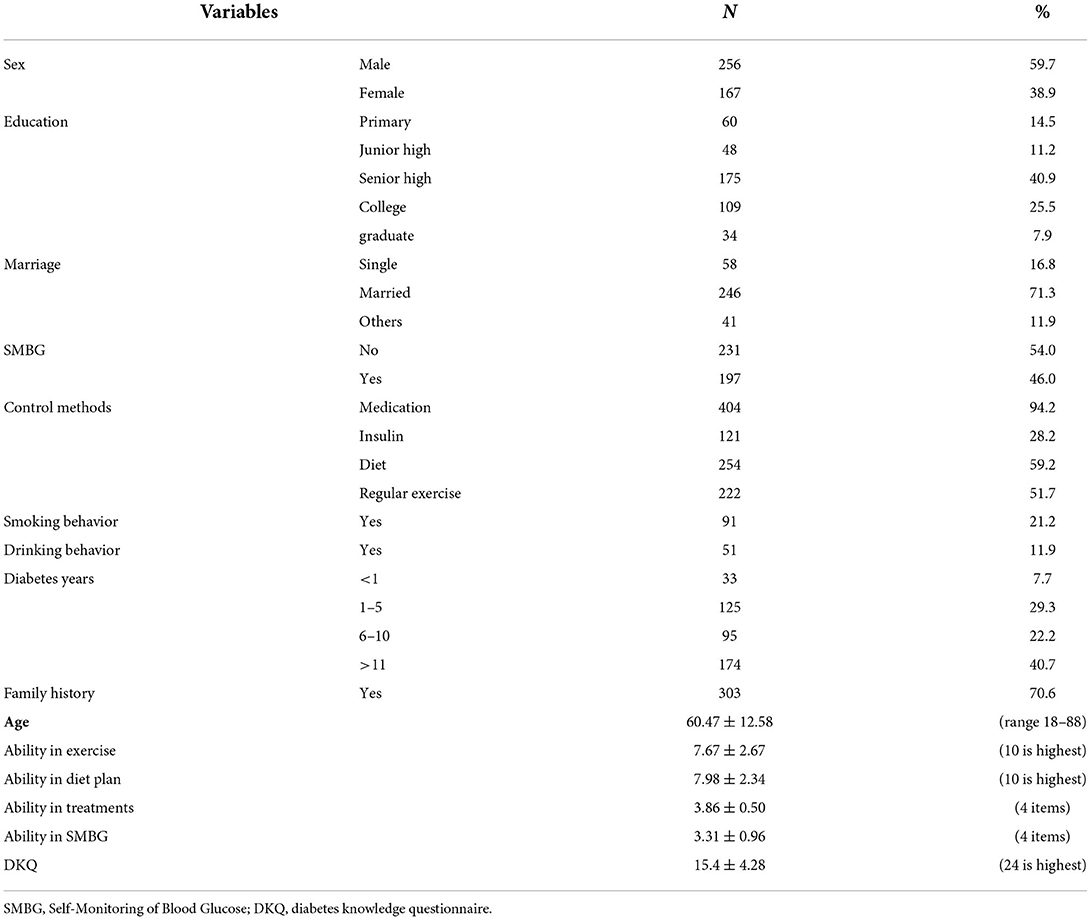
The basic characteristics of the participants are presented in Table 1. The majority were male (59.7%), married (71.3%), had no smoking or drinking behavior, had a family history of diabetes (70.6%), and had a diabetes duration of >11 years (40.7%). Most used medication, and over half followed a controlled diet and took regular exercise, although only 46% of them performed SMBG. The abilities in regular exercise, diet plan, treatment, and SMBG were 7.67, 7.98, 3.86, and 3.31, respectively. The mean DKQ score was 15.4.
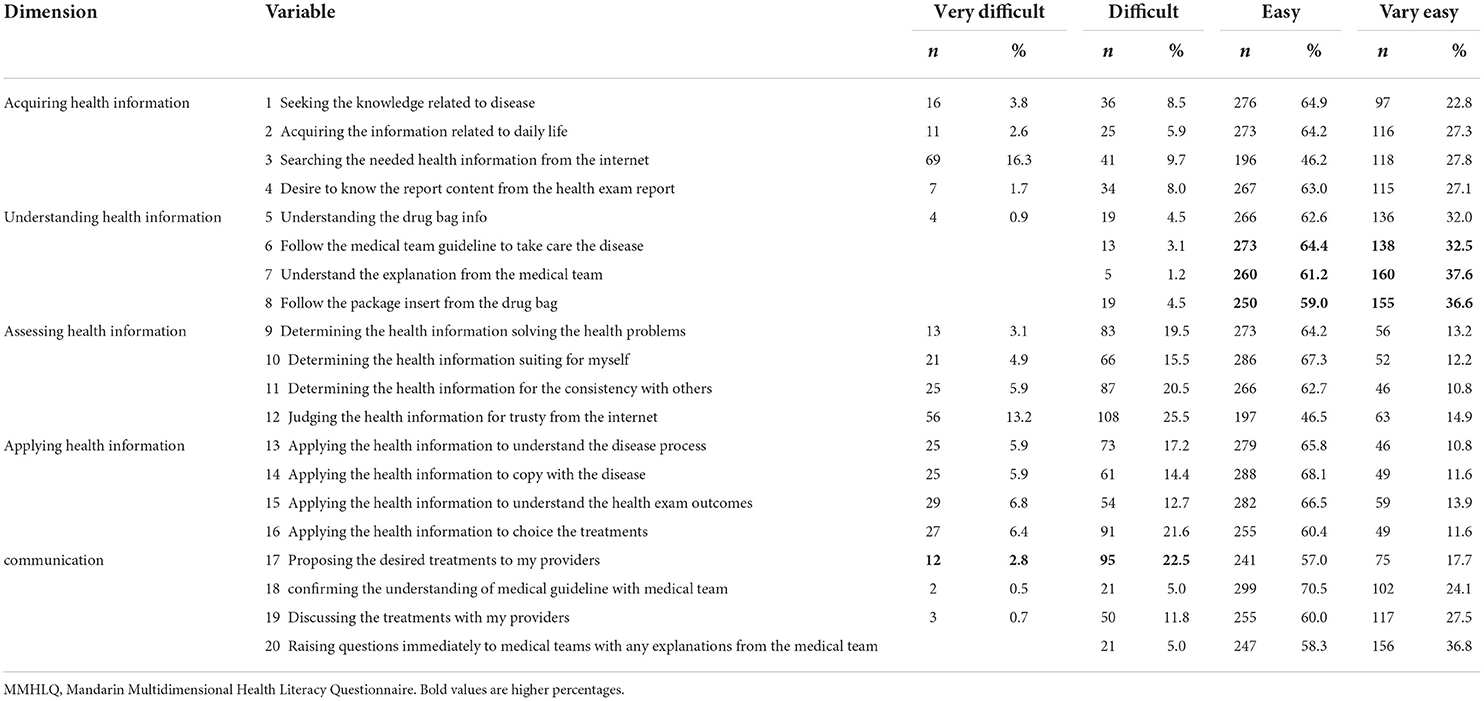
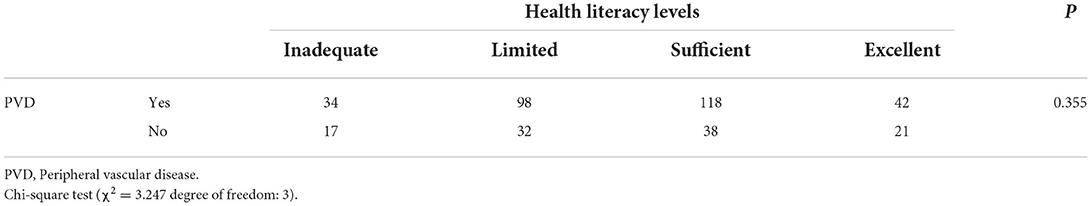
Health literacy was determined as follows: over 25% of patients expressed difficulty in searching for the needed health information from the Internet (acquiring), 38% of patients expressed difficulty in judging the health information for trust from the Internet, 26% of patients expressed difficulty in determining the health information for consistency with others (assessing), 28% of patients expressed difficulty in applying the health information to choose the treatment (applying), and 26% of patients expressed difficulty in proposing the desired treatments to my providers (communication). However, over 95% of patients expressed easy or very easy understanding in the dimension of health literacy (Table 2 with red color). We used the scores to divide the patients into four levels: inadequate, limited/problematic, sufficient, and excellent. We found that combining the sufficient and excellent levels returned 69.9, 91.1, 54.3, 65.9, and 77.2% patient competence in acquiring, understanding, assessing, applying, and communication, respectively. Overall, 12.8, 32.4, 39.2, and 54.8% of patients had inadequate, limited/problematic, sufficient, and excellent health literacy skills, respectively (Table 3).

Table 3. The scores of five dimensions with overall and the distribution of health literacy levels in MMHLQ.
We also identified the association between the other variables we used in the study and health literacy for the overall score and scores for the five subdimensions from chi square or ANOVA test (*significant level, P < 0.05). Younger individuals, those with higher education levels, and those with higher DKQ scores were found to have better health literacy levels (Table 4). Positive associations (+ in Table 4) were also observed between the performance of regular exercise, following the diet plan, and conducting SMBG and better health literacy levels, especially in acquiring, understanding, and assessing health information. However, we did not find a significant association between health levels and PVD risk (P = 0.355) (Table 5). In addition, we provided details in the supplemental file (see Supplementary Tables 1–6).
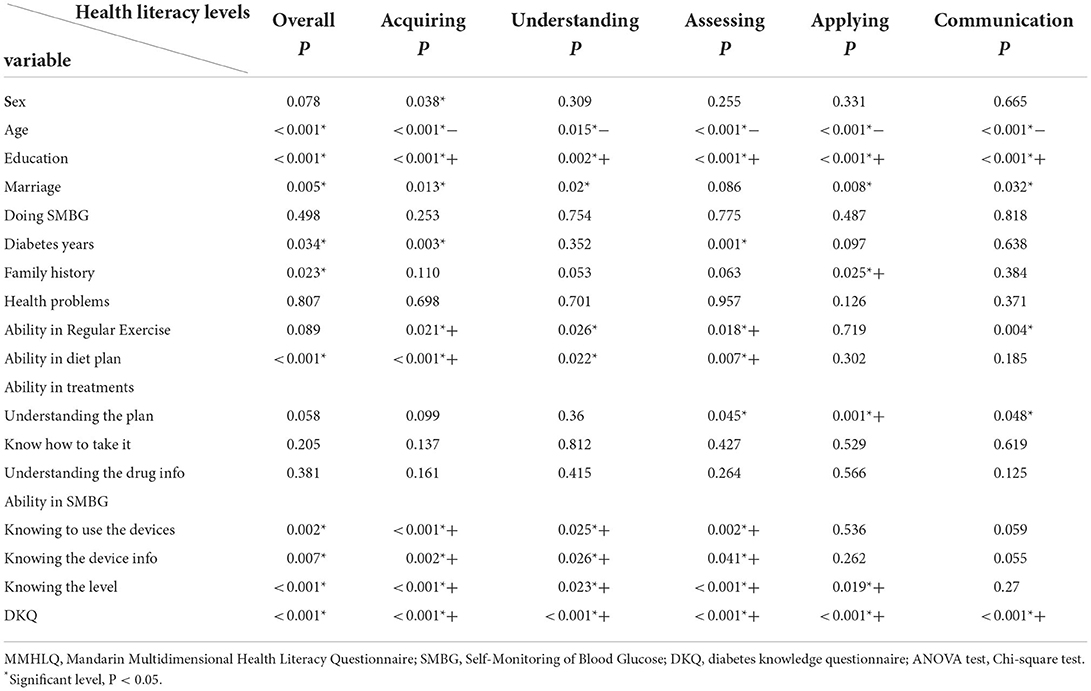
Table 4. The relationship between overall and sub-dimensions health literacy levels (MMHLQ) with other variables.
We used two multivariable logistic regression models to explore the relationship between PVD events and health literacy levels with other variables. We tested the overall health literacy level and five subdimensions of health literacy level separately in the model, and only the dimension of acquiring health information was significant. Therefore, in Model 1, we used the overall health literacy level, and in Model 2, we used acquired health information because most participants had better scores in this health literacy sub-dimension. We found that a longer diabetes duration increased the risk for PVD events (P = 0.044 and 0.028) (Table 6). For health literacy, the overall level was not significant in Model 1; however, a higher level of acquiring health information increased the risk for PVD events in Model 2 (P = 0.034). Other variables were not significantly associated with the risk for PVD events.
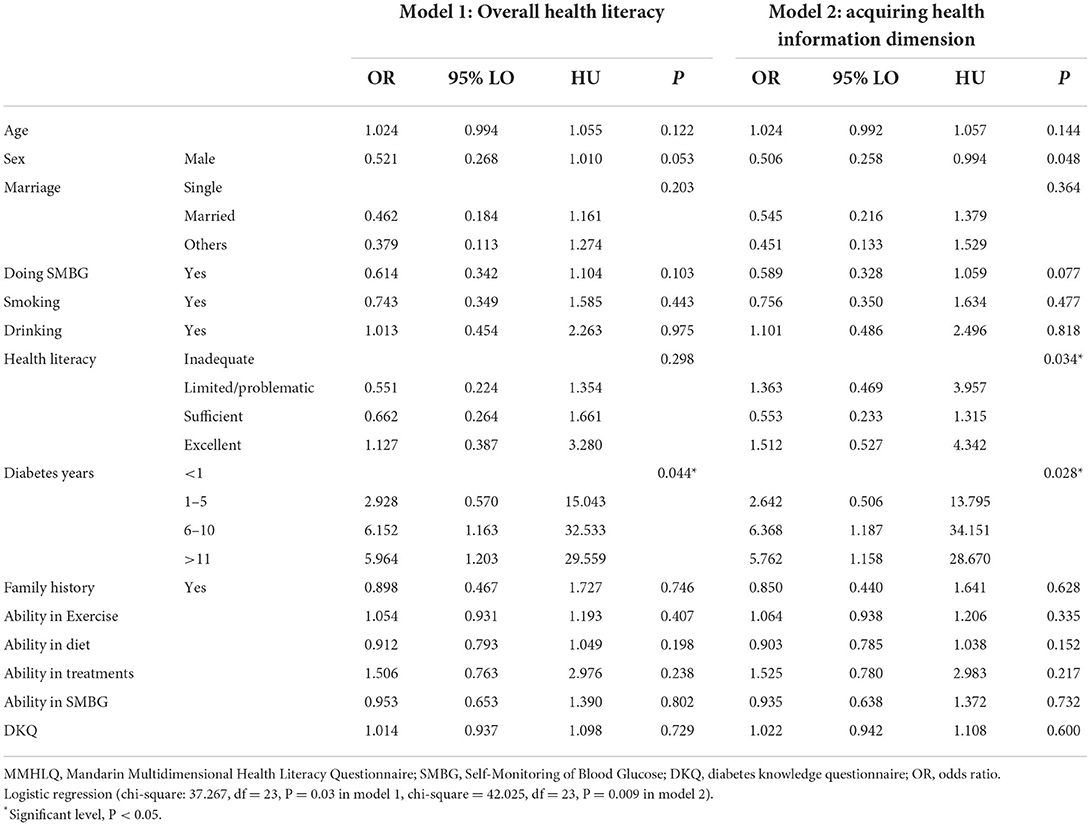
Table 6. The relationship between PVD events with health literacy adjusted with other variables from logistics regression.
Discussion
In this study, we found that the longer the patients have diabetes the more likely they are to experience a PVD even while the overall health literacy levels not significant. Only modest significance was found in the acquisition of health information for the health literacy dimension, and possible explanations did not have sufficient statistical power to identify any health literacy effects in this cross-sectional survey or imply that other factors or pathways need to be explored in further research. Interestingly, those who had a better record in acquiring health information health literacy levels had an increased risk for PVD events. It may be that those with better levels of acquiring health information had better health awareness in their diabetes management and had more opportunity to be made aware of their health status from regular checkups.
We also found that younger individuals had higher levels of health literacy and higher education levels. This result is consistent with many previous studies on its positive associations with age and education levels (19–23). However, mixed results for health literacy have also been found in other studies, relating to differences in measurement, tools, or specific diseases. Those who have better health literacy levels in acquiring health information (understanding health information) and assessing health information dimensions indicated a better ability to understand the merit of regular exercise and diet plans, as well as the ability to perform SMBG. One possible explanation is that patients with T2DM need to understand, assess, and implement health information related to diet, exercise, and SMBG to change their lifestyle, and poor health literacy impedes diabetes self-management to achieve optimal glycemic control (24, 25). However, other studies have indicated weak or no association with health literacy (26, 27). Interestingly, no significant association was found with health literacy and the ability to treat in medication. A possible explanation for this is that patients relied on the authority of providers and, most of them trusted the information that was provided most of the time. Patients with T2DM who had higher health literacy levels had better DKQ scores, which demonstrates the vital role that health literacy plays in diabetes knowledge (28). Clinical teams should understand the positive relationship between health literacy and diabetes knowledge and pay closer attention to detecting the patient's ability to understand and apply health information imparted by diabetes education materials. For this reason, educational materials should be provided or modified to adjust for different health literacy levels.
Our study confirms the increased risk for PVD events with longer diabetes duration, which is consistent with other studies (29, 30). Peripheral vascular disease can cause lower limb amputation or mortality, especially in people with T2DM, due to the risk factors for DM—hypertension, smoking, and hyperlipidemia—along with other traditional risks, such as age or low kidney function (31, 32). At-risk indicators include an older patient cohort, diabetes duration of longer than 10 years, high HbA1c, obesity, and neuropathy (33).
A modest significant effect was found in acquiring health information on health literacy levels associated with PVD events. Clinical staff should identify patients with inadequate or limited health literacy levels and provide easy-to-understand educational materials on diet and exercise plans to help them control their diabetes. In addition, we found positive associations between diet, exercise plan, and SMBG with diabetes knowledge and high levels of acquiring, understanding, and assessing health information. We should conceive useful strategies to help diabetic patients improve their capacity to apply health information and communication, such as mobile eHealth technology; to address health problems, especially among the older adult population, and to overcome these adoption barriers to suffering on the internet.
Limitations
There are several limitations to address. First, although the MMHLQ is reliable and valid in clinical settings, we still need to compare the results with other measurements. However, the application of several health literacy measurements (such as the Test of Functional Health Literacy in Adults, Literacy Assessment for Diabetes, or Diabetes Numeracy Test) not only requires to be considered in terms of patient loading and under different construction conceptions but also faces the challenge of translation and employment in the generality or specialty in disease. However, the distribution of health literacy levels determined by the MMHLQ is acceptable. Second, the cross-sectional survey was limited to establishing a temporal association and diabetes care is long-term work, therefore, one survey can only reflect the information from the patient's diabetes management at that time. This information may not be sufficient to evaluate certain specific situations or the long-term aspects of the patient's diabetes care. Third, our results were obtained using data from a single center and may not be generalizable to other diabetic patients. In addition, patients in the hospital participated in the survey voluntarily and gave written consent; thus, we need to consider the possibility of selection and recall biases, which may have affected the results. These participants may have more health awareness of their disease situation; so they may have more positive factors in their diabetes management. Finally, considering the limited time in this study for answering the survey in the older adults group with type 2 diabetes, some items in the survey (for example, smoking, and drinking behavior) used the dichotomous scale without details which may underestimate the effect on outcomes. Further studies will be needed to provide evidence to clarify relationships in these items.
Conclusions
More evidence was identified regarding the different dimensions of health literacy levels and the ability to control diabetes. A certain number of older adult patients with type 2 diabetes need assistance to search for, judge, determine, and apply health information acquired from the internet. Providing trustworthy and easy-to-understand health information from modern technology may be vital for diabetes care management. In addition, those who have a higher health literacy level may be more aware of their disease situation and seek and cooperate with their providers earlier than those who have inadequate health literacy. These results may help providers increase adequate and sustainable self-management tools in diabetes patients with poor health literacy.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Survey Research Data Archive (SRDA) in Academia Sinica in Taiwan.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Taipei City Hospital Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
S-JC and Y-JC contributed to the development of study methodology and study conceptualization. KL and C-DC provided clinical input. S-JC is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to interpretation of results, reviewed and drafting the manuscript and approved the final version.
Funding
This work was supported by the Ministry of Science and Technology (MOST 109-2410-H-227-001-SSS). The funder had no role in study design, and analysis, or decision to publish.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.946889/full#supplementary-material
References
1. Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab. (2016) 20:546–51. doi: 10.4103/2230-8210.183480
2. Speight J, Holmes-Truscott E, Hendrieckx C, Skovlund S, Cooke D. Assessing the impact of diabetes on quality of life: what have the past 25 years taught us? Diabet Med. (2020) 37:483–92. doi: 10.1111/dme.14196
3. Nijpels G, Beulens JW, van der Heijden AA, Elders PJ. Innovations in personalised diabetes care and risk management. Eur J Prev Cardiol. (2019) 26:125–32. doi: 10.1177/2047487319880043
4. van der Heide I, Poureslami I, Mitic W, Shum J, Rootman I, FitzGerald JM. Health literacy in chronic disease management: a matter of interaction. J Clin Epidemiol. (2018) 102:134–8. doi: 10.1016/j.jclinepi.2018.05.010
5. Dunn P, Conard S. Improving health literacy in patients with chronic conditions: a call to action. Int J Cardiol. (2018) 273:249–51. doi: 10.1016/j.ijcard.2018.08.090
6. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
7. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. (2004) 19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x
8. Cavanaugh KL. Health literacy in diabetes care: explanation, evidence and equipment. Diabetes Manag. (2011) 1:191–9. doi: 10.2217/dmt.11.5
9. Weiss BD, Hart G, McGee DL, D'Estelle S. Health status of illiterate adults: relation between literacy and health status among persons with low literacy skills. J Am Board Fam Pract. (1992) 5:257–64.
10. Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. (1997) 87:1027–30. doi: 10.2105/AJPH.87.6.1027
11. Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. (1998) 13:791–8. doi: 10.1046/j.1525-1497.1998.00242.x
12. Huysman E, Mathieu C. Diabetes and peripheral vascular disease. Acta Chir Belg. (2009) 109:587–94. doi: 10.1080/00015458.2009.11680493
13. Adler AI, Stevens RJ, Neil A, Stratton IM, Boulton AJ, Holman RR. UKPDS 59: hyperglycemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 diabetes. Diabetes Care. (2002) 25:894–9. doi: 10.2337/diacare.25.5.894
14. Garcia AA, Villagomez ET, Brown SA, Kouzekanani K, Hanis CL. The Starr County Diabetes Education Study: development of the Spanish-language diabetes knowledge questionnaire. Diabetes care. (2001) 24:16–21. doi: 10.2337/diacare.24.1.16
15. Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. (2011) 2:53–5. doi: 10.5116/ijme.4dfb.8dfd
16. Wu CL, Liou CH, Liu SA, Sheu WH, Tsai SF. Mandarin multidimensional health literacy questionnaire for patient supporting groups: a quality improvement article. Medicine. (2020) 99:e23182. doi: 10.1097/MD.0000000000023182
17. Wu C-L, Liou C-H, Liu S-A, Sheu WH-H, Tsai S-F. Health literacy varies according to different background disease natures and characteristics of participants for patient support groups. Int J Environ Res Public Health. (2020) 17:5702. doi: 10.3390/ijerph17165702
18. Wei M-H, Wang Y-W, Chang M-C, Hsieh J-G. Development of Mandarin Multidimensional Health Literacy Questionnaire (MMHLQ). Taiwan J Public Health. (2017) 36:556–70. doi: 10.6288/TJPH201736106061
19. Chesser AK, Keene Woods N, Smothers K, Rogers N. Health literacy and older adults: a systematic review. Gerontol Geriatr Med. (2016) 2:2333721416630492. doi: 10.1177/2333721416630492
20. Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. J Gerontol B Psychol Sci Soc Sci. (2000) 55:S368–74. doi: 10.1093/geronb/55.6.S368
21. Rouquette A, Nadot T, Labitrie P, Van den Broucke S, Mancini J, Rigal L, et al. Validity and measurement invariance across sex, age, and education level of the French short versions of the European Health Literacy Survey Questionnaire. PLoS ONE. (2018) 13:e0208091. doi: 10.1371/journal.pone.0208091
22. Bayati T, Dehghan A, Bonyadi F, Bazrafkan L. Investigating the effect of education on health literacy and its relation to health-promoting behaviors in health center. J Educ Health Promot. (2018) 7:127. doi: 10.4103/jehp.jehp_65_18
23. Kickbusch I, Pelikan JM, Apfel F, Tsouros AD. Health Literacy: The Solid Facts. World Health Organization (2013).
24. Sarkar U, Karter AJ, Liu JY, Moffet HH, Adler NE, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. (2010) 25:962–8. doi: 10.1007/s11606-010-1389-7
25. Ji M, Ren D, Dunbar-Jacob J, Gary-Webb TL, Erlen JA. Self-management behaviors, glycemic control, and metabolic syndrome in type 2 diabetes. Nurs Res. (2020) 69:E9–17. doi: 10.1097/NNR.0000000000000401
26. Mbaezue N, Mayberry R, Gazmararian J, Quarshie A, Ivonye C, Heisler M. The impact of health literacy on self-monitoring of blood glucose in patients with diabetes receiving care in an inner-city hospital. J Natl Med Assoc. (2010) 102:5–9. doi: 10.1016/S0027-9684(15)30469-7
27. Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. (2013) 28:444–52. doi: 10.1007/s11606-012-2241-z
28. Marciano L, Camerini A-L, Schulz PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med. (2019) 34:1007–17. doi: 10.1007/s11606-019-04832-y
29. Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: epidemiology, mechanisms, and outcomes. World J Diabetes. (2015) 6:961–9. doi: 10.4239/wjd.v6.i7.961
30. Höbaus C, Herz CT, Wrba T, Koppensteiner R, Schernthaner G-H. Peripheral arterial disease and type 2 diabetes: Older patients still exhibit a survival benefit from glucose control. Diabetes Vasc Dis Res. (2020) 17:1479164120914845. doi: 10.1177/1479164120914845
31. Aboyans V, Criqui MH, Denenberg JO, Knoke JD, Ridker PM, Fronek A. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. (2006) 113:2623–9. doi: 10.1161/CIRCULATIONAHA.105.608679
32. Shukla V, Fatima J, Ali M, Garg A. A study of prevalence of peripheral arterial disease in type 2 diabetes mellitus patients in a teaching hospital. J Assoc Physicians India. (2018) 66:57–60.
Keywords: health literacy, peripheral vascular disease, type 2 diabetes, diabetes management, survey
Citation: Chiou S-J, Chang Y-J, Liao K and Chen C-D (2022) Modest association between health literacy and risk for peripheral vascular disease in patients with type 2 diabetes. Front. Public Health 10:946889. doi: 10.3389/fpubh.2022.946889
Received: 18 May 2022; Accepted: 08 August 2022;
Published: 24 August 2022.
Edited by:
Jonathan Ling, University of Sunderland, United KingdomReviewed by:
Tung-Sung Tseng, Louisiana State University, United StatesOrsolya Papp-Zipernovszky, University of Szeged, Hungary
Copyright © 2022 Chiou, Chang, Liao and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shang-Jyh Chiou, c2hhbmdqeWhAbnR1bmhzLmVkdS50dw==
 Shang-Jyh Chiou
Shang-Jyh Chiou Yen-Jung Chang2
Yen-Jung Chang2