
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 30 September 2022
Sec. Family Medicine and Primary Care
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.945988
 Manjari Rain1‡
Manjari Rain1‡ Goverdhan Dutt Puri2†
Goverdhan Dutt Puri2† Aashish Bhalla3†
Aashish Bhalla3† Pramod Avti4*‡
Pramod Avti4*‡ Balachundhar Subramaniam5
Balachundhar Subramaniam5 Vipin Kaushal6
Vipin Kaushal6 Vinod Srivastava7
Vinod Srivastava7 Pranay Mahajan6
Pranay Mahajan6 Mini Singh8
Mini Singh8 Navin Pandey6
Navin Pandey6 Pankaj Malhotra3
Pankaj Malhotra3 Sonu Goel9
Sonu Goel9 Krishan Kumar10
Krishan Kumar10 Naresh Sachdeva11
Naresh Sachdeva11 Kalyan Maity1,12
Kalyan Maity1,12 Prashant Verma1,13
Prashant Verma1,13 Nishant Dixit14
Nishant Dixit14 Sheetal Jindal Gupta1,12
Sheetal Jindal Gupta1,12 Priya Mehra1,15
Priya Mehra1,15 Pooja Nadholta1
Pooja Nadholta1 Radhika Khosla1
Radhika Khosla1 Shweta Ahuja16
Shweta Ahuja16 Akshay Anand1,17,18*‡
Akshay Anand1,17,18*‡Background: Regulated breathing facilitates ventilation and reduces breathlessness. However, the effect of Yogic breathing on patients with COVID remains unclear. We aimed to evaluate the efficacy of two breathing protocols, i.e., short breathing technique (SBT) and long duration breathing technique (LBDT).
Methods: Three groups including COVID-positive patients, COVID-recovered patients, and healthcare workers (HCWs) were included in the study and segregated into Yoga and control groups. SBT was administered to COVID-positive patients. Both SBT and LBDT were administered to COVID-recovered patients and HCWs. A total of 18 biochemical parameters, a 6-min walk test (6MWT), and a 1-min sit-stand test (1MSST) were assessed on 0th, 7th, and 15th days, where biochemical parameters were the primary outcome. Pre-post estimation of neuropsychological parameters (nine questionnaires) and heart rate variability (HRV) were carried out. The paired t-test or Wilcoxon rank test was applied for pre-post comparison and the Student's t-test or Mann–Whitney U test was used for group comparison. Repeated measures test was applied for data recorded at three time points.
Results: A significant elevation in white blood cell (WBC) count was observed in COVID-positive intervention (p < 0.001) and control groups (p = 0.003), indicating no role of intervention on change in WBC number. WBC count (p = 0.002) and D-dimer (p = 0.002) significantly decreased in the COVID-recovered intervention group. D-dimer was also reduced in HCWs practicing Yogic breathing as compared to controls (p = 0.01). D-dimer was the primary outcome, which remained below 0.50 μg/ml (a cutoff value to define severity) in the COVID-positive yoga group (CYG) and decreased in the COVID-recovered yoga group (RYG) and the HCW yoga group (HYG) after intervention. A 6-min walk test (6MWT) showed an increase in distance covered among the COVID-positive patients (p = 0.01) and HCWs (p = 0.002) after intervention. The high-frequency power (p = 0.01) was found to be reduced in the COVID-positive intervention group. No significant change in neuropsychological parameters was observed.
Conclusion: Yogic breathing lowered D-dimer, which is helpful in reducing thrombosis and venous thromboembolism in patients with COVID-19 besides lowering the chances of vaccine-induced thrombotic thrombocytopenia in vaccinated individuals. The breathing intervention improved exercise capacity in mild to moderate cases of COVID-19. Further studies can show if such breathing techniques can influence immunity-related genes, as reported recently in a study. We suggest that Yogic breathing may be considered an integrative approach for the management of patients with COVID.
Trial registration: http://ctri.nic.in/Clinicaltrials/login.php, identifier: CTRI/2020/10/028195.
Prevention of COVID-19 and its management has been a daunting task worldwide. Post-COVID complications have also posed several challenges with children being most vulnerable to COVID infections (1). The ongoing public health crisis associated with new variants of COVID-19 and comorbidities (heart disease, diabetes, respiratory problems, and immune disorders) has escalated the fatality rates, adversely impacting the resource-deficient countries with the large population (2–4). The possibility of COVID-like outbreaks appears more likely than previously thought, and it is likely that previously developed vaccines will not be as effective for new variants like omicron (5, 6).
An integrative treatment protocol combining traditional knowledge with modern medicine is being developed in India to manage COVID-19 (7, 8). In some recent studies, various treatment modalities have been proposed to test the effectiveness of yoga and meditation; however, the outcome measures have remained limited to subjective measures (2, 5, 7, 9).
Popular practices like yoga, meditation, and Ayurveda are often argued as affordable adjunct therapies that may reduce the risks of infectious diseases associated with respiratory distress (2, 5, 7, 9–13). A deep breathing technique has also been shown to have promising results in COVID-19 management with a few physicians using it for patients with COVID-19 (14). Yogic breathing techniques are believed to facilitate ventilation and are instrumental in reducing breathlessness, thereby bringing comfort to patients in isolation (15–17). Such techniques alleviate stress, anxiety, and psychosomatic symptoms, improve cognition, and are useful in the management of diabetes and hypertension (18–24). It has been previously shown that meditation and yoga result in a decrease in hemoglobin A1c (HbA1C, a diabetes biomarker) levels, inflammation, and oxidative stress besides improving the lipid profile in diabetes and hypertension, contributing to COVID-19 risk reduction (20–23). These comorbid conditions are well known to exacerbate the severity of COVID-19 (25–27). Therefore, breathing techniques that can improve the respiratory capacity are ideal for studying their efficacy in COVID-19 management.
This study analyzes the effectiveness of yogic breathing techniques, i.e., short breathing technique (SBT) and longer duration breathing technique (LDBT), in the management of COVID-19. We aimed to investigate the effect of 15-day yogic breathing intervention (short and long duration) during COVID-19 infection, post-COVID-19 infection, and among healthcare workers (HCWs), all of whom are vulnerable to the disease while working in COVID-19 wards. The results were obtained by analyzing neuropsychological and biochemical parameters in tandem with the assessment of heart rate variability (HRV) and 6-min walk test (6MWT). A 1-min sit-stand test (1MSST) that is a reliable triage marker was also included in this study (28). A control non-intervention group was also included. In addition, to test the interindividual variability in disease presentation and different outcomes of intervention, we clinically stratified the study participants into different Prakriti, which is a basic constitution of an individual described in Ayurveda, an ancient Indian medical system. Prakriti of an individual renders a person to certain personality and physiological outcomes, thus predisposing them to certain health conditions (16, 17). Recent studies have reported genetic predisposition for COVID-19 infection, progression, and immune response (29–34). It is to be noted here that human leukocyte antigen (HLA), which is associated with COVID-19, has varying genotype across different Prakriti types (33–35). Interestingly, biochemical profiles, such as biomarkers of liver function, lipid profiles, and hemoglobin (Hb), which are readily checked in patients with COVID-19, differ among Prakriti types (36). Thus, evaluating clinical and biochemical parameters based on Prakriti can provide important insights into the treatment of COVID-19.
Prakriti has been described to be the result of the interaction of genetic and environmental factors and has a difference in molecular framework involving transport, regulation of cyclin-dependent protein kinase activity, immune response, and regulation of blood coagulation as reported by a whole-genome expression study (36, 37). Prakriti is widely believed to be inheritable (38). Individuals were assigned to different Prakriti types or doshas, namely, the Kapha, Pitta, Vata, and combination of these three by a qualified practitioner of Ayurveda based on their clinical phenotypes such as hair color, skin type, behavioral, and lifestyle preferences. Each of this dosha is responsible for a specific physiological process. Broadly, Kapha regulates lubrication, cohesion, and structure; Pitta regulates energy; and Vata regulates movements (39).
The biochemical parameters were the primary outcome of the study as some of these were routinely tested among patients with COVID-19 to define severity and modify treatment accordingly.
The study was registered under the Clinical Trials Registry – India (CTRI/2020/10/028195) on 1 October 2020. The study subjects were recruited from Nehru Hospital Extension (NHE), Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, after the approval from the Institutes Ethics Committee (IEC no. IEC-05/2020-1646), between October 2020 and January 2021. Three groups were identified for this study, namely, (1) COVID-positive group included patients who were confirmed positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at the time of the recruitment, (2) COVID-recovered group represented those who were positive at least 1 month before the recruitment, and (3) HCW group comprised those individuals working at NHE/COVID-19 block of PGIMER, Chandigarh, India. HCWs were negative for COVID-19 before and during the study. The COVID-positive group was followed for 45 more days to document any episode of recurrence. The details of admitted COVID-positive patients were provided by NHE staff daily; the patients were approached in person to explain the study and recruited after consent was obtained. The recruitment in the COVID-positive group was carried out following the Institute's Ethical Guidelines under PPE protection. NHE staff also provided the details of previously admitted COVID patients (who had recovered); these patients were contacted over the phone and recruited under the COVID-recovered group after consent was obtained. HCWs working at NHE were recruited under the third group after obtaining consent.
Furthermore, each group was randomly divided into two subgroups by manual chit-picking method; the subgroups included an intervention or yoga group and a non-intervention or control group. The groups were COVID-positive control group (CCG), COVID-positive yoga group (CYG), COVID-recovered control group (RCG), COVID-recovered yoga group (RYG), HCW control group (HCG), and HCW yoga group (HYG). The participants' age varied from 20 to 65 years. The subjects were not recruited if they were yoga practitioners or refused to give consent. Patients with COVID-19 on ventilators, not cleared by treating clinicians for the breathing yoga protocols, or with epilepsy, brain tumor, brain aneurysm, pregnancy, and other critical health conditions were excluded.
The protocol for breathing intervention was based on the theoretical framework of Yogic scriptures and is harmless. It included two techniques, namely, SBT (Supplementary Table 1, Supplementary Video 1) and LDBT (Supplementary Video 2) (40). SBT was administered in the morning to the COVID-19 yoga group for 15 days. SBT and LDBT was administered in the morning and evening, respectively, to the yoga group of COVID-recovered and HCWs for 15 days. Certified yoga trainers administered yogic breathing intervention via video to subjects with COVID-positive and via video calls to other two groups. Videos and/or pictures of the interventions were recorded, and records were retained following the approved research protocols by researchers to increase the data credibility and validity.
SBT, LDBT, or any other forms of exercise were not provided to the control group. Controls were under usual clinical care and were not wait-listed for intervention.
Videos and/or pictures were captured during randomization and data collection for transparency and fidelity measurement. The data were compiled on Microsoft Excel, and the entries were validated twice by two blinded researchers, before analysis, in order to maintain the accuracy of curated data. The validated data were subjected to various quality control measures based on the data type. Hence, the sample size was shown differently for each parameter.
Many participants did not give consent to the 7th-day blood sampling, which resulted in performing the analysis for the baseline, and the 15th day for the biomarker analysis. One participant in HYG was excluded from biomarker analysis as 15th-day sampling could not be done due to drop out of the participant.
Neuropsychological data were quality controlled by excluding the participants who did not attempt to complete ≥80% of the total pre- or post-questionnaires. Each questionnaire with over 80% answered questions was considered for analysis. Post-Traumatic Growth Inventory (PTGI) was not considered for estimating the cutoff value because all participants did not experience trauma or considered COVID-19 to be a traumatic situation.
For 6MWT and 1MSST, participants were considered for repeated measure analysis when measurements were made on all three time points. The sample size was the same for 6MWT and 1MSST, except for one participant of RYG, who could not perform 1MSST on the 15th day due to health issues. Hence, he was excluded from the 1MSST analysis. Similarly, HRV data were considered if the recording of 360 s was available for baseline and 15th day. The final sample size is mentioned in each Table and Figure.
The included blood markers were routinely checked for monitoring the health of patients. Hence, these biochemical parameters were the primary outcome of the study and the remaining parameters were the secondary outcome. Several biomarker tests, namely, complete blood count (CBC), Hb, activated partial thromboplastin time (aPTT), D-dimer, cortisol, procalcitonin, liver function test (LFT), and renal function test (RFT) were conducted on the baseline, 7th, and 15th days for control and yoga groups. LFT included alanine transaminase (ALT), aspartate transaminase (AST), conjugated bilirubin, total bilirubin, and alkaline phosphatase (ALP) tests, and RFT included creatinine, C-reactive protein (CRP), calcium, and urea.
An automated cell counter was used for CBC, Hb, and aPTT. D-dimer was estimated by Nephelometry using a MISPA-i2 detection kit (AGAPPE Diagnostic Ltd., India). Elecsys BRAHMS PCT and Elecsys CORTISOL kit (Roche Molecular Diagnostics, USA) were used to detect procalcitonin and cortisol, respectively. The enzymatic assay was done for detecting ALT, AST, and ALP (Arkray, Japan). In addition, bilirubin (conjugated and total) was detected by the Diazo method using a T&D Bilirubin kit (Arkray, Japan). The urease method was used for detecting urea (Arkray, Japan) and the Jaffe's method was used for estimating creatinine (Q-line, POCT Services Pvt Ltd., India). The o-cresolphthalein complexone (OCPC) method was used for estimating calcium (Arkray, Japan), and Turbigold CRP Test Kit (Arkray, Japan) was used for estimating CRP.
Mental wellbeing, wellness, resilience, and quality of life were measured using questionnaires at the baseline and on the 15th day. Stress was measured by the Perceived Stress Score (PSS), and changes in mood states were measured by Profile of Mood States (POMS). The Mindful Attention Awareness Scale (MAAS) was used to evaluate mindfulness, and the Dispositional Positive Emotion Scales – JOY subscale (DPES-JOY) was administered to assess joy. Anxiety and depression were assessed by the Patient Health Questionnaires (PHQ-4), and the Warwick-Edinburgh Wellbeing Scale (WEMWBS) was used to evaluate patients' overall wellbeing. The Brief Resilience Scale (BRS) and PTGI measured resilience (toward any trauma). Quality of life was estimated by using the WHO Quality of Life (WHOQOL) scale. WHOQOL has four domains, where Domain one represents physical health, Domain two measures psychological health, Domain three corresponds to social relationships, and Domain four assesses environmental health. Prakriti was assessed by the Sushrutha Prakriti Inventory Questionnaire.
A 6MWT was performed to assess the aerobic exercise capacity and endurance on baseline, 7th, and 15th days as per the published protocol (41). The specific distance was measured using a measuring tape, and two ends were marked on the available space. All participants were requested to walk for 6 min between the two points without talking or using the phone. Cardiovascular physiological parameters like pulse rate (PR), oxygen saturation (SpO2) (Crosso Pulse Oximeter, India), and blood pressure (Morepen Laboratories Ltd., India) were monitored before and after the walk. The covered distance was recorded for each participant, and the participants were requested to rate how much tiredness/breathlessness they felt during the walk using the Borg Breathless Scale, ranging between 0 and 10.
The participants performed the 1MSST on a standard chair/stool with a height of 46–48 cm. The chair was without an armrest and had a flat seat. Participants sat upright straight with their knees bent to 90° on the chair with folded hands in front to avoid taking any support during movement (42). A stopwatch was used to measure participants' cycles of one sit and one stand for 1 min. Participants were instructed to stand straight and sit straight on the chair with their bottom touching the seat without leaning back. SpO2, PR, and blood pressure were recorded before and after the test on the baseline, 7th, and 15th days.
Electrocardiogram (ECG) captured on the baseline and 15th day was used to analyze HRV. MP45 HRV Machine (BIOPAC systems, Inc., CA, USA) that used the Biopac Student Lab software version 4.1.1 and Physiograph-D (Recorders Medicare Systems Pvt. Ltd., India) that used the Physiograph-D software were used to calculate HRV. The MP45 HRV instrument was used in the COVID-positive group.
IBM SPSS version 21.0 was used for statistical analysis. A paired t-test or Wilcoxon rank test was applied to estimate significance in blood markers and neuropsychological parameters, depending upon whether the data are normal or non-normal. Similarly, subgroup comparisons were performed by the Student's t-test or Mann–Whitney U-test. A repeated measure was used to evaluate the change in the difference between before-test and after-test measures of SpO2, PR, and blood pressure for 1MSST and 6MWT. In 6MWT, the difference in distance was evaluated by ANOVA and Tukey's post-hoc test. The significance level was p-value ≤ 0.05. P-values were adjusted with age and gender for comparisons between the subgroups and correlations. The Bonferroni correction for multiple comparisons was performed wherever applicable.
The data for the patients with COVID-19 were acquired from NHE, PGIMER, Chandigarh, India, from which COVID-positive and COVID-recovered subjects were recruited. HCWs posted at NHE were also recruited in the third group. The details of enrolment and 6 subgroups are summarized in Figure 1. The sociodemographic data included age, body mass index (BMI), gender, smoking and alcohol consumption, diet, physical activity, and duration of sleep. A significant difference was observed in the age of RCG and RYG (p = 0.04) and the diet of HCG and HYG (p = 0.03) (Supplementary Table 2). None of the COVID-positive patients showed recurrence of COVID-19 after 45 days of study.
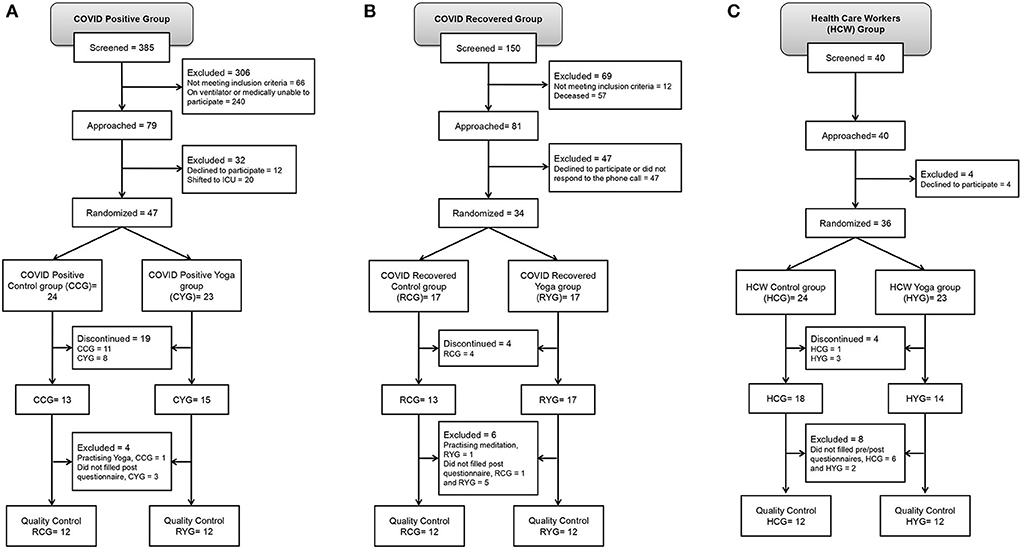
Figure 1. Study participant recruitment as per CONSORT. (A) COVID-positive group, (B) COVID-recovered group and (C) HCW group.
A significant increase in WBC count was observed in CYG and CCG, as the condition of patients improved in both the subgroups (Table 1). WBC count significantly decreased in RYG after intervention (Table 1). D-dimer was found high in RYG at baseline, which was reduced after the intervention (Table 1). In the HCW group, ALP was found to be decreased significantly after the intervention, while ALT was found to be increased, and creatinine was found to be decreased significantly in the control subgroup (Table 1). The low levels of cortisol were observed in HYG than in HCG on the 15th day (Table 1). The cutoff value for significance was 0.003 after the Bonferroni correction.
Yogic breathing is known to improve psychological parameters such as stress, anxiety, awareness, and quality of life (18, 19). Nine neuropsychological questionnaires were used to evaluate these parameters. However, neuropsychological changes were not found significant in any of the groups after 15 days of the intervention (Supplementary Tables 3–5). The Prakriti type of participants infected with SARS-CoV-2 (COVID-positive and COVID-recovered) were predominantly Kapha (48.9 %), followed by Pitta (34.0 %), Vata (12.8 %), and a combination of Kapha-Pitta (4.3 %).
The 6MWT showed increased exercise capacity and stamina among participants practicing SBT in the COVID-positive group and both SBT and LDBT in the HCW group. The distance covered was significantly more in the CYG and HYG on the 15th day as compared to the baseline (Figure 2). It was greater in the HYG on the 7th and 15th days as compared to HCG. Although a greater covered distance was observed in CYG than in CCG on the 15th day, the difference was not significant (Figure 2). No specific trend was noticed in the clinical parameters measured before and after the 6MWT (Supplementary Table 6). Similarly, no comparable trend was observed in clinical parameters estimated during 1MSST (Supplementary Table 7).
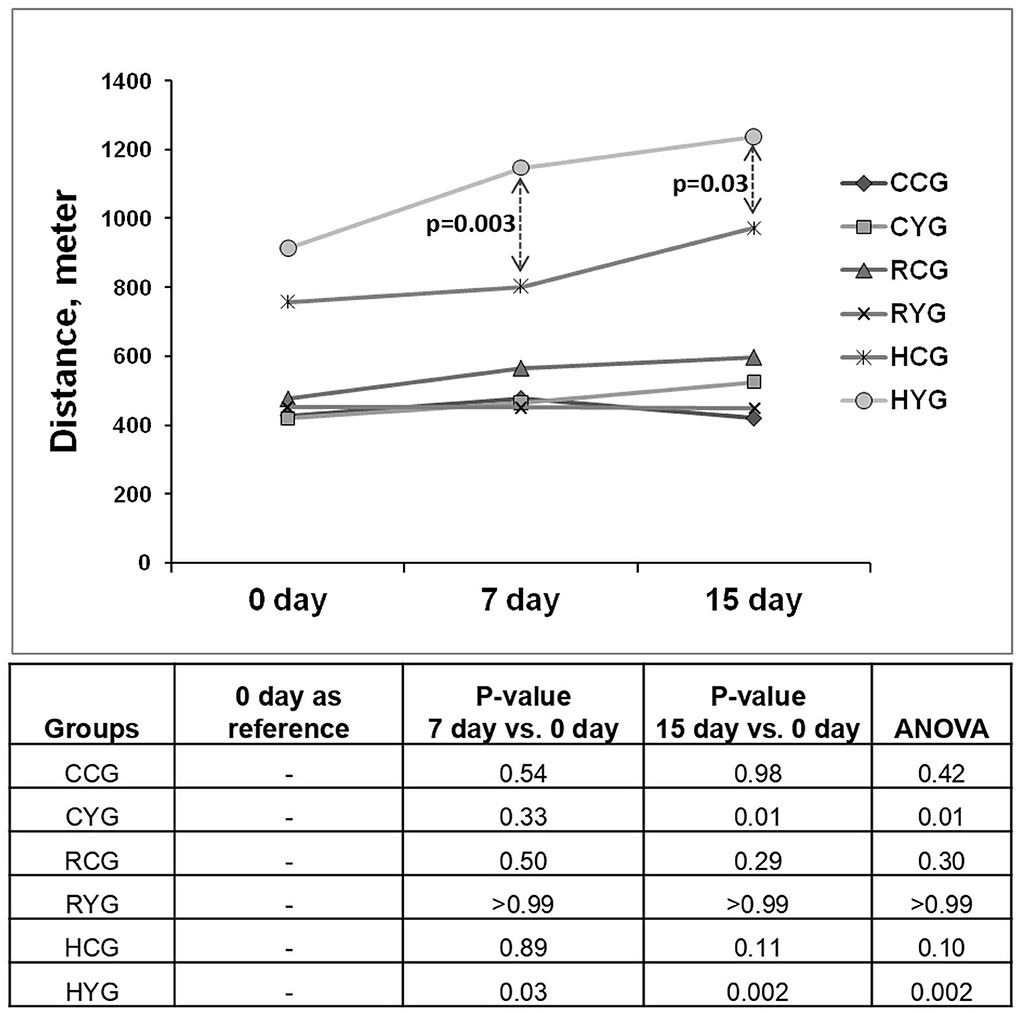
Figure 2. Distance covered in 6-min walk test. Significance was observed at p ≤ 0.05. P-values calculated for between-group comparisons were adjusted with age and gender. CCG (N = 10), COVID-positive control group; CYG (N = 12), COVID-positive yoga group; RCG (N = 8), COVID-recovered control group; RYG (N = 10), COVID-recovered yoga group; HCG (N = 7), HCW control group; HYG (N = 12), HCW yoga group.
The root mean square of the successive difference (RMSSD), which is a measure of HRV, was not significantly found to be altered in any group. Heart rate was noted to be lower (significant before the Bonferroni correction) in CYG than in CCG after intervention. Furthermore, high-frequency power (HF%) was significantly reduced in CYG. No changes were observed in the HRV of the COVID-recovered or HCW group (Supplementary Table 8).
Furthermore, there was no correlation of distance covered under 6MWT with neuropsychological and biochemical parameters.
The correlation between neuropsychological and biochemical parameters was also evaluated but no correlation was observed. Each intervention group was also analyzed based on Prakriti type. The investigated clinical, biochemical, and neuropsychological parameters were compared within each Prakriti type, and the three Prakriti types were compared with each other. However, no significant and conclusive observations were noted.
The breathing interventions in the COVID-positive patients, COVID-recovered patients, and HCWs show encouraging results with respect to a D-dimer and exercise capacity. WBC count was found to be increased in the COVID-positive subjects regardless of intervention because WBC count is low at the baseline in patients due to viral infection and it improves with health. We observed that D-dimer, a predictor of COVID-19 severity, was maintained below 0.50 μg/ml in CYG, but it was found to be increased in CCG. Elevated D-dimer with ≥0.50 μg/ml level indicates the formation and destruction of thrombus in the body (43–45). D-dimer was also decreased in RYG and HYG practicing breathing protocols (Table 1). Lowering D-dimer by yogic breathing may be helpful in reducing thrombosis and venous thromboembolism in patients with COVID-19 and in lowering the chances of vaccine-induced thrombotic thrombocytopenia in vaccinated individuals (46–49). These findings suggest that the severity of COVID-19 can possibly be modulated by practicing Yogic breathing techniques. However, a study on severe cases is warranted to validate these results in the future.
The 6MWT is a test that can aid in assessing the respiratory capacity, exercise, or functional capacity of patients with cardiopulmonary or pulmonary disease (50). Breathing intervention improved exercise capacity and stamina in CYG and HYG over a period of 15 days, which was noticed more in the yoga groups than in their respective control groups. Increased distance covered in CYG also suggests an improved prognosis (51, 52). In addition, HF% was found to be lowered in the CYG. Reduced HF% indicates decreased parasympathetic activity.
Integrating SBT and LBDT in COVID and post-COVID management appears to be beneficial and perhaps essential with emerging new variants every few months. The recent SARS-CoV-2 variant, omicron, which originated in November 2021, is resistant to the existing treatment and vaccination as it has been reported to not being neutralized by antibodies present in vaccinated and COVID-positive patients' sera (4, 6). A booster dose of Pfizer was able to generate neutralizing response against omicron but it was lower than that against the delta variant (6). Hence, exploring different strategies in COVID-19, including controlled breathing achieved by mindfulness meditation (SBT and LBDT), is useful. Immunity can be enhanced by meditation possibly by upregulating immune genes, which are dysfunctional in severe COVID-19, without affecting inflammatory genes (53).
In addition, we report that individuals with Prakriti-type Kapha are at a higher risk of getting infected with SARS-CoV-2, which was not reported earlier. The study suggests COVID-19 susceptibility of patients of Kapha dominant groups, followed by patients of Pitta, Vata, and a combination of Kapha-Pitta. In a recent study, Rajan et al. reported the highest frequency of Vata-Kapha Prakriti among 117 COVID-positive patients (54). Ayurgenomic approach has earlier shown that Prakriti type bears a relationship with genetic pathways. As reported in rheumatic arthritis, the Pitta group showed increased expression of oxidative stress genes and the Vata group was characterized by overexpression of inflammatory genes. This indicates the unexplored determinants of genetic pathways involved in disease (55). Prakriti types have been found to have unique genetic variability that could address phenotypic heterogeneity of patients and understand their disease susceptibility, conditioning, and predictive health outcomes (55, 56). Different trajectories of immune response, thrombosis, and bleeding are reported among the Prakriti types based on genetic variations in IFIT5 and SERPINA10 genes (57). These biological pathways are crucial in the case of COVID-19 and other infectious and noninfectious diseases. Moreover, genetic variants in HLA vary in different Prakriti types which is associated with susceptibility toward COVID-19 (33–35). Prakriti types also influence an individual's response toward an intervention, as it has been shown that only Pitta Prakriti individuals show an increment in oxygen saturation at high altitude after mindfulness meditation (58). We segregated the subjects according to Prakriti and evaluated neuropsychological and biochemical changes due to intervention in each type. However, significant trends could not be observed due to a small sample size. It would be attractive to investigate further whether types or combinations of complications, such as severe inflammation and requirement of ventilator, arise in various Prakriti types of patients with COVID-19. This may help examine the outcomes arising from dietary, environmental factors, yoga regimen, and lifestyle-related changes.
We highlight here some limitations that may affect the interpretation of the study. The sample size of the study was small due to a significant number of patients dropping out due to fear of growing mortality rate worldwide at that time. The fear that unconventional interventions (like SBT and LBDT) may have adverse effects on the prognosis, coupled with the scarce medical resources due to the COVID-19 outbreak, may have affected the outcomes. No significant neuropsychological changes were noticed in any of the groups. This may be due to the short duration of interventions. There was no difference between control and yoga groups in neuropsychology because the participants, irrespective of control or yoga groups, were known to the symptoms, vaccines, and underlying risks of COVID-19 through media and were under similar surroundings. Breathing exercise is generally more effective for symptomatic anxiety and when it is a trait in the individual, the breathing exercise did not have any effect on the situational anxiety created by COVID-19. One can assume that the large number of questionnaire may have disengaged the subjects from active participation. However, we tried to reduce disengagement by giving short intervals during questionnaire filling to avoid the fatigability effect. Doubts about the vaccine and the general uncertainty of the effectiveness of available medical help at that time may have influenced the psychological parameters and no change was observed. However, it has been reported that those who practice yoga are less stressed and could successfully cope with restrictions and adversity associated with COVID-19 during lockdown (13). Despite these limitations, we observed favorable outcomes in patients with COVID-19, a decrease in COVID-19 severity indicated by some of the biomarkers. The study could not include severe COVID-19 cases, as these patients were often mechanically supported for breathing and were unable to adapt to the breathing techniques. A shorter duration of intervention may have limited the scope of the study and might also have impacted the effectiveness of the interventions. A consistent practice of these breathing techniques over 4–6 weeks may have improved the outcomes, especially in measuring the neuropsychological outcomes.
In conclusion, the study revealed that breathing intervention lowered the D-dimer. Hence, the intervention was capable of reducing severity in mild to moderate cases of COVID-19. In addition, the exercise capacity and stamina of the patients improved, as a result of a breathing intervention protocol. The intervention can be easily administered to patients either in person or online. Therefore, this breathing protocol can be considered for integration in the management of COVID-positive and post-COVID cases.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Institutes Ethics Committee, PGIMER Chandigarh (IEC no. IEC-05/2020-1646). The patients/participants provided their written informed consent to participate in this study.
MR collected, validated and analyzed the data and wrote the first draft with Figures and Tables. Literature search and data interpretation were done by MR and AA. AA, PA, and BS conceptualized the study. AA designed the study. AA and VS edited and critically reviewed the manuscript. AB, GP, PA, AA, VK, PMah, MS, NP, PMal, SGo, KK, NS, and SA facilitated the study and critically reviewed the manuscript. KM, PV, ND, SGu, PMe, and PN collected the data, performed tests, and validated the data. RK validated and analyzed the data. All the authors have read and agreed to the final manuscript and authorship order.
Ministry of AYUSH, Government of India, New Delhi, India funded this study under grant no. Z-28015/48/2020-HPC (EMR)-AYUSH. The funds were provided for the execution of the study.
We acknowledge the Ministry of AYUSH, Government of India, New Delhi, India [Grant No. Z-28015/48/2020-HPC (EMR)-AYUSH] for funding this study. We extend our thanks to Dr. Ishwar Chander for guiding us in Prakriti assessment and Dr. Raman Nautiyal and Dr. Suresh Sharma for providing their valuable suggestions for statistical analysis. We are also grateful to Ms. Kanupriya and Ms. Priya Battu for helping in data collection and Ms. Navneet Kaur for helping in data analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.945988/full#supplementary-material
1. Ayres JS, A. metabolic handbook for the COVID-19 pandemic. Nat Metab. (2020) 2:572–85. doi: 10.1038/s42255-020-0237-2
2. Nagarathna R, Nagendra HR, Majumdar V. A perspective on yoga as a preventive strategy for coronavirus disease 2019. Int J Yoga. (2020) 13:89–98. doi: 10.4103/ijoy.IJOY_22_20
3. Rubin EJ, Baden LR, Abdool Karim SS, Morrissey S. audio interview: the omicron variant of SARS-CoV-2. N Engl J Med. (2021) 385:e96. doi: 10.1056/NEJMe2118839
4. WHO. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online at: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern. (2021).
5. Wadhen V, Cartwright T. Feasibility and outcome of an online streamed yoga intervention on stress and wellbeing of people working from home during COVID-19. Work. (2021) 69:331–49. doi: 10.3233/WOR-205325
6. Planas D, Saunders N, Maes P, Guivel-Benhassine F, Planchais C, Buchrieser J, et al. Considerable escape of SARS-CoV-2 omicron to antibody neutralization. Nature. (2022) 602:671–5. doi: 10.1038/s41586-021-04389-z
7. Kotwani P, Patwardhan V, Patel GM, Williams CL, Modi E. A holistic care approach to combat the COVID-19 disease. J Family Med Prim Care. (2021) 10:844–9. doi: 10.4103/jfmpc.jfmpc_1549_20
8. Mohanty S, Singh A, Avti P. Integrative medicine as a panpharmacon for COVID-19 pandemic: a call for global advocacy. Ann Neurosci. (2021) 28:8–10. doi: 10.1177/0972753120950052
9. Zope SA, Zope RA, Biri GA, Zope CS. Sudarshan Kriya Yoga: A Breath of Hope during COVID-19 Pandemic. Int J Yoga. (2021) 14:18–25. doi: 10.4103/ijoy.IJOY_102_20
10. Bushell W, Castle R, Williams MA, Brouwer KC, Tanzi RE, Chopra D, et al. Meditation and yoga practices as potential adjunctive treatment of SARS-CoV-2 infection and COVID-19: a brief overview of key subjects. J Altern Complement Med. (2020) 26:547–56. doi: 10.1089/acm.2020.0177
11. Mahalle NP, Kulkarni MV, Pendse NM, Naik SS. Association of constitutional type of Ayurveda with cardiovascular risk factors, inflammatory markers and insulin resistance. J Ayurveda Integr Med. (2012) 3:150–7. doi: 10.4103/0975-9476.100186
12. Sivapuram MS, Srivastava V, Kaur N, Anand A, Nagarathna R, Patil S, et al. Ayurveda body-mind constitutional types and role of yoga intervention among type 2 diabetes mellitus population of Chandigarh and Panchkula regions. Ann Neurosci. (2020) 27:214–23. doi: 10.1177/09727531211000040
13. Nagarathna R, Anand A, Rain M, Srivastava V, Sivapuram MS, Kulkarni R, et al. Yoga practice is beneficial for maintaining healthy lifestyle and endurance under restrictions and stress imposed by lockdown during COVID-19 pandemic. Front Psychiatry. (2021) 12:613762. doi: 10.3389/fpsyt.2021.613762
14. Hamzelou J. Can breathing exercises help protect you from COVID-19? New Sci. (2020) 246:10–1. doi: 10.1016/S0262-40792030789-2
15. Kaminsky DA, Guntupalli KK, Lippmann J, Burns SM, Brock MA, Skelly J, et al. Effect of yoga breathing (pranayama) on exercise tolerance in patients with chronic obstructive pulmonary disease: a randomized, controlled trial. J Altern Complement Med. (2017) 23:696–704. doi: 10.1089/acm.2017.0102
16. Sankar J, Das RR. Asthma - A disease of how we breathe: role of breathing exercises and pranayam. Indian J Pediatr. (2018) 85:905–10. doi: 10.1007/s12098-017-2519-6
17. Lu Y, Li P, Li N, Wang Z, Li J, Liu X, et al. Effects of home-based breathing exercises in subjects with COPD. Respir Care. (2020) 65:377–87. doi: 10.4187/respcare.07121
18. Erdogan Yüce G, Taşci S. Effect of pranayama breathing technique on asthma control, pulmonary function, and quality of life: a single-blind, randomized, controlled trial. Complement Ther Clin Pract. (2020) 38:101081. doi: 10.1016/j.ctcp.2019.101081
19. Sharma VK. M R, S V, Subramanian SK, Bhavanani AB, Madanmohan, et al. Effect of fast and slow pranayama practice on cognitive functions in healthy volunteers. J Clin Diagn Res. (2014) 8:10–3.
20. Sadhasivam S, Alankar S, Maturi R, Williams A, Vishnubhotla RV, Hariri S, et al. Isha Yoga practices and participation in samyama program are associated with reduced HbA1C and systemic inflammation, improved lipid profile, and short-term and sustained improvement in mental health: a prospective observational study of meditators. Front Psychol. (2021) 12:659667. doi: 10.3389/fpsyg.2021.659667
21. Viswanathan V, Sivakumar S, Sai Prathiba A, Devarajan A, George L, Kumpatla S. Effect of yoga intervention on biochemical, oxidative stress markers, inflammatory markers and sleep quality among subjects with type 2 diabetes in South India: results from the SATYAM project. Diabetes Res Clin Pract. (2021) 172:108644. doi: 10.1016/j.diabres.2020.108644
22. Yu Y, Gao Q, Xia W, Zhang L, Hu Z, Wu X, et al. Association between physical exercise and biomarkers of oxidative stress among middle-aged and elderly community residents with essential hypertension in China. Biomed Res Int. (2018) 2018:4135104. doi: 10.1155/2018/4135104
23. Khandekar JS, Vasavi VL, Singh VP, Samuel SR, Sudhan SG, Khandelwal B. Effect of yoga on blood pressure in prehypertension: a systematic review and meta-analysis. Sci World J. (2021) 2021:4039364. doi: 10.1155/2021/4039364
24. Divya K, Bharathi S, Somya R, Darshan MH. Impact of a yogic breathing technique on the well-being of healthcare professionals during the COVID-19 pandemic. Glob Adv Health Med. (2021) 10:2164956120982956. doi: 10.1177/2164956120982956
25. Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: a meta-analysis. Psychoneuroendocrinology. (2017) 86:152–68. doi: 10.1016/j.psyneuen.2017.08.008
26. Kiecolt-Glaser JK, Christian L, Preston H, Houts CR, Malarkey WB, Emery CF, et al. Stress, inflammation, and yoga practice. Psychosom Med. (2010) 72:113–21. doi: 10.1097/PSY.0b013e3181cb9377
27. Bali P, Kaur N, Tiwari A, Bammidi S, Podder V, Devi C, et al. Effectiveness of yoga as the public health intervention module in the management of diabetes and diabetes associated dementia in South East Asia: a narrative review. Neuroepidemiology. (2020) 54:287–303. doi: 10.1159/000505816
28. Guha Niyogi S, Agarwal R, Suri V, Malhotra P, Jain D, Puri GD. One minute sit-to-stand test as a potential triage marker in COVID-19 patients: a pilot observational study. Trends in Anaesth Crit Care. (2021) 39:5–9. doi: 10.1016/j.tacc.2021.04.007
29. Hou Y, Zhao J, Martin W, Kallianpur A, Chung MK, Jehi L, et al. New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis. BMC Med. (2020) 18:216. doi: 10.1186/s12916-020-01673-z
30. Verma S, Abbas M, Verma S, Khan FH, Raza ST, Siddiqi Z, et al. Impact of I/D polymorphism of angiotensin-converting enzyme 1 (ACE1) gene on the severity of COVID-19 patients. Infect Genet Evol. (2021) 91:104801. doi: 10.1016/j.meegid.2021.104801
31. Gómez J, Albaiceta GM, García-Clemente M, López-Larrea C, Amado-Rodríguez L, Lopez-Alonso I, et al. Angiotensin-converting enzymes (ACE, ACE2) gene variants and COVID-19 outcome. Gene. (2020) 762:145102. doi: 10.1016/j.gene.2020.145102
32. Guo X, Chen Z, Xia Y, Lin W, Li H. Investigation of the genetic variation in ACE2 on the structural recognition by the novel coronavirus (SARS-CoV-2). J Transl Med. (2020) 18:321. doi: 10.1186/s12967-020-02486-7
33. Wang F, Huang S, Gao R, Zhou Y, Lai C, Li Z, et al. Initial whole-genome sequencing and analysis of the host genetic contribution to COVID-19 severity and susceptibility. Cell Discov. (2020) 6:83. doi: 10.1038/s41421-020-00231-4
34. Nguyen A, David JK, Maden SK, Wood MA, Weeder BR, Nellore A, et al. Human leukocyte antigen susceptibility map for severe acute respiratory syndrome Coronavirus 2. J Virol. (2020) 94:e00510–20. doi: 10.1128/JVI.00510-20
35. Bhushan P, Kalpana J, Arvind C. Classification of human population based on HLA gene polymorphism and the concept of Prakriti in Ayurveda. J Altern Complement Med. (2005) 11:349–53. doi: 10.1089/acm.2005.11.349
36. Prasher B, Negi S, Aggarwal S, Mandal AK, Sethi TP, Deshmukh SR, et al. Whole genome expression and biochemical correlates of extreme constitutional types defined in Ayurveda. J Transl Med. (2008) 6:48. doi: 10.1186/1479-5876-6-48
37. Prasher B, Gibson G, Mukerji M. Genomic insights into ayurvedic and Western approaches to personalized medicine. J Genet. (2016) 95:209–28. doi: 10.1007/s12041-015-0607-9
38. Hankey A. Establishing the scientific validity of Tridosha part 1: Doshas, Subdoshas and Dosha Prakritis. Anc Sci Life. (2010) 29:6–18.
39. Bhat V, Borse S, Chavan-Gautam P, Joshi K. Exploring AyuGenomics approach for understanding COVID-19 predisposition and progression. J Ayurveda Integr Med. (2022) 13:100463. doi: 10.1016/j.jaim.2021.06.003
40. Rain M, Subramaniam B, Avti P, Mahajan P, Anand A. Can Yogic breathing techniques like Simha Kriya and Isha Kriya regulate COVID-19-related stress? Front Psychol. (2021) 12:635816. doi: 10.3389/fpsyg.2021.635816
41. Enright PL, McBurnie MA, Bittner V, Tracy RP, McNamara R, Arnold A, et al. Cardiovascular Health Study. The 6-min walk test: a quick measure of functional status in elderly adults. Chest. (2003) 123:387–98. doi: 10.1378/chest.123.2.387
42. Vaidya T, de Bisschop C, Beaumont M, Ouksel H, Jean V, Dessables F, et al. Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. Int J Chron Obstruct Pulmon Dis. (2016) 11:2609–16. doi: 10.2147/COPD.S115439
43. Zhang L, Zhang F, Yu W, He T, Yu J, Yi CE, et al. Antibody responses against SARS coronavirus are correlated with disease outcome of infected individuals. J Med Virol. (2006) 78:1–8. doi: 10.1002/jmv.20499
44. Bounds EJ, Kok SJ D Dimer. Treasure Island, FL: StatPearls Publishing. Available online at https://www.ncbi.nlm.nih.gov/books/NBK431064/. (2021).
45. Goldenberg NA, Knapp-Clevenger R, Manco-Johnson MJ. Mountain States Regional Thrombophilia Group. Elevated plasma factor VIII and D-dimer levels as predictors of poor outcomes of thrombosis in children. N Engl J Med. (2004) 351:1081–8. doi: 10.1056/NEJMoa040161
46. Lobbes H, Mainbourg S, Mai V, Douplat M, Provencher S, Lega JC. Risk factors for venous thromboembolism in severe COVID-19: a study-level meta-analysis of 21 studies. Int J Environ Res Public Health. (2021) 18:12944. doi: 10.3390/ijerph182412944
47. Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A. Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci. (2021) 428:117607. doi: 10.1016/j.jns.2021.117607
48. Favaloro EJ. Laboratory testing for suspected COVID-19 vaccine-induced (immune) thrombotic thrombocytopenia. Int J Lab Hematol. (2021) 43:559–70. doi: 10.1111/ijlh.13629
49. Hafeez MU, Ikram M, Shafiq Z, Sarfraz A, Sarfraz Z, Jaiswal V, et al. COVID-19 vaccine-associated thrombosis with thrombocytopenia syndrome (TTS): a systematic review and post hoc analysis. Clin Appl Thromb Hemost. (2021) 27:10760296211048815. doi: 10.1177/10760296211048815
50. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. (2014) 44:1428–46. doi: 10.1183/09031936.00150314
51. Mantha S, Tripuraneni SL, Roizen MF, Fleisher LA. Proposed modifications in the 6-minute walk test for potential application in patients with mild COVID-19: a step to optimize triage guidelines. Anesth Analg. (2020) 131:398–402. doi: 10.1213/ANE.0000000000004986
52. Paglia S, Nattino G, Occhipinti F, Sala L, Targetti E, Cortellaro F, et al. The quick walk test: a noninvasive test to assess the risk of mechanical ventilation during COVID-19 outbreaks. Acad Emerg Med. (2021) 28:244–47. doi: 10.1111/acem.14180
53. Chandran V, Bermúdez ML, Koka M, Chandran B, Pawale D, Vishnubhotla R, et al. Large-scale genomic study reveals robust activation of the immune system following advanced Inner Engineering meditation retreat. Proc Natl Acad Sci U S A. (2021) 118:e2110455118. doi: 10.1073/pnas.2110455118
54. Rajan S, Munjal Y, Shamkuwar M, Nimabalkar K, Sharma A, Jindal N, et al. Prakriti analysis of COVID 19 patients: an observational study. Altern Ther Health Med. (2021) 27:12–7.
55. Juyal RC, Negi S, Wakhode P, Bhat S, Bhat B, Thelma BK. Potential of ayurgenomics approach in complex trait research: leads from a pilot study on rheumatoid arthritis. PLoS ONE. (2012) 7:e45752. doi: 10.1371/journal.pone.0045752
56. Aggarwal S, Negi S, Jha P, Singh PK, Stobdan T, Pasha MA, et al. Indian Genome Variation Consortium, Prasher B, Mukerji M. EGLN1 involvement in high-altitude adaptation revealed through genetic analysis of extreme constitution types defined in Ayurveda. Proc Natl Acad Sci U S A. (2010) 107:18961–6.
57. Abbas T, Chaturvedi G, Prakrithi P, Pathak AK, Kutum R, Dakle P, et al. Whole exome sequencing in healthy individuals of extreme constitution types reveals differential disease risk: a novel approach towards predictive medicine. J Pers Med. (2022) 12:489. doi: 10.3390/jpm12030489
Keywords: COVID-19, breathing technique, D-dimer, mindfulness, yoga, SpO2
Citation: Rain M, Puri GD, Bhalla A, Avti P, Subramaniam B, Kaushal V, Srivastava V, Mahajan P, Singh M, Pandey N, Malhotra P, Goel S, Kumar K, Sachdeva N, Maity K, Verma P, Dixit N, Gupta SJ, Mehra P, Nadholta P, Khosla R, Ahuja S and Anand A (2022) Effect of breathing intervention in patients with COVID and healthcare workers. Front. Public Health 10:945988. doi: 10.3389/fpubh.2022.945988
Received: 17 May 2022; Accepted: 29 August 2022;
Published: 30 September 2022.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Mansoor Malik, Johns Hopkins Medicine, United StatesCopyright © 2022 Rain, Puri, Bhalla, Avti, Subramaniam, Kaushal, Srivastava, Mahajan, Singh, Pandey, Malhotra, Goel, Kumar, Sachdeva, Maity, Verma, Dixit, Gupta, Mehra, Nadholta, Khosla, Ahuja and Anand. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akshay Anand, YWtzaGF5MWFuYW5kQHJlZGlmZm1haWwuY29t; Pramod Avti, cHJhbW9kLmF2dGlAZ21haWwuY29t
†These authors have contributed equally to this work and share second authorship
‡ORCID: Manjari Rain orcid.org/0000-0002-1016-2789
Pramod Avti orcid.org/0000-0001-5603-4523
Akshay Anand orcid.org/0000-0001-9003-3532
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.