
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 26 July 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.937008
This article is part of the Research TopicCOVID-19: Integrating Artificial Intelligence, Data Science, Mathematics, Medicine and Public Health, Epidemiology, Neuroscience, Neurorobotics, and Biomedical Science in Pandemic Management, volume IIView all 92 articles
Background: The characteristic symptom of coronavirus disease 2019 (COVID-19) is respiratory distress, but neurological symptoms are the most frequent extra-pulmonary symptoms. This study aims to explore the current status and hot topics of neurology-related research on COVID-19 using bibliometric analysis.
Methods: Publications regarding neurology and COVID-19 were retrieved from the Web of Science Core Collection (WoSCC) on March 28 2022. The Advanced search was conducted using “TS = (‘COVID 19’ or ‘Novel Coronavirus 2019’ or ‘Coronavirus disease 2019’ or ‘2019-nCOV’ or ‘SARS-CoV-2’ or ‘coronavirus-2’) and TS = (‘neurology’or ‘neurological’ or ‘nervous system’ or ‘neurodegenerative disease’ or ‘brain’ or ‘cerebra’ or ‘nerve’)”. Microsoft Excel 2010 and VOSviewer were used to characterize the largest contributors, including the authors, journals, institutions, and countries. The hot topics and knowledge network were analyzed by CiteSpace and VOSviewer.
Results: A total of 5,329 publications between 2020 and 2022 were retrieved. The United States, Italy, and the United Kingdom were three key contributors to this field. Harvard Medical School, the Tehran University of Medical Sciences, and the UCL Queen Square Institute of Neurology were the major institutions with the largest publications. Josef Finsterer from the University of São Paulo (Austria) was the most prolific author. Tom Solomon from the University of Liverpool (UK) was the most cited author. Neurological Sciences and Frontiers in Neurology were the first two most productive journals, while Journal of Neurology held the first in terms of total citations and citations per publication. Cerebrovascular diseases, neurodegenerative diseases, encephalitis and encephalopathy, neuroimmune complications, neurological presentation in children, long COVID and mental health, and telemedicine were the central topics regarding the neurology-related research on COVID-19.
Conclusion: Neurology-related research on COVID-19 has attracted considerable attention worldwide. Research topics shifted from “morality, autopsy, and telemedicine” in 2020 to various COVID-19-related neurological symptoms in 2021, such as “stroke,” “Alzheimer's disease,” “Parkinson's disease,” “Guillain–Barre syndrome,” “multiple sclerosis,” “seizures in children,” and “long COVID.” “Applications of telemedicine in neurology during COVID-19 pandemic,” “COVID-19-related neurological complications and mechanism,” and “long COVID” require further study.
The coronavirus disease (COVID-19) pandemic continues, with new cases continuing to rise globally (1). As of 24 April 2022, more than 500 million confirmed cases and more than 6 million deaths have been recorded (https://covid19.who.int/). Although the characteristic symptom of COVID-19 is respiratory distress, neurologic symptoms are the most common extra-pulmonary symptoms (2), such as headaches, anosmia, cognitive dysfunction, and acute cerebrovascular disorders, which have been reported in numerous studies (3, 4). These symptoms appear to be a combination of nonspecific complications of systemic disease, effects of direct viral infection, or inflammation of the neurological and vascular systems (3). Varatharaj et al. conducted a national inter-professional surveillance study, including 153 patients with acute neurological and psychiatric complications associated with COVID-19. Of these, 62% (77/125) of them presented with cerebrovascular events, including 57 with ischemic strokes, nine with cerebral hemorrhages, and one with central nervous system vacuity. Overall, 31% (39/125) of the patients presented with altered mental status, including nine with unspecified encephalopathy and seven with encephalitis (5). In addition, the long-term neurological symptoms of acute sequelae of COVID-19 or “long COVID” can affect the entire spectrum of COVID-19 patients, ranging from mild to severe. Similar to acute COVID-19, long COVID may involve multiple organs and affect many systems, especially the neurological system. Symptoms of long COVID include fatigue, dyspnea, cardiac abnormalities, cognitive impairment, sleep disturbances, PTSD symptoms, muscle pain, distraction, and headaches (6). Considering the variety of neurological symptoms and complications of COVID-19, scholars have conducted many reviews on the association between COVID-19 and neurology (3, 7, 8). However, there are still some shortcomings that need to be addressed: (1) Most reviews use a meta-based approach, and this type of review does not provide an overview of all neurological research publications related to COVID-19. (2) Samples in some systematic reviews are subjectively screened, with small sample sizes. (3) The studies included were not comprehensive (e.g., reviews of randomized controlled trials or those with focus only on specific and limited aspects).
Bibliometric analysis is a widely accepted quantitative technique for analyzing big data of articles in a given field (9). It typically applies bibliometric tools (e.g., Bibliometrix R, Gephi, Pajek, CiteSpace, and VOSviewer) to analyze publication trends, popular articles, major contributors, central themes, and frontier topics in a given field (10). Several bibliometric analyses exist on different disciplines of COVID-19, such as pediatrics (11), urology (12), and rheumatology (13). These works provide readers and researchers with an overview of COVID-19-related research in specific disciplines. However, no study provides a state-of-the-art overview of neurology-related research on COVID-19. Therefore, in this study, we analyzed the neurology-related research on COVID-19 based on the WoSCC using the most popular bibliometric tools CiteSpace and VOSviewer (14). The aim of this article is to answer the following research questions.
• Question 1: What are the published trends in neurology-related research on COVID-19?
• Question 2: What are the most influential articles and major contributing authors, institutions, countries, and journals for neurology-related research on COVID-19?
• Question 3: Who are the potential collaborators (authors, institutions, countries/regions) for neurology-related research on COVID-19?
• Question 4: What are the important topics and frontier themes in neurology-related research on COVID-19?
Just as other bibliometric analysis steps, we began our search with the keyword “Neurology” or in the category of “Neuroscience and Neurology” on the WoSCC. However, the results did not include all publications on neurology and the COVID-19 discipline. Therefore, we used the following keywords: TS=(“COVID 19” or “Novel Coronavirus 2019” or “Coronavirus disease 2019” or “2019-nCOV” or “SARS-CoV-2” or “coronavirus-2”) and TS= (“neurology” or “neurology” or “neurological” or “neurodegenerative disease” or “brain” or “cerebral” or “neurological”) to filter publications in the field of neurology focused on COVID-19 or SARS-CoV-2. The online search was conducted on 28 March 2022 on the WoSCC. For this review, two researchers (Qian Zhang and Jian Li) independently searched the database, screening titles and abstracts and eliminating irrelevant articles. Any disagreements were resolved by discussing with the senior neurologist (Ling Weng) until consensus was reached.
We exported full records and cited references of all publications from the WoSCC. In addition, the bibliometric parameters (e.g., title, keywords, journal, publication year, citation, author, institution, country, and reference) were extracted. These data were then imported into Microsoft Excel 2010 (Redmond, WA, US) and VOSviewer (Leiden University, Leiden, and The Netherlands) to identify the most prolific contributors (e.g., prolific authors, institutions, and countries). In VOSviewer, node size is positively correlated with the number of articles. Co-authorship analysis was used to assess collaboration among different authors, countries, and institutions (15). The total link strength (TLS; the sum of link weights connected to a node) indicates the power of cooperation between two nodes. The width of links between two nodes is positively correlated with the cooperation strength. CiteSpace (version 5.8.R1) and VOSviewer were used to visualize keyword co-occurrence analysis and reference analysis (16).
Figure 1 illustrates the process of data screening and bibliometric analysis. After excluding articles written in languages other than English and limiting them to original articles and reviews, 5,341 publications remained. Of these, 12 articles containing the term “brain natriuretic peptide” and focusing on cardiovascular issues in patients with COVID-19 were excluded. Therefore, 5,329 publications were selected for further analysis, of which 72% were original articles (n = 3,829) and the rest were reviews (n = 1,500; Figure 2B). A total of 69,908 citations were received, with 13.12 citations per article and an H-index of 98. A total of 142 countries/regions, 7,684 institutions, 30,547 authors, and 1,646 journals contributed to these publications. Fudan University published the first article titled “A multicentre observational study on neonates exposed to SARS-CoV-2 in China: the Neo-SARS-CoV-2 study protocol” in China in March 2020 (17). The number of publications increased from 1,465 in 2020 to 3,177 in 2021 and 687 in the first 4 months of 2022 (Figure 2A).
The top 10 contributing countries are shown in Figure 3. The United States dominates the field, with 1,677 publications (31.4% of the total) and 31,371 total citations (44.8% of the total). Italy ranked second, with 628 publications and 7,691 total citations, and the United Kingdom ranked third, with 530 publications and 16,082 total citations (Figure 3A). We used VOSviewer to depict the international collaboration in this field. The minimum number of publications was set at 50. Finally, 28 countries were selected for visualization. The United States, Italy, the United Kingdom, India, and China are the largest nodes and more broadly connected, indicating their close collaboration and significant academic influence in the field (Figure 3B). The United Kingdom (115 TLS) and Canada (102 TLS) cooperate closely with the United States.
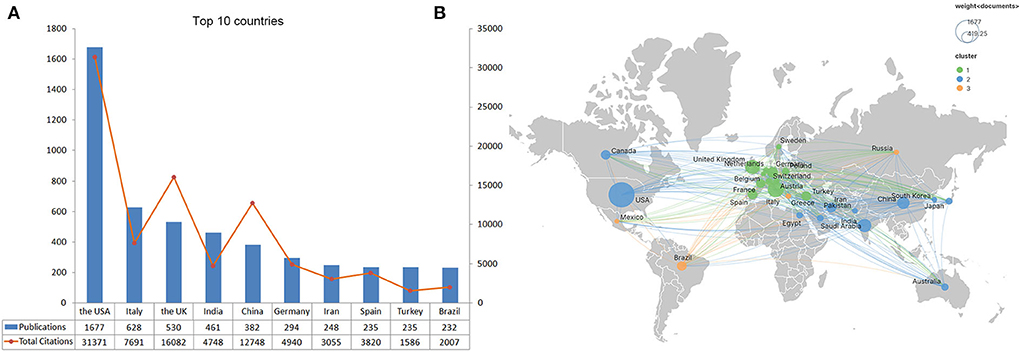
Figure 3. Top 10 prolific countries/regions and inter-national collaboration network of neurology-related research on COVID-19. (A) Number of publications and total citations for each country. (B) Collaboration among countries. Node size indicates the number of articles produced. The width of links indicated the cooperation strength.
Table 1 lists the top 10 most prolific and highly cited institutions for neurology-related research on COVID-19. Together, these institutions published 11.8% of the articles in the field. Specifically, Harvard Medical School (USA) ranked first, with 118 articles. The Tehran University of Medical Sciences (Iran) ranked second, with 68 articles. The UCL Queen Square Institute of Neurology ranked third, with 63 articles. Among the most influential institutions, the Huazhong University of Science and Technology (China), the UCL Queen Square Institute of Neurology (UK), and King's College London (UK) ranked the top three, with 6,162, 5,309, and 3,866 total citations, respectively. Figure 4A displays the network of collaborations among institutions. Harvard Medical School (US), Massachusetts General Hospital (US), and Mayo Clinic (US) are the central nodes in North America. King's College London (UK), the UCL Queen Square Institute of Neurology (UK), and the University of Liverpool (UK) present the central in the United Kingdom. The University of Milan plays an important role in Italy. The Tehran University of Medical Sciences (Iran) is a central node in the Middle East. Collaborations are more common among institutions that are geographically close to each other. As shown in Figure 4B, more collaborations occur among North American institutions.
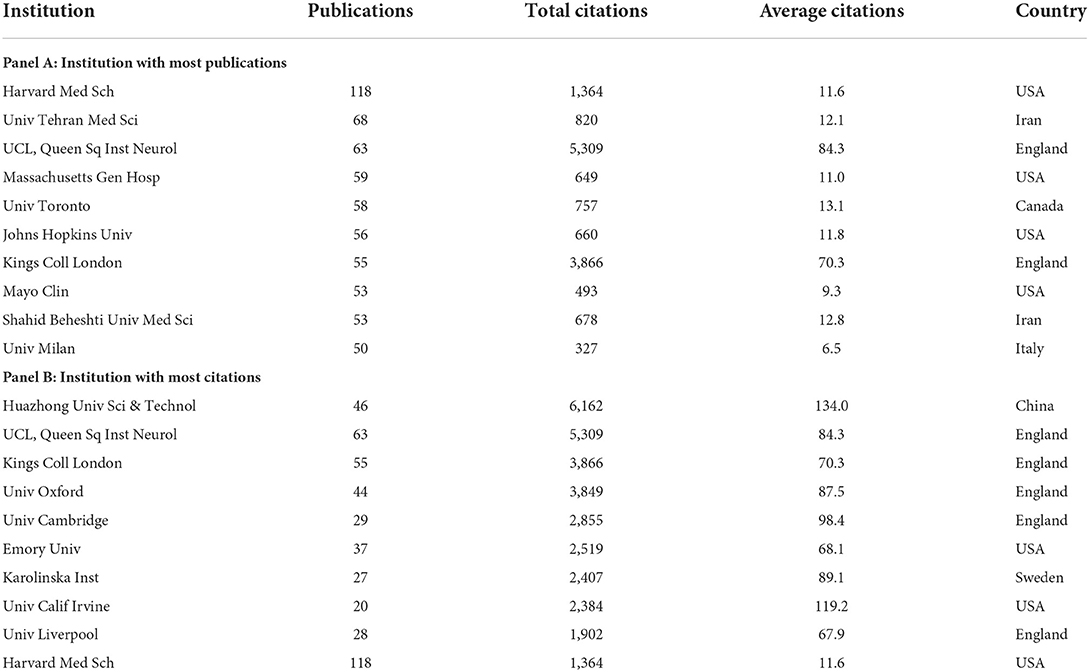
Table 1. The top 10 most prolific institutions and highly cited institutions for neurological COVID-19.
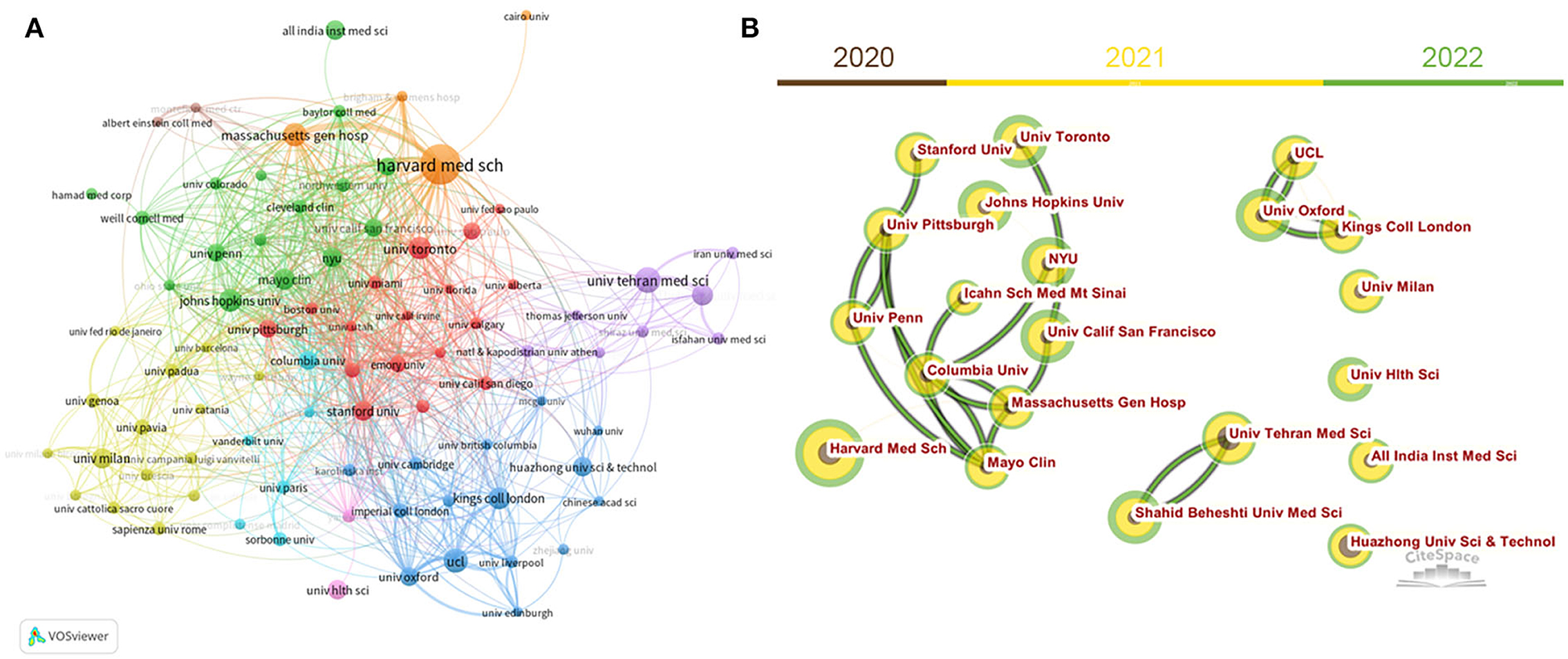
Figure 4. Inter-institution cooperative network built by VOSviewer (A) and CiteSpace (B). Node size indicates the number of articles produced. The width of links indicates the cooperation strength.
Table 2 lists the top 10 contributing authors for neurology-related research on COVID-19. The most prolific authors (n = 14 publications) were Josef Finsterer from the University of São Paulo (Austria), David García-Azorín from Hospital Clinical University Valladolid (Spain), Nima Rezaei from the Tehran University of Medical Sciences (Iran), and Henrik Zetterberg from the Queen Square Institute of Neurology (UK). The most influential author, however, was Tom Solomon from the University of Liverpool (UK), with 1,100 total citations and 185 citations per article, followed by Henrik Zetterberg from Sahlgrenska University (UK), with 581 total citations and 41.5 citations per article, and Ali Asadi-Pooya from the Shiraz University of Medical Science (Iran), with 482 total citations and 80.3 citations per article. Co-authorship of authors in VOSviewer was used to identify collaborations among researchers. The minimum number of publications was 6. Ultimately, 69 authors were included in the visual analysis. Figure 5A shows top 10 prolific authors in this field. Figure 5B displays the author collaborative network, with Alessandro Padovani (Italy) being the first-tier author with 47 TLS. Gioacchino Tedeschi (Italy) and Andrea Pilotto (Italy) were the first to collaborate with 46 TLS and 43 TLS, respectively.
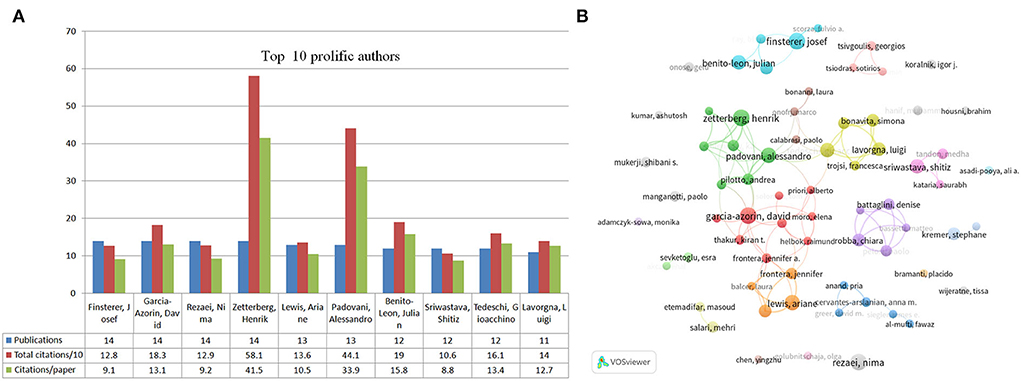
Figure 5. Top 10 most productive authors and collaboration among these authors. (A) Number of publications, total citations, and citations per publication in the top 10 prolific authors. (B) Collaboration among these prolific authors built by VOSviewer. Node size indicates the number of articles. The width of links indicates the cooperation strength.
The top 10 active journals contributed 14.9% of the articles in this field. Table 3 lists the top 10 active journals in a descending numerical order. Specifically, the top three prolific journals are Neurological Sciences (n = 121), Frontiers in Neurology (n = 118), and Cureus (n = 109). However, in terms of impact, Journal of Neurology ranked first (with 1,535 total citations), followed by Journal of Neuroscience (n = 1,359) and Frontiers in Neurology (n = 1,217).
Almost half of the top 20 most cited publications are the review type (Table 4). Mao et al. produced the most cited article published in JAMA Neurology entitled “Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China”, with 1,219 total citations (4). Most of the articles discussed neurological manifestations and complications related to COVID-19, such as stroke (18), meningitis/encephalitis (19), multiple sclerosis (20), and demyelinating diseases (21). Several publications discussed COVID-19-related mental health and neuropsychiatric manifestations (5, 22). Totally, five articles focused on the neuroinvasive mechanisms of SARS-CoV-2 (23–25).
To present the key references and hot topics in the field, we conducted a reference analysis with CiteSpace and a keyword co-occurrence analysis with VOSviewer. As shown in Figure 6A, CiteSpace identified key references in neurology-related research on COVID-19 for different time periods. The main topic focused on “ethics, autopsy, and telemedicine” in 2020 and shifted to the various COVID-19-related neurological complications in 2021, such as stroke, Guillain–Barre syndrome (GBS), epilepsy, and long COVID. The most cited references are considered to be the basis for the frontier direction in a given field. Therefore, the reference analysis in CiteSpace was used to identify key references related for neurology-related research on COVID-19. In Figure 6B, the top 24 references with the highest citation burst were identified. The highest citation burst reference was generated by Arabi et al. The authors described three patients infected with Middle East respiratory syndrome coronavirus (MERS-CoV)-associated neurological syndrome in 2015. It is emphasized that the CNS may also be a target of MERS-COV (26). The second highest citation burst was produced by Khosravani et al. In this article, the authors introduced a framework for the management of hyperacute stroke during the COVID-19 pandemic, providing guidelines for researchers and neurologists, neurosurgeons, and policymakers to manage patients with COVID-19 and stroke (27). In VOSviewer, we performed a keyword occurrence analysis (Figure 7). The minimum number of occurrences was 20. Thesaurus (Supplementary Table S1) was used to remove duplicate keywords, such as COVID 19. Novel coronavirus 2019 were replaced by COVID-19. Finally, 104 keywords were selected from a total of 9,443 keywords. The top six most frequent keywords were “COVID-19 (n = 3,367), SARS-CoV-2 (n = 1,780), stroke (n = 244), neurology (n = 181), neurological manifestation (n = 168), and telemedicine (n = 137)”. As shown in Figure 7, seven research directions were formed based on these keywords: (1) cerebrovascular diseases associated with COVID-19 (brown): stroke, ischemic stroke, cytokine storm, and coagulation disorders; (2) neurodegenerative diseases associated with COVID-19 (green): inflammation, ACE2, Alzheimer's disease, Parkinson's disease, and oxidative stress; (3) COVID-19-related encephalitis and encephalopathy (yellow): central nervous system, brain, encephalitis, encephalopathy, and neuroinvasive; (4) neuroimmune complications associated with SARS-CoV-2 and its vaccine (purple): Guillain–Barre syndrome, multiple sclerosis, Bell's palsy, vaccine, and case report; (5) long COVID and mental problems associated with COVID-19 (dark blue): depression, mental health, stress, anxiety, long COVID, dementia, and rehabilitation; (6) neurological manifestations in children associated with COVID-19 (light blue): seizures, epilepsy, pediatrics, and persistent epilepsy; and (7) telemedicine during the COVID-19 pandemic (orange): pandemic, telemedicine, telemedicine, and tele-neurology.
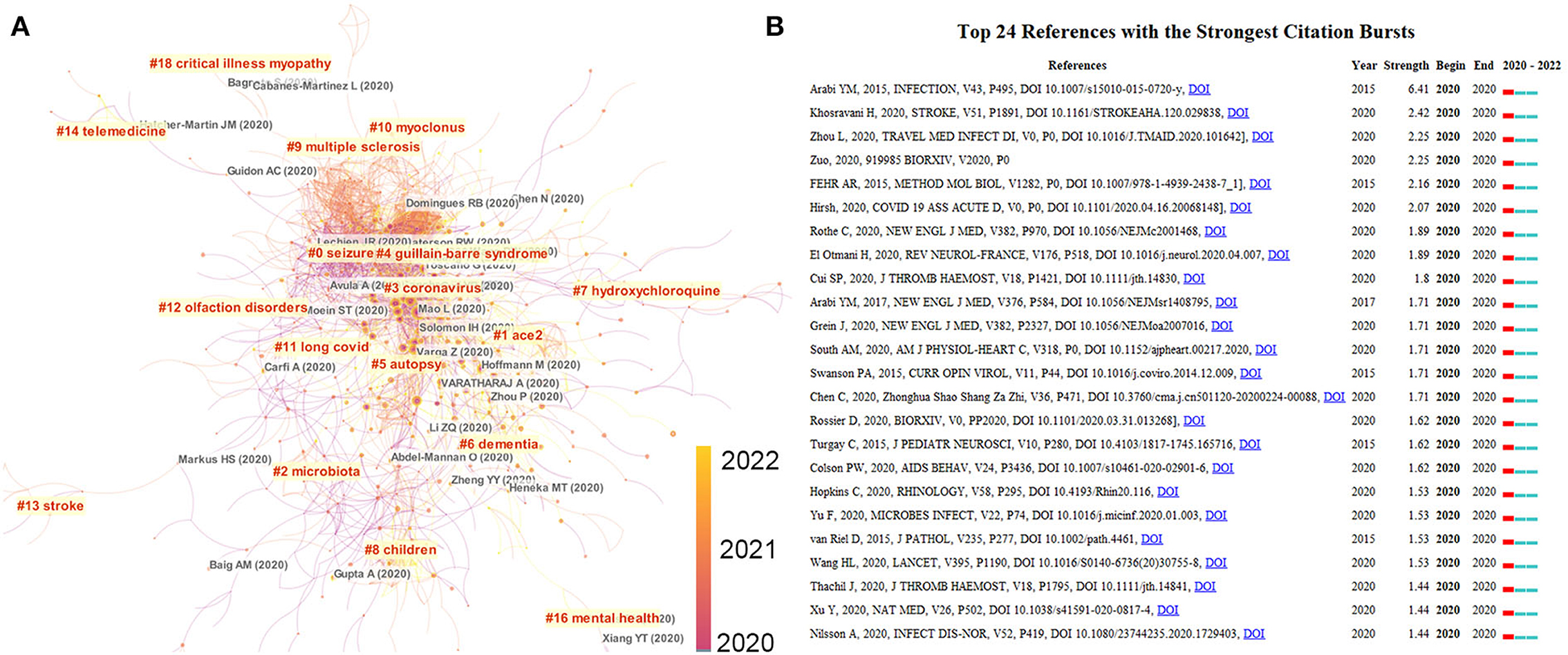
Figure 6. Analysis of references of neurology-related research on COVID-19. (A) Reference clusters named by CiteSpace (find cluster, keyword, LLR). (B) References citation burst visualized by CiteSpace. The top 24 references with the strongest citation bursts of neurology-related research on COVID-19 from 2019 to 2022. The red segment of the blue line denotes the burst duration of the reference.
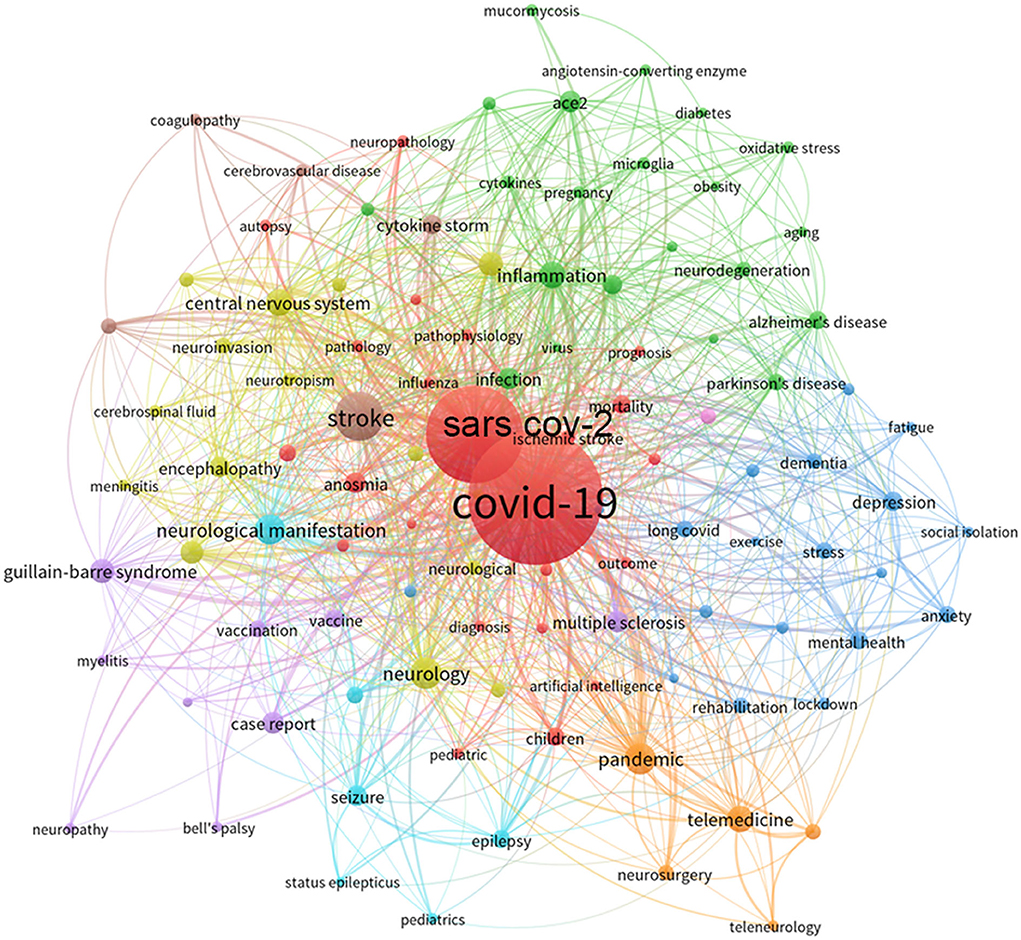
Figure 7. Co-occurrence networks of keywords visualized by VOSviewer. The keywords were clustered into six groups according to their color. Large nodes represent keywords with high frequency.
Although the proportion of neurological disease caused by COVID-19 infection remains small, with a multitude of people infected, the overall number of neurological patients and their associated health burden may be large (3). The number of publications increased rapidly in 2021 compared to that in 2020, suggesting that researchers have been mobilized to uncover the neurological features of the COVID-19 pandemic. Its neurological manifestations, control measures, and acute and long-term complications have also attracted considerable attention worldwide. However, enthusiasm for neurology-related research on COVID-19 may decline, with only 687 publications in the first 4 months of 2022. With the COVID-19 pandemic lasting for 2 years, people seem to have passed the most panic phase, and researchers have lowered their interest in COVID-19. This can be confirmed by the new COVID-19 variant Omicron, which has a character of faster transmission, lower fusogenicity, and reduced pathogenicity (28).
The existing publications include 142 countries/territories and 7,684 institutions, indicating that the neurology-related research on COVID-19 attracted the attention of global scholars. Among the top 20 prolific countries, 12 are from developed countries and eight are from developing countries. Of the top 10 prolific institutions, eight are from developed countries and only two are from developing countries. The United States, as the most productive country, dominates the field, with 1,677 publications (31.4% of the total) and 31,371 total citations (44.8% of the total). Previous studies have shown that the number of publications by country is positively correlated with the duration of the COVID-19 pandemic (29). The United States is one of the countries hardest hit by the COVID-19 pandemic. As of 24 April 2022, more than 80 million confirmed cases and more than 986,000 deaths have been reported in the United States. More importantly, inter-institution collaboration is more frequent in the United States (Figures 4A,B), which corroborates its dominate role in this field. Italy ranks second in terms of the number of publications. Since the emergence of the pandemic in China, there has been an outbreak of COVID-19 in Europe, particularly in Italy and the United Kingdom. This could explain why a large number of articles have been published in Italy as well. The University of Oxford, University College London, the UCL Queen Square Institute of Neurology, and King's College London collaborate closely. This may partly explain why the United Kingdom ranks third, with 530 articles, but second in terms of total citations. Other bibliometric analyses on COVID-19 (e.g., urology (12), rheumatology (13), and pediatrics (30)) also reported the leading position of the United States, Italy, and the United Kingdom, which is consistent with our results. In terms of international collaborations, the United States ranks first in terms of the number of collaborations with different countries, especially with Canada. By contrast, six of the top 10 highest collaborative countries are located in Europe, suggesting that different countries prefer to cooperate with those countries that are geographically close, especially during social isolation policies.
Among the top 10 prolific institutions, four are located in the United States, suggesting the United States conducted more research on neurology-related work on COVID-19 and the U.S. institutions have relatively tighter cooperation in this field (Figures 4A,B). The Huazhong University of Science and Technology (China) ranked first in terms of the total citations. Mao et al. (Tongji Medical College, Huazhong University of Science and Technology, China) first reported that 36.4% of hospitalized patients with COVID-19 had neurological manifestations. This article was also the most cited article in this field, accounting for 80% of the total citations of the Huazhong University of Science and Technology. COVID-19 was first reported in Wuhan, China. There is no doubt that the city's experience has provided researchers with valuable information regarding the characterization and early treatment of COVID-19-related neurological disorders (31, 32).
The most prolific authors (n = 14 publications) were Josef Finsterer from the University of São Paulo (Austria), David Garcia-Azorin from the University Clinical Hospital of Valladolid (Spain), Nima Rezaei from the Tehran University of Medical Sciences (Iran), and Henrik Zetterberg from the UCL Queen Square Neurological Institute (UK). In terms of citations and citations per article, Tom Solomon ranked first, with 1,100 total citations and 185 citations per article. Focusing on these scholars may help new researchers design their studies and grasp the hot spots in neurological on COVID-19. For example, Josef Finsterer focuses on COVID-19-related cranial neuropathy (33, 34) and COVID-19-related GBS (35–37). David Garcia-Azorin focuses on post-pandemic neurological syndromes (e.g., persistent headache (38, 39) and insomnia (40)). Nima Rezaei first mainly focused on neurological complications of COVID-19 (41, 42) and then shifted to the neurological side effects of COVID-19 vaccination (43). Henrik Zetterberg focused on exploring potential neurochemical biomarkers and underlying mechanisms of COVID-19-related neuropathy (44–46), Tom Solomon was the most cited author because he published two articles in Lancet Neurology (3) and Lancet Psychiatry (5) that give readers a comprehensive understanding of the neurological and neuropsychiatric complications of COVID-19.
Neurological Sciences and Frontiers in Neurology were the top two prolific journals listed as Q2 by the Journal Citation Reports (JCR). In terms of impact, Journal of Neurology ranked first, with 1,535 total citations and 23.6 citations per article, and also ranked Q2 by the JCR. However, most of the highly cited articles were published in the top journals such as JAMA Neurology (4), Lancet Neurology (3), Lancet Psychiatry (47), and Brain Behavior and Immunity (48). None of the most cited articles appear in the list of the top 10 most prolific journals. This partly reflects the position of the leading journals in the field of COVID-19-related neurology. Therefore, researchers can read the classic articles in these top journals to build their knowledge base in the field and stay updated with these prolific journals.
There can be no scientific investigation without prior knowledge. Keyword analysis and reference analysis help researchers gain quick insights into a given field (49). In this study, VOSviewer was used for keyword co-occurrence analysis and CiteSpace for reference analysis. A total of 104 keywords appeared more than 20 times and were clustered into seven groups by VOSviewer. CiteSpace identified 13 groups, of these seven groups represented popular topics for neurology-related research on COVID-19.
The primary keywords include stroke, ischemic stroke, cytokine storm, and coagulopathy. In addition to respiratory distress symptoms in COVID-19 patients, neurological manifestations are the most common presentations. Among them, hemorrhagic stroke and ischemic stroke (IS) (50, 51) are also the most common and severe neurological complications after SARS-CoV-2 infection. Clinical studies have reported that the IS incidence ranges from 0.1 to 6.9% among hospitalized patients with COVID-19 (52). The IS incidence is higher in COVID-19 patients than in non-COVID-19 patients, especially in those with severe infections and ICU admissions (53). Moreover, COVID-19 patients with IS are younger and have more severe neurological symptoms than non-COVID-19 patients (51). Apart from arterial cerebral disorders, cerebral venous thrombosis (CVT) has also been found in some cases (54, 55). Because of mass vaccination, vaccine-induced cerebral venous sinus thrombosis (CVT) has also reported by several researchers. D'Agostino et al. reported a rare case of CVT and disseminated intravascular coagulation 12 days after COVID-19 vaccination (56). Schultz et al. (57) found that a 0.55% incidence of CVT within 1 month since the first dose vaccination and that women are more likely to develop CVT after vaccination. Mechanistically, RAS system imbalance, endothelial damage, cytokine storm, hypercoagulable state, and impaired immune function are suspected to contribute to acute cerebrovascular events and deserve more research in future (32).
The main keywords include inflammation, ACE2, Alzheimer's disease (AD), Parkinson's disease (PD), and oxidative stress. Although there is insufficient evidence that PD and AD per se increase the risk of COVID-19 (58), COVID-19-related anosmia is a common feature of early PD. Blood leakage of the blood brain barrier in AD is also a target for COVID invasion. In addition, coronaviruses can be detected in the CNS of patients with PD and AD (59). All of these shows the close relationship between COVID-19 and AD or PD. Mechanically, cytokine storms and excessive oxidative stress induced by COVID-19 may trigger deleterious effects of immune responses, accelerate or exacerbate pre-existing cognitive deficits, or induce neurodegenerative diseases. Therefore, Verkhratsky et al. hypothesized that a population might be at risk of developing degenerative diseases after COVID-19 (60). Studies have shown that symptoms of movement disorders and dementia have been identified as risk factors for mortality in COVID-19 patients compared to AD and PD themselves (61). Quarantine may lead to a lack of motivation, physical disability, and increased stress and anxiety in patients with PD or AD, preventing them from engaging in active lifestyles. In addition, patients with PD and AD require routine clinical visits for physical assessment and medication modification. However, the lockdown and social isolation makes it hard during this particular time. As a result, numerous studies have explored telemedicine, transforming face-to-face clinical consultations into virtual physical examinations and consultations for patients with AD and PD (62, 63). For this, the International Parkinson's and Movement Disorders Association developed a practical step-by-step guide for implementing telemedicine in movement disorders clinics on its website (https://www.movementdisorders.org/MDS/About/Committees-other-groups/telemedicine-in-your-movement-obstacle-practice-A-Step-by-Step-Guide.htm).
The main keywords include central nervous system, brain, encephalitis, encephalopathy, and neuroinvasive. Moriguchi et al. described the first case of meningitis and encephalitis associated with COVID-19, which occurred in a 24-year-old Japanese man. Interestingly, COVID-19-specific RNA was not detected in a nasopharyngeal swab but in the patient's cerebrospinal fluid (CSF) sample (19). By contrast, Kremer et al. reported a French multicenter cohort study involving 64 patients with confirmed neurological manifestations of COVID-19. The incidence of encephalitis was 13%, and no positive COVID-19-specific RNA was found in the CSF of these patients (64). Regarding encephalopathy, Meppiel et al. reported COVID-19-related encephalopathy in 30.2% (67/222) of patients. The authors hypothesized that toxic and metabolic causes, immune dysfunction, antiviral drugs, and hypoxia, rather than the virus itself, may cause COVID-19-related encephalopathy (65). Rutkai et al. infected SARS-CoV-2 on eight non-human primates via aerosol or multiple routes of exposure (e.g., conjunctival, nasal, pharyngeal, and intratracheal routes). The authors found that neuroinflammation, microhemorrhages, cerebral hypoxia, hypoxic-ischemic injury, neuronal degeneration, and apoptosis in the brains of these primates. They demonstrated the neuroinvasive nature of SARS-CoV-2, and these pathological findings may help provide insights into the neurological symptoms associated with long COVID (2).
The main keywords include Guillain–Barre syndrome (GBS), multiple sclerosis (MS), Bell's palsy, vaccine, and case report. The main neuroimmune disorders related to COVID-19 were GBS, MS, and Bell's palsy, all of which were characterized by demyelination and inflammation (66). Ottaviani et al. reported a woman who suffered from rapidly progressive flaccid paralysis and unilateral facial neuropathy after infected with SARS-CoV-2. Coronavirus was detected in a nasopharyngeal swab but was negative in her CSF (67). In agreement with this, in the first 6 months after the COVID-19 outbreak, Uncini et al. (68) reviewed 42 patients with COVID-19-related GBS, all of which were diagnosed with albuminocytological dissociation, rather than PCR positivity for COVID-19-specific RNA in CSF. It appears that the GBS occurrence after SARS-CoV-2 infection is not due to direct viral invasion of the nerve or CNS but rather due to immune dysfunction after COVID-19 infection. Future studies should compare patients with COVID-19-associated GBS to those with non-COVID-19-associated GBS over the same period and determine whether the incidence of GBS is elevated in COVID-19 patients in large cohorts. In the case of MS, COVID-19 does not appear to stimulate the initiation of MS. However, many researchers were interested in identifying whether the immunomodulatory treatment for COVID-19 has a negative effect on MS patients with COVID-19 infection. Loonstra et al. reported a Dutch multi-cohort study involving 86 Dutch MS patients. They found no significant negative effects of immunosuppression on patients with MS (69). Kovvuru et al. (37) also reported the same results. Immunosuppressive therapy does not make MS patients more susceptible to COVID-19. In addition to the most occurred vaccine-induced immunothrombotic events, Bell's palsy, encephalomyelitis, GBS, and transverse myelitis have been reported after COVID-19 vaccination (70). However, the authors noted that these immune-mediated neurological outcomes are rare in the vaccinated people when compared to the observed risks associated with unvaccinated COVID-19 people. Most of neurological complications related to SARS-CoV-2 vaccination are case reports. COVID-19-related mortality can currently be reduced most effectively through vaccination (71). Neurologists and policymakers should minimize reporting adverse effects related to COVID-19 vaccination and build public trust in vaccination programs to improve vaccination rates and curb the spread of infection.
The main keywords include depression, mental health, stress, anxiety, long covid, dementia, and rehabilitation. After the initial surge of infection, concerns about acute mortality and complications of COVID-19 shifted to managing the long-term disease sequelae in survivors. As a result, post-acute COVID-19 syndrome (also known as long COVID) becomes a common syndrome. Davis et al. (72) reported the results of symptoms after 7 months of infection with COVID-19 in an international research containing 56 countries and 3,762 patients. The most common symptoms include fatigue (86.7%), post-exercise discomfort (85.9%), and cognitive dysfunction or memory issues (88%). These patients continue to suffer from the burden of these symptoms in their daily lives and are unable to return to the same level of work as they did before SARS-CoV-2 infection even months after infection. Interestingly, Duarte Romero et al. (73) reported the “long COVID” outcomes of 969 patients with severe COVID-19 after 6 months. Only 33% patients develop neurological and mental health problems. In addition, the authors found that women had a higher frequency of headaches and mental health problems. Lombardo et al. (74) reported the outcomes 1 year after COVID-19 infection, with the most prevalent symptoms being fatigue (52%), pain (48%), and sleep disturbance (47%). In addition, Kim et al. (75) reported the results of a 1-year follow-up research containing 241 patients with SARS-CoV-2 infection in Korea. The main symptoms are inattention, cognitive dysfunction, forgetfulness, depression, fatigue, and anxiety. In addition, 5.0% of the patients were receiving outpatient treatment for such symptoms after the infection was over. Older age, female gender, and disease severity were identified as risk factors for persistent neuropsychiatric symptoms. Petersen et al. (76) investigated the 8-month follow-up results of long COVID in 226 non-hospital individuals with confirmed COVID-19 diagnosis. The most common symptoms were fatigue (16%), and smell (17%), and taste (14%) dysfunction. Long COVID was more common in people taking medications every day. As for the mechanism, Dani et al. (77) proposed that long COVID may be associated with viral or immune-mediated disruption of the autonomic nervous system, leading to orthostatic intolerance syndrome. Newell et al. (78) concluded that immunological misfiring, inflammatory storms, and persistent inflammation played a key role in long COVID. However, there is a lack of concrete and consistently definition and characterization of “long COVID”. The reported prevalence of the so-called “long COVID” varies greatly. However, all physicians should be able to recognize this condition and comprehend its symptom burden. Moreover, with an increasing number of COVID-19 patients developing post-COVID manifestations, there is an urgent need to define the formal clinical “long COVID” and identify affected individuals early enough to provide the most appropriate and effective treatment.
The main keywords include seizures, epilepsy, pediatrics, and persistent epilepsy. Children infected with COVID-19 usually remain asymptomatic after infection, but some infected children will develop life-threatening multisystem inflammatory syndromes (MIS-C) (79). In addition to MIS-C, children with COVID-19 often develop neurological manifestations. A multicenter study of children diagnosed with MIS-C and COVID-19 showed that 5% of the children suffered severe neurological complications (e.g., seizures, coma, encephalitis, demyelinating disease, and aseptic meningitis). Among these neurological conditions, seizures were the most common reason for children visiting hospital (80). Kurd et al. (81) pointed out that seizures occurred in an early phase once children were infected with SARS-CoV-2 and may be the main manifestation of acute COVID-19 in children (11/175). Similarly, Dilber et al. (82) reported results of Turkey, where seizures (18/382) were the most common cause of hospitalization in children with COVID-19. In addition to the incidence of seizures attracted the interest from neurologists, the management of seizures also poses a significant challenge to neurologists and caregivers. Davico et al. (83) noted that during the COVID-19 pandemic, the hospital emergency visits due to childhood seizures decreased by 37% compared to those in the previous period. Furthermore, because of social isolation and lockdown policy, a large proportion of children with epilepsy have difficulties with regular clinic visits and medication refills (84). Panda et al. described their experience in providing medical advice to children with epilepsy via telephonic consultation during the pandemic. The results showed that 96% of caregivers were satisfied with the quality of this telemedicine service (85). Another study from India also found that video tele-consultation using cell phones improved the management of patients with epilepsy (86). Perhaps, telemedicine may be actively explored as an alternative strategy for the management and supervision of treatment of epilepsy patients in future.
The main keywords include epidemic, telemedicine, telehealth, and tele-neurology. Telemedicine refers to the delivery of medical care to a patient by a physician or other healthcare workers from a distance (87). The need for “social distance” and “lockdown policy” during the COVID-19 pandemic created a surging demand in the number of tele-neurology visits (88). Grossman et al. (89) described the transition of their neurology department from a face-to-face clinic to a virtual neurology practice in response to the COVID-19 pandemic. In addition, they performed a virtual neurological examination using the electronic medical record applications. Their experience suggests that changes in government rules, regulations, and payer-driven reimbursement policies during the COVID-19 period contributed to telemedicine. However, Fasano et al. (90) and Mok et al. (91) pointed out that telemedicine is only available in a few cases and limited to email or telephone contact. The authors advocate for remote management of patients with chronic neurological conditions, especially those with advanced dementia patients (e.g., AD and PD). Rametta et al. (92) analyzed 2,589 child tele-neurology visits during the COVID-19 pandemic. The results showed that 93% of clinicians (1,200/1,286) were satisfied with telemedicine services, and 89% (1,144/1,286) recommended telemedicine as an integral part of follow-up care after the COVID-19 pandemic. However, in a survey of telepractice visits to pediatric epilepsy clinics, physicians (79.9%) were less satisfied with telepractice than parents (91.3%) who used the telephone for their children remote encounters (93). Challenges to the widespread use of telemedicine in neurology clinics include (1) the lack of effective clinical examinations; (2) increased social isolation; (3) difficulties with patients with cognitive impairment; (4) workflow and technology availability challenges; and (5) legal issues and reimbursement problems (94). As the COVID-19 pandemic has caused worldwide social dislocation and operational and economic dysfunction, and its impacts on routine healthcare delivery may last for a long time, healthcare planners, policymakers, and academics should address these problems in future.
First, we only extracted data from the WoSCC to meet the data formatting standards of visualization tools such as CiteSpace and VOSviewer. However, the WoSCC database, as one of the most widely available and recognized global resources, has been used in several previous high-quality bibliometric studies (95, 96). Second, this study produced a language and article-type bias as we only selected “English” literature published as “original articles or reviews”. Although “English” remains the most common language for academic publications worldwide, several articles have been published in non-English languages, such as Chinese, Japanese, and Portuguese. We excluded documents such as letters to the editor and editorials because the detailed information (e.g., authors, affiliations, keywords, and cited references) is often incomplete in these publication types. Third, total citations and citations per article are affected by time and remain controversial as a comprehensive indicator of the quality of an article or an author. Similarly, the number of publications is not the only indicator of a journal's impact or activity as other metrics (e.g., impact factor, SNIP, CiteSpace, and SJR) are widely used. Fourth, articles published in 2022 only cover the first 4 months of the year, and database updates may result in discrepancies. However, we believe that the low citation frequency of new publications has less impact on our conclusions.
This study provides researchers with valuable information on publication trends, potential collaborations, topical issues, and frontier research topics in neurology-related research on COVID-19. During the COVID-19 pandemic, there has been a growing interest in this field. Research topics have shifted from “ethics, autopsy, and telemedicine” in 2020 to various neurological conditions related to COVID-19 in 2021, such as stroke, AD, PD, GBS, MS, childhood seizures, and long COVID. The following three topics deserve further research in future: tele-neurology during the COVID-19 pandemic, COVID-19-related neurological complications and mechanisms, and long COVID.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
QZ conceived of the study, participated in its design, and drafted the manuscript. JL was involved in the study design, obtained data and contributed to interpretation, and helped to draft the manuscript. LW provided the theoretical frameworks and performed much of the editing of the manuscript. All authors read and approved the final manuscript.
This research was supported by National Key R&D Program of China (No. 2020YFC2005401), National Natural Science Foundation of China (No. 81902551), and Natural Science Foundation of Hunan Province (No. 2021JJ31072).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.937008/full#supplementary-material
1. Kwon S, Joshi AD, Lo CH, Drew DA, Nguyen LH, Guo CG, et al. Association of social distancing and face mask use with risk of COVID-19. Nat Commun. (2021) 12:3737. doi: 10.1038/s41467-021-24115-7
2. Rutkai I, Mayer MG, Hellmers LM, Ning B, Huang Z, Monjure CJ, et al. Neuropathology and virus in brain of SARS-CoV-2 infected non-human primates. Nat Commun. (2022) 13:1745. doi: 10.1038/s41467-022-29440-z
3. Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. (2020) 19:767–83. doi: 10.1016/S1474-4422(20)30221-0
4. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. (2020) 77:683–90. doi: 10.1001/jamaneurol.2020.1127
5. Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. (2020) 7:875–82. doi: 10.2139/ssrn.3601761
6. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. BMJ. (2021) 374:n1648. doi: 10.1136/bmj.n1648
7. Pezzini A, Padovani A. Lifting the mask on neurological manifestations of COVID-19. Nat Rev Neurol. (2020) 16:636–44. doi: 10.1038/s41582-020-0398-3
8. Iadecola C, Anrather J, Kamel H. Effects of COVID-19 on the nervous system. Cell. (2020) 183:16–27.e1. doi: 10.1016/j.cell.2020.08.028
9. Yao Q, Lyu PH, Ma FC, Yao L, Zhang SJ. Global informetric perspective studies on translational medical research. BMC Med Inform Decis Mak. (2013) 13:77. doi: 10.1186/1472-6947-13-77
10. Kumar S, Sharma D, Rao S, Lim WM, Mangla SK. Past, present, and future of sustainable finance: insights from big data analytics through machine learning of scholarly research. Ann Oper Res. (2022) 1–44. doi: 10.1007/s10479-021-04410-8
11. Chan KIP, Ignacio KHD, Omar AT 2nd, Khu KJO. Top 100 most cited neurologic and neurosurgical articles on COVID-19: a bibliometric analysis. World Neurosurg. (2022) 157:e137–47. doi: 10.1016/j.wneu.2021.09.118
12. Soytas M, Danacioglu YO, Boz MY, Horuz R, Albayrak S. COVID-19 and urology: a bibliometric analysis of the literature. Int J Clin Pract. (2021) 75:e14965. doi: 10.1111/ijcp.14965
13. Pasin O, Pasin T. A bibliometric analysis of rheumatology and COVID-19 researches. Clin Rheumatol. (2021) 40:4735–40. doi: 10.1007/s10067-021-05844-y
14. Pan X, Yan E, Cui M, Hua W. Examining the usage, citation, and diffusion patterns of bibliometric mapping software: a comparative study of three tools. J Informetr. (2018) 12:481–93. doi: 10.1016/j.joi.2018.03.005
15. Ma Y, Uzzi B. Scientific prize network predicts who pushes the boundaries of science. Proc Natl Acad Sci USA. (2018) 115:12608–15. doi: 10.1073/pnas.1800485115
16. You Y, Li W, Liu J, Li X, Fu Y, Ma X. Bibliometric review to explore emerging high-intensity interval training in health promotion: a new century picture. Front Public Health. (2021) 9:697633. doi: 10.3389/fpubh.2021.697633
17. Xiao T, Xia S, Zeng L, Lin G, Wei Q, Zhou W, et al. A multicentre observational study on neonates exposed to SARS-CoV-2 in China: the Neo-SARS-CoV-2 Study protocol. BMJ Open. (2020) 10:e038004. doi: 10.1136/bmjopen-2020-038004
18. Hess DC, Eldahshan W, Rutkowski E. COVID-19-related stroke. Transl Stroke Res. (2020) 11:322–5. doi: 10.1007/s12975-020-00818-9
19. Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. (2020) 94:55–8. doi: 10.1016/j.ijid.2020.03.062
20. Louapre C, Collongues N, Stankoff B, Giannesini C, Papeix C, Bensa C, et al. Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol. (2020) 77:1079–88. doi: 10.1001/jamaneurol.2020.2581
21. Zanin L, Saraceno G, Panciani PP, Renisi G, Signorini L, Migliorati K, et al. SARS-CoV-2 can induce brain and spine demyelinating lesions. Acta Neurochir. (2020) 162:1491–4. doi: 10.1007/s00701-020-04374-x
22. Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
23. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. (2020) 92:552–5. doi: 10.1002/jmv.25728
24. Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. (2020) 11:3572. doi: 10.1038/s41467-020-17436-6
25. Meinhardt J, Radke J, Dittmayer C, Franz J, Thomas C, Mothes R, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci. (2021) 24:168–75. doi: 10.1101/2020.06.04.135012
26. Arabi YM, Harthi A, Hussein J, Bouchama A, Johani S, Hajeer AH, et al. Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV). Infection. (2015) 43:495–501. doi: 10.1007/s15010-015-0720-y
27. Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. (2020) 51:1891–5. doi: 10.1161/STROKEAHA.120.029838
28. Suzuki R, Yamasoba D, Kimura I, Wang L, Kishimoto M, Ito J, et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature. (2022) 603:700–5. doi: 10.1038/s41586-022-04462-1
29. Cicek Korkmaz A, Altuntas S. A bibliometric analysis of COVID-19 publications in nursing by visual mapping method. J Nurs Manag. (2022). 16. doi: 10.1111/jonm.13636
30. Hu S, Wang X, Ma Y, Cheng H. Global research trends in pediatric COVID-19: a bibliometric analysis. Front Public Health. (2022) 10:798005. doi: 10.3389/fpubh.2022.798005
31. Zhai H, Lv Y, Xu Y, Wu Y, Zeng W, Wang T, et al. Characteristic of Parkinson's disease with severe COVID-19: a study of 10 cases from Wuhan. J Neural Transm. (2021) 128:37–48. doi: 10.1007/s00702-020-02283-y
32. Wang M, Zhang H, He Y, Qin C, Liu X, Liu M, et al. Association between ischemic stroke and COVID-19 in China: a population-based retrospective study. Front Med. (2021) 8:792487. doi: 10.3389/fmed.2021.792487
33. Finsterer J, Scorza FA, Scorza C, Fiorini A. COVID-19 associated cranial nerve neuropathy: a systematic review. Bosn J Basic Med Sci. (2022) 22:39–45. doi: 10.17305/bjbms.2021.6341
34. Finsterer J, Scorza FA, Scorza CA, Fiorini AC. SARS-CoV-2 impairs vision. J Neuroophthalmol. (2021) 41:166–9. doi: 10.1097/WNO.0000000000001273
35. Finsterer J. Exacerbating guillain-barre syndrome eight days after vector-based COVID-19 vaccination. Case Rep Infect Dis. (2021) 2021:3619131. doi: 10.1155/2021/3619131
36. Finsterer J, Scorza FA. Guillain-Barre syndrome in 220 patients with COVID-19. Egypt J Neurol Psychiatr Neurosurg. (2021) 57:55. doi: 10.1186/s41983-021-00310-7
37. Kovvuru S, Nalleballe K, Onteddu SR, Sharma R, Jasti M, Kapoor N, et al. Immunosuppression in chronic autoimmune neurological disorders during the COVID-19 pandemic. J Neurol Sci. (2021) 420:117230. doi: 10.1016/j.jns.2020.117230
38. Garcia-Azorin D, Layos-Romero A, Porta-Etessam J, Membrilla JA, Caronna E, Gonzalez-Martinez A, et al. Post-COVID-19 persistent headache: a multicentric 9-months follow-up study of 905 patients. Cephalalgia. (2022) 42:804–809. doi: 10.1177/03331024211068074
39. Garcia-Azorin D, Trigo J, Talavera B, Martinez-Pias E, Sierra A, Porta-Etessam J, et al. Frequency and type of red flags in patients with Covid-19 and headache: a series of 104 hospitalized patients. Headache. (2020) 60:1664–72. doi: 10.1111/head.13927
40. Talavera B, Garcia-Azorin D, Martinez-Pias E, Trigo J, Hernandez-Perez I, Valle-Penacoba G, et al. Anosmia is associated with lower in-hospital mortality in COVID-19. J Neurol Sci. (2020) 419:117163. doi: 10.1016/j.jns.2020.117163
41. Sadeghmousavi S, Rezaei N. COVID-19 infection and stroke risk. Rev Neurosci. (2021) 32:341–9. doi: 10.1515/revneuro-2020-0066
42. Zamani R, Pouremamali R, Rezaei N. Central neuroinflammation in Covid-19: a systematic review of 182 cases with encephalitis, acute disseminated encephalomyelitis, and necrotizing encephalopathies. Rev Neurosci. (2021). 33:397–412. doi: 10.1515/revneuro-2021-0082
43. Aliasin MM, Yazdanpanah N, Rezaei N. Neurological and neuropsychological adverse effects of SARS-CoV-2 vaccines - where do we stand? Rev Neurosci. (2022). doi: 10.1515/revneuro-2022-0006
44. Ziff OJ, Ashton NJ, Mehta PR, Brown R, Athauda D, Heaney J, et al. Amyloid processing in COVID-19-associated neurological syndromes. J Neurochem. (2022) 161:146–57. doi: 10.1111/jnc.15585
45. Patel H, Ashton NJ, Dobson RJB, Andersson LM, Yilmaz A, Blennow K, et al. Proteomic blood profiling in mild, severe and critical COVID-19 patients. Sci Rep. (2021) 11:6357. doi: 10.1038/s41598-021-85877-0
46. Eden A, Simren J, Price RW, Zetterberg H, Gisslen M. Neurochemical biomarkers to study CNS effects of COVID-19: a narrative review and synthesis. J Neurochem. (2021) 159:61–77. doi: 10.1111/jnc.15459
47. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. doi: 10.1016/S2215-0366(20)30203-0
48. Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. (2020) 87:18–22. doi: 10.1016/j.bbi.2020.03.031
49. Chen C, Song M. Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS ONE. (2019) 14:e0223994. doi: 10.1371/journal.pone.0223994
50. Guan WJ Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
51. Ntaios G, Michel P, Georgiopoulos G, Guo Y, Li W, Xiong J, et al. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke. (2020)51:e254−8. doi: 10.1161/STROKEAHA.120.031208
52. Sagris D, Papanikolaou A, Kvernland A, Korompoki E, Frontera J, Troxel A, et al. COVID-19 and ischemic stroke. Eur J Neurol. (2021). 28:3826–36. doi: 10.1111/ene.15008
53. Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. (2020) 51:2002–11. doi: 10.1161/STROKEAHA.120.030335
54. Sweid A, Hammoud B, Bekelis K, Missios S, Tjoumakaris SI, Gooch MR, et al. Cerebral ischemic and hemorrhagic complications of coronavirus disease 2019. Int J Stroke. (2020) 15:733–42. doi: 10.1177/1747493020937189
55. Mowla A, Shakibajahromi B, Shahjouei S, Borhani-Haghighi A, Rahimian N, Baharvahdat H, et al. Cerebral venous sinus thrombosis associated with SARS-CoV-2; a multinational case series. J Neurol Sci. (2020) 419:117183. doi: 10.1016/j.jns.2020.117183
56. D'Agostino V, Caranci F, Negro A, Piscitelli V, Tuccillo B, Fasano F, et al. A rare case of cerebral venous thrombosis and disseminated intravascular coagulation temporally associated to the COVID-19 vaccine administration. J Pers Med. (2021) 11:285. doi: 10.3390/jpm11040285
57. Schulz JB, Berlit P, Diener HC, Gerloff C, Greinacher A, Klein C, et al. COVID-19 vaccine-associated cerebral venous thrombosis in Germany. Ann Neurol. (2021) 90:627–39. doi: 10.1101/2021.04.30.21256383
58. Stoessl AJ, Bhatia KP, Merello M. Movement disorders in the world of COVID-19. Mov Disord. (2020) 35:709–10. doi: 10.1002/mds.28069
59. Ferini-Strambi L, Salsone M. COVID-19 and neurological disorders: are neurodegenerative or neuroimmunological diseases more vulnerable? J Neurol. (2021) 268:409–19. doi: 10.1007/s00415-020-10070-8
60. Verkhratsky A, Li Q, Melino S, Melino G, Shi Y. Can COVID-19 pandemic boost the epidemic of neurodegenerative diseases? Biol Direct. (2020) 15:28. doi: 10.1186/s13062-020-00282-3
61. Bianchetti A, Rozzini R, Guerini F, Boffelli S, Ranieri P, Minelli G, et al. Clinical presentation of COVID19 in dementia patients. J Nutr Health Aging. (2020) 24:560–2. doi: 10.1007/s12603-020-1389-1
62. Motolese F, Magliozzi A, Puttini F, Rossi M, Capone F, Karlinski K, et al. Parkinson's disease remote patient monitoring during the COVID-19 lockdown. Front Neurol. (2020) 11:567413. doi: 10.3389/fneur.2020.567413
63. Del Prete E, Francesconi A, Palermo G, Mazzucchi S, Frosini D, Morganti R, et al. Prevalence and impact of COVID-19 in Parkinson's disease: evidence from a multi-center survey in Tuscany region. J Neurol. (2021) 268:1179–87. doi: 10.1007/s00415-020-10002-6
64. Kremer S, Lersy F, Anheim M, Merdji H, Schenck M, Oesterle H, et al. Neurologic and neuroimaging findings in patients with COVID-19: a retrospective multicenter study. Neurology. (2020) 95:e1868−82. doi: 10.1212/WNL.0000000000010112
65. Meppiel E, Peiffer-Smadja N, Maury A, Bekri I, Delorme C, Desestret V, et al. Neurologic manifestations associated with COVID-19: a multicentre registry. Clin Microbiol Infect. (2021) 27:458–66. doi: 10.1101/2020.07.15.20154260
66. McLean NA, Popescu BF, Gordon T, Zochodne DW, Verge VM. Delayed nerve stimulation promotes axon-protective neurofilament phosphorylation, accelerates immune cell clearance and enhances remyelination in vivo in focally demyelinated nerves. PLoS ONE. (2014) 9:e110174. doi: 10.1371/journal.pone.0110174
67. Ottaviani D, Boso F, Tranquillini E, Gapeni I, Pedrotti G, Cozzio S, et al. Early Guillain-Barre syndrome in coronavirus disease 2019 (COVID-19): a case report from an Italian COVID-hospital. Neurol Sci. (2020) 41:1351–4. doi: 10.1007/s10072-020-04449-8
68. Uncini A, Vallat JM, Jacobs BC. Guillain-Barre syndrome in SARS-CoV-2 infection: an instant systematic review of the first six months of pandemic. J Neurol Neurosurg Psychiatry. (2020) 91:1105–10. doi: 10.1136/jnnp-2020-324491
69. Loonstra FC, Hoitsma E, van Kempen ZL, Killestein J, Mostert JP. COVID-19 in multiple sclerosis: the Dutch experience. Mult Scler. (2020) 26:1256–60. doi: 10.1177/1352458520942198
70. Li X, Raventos B, Roel E, Pistillo A, Martinez-Hernandez E, Delmestri A, et al. Association between covid-19 vaccination, SARS-CoV-2 infection, and risk of immune mediated neurological events: population based cohort and self-controlled case series analysis. BMJ. (2022) 376:e068373. doi: 10.1136/bmj-2021-068373
71. Logunov DY, Dolzhikova IV, Zubkova OV, Tukhvatullin AI, Shcheblyakov DV, Dzharullaeva AS, et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. (2020) 396:887–97.
72. Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. (2021) 38:101019. doi: 10.1016/j.eclinm.2021.101019
73. Romero-Duarte A, Rivera-Izquierdo M, Guerrero-Fernandez de Alba I, Perez-Contreras M, Fernandez-Martinez NF, Ruiz-Montero R, et al. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. (2021) 19:129. doi: 10.1186/s12916-021-02003-7
74. Lombardo MDM, Foppiani A, Peretti GM, Mangiavini L, Battezzati A, Bertoli S, et al. Long-term coronavirus disease 2019 complications in inpatients and outpatients: a one-year follow-up cohort study. Open Forum Infect Dis. (2021) 8:ofab384. doi: 10.1093/ofid/ofab384
75. Kim Y, Bitna H, Kim SW, Chang HH, Kwon KT, Bae S, et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis. (2022) 22:93. doi: 10.1186/s12879-022-07062-6
76. Petersen MS, Kristiansen MF, Hanusson KD, Foldbo BM, Danielsen ME, Steig BA, et al. Prevalence of long COVID in a national cohort: longitudinal measures from disease onset until 8 months follow up. Int J Infect Dis. (2022). 122:437–41. doi: 10.1016/j.ijid.2022.06.031
77. Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, et al. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med. (2021) 21:e63–7. doi: 10.7861/clinmed.2020-0896
78. Newell KL, Waickman AT. Inflammation, immunity, and antigen persistence in post-acute sequelae of SARS-CoV-2 infection. Curr Opin Immunol. (2022) 77:102228. doi: 10.1016/j.coi.2022.102228
79. Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. (2021) 4:e2111182. doi: 10.1001/jamanetworkopen.2021.11182
80. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al. Multisystem inflammatory syndrome in US children and adolescents N Engl J Med. (2020) 383:334−46. doi: 10.1056/NEJMoa2021680
81. Kurd M, Hashavya S, Benenson S, Gilboa T. Seizures as the main presenting manifestation of acute SARS-CoV-2 infection in children. Seizure. (2021) 92:89–93. doi: 10.1016/j.seizure.2021.08.017
82. Dilber B, Aydin ZGG, Yesilbas O, Sag E, Aksoy NK, Gundogmus F, et al. Neurological manifestations of pediatric acute COVID infections: a single center experience. J Trop Pediatr. (2021) 67:fmab062. doi: 10.1093/tropej/fmab062
83. Davico C, Marcotulli D, Lux C, Calderoni D, Terrinoni A, Di Santo F, et al. Where have the children with epilepsy gone? An observational study of seizure-related accesses to emergency department at the time of COVID-19. Seizure. (2020) 83:38–40. doi: 10.1016/j.seizure.2020.09.025
84. Wanigasinghe J, Jayawickrama A, Hewawitharana G, Munasinghe J, Weeraratne CT, Ratnayake P, et al. Experience during COVID-19 lockdown and self-managing strategies among caregivers of children with epilepsy: a study from low middle income country. Seizure. (2021) 84:112–5. doi: 10.1016/j.seizure.2020.12.001
85. Panda PK, Dawman L, Panda P, Sharawat IK. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. (2020) 81:29–35. doi: 10.1016/j.seizure.2020.07.013
86. Nair PP, Aghoram R, Thomas B, Bharadwaj B, Chinnakali P. Video teleconsultation services for persons with epilepsy during COVID-19 pandemic: an exploratory study from public tertiary care hospital in Southern India on feasibility, satisfaction, and effectiveness. Epilepsy Behav. (2021) 117:107863. doi: 10.1016/j.yebeh.2021.107863
87. Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. (2015) 72:349–54. doi: 10.1001/jamaneurol.2014.3844
88. Roy B, Nowak RJ, Roda R, Khokhar B, Patwa HS, Lloyd T, et al. Teleneurology during the COVID-19 pandemic: a step forward in modernizing medical care. J Neurol Sci. (2020) 414:116930. doi: 10.1016/j.jns.2020.116930
89. Grossman SN, Han SC, Balcer LJ, Kurzweil A, Weinberg H, Galetta SL, et al. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology. (2020) 94:1077–87. doi: 10.1212/WNL.0000000000009677
90. Fasano A, Antonini A, Katzenschlager R, Krack P, Odin P, Evans AH, et al. Management of advanced therapies in Parkinson's disease patients in times of humanitarian crisis: the COVID-19 experience. Mov Disord Clin Pract. (2020) 7:361–72. doi: 10.1002/mdc3.12965
91. Mok VCT, Pendlebury S, Wong A, Alladi S, Au L, Bath PM, et al. Tackling challenges in care of Alzheimer's disease and other dementias amid the COVID-19 pandemic, now and in the future. Alzheimers Dement. (2020) 16:1571–81. doi: 10.1002/alz.12143
92. Rametta SC, Fridinger SE, Gonzalez AK, Xian J, Galer PD, Kaufman M, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. (2020) 95:e1257–66. doi: 10.1212/WNL.0000000000010010
93. Teng T, Sareidaki DE, Chemaly N, Bar C, Coste-Zeitoun D, Kuchenbuch M, et al. Physician and patient satisfaction with the switch to remote outpatient encounters in epilepsy clinics during the Covid-19 pandemic. Seizure. (2021) 91:60–5. doi: 10.1016/j.seizure.2021.05.013
94. De Marchi F, Contaldi E, Magistrelli L, Cantello R, Comi C, Mazzini L. Telehealth in neurodegenerative diseases: opportunities and challenges for patients and physicians. Brain Sci. (2021) 91:60–65. doi: 10.3390/brainsci11020237
95. Zhang Q, Chen J, Liu J. Global trends and hot-spots in research on virtual simulation in nursing: a bibliometric analysis from 1999 to 2021. Front Public Health. (2022) 10:890773. doi: 10.3389/fpubh.2022.890773
Keywords: COVID-19, neurology, bibliometric analysis, Citespace, VOSviewer
Citation: Zhang Q, Li J and Weng L (2022) A bibliometric analysis of COVID-19 publications in neurology by using the visual mapping method. Front. Public Health 10:937008. doi: 10.3389/fpubh.2022.937008
Received: 05 May 2022; Accepted: 30 June 2022;
Published: 26 July 2022.
Edited by:
Reza Lashgari, Shahid Beheshti University, IranCopyright © 2022 Zhang, Li and Weng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Weng, bGluZ3dlbmdAY3N1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.