
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 11 July 2022
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.933005
This article is part of the Research TopicHealth in Afghanistan: Some Insights from Socio-epidemiological ResearchView all 5 articles
 Mohammad Yasir Essar1,2
Mohammad Yasir Essar1,2 Khalid Jan Rezayee3
Khalid Jan Rezayee3 Shoaib Ahmad4
Shoaib Ahmad4 Manar Ahmed Kamal5
Manar Ahmed Kamal5 Reshaduddin Nasery6
Reshaduddin Nasery6 Tamim Jan Danishmand7
Tamim Jan Danishmand7 Michael Head2
Michael Head2 Arash Nemat8*
Arash Nemat8*Background: Tuberculosis (TB) is a high-burden respiratory infectious disease. There was a sharp decline in the number of confirmed TB cases during the pandemic; this is likely to be influenced by the COVID-19 pandemic response, with under-reporting due to resource diversion. There are typically 13,000 tuberculosis-associated deaths in Afghanistan annually, with significant problems posed by drug-resistant TB.
Method: A cross-sectional descriptive study was conducted in Afghanistan on Kabul residents who visited the adult outpatient departments of public hospitals for any health-related reason from 1st January to 20th March 2022. The study scored their knowledge, attitude, and practices (KAP) toward tuberculosis. The sample size was calculated using Epi-Info, and the minimum sample size was 385. The sampling method is chosen the non-probability convenient sampling for data gathering. Data were analyzed using SPSS version 28, and we used the Mann-Whitney test, Chi-square or fisher extract test, spearman correlations, and binary logistic regression model.
Results: Of 829 participants, 450 (54.3%) were males and 379 (45.7) females. The median age was 28 years, and 63.3% were married. Most participants were unemployed (75.5%), but 54% had a monthly income >3,000 Afghanis, indicating the reliance on family. By TB knowledge score, 727 (87.7%) participants had good knowledge, and 800 (96.5%) participants had a positive attitude toward treatment and control. Only 2 participants reported poor practices regarding prevention. Regarding the binary logistic regression, young age, being a male, belonging to the “1,000–3,000” Afghani monthly income category, and having a positive attitude were significant predictors of good TB knowledge (P-value = 0.009, 0.000, 0.003, and 0.009), respectively. A positive attitude was expected to have good knowledge 6.035 times more than a negative attitude (95% CI: 1.572–23.167).
Conclusion: The study findings highlighted that outpatients in Kabul had good knowledge, attitude, and practice toward TB. More studies are needed to highlight KAP in different Afghan populations, including in other parts of the country.
Tuberculosis (TB) is a bacterial infection responsible for ~1.5 m deaths in 2020 (1). Transmission is via respiratory droplets and aerosols from one person to another, including coughing, sneezing, fever, and headache (2). On average, one TB patient can infect 10–15 people (3). On-time screening and medications are essential for managing TB to reduce the likelihood of multidrug-resistant TB. Multidrug-resistant TB is a growing public health challenge that emerges if mismanagement in the treatment of TB occurs (4). With the emergence of the COVID-19 pandemic, there was a global disruption in many areas of healthcare and surveillance, including TB control programs; this is more visible in countries with the highest burden of TB- a sharp decline in confirmed TB cases was observed during 2020 and 2021, likely to be due to under-reporting (5).
The COVID-19 outbreak has undone decades of progress in the fight against TB, according to the Global Tuberculosis Report 2021. TB fatalities have surged for the first time in more than 10 years. In addition, fewer patients than in 2019 have received TB diagnoses or preventative treatment (6).
Afghanistan is a low-income country with an estimated population of 37 m people. There is a disproportionately high burden of tuberculosis that greatly impacts peoples' lives, with annually ~13,000 tuberculosis-associated deaths (7) and an estimated 9,800 deaths in 2020 (8). Countries with a high burden of TB and cases include Indonesia, China, Philippines, Pakistan, Nigeria and South Africa (9). The high burdens are associated with multiple factors, including cultural beliefs, illiteracy, low outreach and access to health facilities, stigma, and poverty (10). It has also been identified that TB infects women more than men in Afghanistan (10). This is similar to what's reported in other parts of the world. For instance, in a study conducted in China, a high rate of stigma among TB patients was observed, particularly among females (11). Similarly, in Peru, where TB is a high burdened disease, there is a considerable lack of knowledge among participants on the symptoms; this further emphasizes the need for health literacy and education awareness (12).
The response to the COVID-19 pandemic in Afghanistan has seen disruption in health services. For example, the polio program was suspended amidst the pandemic, later attributed to a spike in polio cases among children (13). Now, with the multiple waves of the pandemic, the crumbling healthcare system is struggling with a set of challenges, such as the global emergence of new variants of the novel coronavirus, oxygen and bed shortages (14).
Concurrently, the Taliban is dominating the country and causing significant political tension. Therefore, there is a lack of support and funding from international organizations because of the new government's dominance. Many health facilities are not properly functioning (15). Without external support, TB would remain a serious health issue. Therefore, the main objective of this study was to assess the Hospital's patients' knowledge, attitude, and practice toward TB in Kabul, Afghanistan, to report an updated overview of the TB burden in the country to the local and international communities and stakeholders. In addition, it provides an insight for the researchers to study the subject more in-depth.
A cross-sectional descriptive study was conducted on Kabul residents who visited the adult outpatient departments (OPD) of public health facilities for various health services; this included, but was not restricted to, attendance for follow-up on a confirmed case of tuberculosis. Data collection took place from 1st January to 20th March 2022 from public health facilities such as (Jamhoriat, Ibni Sina, Maiwand, Estiqlal, Barchi, Ali Abad, Aryana, Amiri, Royal, Global, Shaikh Zayid, Wazir Akbar Khan, Indragandi, Bed Khair Khana, Sama, Khatumul Nabeyeen, Milat, Malalai, and Rabeya Balkhi).
For this study, inclusion and exclusion criteria were all patients 18 years of age or above and were Outpatient departments referral. Exclusion criteria were patients under 18 and were not Outpatient departments referral.
The survey questionnaire was adapted from a similar study conducted in Ethiopia (16). The questionnaire was modified slightly according to the context. Here, questions were asked in person, and data were recorded on paper forms (Supplementary File 1).
The study asked basic sociodemographic questions such as age, gender, marital status, educational status, occupation, and average monthly income (afghani), which were categorized into three classes, namely, <1,000 (afghani), 1,000–3,000 (afghani), and >3,000 (afghani). The median monthly income in Kabul is 5,000 Afghani, equating to ~57.14 US dollars.
We ask about TB mode of transmission, TB preventability, and TB symptoms. The knowledge grade was calculated by giving a (correct answer a score of 1 and a wrong answer a score of 0). We had nine points, so the maximum score was nine, and the minimum score was zero (0-9). We categorized the knowledge as follows—Poor knowledge (0–5) and Good knowledge (6–9). This scoring system was based on a similar study done in Ethiopia. The area under the receiver operator characteristic (ROC) curve (AUC) results of the knowledge were considered good and equalled 0.86.
We ask whether participants considered TB a dangerous disease for the community, whether TB transmission from human to human and the presence of stigma for TB patients. The attitude grade was calculated according to (true answer = one and wrong answer = 0). We had three points, so the maximum score was three, and the minimum score was zero (0–3). We categorized the attitude as follows [Positive attitude (2–3) and Negative attitude (0–1)]. The area under the ROC curve (AUC) attitude results were considered good and equalled 0.801.
We ask about participant knowledge around good practices for controlling TB, including opening house windows regularly, opening car window's during traveling, TB screening, having TB health education, having TB, and action after having TB. The practice grade was calculated according to (true answer = one and wrong answer = 0). We had eight points, so the maximum score was eight, and the minimum score was zero (0–8). We categorized the practice as follows [Poor practice (0–4) and Good practice (5–8)]. The area under the practice's ROC curve (AUC) results were considered excellent and equalled 0.998.
All participants fulfilling the inclusion criteria were invited to participate. The sample size was calculated using Epi-Info. Kabul's population has an estimated 4 million 400 thousand with a 95% confidence level, 50% expected frequency, 1.0 effected size, and 5% margin of error. The measured required minimum sample size was 385 participants. The sampling method is chosen the non-probability convenient sampling for data gathering.
The questionnaire was pre-tested on a small sample of participants (70 participants) to confirm the practicability and clarity of questions. Expert researchers reviewed the questionnaire for content validity and considered their comments. For reliability, Cronbach's alpha was 0.753 for every questionnaire section, indicating an acceptable level of consistency. Observations of the pilot study were not included in the final analysis.
Ethical approval was obtained from the Microbiology Department of Kabul University of Medical Sciences Research Committee (KUMS-MD-2241). Informed consent was taken from the participants before they participated in the study.
The knowledge scoring was based on the three knowledge questions. The extracted data was presented in an excel sheet, and data were analyzed using SPSS version 28. The optimal cutoff point was evaluated using the ROC curve. The area under the ROC curve (AUC) results were considered excellent for AUC values between 0.9 and 1, good for AUC values between 0.8 and 0.9, fair for AUC values between 0.7 and 0.8, poor for AUC values between 0.6 and 0.7 and failed for AUC values between 0.5 and 0.6 (17). Normality was tested using the Kolmogorov-Smirnov test, and histogram. For continuous non-normally distributed data, median and interquartile range (IQR) was used, and comparisons were made using the Mann-Whitney test. Results were summarized using counts (n) and percentages (%) for categorical data with comparisons made using the Chi-square or Fisher extract test. A value of p < 0.05 was considered statistically significant. The association between knowledge, attitude, and practices toward tuberculosis was tested using spearman correlations. The binary logistic regression model was interpreted using odds ratio (OR) and 95% confidence interval (CI).
Of the 829 participants, 450 (54.3%) were males, 379 (45.7) were females, and the median age was 28 years (IQR = 20) and ranged from 9 to 80. The majority of our sample was unemployed participants (75.5%), but 54% of the participants had a monthly income >3,000 Afghanis (34.29$) Table 1.
Overall, 727 (87.7%) participants had good TB knowledge, and 800 (96.5%) participants had a positive attitude toward TB treatment and control. Moreover, only 2 participants reported poor practices regarding TB prevention. The baseline characters are shown in Table 2.
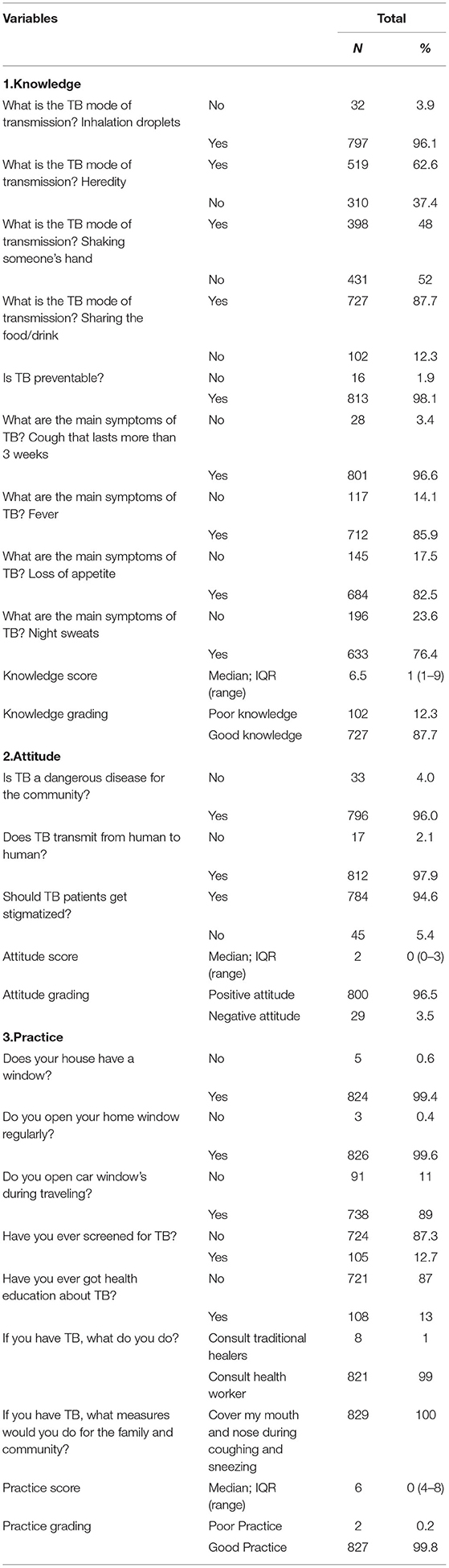
Table 2. Knowledge, attitude, and practices toward tuberculosis among hospital outpatients in Kabul, Afghanistan (N= 829).
Males significantly had better knowledge more than females (n = 369 and 358, respectively) (Overall P-value = 0.001). Belonging to the “>3,000” Afghani monthly income category significantly had better knowledge more than other categories (1,000–3,000 and <1,000) (n = 403, 111, and 1) (Overall P-value = 0.006). A positive attitude was significantly associated with good knowledge (Overall P-value = 0.019).
Regarding the binary logistic regression, young age, being a male, belonging to the “1,000–3,000” Afghani monthly income category, and having a positive attitude were significant predictors of good TB knowledge (P-value = 0.009, 0.000, 0.003, and 0.009), respectively (Table 3).
Belonging to a can read and write education level is predicted to have good knowledge 1.318 times more than belonging to a cannot read and write level (95% CI: 0.664–2.616). Being employed was predicted to have good knowledge 1.177 times more than being unemployed (95% CI: 0.660–2.100). Belonging to the “ <1,000” Afghani monthly income category expected to have good knowledge 2.171 times more than other categories (1,000–3,000 and >3,000) (95% CI: 1.306–3.608). A positive attitude was expected to have good knowledge 6.035 times more than a negative attitude (95% CI: 1.572–23.167) (Table 3).
Males significantly had positive attitude more than females (n = 427 and 373, respectively) (Overall P-value = 0.007). Good knowledge was significantly associated with a positive attitude (Overall P-value = 0.019) (Table 4).
Regarding the binary logistic regression, being a male, belonging to a can read and write education level, and being employed were significant predictors of positive TB attitude (P-value = 0.018, 0.027, and 0.024), respectively (Table 4). Being a male was predicted to have a positive attitude 4.726 times more than being a female (95% CI: 1.310–17.043). Belonging to a can-read and write education level was predicted to have a positive attitude 10.761 times more than belonging to a cannot read and write level (95% CI: 1.317–87.953) (Table 4).
All single participants showed good practices against TB 279 (100%). Males had non-significant good practice more than females (Overall P-value = 1). Overall, very good practices against the prevention of TB were noted throughout (Table 5).
Regarding the binary logistic regression, attitude score was found to be a significant predictor related to the practices toward TB [OR = 0.031 (95% CI: 0.002–0.506), P-value = 0.015] as shown in Table 5.
Young participants were expected to have a good practice 1.013 times more than old participants (95% CI: 0.911–1.128). A male was predicted to have a good practice 1.188 times more than a female (95% CI: 0.074–19.055). Being employed was predicted to have a good practice 3.094 times more than being unemployed (95% CI: 0.193–49.691) (Table 5).
A strong positive correlation was noted between knowledge grading and knowledge score [Rho (R)-value = 0.696 and P-value = 0.001]. A low positive correlation was noted between practice grading and practice score (R-value = 0.152 and P-value = 0.001). A strong negative correlation was noted between attitude grading and attitude score (R-value = −0.747 and P-value = 0.001) (Table 6).
In this study, most participants had good knowledge (87.7%) and attitude (96.5%) toward TB. Similarly, participants ranked highly overall for TB practice. Higher monthly income and being female were observed predictors for higher scores.
However, this may not genuinely reflect the extent of TB KAP among the participants, as the country is going through unique circumstances. The Taliban regime has come into power. The dominance was followed by sanctions from different countries and international organizations, which resulted in funding suspension. Since then, the already-fragile healthcare system has not been functioning properly. The country's largest healthcare services provider “Sehatmandi” program, has lost its full functionality (14). The program aimed to provide essential health services to hospitals nationwide. Considering the unfolding events in Afghanistan and the lack of healthcare functionality, TB patients may remain undiagnosed. There is little or no health promotion activity to raise awareness and provide useful information about TB. Moreover, TB may spread among internally displaced refugees who are displaced because of conflict and war; thus, it may further wreak havoc on the healthcare system.
The finding of this study regarding knowledge about TB is reported higher than in a study done in the Mecha district of Ethiopia (also a low-income country), where 54% of participants had good knowledge about TB (16). However, the present finding is in line with another Ethiopian study carried out in the Shinile town of eastern Ethiopia. The majority of the participants had good knowledge about TB (18). A further cross-sectional study in Southern Ethiopia showed that 48.6% of the participants were considered to have good knowledge of TB (19). In this latter study, the score was significantly associated with gender and age. Other differences could be due to socio-economic, cultural, and environmental factors, particularly observed in a study conducted in the Gambia, where two-thirds of all participants had good or appropriate knowledge. Good TB knowledge was associated with age, marital status, education, employment, and a good TB attitude and practice (20).
Regarding the attitude, 96.5% of the participants had a good attitude toward TB. Females had a better attitude than their male counterparts; this is in line with a study conducted in Shingle town, eastern Ethiopia, where half of the participants considered TB a very serious disease (18). In another study conducted in the North Mecha district of Ethiopia, 68% of the participants stated a good attitude, and 44% were ranked as having good practice (16). Similarly, in a study conducted in Thailand, 47.9% of study participants were categorized with a high level of attitude TB (21).
In this Afghanistan study, those participants with a better attitude had good practice toward TB. Only a few participants reported poor practice regarding TB. Furthermore, male participants had better practice, but it was not statistically significant. Observed differences may reflect social dynamics, environment, and perceived access to healthcare facilities. These patients were interviewed in the health settings of Kabul, the capital of Afghanistan, where access to TB medication is available. However, this does not apply to all country contexts, especially rural ones.
In this study, 98% of the participants stated that TB is preventable in our study. This high number could be attributable to Kabul's awareness program and widely available treatment centers. The finding is similar to what is reported in Shinali town, where 79.3% of the participants responded that transmission of TB would be preventable (16). However, in another study conducted in Tepi General Hospital of Ethiopia, the majority (70%) of participants responded that its transmission is not preventable, while 92 (22.4%) replayed that covering the mouth and nose while coughing or sneezing is a possible method to prevent the transmissions (22).
Most participants (96.6%) stated cough as the main symptom, followed by fever and loss of appetite. Similar symptoms were reported by other participants in other studies (16, 20, 23).
Gender and level of education were associated with better knowledge of TB; this is in line with a study conducted in Khyber Pakhtunkhwa, Pakistan, where females and education level was correlated with better knowledge of TB (24).
Our study has several limitations. The study was conducted only in the capital, Kabul. The findings cannot be generalized to the whole country. Further studies are needed to provide a more in-depth assessment of TB in the country. Moreover, the study was done in hospital settings. Hence, there could be differences among participants in the community. Thus, another study could provide greater insight into this.
The study concluded that participants had good knowledge, attitude, and practice toward TB. A recommendation for policymakers is that TB knowledge is high in this study population, which can be used as a stepping-stone for future health promotion activities. Future awareness-raising campaigns will need to be tailored to the needs and socio-economic circumstances of the target communities. This study can contribute to the evidence base that informs those campaigns. Further research is warranted to provide additional data from other Afghanistan populations to allow comparisons with the findings from this study; this should include vulnerable individuals who find it difficult to access healthcare, residents in rural areas where healthcare is especially limited, and internally displaced or refugee Afghan populations. These are all groups at higher risk of both tuberculosis and drug-resistant tuberculosis.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Microbiology Department of Kabul University of Medical Sciences Research Committee (KUMS-MD-2241). The patients/participants provided their written informed consent to participate in this study.
ME and AN conceived the concept of the paper. ME, SA, and MK wrote the first draft and performed the analysis. KR, RN, and TD contributed data collection. AN and MH edited the second draft. All authors read and approved the final draft.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.933005/full#supplementary-material
1. Global Tuberculosis Report s. Available online at: https://www.who.int/teams/global-tuberculosis-programme/tb-reports (accessed April 9, 2022).
2. Tuberculosis - Symptoms and Causes - Mayo Clinic. Available online at: https://www.mayoclinic.org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250 (accessed March 31, 2022).
3. Tuberculosis. Available online at: https://www.who.int/news-room/questions-and-answers/item/tuberculosis (accessed March 31, 2022).
4. Tuberculosis: Multidrug-Resistant Tuberculosis (MDR-TB). Available online at: https://www.who.int/news-room/questions-and-answers/item/tuberculosis-multidrug-resistant-tuberculosis-(mdr-tb) (accessed March 31, 2022).
5. Chanda-Kapata P, Ntoumi F, Kapata N, Lungu P, Mucheleng'anga LA, Chakaya J, et al. Tuberculosis, HIV/AIDS and Malaria Health Services in sub-Saharan Africa – A Situation Analysis of the Disruptions and Impact of the COVID-19 Pandemic. (2022). Available online at: https://www.sciencedirect.com/science/article/pii/S1201971222001734 (accessed March 31, 2022).
6. Global Tuberculosis Report. (2021). Available online at: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2021 (accessed June 16, 2022).
7. Afghanistan. Tuberculosis Kills 13 000 Afghans Every Year. World Health Organization - Regional Office for the Eastern Mediterranean. Available online at: http://www.emro.who.int/afg/afghanistan-news/tuberculosis-kills-13-000-afghans-every-year.html (accessed March 31, 2022).
8. More Afghans Killed by Tuberculosis Than COVID in 2020. Available online at: https://www.aa.com.tr/en/asia-pacific/more-afghans-killed-by-tuberculosis-than-covid-in-2020/2187078 (accessed March 31, 2022).
9. Knowledge, Attitudes and Practices on Tuberculosis Infection Prevention and Associated Factors Among Rural and Urban Adults in Northeast Tanzania: A Cross-Sectional Study | PLOS Global Public Health. Available online at: https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0000104 (accessed June 16, 2022).
10. Tuberculosis Hits More Men Than Women. But Not in Afghanistan. The New Humanitarian. (2021). Available online at: https://www.thenewhumanitarian.org/news-feature/2021/2/24/tuberculosis-hits-more-women-in-afghanistan (accessed March 31, 2022).
11. Chen X, Du L, Wu R, Xu J, Ji H, Zhang Y, et al. Tuberculosis-related stigma and its determinants in Dalian, Northeast China: a cross-sectional study. BMC Public Health. (2021) 21:6. doi: 10.1186/s12889-020-10055-2
12. Health Literacy Knowledge Related to Tuberculosis Among Outpatient | RRTM. Available online at: https://www.dovepress.com/health-literacy-and-knowledge-related-to-tuberculosis-among-outpatient-peer-reviewed-fulltext-article-RRTM (accessed June 16, 2022).
13. Tharwani ZH, Shaeen SK, Arshad MS, Khalid MA, Islam Z, Nemat A, et al. Polio amid a humanitarian crisis in Afghanistan: challenges and recommendations. Lancet Infect Dis. (2022) 22:168–9. doi: 10.1016/S1473-3099(22)00004-4
14. Shah J, Essar MY, Qaderi S, Rackimuthu S, Nawaz FA, Qaderi F, et al. Respiratory health and critical care concerns in Afghanistan. Lancet Resp Med. (2022) 10:229–31. doi: 10.1016/S2213-2600(21)00583-X
15. Narain K, Rackimuthu S, Essar MY, Vink M. Call for solidarity: the war may be over in Afghanistan but the health crises continue. J Glob Health. (2022) 12:03002. doi: 10.7189/jogh.12.03002
16. Kasa AS, Minibel A, Bantie GM. Knowledge, attitude and preventive practice towards tuberculosis among clients visiting public health facilities. BMC Res Notes. (2019) 12:276. doi: 10.1186/s13104-019-4292-2
17. Metz CE. Basic principles of ROC analysis. Semin Nucl Med. (1978) 8:283–98. doi: 10.1016/S0001-2998(78)80014-2
18. Tolossa D, Medhin G, Legesse M. Community knowledge, attitude, and practices towards tuberculosis in Shinile town, Somali regional state, eastern Ethiopia: a cross-sectional study. BMC Public Health. (2014) 14:804. doi: 10.1186/1471-2458-14-804
19. Arja A, Godana W, Hassen H, Bogale B. Patient delay and associated factors among tuberculosis patients in Gamo zone public health facilities, southern ethiopia: an institution-based cross-sectional study. PLoS ONE. (2021) 16:e0255327. doi: 10.1371/journal.pone.0255327
20. Bashorun AO, Linda C, Omoleke S, Kendall L, Donkor SD, Kinteh M-A, et al. Knowledge, attitude and practice towards tuberculosis in Gambia: a nationwide cross-sectional survey. BMC Public Health. (2020) 20:1566. doi: 10.1186/s12889-020-09685-3
21. Sreechat S. Assessment of knowledge, attitude and preventive behavior of pulmonary tuberculosis among myanmar refugees in ban mai nai soi temporary shelter, Mae Hong Son, Thailand. J Health Res. (2013) 27:391–8.
22. Angelo AT, Geltore TE, Asega T. Knowledge, attitude, and practices towards tuberculosis among clients visiting tepi general hospital outpatient departments, 2019. Infect Drug Resist. (2020) 13:4559–68. doi: 10.2147/IDR.S287288
23. Datiko DG, Habte D, Jerene D, Suarez P. Knowledge, attitudes, and practices related to TB among the general population of Ethiopia: findings from a national cross-sectional survey. PLoS ONE. (2019) 14:e0224196. doi: 10.1371/journal.pone.0224196
24. Knowledge, Awareness and Health-Seeking Behaviour Regarding Tuberculosis in a Rural District of Khyber Pakhtunkhwa, Pakistan. Available online at: https://www.hindawi.com/journals/bmri/2020/1850541/ (accessed April 14, 2022).
Keywords: tuberculosis, healthcare system, Afghanistan, COVID-19, crisis
Citation: Essar MY, Rezayee KJ, Ahmad S, Kamal MA, Nasery R, Danishmand TJ, Head M and Nemat A (2022) Knowledge, Attitude, and Practices Toward Tuberculosis Among Hospital Outpatients in Kabul, Afghanistan. Front. Public Health 10:933005. doi: 10.3389/fpubh.2022.933005
Received: 30 April 2022; Accepted: 20 June 2022;
Published: 11 July 2022.
Edited by:
Syed Mohammed Basheeruddin Asdaq, University of Almaarefa, Saudi ArabiaReviewed by:
Basheerahmed Abdulaziz Mannasaheb, Almaarefa University, Saudi ArabiaCopyright © 2022 Essar, Rezayee, Ahmad, Kamal, Nasery, Danishmand, Head and Nemat. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arash Nemat, ZHIuYXJhc2huZW1hdEB5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.