- 1Department of Sports and Exercise Medical Sciences, School of Sports and Exercise Medicine, University of Health and Allied Science, Ho, Ghana
- 2Medical Sociology and Psychobiology, Department of Health and Physical Activity, University of Potsdam, Potsdam, Germany
Background: Physical activity (PA) and exercise have been identified to improve the general fitness and health. Although, the Pregnancy Physical Activity Questionnaire (PPAQ) has been validated for use in assessing PA in pregnant women. However, understanding the knowledge and participation levels of PA in pregnant women in the underdeveloped regions of Ghana is of clinical relevance to foster education and promotion of PA. In Ghana, pregnant women believe the “myth” (mostly in rural areas and underdeveloped regions) that exercising in the first trimester might lead to miscarriage. Thus, the main objective of this study was to investigate the extent of knowledge and participation levels in PA among pregnant women in Ho, Ghana using a self-developed questionnaire which consisted of some questions adapted from the PPAQ.
Methods: Seventy-seven (n = 77) pregnant women between the ages of 18–50 years were recruited from three hospitals across the Ho municipality of Ghana. A self-developed questionnaire which consisted of some questions taken from the PPAQ was administered to participants under the researchers' supervision. Spearman's correlation analysis was used to find the association between the level of participation in PA, knowledge of PA and gestational age among pregnant women.
Results: From the total participants (n = 77) recruited, 57 (74%) of the participants scored high in PA knowledge. Most of the participants 48 (62.3%) answered that PA promotes healthy pregnancy. Participants who reported barriers to PA during pregnancy were no exercise habits 51 (66.2%), having no time 17 (22.1%) and fear of miscarriage 9 (11.7%). There was a significant (p < 0.05) association between the level of participation and gestational age. No significant (p > 0.05) association between the level of participation and knowledge of PA was observed.
Conclusion: There is a high level of knowledge of PA among pregnant women in Ho, Ghana. However, most pregnant women rather engage in PA as their gestational age increases. Thus, to foster sustainable exercise participation during pregnancy, all healthcare providers saddled with the responsibility of providing maternal healthcare must strengthen the education and promotion of exercise and PA among pregnant women in Ho, Ghana.
Introduction
Physical Activity (PA) is any voluntary movement produced by skeletal muscle contractions which require energy (1). Exercise is PA that is planned, structured and repetitive for conditioning the body (2). Regular participation in PA improves the overall general health and fitness of pregnant women (3). The maternity period is a vital part of the reproductive life of women with many physical and biological changes in the body during pre-post pregnancy (4). PA amongst pregnant women improve posture and decreases discomforts such as backaches and fatigue (5). During pregnancy, physical and biological changes cause hormonal imbalances which lead to anxiety and stress among pregnant women (6). However, PA during pregnancy rather improves mood (7, 8), self-esteem (9, 10), anxiety (11, 12), and depressive disorders (13). Liu et al. (14) suggested exercises usually prescribed for pregnant women include water aerobics, running, brisk walking, yoga, Kegel and breathing exercises. Exercises such as brisk walking, stationary cycling and swimming improve both cardiovascular and muscular systems and have been recommended for pregnant women (14–16). Additionally, special antenatal yoga and pilates designed for expectant mothers reduce stress, improve flexibility, and encourage stretching and focused breathing (17). These exercises are safe and may not expose these expectant mothers to any risks or complications. Furthermore, there is evidence that PA may prevent gestational diabetes, relieve stress, and build more stamina needed for labor and delivery (18, 19). There are certain contraindications to exercise during pregnancy which may include but are not limited to: cervical insufficiency, pre-eclampsia, heart and lung diseases, placenta previa and severe anemia (20, 21). Thus, a clinical decision should be sought to rule out any contraindications to exercise during pregnancy (22, 23).
PA in the general population is considered too low and this is reflected in pregnant women as well (24, 25). The American College of Obstetricians and Gynecologists (ACOG) has suggested that healthy pregnant women should engage in 150 min of moderate PA per week (26, 27). Despite this, there have been some misconceptions associated with PA and exercises during pregnancy including miscarriage, low birth weight, and early delivery (28, 29). In Ghana, pregnant women (mostly in rural areas and underdeveloped regions), believe the myth that exercising in the first trimester might lead to miscarriage (30). Interestingly, barriers to the participation of exercise among pregnant women have been reported and these barriers are a combination of physical, psychological, and social factors (31, 32). Whilst some pregnant women reported embarrassment about their body appearance, others also reported that the lack of social support from loved ones, and the fear of danger of exercise to themselves and the growing fetus are some of the reasons for which they would rather not participate in exercise or PA (32–35). Some studies (32, 34) reported a lack of education and knowledge of safe ways to exercise during pregnancy. It is said that women who exercise regularly before pregnancy are more likely to keep this attitude during pregnancy than those who were sedentary before becoming pregnant (36, 37). Thus, education and health promotion programs targeting women in their reproductive years are of vital importance for achieving sustainable health practices.
The Royal Australian and New Zealand College of Obstetricians and Gynecologists conducted a study to evaluate the knowledge of PA among pregnant women. They reported that most of the participants correctly reported knowledge of safe levels of PA in pregnancy in line with the recommendation for exercise during pregnancy (38). Also, a study conducted in South Africa reported that (70.2%) pregnant women received PA information from television, the radio, and other media sources (39). However, a study conducted in Nigeria on the knowledge and attitude of pregnant Nigerian women toward antenatal exercise reported that (15.8%) of the respondents had a negative attitude toward antenatal exercise due to limited information on exercise (83.3%) and tiredness (70.0%) as another factor (29). In Ghana, Moses et al. (30) reported that (71.5%) pregnant women were aware of the importance of PA in the Kumasi metropolis but concluded that pregnant women do not spend more time performing PA. Existing literature on the association between knowledge of PA and participation in PA among pregnant women are limited especially in sub-Sahara Africa (29, 39). Only one study (30) has been conducted and published in Ghana. The Volta region of Ghana is one of the less developed regions with poor infrastructures and amenities. The Pregnancy Physical Activity Questionnaire (PPAQ) has been validated for use in assessing PA in pregnant women (40, 41). However, implementing the standardized PPAQ can be problematic in context where cultural and health beliefs toward exercising during pregnancy exist. Thus, understanding the knowledge and participation levels in PA of pregnant women in underdeveloped regions in Ghana is of clinical relevance to foster education and promotion of PA. The main objective of this study was to investigate the extent of knowledge and participation levels of PA among pregnant women in Ho, Ghana using a self-developed questionnaire which consisted of some questions taken from the PPAQ.
Materials and methods
Study population
Participants were recruited through advertisement via posters pasted in the consulting rooms in hospitals and direct word-of-mouth communication of the research topic to the participants. A total of 77 participants with ages between 18 and 50 years were recruited for the study. The study population consisted of pregnant women in Ho, who regularly visited the antenatal clinics of Ho Teaching Hospital, Ho Municipal Hospital and Ho Royal Hospital of Ghana. Exclusion criteria were: pregnant women who had critical health conditions like uncontrolled gestational diabetes, pre-eclampsia, and placenta previa because researchers were aware that such women were advised by healthcare providers to rest and avoid any form of physical stress or strain to prevent complications. Again, pregnant women who were not frequent with their antenatal visits were excluded because researchers had limited time for data collection hence could only use participants who were readily available. Lastly, those below 18 years were also excluded because researchers needed to seek consent from their guardians before administering the questionnaires. Ethical approval for the study was sought from the Research and Ethics Committee of the University of Health and Allied Health Sciences [Protocol Identification Number: UHAS-REC A.8 (11) 20-21] and written informed consent was obtained from all participants.
Measures
A new self-developed questionnaire which consisted of some questions adapted from the PPAQ were administered to the participants. The questions taken from the standardized PPAQ was necessary for the setting of the current study. The PPAQ has been successfully used in studies published elsewhere (40, 41). The new self-developed questionnaire was administered to participants to fill to assess their knowledge and participation levels in PA. Data collection started from March 16th to May 12th of 2021. Caution was taken to prevent COVID-19 infection. Chasan-Taber et al. (41) developed the PPAQ with 32 activities including household/caregiving (13 activities), occupational (five activities), sports/exercise (eight activities), transportation (three activities), and inactivity (three activities), respectively. The new self-developed questionnaire consisted of 25 questions which were divided into three (3) sections. Section one consisted of 8 questions on socio-demographic information [Adapted PPAQ (n = 0, 0%) vs. New self-developed questionnaire (n = 8, 100%)]. The second section consisted of 5 questions on knowledge of PA, positive role of PA during pregnancy, and the source of information on PA [Adapted PPAQ (n = 0, 0%) vs. New self-developed questionnaire (n = 5, 100%)]. Section three of the questionnaire consisted of 12 questions focusing on household/caregiving activities [Adapted PPAQ questions (n = 6, 100%) vs. New self-developed questionnaire (n = 0, 0%)], occupational activities [Adapted PPAQ (n = 2, 66.7 %) vs. New self-developed questionnaire (n = 1, 33.3%)], sports/exercise activities [Adapted PPAQ (n = 0, 0%) vs. New self-developed questionnaire (n = 1, 100%)], barriers to PA [Adapted PPAQ (n = 0, 0%) vs. New self-developed questionnaire (n = 1, 100%)], and benefit of PA during pregnancy [Adapted PPAQ (n = 0, 0%) vs. New self-developed questionnaire (n = 1, 100%)] (see Supplementary Table S1).
Sample size
The sample size was determined using records of attendance of the pregnant women visiting the antenatal clinics from the various hospitals. The total amount of pregnant women attendance to the antenatal clinic from August 2020–February 2021 was 96. The Slovin's formular was used for calculating sample size for the study with a confidence interval of 95% and p = 0.05 (42). The sample size of (n = 77) was obtained using the Slovin's formular below.
where “n” is the sample size, “N” is the population size and “e” is the margin error.
Statistical analysis
Data were analyzed using Jamovi version 1.6.23 software. Descriptive statistics was used to report the demographics and estimate the level of knowledge and participation in PA. Data were represented in frequency tables. Spearman's correlation analysis was used to find the association between the level of participation in PA, knowledge of PA and gestational age among pregnant women. The level of significance was set at p < 0.05.
Results
Participant demographics
There were (n = 77) participants in this study. The demographic data are presented according to the following variables: age, relationship status, educational level, occupation, planned pregnancy, antenatal care type and previous history of abortion (see Table 1). Most participants were between the ages of 21–30, (n = 41, 53.3%) and 31–40, (n = 34, 44.2%) whereas (n = 2, 2.6%) were age of <20. Of the total participants; (n = 10, 13.0%) were single whilst (n = 67, 87.0%) were married. The highest level of education of participants were: primary (n = 13, 16.9%), JHS (n = 5, 6.5%), SHS (n = 22, 28.6%) and Tertiary (n = 37, 48%). Occupations of the participants were: government staff (n = 27, 35.1%), private sector workers (n = 36, 46.8%), and traders (n = 5, 6.5%) whilst (n = 4, 6.5%) were students and (n = 5, 5.3%) were unemployed. 56 (72.7%) of the participants planned their pregnancies, whilst 21 (27.3%) were unplanned. The antenatal care types of the participants were public hospital (n = 54, 70.1%) and private hospital (n = 23, 29.9%), respectively. Regarding the history of abortion, (n = 7, 9.1%) of participants had a history of abortions whilst (n = 70, 90.9%) had none (see Table 1).
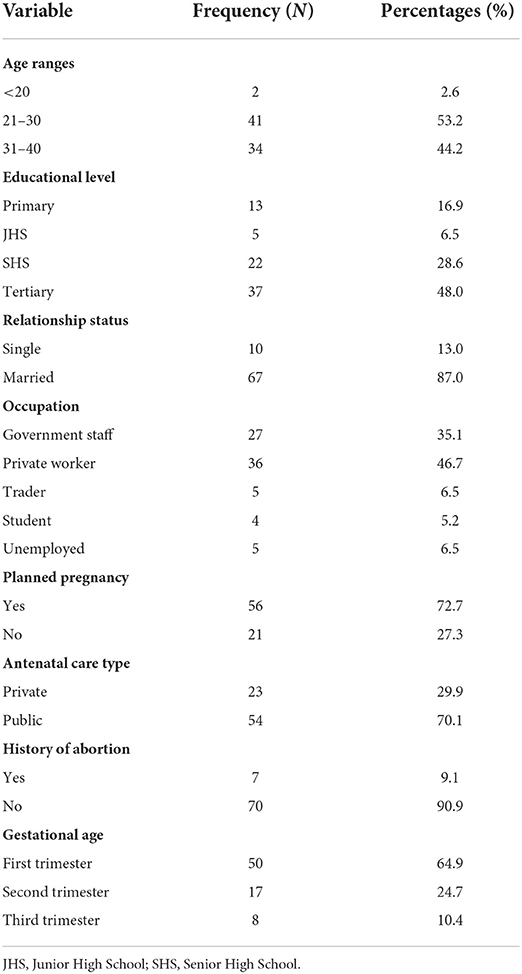
Table 1. Profile of participants by age, educational level, relationship status, occupation, planned pregnancy, antenatal care type and history of abortion (n = 77).
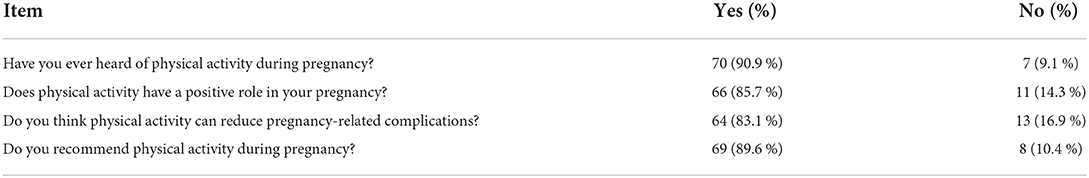
Knowledge of physical activity
A set of questions that required a “Yes” or “No” answering system was used to assess the level of PA knowledge among the participants, where “1” or “0” were scored, respectively. Four questions were asked in this section to ascertain if participants knew PA and exercise. First, (90.9%) responded “Yes” whilst (9.1%) responded “No” on ‘if they had ever heard of PA during pregnancy. Secondly, 66 (85.7 %) responded “Yes” whilst 11 (14.3 %) responded “No” “if they know that PA has a positive role in pregnancy”. Also, most of the participants 64 (83.1 %) said “Yes” to “Do you think PA can reduce pregnancy-related complications” whilst the remaining 13 (16.9 %) said “No.” Lastly, participants were asked “if they recommend PA during pregnancy” and 69 (89.6 %) said “Yes” whilst 8 (10.4 %) said “No” (see Table 2).
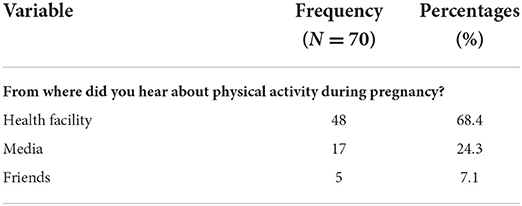
Source of knowledge
As follow-up questions, participants were given three options of possible sources of information about PA and pregnancy and the following were their responses: Health facility 48 (68.4%), media 17 (24.3%), and friends 5 (7.1%) (see Table 3).
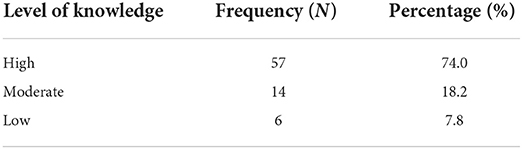
Level of knowledge
To be able to assess the overall level of knowledge of PA among participants, a set of questions that also required a “Yes” or “No” answering system was used. These questions covered basic household, occupational and leisure time activities. A set of 10 questions with individual score values of 1 for a “Yes” response and 0 for a “No” response was asked. The cumulative scores of the responses were graded as High for a score of (8–10), Moderate for a score of (5–7), and Low for a score of (0–4). Each participant was required to score between 0 and 10 which upon grading represented their level of PA. 57 (74.0%) of the participants scored “High,” 14(18.2%) scored “Moderate,” and 6 (7.8%) scored “Low” for the levels of knowledge of the PA category (see Table 4). No significant (r = 0.061, p > 0.05) association between the level of participation and knowledge of PA was observed. This shows that level of knowledge does not increase the level of participation in PA (see Table 5). There was a significant (r = 0.280, p < 0.05) association between level of participation and gestational age. This shows that pregnant women engage in PA as their gestational age increases (see Table 6).
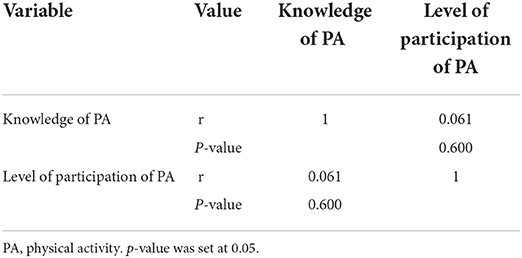
Table 5. Correlation analysis between knowledge of PA and level of participation of PA in pregnant women.
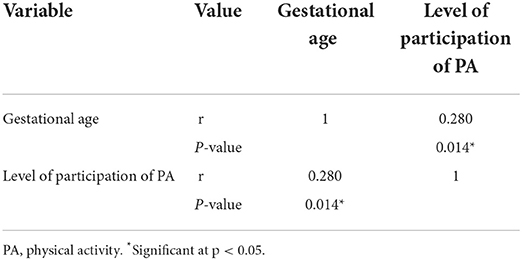
Table 6. Correlation analysis between the level of participation of PA and gestation age of pregnant women.
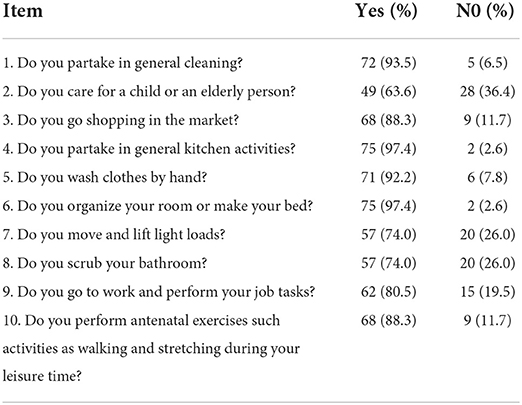
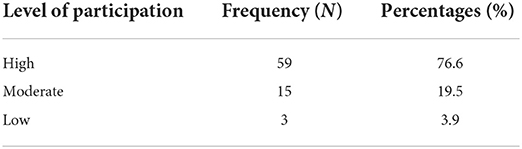
Type of physical activity
Some basic PA were listed in Table 7 for participants to select the type of activities they engage in to assess their level of participation in PA and antenatal exercises. The same scoring method to assess the level of knowledge of PA was used here to classify whether the level of participation was high, moderate, or low. 59 (76.6%) scored “High,” 15 (19.5%) scored “Moderate,” and 3 (3.9%) scored “Low” (see Table 8).
Barriers to physical activity
As part of assessing the participants' level of participation in PA, participants were asked about the barriers to participating in antenatal exercises. Participants reported barriers to PA during pregnancy were no exercise habits 51 (66.2%), no time 17 (22.1%) and fear of miscarriage 9 (11.7%) (see Table 9).
Benefits of exercise during pregnancy
The participants were asked why PA during pregnancy is beneficial. 48 (62.3%) of the participants reported “it promotes healthy pregnancy,” 23 (29.9%) reported “it facilitates delivery” whilst the remaining 6 (7.8%) of the participants reported “it reduces pregnancy-related complications” (see Table 10).
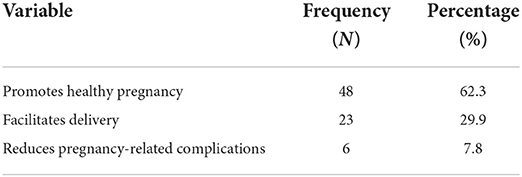
Table 10. Participant's specific responses to why physical exercise during pregnancy is beneficial (n = 77).
Discussions
The main aim of the current study was to evaluate the knowledge and participation levels of PA among pregnant women in Ho, Ghana using a self-developed questionnaire which consisted of some questions adapted from the PPAQ. There was a 100% response rate for this study, the study population constituted participants from a wide range of pregnant women (from both public and private hospitals) from different age groups (i.e., 18–50 years) giving a good representation of the population. Per the findings of this study, majority (74.0%) of the study participants had high knowledge of PA. This is similar to the results reported by Moses et al. (30) in the Ashanti region of Ghana. However, Sujindra et al. (43) and Mbada et al. (29) both reported an overall low level of knowledge of PA among study participants. These contrasting results between this study and the previous studies were due to the different PA and exercise questionnaires consisting of specific knowledge about antenatal exercise variables such as breathing, back care, abdominal exercises, and aerobics exercises such as swimming and cycling during pregnancy were assessed. However, the questionnaires used in this current study consisted of basic household chores and focused on whether the participants had ever heard of PA during pregnancy, whether it had a positive role in their pregnancy, whether they thought it could reduce pregnancy-related complications and whether they would recommend PA during pregnancy to others.
It should be indicated that in the study by Mbada et al. (29) among Nigerian women, nearly 70% were employed and had undergone tertiary education, whiles 48.1% of the current study subjects had completed tertiary education. Additionally, the lack of education and knowledge about safe exercise practices during pregnancy can be a barrier to exercise (31, 32, 34) and this could prevent pregnant women to begin and sustain exercise practicing during and after pregnancy. The results indicated that (76.6%) of the study participants had a high level of participation in PA, whiles (19.5%) had a moderate level of participation in PA. Participants were asked objectively whether they thought PA during pregnancy was beneficial and the responses were as follows; 62.3% of the participants said that it promotes healthy pregnancy whilst 29.9% said that it facilitates delivery. Okafor and Ter Goon (39) reported in their study that; the majority of their participants' reported PA was beneficial in improving cardiovascular function (86.3%) and reducing infant weight (61.4%), reducing musculoskeletal discomfort (82.7%), reducing back pain (85.7%) and incidence of muscle cramps and oedema in the lower limbs (91.3%). These findings were synonymous to data from the current study and show that PA is beneficial during pregnancy. From the results, (68.6%) of the study participants heard about PA from health facilities whilst (24.3%) reported hearing about PA during pregnancy via the media. In contrast, Okafor and Ter Goon (39) reported that (70.2%) of their study participants heard of PA from the media whilst (27.0%) heard it from their friends. This shows that social media and social support can be used as an avenue for exercise participation and health promotion (44). Additionally, using telemedicine as a form of exercise guidance has been reported to significantly lower premature delivery (45).
According to the findings of this study, the barriers for not engaging in PA by participants were no exercise habits, having no time and fear of miscarriage which was similar to the findings of Okafor and Ter Goon (39). Muzigaba et al. (46) recorded similar results as participants reported fear of hurt for baby and mother as well as no time as barriers to engaging in PA during pregnancy. Unsupportive environment as well as not knowing when and how to participate in PA were also recorded as barriers (46). This shows that education and sustainable exercise programs structured by healthcare providers especially exercise professionals are needed to facilitate PA participation among pregnant women. Likewise, education to the general public on supporting and encouraging expectant mothers should be considered, and to promote social support to these women. PA and exercise training should also be included in the education given at antenatal clinics to increase the knowledge of PA during pregnancy. This will help pregnant women to feel confident and engage in exercise participation which has been proven to be beneficial for pregnancy outcomes (8, 29, 45, 47).
Furthermore, the results indicated no significant (p > 0.05) association between the level of knowledge of PA of the participants and their level of participation in PA. On the contrary, Abedzadeh et al. (48) reported a significant association between their participants' knowledge and PA participation during pregnancy. Also, the significant association (p < 0.05) between the gestational age of the participants and their levels of participation in PA suggested that pregnant women would rather engage in PA as their gestational age increases in the current study. Conversely, it was reported by Watson et al. (49) that pregnant urban black South African women decreased their participation in PA from the second to third trimester. This is interesting and noteworthy because one would think that women living in the urban areas are more informed on the health benefits of PA during pregnancy due to the improved health infrastructures and access to information as compared to those in the rural areas (50). Again, uncertainty still remains in linking educational background to the level of PA participation. This could be a contributing factor as Watson et al. (49) reported that majority of the participant's highest level of education was secondary level, whereas that of this study was at the tertiary level. Ultimately, women should be encouraged to cultivate an active lifestyle even before pregnancy to ensure that this behavior is practiced, during the pregnancy period, and thereafter to guarantee a reduction in pregnancy-related complications. Abedzadeh et al. (48) stated in their study that, (48.7%) of pregnant women had continued to exercise till the 9th month of their pregnancy. Interestingly, active women continue to exercise even during pregnancy more than non-active women before becoming pregnant (36, 37).
The standardized PPAQ has been validated to use in assessing PA in pregnant women (40, 41). Whilst the standardized PPAQ may create uniformity among studies assessing PA in pregnant women, it may be difficult to apply the standardized PPAQ in a cultural context where there exist cultural and health beliefs toward exercise during pregnancy. But this current new self-developed questionnaire consisting of some questions adapted from the PPAQ can be the first step and a simple tool to be used in assessing PA in pregnant women in less developed regions of Ghana, and especially in rural areas that believe in a myth that exercising during the first trimester might lead to miscarriage (30). This simple questionnaire could be used in epidemiological studies to assess the knowledge and level of PA in pregnant women in the other less developed regions of Ghana to help develop PA programs for pregnant women as well as women in their reproductive ages. In the clinical settings, healthcare professionals can use this simple questionnaire to assess the knowledge and level of participation of PA in pregnant women, especially in rural and less developed regions of Ghana. Thus, to foster sustainable exercise participation during pregnancy, decision-making bodies, stakeholders, and healthcare providers saddled with the responsibility of providing maternal healthcare must strengthen the education and promotion of PA among pregnant women in Ho, Ghana.
Strengths and limitations
This is the first study to assess the knowledge and level of PA of pregnant women in Ho, Ghana. The study adds to the body of literature on how the knowledge and level of PA can be assessed in pregnant women in a less developed region of Ghana. In the clinical settings, healthcare professionals can use this simple questionnaire to assess the knowledge and level of participation of PA in pregnant women especially in rural and underdeveloped regions of Ghana. Thus, setting the foundation for education and promotion of PA programs for pregnant women in less developed regions in Ghana. Despite these strengths, the current study had several limitations. Pregnancy is considered sacred and so only a few participants were willing to participate in the current study. Future studies implementing longitudinal research design with a large sample size are warranted. There was limited availability of published materials, especially within Ghana and the Sub-Saharan African continent, for possible comparison of results. Lastly, care should be taken when interpreting the results, as questionnaires may lead to over-estimation of reporting by participants (51, 52). The PPAQ is validated for assessing PA in pregnant women. The current new self-developed questionnaire consisting of some questions adapted from the PPAQ needs validation.
Conclusion
There is a high knowledge of PA amongst pregnant women in Ho, Ghana. However, most pregnant women rather engage in PA as their gestational age increases. Thus, to foster sustainable exercise participation during pregnancy, decision-making bodies, stakeholders, and healthcare providers saddled with the responsibility of providing maternal healthcare must strengthen the education and promotion of PA among pregnant women in Ho, Ghana.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Research and Ethics Committee of the University of Health and Allied Health Sciences [Protocol Identification Number: UHAS-REC A.8 [11] 20-21]. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DA designed the study. DA and FO wrote and revised the manuscript. FA-S and VN collected the data and conducted the analyses. All authors provided critical feedback, contributed to the final manuscript, and approved the final version of the manuscript.
Acknowledgments
The data for this article came from pregnant women visiting the antenatal clinics of the Ho Teaching Hospital, Ho Municipal Hospital, and Ho Royal Hospital. We thank all the participants and midwives for their support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.927191/full#supplementary-material
References
1. Melzer K, Lazzeri M, Armand S, Boulvain M, Schutz Y, Kayser B. Validation of the Actiheart for estimating physical activity-related energy expenditure in pregnancy. e-SPEN J. (2012) 7:e5–10. doi: 10.1016/j.eclnm.2011.12.008
2. Pascoe M, Bailey AP, Craike M, Carter T, Patten R, Stepto N, et al. Physical activity and exercise in youth mental health promotion: a scoping review. BMJ Open Sport Exerc Med. (2020) 6:e000677. doi: 10.1136/bmjsem-2019-000677
3. Harrison CL, Brown WJ, Hayman M, Moran LJ, Redman LM. March. The role of physical activity in preconception, pregnancy and postpartum health. Semin Reprod Med. (2016) 34:e28–37. doi: 10.1055/s-0036-1583530
4. Konlan KD, Kombat JM, Japiong M, Konlan KD. Perception of pregnant women on maternity care services at the volta regional hospital, Ghana. Int J Commun Med Public Health. (2018) 5:2699. doi: 10.18203/2394-6040.ijcmph20182602
5. Rodrigues WFG, Silva LRD, Nascimento MADL, Pernambuco CS, Giani TS, Dantas EHM. Prevalence of lower back pain and physical inactivity: the impact of psychosocial factors in pregnant women served by the family health strategy. Einstein. (2011) 9:489–93. doi: 10.1590/s1679-45082011ao2186
6. Talge NM, Neal C, Glover V, Early Early Stress Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health. Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. (2007) 48:245–61. doi: 10.1111/j.1469-7610.2006.01714.x
7. Cai C, Busch S, Wang R, Sivak A, Davenport MH. Physical activity before and during pregnancy and maternal mental health: # systematic review and meta-analysis of observational studies. J Affect Disord. (2022) 309:393–403. doi: 10.1016/j.jad.2022.04.143
8. Evenson KR, Mottola MF, Owe KM, Rousham EK, Brown WJ. Summary of international guidelines for physical activity following pregnancy. Obstet Gynaecol Surv. (2014) 69:407. doi: 10.1097/OGX.0000000000000077
9. Ribeiro MM, Andrade A, Nunes I. Physical exercise in pregnancy: benefits, risks and prescription. J Perinat Med. (2022) 50:4–17. doi: 10.1515/jpm-2021-0315
10. Shivakumar G, Brandon AR, Snell PG, Santiago-Muñoz P, Johnson NL, Trivedi MH, et al. Antenatal depression: a rationale for studying exercise. Depress Anxiety. (2011) 28:234–42. doi: 10.1002/da.20777
11. Abubakar IA. Regular physical activity during pregnancy improves maternal depressive symptoms. J Pharm Pract Commun Med. (2021) 7:17. doi: 10.5530/jppcm.2021.1.4
12. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
13. Kołomańska D, Zarawski M, Mazur-Bialy A. Physical activity and depressive disorders in pregnant women—a systematic review. Medicine. (2019) 55:212. doi: 10.3390/medicina55050212
14. Liu J, Blair SN, Teng Y, Ness AR, Lawlor DA, Riddoch C. Physical activity during pregnancy in a prospective cohort of British women: results from the Avon longitudinal study of parents and children. Eur J Epidemiol. (2011) 26:237–47. doi: 10.1007/s10654-010-9538-1
15. Córdoba-Caro LG, Barrantes-Borrachero I, Corchado-Gómez M, Oliva-Mendoza G, Parra-Chamizo M, Viera-León C. Systematic Review of the Effects of Physical Activity During Pregnancy. (2021). p. 174. doi: 10.18176/archmeddeporte.00040
17. Bisson M, Alméras N, Dufresne SS, Robitaille J, Rhéaume C, Bujold E, et al. A 12-week exercise program for pregnant women with obesity to improve physical activity levels: an open randomised preliminary study. PLoS ONE. (2015) 10:e0137742. doi: 10.1371/journal.pone.0137742
18. Cid M, González M. Potential benefits of physical activity during pregnancy for the reduction of gestational diabetes prevalence and oxidative stress. Early Hum Dev. (2016) 94:57–62. doi: 10.1016/j.earlhumdev.2016.01.007
19. Sanabria-Martínez G, García-Hermoso A, Poyatos-León R, Álvarez-Bueno C, Sánchez-López M, Martínez-Vizcaíno V. Effectiveness of physical activity interventions on preventing gestational diabetes mellitus and excessive maternal weight gain: a meta-analysis. BJOG Int J Obstet Gynaecol. (2015) 122:1167–74. doi: 10.1111/1471-0528.13429
20. Meah VL, Davies GA, Davenport MH. Why can't I exercise during pregnancy? time to revisit medical ‘absolute' and ‘relative contraindications: a systematic review of the evidence of harm and a call to action. Br J Sport Med. (2020) 54:1395–404. doi: 10.1136/bjsports-2020-102042
21. Tsakiridis I, Bakaloudi DR, Oikonomidou AC, Dagklis T, Chourdakis M. Exercise during pregnancy: a comparative review of guidelines. J Perinat Med. (2020) 48:519–25. doi: 10.1515/jpm-2019-0419
22. Tsironikos GI, Perivoliotis K, Bargiota A, Zintzaras E, Doxani C, Tatsioni A. Effectiveness of exercise intervention during pregnancy on high-risk women for gestational diabetes mellitus prevention: a meta-analysis of published RCTs. PLoS ONE. (2022) 17:e0272711. doi: 10.1371/journal.pone.0272711
23. Olson D, Sikka RS, Hayman J, Novak M, Stavig C. Exercise in pregnancy. Curr Sport Med Rep. (2009) 8:147–53. doi: 10.1249/JSR.0b013e3181a61d51
24. Lindqvist M, Lindkvist M, Eurenius E, Persson M, Ivarsson A, Mogren I. Leisure time physical activity among pregnant women and its associations with maternal characteristics and pregnancy outcomes. Sex Reprod Healthcare. (2016) 9:14–20. doi: 10.1016/j.srhc.2016.03.006
25. Bouchard C, Blair SN, Haskell WL. Physical Activity and Health. Human Kinetics. Champaign, IL: Human Kinetics (2012). doi: 10.5040/9781492595717
26. Yang X, Li H, Zhao Q, Han R, Xiang Z, Gao L. Clinical practice guidelines that address physical activity and exercise during pregnancy: a systematic review. J Midwifery Womens Health. (2022) 67:53–68. doi: 10.1111/jmwh.13286
27. ACOG committee opinion number 804. Physical activity and exercise during pregnancy and the postpartum period Obstet Gynecol. (2020) 135:e178–88. doi: 10.1097/AOG.0000000000003772
28. Brown WJ, Hayman M, Haakstad LA, Lamerton T, Mena GP, Green A, et al. Australian guidelines for physical activity in pregnancy and postpartum. J Sci Med Sport. (2022) 25:511–9. doi: 10.1016/j.jsams.2022.03.008
29. Mbada CE, Adebayo OE, Adeyemi AB, Arije OO Dada OO, Akinwande OA, et al. Knowledge and attitude of Nigerian pregnant women towards antenatal exercise: a cross-sectional survey. ISRN Obstet Gynecol. (2014) 2014:260539. doi: 10.1155/2014/260539
30. Moses MO, Donkoh S, Falola K. Physical activity and exercise participation duration of antenatal mothers. Am Int J Contemp Sci Res. (2015) 2:68–74.
31. Kandel P, Lim S, Pirotta S, Skouteris H, Moran LJ, Hill B. Enablers and barriers to women's lifestyle behavior change during the preconception period: a systematic review. Obes Rev. (2021) 22:e13235. doi: 10.1111/obr.13235
32. Leiferman J, Swibas T, Koiness K, Marshall JA, Dunn AL. My baby, my move: an examination of perceived barriers and motivating factors related to antenatal physical activity. J Midwifery Womens Health. (2011) 56:33–40. doi: 10.1111/j.1542-2011.2010.00004.x
33. Thornton PL, Kieffer EC, Salabarría-Peña Y, Odoms-Young A, Willis SK, Kim H, et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. (2006) 10:95–104. doi: 10.1007/s10995-005-0025-3
34. Clarke PE, Gross H. Women's behaviour, beliefs and information sources about physical exercise in pregnancy. Midwifery. (2004) 20:133–41. doi: 10.1016/j.midw.2003.11.003
35. Kieffer EC, Willis SK, Arellano N, Guzman R. Perspectives of pregnant and postpartum Latino women on diabetes, physical activity, and health. Health Educ Behav. (2002) 29:542–56. doi: 10.1177/109019802237023
36. Shum KW, Ang MQ, Shorey S. Perceptions of physical activity during pregnancy among women: a descriptive qualitative study. Midwifery. (2022) 107:103264. doi: 10.1016/j.midw.2022.103264
37. Gaston A, Cramp A. Exercise during pregnancy: a review of patterns and determinants. J Sci Med Sport. (2011) 14:299–305. doi: 10.1016/j.jsams.2011.02.006
38. Sword W, Heaman MI, Brooks S, Tough S, Janssen PA, Young D, et al. Women's and care providers' perspectives of quality prenatal care: a qualitative descriptive study. BMC Pregnancy Childbirth. (2012) 12:1–18. doi: 10.1186/1471-2393-12-29
39. Okafor UB, Ter Goon D. Physical activity in pregnancy: beliefs, benefits, and information-seeking practices of pregnant women in South Africa. J Multidiscip Healthcare. (2021) 14:787. doi: 10.2147/JMDH.S287109
40. Yin YN, Huang Y, Liu XH, Luo BR. Assessment of physical activity status among pregnant women in southwestern China. Front Nurs. (2019) 6:135–41. doi: 10.2478/FON-2019-0020
41. Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a pregnancy physical activity questionnaire. Med Sci Sports Exerc. (2004) 36:1750–60. doi: 10.1249/01.MSS.0000142303.49306.0D
43. Sujindra E, Bupathy A, Suganya A, Praveena R. Knowledge, attitude, and practice of exercise during pregnancy among antenatal mothers. Int J Educ Psychol Res. (2015) 1:234. doi: 10.4103/2395-2296.158347
44. Jane M, Hagger M, Foster J, Ho S, Pal S. Social media for health promotion and weight management: a critical debate. BMC Public Health. (2018) 18:1–7. doi: 10.1186/s12889-018-5837-3
45. Yang P, Lo W, He ZL, Xiao XM. Medical nutrition treatment of women with gestational diabetes mellitus by a telemedicine system based on smartphones. J Obstet Gynaecol Res. (2018) 44:1228–34. doi: 10.1111/jog.13669
46. Muzigaba M, Kolbe-Alexander TL, Wong F. The perceived role and influencers of physical activity among pregnant women from low socioeconomic status communities in South Africa. J Phys Act Health. (2014) 11:1276–83. doi: 10.1123/jpah.2012-0386
47. Ribeiro CP, Milanez H. Knowledge, attitude and practice of women in Campinas, São Paulo, Brazil concerning physical exercise in pregnancy: a descriptive study. Reprod Health. (2011) 8:1–7. doi: 10.1186/1742-4755-8-31
48. Abedzadeh M, Taebi M, Sadat Z, Saberi F. Knowledge and performance of pregnant women referring to Shabihkhani hospital on exercises during pregnancy and postpartum periods. J Jahrom Univ Med Sci. (2011) 8:212–8. doi: 10.29252/jmj.8.4.43
49. Watson ED, Brage S, White T, Westgate K, Norris SA, Van Poppel MN, et al. The influence of objectively measured physical activity during pregnancy on maternal and birth outcomes in urban black South African women. Matern Child Health J. (2018) 22:1190–9. doi: 10.1007/s10995-018-2504-3
50. Chen Y, Jin GZ. Does health insurance coverage lead to better health and educational outcomes? evidence from rural China. J Health Econ. (2012) 31:1–14. doi: 10.1016/j.jhealeco.2011.11.001
51. Sanda B, Vistad I, Haakstad LAH, Berntsen S, Sagedal LR, Lohne-Seiler H, et al. Reliability and concurrent validity of the International Physical Activity Questionnaire short form among pregnant women. BMC Sport Sci Med Rehabil. (2017) 9:1–10. doi: 10.1186/s13102-017-0070-4
Keywords: physical activity, barriers to physical activity, education, pregnancy, gestational age
Citation: Asante DO, Osei F, Abdul-Samed F and Nanevie VD (2022) Knowledge and participation in exercise and physical activity among pregnant women in Ho, Ghana. Front. Public Health 10:927191. doi: 10.3389/fpubh.2022.927191
Received: 24 April 2022; Accepted: 21 October 2022;
Published: 16 November 2022.
Edited by:
Estelle D. Watson, The University of Auckland, New ZealandReviewed by:
Daniel Goon, University of Fort Hare, South AfricaRita Santos-Rocha, Polytechnic Institute of Santarém, Portugal
Copyright © 2022 Asante, Osei, Abdul-Samed and Nanevie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Drusilla Obenewaa Asante, ZGFzYW50ZUB1aGFzLmVkdS5naA==
†These authors have contributed equally to this work and share last authorship
 Drusilla Obenewaa Asante
Drusilla Obenewaa Asante Francis Osei
Francis Osei Fridaus Abdul-Samed
Fridaus Abdul-Samed Victoria Dzifa Nanevie1†
Victoria Dzifa Nanevie1†