
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 09 September 2022
Sec. Health Economics
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.925616
This article is part of the Research Topic Healthcare Organization and Delivery Strategies, Models, and Cost Savings View all 6 articles
Aims: Crohn's disease (CD) is a global disease that is dramatically increasing. This study aimed to identify the primary drivers of hospitalization expenses for CD patients to provide guidance on the allocation and control of health care costs.
Methods: This study retrospectively collected the homepage data of the electronic medical records of CD patients in two tertiary hospitals in Zhejiang Province, China, from January 2016 to December 2021. The influencing factors of hospitalization expenses for CD were analyzed. A linear mixed model with least absolute shrinkage (LASSO-LMM) was used to develop a predictive model for hospitalization expenses for CD patients.
Results: A total of 4,437 CD patients were analyzed in this study. CD patients' age, length of hospital stay, admission route, comorbidities, and main treatment were found to be statistically significant variables for CD patients' hospitalization expenses. The AIC and BIC of LASSO-LMM model were 319.033 and 306.241, respectively. Patients who were older, had a longer hospital stay, and had comorbidities had higher hospitalization expenses. The hospitalization expenses of outpatients were lower than those of emergency patients. The weight of surgical treatment was the highest among three treatments (0.602).
Conclusions: Identifying and examining factors that influence hospitalization expenses for CD patients can help to control healthcare expenditures. Treatment mode was the most important impact on CD hospitalization expenses. Medical security departments can consider implement personalized and precise hospitalization expense compensation scheme base on LASSO-LMM prediction model in the future.
Crohn's disease (CD) is a chronic inflammatory disease with a relapse-remission process, showing a different disease spectrum (1). It is one of the most prevalent inflammatory bowel diseases (IBD).The etiology of CD is still unknown, but genetic, immune, and environmental factors increase the risk of onset and progression of the disease (2).CD is characterized by skipping intestinal injury anywhere in the gastrointestinal tract and involves chronic, recurrent wall inflammation, which can cause chronic abdominal pain, diarrhea, obstruction and / or perianal injury (2, 3).
In the past, CD was commonly seen in Western regions such as North America and Northern Europe, with the highest prevalence rates being in Europe (322 per 100 000), Canada (319 per 100 000) and the USA (214 per 100 000) (2). The incidence of CD has risen globally since the beginning of the 21st century, as rapidly reported in emerging industrialized countries in Asia, Africa, and South America (4). In China, a retrospective analysis showed that the incidence of CD is on the rise. It is estimated that the prevalence of CD in China has reached 1.4 per 100,000 person-years (5), which is the highest in Asia (6).
The increasing number of CD patients has caused a corresponding increase in CD treatment costs. It is well established that CD's economic burden is unbalanced due to the heterogeneity of disease processes and complications. A systematic review estimated that the pooled mean hospitalization cost per patient per year for CD patients was €2004.83. The main contributors toward total CD health expenditure were biologics (€5554.58) and medications (€3096.53), followed by hospitalization (€2004.83) and surgery (€1883.67) (7). In China, the economic burden of CD was 54,246 Yuan, which exceeds the cost of other chronic diseases such as diabetes (8). A web-based study on the financial burden and medical service availability of IBD patients in China showed that Chinese IBD patients had huge economic burdens and difficulties in acquiring health care, which enlarged their economic anxiety and inevitably affected the outcomes of their disease (9). Given the intermittent periods of hospitalizations, surgery, and pharmacotherapy, CD patients go through the management of flare-ups and disease complications during their lifetime, CD accounts for a substantial amount of costs to health care systems and society in general (10, 11).
The traditional models for screening the influencing factors of hospitalization expenses include multiple linear regression model (12, 13), partial least square structural equation model (14), data mining method (15, 16) and others. As hospitalization expenses are affected by patients' own characteristics and treatment methods, they often present a multi-level distribution. The linear mixed model (LMM), also known as a multi-level model, contains both fixed effects and random effects. It can not only deal with the relationship between different levels of factors, but also explore the impact of various levels of influencing factors on hospitalization expenses. However, there are many factors affecting the hospitalization expenses of CD patients, and certainly not all of these factors play a key role in hospitalization expenses, and some factors may even interfere with the changes of hospitalization expenses. Recently, with the development of big data, a method of factor selection through coefficient compression has attracted increasing attention from scholars. A past study (15) used a Random Forest (RF) model and Least Absolute Shrinkage and Selection Operator (LASSO) Regression to predict the medical expenses of chronic renal failure patients. Another study (17) explored four machine learning models, including ordinary least squares linear regression, regularized regression, gradient booster, and recurrent neural network, to predict health care expenditures. However, the research on the prediction and influencing factors of the hospitalization expenses in CD patients has, to the current authors' knowledge, not been reported.
The hospitalization expense has become a direct financial burden for patients, it also concerned by medical insurance departments. The China Medical Insurance Administration is currently implementing a new medical reform policy, and has introduced medical insurance payment methods for disease diagnosis-related groups (DRG) and diagnostic intervention packages (DIP) to address the burden of medical expenses (15). These payment methods have comprehensively considered China's medical insurance policies, innovatively integrated the characteristics of various diseases, which puts forward higher requirements for medical insurance payment standards. Therefore, the linear mixed model with least absolute shrinkage (LASSO-LMM) presents a new prospective for rational allocation and control of hospitalization expenditure, particularly in the era of big data.
This study selected CD inpatients from two tertiary hospitals in Zhejiang Province as the research participant. Our study intends to use the method of LASSO-LMM to predict individuals' hospitalization expenses and assess associated factors according to data from the homepage of CD patients' hospital records. This is so we can realistically evaluate the influencing factors of hospitalization expenses and provide a reference point for future health policies and medical expense reimbursement systems related to CD patients in China.
This study retrospectively collected the homepage data of the electronic medical records of CD patients in two tertiary hospitals in Zhejiang Province from January 2016 to December 2021. The data was used to identify patients with CD through the International Diagnosis Classification Code, 10th Revision (ICD-10). The first three code K50 in ICD-10 represents the classification of CD. In this study, a total of 20,795 hospitalized medical records were retrieved with K50 as the main diagnostic code. Guided by the relevant reports (15, 18, 19), the data set used in our research included patient details such as age, sex, marital status, medical payment method, admission route, length of hospital stay, comorbidities, major procedures, main treatment, rehospitalization plan within 31 days of discharge, and discharge method. The target variable was total hospitalization expenses. All expenditure variables were converted to 2016 Chinese Yuan (¥) using the Consumer Price Index.
To protect patients' privacy, their identities were concealed, and only medical record numbers were used. This study was conformed with the “Ethics review methods for biomedical research involving humans” promulgated by the Ministry of Health of The People's Republic of China and was performed according to the principles of the Helsinki Declaration.
In order to ensure the reliability of the results, according to the purpose of this study, we excluded cases where patients left the hospital on the first day, there was missing data, variables with small sample sizes (n < 10), and hospitalization expenses outliers.
To eliminate the influence of the unit difference between different variables affecting hospitalization expenses, the normal transformation function was used to standardize continuous variables. Where μ and σ were the mean and standard deviation of the variable, respectively. The data value > μ+3σ or < μ−3σ were considered outliers and removed.
Since age, length of stay, number of comorbidities, and hospitalization expenses were continuous variables, by calculating skewness and kurtosis, none of these variables followed a distribution distribution. Thus, these continuous variables were grouped, statistically described as counts and proportions, and the median and quartile of the total medical expenses were calculated for each group.
Continuous variables with normal distribution were expressed as mean ± standard deviation (SD). Continuous variables with non-normal distribution or ordinal variables were expressed as median (the lower four quantile, the upper four quantile). Categorized variables were summarized as counts and proportions. Mann-Whitney U test or Kruskal-Wallis H test was used to compare hospital expenses for each group. Then, linear mixed-effects model with LASSO (LASSO-LMM) was used to further explore the influencing factors of CD hospitalization expenses.
Least Absolute Shrinkage and Selection Operator (LASSO) is a factor screening method, which compresses variable coefficients by constructing penalty functions to solve the problem of over-fitting regression models. The basic idea of the algorithm is to minimize the sum of absolute values of regression coefficients under the constraint of a constant, and to minimize the sum of squares of residuals, so that some regression coefficients are strictly contracted to zero.
In the formula, the penalty term is the absolute value of the factor coefficient of hospitalization expenses, and the penalty parameter is used to control the shrinkage of the regression coefficient of the linear mixed model. When λ is large enough, it will compress the regression coefficient and make it tend to 0, so as to achieve the purpose of screening the key influencing factors of hospitalization expenses.
Linear mixed–effects model, as an important statistical model widely used in economic, medical, financial and other fields, includes fixed effects and random effects. Suppose there are n subjects with Gaussian response{yi:i = 1, 2, …, n}, some important covariates Xi = (x1, x2, …, xq) are considered for the fixed effects. Denote Zi = (z1, z2, …, zq) as a set of random effect covariates that represent individual departure from the fixed effect. The basic mixed effects model is:
Where Xi and Zi are ni× p and ni× q matrices, respectively; and yi, β, bi and eiare ni× 1, p× 1, q× 1and ni× 1vectors. In the above model, β represents the fixed effects, bi represents the random effects and ei represents observation errors.
The above linear mixed effects model has been deeply studied in some literature (20, 21).
The Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) were used to evaluate the fitting effect of LASSO-LMM model. The smaller their values, the better the model.
The above statistical analyses were performed with the IBM SPSS statistics software (IBM SPSS Statistics for Windows, Version 25.0. Armonk, New York) and R version 4.1.1. All statistics were two-sided and considered significant if the P-value was <0.05.
We ultimately identified 4,437 hospitalized patients with CD according to inclusion and exclusion criteria (Figure 1). Of the hospitalized patients, 3,001 were male (67.6%); the median (IQR) age was 34 years old (24~42), and 40.5% of patients were 19 to 30 years old. Nearly half of the patients (45.1%) were married. The majority of hospital admissions were from outpatients (95.0%), with an average length of stay of 10.89 days. There were 3,544 patients with comorbidities or complications (79.9%). A large number of patients underwent surgical or procedural treatment (71.4%). Most patients had no readmission plan within the 31 days after they were discharged (84.4%). The average hospitalization expense was 14,654 Yuan.
Table 1 displays hospitalization expenses of patients with CD under different clinical characteristics. The Mann-Whitney U-test and Kruskal-Wallis H-test were performed.
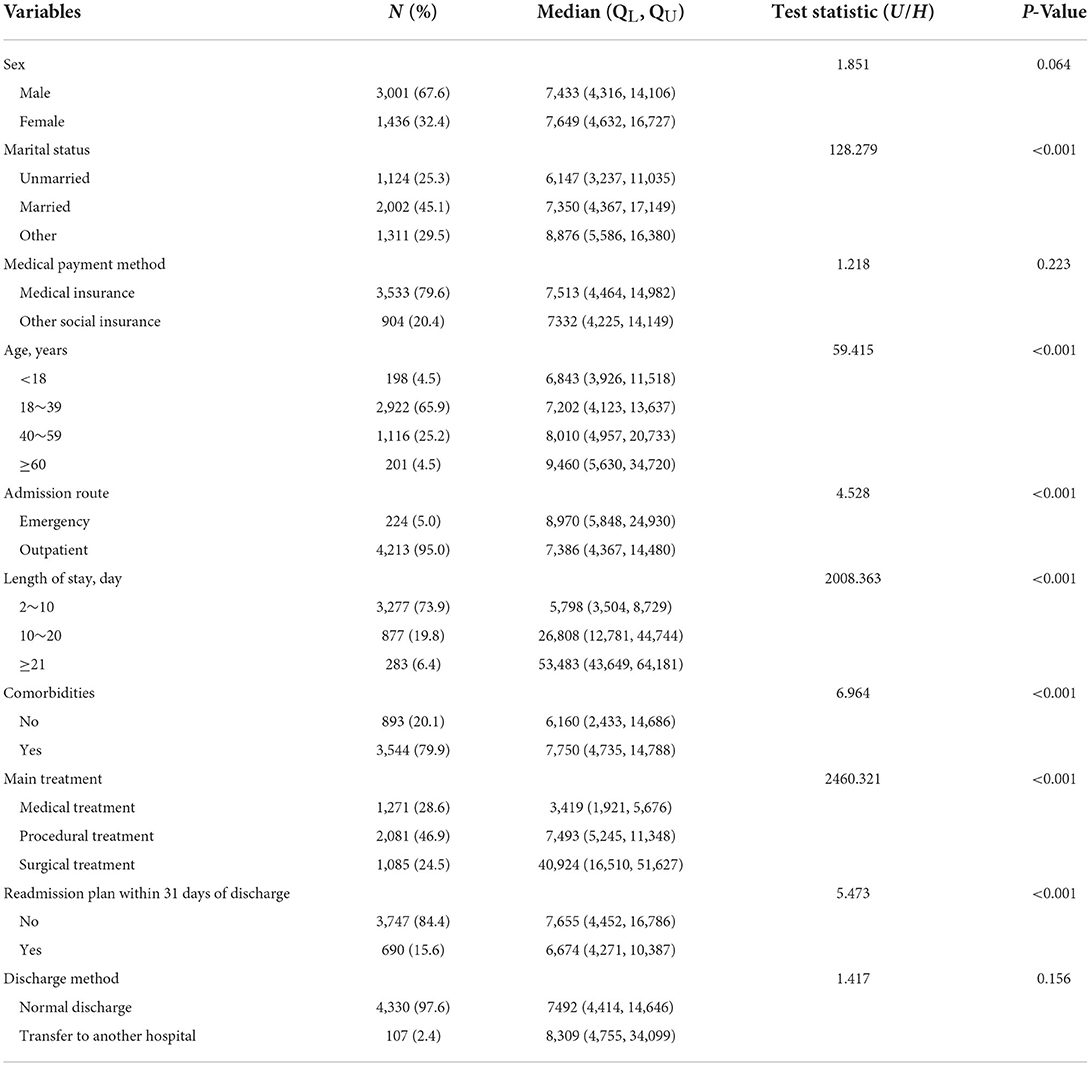
Table 1. Baseline characteristics and difference in hospitalization expenses of Crohn's disease (N = 4,437).
The pairwise comparison results for further post-hoc tests were presented in Table 2.
The Bonferroni-adjusted alpha level was used to determine whether there were significant differences between variables with a significant influence on hospitalization expenses.
The results showed that there was no significant difference in hospitalization expenses in terms of sex (P = 0.064), medical payment method (P = 0.223) and discharge method (P = 0.156). However, the hospitalization expenses of CD patients significantly influenced by marital status, age, admission route, length of stay, comorbidites, main treatment methods and readmission plan within 31 days of discharge (P < 0.05). The hospitalization expenses of patients were positively correlated with age and length of stay. The expenses of patients over 60 years old were the highest (median: 9,460 Yuan, IQR: 5,630–34,720 Yuan). The expenses of those who stayed for more than 20 days (median: 53,483 Yuan, IQR: 43,649–64,181 Yuan) were twice as high as those of patients who stayed <20 days. The hospitalization expenses of patients who were admitted to the emergency department (median: 8,970 Yuan, IQR: 5,848–24,930 Yuan), with comorbidities (median: 7,750 Yuan, IQR: 4,735–14,788 Yuan), and without a 31-day readmission plan (median: 7,655 Yuan, IQR: 4,452–16,786 Yuan) were higher than those of other conditions. The hospitalization expenses of surgical treatment was the highest (median: 40,924 Yuan, IQR: 16,510–51,627 Yuan), followed by procedural treatment (median: 7,493 Yuan, IQR: 5,245–11,348 Yuan). Medical treatment had the lowest expenses (median: 3,419 Yuan, IQR: 1,921–5,676 Yuan).
The optimal penalty parameter λ of the LASSO-LMM was determined by the 10-fold cross-validation method, and the values of lambda.min and lambda.1se were 0.001467 and 0.015013, respectively. We chose the lammda.1se as the optimal parameter of the model, and the six variables including age, length of hospital stay, marital status, admission route, comorbidities, and treatment methods were used as the influencing factors of CD hospitalization costs. The regression coefficients of all the other factors were 0. The changes in λ and the coefficients are presented in Figures 2, 3.
We fitted the LASSO-LMM model with marital status and year as random effects and the remaining five variables as fixed effects. The AIC and BIC of LASSO-LMM model were 319.033 and 306.241, respectively. As shown in Table 3, mode of treatment was the most important factor affecting hospitalization expenses. Compared with medical treatment, the coefficients of surgical treatment and procedural treatment on hospitalization expenses were 0.602 and 0.279, respectively. Patients who were older, had longer hospitalization days, and had comorbidities had higher hospitalization expenses, with coefficients of 0.002, 0.033, and 0.058, respectively. The hospitalization expenses of outpatients were lower than those of emergency patients.
The prevalence of CD has been increasing worldwide. CD is a chronic and potentially disabling disease, commonly results in hospitalization, decreased quality of life and inability to work. It inevitably generates an increasing economic burden on health care systems, as CD is incurable and generally requires lifelong care and medication. Thus, it is imperative to explore the direct economic burden of CD to recognize its economic impact on health care systems and patients. Further, it is important to make decisions on health resource allocation to combat CD's economic impact. Our study provided a detailed description of the influencing factors of hospitalization expenses for CD patients in China. Linear mixed-effects models with a LASSO method were used to identify the key influencing factors associated with CD hospitalization expenses. We found that the hospitalization expenses of CD patients were related to the six factors, that are, age, length of hospital stay, marital status, admission route, comorbidities, and treatment methods.
Over the past 20 years due to the widespread availability of biological therapy, surgery rates for CD have declined. Nevertheless, approximately 30–40% of patients with CD still inevitably require surgery at some point in their lifetime (22). During patients' course of CD, their inflammatory activity periods alternate with remission periods. Whether biological treatment can modify the course of the disease and surgical rate of CD patients remains unproven. A registry study from Canada in 2019 showed that the introduction of biological therapy had not yielded the expected reductions in the rates of CD-associated hospitalizations and/or intestinal resections (23). Drug therapy and surgical procedures should be considered as equally viable treatment strategies (24).
CD leads to a considerable burden on health care systems due to its medical and surgical treatment. Our study showed that the hospitalization expenses of CD patients were closely related to the chosen treatment method, for which the expenses of surgical treatment was the highest, followed by procedural treatments. Based on the natural course of CD, the possibility of surgery increases over time. Hence, surgical or procedural therapy is still required for a proportion of patients with refractory or associated complications. As a result, the additional surgical and procedural treatments lead to increased hospitalization expenses. A prospective community-based study found that the total expenditure of surgery and procedures accounted for 31% of total expenditure (25). It showed that while the amount of surgery-related health care costs for the treatment of CD has declined, surgery costs remain an important factor in the cost of hospitalization for patients.
Our study shows that comorbidities were another important factor affecting the expenses of CD hospitalization. The presence of comorbidities in IBD patients had been proven to adversely affect their health-related quality of life, prolong their hospital stay and increase the risk of postoperative complications (26). Possibly due to common pathogenic pathways with other immune-mediated inflammatory diseases, CD has been associated with multiple chronic comorbidities such as bone diseases, cardiovascular diseases, iron-deficiency anemia, pain, psychological disorders and respiratory illness. It was found that persons with IBD have a more comorbidities burden than persons without IBD (27). A population-based registry study in Denmark also emphasized that some immune-mediated diseases (IMDs) and CD may have overlapping pathogenic pathways and that IMDs are usually more common in CD patients (28). The impact of CD comorbidities on medical practice and medical costs clearly cannot be ignored. Related diseases can alter or confuse the clinical manifestations and activity of CD, possibly affecting the disease's prognosis. Moreover, drug therapy, which has lower expenses than surgical procedural treatment, may be limited in CD patients with comorbidities. Building multidisciplinary teams to empower patient care is especially important for these patients (29). This means that they have more complex medical activities and increased care costs compared to other patients without comorbidities. A cross-sectional study conducted in Switzerland showed that compared with the non-IBD population, common comorbidities for IBD patients can more than double total costs (30). Our findings also suggest that the high medical costs caused by the comorbidities of CD patients deserve further investigation.
Admission through the emergency department and prolongation of hospital stay were independent predictors of higher hospitalization expenses for CD patients. Despite the current therapeutic arsenal for the treatment of CD, some patients with CD complications (6–16%) show acute complications and require emergency treatment (31). Acute complications that may occur in patients with CD include acute severe colitis, toxic megacolon, uncontrolled bleeding, perforation, abscess, intestinal obstruction and others. When patients are admitted through the emergency department, more urgent laboratory tests, imaging tests, and colonoscopies are required to assess their condition. In life-threatening situations, abscess drainage, colectomy, or total parenteral nutrition may be considered, which would result in additional resource consumption and increased healthcare costs.
The results of this study indicate that the hospitalization expenses of CD patients are positively correlated with age (rs= 0.127, P < 0.001) and length of hospital stay (rs= 0.804, P < 0.001). Patient age was weakly associated with hospitalization expenses. The pairwise comparison results of the age groups in Table 2 suggest that there was no significant difference in the hospitalization expenses of CD patients under 40 years old, while there existed differences in age groups above this age. The epidemiology, clinical characteristics, phenotype, disease course, cancer risks, therapeutic and monitoring strategy of CD patients are vary significantly by age of onset. This may lead to heterogeneity among CD hospitalization costs, highlighting the need for further research on hospitalization costs in CD patients of different ages. Length of hospital stay was strongly associated with hospitalization expenses. For CD patients, longer hospital stays often reflect disease severity or a lack of response to medication. The presence of IBD-specific complications involving malnutrition, the need for total parenteral nutrition, non-elective operation, clostridium difficile infection, venous thromboembolism, and hospital-acquired infections have all been shown to result in prolonged hospital stays (32). All of these situations require more nursing and medical support, which results in greater medical costs. Consequently shortening the length of hospital stay was considered to be one of the key strategies to mitigate healthcare financial stress and improve patient outcomes (33).
In our study, sex, discharge method, and medical payment method had no significant effect on the hospitalization expenses of CD patients. The Chinese government has achieved full coverage on the basic medical insurance for citizens, including the rural new cooperative medical scheme, urban resident-based basic medical insurance scheme and urban employee-based basic medical insurance scheme (34). Some biological agents used in the treatment of CD, such as infliximab, have been admitted into the reimbursement list of basic medical insurance in China. Therefore, medical payment method was not a factor affecting CD hospitalization expenses. While the results of the univariate analysis in Table 1 show that hospitalization expenses without readmission plans within 31 days after discharge are higher than those with planned readmissions, the multivariate analysis of the LASSO-LMM model in Table 3 indicates that the 31-day readmission plan factor has no significant effect on the hospitalization expenses of CD patients after controlling for other factors. In general, CD flare-ups, infections, or complications from unplanned operations during hospitalization are the most common reasons for readmissions (35). Hospital readmissions are costly to the national healthcare system. Especially, in the context of the implementation of DRG payment in China, reducing the unplanned readmission rate has become an important aspect of increasing the quality of healthcare services and decreasing the cost of medical services for patients with chronic diseases like CD.
This study has several limitations. First, we only described the medical expenses of two hospitals, and we were unable to assess health care received outside of our centers, so medical expense may be potentially underestimated. Second, our study only included data from the homepage of the medical records. The data have limited independent variables. Future research needs to incorporate more variables to establish better predictive models and to elucidate the impact of hospitalization expenses in CD patients. Lastly, our sample data were obtained from only two tertiary first-class hospitals. A larger sample size including patients from multiple different hospitals would further enhance the precision of estimates generated.
Our study identified multiple factors that influence hospitalization expenses for CD patients. The degree of each influencing factor was different, with treatment mode being the most important impact on CD hospitalization expenses. Identifying and examining such factors can help to control healthcare expenditures. In the context of the current trial of DRG payment in China, our model can propose effective strategies for medical security departments to consider implementing personalized and precise hospitalization expense compensation scheme in the future. With all the above noted, reducing and/or controlling the hospitalization expenses of CD patients is bound to be a complex process that requires collaborative efforts. These urgently need to be addressed by medical security departments, hospital and patients themselves. It will be beneficial to reduce the economic burden of patients and the pressure of medical insurance fund through the medical security department formulating reasonable compensation programs, medical institutions providing optimal therapeutic regimens, and patients accepting treatment and nursing.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University school of Medicine and the Ethics Committee of the First Affiliated Hospital of Zhejiang Chinese Medical University. The Ethics Committee waived the requirement of written informed consent for participation.
Conceptualization and funding acquisition: LW and ZL. Data curation: PZ. Methodology: LW and LL. Project administration and writing—review and editing: ZL. Software: LL. Writing—original draft: LW. All authors have read and approved the final manuscript.
This research was funded by Zhejiang Provincial Natural Science Foundation of China (No. LQ20G030015), Health Commission of Zhejiang Province (No. 2020KY201), and Zhejiang Pharmaceutical Association (No. 2022ZYJ14).
The authors sincerely thank Dr. Qiuhua Zhang, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, for her help in the retrieval strategy of this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. (2007) 369:1627–40. doi: 10.1016/S0140-6736(07)60750-8
2. Torres J, Mehandru S, Colombel J-F, Peyrin-Biroulet L. Crohn's disease. Lancet. (2017) 389:1741–55. doi: 10.1016/S0140-6736(16)31711-1
3. Roda G, Chien Ng S, Kotze PG, Argollo M, Panaccione R, Spinelli A, et al. Crohn's disease. Nat Rev Dis Primers. (2020) 6:22. doi: 10.1038/s41572-020-0156-2
4. Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. (2017) 390:2769–78. doi: 10.1016/S0140-6736(17)32448-0
5. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. (2017) 152:313–21. doi: 10.1053/j.gastro.2016.10.020
6. Ng SC, Kaplan GG, Tang W, Banerjee R, Adigopula B, Underwood FE, et al. Population density and risk of inflammatory bowel disease: a prospective population-based study in 13 countries or regions in asia-pacific. Am J Gastroenterol. (2019) 114:107–15. doi: 10.1038/s41395-018-0233-2
7. Santiago M, Dias CC, Alves C, Ministro P, Goncalves R, Carvalho D, et al. The magnitude of crohn's disease direct costs in health care systems (from different perspectives): A systematic review. Inflamm Bowel Dis. (2022). doi: 10.1093/ibd/izab334. [Epub ahead of print].
8. Zhou WP, Mu N, Jian WY, Wang HH. Economic burden and factors associated with Crohn's disease. Beijing Da Xue Xue Bao Yi Xue Ban. (2021) 53:555–9. doi: 10.19723/j.issn.1671-167X.2021.03.019
9. Yu Q, Zhu C, Feng S, Xu L, Hu S, Chen H, et al. Economic burden and health care access for patients with inflammatory bowel diseases in china: web-based survey study. J Med Int Res. (2021) 23:e20629. doi: 10.2196/20629
10. Boschetti G, Nancey S, Daniel F, Pariente B, Lerebours E, Duclos B, et al. Costs of crohn's disease according to severity states in france: a prospective observational study and statistical modeling over 10 years. Inflamm Bowel Dis. (2016) 22:2924–32. doi: 10.1097/MIB.0000000000000967
11. Lichtenstein GR, Shahabi A, Seabury SA, Lakdawalla DN, Espinosa OD, Green S, et al. Lifetime economic burden of crohn's disease and ulcerative colitis by age at diagnosis. Clin Gastroenterol Hepatol. (2020) 18:889. doi: 10.1016/j.cgh.2019.07.022
12. Li JM, Luo WL. Hospitalization expenses of acute ischemic stroke patients with atrial fibrillation relative to those with normal sinus rhythm. J Med Econ. (2017) 20:114–20. doi: 10.1080/13696998.2016.1229322
13. Ruan F, Ding X, Li H, Wang Y, Ye K, Kan H. Back propagation neural network model for medical expenses in patients with breast cancer. Math Biosci Eng. (2021) 18:3690–8. doi: 10.3934/mbe.2021185
14. Pineda-Rico U, Stevens-Navarro E. Hybrid fast least-squares solution-seeker algorithm with partial channel-knowledge for precoding in MIMO systems. IEICE T Commun. (2013) E96b:569–76. doi: 10.1587/transcom.E96.B.569
15. Dai P, Chang W, Xin Z, Cheng H, Ouyang W, Luo A. Retrospective study on the influencing factors and prediction of hospitalization expenses for chronic renal failure in china based on random forest and LASSO regression. Front Public Health. (2021) 9:678276. doi: 10.3389/fpubh.2021.678276
16. Yu TZ, He Z, Zhou QH, Ma J, Wei LH. Analysis of the factors influencing lung cancer hospitalization expenses using data mining. Thoracic Cancer. (2015) 6:338–45. doi: 10.1111/1759-7714.12147
17. Yang C, Delcher C, Shenkman E, Ranka S. Machine learning approaches for predicting high cost high need patient expenditures in health care. Biomed Eng. (2018) 17:131. doi: 10.1186/s12938-018-0568-3
18. Luo AJ, Chang WF, Xin ZR, Ling H, Li JJ Dai PP, et al. Diagnosis related group grouping study of senile cataract patients based on E-CHAID algorithm. Int J Ophthalmol. (2018) 11:308–13. doi: 10.18240/ijo.2018.02.21
19. Meng Z, Zhu M, Cai Y, Cao X, Wu H. Effect of a typical systemic hospital reform on inpatient expenditure for rural population: the Sanming model in China. BMC Health Serv Res. (2019) 19:231. doi: 10.1186/s12913-019-4048-7
20. Lai Y, Albert PS. Identifying multiple change points in a linear mixed effects model. Stat Med. (2014) 33:1015–28. doi: 10.1002/sim.5996
21. Wang Y, Chen H. On testing an unspecified function through a linear mixed effects model with multiple variance components. Biometrics. (2012) 68:1113–25. doi: 10.1111/j.1541-0420.2012.01790.x
22. Ferrari L, Krane MK, Fichera A. Inflammatory bowel disease surgery in the biologic era. World J Gastrointest Surg. (2016) 8:363–70. doi: 10.4240/wjgs.v8.i5.363
23. Murthy SK, Begum J, Benchimol EI, Bernstein CN, Kaplan GG, McCurdy JD, et al. Introduction of anti-TNF therapy has not yielded expected declines in hospitalisation and intestinal resection rates in inflammatory bowel diseases: a population-based interrupted time series study. Gut. (2020) 69:274–82. doi: 10.1136/gutjnl-2019-318440
24. Stoss C, Berlet M, Reischl S, Nitsche U, Weber MC, Friess H, et al. Crohn's disease: a population-based study of surgery in the age of biological therapy. Int J Colorectal Dis. (2021) 36:2419–26. doi: 10.1007/s00384-021-03930-w
25. Burisch J, Vardi H, Schwartz D, Friger M, Kiudelis G, Kupcinskas J, et al. Health-care costs of inflammatory bowel disease in a pan-European, community-based, inception cohort during 5 years of follow-up: a population-based study. Lancet Gastroenterol Hepatol. (2020) 5:454–64. doi: 10.1016/S2468-1253(20)30012-1
26. Marin-Jimenez I, Bastida G, Forés A, Garcia-Planella E, Argüelles-Arias F, Sarasa P, et al. Impact of comorbidities on anti-TNFα response and relapse in patients with inflammatory bowel disease: the VERNE study. BMJ Open Gastroenterol. (2020) 7:e000351. doi: 10.1136/bmjgast-2019-000351
27. Bernstein CN, Nugent Z, Shaffer S, Singh H, Marrie RA. Comorbidity before and after a diagnosis of inflammatory bowel disease. Aliment Pharmacol Ther. (2021) 54:637–51. doi: 10.1111/apt.16444
28. Halling ML, Kjeldsen J, Knudsen T, Nielsen J, Hansen LK. Patients with inflammatory bowel disease have increased risk of autoimmune and inflammatory diseases. World J Gastroenterol. (2017) 23:6137–46. doi: 10.3748/wjg.v23.i33.6137
29. Roman AL, Munoz F. Comorbidity in inflammatory bowel disease. World J Gastroenterol. (2011) 17:2723–33. doi: 10.3748/wjg.v17.i22.2723
30. Bähler C, Schoepfer AM, Vavricka SR, Brüngger B, Reich O. Chronic comorbidities associated with inflammatory bowel disease: prevalence and impact on healthcare costs in Switzerland. Eur J Gastroenterol Hepatol. (2017) 29:916–25. doi: 10.1097/MEG.0000000000000891
31. De Simone B, Davies J, Chouillard E, Di Saverio S, Hoentjen F, Tarasconi A, et al. WSES-AAST guidelines: management of inflammatory bowel disease in the emergency setting. World J Emerg Surg. (2021) 16:23. doi: 10.1186/s13017-021-00362-3
32. Kelso M, Weideman RA, Cipher DJ, Feagins LA. Factors associated with length of stay in veterans with inflammatory bowel disease hospitalized for an acute flare. Inflamm Bowel Dis. (2017) 24:5–11. doi: 10.1093/ibd/izx020
33. Lim J. Big data-driven determinants of length of stay for patients with hip fracture. Int J Environ Res Public Health. (2020) 17:4949. doi: 10.3390/ijerph17144949
34. Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. (2015) 386:1484–92. doi: 10.1016/S0140-6736(15)00342-6
Keywords: Crohn's disease, LASSO, linear mixed model, hospital expenses, influencing factors
Citation: Wu L, Lv Z, Lai L and Zhou P (2022) Assessment of influencing factors of hospitalization expenses for Crohn's disease patients: Based on LASSO and linear mixed model. Front. Public Health 10:925616. doi: 10.3389/fpubh.2022.925616
Received: 21 April 2022; Accepted: 23 August 2022;
Published: 09 September 2022.
Edited by:
Adriana Castelli, University of York, United KingdomReviewed by:
Rahim Alhamzawi, University of Al-Qadisiyah, IraqCopyright © 2022 Wu, Lv, Lai and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhijie Lv, bG9ycnkzNzRAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.