
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 August 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.924741
This article is part of the Research Topic Behavioural Patterns and Mental Health in Early Life View all 4 articles
Background: This current study set out to investigate the status of sleep health in 7–20-year-old students in Fuzhou and explore the related influencing factors of sleep health.
Methods: A total of 38,467 children and adolescents in Fuzhou were included in the study through a random stratified cluster sampling. Data were collected from May to June 2019, in 18 primary schools and 18 middle schools from nine districts, Fuzhou. Children's parents and adolescents of sampled classes were invited to fill out a series of questionnaires about the performance of the last 6 months (sociodemographic characteristics, sleep-related lifestyle behaviors, and electronic-products usage). Multiple linear regression was carried out to analyze data.
Results: Of the total 40,888 questionnaires we released, 38,467 were valid and effective with the response rate was 94.08%. The age of the surveyed participants was 11.85 ± 3.1, including 20,013 boys and 18,454 girls. The multiple linear regression analysis identified factors associated with sleep health (p < 0.05): Boy (coef = 0.073, 95% CI: 0.030–0.115), age (coef = 1.797, 95% CI: 0.224–0.243), key school (coef = 2.069, 95% CI: 0.105–0.193), urban (coef = 0.096, 95% CI: 0.054–0.139), excessive daytime sleepiness (coef = 0.535, 95% CI: 0.432–0.639), unhealthy sleep habits (coef = 0.363, 95% CI: 0.307–0.419), eating before sleep (coef = 0.578, 95% CI: 0.527–0.630), using electronic products in bedroom (coef = 0.074, 95% CI: 0.028–0.121), screen time per day during school (coef = 0.260, 95% CI: 0.235–0.284), frequency of using electronics 30 min before bedtime (coef = 0.150, 95% CI: 0.134–0.166), strained relationship with parents (coef = 0.361, 95% CI: 0.270–0.452), strained relationship with peers (coef = 0.267, 95% CI: 0.171–0.363), excessive homework or learning (coef = 0.189, 95% CI: 0.141–0.237), time for doing homework (coef = 0.266, 95% CI: 0.245–0.287), and mood swings frequently (coef = 1.174, 95% CI: 1.127–1.221) negatively impact sleep health. Sleep alone (coef = −0.204, 95% CI: −0.262–0.147) were the risk factors for sleep health. Furthermore, frequent mood swings was considered the most influential factor on overall variables.
Conclusions: Sleep health is associated with factors covered sociodemographic characteristics, family sleep habits, and routine activities before bedtime. Multiple measures should be taken to improve sleep quality in a targeted manner.
Sleep health is a notable concern during school age and adolescence, with the majority of them reporting poor sleep patterns, including insufficient and inferior quality sleep. Sleep problems are estimated to affect 30–70% of adolescents in Europe and North America and 14 to 68% of students sleeping less than recommended on school days (1, 2). Just half (50.19%) of the children slept for >8 h per day and only one-third of children (35.37%) reported good sleep quality in China (3). Compared with other age groups, healthy sleep is challenged by unique features for elementary and junior high school students: extrinsic factors such as social activities and academic demands (with early school start times) interact with autonomy regarding their sleep schedules that cause irregular sleep patterns (1). Previous research has shown that poor sleep in children and adolescents is associated with a variety of problematic outcomes including reduced life satisfaction (4), increased feelings of anxiety and depression (5), increased diagnosis of diseases [attention-deficit/ hyperactivity disorder (6), obesity (7), and diabetes (8), and increased risk for suicide (9)], underscoring the need to include healthy sleep into students health promotion efforts.
Given the high prevalence of sleep deficiency in children and adolescents, the negative impact on a range of outcomes, and the particular sleep characteristics such as sleep duration, sleep disturbance, and sleep quality, it is important to assess factors influencing sleep health in this age group for improving their sleep quality. Sleep health is multifaceted, and requires adequate duration, high quality, and without disturbance such as difficulty falling and staying asleep (10). However, only a few studies have been conducted on the sleep health of primary and middle school students, and even most of these studies focused on sleep duration with little attention to sleep quality. Besides, comparable data about sleep deficiency in children and adolescents from China is limited and related research in Fujian Province is scarce based on reference literature. Hence, this study will therefore provide such estimates.
In this study, data on sleep collected in school-based surveys of primary and middle school students in Fuzhou, Fujian Province, China, were enrolled to describe the sleep patterns in children and adolescents and to assess the factors influencing sleep health (involving sleep quality, sleep duration, and sleep disturbance). This is a rare large-scale study on the sleep health of primary and middle school students in China, which fills the gap in relevant studies in Fujian Province and provides a theoretical basis for formulating measures to improve the sleep of children and adolescents.
A cross-sectional, randomized, stratified, multistage cluster sampling methodology was conducted to select 36 schools in Fuzhou, a city divided into 13 districts classified as three regions including five urban Districts, six rural districts, and two county-level cities.
Based on the statistical formula:
(where n, p, and δ are sample size, positive rate, and acceptable error, respectively), supposing sleep disorder prevalence = 4.43% in children (11), significance at α = 0.05 with Zα/2 of 1.96, and acceptable error at 0.1 P the sample size was calculated as 8,288.
Allowing for non-response (deff = 2), the final intended sample size was set as 16,576. In stage 1, depending on account of regional economic development, five urban districts and four rural Districts were randomly selected from all 13 Districts (five urban Districts, six rural districts and two county-level city) in Fuzhou. In stage 2, two primary schools and two junior middle schools were randomly chosen from the selected Districts (Taijiang District, Mawei District, Canshan District, Fuqing District, Minhou District, Minqing District, Yongtai District, Gulou District, and Jinan District) (Figure 1). In stage 3, classes were selected by the principals in reasoned consideration of the class schedule. Participation was voluntary and anonymous. All students, besides Grade 6, 9, and 12 in chosen schools, were invited to participate in the survey. The students in the presence of a researcher and children's parents completed the self-administered questionnaire about their performance over the last 6 months in normal classroom settings. Data collection occurred from May to June 2019.

Figure 1. Districts selected in Fuzhou. List of schools: 18 primary schools and 18 middle schools were randomly chosen from 9 selected Districts. Specific list: Yanan Middle School, Yangqiao Middle School, No.2 Primary School, Huaqiao Primary School (Gulou); No.8 Middle School, No.15 Middle School, Shuanghong Primary School, No.5 primary school (Taijiang); No.40 Middle School, No.12 Middle School, Jianshan primary school, No.1 Middle School (Cangshan); Gushan High School, No.20 Middle School, Gucheng Primary School, Jincheng Primary School (Jinan); Langqi Middle School, No.2 High School, Rujiang Primary School, Experimental Primary School (Mawei); Fuqing No.2 Middle School, Yuanqiao Middle School, Shimen Primary School, Jinyin Primary School (Fuqing); Minhou No.6 Middle School, Shangjie Experimental Primary and Middle School, Shangjie Hongfei Primary School (Minhou); Chengguan Middle School, No.3 Middle School, Zhangcheng Primary School, Qingliang Primary School (Yongtai); Minqing Middle School, Chengguan Middle School, Minqing No.2 primary school, Minqing Experimental Primary School (Minqing).
The sleep quality assessment uses a sleep self-made questionnaire, which is divided into three dimensions: sleep duration, sleep disturbance, and subjective sleep quality (Supplementary Table 1). Sleep health is multi-faceted, including sleep duration, sleep disturbance, and subjective sleep quality.
Sleep duration involves four items (What time do you go to bed on weekdays and weekends? How many hours do you sleep on weekdays and weekends?); Sleep duration scores that vary within a range (4–16). Sleep disturbance includes six items (Do you have nightmares while sleeping? Is there any apnea or awakening while sleeping? Will you wake up more than 2 times a night? Is it difficult to fall asleep during waking up at night? Do you often feel that you can't move when you wake up? Do you feel physical pain during sleep?); The range of sleep disturbance scores varies from 2 to 12. Subjective sleep quality dose consists of three items (Did you have a good sleep? How long have you been sleepless? Do you feel a lack of sleep?); Subjective sleep quality score that varies within a range (1–7). The sum score of these three dimensions is the sleep health score (range: 7–35). The higher the score, the worse the sleep health became.
Reliability tests are tests aiming at improving the precision of a questionnaire. Cronbach's alpha coefficient (α) is used to evaluate the internal consistency. In our survey, Cronbach's α of the present study indicated good reliability of the scale (Cronbach's α = 0.716). Pearson correlation coefficients are used to assess the test-retest reliability. The correlation between overall sleep quality and three dimensions and the distinguishing validity of the scale. Construct validity is measured by Principal components analysis. After standardizing the scores of all items of each scale and establishing a correlation coefficient matrix, Principal components analysis is used to verify construct validity, extracting the common factor through the fourth-order maximum orthogonal rotation. See appendix for the details (Supplementary Tables 2, 3).
In addition, questionnaires dealt with demographic characteristics (sex, age, type of school, area), sleep-related lifestyle behaviors (excessive daytime sleepiness, unhealthy sleep habits, unhealthy eating habits, eating before sleep and sleep alone), electronic-products usage (using electronic products in bedroom, screen time per day during school, frequency of using electronics 30 min before bedtime), and emotional factors (mood swings frequently, a strained relationship with parents, strained relationship with peers) or heavy academic stress (excessive homework or learning, time for doing homework).
The definition of a key school is as follows: key schools, generally under the supervision of the municipal or provincial education authorities, are given priority treatment by various good policies. Key schools will have better educational equipment, quality of students, educational resources, and teaching staff. “unhealthy eating habits” were determined by the following questions: “Do you eat snacks?” (snacking); “Does your eating speed more quickly than other people?” (eating quickly); “Do you continue to eat only a limited variety of foods, rejecting certain types of foods—both familiar and unfamiliar” The answer options were “yes” or “no”. Those who answered yes to a question were defined as having that particular unhealthy eating habit. As this is a study of sleep, there is zeitgeber, so “Eating before sleep” is separated out: “Do you have night meals or snacks within two hours before bedtime?” “excessive homework or learning” is the estimated amount of homework assigned. “Time for doing homework” is the actual time spent on homework. “Strained relationship with parents, a strained relationship with peers” were self-reported by the students and children's parents: “Do you seek support from parents and peers for personal problems” or “Do parents or peers comfort, console, praise, and embrace or express their love through words and actions for you.”
Data collation and analysis were conducted using Epidata 3.0 and SPSS 19.0. Descriptive analysis was performed. Results for continuous variables with normal distributions were described by mean ± standard deviations (SD) and compared using a two-tailed Student's t-test or variance analysis. The continuous data were reported as correlation using Pearson's method. Results for discrete variables were displayed as a percentage (%) and distribution differences were examined by the chi square (χ2) test. We estimated the strength of the association between overall sleep quality score and predictors by regression coefficient (coef) and 95% confidence interval (CI). Two-sided p < 0.05 was considered to be statistically significant.
In total 40,888 questionnaires we released, and 38,467 completed questionnaires were collected. Thus, the valid response rate was 94.08%. The demographic and background characteristics of participants are shown in Table 1. The surveyed participants included 20,013 (52.0%) boys and 18,454 (48.0%) girls. Among all subjects in the sample in this study, almost two-thirds of the participants (62.0%) were from key schools. In terms of area, 47.3% lived in urban while 52.7% lived in rural. The mean age was 11.9 ± 3.1years, and the distribution of age was 53.0% for ≤ 12 years, 30.6% for 13–15 years, and 16.3% for ≥ 16 years.
Table 2 showed the results from the comparison of sleep scores by different characteristics. Students aged > 12 years had a higher sleep health score, sleep duration score, sleep disturbance score, and subjective sleep quality score than participants aged ≤ 12 years.
We investigated the relationship between behavioral and emotional factors and sleep quality by comparing the sleep health score, sleep duration score, sleep disturbance score, and subjective sleep quality score of children according to the presence or absence of behavioral and emotional problems (Table 3 and Figure 2). We found that behavioral factors such as excessive daytime sleepiness, unhealthy sleep habits, unhealthy eating habits, eating before sleep, electronic media use (using electronic products in the bedroom, screen time per day during school, frequency of using electronics 30 min before bedtime) and sleep alone have an unhealthy impact in sleep quality. In terms of emotional factors, participants who suffered from strained relations with parents/peers or heavy academic stress (excessive homework or learning, time for doing homework) had poor sleep quality. And moreover, the sleep health score was significantly higher in the presence of fluctuating emotions.
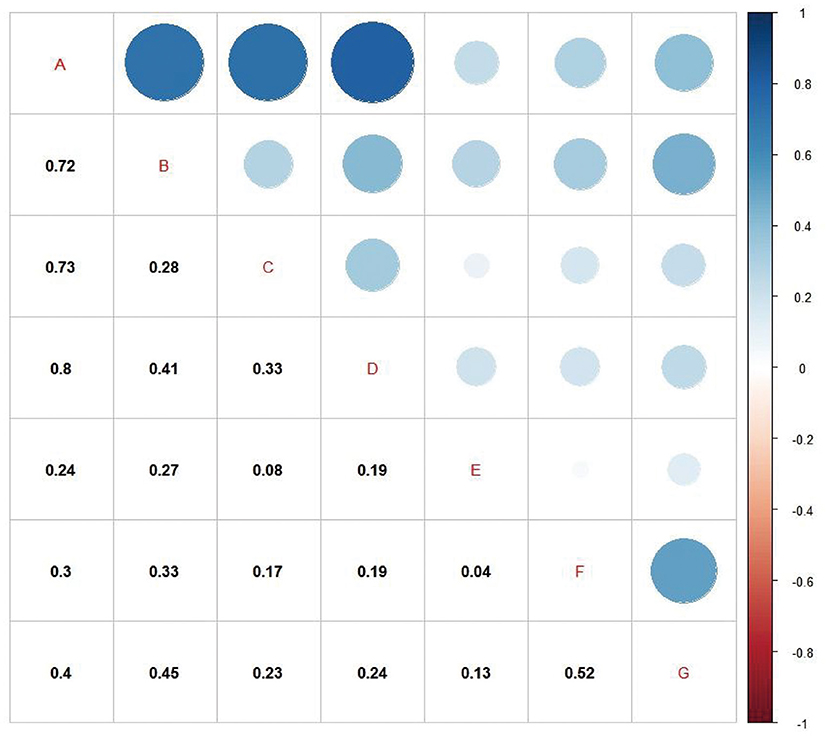
Figure 2. Correlation analysis of factors affecting sleep health. (A) Sleep health score; (B) Sleep duration score; (C) Sleep disturbance score; (D) Subjective sleep quality score; (E) Time for doing homework; (F) Screen time per day during school; (G) Frequency of using electronics 30 min before bedtime. All of p < 0.001. The color shades and size of the circle indicate the correlation coefficient (r) between any two factors.
Additionally, the correlation coefficient (r) between any two factors was statistically significant (p < 0.05). Sleep health score was positively correlated with sleep duration score (r = 0.72), sleep disturbance score (r = 0.73), and subjective sleep quality score (r = 0.8) (Figure 2).
Multiple linear regression was conducted to determine the influence of lifestyle and other factors on sleep health, sleep duration, sleep disturbance, and subjective sleep quality, using “Backward elimination.” We include the factors in the above test and demographic characteristics into the equation of multiple linear regression, which shows items such as demographic characteristics, lifestyle behaviors, and emotional factors that affected sleep health, sleep duration, sleep disturbance, and subjective sleep quality. The collinearity diagnosis found that the VIFs were all < 5, which can be preliminarily considered that the problem of collinearity between independent variables can be ignored.
Boy (coef = 0.073, 95% CI: 0.030–0.115), age (coef = 1.797, 95% CI: 0.224–0.243), key school (coef = 2.069, 95% CI: 0.105–0.193), urban (coef = 0.096, 95% CI: 0.054–0.139), excessive daytime sleepiness (coef = 0.535, 95% CI: 0.432–0.639), unhealthy sleep habits (coef = 0.363, 95% CI: 0.307–0.419), eating before sleep (coef = 0.578, 95% CI: 0.527–0.630), using electronic products in bedroom (coef = 0.074, 95% CI: 0.028–0.121), screen time per day during school (coef = 0.260, 95% CI: 0.235–0.284), frequency of using electronics 30 min before bedtime (coef = 0.150, 95% CI: 0.134–0.166), strained relationship with parents (coef = 0.361, 95% CI: 0.270–0.452), strained relationship with peers (coef = 0.267, 95% CI: 0.171–0.363), excessive homework or learning (coef = 0.189, 95% CI: 0.141–0.237), time for doing homework (coef = 0.266, 95% CI: 0.245–0.287) and mood swings frequently (coef = 1.174, 95% CI: 1.127–1.221) negatively impact sleep health. sleep alone (coef = −0.204, 95% CI: −0.262– −0.147) were the risk factors for sleep health. Furthermore, mood swings frequently was considered the most influential factor on overall variables (Table 4).
Healthy sleep is essential for children's and adolescents' physical and mental well-being. As we know, the investigation of sleep problems for children and adolescents is relatively limited in China up to now. In the present study conducted in a large sample of primary and middle school students in Fujian Province, China, we explore whether sleep health (sleep duration, sleep disturbance, subjective sleep quality) was associated with behavioral, social, and physical factors to provide some reference value for suggestions for their sleep health in the future.
We observed that factors like sex, age, types of school, and regional differences suggest the need for tailored sleep promotion recommendations for children and adolescents with different characteristics. Boys had higher sleep health scores and lower sleep quality than girls, which is in the line with that shown in the previous studies (12, 13). The older the age in our study, the higher the sleep score, where a higher score means worse sleep. Some biological factors such as reduced homeostatic sleep pressure and delayed circadian rhythms in conjunction, as well as early high school start times and psychological changes from childhood to adolescence, might account for the differences in sleep patterns among children and adolescents (14, 15). Elementary and junior high school students living in urban areas had more adverse sleep than those living in rural areas. Urban students have more night activities compared to rural students because of social and economic developmental disparities, which might result in reduced sleep duration for urban students and have a negative impact on sleep (16). The types of school differences in children and adolescents are also indicated in this study. A 12-country study demonstrates that experiencing some or a lot of fast-paced and highly competitive school environment (in comparison to none or a little school pressure) was associated with a decrease in sleep duration of 4.56 min per day and an increase in sleep onset difficulties of 0.32, respectively (17). Based on this study as well as previous research, we speculate that the difference may be due to students in key schools suffering from a high academic burden and test stress, placing them under a high level of psychological stress that may aggravate the sensitization of the sleep system and lead to heightened alertness, physiological arousal, and difficulty in falling asleep (18).
It is known that lifestyles have an effect on sleep health. In the current study, unhealthy living and behavioral characteristics include excessive daytime sleepiness, unhealthy sleep habits, eating before sleep, social media usage (screen time per day during school, frequency of using electronics 30 min before bedtime, using electronic products in the bedroom), and co-sleeper negatively impacting on sleep health.
Our study result shows that activities related to electronic products or media exposure before bedtime increased the incidence of sleeping problems in children and teenagers and found that one in five adolescents or children were classed as very high users, the crowd of using electronics 30 min before bedtime everyday. With the popularity of electronic products or media, the proportion of users who own mobile phones increased, which has caused a series of critical health problems (19–21). Accumulating studies for the past 10 years suggested that students who had used electronic products or inculcated media habits before bedtime had made easily sleep health worse than others (12, 22, 23). Consistent with these studies, Akçay demonstrated that as teenagers in Konya High School spent more time on their social media, their sleep quality become progressively worse (24). The decrease in self-reported sleep duration was also noted among U.S. adolescents from 2009–2015, which correlated with new media screen time (25). More than 50% of adolescents in our study had electronic products or media such as computers, iPad, cellphone, or television in their bedrooms. Continente demonstrated that adolescents with media devices in their bedrooms were more likely to be short sleepers (26). Through electronic products or media (computer, Internet, smartphone, et al.) usage, teenagers often play games, watch movies, TV series, or entertainment shows, chat online, or do other activities. These activities, a stimulus for brain stimulating neurons contributed to increasing the occurrence of adverse sleep outcomes in students. Moreover, as long time use a screen at night, the eyes of students are exposed to strong light, and its blue spectrum has a strong and specific effect on the retina (27). Light can not only prevent the secretion of melatonin leading to circadian rhythm disorder but also cause the desire of awakening to delay sleep (28). Besides, some adolescents reported having difficulties disengaging from social media to sleep (29).
About 19.9% of the current sample had co-sleeper, which associate negatively with sleep healthSince co-sleepers may do more activities, such as talking and playing before going to bed or make sleeping environment noisy, sleep problems are prone to come out easily in students sharing bed or room (30), which makes it easier for students to fall into the unhealthy habit of sleep. Of course, this result was influenced by the age of the participant. Younger people are likely to have co-sleepers because of parental care. With the increase of age, the number of co-sleepers decreases, but some co-sleeping occurred due to the family's economic situation. Meanwhile, our results also show unhealthy sleep habits such as getting up late in the morning, staying up late, and doing energetic exercise before bed, were related to sleep health. Furthermore, excessive daytime sleepiness is related significantly to sleep health. We suspect if a student is drowsy during the day, there will be fragmentation of night sleep and increased sleep pressure, which will affect night sleep. Our findings suggest that food intake preceding sleep has a negative impact on sleep health, consistent with previous studies (31, 32). A previous study showed snacking and drinking caffeinated beverages before going to bed were associated with significantly short sleep duration and poorer sleep quality (OR = 1.49 and 1.83, respectively) (33).
Relationships with families and peers also appeared to play a pivotal role in sleep health. Because home and school are the two places in which students' lives are mainly involved, students who received more social support from family and friends reported greater life satisfaction. According to previous research, for children and adolescents, higher psychosocial well-being was linked to longer nocturnal sleep duration and lower levels of sleep disturbances (34). In our study, students who are satisfied with their family life/classmates relationships sleep better. The hypothalamic-pituitary-adrenal axis was activated with the release of hormones that affect sleep architecture due to enduring stress (35) which in childhood can emerge from various sources like problems with the family and peers (36).
In the current study, fluctuation of emotions is an important factor for unhealthy sleep, which is consistent with previous studies (37, 38). Emotion and sleep are closely linked and many studies have shown that heightened emotional reactivities including strong positive and negative emotions are related to the maintenance of insomnia symptoms (39). According to previous studies, affective processes mediate the effect of cognitive and autonomic hyperarousal on sleep (40). Sleep problems are confirmed to be associated with decreased levels of vagal suppression, which is considered indices of emotion regulation. Additionally, higher levels of emotional intensity tied in with reduced sleep duration and increased nocturnal activity (41). However, the relationship between mood and sleep is complex and bidirectional because poor emotions can worsen sleep and vice versa (42), further research is needed.
To data, comparable data on sleep deprivation among children and adolescents in Fujian is limited, but our study adds relevant research evidence in this aspect. Furthermore, another strength of the current study is a Cross-sectional study of a relatively large sample size and comprehensive assessments of a series of sleep health variables, which make us research the potential factors influencing sleep. However, several limitations should be noted. The first is that causality will be difficult to demonstrate in a cross-sectional design, although there are multiple theories to support our findings. Second, the current research does not include factors such as family structure and socioeconomic status, school timetable, and parents' sleeping habits, which may be significantly related to the sleep health of Chinese students. Moreover, as a result of graduation having heavy academic stress, the last-year students (grades 6, 9, and 12) were not included in investigation. And we haven't considered the effect of students taking sleeping pills for the time being and have not excluded it. Although the sampling method takes into account regional economic development, however, the randomly selected areas appear to be unevenly distributed geographically.
Overall, this study found that a series of factors are significantly associated with adverse sleep outcomes among children and adolescents. The results of the study have valuable clinical significance as our findings indicated that the existing sleep problem in children and teenagers could be, at least partly, intervened by reducing the use of electronic products before bedtime, especially cellphone, by avoiding mood swings frequently and by improving the routine habit before bedtime. Based on our results, we recommend the combination of school with family intervention, and parents, teachers, health professionals, and students should raise awareness of developing healthy sleep habits in usual life, which may be more effective in improving students' sleep health.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Designed and modified the manuscript: SWe and SWu. Designed the research and participated in the experimental design, coordinated and drafted the manuscript, data collection, achievement interpretation, and manuscript writing: XX, FZ, YC, JL, and ZZ. Analyzed the data: XX and YC. All authors have read and agreed to the published version of the manuscript.
This research was funded by Joint Funds for the Innovation of Science and Technology, Fujian Province (2018Y9089), the Natural Science Foundation of Fujian Province (2019J01315), Professor Development Fund Project of Fujian Medical University (JS15002), Investigation and comprehensive exploration of intervention strategies on obesity and nutritional status of primary and middle school students in Fuzhou (2019B011), and Fujian Provincial hospital-high level hospital construction program (2018-GSP-001).
We thank the participants and participating physicians for their participation in this study. We are especially grateful to the staffs of First Affiliated Hospital of Fujian Medical University and Fujian Medical University Union Hospital, China for making this research possible. This research received no specific grant from any funding agency, commercial or not for profit sectors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.924741/full#supplementary-material
1. Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. (2011) 12:110–8. doi: 10.1016/j.sleep.2010.11.008
2. Gariepy G, Danna S, Gobina I, Rasmussen M, Gaspar de Matos M, Tynjälä J, et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 European and North American countries. J Adolesc Health. (2020) 66:S81–8. doi: 10.1016/j.jadohealth.2020.03.013
3. Xu T, Liu J, Zhu G, Han S. Prevalence and associated lifestyle factors of suboptimal health status among chinese children using a multi-level model. Int J Environ Res Public Health. (2020) 17:1497. doi: 10.3390/ijerph17051497
4. Blackwell CK, Hartstein LE, Elliott AJ, Forrest CB, Ganiban J, Hunt KJ, et al. Better sleep, better life? How sleep quality influences children's life satisfaction. Qual Life Res. (2020) 29:2465–74. doi: 10.1007/s11136-020-02491-9
5. Orchard F, Gregory AM, Gradisar M, Reynolds S. Self-reported sleep patterns and quality amongst adolescents: cross-sectional and prospective associations with anxiety and depression. J Child Psychol Psychiatry. (2020) 61:1126–37. doi: 10.1111/jcpp.13288
6. Liu X, Liu Z, Liu B, Sun S, Jia C. Associations between sleep problems and ADHD symptoms among adolescents: findings from the Shandong Adolescent Behavior and Health Cohort (SABHC). Sleep. (2020) 43(6):zsz294. doi: 10.1093/sleep/zsz294
7. Kracht CL, Chaput J, Martin CK, Champagne CM, Katzmarzyk PT, Staiano AE. Associations of sleep with food cravings, diet, and obesity in adolescence. Nutrients. (2019) 11:2899. doi: 10.3390/nu11122899
8. von Schnurbein J, Boettcher C, Brandt S, Karges B, Dunstheimer D, Galler A, et al. Sleep and glycemic control in adolescents with type 1 diabetes. Pediatr Diabetes. (2018) 19:143–9. doi: 10.1111/pedi.12538
9. Yildiz E, Sac R, Işik Ü, Özaydin MS, Taşar MA, Cakir I, et al. Comparison of the sleep problems among adolescents who attempted suicide and healthy adolescents. Nerv Ment Dis. (2020) 208:294–8. doi: 10.1097/NMD.0000000000001122
10. Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. (2014) 37:9–17. doi: 10.5665/sleep.3298
11. Huang MM, Qian Z, Wang J, Vaughn MG, Lee YL, Dong GH. Validation of the sleep disturbance scale for children and prevalence of parent-reported sleep disorder symptoms in Chinese children. Sleep Med. (2014) 15:923–8. doi: 10.1016/j.sleep.2014.03.023
12. Li X, Tai J, Xu Z, Wang G, Wu Y, Du J, et al. Sleep duration and factors related to sleep loss in 3-14-year-old children in Beijing: a cross-sectional survey. Chin Med J. (2018) 131:1799–807. doi: 10.4103/0366-6999.237403
13. James S, Chang AM, Buxton OM, Hale L. Disparities in adolescent sleep health by sex and ethnoracial group. SSM Popul Health. (2020) 11:100581. doi: 10.1016/j.ssmph.2020.100581
14. Barclay NL, Gregory AM. Sleep in childhood and adolescence: age-specific sleep characteristics, common sleep disturbances and associated difficulties. Curr Top Behav Neurosci. (2014) 16:337–65. doi: 10.1007/978-3-662-45758-0_239
15. Palmer CA. Tired teens: sleep disturbances and heightened vulnerability for mental health difficulties. J Adolesc Health. (2020) 66:520–1. doi: 10.1016/j.jadohealth.2020.01.023
16. Kim J, Noh JW, Kim A, Kwon YD. Demographic and socioeconomic influences on sleep patterns among adolescent students. Int J Environ Res Public Health. (2020) 17:4378. doi: 10.3390/ijerph17124378
17. Vandendriessche A, Ghekiere A, Van Cauwenberg J, De Clercq B, Dhondt K, DeSmet A, et al. Does sleep mediate the association between school pressure, physical activity, screen time, and psychological symptoms in early adolescents? A 12-country study. Int J Environ Res Public Health. (2019) 17:4378. doi: 10.3390/ijerph16061072
18. Kalmbach DA, Anderson JR, Drake CL. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. (2018) 27:e12710. doi: 10.1111/jsr.12710
19. Scott H, Biello SM, Woods HC. Social media use and adolescent sleep patterns: cross-sectional findings from the UK millennium cohort study. BMJ Open. (2019) 9:e031161. doi: 10.1136/bmjopen-2019-031161
20. Felix E, Silva V, Caetano M, Ribeiro MVV, Fidalgo TM, Rosa Neto F, et al. Excessive screen media use in preschoolers is associated with poor motor skills. Cyberpsychol Behav Soc Netw. (2020) 23:418–25. doi: 10.1089/cyber.2019.0238
21. Kelleghan AR, Leventhal AM, Cruz TB, Bello MS, Liu F, Unger JB, et al. Digital media use and subsequent cannabis and tobacco product use initiation among adolescents. Drug Alcohol Depend. (2020) 212:108017. doi: 10.1016/j.drugalcdep.2020.108017
22. Royant-Parola S, Londe V, Tréhout S, Hartley S. The use of social media modifies teenagers' sleep-related behavior. Encephale. (2018) 44:321–8. doi: 10.1016/j.encep.2017.03.009
23. Xie YJ, Cheung DS, Loke AY, Nogueira BL, Liu KM, Leung AY, et al. Relationships between television viewing, computer and mobile phone usage and sleep quality in a Chinese population: a community-based cross-sectional study. Med Internet Res. (2020) 22:18095. doi: 10.2196/18095
24. Akçay D, Akçay BD. The influence of media on the sleep quality in adolescents. Turk J Pediatr. (2018) 60:255–63. doi: 10.24953/turkjped.2018.03.004
25. Twenge J.M., Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009-2015 and association with new media screen time. Sleep Med. (2017) 39:47–53. doi: 10.1016/j.sleep.2017.08.013
26. Continente X, Pérez A, Espelt A, López MJ. Media devices, family relationships and sleep patterns among adolescents in an urban area. Sleep Med. (2017) 32:28–35. doi: 10.1016/j.sleep.2016.04.006
27. Behar-Cohen F, Martinsons C, Viénot F, Zissis G, Barlier-Salsi A, Cesarini J, et al. et al. Light-emitting diodes (LED) for domestic lighting: any risks for the eye? Prog Retin Eye Res. (2011) 30:239–57. doi: 10.1016/j.preteyeres.2011.04.002
28. Cajochen C, Frey S, Anders D, Späti J, Bues M, Pross A, et al. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. J Appl Physiol. (2011) 110:1432–8. doi: 10.1152/japplphysiol.00165.2011
29. Scott H, Woods HC. Fear of missing out and sleep: cognitive behavioural factors in adolescents' nighttime social media use. J Adolesc. (2018) 68:61–5. doi: 10.1016/j.adolescence.2018.07.009
30. Palmer CA, Clementi MA, Meers JM, Alfano CA. Co-sleeping among school-aged anxious and non-anxious children: associations with sleep variability and timing. J Abnorm Child Psychol. (2018) 46:1321–32. doi: 10.1007/s10802-017-0387-1
31. Khan MKA, Faught EL, Chu YL, Ekwaru JP, Storey KE, Veugelers PJ. Is it nutrients, food items, diet quality or eating behaviours that are responsible for the association of children's diet with sleep? J Sleep Res. (2017) 26:468–76. doi: 10.1111/jsr.12466
32. Crispim CA, Zimberg IZ, dos Reis BG, Diniz RM, Tufik S, de Mello MT. Relationship between food intake and sleep pattern in healthy individuals. J Clin Sleep Med. (2011) 7:659–64. doi: 10.5664/jcsm.1476
33. Galland BC, de Wilde T, Taylor RW, Smith C. Sleep and pre-bedtime activities in New Zealand adolescents: differences by ethnicity. Sleep Health. (2020) 6:23–31. doi: 10.1016/j.sleh.2019.09.002
34. Thumann BF, Börnhorst C, Michels N, Veidebaum T, Solea A, Reisch L, et al. Cross-sectional and longitudinal associations between psychosocial well-being and sleep in European children and adolescents. J Sleep Res. (2019) 28:e12783. doi: 10.1111/jsr.12783
35. Nollet M, Wisden W, Franks NP. Sleep deprivation and stress: a reciprocal relationship. Interface Focus. (2020) 10:20190092. doi: 10.1098/rsfs.2019.0092
36. Ryan-Wenger NA, Sharrer VW, Campbell KK. Changes in children's stressors over the past 30 years. Pediatr Nurs. (2005) 31:282–8.
37. van Kooten JAMC, Maurice-Stam H, Schouten AYN, van Vuurden DG, Granzen B, Gidding C, et al. High occurrence of sleep problems in survivors of a childhood brain tumor with neurocognitive complaints: the association with psychosocial and behavioral executive functioning. Pediatr Blood Cancer. (2019) 66:e27947. doi: 10.1002/pbc.27947
38. Medda E, Alessandri G, Delfino D, Fagnani C, Ferri M, Violani C, et al. Adolescents self-reported sleep quality and emotional regulation: a discordant twin study. Ann Ist Super Sanita. (2019) 55:118–23. doi: 10.4415/ANN_19_02_03
39. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. (2010) 14:227–38. doi: 10.1016/j.smrv.2009.10.007
40. Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. (2002) 53:215–43. doi: 10.1146/annurev.psych.53.100901.135243
41. El-Sheikh M, Buckhalt JA. Vagal regulation and emotional intensity predict children's sleep problems. Dev Psychobiol. (2005) 46:307–17. doi: 10.1002/dev.20066
Keywords: sleep health, children and adolescents, factors, sleep habits, Fuzhou
Citation: Xu X, Zheng F, Cai Y, Lin J, Zeng Z, Wei S and Wu S (2022) Sleep health and its related influencing factors in primary and middle school students in Fuzhou: A large multi-center cross-sectional study. Front. Public Health 10:924741. doi: 10.3389/fpubh.2022.924741
Received: 20 April 2022; Accepted: 13 July 2022;
Published: 04 August 2022.
Edited by:
Xia Jiang, Karolinska Institutet (KI), SwedenReviewed by:
Cynthia S. T. Wu, Hong Kong Polytechnic University, Hong Kong SAR, ChinaCopyright © 2022 Xu, Zheng, Cai, Lin, Zeng, Wei and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shichao Wei, d2Vpc2MwNTA2QDE2My5jb20=; Siying Wu, Zm11d3N5QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.